Evaluation of M-Health On Medication Adherence In Tuberculosis Patients: A Systematic Review
Rd. Mustopa1*, Damris2, Syamsurizal2, M. Dwi Wiwik Emawati2
1Department of Medical Laboratory Technology, Health Polytechnic of Jambi, Jambi, Indonesia
2Doctoral Study Program, Faculty of Mathematics and Natural Sciences, Jambi University, Jambi, Indonesia
Corresponding author. Rd. Mustopa, JL. Haji Agus Salim Nomor 09 Kota Baru – Jambi 36361, Indonesia.
Orcid : https://orcid.org/0000-0002-6407-1452.
Phone: +62 821-9668-7959
Email: rdmustopa979@gmail.com
Cite this article
ABSTRACT
Background & Aim: The success of the TB control program is closely related to patient adherence to treatment. Previous studies have provided many views regarding the use of variants of mHealth on TB patient adherence, but the results still need to be clarified. This review aims to evaluate and provide an overview of mHealth RCTs on medication adherence in the patient with tuberculosis.
Methods & Materials: The PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guideline was followed to report study findings. A literature search for studies in the period of 2018-2022 in PubMed, Cochrane, CINAHL and Sciencedirect databases was conducted. Randomized controlled trials (RCTs) that analyzed the effect of mHealth on medication adherence outcomes (treatment completion, treatment adherence, missed doses, and non-completed rate) were included. Adult patients with either active or latent TB infection were included. The Cochrane ’Risk of bias’ assessment tool was used to assess the risk of bias of eligible studies.
Result: Overall, searches on databases generated 2,607 articles, and only 18 articles met the criteria. Two authors independently screened and extracted data from eligible studies. There are two devices used in mHealth in the last five years: software (SMS, We chat, and Whatsapp) and hardware (MERM, eDOT, WOT). Based on descriptive analysis, the hardware mHealth is superior to the software mHealth. Close monitoring and measurement of the use of DOT hardware demonstrates the accuracy of treatment success.
Conclusion: It was found that mHealth interventions can be an advantageous approach. However, the interventions showed variable effects regarding the direction of effect and the rate of improvement of TB treatment adherence and clinical outcomes.
Keywords: Tuberculosis; eHealth; digital health; Adherence; digital adherence.
INTRODUCTION
Tuberculosis is a disease that requires the sufferer’s adherence to a standardized treatment program to completely get rid of Mycobacterium, which is the main cause of this disease, from the sufferer’s body [1–3]. A total of 1.6 million people died from TB in 2021 (including 187,000 people living with HIV). Worldwide, TB is the 13th leading cause of death and the second infectious killer after COVID-19 (above HIV/AIDS). TB is a treatable and curable disease. Drug-susceptible TB disease is treated with a standard 4-month or 6-month course of 4 antimicrobial drugs (isoniazid and rifampicin) that are provided with support to the patient by a health worker or trained treatment supporter [4]. The high number of TB cases worldwide is part of patient non-adherence with treatment programs, which allows for an increase in new TB cases [5]. Non-adherence of TB patients to treatment can be seen from the large number of TB patients who are resistant to standard therapy or what is known as Drug Resistant-Tuberculosis (DR-TB). There are 157,903 Drug Resistant-Tuberculosis (DR-TB) cases in 2020 [6]. To overcome this situation, since 1995 WHO has introduced the DOTs (Directly Observed Treatment, Short-course) strategy. The study states that knowledge is the biggest variable in this aspect of non-adherence, without neglecting other variables such as attitudes and behaviour of TB patients [7]. For this reason, the focus of TB control should be on increasing compliance and changing patient behaviour [8].
The World Health Organization (WHO) has provided a good strategy for managing TB, primarily targeting patient compliance, which has long been known as Directly Observed Treatment (DOT). The strategy consisted of standard treatment using Rifampicin for six months for new cases and eight months for repeat cases [9]. These repeat cases were patients who had dropped out of treatment or failed to undergo previous treatment [10,11]. So, the DOT strategy and program are fine. This strategy requires a better approach and is adapted to the conditions of society. The limitations of the officers who will run this program should be a consideration for the birth of innovations to find which approach is better to do to significantly improve and change the compliance and behaviour of TB patients [12,13]. The birth of a very progressive digital technology that began in the 20th century can be the main choice in solving the problem of treating tuberculosis in the community through innovations in delivering pre-existing programs [14]. In several decades, studies on the use of digital technology to improve TB patient adherence and behaviour have increased sharply in various parts of the world.
The term commonly known today for using mobile devices to support public health care and practice is ‘mHealth, as introduced by WHO. mHealth also includes all mobile devices that use wireless or Bluetooth technology [9]. mHealth is particularly suitable for adherence interventions, as it involves using devices such as smartphones, Personal Digital Assistants (PDAs), tablets and many others [15–18]. These devices support several media, such as Short Messaging Services (SMS) or text messaging, voice or video calls, and specialized software applications (Apps) [15]. Previous studies involving mHealth included Liu and his team, who used a telephone reminder system to increase TB patient compliance [11]. In addition, there are studies using media SMS to serve as reminders for TB patients with good results [19–21].
Based on our initial search of the available studies, the results still need to be clarified. There are no results that show the certainty of the effectiveness of mHealth used. In addition, most of the studies over the five years showed that mHealth variations were similar. Likewise, previous review studies evaluate a lot from just one mHealth variant. To that end, the current review aims to evaluate and provide an overview of mHealth RCTs on medication adherence in the patient with tuberculosis.
METHODS
Design
This review was compiled based on the 2020 Preferred Reporting Items for Systematic-review and Meta-Analysis (PRISMA) guidelines [22].
Eligibility Criteria
This review was restricted to studies published in English, and included studies published through 2018 to 2023. Study types were limited to RCTs. In this review, an intervention for adherence and behaviour were defined as any strategy (e.g., self-management for diseases, and medication reminder) to change or maintain patient’s adherence and behaviour to improve health. We included studies on interventions that used mobile devices (wireless and portable electronics including cellular phones, wearable devices, laptop, personal assistance devices, and tablet PC) or mobile technologies (any technologies that enable communication with remote areas, such as phone call, video call, short messaging service [SMS], multimedia messaging service, online-chat, and email) to promote medication adherence. Observational study, non-intervention study, case report, study protocol, and commentary were excluded in this review.
Information Source
A literature search was performed on several reputable databases, such as PubMed, Sciencedirect, CINAHL, and Cochrane. The search was carried out in the period November 2022 to January 2023.
Search Strategy
The keyword structure was compiled based on study population, intervention, comparison, outcome, and design were developed for the specific databases used. The search strategies for each database provided in the search string table (Table 1).
Selection Process
Two authors independently screened all titles and abstracts from the collected literature. Then read the entire text of each article to assess its eligibility based on predetermined inclusion criteria. Discrepancies that arise are resolved through discussion, even if it is possible to ask for the consideration of the first author. The selection process is described in detail in the PRISMA diagram.
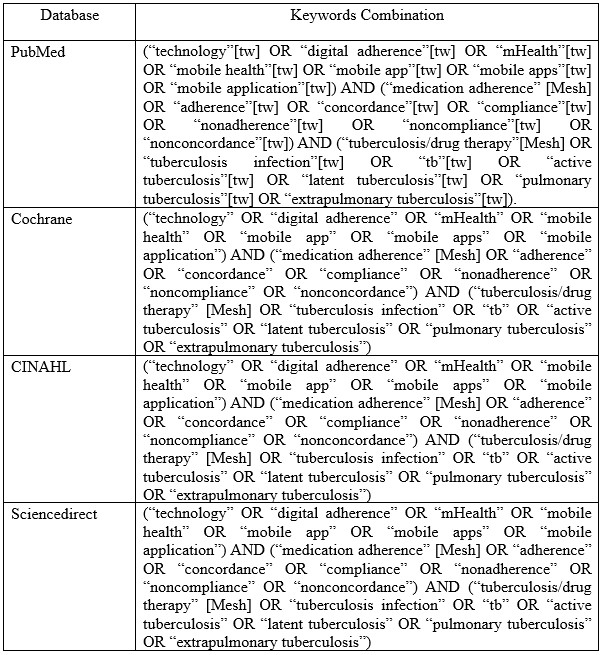
Table 1. Search string in databases
Data Extraction
DM and SR conducted eligibility evaluation based on the title and abstract. The full texts of potentially eligible articles were retrieved and assessed by DM, SR and MD conducted further independent verification of the abstract and full-text screening. Any disagreements among the reviewers were resolved by discussion. Data from the selected articles were extracted by DM, SR, MD and then verified by RM for relevant information, such as publication year, type of mHealth intervention, setting, population, main findings, and control groups.
Assessment of risk of bias in included studies
Two review authors independently assess the risk of bias of each included trial using the Cochrane ’Risk of bias’ assessment tool, and discuss any differences of opinion (Higgins et al., 2011). In the case of missing or unclear information, we will contact the trial authors for clarification. The Cochrane approach assesses risk of bias across six domains: sequence generation and allocation concealment (selection bias), blinding of participants and personnel (performance bias), blinding of outcome assessors (detection bias), incomplete outcome data (attrition bias), selective outcome reporting (reporting bias), and other potential biases. For each domain we will record the methods used by the trial authors to reduce the risk of bias and assign a judgment of either ’low’, ’high’, or ’unclear’ risk of bias.
RESULTS
Overall search on databases resulted in a total of 2,607 articles. After removing 2070 articles for duplication, ineligibility and other reasons, 537 articles were left ready for screening. In the end, 18 articles were declared eligible to be included in this review study after removing 16 articles for reasons including not being an RCT study, not being focused on TB, and being a protocol study.
In full regarding the process of searching for articles can be seen in figure 1, while, in table 2 we reported the characteristics of the articles included in our study
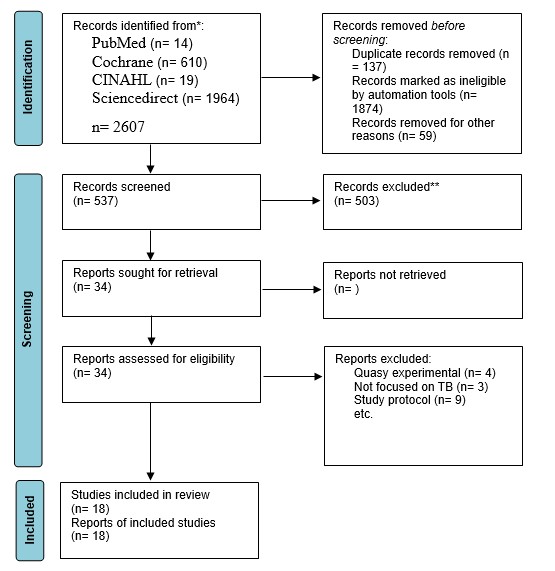
Figure 1. Flow diagram of the studies selection
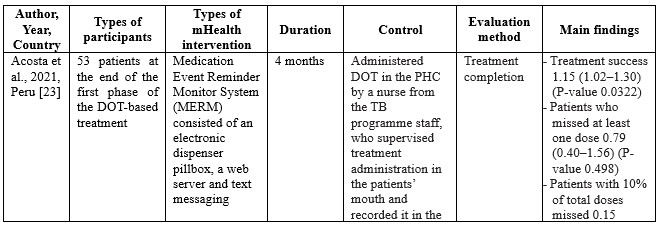

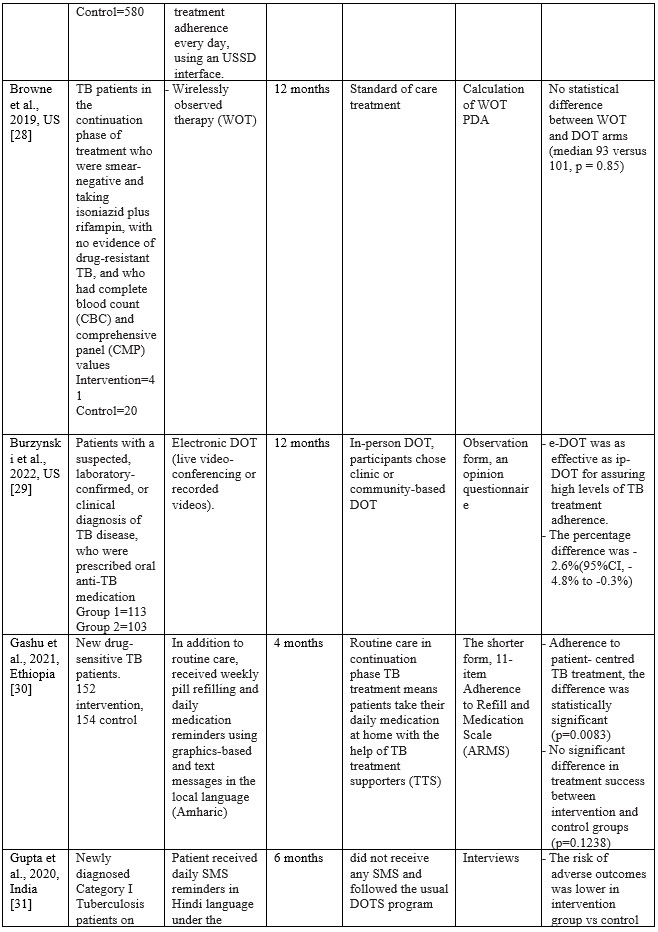
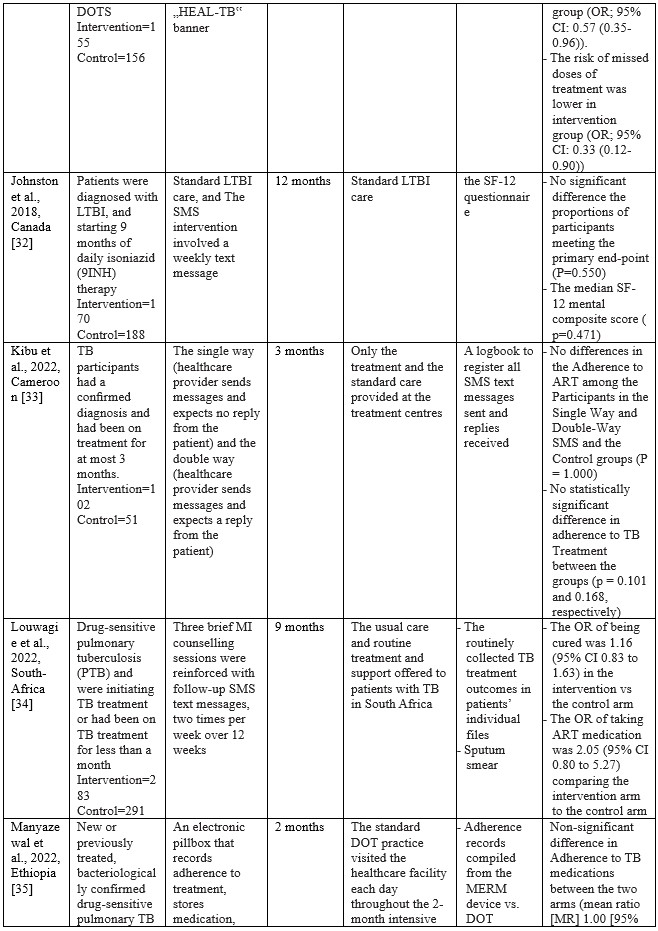
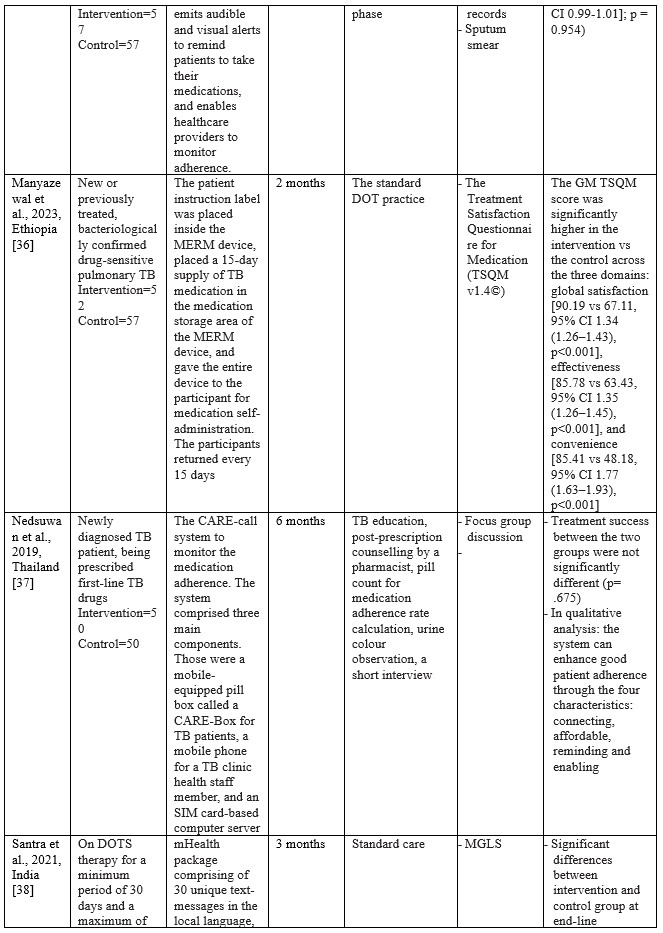

Table 2. Characteristics of Studies Included
Summary of Risk of Bias assessment
The risk of bias in eligible studies using The Cochrane Collaboration’s tool resulted in the conclusion that there were four studies with a high risk of bias and one unclear.
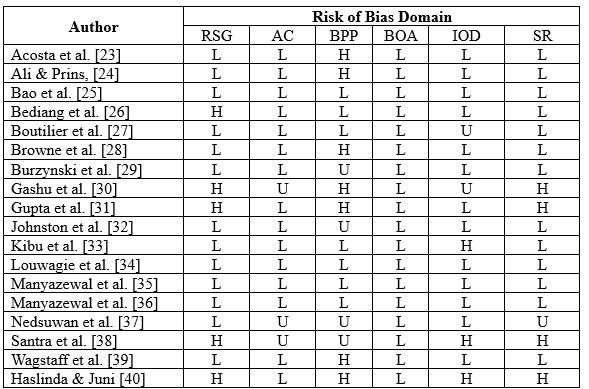
*RSG= Random sequence generation, AC= Allocation Concealment, BPP= Blinding Of Participants and Personnel, BOA= Blinding of Outcome assessment, IOD= Incomplete Outcome Data, SR= Selective Reporting; H= High risk of bias; U= Unclear risk of bias; L= Low risk of bias.
Characteristics of eligible studies
Studies on using m-health applications as innovations to improve adherence, change behaviour, and the success of TB treatment in the last decade have shown a significant increase. We have collected 18 RCT studies from several countries, including Ethiopia (n=3), South Africa (n=2), India (n=2), Cameroon (n=2), US (n=2), and one study each in Thailand, Peru, Sudan, China, Kenya, Canada, and Malaysia. The number of TB patients included in the study ranged from 61 to 1,189, ranging from 18 to 60 years. Most of the studies involved participants newly diagnosed with TB based on positive bacteriology, On DOTS therapy, smears, negative pulmonary tuberculosis (PTB), being prescribed first-line TB drugs, and drug-sensitive pulmonary tuberculosis (PTB). The shortest duration of intervention given was two months, and the longest was 12 months.
m-Health intervention used
Based on the collected studies, the applications used include Short Messages Service (SMS), Medication Event Reminder Monitor System (MERM), WeChat groups, USSD interface, Wirelessly observed therapy (WOT), Digital Adherence Technologies (DATs), Electronic DOT (live video-conferencing or recorded videos), The CARE-call system, and TB@Clicks (Whatsapp).
Several m-Health collected from eligible studies can be broadly grouped into software and hardware applications. In general, m-health applications that use software provide information as reminders and TB education in writing or pictures. Through the SMS route, various interventions are carried out, starting every day, every two days, twice a week, and every week [24,26,27,31–34,38,39]. Through the We-Chat application, there is no time limit for interactions between patients and supervisors taking medication; at any time, patients can discuss all obstacles and questions with supervisors and fellow patients [25]. As for the Whatsapp application, studies report that in the intensive phase, reminders are given to patients every day and 1 to 3 months after the intervention package is carried out [40]. Through telephone calls, patients are also reminded and controlled by supervisors. The duration of each phone call is 10 minutes [24,38].
The hardware used in the intervention includes the Medication Event Reminder Monitor System (MERM), which is a pillbox dispenser that will sound an alarm at the set time to take medicine [23,35,36]. This model is similar to another system called CARE box; it is just that, in this system, when the lid of the box is opened, it will automatically make a missed call to the server [37]. Another device is Wirelessly Observed Therapy (WOT), a sensory device that enters the body to record what the patient consumes, including TB drugs. The data stored on the sensor is linked to a mobile device as information material for supervisors [28]. For E-DOT, a camera device records real-time video of the patient’s medication-taking activities; this system is also used to conduct video conferencing between supervisors and patients [29].
Effects of m-Health on TB patient adherence
In summary, m-Health, with its various variants, has a positive effect in that patients experience increased adherence and changes in behaviour, even though this is not stated explicitly. Several studies have found a positive effect on treatment success related to patient adherence, with P values of 0.0322 [23,24], 0.88 [26], 0.001 [27], 0.85 [28], 0.1238 [30], 0.782 [31], 0.550 [32], 0.101 [33], 0.443 [34], 0.954 [35], 0.001 [36], 0.675 [37], 0.005 [38], 0.03 [40]. Meanwhile, changes in patient behaviour can be seen in findings such as increased self-management behaviour with a P value <0.001 [25], lower risk of missed doses [31], taking ART medication with an OR value 2.05 [34], return to the clinic with a P value of 0.001 [39].
Comparisons between the intervention and control groups in all studies showed no significant differences. However, the intervention using the m-Health variant showed superiority compared to the control group, most of which were in the main form of standard care, Directly Observation Treatment (DOT).
Using MERM, TB patient adherence to treatment is higher than the DOT standard, where TB patients are 1.15 times more compliant when intervened with MERM than the DOT standard [23]. The patients in the SMS intervention group had a lower failure rate (6.8%; 5 of 74 patients) compared to the control group (10.8%; 8 of 74 patients) [24]. In a study conducted by Bediang and colleagues using m-Health in the form of SMS, treatment success was higher in the intervention group compared to the control group (111 patients: 106 patients) [26]. Using SMS messages daily and an unstructured supplementary services data (USSD) interface shows that the probability of unsuccessful treatment outcomes for individuals in the intervention group is approximately 0.08 less than for individuals in the control group [41]. Browne and colleagues found that WOT was superior to DOT in supporting confirmed daily adherence to TB medications, where (3,738 out of 4,022) prescribed doses were confirmed in the WOT treatment, significantly different (p < 0.001) from the 63.1% (1,202 out) of 1,904) of prescribed doses observed in the DOT arm [28]. One hundred seventy-three patients completed the treatment program through the DOT electronic intervention [29]. One hundred ten patients out of a total of 139 TB patients adhered to treatment after intervention using a Mobile phone-based weekly refilling with a daily medication reminder system [30]. Gupta and colleagues found that the treatment success rates in the intervention group using SMS reminders were 86.4%, and the control group was 76.2% [42]. Louwagie and colleagues found that after six months of text SMS intervention, 120 of 133 patients adhered to the TB treatment given [34]. Manyazewal and colleagues using MERM found seven patients completed treatment compared to the control group of 5 [35]. Nedsuwan and colleagues found that using the mobile-based CARE-call system, the number of non-adherence patients in the intervention group was significantly lower than that of the control group (7.5% vs. 27.5%) [37]. Santra and colleagues found that the proportion of participants adherent to DOTS in the intervention group using phone calls and text messages increased from 85.5% at baseline to 96.4% at endline, postintervention [38]. Wagstaff and colleagues found that using SMS messages, as many as 62.0% of patients returned to the clinic in two days compared to 51.5% in the control group [39]. Using the Whatsapp message intervention, Haslinda and Juni found that the number of respondents who adhered to medication was higher in the group that received the intervention (81.8%) compared to the control group (69.1%) [40].
DISCUSSION
This systematic review study aims to evaluate and provide an overview of mHealth RCTs on medication adherence in the patient with tuberculosis which we have successfully conducted by collecting eighteen eligible studies from 2018 to 2022. One of the reasons we limited our literature search to the last five years was to see application innovations that were used along with the development of the digital world in this period. The expectancy is that the latest technological advances in this digitalization era will make it more straightforward to develop information innovations, especially concerning the health sector, to educate patients and the public.
Since the emergence of digital devices, health practitioners are increasingly competing to take advantage of this progress as a good opportunity to help improve public health in preventive and curative ways. M-Health has been attracting attention since it emerged as an innovation that effectively streamlines interactions between healthcare workers and patients, especially in supervising patients such as TB with strict rules for taking drugs for a certain duration. With a relatively lower cost, m-Health can be the first choice in addition to existing programs for monitoring TB patients. For this reason, this study provides an overview of the effectiveness of the m-Health variant from RCT studies in the 2018 to 2022 period regarding adherence and behaviour changes in TB sufferers during the treatment period. The m-Health variants used in the study are software and hardware. This review study analyzed m-Health variants that were not discussed in several previous systematic reviews [43–46].
The m-Health used in the last Five years
Until the last five years, SMS is still an option to remind TB patients to take their medicine. In contrast to previous review studies [45,46], the effectiveness of SMS in monitoring the treatment of TB patients in this review showed no significant difference between the SMS intervention group and the control group with standard care using DOT. Even using the Whatsapp application, TB patient compliance did not show any significance, even though adherence to treatment in the intervention group was higher than the control group [40]. However, with the widespread use of cellphones with the Android system or iPhone Operating System (iOS) among the public, choosing intervention using SMS or chat remains the best choice considering the low cost and efficient application. In contrast to the findings of Bao and colleagues in China, the We-Chat application used as an intervention showed a significant increase in adherence and repeat visits to the clinic during a TB treatment program [25]. Besides the effectiveness of existing smartphone-based applications, various obstacles can be faced, especially for populations in remote areas, where cellular networks and even the internet may be inadequate, especially if the quality of the patient’s cell phone does not support the use of these applications [47].
Behaviours expected of TB sufferers include not spitting, covering the nose and mouth when coughing or sneezing, and wearing a mask [48]. Of course, TB sufferers expect this behaviour to be carried out as one of the steps to prevent the spread of the disease in the surrounding environment [49]. However, the family should be involved in education on the prevention and care of TB patients. The family has an important role in the patient’s treatment process, including preventing the spread of the disease so that it does not affect the people who live in the same house and the people around the house. Families can provide arrangements at home according to good health standards, especially for TB patients. For this reason, further studies need to analyze this educational intervention for families with TB sufferers.
Some of the studies included in this review also provide interventions using a variety of hardware such as the Medication Event Reminder Monitor System (MERM), CARE box, Wirelessly Observed Therapy (WOT), and Electronic-Directly Observation Treatment (E-DOT). These devices are under recommendations from the World Health Organization (WHO) to increase the adherence of TB patients undergoing six months of treatment [14]. Of the six studies that implemented these hardware devices, overall, they showed better success than using software on TB patient adherence to taking medication. The MERM system allows TB patients to take medication daily because the device cover will open at a predetermined time [23]. Manyazewal and the team also used a MERM system with a tool called evriMED500, in the form of a pillbox consisting of a medicine container and an electronic module connected to an indicator light and an alarm [35,36]. The MERM system in the study did not show superiority over the standard care of the control group. However, it should be recognized that the adherence dimension has many independent variables that may play a large role in influencing interventions. Unfortunately, the study of the use of the MERM system that we found did not carry out an analysis of the potential factors. So that bias in the study is likely to occur.
Another device used is Wirelessly Observed Therapy (WOT), a sensory device that enters the body through the mouth. A patch detector in the torso area will read all sensor activity. The data recorded from the patch detector is transmitted wirelessly via Bluetooth technology to mobile phones, computers, or other gadgets [50]. Browne stated that WOT is very safe to apply without significant side effects, only in the form of minimal irritation due to the direct use of patches on the skin [28]. Statistically, WOT is superior to DOT; in other words, WOT is effective in increasing TB patient adherence to treatment. However, the application of WOT is likely to be constrained, especially in countries with lower middle incomes, because this technology is still relatively expensive, and there are suggestions to replace the patch every five days to avoid irritation [28]. Previous studies have also confirmed that using WOT can increase adherence to antiviral HCV therapy in populations at high risk of non-adherence [51].
Another hardware option we found in one study was the use of e-DOT in real-time or recorded video, depending on patient preference [29]. Real-time video allows patients to interact directly with TB program officers with the help of Skype software. Burzynski and colleagues found that e-DOT is similar to in-person-DOT but has equal effectiveness. For this reason, e-DOT can be applied according to the patient’s choice. Especially during a pandemic such as COVID-19, electronic DOT is the best choice to reduce the spread and worsen TB patients’ conditions, as found by Lippincott and colleagues in implementing the Vdot COVID-19 pandemic where this method has high effectiveness and is the first choice. In contrast, in-person DOT is recommended to be carried out later [52]. Haberer and Subbaraman added that implementing eDOT might encounter technical challenges, inaccuracies, costs, and an unsupportive health system [47].
The potential of mHealth on TB patient adherence
Compliance of TB patients with the treatment program can be seen from the success of the treatment. Of the various types of mHealth that we collected, almost all showed an increase in adherence of TB sufferers to the treatment given. Although, comparison with the control group mostly showed insignificant differences.
The use of SMS text generally shows more potential than the DOT standard. Two studies show that compliance with TB patients using SMS text interventions is similar to DOT standards [32,33]. The study states that there may be several factors that influence the failure of TB patient compliance even though they have been reminded via SMS messages, including the lack of more personalized engagement, the didactic nature of the messages, and the SMS message is received when the patient was not near his/her medication all contributed to the failure to reduce poor adherence [53]. For this reason, in the future, this can be a consideration in implementing interventions using text SMS, where controlling these situations is essential to consider. However, based on the success of increasing adherence from studies using text SMS, it was stated that patient compliance was one time greater than the DOT standard. The same thing was also found in the use of Whatsapp, where significant treatment success occurred in TB patients who were given education through messages via Whatsapp [40].
The medication event reminder monitor (MERM) system in studies using it also shows positive potential to improve TB patient adherence to treatment. In addition, using MERM can also reduce the workload of health workers [54]. One problem identified using MERM is the possibility of removal of the medication from the pillbox, for example, for work-related reasons, which prevents the recording of pill dispensing. Although the potential of MERM is not superior to in-person DOT, MERM can be used as an alternative to improve TB patient compliance. The identical thing is also found in using electronic DOT and WOT. This hardware allows stricter supervision and accurate recording of each drug-taking activity so that health workers can more easily measure treatment success.
LIMITATION
The limitations encountered in this review include limited access to several reputable databases, which does not allow us to explore further relevant articles. In addition, this review includes studies of low to high quality due to the small number of articles we have collected. For this reason, writers who want to use the results of this review must be careful and analyze them more carefully.
CONCLUSION
This review shows that using m-Health can be the first choice in handling TB cases with the DOT strategy. Hardware as part of mHealth has more potential to increase TB patient adherence and behaviour change. TB patient compliance with medication programs and stopping the spread of TB through good behaviour will be very significant in reducing TB cases, recurrent cases and new cases. mHealth is the best choice as a companion to the ongoing DOT program, primarily as a medium for disseminating information needed by patients during their treatment period. In the era of digitalization today and in the future, mHealth is undoubtedly the main route in health services, as illustrated during the pandemic of certain diseases that did not allow face-to-face meetings. However, further efficacy studies at the clinical level are needed, while always protecting privacy.
REFERENCES
- Acharya B, Acharya A, Gautam S, Ghimire SP, Mishra G, Parajuli N, et al. Advances in diagnosis of Tuberculosis: an update into molecular diagnosis of Mycobacterium tuberculosis. Molecular biology reports. 2020;47:4065–75.
- Asriati A, Kusnan, Adius, Alifariki L. Faktor Risiko Efek Samping Obat dan Merasa Sehat Terhadap Ketidakpatuhan Pengobatan Penderita Tuberkulosis Paru. JURNAL KESEHATAN PERINTIS (Perintis’s Health Journal). 2019;6(2):134–9.
- Putri S, Alifariki LO, Fitriani F, Mubarak M. The Role of Medication Observer And Compliance In Medication Of Pulmonary Tuberculosis Patient. Jurnal Kesehatan Prima [Internet]. 2020 Feb 29;14(1). Available from: http://jkp.poltekkes-mataram.ac.id/index.php/home/article/view/248
- World Health Organization (WHO). Tuberculosis [Internet]. 27 October 2022. 2022. Available from: https://www.who.int/news-room/fact-sheets/detail/tuberculosis
- Harding E. WHO global progress report on tuberculosis elimination. The Lancet Respiratory Medicine. 2020;8(1):19.
- Dean AS, Auguet OT, Glaziou P, Zignol M, Ismail N, Kasaeva T, et al. 25 years of surveillance of drug-resistant tuberculosis: achievements, challenges, and way forward. The Lancet Infectious Diseases. 2022;
- Ghozali MT, Murani CT. Relationship between knowledge and medication adherence among patients with tuberculosis: a cross-sectional survey. Bali Medical Journal. 2023;12(1):158–63.
- Asriati A. Faktor Risiko Ketidakpatuhan Pengobatan Penderita Tuberkulosis Paru di Kota Kendari. Jurnal Keperawatan Terapan (e-Journal). 2019;5(2):103–10.
- World Health Organization. Digital health for the End TB Strategy: an agenda for action. World Health Organization; 2015.
- El Emeiry F, Shalaby S, El-Magd GHA, Madi M. Treatment outcomes of tuberculosis among new smear-positive and retreatment cases: a retrospective study in two Egyptian governorates. The Egyptian Journal of Chest Diseases and Tuberculosis. 2019;68(3):274.
- Ying R, Huang X, Gao Y, Wang J, Liu Y, Sha W, et al. In vitro Synergism of Six Antituberculosis Agents Against Drug-Resistant Mycobacterium tuberculosis Isolated from Retreatment Tuberculosis Patients. Infection and Drug Resistance. 2021;3729–36.
- Margineanu I, Louka C, Vincenti-Gonzalez M, Saktiawati AMI, Schierle J, Abass KM, et al. Patients and medical staff attitudes toward the future inclusion of ehealth in tuberculosis management: perspectives from six countries evaluated using a qualitative framework. JMIR mHealth and uHealth. 2020;8(11):e18156.
- Zhang J, Yang Y, Qiao X, Wang L, Bai J, Yangchen T, et al. Factors influencing medication nonadherence to pulmonary tuberculosis treatment in tibet, china: a qualitative study from the patient perspective. Patient preference and adherence. 2020;1149–58.
- World Health Organization. Handbook for the use of digital technologies to support tuberculosis medication adherence. World Health Organization; 2017.
- Hamine S, Gerth-Guyette E, Faulx D, Green BB, Ginsburg AS. Impact of mHealth chronic disease management on treatment adherence and patient outcomes: a systematic review. Journal of medical Internet research. 2015;17(2):e52.
- Bartels SL, Van Knippenberg RJM, Dassen FCM, Asaba E, Patomella A-H, Malinowsky C, et al. A narrative synthesis systematic review of digital self-monitoring interventions for middle-aged and older adults. Internet interventions. 2019;18:100283.
- He Q, Zhao X, Wang Y, Xie Q, Cheng L. Effectiveness of smartphone application–based self‐management interventions in patients with type 2 diabetes: A systematic review and meta‐analysis of randomized controlled trials. Journal of advanced nursing. 2022;78(2):348–62.
- Zhu MM, Choy BNK, Lam WWT, Shum J. Randomized control trial of the impact of Patient Decision Aid (PDA) developed for Chinese primary open-angle glaucoma patients. Ophthalmic Research. 2023;
- Hirsch-Moverman Y, Daftary A, Yuengling KA, Saito S, Ntoane M, Frederix K, et al. Using mHealth for HIV/TB treatment support in Lesotho: enhancing patient–provider communication in the START study. Journal of acquired immune deficiency syndromes (1999). 2017;74(Suppl 1):S37.
- Mohammed S, Glennerster R, Khan AJ. Impact of a daily SMS medication reminder system on tuberculosis treatment outcomes: a randomized controlled trial. PloS one. 2016;11(11):e0162944.
- Farooqi RJ, Ahmed H, Ashraf S, Zaman M, Farooq S, Farooqi JI. Feasibility and acceptability of Mobile SMS reminders as a Strategy to improve drugs adherence in TB Patietns. Pakistan Journal of Chest Medicine. 2017;23(3):93–100.
- Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. International Journal of Surgery. 2021;88:105906.
- Acosta J, Flores P, Alarcon M, Grande-Ortiz M, Moreno-Exebio L, Puyen ZM. A randomised controlled trial to evaluate a medication monitoring system for TB treatment. The International Journal of Tuberculosis and Lung Disease. 2022;26(1):44–9.
- Ali AOA, Prins MH. Mobile health to improve adherence to tuberculosis treatment in Khartoum state, Sudan. Journal of Public Health in Africa. 2019;10(2).
- Bao Y, Wang C, Xu H, Lai Y, Yan Y, Ma Y, et al. Effects of an mHealth intervention for pulmonary tuberculosis self-management based on the integrated theory of health behavior change: randomized controlled trial. JMIR public health and surveillance. 2022;8(7):e34277.
- Bediang G, Stoll B, Elia N, Abena J-L, Geissbuhler A. SMS reminders to improve adherence and cure of tuberculosis patients in Cameroon (TB-SMS Cameroon): a randomised controlled trial. BMC public health. 2018;18:1–14.
- Boutilier JJ, Yoeli E, Rathauser J, Owiti P, Subbaraman R, Jónasson JO. Can digital adherence technologies reduce inequity in tuberculosis treatment success? Evidence from a randomised controlled trial. BMJ Global Health. 2022;7(12):e010512.
- Browne SH, Umlauf A, Tucker AJ, Low J, Moser K, Gonzalez Garcia J, et al. Wirelessly observed therapy compared to directly observed therapy to confirm and support tuberculosis treatment adherence: a randomized controlled trial. PLoS medicine. 2019;16(10):e1002891.
- Burzynski J, Mangan JM, Lam CK, Macaraig M, Salerno MM, deCastro BR, et al. In-person vs electronic directly observed therapy for tuberculosis treatment adherence: A randomized noninferiority trial. JAMA Network Open. 2022;5(1):e2144210–e2144210.
- Gashu KD, Gelaye KA, Lester R, Tilahun B. Effect of a phone reminder system on patient-centered tuberculosis treatment adherence among adults in Northwest Ethiopia: a randomised controlled trial. BMJ Health & Care Informatics. 2021;28(1).
- Gupta A, Bhardwaj AK, Singh H, Kumar S, Gupta R. Effect of ‘mHealth’Interventions on adherence to treatment and outcomes in Tuberculosis patients of district Shimla, Himachal Pradesh, India: A Randomised Control Trial. Indian Journal of Preventive & Social Medicine. 2020;51(3):125–36.
- Johnston JC, van der Kop ML, Smillie K, Ogilvie G, Marra F, Sadatsafavi M, et al. The effect of text messaging on latent tuberculosis treatment adherence: a randomised controlled trial. European Respiratory Journal. 2018;51(2).
- Kibu OD, Siysi VV, Albert Legrand SE, Asangbeng Tanue E, Nsagha DS. Treatment Adherence among HIV and TB Patients Using Single and Double Way Mobile Phone Text Messages: A Randomized Controlled Trial. Journal of Tropical Medicine. 2022;2022.
- Louwagie G, Kanaan M, Morojele NK, Van Zyl A, Moriarty AS, Li J, et al. Effect of a brief motivational interview and text message intervention targeting tobacco smoking, alcohol use and medication adherence to improve tuberculosis treatment outcomes in adult patients with tuberculosis: a multicentre, randomised controlled tri. BMJ open. 2022;12(2):e056496.
- Manyazewal T, Woldeamanuel Y, Holland DP, Fekadu A, Marconi VC. Effectiveness of a digital medication event reminder and monitor device for patients with tuberculosis (SELFTB): a multicenter randomized controlled trial. BMC medicine. 2022;20(1):310.
- Manyazewal T, Woldeamanuel Y, Getinet T, Hoover A, Bobosha K, Fuad O, et al. Patient-reported usability and satisfaction with electronic medication event reminder and monitor device for tuberculosis: a multicentre, randomised controlled trial. eClinicalMedicine. 2023;56:101820.
- Ratchakit-Nedsuwan R, Nedsuwan S, Sawadna V, Chaiyasirinroje B, Bupachat S, Ngamwithayapong-Yanai J, et al. Ensuring tuberculosis treatment adherence with a mobile-based CARE-call system in Thailand: a pilot study. Infectious Diseases. 2020;52(2):121–9.
- Santra S, Garg S, Basu S, Sharma N, Singh MM, Khanna A. The effect of a mhealth intervention on anti-tuberculosis medication adherence in Delhi, India: A quasi-experimental study. Indian Journal of Public Health. 2021;65(1):34.
- Wagstaff A, Van Doorslaer E, Burger R. SMS nudges as a tool to reduce tuberculosis treatment delay and pretreatment loss to follow-up. A randomized controlled trial. PLoS One. 2019;14(6):e0218527.
- Haslinda N, Juni MH. Effectiveness of health education module delivered through Whatsapp to enhance treatment adherence and successful outcome of tuberculosis in Seremban district, Negeri Sembilan, Malaysia. International Journal of Public Health and Clinical Sciences. 2019;6(4):145–59.
- Boutilier JJ, Jónasson JO, Yoeli E. Improving tuberculosis treatment adherence support: the case for targeted behavioral interventions. Manufacturing & Service Operations Management. 2022;24(6):2925–43.
- Das Gupta D, Patel A, Saxena D, Koizumi N, Trivedi P, Patel K, et al. Choice‐Based Reminder Cues: Findings From an mHealth Study to Improve Tuberculosis (TB) Treatment Adherence Among the Urban Poor in India. World Medical & Health Policy. 2020;12(2):163–81.
- Laksono EB, Johan A, Erawati M. The Utilization of Mobile-Health Intervention In Improving Treatment Compliance Behavior In Tuberculosis Patients. Nurse and Health: Jurnal Keperawatan. 2022;11(2):275–86.
- Shariful IM. Theories applied to m-health interventions for behavior change in low-and middle-income countries: a systematic review. Telemedicine and e-Health. 2018;
- Nglazi MD, Bekker L-G, Wood R, Hussey GD, Wiysonge CS. Mobile phone text messaging for promoting adherence to anti-tuberculosis treatment: a systematic review. BMC infectious diseases. 2013;13(1):1–16.
- Sarabi RE, Sadoughi F, Orak RJ, Bahaadinbeigy K. The effectiveness of mobile phone text messaging in improving medication adherence for patients with chronic diseases: a systematic review. Iranian Red Crescent Medical Journal. 2016;18(5).
- Haberer JE, Subbaraman R. Digital technology for tuberculosis medication adherence: promise and peril. Vol. 17, Annals of the American Thoracic Society. American Thoracic Society; 2020. p. 421–3.
- Lucya V. Prevention of Tuberculosis: Literature Review. KnE Life Sciences. 2021;630–4.
- Lönnroth K, Roglic G, Harries AD. Improving tuberculosis prevention and care through addressing the global diabetes epidemic: from evidence to policy and practice. The lancet Diabetes & endocrinology. 2014;2(9):730–9.
- Hafezi H, Robertson TL, Moon GD, Au-Yeung K-Y, Zdeblick MJ, Savage GM. An ingestible sensor for measuring medication adherence. IEEE Transactions on Biomedical Engineering. 2014;62(1):99–109.
- Bonacini M, Kim Y, Pitney C, McKoin L, Tran M, Landis C. Wirelessly observed therapy to optimize adherence and target interventions for oral hepatitis C treatment: observational pilot study. Journal of Medical Internet Research. 2020;22(4):e15532.
- Lippincott CK, Perry A, Munk E, Maltas G, Shah M. Tuberculosis treatment adherence in the era of COVID-19. BMC infectious diseases. 2022;22(1):800.
- Liu X, Lewis JJ, Zhang H, Lu W, Zhang S, Zheng G, et al. Effectiveness of electronic reminders to improve medication adherence in tuberculosis patients: a cluster-randomised trial. PLoS medicine. 2015;12(9):e1001876.
- Wang N, Zhang H, Zhou Y, Jiang H, Dai B, Sun M, et al. Using electronic medication monitoring to guide differential management of tuberculosis patients at the community level in China. BMC infectious diseases. 2019;19(1):1–9.
![]() This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
EFFECT OF GUIDED EDUCATION ON PERCEPTION AND ATTITUDE OF CHILDBEARING WOMEN TOWARDS CAESAREAN SECTION IN NIGERIA
Mary Idowu Edward1*, Oluwaseun Segun Bolarinwa2,
Omowumi Suuru Ajibade3, Temilola Mabel Aregbesola4
1,2,3, Department of Adult and Mental Health Nursing, Faculty of Nursing Science, University of Medical Sciences, Akure Campus, Akure, Ondo State,
4Basic Health Center Iloro, Akure, South, Ondo State, Nigeria
Corresponding Author: Mary Idowu Edward RN, RM, RNE, PhD. Nursing. Department of Adult and Mental Health Nursing, Faculty of Nursing Science, University of Medical Sciences, Akure Campus, Akure, Ondo State. Email: edwardmary@unimed.edu.ng
Cite this article
ABSTRACT
Background: Nigerian women are unwilling to have a Caesarean section because of the general belief that abdominal delivery is a reproductive failure on their part regardless of the feasibility of vaginal birth after Caesarean section and the decreasing mortality from Caesarean sections.
Aim: The primary objective of this study was to investigate the existence of a significant relationship between pregnant women’s knowledge and attitudes toward cesarean delivery before and after training.
Materials and Methods: The study employed a pre/post-test study design, using questionnaires to obtain data from 152 childbearing women attending antenatal in Iloro Basic Health Centre, Akure, Ondo State. Descriptive statistics were used to summarize and present data. Associations between variables were tested using Spearman correlation at a p-value 0.05 level of significance.
Results: The researcher found a significant relationship between the knowledge and attitude of pregnant women towards Caesarean section delivery before and after the training. The findings revealed an increase in the knowledge of mothers after the educational intervention, mothers would opt for a Caesarean section if it is necessary to protect them and the baby and they believe that it is a woman’s right to choose a Caesarean section for herself. Significant relationship exists between knowledge and attitudes toward the Caesarean section.
Conclusion: It was concluded that childbearing mothers still believe that vagina delivery is a natural delivery and there is joy attached to it, however, most women would still prefer vagina delivery to Caesarean section. The study recommends a need for awareness programs to enhance women’s and the community positive perception towards the Caesarean section in Nigeria.
Keywords: Guided Education, Perception, Attitude, Childbearing women, Caesarean Section
Introduction
Worldwide, Caesarean section accounts for about 15% of births. Caesarean section is one of the oldest procedures in obstetric practice and may be a necessary end in the termination of pregnancy to abort or minimize complications to the mother, foetus, or both [1]. At the onset, the operation was associated with high morbidity and mortality rates, largely because of the low level of medical science available at the time [2]. This type of surgery has been in existence throughout medical history and has steadily progressed from being one that is totally fatal to one that is safe for both the mother and the foetus [1]. In developed countries, the operation of Caesarean section has become well established with ease and safety, hence there is a lure for the procedure with women opting for it, increasingly for non-medical reasons [3]. It is the most commonly performed major obstetric operation in the world and there is no doubt that it has contributed to improved obstetric care throughout the world [4]. In Africa, the cesarean section is usually performed when a vaginal birth is deemed hazardous either to the foetus or the mother [5].
Available evidence pertaining to the population-based prevalence of Caesarean section in Nigeria reveals a threshold that is, far below the 10% recommended by the WHO [5]. Moreover, there has been no significant increase in the population-based Caesarean section rates for several years in Nigeria [7]. For instance, in 2008, merely 2% of births were delivered through a Caesarean section in Nigeria, and the rate remained unchanged in 2013. This is considerably low and suggests unmet needs which may contribute to poor maternal and neonatal outcomes in the country [5].
Interestingly, pregnant women’s perception of Caesarean section has been an essential consideration for providers of healthcare in the USA [7]. One of the major reasons is that a positive perception can lead to an effective adaptation to the maternal role whiles a negative perception can leave women with a sense of failure, loss of control, personal disappointment, and a cause to distrust their personal abilities as childbearing women, hence the need to promote positive perceptions in Caesarean section related issues [8]. For a healthy women population, the choice of delivery option is an important decision [9]. In developing countries, the negative perception of Caesarean section has led to the under utilization of the procedure[9]. Although there are many who consider the Caesarean section to be either safe or unsafe, more costly than the normal vaginal delivery, and more prone to complications than the SVD, there are some African women who perceive a Caesarean section to be a sign of female infidelity, a “curse,” or a “failure of womanhood”.
In a study carried out to assess the attitude of women toward a Caesarean section in Nigeria, it was found that vaginal delivery was the preferred mode of delivery by 93% of the respondents while 7% preferred a Caesarean section as the mode of delivery [11]. Expectant parents make many choices which usually include the site for delivery and the choice between spontaneous vaginal delivery and Caesarean section [10]. The reasons for this choice are being a natural process, being good for the mother’s health, and safety, and being an easy process [12]. Most of the women thought that Caesarean delivery can lead to long-term ill effects on the mother’s health. All the women who preferred elective Caesarean delivery initially said that they would rather opt for painless labour and vaginal delivery if offered over Caesarean section [11].
Nonetheless, the world health body emphasizes the need for Caesarean section service provision to every woman in need of it regardless of the prevailing population-based rates [13]. When medically indicated, Caesarean section has the potential for reducing maternal/neonatal mortalities and morbidities including delivery complications such as obstetric fistula [14]. However, a non-medically indicated Caesarean section has no associated additional benefits for mothers and newborns, rather like any surgery, it carries both short-term and/or long-term health risks [14]. Some studies have been conducted on Caesarean section utilization in Nigeria including a survey that examined the perception of pregnant women and found that a high proportion of the study participants were averse to Caesarean section delivery [5]. Significant associations between Caesarean section and parity, maternal weight, child’s birth weight, and previous Caesarean section were reported in another study [13]. However, it is not strange to hear many pregnant women ventilating the wrong attitude toward Caesarean section as an alternative method of birth [15]. In Nigeria, a number of women believe a Caesarean section is a last resort used to deliver pregnant women of their babies, many will even say, being told that they are going to deliver their babies through a Caesarean section is like giving a death warrant [13].
Traditionally, Nigerian women are unwilling to have a Caesarean section because of the general belief that abdominal delivery is a reproductive failure on their part regardless of the feasibility of vaginal birth after Caesarean section and the decreasing mortality from Caesarean sections. Inaccurate cultural perception about Caesarean section delivery accounts for the poor attitude of women towards Caesarean section [5]. Only one-third of women demonstrate a positive attitude towards Caesarean delivery as against 95.5% for vaginal delivery in the same group of respondents. The study concluded no significant differences in attitude and knowledge scores according to women’s levels of education [16]. It is necessary to note that the issue of vaginal birth is not only peculiar to developing countries but also to some developed countries. Women still choose vaginal birth after having a Caesarean section even in the case of postdates slated for elective Caesarean section. Hence, it is imperative to educate the average pregnant woman irrespective of her level of education and parity on Caesarean section. Therefore, this study assessed the effect of guided education on the perception and attitude of childbearing women toward Caesarean section.
Objectives of the study
- The primary objective of this study was to investigate the existence of a significant relationship between pregnant women’s knowledge and attitudes toward cesarean delivery before and after training.
- The secondary objective of the study was to describe the levels of knowledge and attitude of childbearing mothers about cesarean section before and after the educational intervention and the factors for not accepting cesarean section as a mode of delivery among women.
Hypothesis
HO1: There is no significant relationship between the knowledge and attitude of pregnant women towards Caesarean section delivery before and after the intervention.
Materials and Methods
Study Design, Population, and Area
The study utilized a quasi-experimental pre/post-test design. This design was adopted by the researcher because it will help to ascertain the effect of guided education on the perception and attitude of childbearing women towards Caesarean section in Basic Health Center Iloro, Akure South Local Government Area. The research setting for this study is Basic Health Center Iloro, Akure South Local Government Area. The head-quarter of Akure South Local government area is Akure town. Akure is a city in southwestern Nigeria and the capital of Ondo State. The metro area population of Akure in 2022 was 717,000 a 3.76% increase from 2021 which was 691,000[17]. Basic Health Center Iloro is a step above your ordinary health center, they make the provision of primary health care a full package. Health professionals and caregivers are available to give postnatal care.
The population of this study was composed of childbearing women attending the antenatal clinic in Basic Health Center Iloro, Akure South Local Government Area. The study population was randomly selected.
Sample Size Estimation, Sampling Technique, Data, collection, and Analysis
To estimate the minimum number n of childbearing women to investigate the effect of guided education on the perception and attitude toward Caesarean section, we considered the Gaussian theory [18]:
where N is the population size from which the sample size was defined. It resulted that the minimum estimated sample size of childbearing women required for a survey of a population of 255 mothers is equal to 143. It is evaluated, considering a z-score at 95%, an error e = 10% and hypothesizing a prevalence p equal to 70% about the impact of guided education. In addition to reduce statistical biases connected to information/data loss the sample size is enlarged to 152 mothers.

Instruments
The research instrument used was developed ad hoc, considering an extensive search of empirical studies on caesarian sections and was administered before and after the nurse-led education [9,19,21,22,23]. The instrument has the following sections: Demographic characteristics of the respondents (7 items), knowledge of childbearing mothers on caesarean section (8 items), perception of the childbearing mother towards the caesarean section (7 items) and the attitude of a childbearing mother towards the caesarean section (10 items), and factors for not accepting caesarean section as the mode of delivery among the women (8 items). The reliability test of the instruments was Cronbach’s alpha value of 0.83. The demographic, knowledge and factor data were scored using frequency and percentage while perception and attitude data were scored using 3 point likert scale of Agree, Not Sure and Disagree while factors data was obtained using 5 likert scale of strongly agree, agree, Not Sure, disagree and stongly disagree.
Procedure for data collection
The data was collected over a period of 4 weeks. All pregnant women were qualified to be included in the study hence need to randomly select about 20 manageable women during the antenatal visit (two Antenatal clinics per week) out of more than 60 attendance to prevent disruption of antenatal clinic activities and efficiency in data collection. The selected 20 women having been informed about the study and consent gained were administered the pretest. The education intervention which is already prepared materials on what Caesarean section is, when is it needed, types, and how to prepare for a Caesarean section are included in the module of training. The questionnaires were administered at the end of the intervention, that is, post-test.
Statistical analysis
Descriptive analysis like percentages and frequency tables were used to present the summary of the data, Cronbach’s alpha was utilised to test reliability of the instrument and Spearman correlation was used to test the hypotheses – relationship between knowledge and attitude at a 0.05 level of significance. Data were analyzed using the statistical package for social sciences (SPSS) version 20. The knowledge variable was defined by assigning points based on the affirmative response of Yes or No. For example if the number of participants who has correct answer to the questions is below 50%, 1point is assigned, if they are between 50-75% 2 points is assigned while 3points is assigned for participants between 76-100%. The maximum obtainable points of 8 knowledge items is 24 points while the minimum is 8 points. Therefore knowledge is graded thus: 1-8(Low knowledge).9-16 (Medium knowledge) while 17-24 (High Knowledge). The Perception and attitude were scored based on 3 points likert scales thus: Agree(3), Disagree (2) and Not Sure (1). the maximum obtainable score for Perception (7 items) is 21 and the minimum is 7. The maximum obtainable scores for attitude is 30 while the minimum is 10. Factors questionaires were graded on 5 points likert scales. The maximum obtainable mark is 35 while the minimum is 7.
Ethical considerations
Letter of introduction and intention of the study was taking to the Primary Health Care Authority and written permission was obtained. The study is not an invasive study, no formal approval by the Local Ethics Committee was required for this study hence no protocol number was indicated on the letter but the reference number PHCA/AK-S/020/124. However, the participants informed consent were obtained and willingness to participate was expressed before inclusion in the study. All participants were assured anonymity and confidentiality.
Results
Table 1 revealed the socio-demographic characteristics of the respondents.
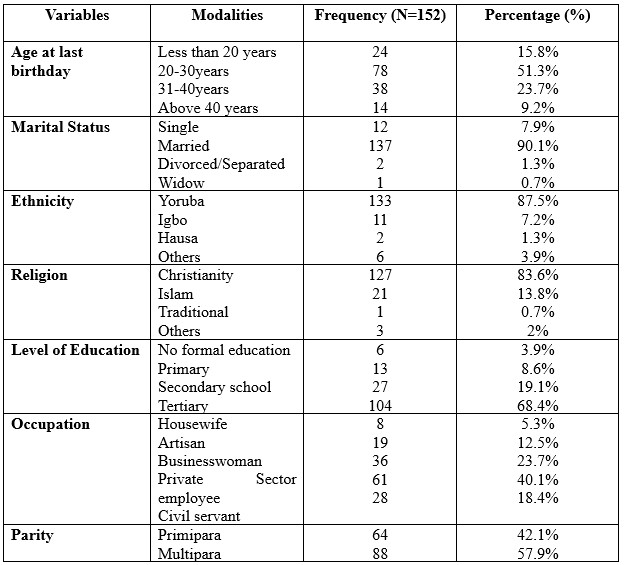
Table 1. Socio-demographic characteristics of the 152 respondents.
The respondents are 152 in number. Of the 152 respondents, 51.3% of the participants fall in the
age group between 20-30 years, and 90.1% are married. 87.5% are Yoruba and 83.6% are Christians. Findings further showed that 68.4% had tertiary education, 40.1% were private sector employees and 57.9% were multipara.
Table 2 above shows the knowledge of childbearing mothers on Caesarean section. Before the intervention, the participants had medium knowledge, that is, the score of 16 which is 66.7% of the responses from study participants while after the intervention, the participants had high knowledge of Caesarean section, that is, the score of 24 which is (100%) of obtainable knowledge scores.
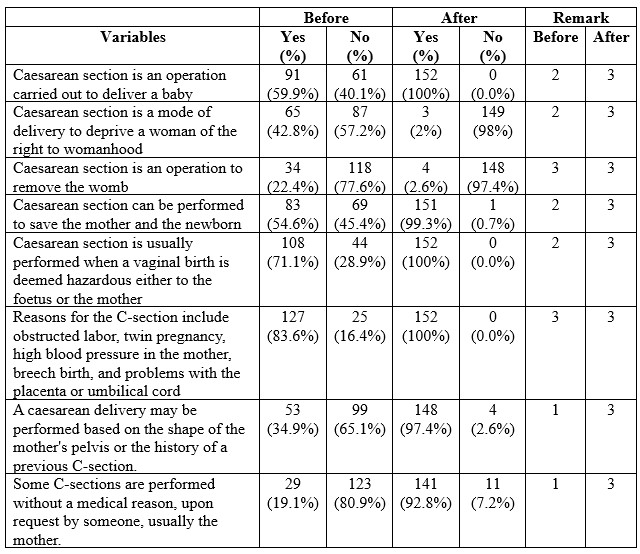
Table 2. Knowledge of 152 childbearing mothers on Caesarean section
Table 3 below shows the perception of childbearing mothers toward Caesarean section. The training improves the perception of mothers toward Caesarean as a method mode of delivery. All the respondents (100%) stated that vaginal delivery is a natural and acceptable mode of delivery.
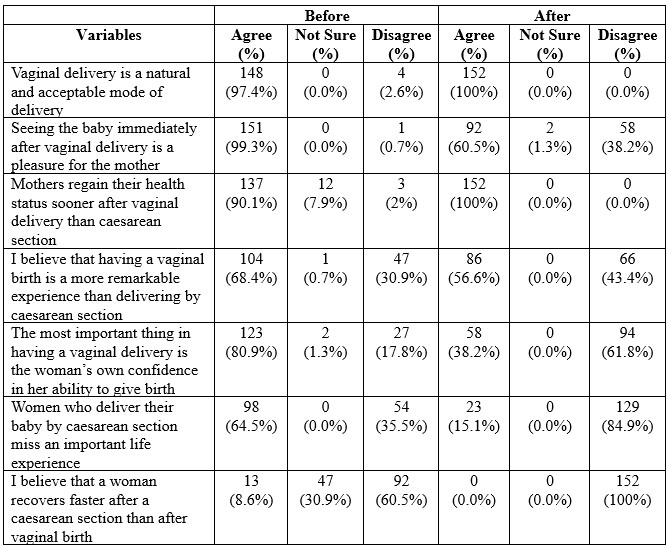
Table 3. Perception of 152 childbearing mothers toward Caesarean section.
Table 4 below shows the attitude of childbearing mothers towards Caesarean section as the accepted mode of delivery among women. Before the training, many mothers had negative attitudes towards Caesarean but this improves after the training.
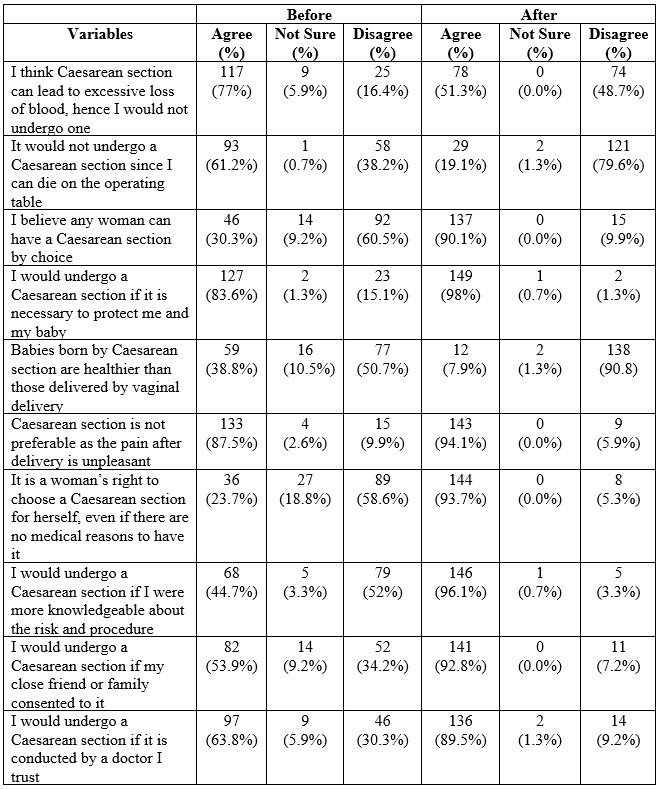
Table 4. The attitude of 152 childbearing mothers towards Caesarean section.
Table 5 above shows factors for not accepting Caesarean section as the mode of delivery among women. The women stated that fear of death, fear of pain, cost of the operation, cultural belief, being a subject of ridicule by friends, husband disapproval, and religion for not accepting Caesarean section as the mode of delivery among the women.
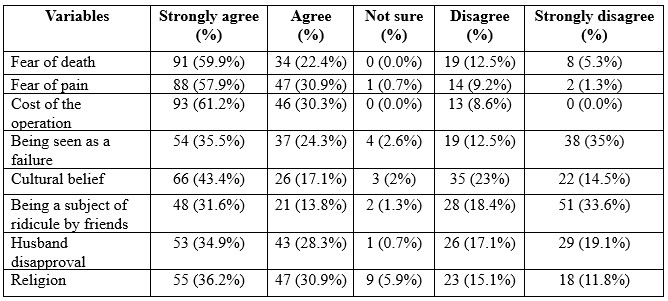
Table 5. Factors for not accepting Caesarean section as the mode of delivery among 152 women.
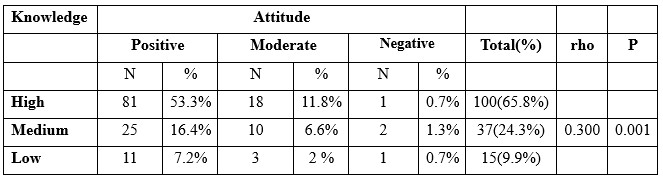
Table 6. Spearman correlation between knowledge and attitude of pregnant women towards caesarean section delivery.
Spearman correlation analysis test was carried out to determine the relationship between knowledge and attitudes, obtained p < 0.001 indicating that p <0.05. H0 is rejected and H1 is accepted, it can be concluded that there is a significant relationship between knowledge and attitude of pregnant women towards caesarean section delivery. It is found that rho = 0.300 and the direction of positive correlation (+). It can be concluded that the strength of the correlation between knowledge and attitude is low, which means that even though in this study there is a significant relationship between the two variables, there are still many factors that influence knowledge and attitude. The results of this study also show a positive correlation direction (+), which means that the relationship between knowledge and unidirectional attitude – meaning that the higher one’s knowledge, the better the attitude.
Discussion of findings
The discussions made on the findings of this study are presented in accordance with the research questions. The sub-headings under which the discussions are provided show in specific what each research question seeks to find.
Demographic characteristics of respondents
Findings from this study revealed that the average age of the respondents is 27 years. The majority (90.1%) were married and multipara and the population were dominated by Yoruba and Christians. More than half of the respondents had tertiary education. This was similar to the study of [19] on the attitude of pregnant women in southwestern Nigeria. The findings are in line with the study of [19]on the perception and attitude of pregnant women towards Caesarean section delivery in the University of Port-Harcourt Teaching Hospital, Rivers State, in which the majority of respondents between the age group of 25-29 years, and 85.9% were married.
Knowledge of childbearing mother on Caesarean section
Based on the findings from this study, it was revealed that there was an increase in the knowledge of mothers after the educational intervention on Caesarean section. The increased level of knowledge among pregnant women may be attributed to the educational intervention and information provided during the training. This is in consonant with the study of [20,21,22] who reported that majority of the women have good knowledge about caesarean section. The study of [23] on pregnant women’s knowledge, perception, and attitudes towards the Caesarean section also showed that the majority of women had adequate knowledge and were aware of all of the factors concerning Caesarean section deliveries. This study was in contrast with the study of [24] who reported good knowledge of 17.4% on Caesarean section delivery. [25] also found that there was a low overall knowledge of mothers about the modes of delivery.
Perception of the Childbearing Mothers towards Caesarean section
The findings from this study revealed that the majority of mothers had a poor perception of a Caesarean section before the training; however, there was an increase in the mothers’ score on the perception of Caesarean section among childbearing mothers after the intervention. Childbearing mothers still believe that vagina delivery is a natural delivery and has joy attached to it, and most women still prefer it over Caesarean section[25]. The study of [27] reported that having a Caesarean section takes away from the joy of giving birth and was of the view that Caesarean section births are not natural and should be reserved for those with medical issues or those who fear pain.
The attitude of Childbearing Mothers toward Caesarean section
The findings from this study revealed improved scores in the attitude of mothers toward Caesarean section. The majority of the mothers reported that they would opt for Caesarean section if it is necessary to protect them and their babies, and they believe it is a woman’s right to choose a Caesarean section for herself, even if there are no medical reasons to have it. They were also of the opinion that Caesarean section is not preferable as the pain associated with it post-delivery is unpleasant. Although before the training majority thought Caesarean section can lead to excessive loss of blood and they could die on the operating table. This assertion corresponds to the finding of [23] who submitted that the fear of death, complications, and other negative perceptions about Caesarean section make women unwilling to opt for it. The study of [28] on perception and attitude towards Caesarean section in Niger/Delta reflected that 83.2% of mothers would accept Caesarean section if it is a necessity that will protect them and their babies [29].
Factors for not accepting Caesarean section as the mode of delivery among the women
Findings from this study revealed fear of death, fear of pain, cost of the operation, being seen as a failure, cultural belief, husband disapproval, and religion were the factors revealed by the mothers for not accepting Caesarean section as the mode of delivery. [31] listed fear of death, denial of womanhood, expensive mode of delivery, and the possibility of being exposed to insults as reasons for opposing Caesarean section for delivery. [29] stated maternal autonomy, women empowerment and gender inequality as several women often need to take permission from their husbands and/or religious leaders before making health-related decisions[29]. According to [30] women’s decision-making in consultation with relatives is the main influencer to accept elective caesarean section.
Discussion of the hypothesis
The primary objective of this study was to investigate the existence of a significant relationship between pregnant women’s knowledge and attitudes toward cesarean delivery before and after training. The secondary objective of the study was to describe the levels of knowledge and attitude of childbearing mothers about cesarean section before and after the educational intervention and the factors for not accepting cesarean section as a mode of delivery among women. Based the inferential statistics carried out in this study, it was revealed that there is a significant difference between the pre and post-intervention knowledge of Caesarean section, and pre and post-intervention attitudes of pregnant women towards Caesarean section delivery. Similarly, [32] found a significant difference between pre and post-intervention knowledge and pre and post-intervention attitudes of pregnant women to Caesarean section. Contrary to these findings, there was no significant association between knowledge about Caesarean section and respondents’ characteristics in relation to age, marital status, occupation, and previous place of delivery [33].
Conclusions
Nigerian women are unwilling to have Caesarean section because of the general belief that abdominal delivery is a reproductive failure on their part regardless of the feasibility of vaginal birth after a Caesarean section and the decreasing mortality from Caesarean sections. The primary objective of this study was to investigate the existence of a significant relationship between pregnant women’s knowledge and attitudes toward cesarean delivery before and after training. The secondary objective of the study was to describe the levels of knowledge and attitude of childbearing mothers about cesarean section before and after the educational intervention and the factors for not accepting cesarean section as a mode of delivery among women. The study revealed an increase in the mothers’ knowledge about Caesarean section after the intervention. In addition, both perception and attitude towards Caesarean section improved following the intervention. The researchers found a significant relationship between the knowledge and attitude of pregnant women towards Caesarean section delivery before and after the intervention. It was concluded that the childbearing mothers still believe that vagina delivery is a natural delivery and there is joy attached to it, most women would only agree to have Caesarean section if the need arises but they would still prefer spontaneous vagina delivery.
Recommendations
Based on the findings, the following recommendations are made:
- There is still a need for awareness programs to increase women’s and community’s understanding about Caesarean section in Nigeria.
- Our society needs further enlightenment on the advantages of antenatal care attendance and hospital deliveries as the problem is rooted in our culture.
- Local, State and Federal Governments should subside the costs of maternity services through an all-inclusive National Health Insurance Scheme. This will go a long way to encourage women to accept Caesarean section when the need arises.
Limitations
The research was carried out in just one health center (Iloro Comprehensive Health Center) in Akure Local government are of Ondo State due limited funds. Future research should utilise more facilities to enhance generalisation.
Conflicts of interest and sources of funding:
None declared. This research did not receive any specific grant from funding agencies in the public, commercial, or not for profit sectors.
Author contributions: All authors equally contributed to the conduct of this study and to preparing this article.
Acknowledgments
The authors appreciate the Management of Basic Health Centre Iloro, Akure, Ondo State, Nigeria, and all the mothers that participated in the study for their cooperation.
References
- Cunningham, F.G., MacDonald, P.C., Gant, N.F., Leveno, K.J, Gilstrap, L.C. & Hankins, G. (2017). Caesarean delivery and Caesarean In: Cunningham, et al, editors. Williams Obstetrics, 20th edition. Stamford, CF: Appleton & Lange; p. 509-31.
- Kerr-Wilson R. (2018). Caesarean section on demand. In: Current Obstetrics and Gynaecology. Harcourt Publishers: 126-28.
- Gomen, R., Tamir, A. & Degani, S. (2014). Obstetricians’ opinions regarding patient choice in caesarean delivery. Obstet Gynecol.;99(4):577 -80.
- Ohanson, R.B., EI-Timini, S., Rigby, C., Young, P. & Jones P. (2019). Caesarean section by choice could fulfi11the inverse care law. Eur J Obstet Gynecol Reprod BioI.;97(1):20-2.
- Ezeonu,P. O.. Ekwedigwe, K. C., Isikhuemen,M. E., Eliboh,M. O., Onoh, R. C., Lawani,L. O., Ajah,L. O. & Dimejesi,E. I. (2017). Perception of Caesarean Section among Pregnant Women in a Rural Missionary Hospital.Advances in Reproductive Sciences, Vol.5 No.3.
- Egwuatu, V.B. & Ezeh, I.O. (2018). Vaginal delivery in Nigeria Women after a previous section. Int J Gynaecol Obstet.;32: 1-6
- Coleman, V.H., Lawrence, H. & Schulkin, J. (2019). Rising Cesarean Delivery Rates. The Impact of Cesarean Delivery on Maternal Request. CME review article 4. ObstetGynecol survey.; 64: 2.
- Penna, L. (2014). Caesarean section on request for non-medical indications. Current Obstet. Gynaecol.; 14: 220-223.
- Naa Gandau, B.B., Nuertey, B.D., Seneadza, N.A.H. et al. Maternal perceptions about caesarean section deliveries and their role in reducing perinatal and neonatal mortality in the Upper West Region of Ghana; a cross-sectional study. BMC Pregnancy Childbirth 19, 350 (2019). https://doi.org/10.1186/s12884-019-2536-8
- Danon, D., Sekar, R., Hack, K.E & Fisk, N.M. (2013). “Increased stillbirth in uncomplicated monochorionic twin pregnancies: a systematic review and meta-analysis”. Obstetrics & Gynecology. 121 (6): 1318–26. doi: 10.1097/AOG.0b013e318292766b. PMID 23812469. S2CID 5152813.
- Onah H.E. & Ugona M.C. (2014). Preference for Caesarean section or symphysiotomy for obstructed labour among Nigerian women. IJOG 2004; 84: 70-91.
- Ezechi, O.C., Fasuba, O.B., Kalu, B.E., Nwokolo, C.A. & Obiesie, L.O. (2014). Caesarean Delivery: Why the aversion? Trop J ObstetGynaecol.; 21 (2): 164-167.
- Chigbu, C. & Iloabachie, G. (2017). The burden of Caesarean section refusal in a developing country setting. BJOG: An International Journal of Obstetrics & Gynaecology; 114: 1261 – 1265.
- Bonney, E.A. & Myers, J.E. (2015). Caesarean section: Techniques and complications. Obstet. Gynaecol Rep Med; 21(4): 97 – 102. http://.dx.doi.org/10.1016/j.ogrm.
- Etuk, S.J. & Ekanem, A.D. (2017). Socio-demographic and Reproductive Characteristics of women who default from orthodox obstetrics care in Calabar, Nigeria. Int. J. Gynaecol. Obstet; 73: 57-60.
- Awoyinka, B.S., Ayinde, O.A & Omigbodun, A.O. (2016). Acceptability of Caesarean delivery to Antenatal patients in a tertiary health facility in south west Nigeria. J Obstet Gynaecol.; 26(3); 208-210.
- United Nations – World Population Prospects: Akure, Nigeria Metro Area Population 1950-2023: -Akure – Historical Population Data https://www.macrotrends.net/cities/21978/akure/population; Retrieved 2023-03-08.
- Colton T., Statistics in Medicine. Little Brown & Co. 1974.
- Faremi, A., Ibitoye I., Olatubi M., Koledoye, P. & Ogbeye G. (2014). Attitude of pregnant women in south western Nigeria towards caesarean section as a method of birth. Int J Reprod Contracept Obstet Gynecol.;3(3):709-714. DOI: 10.5455/2320-1770.ijrcog20140970.
- Robinson-Bassey, G. & Uchegbu, J. (2017). Perception and attitude of pregnant women towards caesarean section delivery in University Of Portharcourt Teaching Hospital, Rivers State. International Journal for Research in Health Sciences and Nursing, Volume-2, Issue-4.
- Orukwowu, U. & Ene-Peter, J. (2022). The Knowledge and Attitude of Pregnant Women towards Cesarean Section in the University of Port Harcourt Teaching Hospital (UPTH). IPS Journalof Basic and Clinical Medicine, 1(3), 1–12. https://doi.org/10.54117/ijbcm.v1i3.3
- Al Sulamy, A. , Yousuf, S. & Thabet, H. (2019) Knowledge and Attitude of Pregnant Women toward Elective Cesarean Section in Saudi Arabia. Open Journal of Nursing, 9, 199-208. doi: 4236/ojn.2019.92020.
- Dorkenoo, J.E. & Abor, P.A. (2021). Pregnant women’s knowledge, perception and attitudes towards caesarian section among obstetrics unit attendants in a teaching hospital. Res. J. of Health Sci. Vol 9(3). http://dx.doi.org/10.4314/rejhs.v9i3.2.
- Saoji, A., Nayse, J., Kasturwar, N. & Reiwani, N. (2017). Women’s knowledge, perception and potential demands towards caesarean section. National Journal of Community Medicine 2(2): 244-248.
- Nusrat, N., Nisar, A. S. & Ahson, M. (2019). Knowledge, attitude and preferences of pregnant women towards modes of delivery. Journal of Liaquat University of medical and Health Sciences, 8 (3): 228-233.
- Gamble, J.A. & Creedy, D.K. (2015). Women’s preference for a caesarean section: incidence and associated factors. Birth. 28(2):101-10.
- Dorkenoo, J.E. & Abor, P.A. (2021). Pregnant women’s knowledge, perception and attitudes towards caesarian section among obstetrics unit attendants in a teaching hospital. Res. J. of Health Sci. Vol 9(3). http://dx.doi.org/10.4314/rejhs.v9i3.2.
- Sunday-Adeoye, I. & Kalu, C.A. (2011). Pregnant Nigerian women’s view of cesarean section Nigerian Journal of Clinical Practice; 14(3), 276-279.
- Abah, M.G. & Umoh, A.V. (2015). Perception and attitude towards Caesarean section by pregnant women attending antenatal clinic in a Niger Delta tertiary facility. DOI: 10.47837/CMJ.19770126.201531167.
- Bam V, Lomotey AY, Kusi-Amponsah Diji A, Budu HI, Bamfo-Ennin D, Mireku G. Factors influencing decision-making to accept elective caesarean section: A descriptive cross-sectional study. Heliyon. 2021 Aug 11;7(8):e07755. doi: 10.1016/j.heliyon.2021.e07755. PMID: 34430742; PMCID: PMC8365447.
- Adewuyi, E.O., Auta, A. & Khanal, V. (2018). Prevalence and factors associated with underutilization of antenatal care services in Nigeria: A comparative study of rural and urban residences based on the 2013 Nigeria demographic and health survey. PLoS One;13:e0197324.
- Ashimi, A.O., Amole, T.G. & Aliyu, L.D. (2013). Knowledge and attitude of pregnant Women to caesarean section in a semi-urban community in northwest Nigeria. Journal of the West African College of Surgeons; 3(2), 46-61.
- Afaya, R.A., Bam, V., Apiribu, F., Agana, V.A. & Afaya, A. (2018) Knowledge of Pregnant Women on Caesarean Section and their Preferred Mode of Delivery in Northern Ghana, NUMID HORIZON: An International Journal of Nursing and Midwifery,; 2(1), 62-73.
![]() This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
THE IMPACT OF INTRODUCING A NURSING EDUCATION PROTOCOL ON THE INCIDENCE OF CLOSTRIDIUM DIFFICILE INFECTIONS IN THE HOSPITAL ENVIRONMENT: A QUASI-EXPERIMENTAL STUDY
Darija Knežević1*, Duška Jović1 & Miroslav Petković2
1. Department of Nursing, University of Banja Luka, Faculty of Medicine, Banja Luka, the Republic of Srpska, Bosnia and Herzegovina
2. Department of Microbiology and Immunology, University of Banja Luka, Faculty of Medicine, Banja Luka, the Republic of Srpska, Bosnia and Herzegovina
* Corresponding author: Darija Knežević, 1.Department of Nursing, University of Banja Luka, Faculty of Medicine, Banja Luka, the Republic of Srpska, Bosnia and Herzegovina. E-mail: darija.a.knezevic@med.unibl.org
Cite this article
ABSTRACT
Introduction: Increased virulence of Clostridium difficile and use of antimicrobial drugs in recent years represent a challenge in the treatment of these infections in healthcare institutions. Improving the overall knowledge on prevention and control of C. difficile infections (CDI) among nurses may be one strategies to help reduce the CDI incidence rate in hospital settings.
Objective: The research objective was to develop, implement and evaluate a protocol for the prevention of CDI in hospital environment through nurses’ education.
Materials and Methods: This study utilized a quasi-experimental pretest–post-test design, which was carried out in tertiary care hospital, Banja Luka, Bosnia and Herzegovina. The educational modules contained detailed description of prevention measures to prevent CDI transmission, and C. difficile toxins in faces were identified using laboratory enzyme immunoassays.
Results: The research included 60 nurses. There was a statistically significant difference (p=0.001) in the evaluation of knowledge in relation to professional experience and education level before the intervention. Nurses showed highly significant (p<0.001) better knowledge about C. difficile and CDI prevention on the test after the education. Before the education of nurses and technicians on preventive measures, CDI incidence was 11.04 per 10,000 patient – days, and after the education 6.49.
Conclusion: The study results showed that continuous medical education about CDI can have contribute to increasing knowledge and awareness about the importance of CDI prevention.
Keywords: Clostridium difficile, infection, prevention, nurses, education.
INTRODUCTION
Hospital-associated diarrhoeas are most often the result of an infection caused by Clostridium difficile (CDI), and the prevention of these infections has public health significance. Decreasing the CDI rate is challenging due to the complex pathogenesis, a many number of colonized patients and the presence of infectious spores [1,2]. The spreading of CDI is a consequence of the uncontrolled use of antibiotics and inappropriate control of hospital-acquired infections (HAI) [3-5]. Therefore, the prevention and control of CDI in healthcare institutions nowadays requires two basic approaches: preventing horizontal spreading of C. difficile and decreasing the risk of CDI in case the infection spreads. The first approach to CDI control involves isolating the infected patient and cleaning and disinfecting the hospital environment according to the guidelines [6,7]. Another approach is to control the use of antibiotics [8,9]. Strategies and guidelines for the prevention of CDI are based on a bundle of measures or a set of data that lead to the best possible outcome. The CDI prevention bundle consists of individual elements or interventions, as it follows: diagnostic testing, empirical control, contact isolation, hand hygiene and disinfection of the hospital environment. Successful implementation of the CDI prevention bundle depends on several persons: physicians, nurses, caregivers, personnel in charge of hygiene, family members and others who are in contact with patients [10]. Considering the high incidence of CDI, healthcare professionals should be familiar with the latest guidelines in the treatment and prevention of CDI [11,12]. Faecal microbiota transplantation (FMT), also called faecal transplantation or faecal bacteriotherapy, is one of the more important, newer approaches to the treatment of CDI. FMT is the infusion of a suspension of faces from a healthy donor into the colon of the CDI patient [13,14]. Nurses have an important role in the modern approach to the treatment of CDI patients, such as FMT and primarily if those patients are housed in an intensive care unit (ICU). Enteric preventive measures and proper isolation of patients with CDI are crucial care procedures [15,16]. Nurses should be alert that after FMT, antibiotic exposure can still lead to recurrent CDI [17]. There is evidence that educational interventions improve the knowledge and practice of nurses with regard to infection prevention both in hospitals and nursing homes [18,19]. Educational interventions included evidence-based information on the etiology, epidemiology, diagnosis, treatment, transmission and prevention of CDI, such as hand hygiene, isolation measures and the use of antibiotics [20-22]. Staff education is one of the most successful measures to prevent the spread of C. difficile, which should include not only medical staff (nurses and physicians), but also non-medical staff, especially those responsible for maintaining the hygiene of the hospital environment [23]. Spagnolo et al. (2018) presented in their research how a multidisciplinary approach to the prevention of CDI, which included several interventions, one of which was the education of nurses and hygiene personnel, proved to be successful in controlling the epidemic in one Italian hospital [24]. However, recent studies published that health workers are not properly following the CDI prevention measures. Some of the possible reasons include more and more complex preventive procedures that lead to confusion and gaps [25–27].
Data from the literature indicate that certain individual and socio-demographic factors, including knowledge, length of service or work experience, gender and type of profession influence adherence to infection prevention and control procedures [28]. However, even when hospital infection prevention protocols are followed, outbreaks of any infectious disease, including CDI, may occasionally occur. Therefore, it is important for nurses to update their knowledge on how to prevent HAI, and about the control and management of infections in healthcare facilities [29]. Continuous educational programmes, professional training and ensuring the availability of the necessary guidelines represent essential steps for improving the knowledge and practice of nurses in relation to the prevention of HAI [30]. Different educational strategies are being used to improve nurses’ knowledge and practice of infection control. Some of the most often used methods include quasi-experimental research in which control and target groups are subjected to both didactic and practical sessions, training based on pre-prepared scenarios, e-learning with a questionnaire and focus group discussions, and computer-assisted learning in infection control education [31]. Due to the rapid pace of scientific discoveries, technological innovations and social changes, knowledge quickly becomes outdated. Andragogy is a useful model for planning and facilitating adult learning [32]. Problem-based learning (PBL) is also an effective educational strategy that can improve critical thinking skills in infection prevention and control [33,34].
Nurses make the largest group of health workers in the healthcare system. They provide services in hospitals seven days a week throughout the year and are in close contact with patients and their families. Nurses working in different hospital departments play an important role in HAI prevention [35]. The present relevant literature has only a few published studies that evaluate the knowledge, perception and practice of nurses regarding CDI [36]. A recently conducted study from Bosnia and Herzegovina showed that nurses’ knowledge about CDI prevention is not at a satisfactory level, which indicates an increasing need for educating nurses about this issue [37].
Therefore, the present study was planned bearing in mind the importance of nurses in CDI prevention, and the importance of an educational intervention on the behaviour of nurses in the practice of infection control.
Objective: The research objective was to develop, implement and evaluate an educational module for the prevention of CDI in the hospital environment through the education of nurses in order to improve the level of knowledge and practice among them.
MATERIALS AND METHODS
Design
The research design used in this study was quasi-experimental design with one group design pretest-posttest approach.
Research Time and Place
The study was conducted in the University Clinical Centre of the Republic of Srpska (UKC RS) in Bosnia and Herzegovina, from April to June 2020.
Study Population
The target population consisted of nurses working in ICU, Clinic for Internal Diseases, Clinic for General and Abdominal Surgery, Clinic for Infectious Diseases and Clinic for Oncology.
Based on a G*Power 3.1.9.4 program calculation of medium effect size, power set at 0.80, and a set at 0.05, a minimum of 47 participants is required. Considering a typical dropout rate of 10% for the experimental design used, 57 is the minimum required sample. The scope in the study initially included 75 participants, but excluded 15 with incomplete answers. A final sample of 60 was reached of nurses who have fully completed the education program, pretesting, and post-testing. Participants were selected from the total population using a simple random technique.
Inclusion and Exclusion Criteria for Nurses population
According to the defined criteria for inclusion in the study, the subjects were nurses providing direct care to patients, of all educational profiles, employed at these clinics, aged 18-65, having passed the state exam (nurses licensed to practice) and working 8 and 12 hours shifts. Nurses working on administrative assignments were not included in the study, according to the defined criteria. The criteria for exclusion at the study were the nurses with incomplete answers.
Inclusion and Exclusion Criteria for Patients population
The study included patients with CDI who were older than 18 years of age and hospitalised at the Intensive Care Unit (ICU), Clinic for Internal Diseases, Clinic for General and Abdominal Surgery, Clinic for Infectious Diseases and Clinic for Oncology, from July to December 2019 (before the intervention) and from July to December 2020 (after the intervention). These clinics were selected for the purpose of the study because they treated patients with increased risk for CDI and had an increased incidence of C. difficile infections in 2019.
A case of hospital-acquired CDI (HA-CDI) was defined according to the criteria of the C. difficile Study Group of the European Society of Clinical Microbiology and Infectious Diseases as follows: any patient who developed symptoms of diarrhoea at least 48 hours after admission to the hospital (HA-CDI case with hospital onset); any patient who was admitted with symptoms of diarrhoea at the hospital with an onset of symptoms in the community within 4 weeks following discharge from the hospital (HA-CDI case with community onset) and patients who had stool samples positive for CD toxin A or B or positive for toxin-producing CD [25]. Only the first positive test for C. difficile in patients during the current hospitalization was included in the study. If patients had more than one positive test during the study period, we included only the first episode. Paediatric population of CDI patients, was not included in the study, along with community-acquired CDI.
Educational Intervention
The educational modules contained detailed description of prevention measures against the transmission of the C. difficile in hospital settings in accordance with the guidelines [6,7], and their implementation would affect the patient’s safety during hospitalisation and the treatment outcome. Each educational module was based on adult learning theories for interactive, self-directed learning, which developed interactive teaching, increased the motivation and interest of nurses, and at the same time made it easier to follow and remember the issue [31-33]. For more successful learning, we used numerous teaching aids (blackboard, flip chart, computers and LCD projector, moderation cards, models and figures). Each didactic session would start with a previously prepared Microsoft Office PowerPoint and video presentations followed by interactive group learning (discussions, case studies, and practical examples). The acquisition of planned knowledge and skills was the foundation for evaluating the success of each educational module.
Knowledge Assessment and Outcome Measures
Anonymous survey questionnaires in the form of a test to examine the knowledge and attitudes of nurses about CDI and its prevention were designed for the needs of this research based on the modified version of the questionnaire by Brady et al. [38] with additional questions about new prevent and treatment methods e.g. FMT according to the guidelines [6,7].
The knowledge was evaluated using multiple-choice questions with only one correct answer. The tests that were offered to the respondents at the beginning of the educational modules (previous test for evaluation of the baseline knowledge) and at the end of the session (final test to evaluate what was learned) were the same. These tests contained 10-15 questions divided into two parts, the first part: included questions about the social and demographic characteristics of the respondents, the second part: included questions related to the evaluation of knowledge about CDI and its prevention. Tests before and after the educational modules were numbered to correlate with each subject’s responses and were not correlated across modules for individual participants. We tested the hypothesis that after the training, the nurses’ knowledge about the prevention and control of CDI in hospital settings was significantly higher than the baseline knowledge.
Evaluation of CDI
The diagnosis of CDI is based on clinically identified diarrhoea and laboratory findings. The toxins of C. difficile in faeces were identified using laboratory enzyme immunoassays.
Ethical Considerations
The study was performed in accordance with the ethical considerations of the Helsinki Declaration. The study was approved by the Ethics Committee of the University of Banja Luka, Medical Faculty No: 18/4.4/20. Written consent for was obtained from all the subjects (nurses) who participated in the study. All data collected were confidential and used only by this study.
Statistical analysis
Descriptive statistics and percentages were used to calculate the answers to the questions. A correct answer to each question was graded with “1”, and an incorrect answer with “0”. The final score of knowledge was obtained by dividing the sum of correct answers by the number of questions, and multiplying the quotient of these two numbers by 10. In that way, it was possible to get a range of scores between 0 and 10. The incidence rate of hospital-associated CDI was calculated as the ratio of the number of infections/10,000 patient days. The incidence defined considering 10,000 according to European Society of Clinical Microbiology and Infectious Diseases (ESCMID) CDI-related guidance documents and the European Centre for Disease Prevention and Control (ECDC) protocol for CDI surveillance in acute care hospitals. Patient-days was calculated by summing the number of days in which a bed is occupied overnight by patients hospitalized during the surveillance period [39]. The level of knowledge before the education was described using Kruskal-Wallis test or one-way analysis of variance (ANOVA). To evaluate the effects of the reality based education program, Wilcoxon rank-sum were used for differences in knowledge before and after the education. Statistical hypotheses were tested at the significance level (alpha) of p˂0.05. Statistical analysis was done using IBM SPSS Statistics 26 software.
RESULTS
The characteristics of respondents in this study include gender, age, education level and years of experience. The age intervals were defined on the basis of the median value for the age of the respondents. The intervals of years of experience were determined based on the fact that we wanted to show whether the length of years in practice affects knowledge about CDI. The following is the frequency distribution of the respondents’ characteristics in this study:

Table 1. Demographic characteristics of study participants
The research included 12 (20%) nurses working at the ICU, and at clinics for internal medicine, abdominal surgery, infectious diseases and oncology. The majority of interviewed nurses were female – 51 (85%), with an average age of 31.06 ± 10.74 years. The highest percentage of respondents completed secondary medical school (70%) and most of them had professional experience of 1-15 years – 33 (55%) of them (Table 1).
Level of knowledge among participants with various lengths of work in the profession before application of the educational interventions, is presented in table 2:

Table 2. The level of knowledge among participants with various lengths of work in the profession before application of the educational interventions
Table 2 presents the descriptive statistics of the respondents’ baseline, theoretical knowledge before education on CDI in relation to the years of work experience in practice. There was a statistically significant difference (p=0.001) in the evaluation of knowledge in relation to years of experience in practice, meaning that knowledge about CDI was the highest among respondents with >15 years of experience in practice, and the lowest among those who had <1 years of experience.
Level of knowledge among participants with various education levels before application of the educational interventions, can be seen in table 3:

Table 3. The level of knowledge among participants with various education levels before application of the educational interventions
We determined a statistically significant difference in the average assessment of knowledge about CDI and the prevention of infections caused by this microorganism, in relation to the level of education (7.5 ± 1.0) (Table 3).
Based on the normality test, the statistical test used for the knowledge is Wilcoxon’s matched-pairs test, with the results as shown in the figure 1.
Figure 1 presented the nurses showed highly significant (p<0.001) better knowledge about C. difficile and CDI on the Module 1and 2 tests after the education. On the Module 1, the mean value of the total score on the knowledge test about C. difficile and CDI was significantly higher after the education (8.29 ± 1.18) compared to mean values of the total score on the test that was performed before the education (5.01 ± 2.00). The mean value of the total score on the CDI prevention knowledge test was significantly higher after the education (8.70 ± 0.67) compared to the mean values of the total score on the test that was performed before the education (4.5 ± 2.13) (Module 2).
SD=standard deviation; *** p<0.001; Wilcoxon’s matched-pairs test

Figure 1. Mean values of the total score of the Module 1 and 2 tests before and after the education
CDI incidence before and after the nurses’ education on CDI prevention measures, is presented in table 4.

Table 4. CDI incidence before and after the nurses’ education on CDI prevention measures
Before the education, in the period from 1 July to 31 December 2019, there were 74 patients diagnosed with CDI hospitalised at the UKC RS, whereas after the education of nurses on CDI prevention, in the period from 1 July to 31 December 2020, there were 42 patients diagnosed with CDI hospitalised at the UKC RS. Before the education of nurses on CDI prevention measures, the CDI incidence was 11.04 per 10,000 patient – hospital days. After education on CDI prevention measures, the incidence was 6.49 (Table 4).
DISCUSSION
CDI represents a challenging problem in the acute care environment. Nurses play in important role in the early recognition, diagnosis and rapid treatment of patients with this bacterial infection [40]. Due to the changing epidemiology and increased virulence of C. difficile, it was necessary to educate nurses on the implementation of contact prevention measures when in contact with patients with CDI in order to prevent the transmission of C. difficile to hospitalised patients, their families, and the nurses themselves. The targeted CDI prevention programme included the development and implementation of an evidence-based protocol [6,7] to improve compliance with prevention measures (hand hygiene, contact isolation, cleaning equipment and surfaces, taking care of patients).
Continuous education of medical staff about CDI represents the foundation in risk management in order to reduce the number of infections, as it enables the transfer of know-how, the development of appropriate procedures and leads to better internal communication. Health care personnel education on CDI could be more important than isolating infected patients in single rooms [41].
The results of this study, the nurses demonstrated better knowledge of C. difficile, prevention and control of CDI after the education. Other studies that also evaluated the impact of educational interventions in improving knowledge about infection prevention among nurses had similar results [42-44].
There is evidence to support the fact that both baseline knowledge, and the knowledge gained after an educational intervention on infection prevention, vary with the level of education, type of work, and years of professional experience [22,45]. The results presented here also showed that there is a statistically significant correlation with the level of nurses’ education and years of professional experience in relation to the level of knowledge about the prevention and control of CDI.
After reviewing the reference literature, we noticed that the knowledge of health workers about CDI, the ways of transmission and prevention differs between countries. The research conducted in England [46], USA [12,47] and South Africa [48] confirmed that nurses’ knowledge about CDI is not satisfactory. The research conducted in Poland demonstrated that despite the average score of 6.85 obtained for correct answers to questions that evaluated the knowledge of medical workers, this value was not satisfactory due to differences in the level of knowledge among different groups. Nurses showed a slightly higher level of knowledge than other health workers [45].
In order to recognize a patient with CDI, healthcare professionals should know how to recognise risk factors, as well as the symptoms present in patients. In the research of Legenza et al. the main barrier in recognising a patient with CDI was insufficient knowledge. Thirteen (50%) participants were not able to describe the risk factors for the occurrence of CDI, which could speed up the diagnosis [48].
The results of the research conducted by Aldeyab et al. [49] provided further evidence that a series of CDI control measures, focusing on risky antibiotics (reduction of quinolone antibiotics), education of staff, patients and their families, implementation of prevention measures and isolation, led to a significant reduction in the incidence of infection in three hospitals in Ireland. The research conducted by Wong-McClure et al. [50] showed similar situation, where infection control strategies implemented proved to be effective in achieving outbreak control and in maintaining the baseline C. difficile incidence rate following it.
Even though our educational modules intended for nurses included a part of units which referred to the use of antimicrobial agents, as the main risk factor for CDI, during the introduction of the protocol the use of high-risk antimicrobial agents was not limited because nurses do not prescribe antibiotics. However, numerous efforts in CDI prevention published in the literature report that antibiotic stewardship programs significantly reduce the incidence of infections and colonization with antibiotic-resistant bacteria and CDI in hospitalised patients [51].
The present study results showed that after educating nurses about CDI prevention measures, the incidence of CDI decreased, but it cannot be claimed that the education itself had an effect on the reduction of this hospital infection. However, some other studies have confirmed that education of nurses about CDI prevention along with control of antibiotic use in patient care can lead to reduction of CDI in acute care hospitals [52-54].
CONCLUSION
The knowledge test on C. difficile has confirmed statistically significant differences among nurses, and in prevention and control of CDI after the education compared to the average values of the total score on the test before the education. The study results showed that continuous medical education about CDI can have contribute to inreasing knowledge and awareness about the importance of CDI prevention.
Limitations
This study had several limitations. One limitation of this study is that we recruited nurses from a single hospital and specific findings may only generalize to settings with similar CDI prevention practices and a similar workflow. Consequently, repeated studies using this education program with nurses from other hospitals are needed. The study focuses on both competencies and skills in nurses. The initial plan for our study was to reduction of CDI. During the study, we did not monitor risk factors for CDI such as patient age, severity of the primary disease, and total antibiotic consumption, which would be necessary for this type of study.
Contact prevention measures, such as the use of personal protective equipment, frequent hand washing and disinfection of surfaces, maintaining distance and isolation of patients have been particularly strengthened since the beginning of the COVID-19 pandemic. It would be good to monitor how well nurses actually practice hand hygiene because epidemiological studies show that most HAI are caused by microorganisms that contaminate the hands of nursing staff. According to some authors, a properly adopted hand washing procedure reduces the risk of CDI infection by half [55]. Additionally, the total sample of subjects included less male persons, which could have influenced the results. However, conducting this type of study can provide guidelines to the hospital infection monitoring and control team so that not only nurses but also other health professionals and persons in charge of hospital hygiene can be educated about CDI in the future. It would be good if this type of CDI education for nurses would be repeated every 6 months and the educational modules are revised according to the new CDI prevention guidelines.
Funding statement
No funding sources were used to support the project.
Conflict of interest
The authors declare no conflict of interest.
Authors’ contribution
All authors equally contributed to preparing this article.
Acknowledgements
The authors would like to express special thanks to all participants in this study.
REFERENCES
- Barker AK, Ngam C, Musuuza JS, Vaughn VM, Safdar N. Reducing Clostridium difficile in the Inpatient Setting: A Systematic Review of the Adherence to and Effectiveness of C. difficile Prevention Bundles. Infect Control Hosp Epidemiol. 2017;38(6):639-50.
- Nasiri MJ, Goudarzi M, Hajikhani B, Ghazi M, Goudarzi H, Pouriran R. Clostridioides [Clostridium] difficile infection in hospitalized patients with antibiotic-associated diarrhea: A systematic review and meta-analysis. 2018;50:32-7.
- Teng C, Reveles KR, Obodozie-Ofoegbu OO, Frei CR. Clostridium difficile Infection Risk with Important Antibiotic Classes: An Analysis of the FDA Adverse Event Reporting System. Int J Med Sci. 2019;16(5):630-5.
- Büchler AC, Wicki M, Frei R, Hinic V, Seth-Smith HMB, Egli A, et al. Matching Clostridioides difficile strains obtained from shoe soles of healthcare workers epidemiologically linked to patients and confirmed by whole-genome sequencing. J Hosp Infect. 2022;126:10-15.
- Landelle C, Verachten M, Legrand P, Girou E, Barbut F, Brun-Buisson C. Contamination of healthcare workers’ hands with Clostridium difficile spores after caring for patients with C. difficile infection. Infect Control Hosp Epidemiol. 2014;35(1):10-5.
- Tschudin-Sutter S, Kuijper EJ, Durovic A, Vehreschild MJGT, Barbut F, Eckert C, et al. Guidance document for prevention of Clostridium difficile infection in acute healthcare settings. Clin Microbiol Infect. 2018;24(10):1051-4.
- McDonald LC, Gerding DN, Johnson S, Bakken JS, Carroll KC, Coffin SE, et al. Clinical Practice Guidelines for Clostridium difficile Infection in Adults and Children: 2017 Update by the Infectious Diseases Society of America [IDSA] and Society for Healthcare Epidemiology of America [SHEA]. Clin Infect Dis. 2018;66(7):e1-e48.
- Schoyer E, Hall K. Environmental Cleaning and Decontamination to Prevent Clostridioides difficile Infection in Health Care Settings: A Systematic Review. J Patient Saf. 2020;16(3S Suppl 1):S12-S15.
- Ramai D, Noorani A, Ofosu A, Ofori E, Reddy M, Gasperino J. Practice measures for controlling and preventing hospital associated Clostridium difficile infections. Hosp Pract (1995). 2019;47(3):123-9.
- Musuuza JS, Hundt AS, Carayon P, Christensen K, Ngam C, Haun N, et al. Implementation of a Clostridioides difficile prevention bundle: Understanding common, unique, and conflicting work system barriers and facilitators for sub-process design. Infect Control Hosp Epidemiol. 2019;40(8):880-8.
- Balsells E, Filipescu T, Kyaw MH, Wiuff C, Campbell H, Nair H. Infection prevention and control of Clostridium difficile: A global review of guidelines, strategies, and recommendations. J Glob Health. 2016;6(2):020410.
- Fayerberg E, Bouchard J, Kellie SM. Knowledge, attitudes and practice regarding Clostridium difficile: A survey of physicians in an academic medical center. Am J Infect Control. 2013;41(3):266-9.
- Kelly BJ, Tebas P. Clinical Practice and Infrastructure Review of Fecal Microbiota Transplantation for Clostridium difficile Infection. Chest. 2018;153(1):266-77.
- Rao K, Safdar N. Fecal microbiota transplantation for the treatment of Clostridium difficile infection. J Hosp Med. 2016;11(1):56-61.
- Guillemin I, Marrel A, Beriot-Mathiot A, et al. How do Clostridium difficile infections affect nurses’ everyday hospital work: a qualitative study. Int J Nurs Pract. 2015; 21(suppl 2):38-45.
- Knežević D, Petković M. Faecal transplantation and Clostridioides difficile infection. Scr Med. 2021;52(3):215-23.
- Liubakka A, Vaughn BP. Clostridium difficile Infection and Fecal Microbiota Transplant. AACN Adv Crit Care. 2016;27(3):324-37.
- Hammond DA, Hughes CA, Painter JT, Pennick RE, Chatterjee K, Boye B, Meena N. Impact of Targeted Educational Interventions on Clostridium difficile Infection Treatment in Critically Ill Adults. Hosp Pharm. 2016 Dec;51(11):901-6.
- Kakkar SK, Bala M, Arora V. Educating nursing staff regarding infection control practices and assessing its impact on the incidence of hospital-acquired infections. J Educ Health Promot. 2021 Jan 28;10:40.
- Koo E, McNamara S, Lansing B, Olmsted RN, Rye RA, Fitzgerald T, et al. Making infection prevention education interactive can enhance knowledge and improve outcomes: Results from the Targeted Infection Prevention [TIP] Study. Am J Infect Control. 2016;44(11):1241-6.
- Mody L, Krein SL, Saint S, Min LC, Montoya A, Lansing B, et al. A targeted infection prevention intervention in nursing home residents with indwelling devices: a randomized clinical trial. JAMA Intern Med. 2015;175(5):714-23.
- Barker AK, Ngam C, Musuuza JS, Vaughn VM, Safdar N. Reducing Clostridium difficile in the Inpatient Setting: A Systematic Review of the Adherence to and Effectiveness of C. difficile Prevention Bundles. Infect Control Hosp Epidemiol. 2017;38(6):639-50.
- Kato H, Hagihara M, Asai N, Shibata Y, Yamagishi Y, Iwamoto T, et al. A systematic review and meta-analysis of decontamination methods to prevent hospital environmental contamination and transmission of Clostridioides difficile. 2022;73:102478.
- Spagnolo AM, Sartini M, Battistella A, Casini B, Lo Pinto G, Schinca E, et al. A Clostridium difficile outbreak in an Italian hospital: The efficacy of the multi-disciplinary and multifaceted approach. J Prev Med Hyg. 2018;59(2):E132-E138.
- European Surveillance of Clostridioides [Clostridium] difficile infections. Surveillance protocol version 2.4. European Centre for Disease Prevention and Control. Stockholm: ECDC; 2019. Available at: ecdc.europa.eu/sites//files/documents/clostridium-difficile-infections-EU-surveillance-protocol-vers2.4.pdf. Last accessed: 2 Mart 2022.
- Vonberg RP, Kuijper EJ, Wilcox MH, Barbut F, Tüll P, Gastmeier P, et al. Infection control measures to limit the spread of Clostridium difficile. Clin Microbiol Infect. 2008;14 Suppl 5:2-20.
- Tsioutis C, Birgand G, Bathoorn E, Deptula A, ten Horn L, Castro-Sánchez E, et al. Education and training programmes for infection prevention and control professionals: mapping the current opportunities and local needs in European countries. Antimicrob Resist Infect Control. 2020;9(1):183.
- Abalkhail A, Alslamah T. Institutional Factors Associated with Infection Prevention and Control Practices Globally during the Infectious Pandemics in Resource-Limited Settings. Vaccines (Basel). 2022;10(11):1811.
- Yoshikawa A, Tashiro N, Ohtsuka H, et al. Protocol for educational programs on infection prevention/control for medical and healthcare student: A systematic review and meta-analysis. PLoS One. 2022;17(10):e0276851.
- Asfaw N. Knowledge and practice of nurses towards prevention of hospital acquired infections and its associated factors. International Journal of Africa Nursing Sciences. 2021;16:100333.
- Gaikwad U N, Basak S, Kulkarni P, Sande S, Cahavan S, et al. Educational Intervention to Foster Best Infection Control Practices Among Nursing Staff. Int J Infect. 2018;5(3):e81531.
- Knowles MS, Holton EF, Swanson RA, Robinson PA. The adult learner: The definitive classic in adult education and human resource development. 9nd ed. Oxfordshire: Routledge. 2020.
- Cole M. Problem-based learning — a case for infection control. British Journal of Infection Control. 2005;6(6):16-9.
- Choi Y-R, Lee Y-N, Kim D, Park WH, Kwon DY, Chang SO. An e-Problem-Based Learning Program for Infection Control in Nursing Homes: A Quasi-Experimental Study. International Journal of Environmental Research and Public Health. 2022;19(20):13371.
- Kakkar SK, Bala M, Arora V. Educating nursing staff regarding infection control practices and assessing its impact on the incidence of hospital-acquired infections. J Educ Health Promot. 2021;10:40.
- Finnimore K, Smyth W, Carrucan J, Nagle C. Nurses’ knowledge, practices and perceptions regarding Clostridioides difficile: Survey results. Infect Dis Health. 2023 Feb;28(1):39-46.
- Miljković I, Topuz A. The knowledge of nurses about prevention of infections caused by the bacteria Clostridium difficile. Biomedicinska Istraživanja. 2021;12(1),61–8.
- Brady RR, Rodrigues MA, Harrison R, Rae C, Graham C, Poxton IR, et al. Knowledge of Clostridium difficile infection among UK health-care workers: development of a knowledge assessment tool. Scott Med J. 2012;57(3):124-30.
- Krutova M, Kinross P, Barbut F, et al. How to: Surveillance of Clostridium difficile infections. Clin Microbiol Infect. 2018;24(5):469-75.
- Keske LA, Letizia M. Clostridium difficile infection: essential information for nurses. Medsurg Nurs. 2010;19(6):329-33.
- Domeniconi G, Serafino S, Migone De Amicis M, Formica S, Lanzoni M, Maraschini A, et al. Clostridium difficile infection epidemiology and management: Comparison of results of a prospective study with a retrospective one in a reference teaching and research hospital in Northern Italy. Am J Infect Control. 2016;44(11):1214-18.
- Kim E, Kim SS, Kim S. Effects of infection control education for nursing students using standardized patients vs. Peer role-play. Int J Environ Res Public Health. 2021;18(1):107.
- Korashy Osman F, Mohamed El Banna H, Youssef Sharaf A, Fathy Mohammed Y. The Effects of Educational Interventions on Nurses’ Knowledge and Practices in Hemodialysis Unit Regarding Infection Control Practices. Egypt J Hosp Med. 2021;84(1):1739-48.
- Gomarverdi S, Khatiban M, Bikmoradi A, Soltanian AR. Effects of a multi-component educational intervention on nurses’ knowledge and adherence to standard precautions in intensive care units. J Infect Prev. 2019;20(2):83-90.
- Kiersnowska ZM, Lemiech-Mirowska E, Semczuk K, Michałkiewicz M, Sierocka A, Marczak M. Level of Knowledge of Medical Staff on the Basis of the Survey in Terms of Risk Management, Associated with Clostridioides difficile Infections. Int J Environ Res Public Health. 2021;18(13):7060.
- Burnett E, Corlett J. Understanding risk perceptions and responses of the public and health care professionals toward Clostridium difficile: A qualitative interpretive description study. Am J Infect Control. 2017;45(2):133-8.
- Legenza L, Barnett S, Rose W, Safdar N, Emmerling T, Peh KH, et al. Clostridium difficile infection perceptions and practices: A multicenter qualitative study in South Africa. Antimicrob Resist Infect Control. 2018;7:125.
- Klatte JM, Myers AL, Livingston RA, Jackson MA. Pediatric physicians’ knowledge, attitudes, and beliefs regarding Clostridium difficile-associated disease prevention, testing, and treatment. Am J Infect Control. 2012;40(6):577.
- Aldeyab MA, Devine MJ, Flanagan P, Mannion M, Craig A, Scott MG, et al. Multihospital Outbreak of Clostridium difficile Ribotype 027 Infection: Epidemiology and Analysis of Control Measures. Infect Control Hosp Epidemiol. 2011;32(3):210-9.
- Wong-McClure RA, Ramírez-Salas E, Mora-Brenes N, Aguero-Sandí L, Morera-Sigler M, Badilla-Vargas X, et al. Long term effect of infection control practices and associated factors during a major Clostridium difficile outbreak in Costa Rica. J Infect Dev Ctries. 2013;7(12):914-21.
- Baur D, Gladstone BP, Burkert F, Carrara E, Foschi F, Döbele S, et al. Effect of antibiotic stewardship on the incidence of infection and colonisation with antibiotic-resistant bacteria and Clostridium difficile infection: a systematic review and meta-analysis. Lancet Infect Dis. 2017;17(9):990-1001.
- Jarodiya V, Singh T, Khan ZH. Decreasing Hospital Clostridium difficile Infections: Impact of an Educational Module. Am J Gastroenterol. 2019;114:S117.
- Pate K, Reece J, Smyre A. A Multifaceted Approach to the Prevention of Clostridioides [Clostridium] Difficile. Clin Nurse Spec. 2019;33(2):75-81.
- Fabre V, Markou T, Sick-Samuels A, Rock C, Avdic E, Shulder S, et al. Impact of Case-Specific Education and Face-to-Face Feedback to Prescribers and Nurses in the Management of Hospitalized Patients with a Positive Clostridium difficile Test. Open Forum Infect Dis. 2018;5(10):ofy226.
- Kiersnowska ZM, Lemiech-Mirowska E, Michałkiewicz M, Marczak M. Hand hygiene as the basic method of reducing Clostridium difficile infections (CDI) in a hospital environment. Ann Agric Environ Med. 2021;28(4):535-40.
![]() This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Single-centre descriptive study of adverse events reported after anti-COVID vaccination
Fabio Giancane1, Angelo Cianciulli1, Silvia De Chiara2, Alessandra Iannelli2,
Marika Finizio4, Rosetta Frammartino1, Andrea Lombardi1,
Domenico Ciro Cristiano1, Francesco Gravante3, Francesco Petrosino1*
1.Nurse, AOU ‘San Giovanni di Dio e Ruggi d’Aragona’, Salerno
2.Pharmacist, AOU ‘San Giovanni di Dio e Ruggi d’Aragona’, Salerno
3.Nurse, Local Health Unit of Aversa, Caserta
4.Nursing graduate, University of Salerno
*Corresponding author: Francesco Petrosino, AOU ‘San Giovanni di Dio e Ruggi d’Aragona’, Salerno. Email: f.petrosino75@gmail.com
Cite this article
ABSTRACT
Introduction: In Italy, approximately 80.5% of the population has completed the primary anti-COVID vaccination cycle with approximately 141 million doses administered. With the introduction of new measures to counter the spread of COVID-19, including compulsory vaccination for certain categories of people, the population expressed fears about the safety and adverse effects of SARS-CoV-2 vaccines. Several factors, such as gender and age, could have influenced the outcomes associated with the vaccine. Our single-centre work seeks to provide such evidence with respect to Pfizer/BioNTech’s BNT162b2 (Comirnaty) and AstraZeneca’s AZD1222 (Vaxzevria) vaccines.
Materials and Methods: Single-centre descriptive study carried out on a sample of subjects who underwent anti-COVID vaccination at the ‘San Giovanni di Dio e Ruggi d’Aragona’ AOU vaccination centre in Salerno. Patients who reported a suspected adverse reaction after receiving a dose of vaccine were included in the study. The regional vaccine platform SORESA and the VigiFarmaco portal were used to collect the data.
Results: During the period covered by the study, 126,928 doses of SARS-CoV-2 vaccine were administered. The Pfizer-BioNTech vaccine group comprised 124,138 administrations. The AstraZeneca vaccine group consisted of 2,790 administrations. 287 post-vaccination adverse reaction reports entered in the National Pharmacovigilance Network were considered. In most of the reactions reported, for both vaccines considered, the symptomatology was attributable to local reactions at the injection site. At the systemic level, however, we noted the prevalence of non-specific events such as fever, headache and diffuse arthromyalgia.
Conclusions: Based on our results and comparison with the literature, the data collected on the vaccines considered in the study suggest a favourable safety profile for their large-scale use. The rate of minor adverse events turned out to be low, with similarly reassuring data compared to serious adverse events, such as not to justify hesitation towards vaccination for COVID-19 disease control.
Keywords: SARS-CoV-2; Surveillance system; COVID-19 vaccination; mRNA; Viral vector; Adverse events following immunisation
INTRODUCTION
Pathogenic viral outbreaks and complex interactions with humans and animals have, over the centuries, caused the transmission of viruses between different species (jumping), posing a great threat to human health and safety[1-3]. Globalisation has increasingly favoured pathogenic transmission between continents, causing different pandemics, in particular viral pandemics[4]. A new public health crisis that threatened the world in 2019 was the spread of the new coronavirus (2019-nCoV) or severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) declared a pandemic by the World Health Organisation (WHO) in March 2020[5]. The rapid spread of the COVID-19 disease has focused researchers’ attention on the repurposing of existing approved drugs that inhibit viral entry, endocytosis, genome assembly, transmission and replication[6]. Most of the available information has been obtained through studies on other members of this family (SARS and MERS)[7]. Many researchers are currently working on the development of various types of specific drugs to treat this disease worldwide[8, 9]. Therefore, the current treatment given to COVID-19 patients is only based on their symptoms[10, 11]. Exposure to a pathogen such as SARS-CoV-2 generates an antibody response that changes over time and in different individuals (antibody kinetics)[12, 13]. It is believed that the limited pre-existing natural immunity to this virus was responsible for the explosive increase in cases[14, 15]. A previous infection, on the other hand, could play a key role in ensuring protection against new infections, and the literature can provide evidence of such protective correlations through longitudinal cohort studies[16-19]. In the absence of specific drugs, only global vaccination has made it possible to contain the spread of the virus, reducing the number of serious clinical cases and hospitalisations[20-22]. In December 2020, the first vaccines against COVID-19 developed with different technologies received Emergency Use Authorisation (EUA) from the US Food and Drug Administration (FDA). Subsequently, globally, they were licensed in 117 countries in North and South America, the United Kingdom, Europe, Africa, Asia and Oceania[23, 24].
In Italy, mRNA vaccines and the adenovirus vaccine AZD1222 have been widely administered. Time saving during the development of COVID-19 vaccines was achieved through unprecedented levels of public financial support, increased tolerance for risky investments in technology and process, and studies on mRNA transport methodology[25-27]. The Italian Medicines Agency defines pharmacovigilance and vaccine vigilance as “a complex set of activities aimed at continuously assessing all information relating to the safety of medicinal products and ensuring that the benefit/risk (B/R) ratio remains favourable over time.” Our country has a pharmacovigilance system that, for many years now, has devoted special attention and a special organisational structure precisely to monitoring what happens after a vaccine is administered. It is an open, dynamic system to which everyone (health professionals, patients, parents, citizens) can send their reports contributing to the monitoring of the safe use of vaccines and medicines in general. Furthermore, the system has full transparency and offers access to aggregated data, which can be queried on the AIFA website. The National Pharmacovigilance Network (NFP) suddenly came into the spotlight when several new vaccines received emergency authorisation and were launched on a large scale at the end of 2020. Vaccines have undergone rigorous clinical testing and evaluation by the authorities, but with the use of new technologies [28] and rapid, large-scale administration of vaccines, the importance of a well-functioning international system of post-marketing safety surveillance has been emphasised[29, 30]. The surveillance of vaccine safety and the collection of reports on suspected adverse events after immunisation (AEFI) [31] is the responsibility of national vaccine regulatory systems, including national regulatory authorities (NRAs) and national immunisation programmes (NIPs). Passive surveillance, defined as the collection and analysis of unsolicited reports of suspected adverse events in the form of individual case safety reports (ICSRs) that are sent to a central database or a health authority, is the basis of safety surveillance for immunisation programmes, in order to identify rare events, evaluate clusters of reports and detect safety signals for further and subsequent studies [32, 33]. Although the identification and quantification of adverse events related to anti-COVID vaccination is not always easy to understand, especially in such a broad context as a pandemic, the analysis of the available data can be an important moment for risk estimation and subsequent safety assessments[34-36].
This paper describes reports of reactions that were observed after administration of the COVID vaccine. Investigating the meaning and causes of these reactions is the task of pharmacovigilance. Investigating every event that appears after a vaccination serves to gather as much information as possible and increase the possibility of identifying truly suspicious events whose nature is important to understand, or which have never been observed before, with the aim of ascertaining whether there is a causal link with the vaccination. In this way, regulatory authorities such as AIFA can verify the safety of vaccines in the real world, confirming what has been observed in pre-authorisation studies and possibly identifying new potential adverse reactions, especially if they are rare (1 in 10,000) and very rare (less than 1 in 10,000). A large number of reports, therefore, does not imply that the vaccine is more dangerous, but is an indication of the high capacity of the pharmacovigilance system to monitor safety.
The anti-Sars-CoV-2 vaccination campaign, which started on 27 December 2020, saw the participation of the ‘San Giovanni di Dio e Ruggi d’Aragona’ AOU of Salerno in ‘Vaccine Day’, the symbolic start date of the vaccination campaign in Italy and across Europe. In what was analysed by this work, in order to make this event – historic for all healthcare worldwide – possible, an organisational and coordination process was implemented that ensured high daily vaccination numbers and minimal risks for users, in full compliance with the quality standards of Public Health.
Several factors, such as gender and age, may have influenced the clinical outcomes associated with the vaccine[37]. To date, in Italy, about 80.5% (48 million subjects) of the population have completed the COVID-19 primary vaccination cycle with about 141 million doses administered. This followed the introduction of new measures to combat the spread of COVID-19, including the compulsory vaccination of certain categories of persons[38].
MATERIAL AND METHODS
Study design
In this paper, we will provide a surveillance report on vaccines administered at the ‘San Giovanni di Dio e Ruggi d’Aragona’ University Hospital (AOU ‘Ruggi’) in Salerno with respect to specific targets:
1.to conduct a descriptive observational study of subjects undergoing vaccination with Pfizer/BioNTech’s BNT162b2 (Comirnaty) and AstraZeneca’s AZD1222 (Vaxzevria) between 27 December 2020 and 30 November 2021
2.to conduct a descriptive analysis of all reports of suspected adverse drug reactions attributed to COVID-19 vaccination (Adverse Events and Severe Adverse Events Following Immunisation, AEFI and sAEFI), collected through the AIFA form and/or the VigiFarmaco system of the Italian Drug Agency (severity, concomitant use of drugs, outcome)
3.to assess the role and statistical association between reported reactions and previously identified variables (age, gender, dose).
Participants
The descriptive observational study was carried out on a sample of subjects who received the vaccine at the ‘San Giovanni di Dio e Ruggi d’Aragona’ AOU vaccination centre in Salerno in the period between 27 December 2020 and 30 November 2021. Patients who reported a suspected adverse reaction after receiving a dose of vaccine were included in the study.
Sample Size
The sample size was evaluated using the GPower software version 3.1.9.7[39]. Power analysis was conducted for a two-tailed t-test, with an effect size = 0.50, a probability of type I error = 0.05, a test power = 0.95 and a sample size ratio of 1:1. The sample size for group 1 is 105 and for group 2 it is 105 for a total of 210 items. For the goodness-of-fit χ2 test, with an effect size = 0.3, a probability of the type 1 error = 0.05, a power of the test = 0.95 and GdL = 1, the sample size for the group is 143 (172 with 2 degrees of tolerance).
Data collection
For the vaccination population, data were obtained from the SINFONIA platform (Sistema Informativo Sanità Campania) and the VigiFarmaco portal for adverse event reporting. They were collected anonymously, formatted, narrowed down to the vaccines of interest for this study and entered into a database using Microsoft Corporation Excel software.
Data analysis
The collected data were processed with SPSS ® (Statistical Package for Social Science – Chicago, IL, USA) statistical software for Windows, version 26.0. A descriptive analysis of the general characteristics of the study population was performed, using absolute frequencies and percentages. Data were stratified by age group, gender and period of administration. For continuous variables, results were expressed as mean ± standard deviation (SD), and as median and Interquartile range (RIQ) for numeric variables. Paired and unpaired data were analysed using Student’s t-test. The Kolmogorov-Smirnov test, which is more appropriate when the sample size is >50, was used to check normality. The Q-Q diagram and the values of skewness and kurtosis were also evaluated. The categorical variables were summarised using frequencies and percentages, and we used the chi-square (χ2) test to compare the categorical variables between the groups.
The Phi coefficient was used to measure the strength of association between the dichotomous variables, while Pearson’s linear correlation coefficient was used to assess the degree of relationship between the variables age and severity.
All tests with p-value (p) < 0.05 were considered statistically significant.
Ethical consideration
Due to the nature of this study, no formal approval to the relevant Ethics Committee was required. The study was conducted in accordance with the principles of the Declaration of Helsinki. The data were extracted from databases for which the processing information had been signed in advance and analysed for the time strictly necessary to achieve the purposes for which they were collected, in compliance with the Regulation (EU) 2016/679 (GDPR) on privacy and guarantee of anonymity. Authorisation for their use was provided by the Corporate Privacy Officer and the legal representative of the organisation.
RESULTS
During the period covered by the study, 126,928 doses of SARS-CoV-2 vaccine were administered. Those who had already received the first dose went to the centre for the administration of the second dose of vaccine. Some of them also received the third dose.
In Table 1, the general trend of the Vaccination Centre is shown, while in Table 2, the trend per macro area (Vaccination Type and Dose) is shown.

Table 1. General performance of the Vaccination Centre

Table 2. Performance by macro area of the Vaccination Centre, with order of priority of categories
A proportion of the vaccinated subjects (404) switched from AstraZeneca to Pfizer-BioNTech due to changes in the Italian Regulatory Authority’s declarations [40] or because they had suffered increased D-dimer levels [41]after the first AZD dose.
The Pfizer-BioNTech vaccine group (BNT) comprised 124,138 administrations (47.8% men and 52.2% women) with a mean age of 49.11±20.94 years (range: 12-101) and a median age of 51 years (RIQ: 31-64).
The distribution is superimposable between first dose (50.6%) and second dose (47.2%). Only 2.2% of the subjects received the third dose.
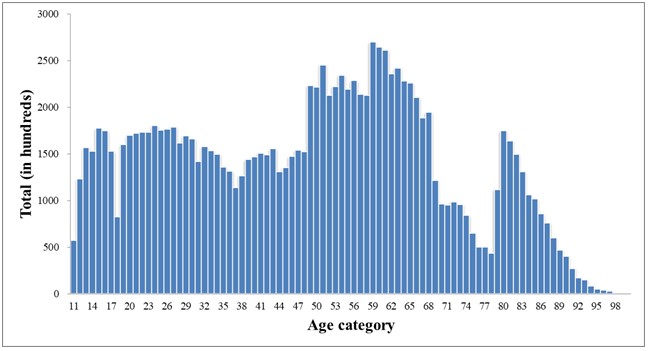
Figure 1. Age distribution BNT Group
The AstraZeneca vaccine group (AZD) consisted of 2,790 administrations (57.7% men and 42.3% women), with a mean age of 47.46±11.77 (range: 18-76 years) and a median age of 49 years (RIQ: 38-57). 58.7% of the sample received the first dose and 41.3% the second dose.

Figure 2. Age distribution AZD Group
The enrolled population was stratified by age decades. The Pfizer-BioNTech group consisted predominantly (18.9%) of individuals aged between 60 and 69 years (Figure 3), whereas the AstraZeneca group comprised more people (23.1%) aged between 40 and 49 years (Figure 4). In particular, several subjects were unable to receive AstraZeneca mainly due to thrombotic risk (e.g. high D-dimer value, coagulation impairment, etc.) and age limitation (initially subjects over 18 years of age were eligible and later over 60 years of age), according to the recommendations in force in Italy. Our study therefore examined the AEFIs and sAEFIs attributed to the SARS-CoV-2 vaccination and recorded by the nursing staff or pharmacists responsible for vaccine preparation and pharmacovigilance at the AOU ‘San Giovanni di Dio e Ruggi d’Aragona’ Vaccine Centre.
At the time of its closure on 30 November 2021, we verified that 287 post-vaccination adverse reaction reports had been entered into the National Pharmacovigilance Network. The data show that the percentage of reported sAEFIs are significantly lower than the risks related to COVID-19 (data from the COVID-19 Integrated Surveillance in Italy).
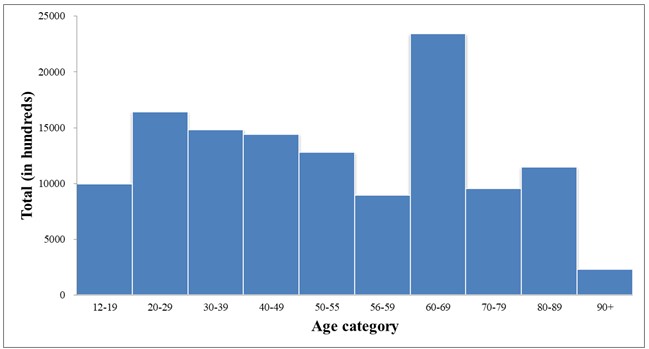
Figure 3. Distribution by age group BNT Group

Figure 4. Age distribution AZD Group
Most of the reported adverse events were classified as non-serious (90.9%) and to a lesser extent as serious (9.1%); in most cases, the outcome was complete resolution or improvement of symptoms. The distribution of reports per type of vaccine follows the distribution of administrations (92% for Pfizer-BioNTech and 8% for AstraZeneca).
The average age of persons reporting a suspected adverse event was 62±22.21 years (range: 15-99). As already observed in the National Surveillance Reports on anti-COVID-19 vaccines, also in what was analysed by this work, the reporting rates for the 2nd dose are lower than for the 1st dose and significantly lower for the 3rd dose. Although these are not absolute incidence rates, the data indicate an overall absence of significant sAEFI events such as to be an alert for regulators to serious safety issues with administered vaccines. On the other hand, in contrast to the overlapping exposure between the genders (52% of doses administered in females and 48% in males), one can note the asymmetric distribution of reports with respect to gender, with 71.1% of reports concerning women and 27.9% concerning men, regardless of the vaccine and the dose administered.
In our statistical analysis, in order to determine whether there were age differences between those who reported a post-vaccination adverse reaction, we performed an independent samples t-test.
To test for normality, we used the Kolmogorov-Smirnov test with Lilliefors correction, which was non-significant for both men (p = 0.071) and women (p = 0.058). Visual inspection of the Q-Q plot shows that age is normally distributed, with a skewness of -0.445 (ES = 0.271, | z | = 1.64) and kurtosis of -0.634 (ES = 0.535) for men and a skewness of 0.006 (ES = 0.171, | z | = 0.035) and kurtosis -0.902 (ES = 0.341) for women[42-43]. Having ascertained the normality of the sample distribution, we evaluated the hypothesis of equality of variance by means of Levene’s test. This turns out to be statistically non-significant (F = 0.255, p = 0.614) and it is therefore possible to use the assumption of homogeneous variance of the age of males and females.
The results suggest that the difference in mean age between the two groups is not significantly different (t(279) = 1.769, p = 0.078). We then looked at whether the 287 subjects in our sample were as likely as the Italian population to have non-serious (81.8%) or serious (18.1%) reactions[44].
We conducted a χ2 test for goodness of fit against the theoretical distribution model. In this case, the results obtained suggest that the two categories do not distribute themselves according to the expected probability (χ2(1) = 15.88, p < 0.001). In particular, in our reference sample, non-serious reactions are more frequent (90.9%) than serious reactions (9.1%). We then conducted a χ2 test to test whether men and women were equally likely to have non-serious or serious reactions. The test results suggest that men and women were equally distributed within the two categories of the severity status variable (χ2(1) = 2.83, Phi = -0.100, p = 0.093). In other words, there is no evidence of linear dependence between gender and the occurrence of a serious adverse reaction, with a small linkage effect between the two variables, as suggested by the value close to 0 for the Phi coefficient. We also conducted a χ2 test to test whether there was a relationship between the number of doses received and the occurrence of a severe reaction. These results also suggest that the groups are equally distributed within the two categories of the severity status variable (χ2(2)= 0.418, p = 0.811, V = 0.038). In other words, dose and severity of the reaction are independent in distribution. Finally, Pearson’s linear correlation coefficient was calculated to investigate the correlation between the variables age and severity considering the reported adverse reaction (r = -0.279, p = 0.01).
The results suggest that as age decreases, there is a weak correlation with the presentation of a severe reaction. In this analysis, the source variable (severity) was coded into a nominal dichotomous qualitative variable with value 0 (no severe reaction) and 1 (severe reaction).
Below are some of the reactions detected and their incidence in relation to the total number of detections (Figure 5).
Figure 6 shows some detected reactions and their incidence for the Pfizer-BioNTech vaccine and Figure 7 for AstraZeneca.

Figure 5. All types of adverse events observed on our sample.

Figure 6. All types of adverse events observed by Comirnaty vaccine.

Figure 7. All types of adverse events observed by Vaxzevria vaccine.
Finally, Figure 8 shows the reports of sAEFI aggregated by symptomatology. It can be noted that,

Figure 8. All types of severe adverse events observed.
Figure 8 shows the reports of severe AEFIs aggregated by symptomatology. It can be seen that, in addition to overlapping with the AEFIs in terms of typology, they are characterised by events attributable to general pathologies. For all reported sAEFIs, the outcome was improvement of symptoms.
DISCUSSIONS
Our study examined AEFIs and sAEFIs spontaneously reported at the AOU ‘San Giovanni di Dio e Ruggi d’Aragona’ in Salerno through the AIFA pharmacovigilance system and attributed to anti-COVID vaccination. Our data, although related to a small sample, demonstrate the few reports of serious reactions and the low risk of outcomes when compared to historical pandemic data and in line with national data. In contrast to an overlapping exposure between the sexes with respect to total administrations, AEFIs were predominantly reported in the female sex (71%). The percentage of sAEFI is almost overlapping between the sexes, with a prevalence for Pfizer-BioNTech’s Comirnaty vaccine (78%) at the first dose (77%). In most of the AEFIs reported, for both vaccines considered, the symptomatology was attributable to local reactions at the injection site (e.g. pain, swelling, redness). At the systemic level, however, we noted the prevalence of non-specific events such as fever, headache and diffuse arthromyalgia. The same applies to reactions reported as serious; the latter, identified as such due to the prolonged observation period at the vaccination centre, in rare cases led to the hospitalisation of those involved. All these reports resulted in an improvement in symptoms. In line with the literature, our study showed that the onset of AEFI can be influenced by gender. This could be related to the opposite role of sex hormones [42] as well as pharmacokinetic parameters that may differ between males and females [43].
Disease control efforts by health authorities should seriously consider the relationship between the risks involved in immunising the population versus the benefits against the disease[45]. While there is no general acceptable risk threshold, the number of deaths worldwide from COVID-19, the risk of collapse of health systems, shutdowns and damage to economies, should lead epidemiologists, health organisations and governments to set this threshold as soon as possible.
CONCLUSIONS
Based on our results and the comparison with the literature[46, 47], both vaccines showed a favourable safety profile, with reassuring data that does not justify hesitation towards vaccination for COVID-19 disease control[48-50]. We therefore highlighted the few differences in the incidence and type of AEFI and sAEFI associated with Pfizer/BioNTech’s Comirnaty (BNT162b2) and AstraZeneca’s Vaxzevria (AZD1222). For these reasons, the guidelines issued by many countries, such as Italy, whose main objective is to increase the number of vaccinated persons with a ‘fourth dose’ to protect the over 60s and the frailest of the population. It is therefore necessary to disseminate surveillance and public health data to counter vaccination hesitancy in the general population and the reluctance of “no vax” subjects towards vaccinations, also in view of possible future pandemic events.
LIMITS
The study has some limitations. Pharmacovigilance information is based on a voluntary and passive reporting system that may not capture every single event related to AEFI and sAEFI. Direct verification is not always possible to determine whether every reported adverse reaction is actually related to the vaccine. In particular, the lack of reporting could lead to an underestimation of all the adverse events that actually occurred.
Another limitation of the study is that, to the exclusion of age and gender, other individual characteristics were not taken into account, such as underlying or previous diseases (myocarditis, autoimmune or immune-mediated diseases, oncological pathologies) or chronically taken medications, which might instead predispose vaccinated subjects to be susceptible to AEFIs and sAEFIs.
ACKNOWLEDGEMENTS
We thank Prof Francesco De Caro (UOC Risk Assessment Management and Reporting) and Dr Maria Grazia Lombardi (UOC Pharmacy), AOU ‘San Giovanni di Dio e Ruggi d’Aragona’, Salerno.
FUNDING
This research did not receive any external funding or support.
CONFLICTS OF INTEREST
The authors declare that they have no conflicts of interest associated with the study.
AUTHORS’ CONTRIBUTION
FG and AC were responsible for the conception and design of the study; SDC and AI performed the data collection; FG and FP performed the data analysis; MF and RF were responsible for drafting the manuscript; AL and DCC made critical revisions to the article.
REFERENCES
- Sharma A, Tiwari S, Deb MK, Marty JL. Severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2): a global pandemic and treatment strategies. Int J Antimicrob Agents. 2020;56(2):106054.
- Reperant LA, Osterhaus ADME. AIDS, Avian flu, SARS, MERS, Ebola, Zika… what next?. Vaccine. 2017;35(35 Pt A):4470-4474.
- Reperant LA, Cornaglia G, Osterhaus AD. The importance of understanding the human-animal interface: from early hominins to global citizens. Curr Top Microbiol Immunol. 2013; 365:49-81.
- Liu J, Dai S, Wang M, Hu Z, Wang H, Deng F. Virus like particle-based vaccines against emerging infectious disease viruses. Virol Sin. 2016;31(4):279-287.
- Wang C, Horby PW, Hayden FG, Gao GF. A novel coronavirus outbreak of global health concern [published correction appears in Lancet. 2020 Jan 29;:]. Lancet. 2020;395(10223):470-473.
- Muralidar S, Ambi SV, Sekaran S, Krishnan UM. The emergence of COVID-19 as a global pandemic: Understanding the epidemiology, immune response and potential therapeutic targets of SARS-CoV-2. Biochimie. 2020;179:85-100.
- Chan-Yeung M, Xu RH. SARS: epidemiology. Respirology. 2003;8 Suppl(Suppl 1):S9-S14.
- Parums DV. Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Patients. Med Sci Monit. 2022;28:e935952.
- Zarandi PK, Zinatizadeh MR, Zinatizadeh M, Yousefi MH, Rezaei N. SARS-CoV-2: From the pathogenesis to potential anti-viral treatments. Biomed Pharmacother. 2021;137:111352.
- Hosoki K, Chakraborty A, Sur S. Molecular mechanisms and epidemiology of COVID-19 from an allergist’s perspective. J Allergy Clin Immunol. 2020;146(2):285-299.
- Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China [published correction appears in Lancet. 2020 Jan 30;:]. Lancet. 2020;395(10223):497-506.
- Huang AT, Garcia-Carreras B, Hitchings MDT, et al. A systematic review of antibody mediated immunity to coronaviruses: kinetics, correlates of protection, and association with severity. Nat Commun. 2020;11(1):4704.
- Grifoni A, Sidney J, Vita R, et al. SARS-CoV-2 human T cell epitopes: Adaptive immune response against COVID-19 [published correction appears in Cell Host Microbe. 2022 Dec 14;30(12):1788]. Cell Host Microbe. 2021;29(7):1076-1092.
- Wallinga J, Teunis P. Different epidemic curves for severe acute respiratory syndrome reveal similar impacts of control measures. Am J Epidemiol. 2004;160(6):509-516.
- Dan JM, Mateus J, Kato Y, et al. Immunological memory to SARS-CoV-2 assessed for up to 8 months after infection. Science. 2021;371(6529):eabf4063.
- Qu G, Li X, Hu L, Jiang G. An Imperative Need for Research on the Role of Environmental Factors in Transmission of Novel Coronavirus (COVID-19). Environ Sci Technol. 2020;54(7):3730-3732.
- Wu Y, Kang L, Guo Z, Liu J, Liu M, Liang W. Incubation Period of COVID-19 Caused by Unique SARS-CoV-2 Strains: A Systematic Review and Meta-analysis [published correction appears in JAMA Netw Open. 2022 Sep 1;5(9):e2235424]. JAMA Netw Open. 2022;5(8):e2228008.
- Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study [published correction appears in Lancet. 2020 Mar 28;395(10229):1038] [published correction appears in Lancet. 2020 Mar 28;395(10229):1038]. Lancet. 2020;395(10229):1054-1062.
- Seow J, Graham C, Merrick B, et al. Longitudinal observation and decline of neutralizing antibody responses in the three months following SARS-CoV-2 infection in humans. Nat Microbiol. 2020;5(12):1598-1607.
- Moreira ED Jr, Kitchin N, Xu X, et al. Safety and Efficacy of a Third Dose of BNT162b2 Covid-19 Vaccine. N Engl J Med. 2022;386(20):1910-1921.
- Tarke A, Coelho CH, Zhang Z, et al. SARS-CoV-2 vaccination induces immunological T cell memory able to cross-recognize variants from Alpha to Omicron. Cell. 2022;185(5):847-859.e11.
- Wajnberg A, Amanat F, Firpo A, et al. Robust neutralizing antibodies to SARS-CoV-2 infection persist for months. Science. 2020;370(6521):1227-1230.
- van Riel D, de Wit E. Next-generation vaccine platforms for COVID-19. Nat Mater. 2020;19(8):810-812.
- Cai C, Peng Y, Shen E, et al. A comprehensive analysis of the efficacy and safety of COVID-19 vaccines. Mol Ther. 2021;29(9):2794-2805.
- Hahn WO, Wiley Z. COVID-19 Vaccines. Infect Dis Clin North Am. 2022;36(2):481-494.
- Nakagami H. Development of COVID-19 vaccines utilizing gene therapy technology. Int Immunol. 2021;33(10):521-527.
- Wallace M, Moulia D, Blain AE, et al. The Advisory Committee on Immunization Practices’ Recommendation for Use of Moderna COVID-19 Vaccine in Adults Aged ≥18 Years and Considerations for Extended Intervals for Administration of Primary Series Doses of mRNA COVID-19 Vaccines – United States, February 2022. MMWR Morb Mortal Wkly Rep. 2022;71(11):416-421.
- Rauch S, Jasny E, Schmidt KE, Petsch B. New Vaccine Technologies to Combat Outbreak Situations. Front Immunol. 2018;9:1963.
- Black S, Eskola J, Siegrist CA, et al. Importance of background rates of disease in assessment of vaccine safety during mass immunisation with pandemic H1N1 influenza vaccines [published correction appears in Lancet. 2010 Jan 30;375(9712):376]. Lancet. 2009;374(9707):2115-2122.
- Klein NP, Lewis N, Goddard K, et al. Surveillance for Adverse Events After COVID-19 mRNA Vaccination. JAMA. 2021;326(14):1390-1399.
- Dudley MZ, Halsey NA, Omer SB, et al. The state of vaccine safety science: systematic reviews of the evidence. Lancet Infect Dis. 2020;20(5):e80-e89.
- Rudolph A, Mitchell J, Barrett J, et al. Global safety monitoring of COVID-19 vaccines: how pharmacovigilance rose to the challenge. Ther Adv Drug Saf. 2022;13:20420986221118972.
- Kochhar S, Salmon DA. Planning for COVID-19 vaccines safety surveillance. Vaccine. 2020;38(40):6194-6198.
- Soiza RL, Scicluna C, Thomson EC. Efficacy and safety of COVID-19 vaccines in older people. Age Ageing. 2021;50(2):279-283.
- Kamidani S, Rostad CA, Anderson EJ. COVID-19 vaccine development: a pediatric perspective. Curr Opin Pediatr. 2021;33(1):144-151.
- Menni C, Klaser K, May A, et al. Vaccine side-effects and SARS-CoV-2 infection after vaccination in users of the COVID Symptom Study app in the UK: a prospective observational study. Lancet Infect Dis. 2021;21(7):939-949.
- COVID-19 vaccine safety: the AIFA annual report.
- Dumyati G, Jump RLP, Gaur S. Mandating COVID-19 Vaccine for Nursing Home Staff: An Ethical Obligation. J Am Med Dir Assoc. 2021;22(10):1967-1968.
- Faul F, Erdfelder E Fau – Lang A-G, Lang Ag Fau – Buchner A, Buchner A. G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. (1554-351X (Print)).
- https://www.aifa.gov.it/documents/20142/1289678/Comunicato_AIFA_n.627.pdf.
- Sharifian-Dorche M, Bahmanyar M, Sharifian-Dorche A, Mohammadi P, Nomovi M, Mowla A. Vaccine-induced immune thrombotic thrombocytopenia and cerebral venous sinus thrombosis post COVID-19 vaccination; a systematic review. J Neurol Sci. 2021;428:117607.
- Läärä E. Statistics: Reasoning on Uncertainty, and the Insignificance of Testing Null. Annales Zoologici Fennici. 2009;46:138-57.
- Kim HY. Statistical notes for clinical researchers: assessing normal distribution (2) using skewness and kurtosis. Restor Dent Endod. 2013;38(1):52-4.
- Rapporto sulla Sorveglianza dei vaccini anti-COVID.
- Kislaya I, Machado A, Magalhães S, et al. COVID-19 mRNA vaccine effectiveness (second and first booster dose) against hospitalisation and death during Omicron BA.5 circulation: cohort study based on electronic health records, Portugal, May to July 2022. Euro Surveill. 2022;27(37):2200697.
- Tran Kiem C, Andronico A, Bosetti P, et al. Benefits and risks associated with different uses of the COVID-19 vaccine Vaxzevria: a modelling study, France, May to September 2021. Euro Surveill. 2021;26(26):2100533.
- Fiolet T, Kherabi Y, MacDonald CJ, Ghosn J, Peiffer-Smadja N. Comparing COVID-19 vaccines for their characteristics, efficacy and effectiveness against SARS-CoV-2 and variants of concern: a narrative review. Clin Microbiol Infect. 2022;28(2):202-221.
- Troiano G, Nardi A. Vaccine hesitancy in the era of COVID-19. Public Health. 2021;194:245-251.
- Joshi A, Kaur M, Kaur R, Grover A, Nash D, El-Mohandes A. Predictors of COVID-19 Vaccine Acceptance, Intention, and Hesitancy: A Scoping Review. Front Public Health. 2021;9:698111. Published 2021 Aug 13.
- Hudson A, Montelpare WJ. Predictors of Vaccine Hesitancy: Implications for COVID-19 Public Health Messaging. Int J Environ Res Public Health. 2021;18(15):8054. Published 2021 Jul 29.
![]() This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
FEASIBILITY STUDY FOR THE IMPLEMENTATION OF THE SEE AND TREAT PATHWAY IN THE EMERGENCY DEPARTMENT OF SAN CAMILLO-FORLANINI HOSPITAL
Venditti Riccardo1, Marti Flavio2*, Latina Roberto3, Mitello Lucia2, Romanelli Antonio1,
Pucci Antonello1, Mauro Lucia4, Campagna Giuseppe5 and Marucci Anna Rita2
1.Emergency Department Acceptance and Clinical Area, San Camillo-Forlanini Hospital, Rome
2.Department of Health Professions, San Camillo-Forlanini Hospital, Rome
3.PROMISE Department, University of Palermo, Palermo
4.Department of Surgical Sciences, San Camillo-Forlanini Hospital, Rome
5.Department of Medical-Surgical Sciences and Translational Medicine, “La Sapienza” University of Rome, Rome
* Corresponding Author: Flavio Marti. Department of Health Professions, Educational Director Postgraduate Degree in Nursing and Midwifery Sciences, Sapienza University of Rome, San Camillo Forlanini Hospital, C.ne Gianicolense 87, 00159 Rome (Italy). E-mail: flavio.marti@uniroma1.it
ABSTRACT
Introduction: To date, Emergency Department overcrowding represents one of the most important problems regarding the organisation of emergency healthcare. See and Treat was devised in England around the 1980s to provide an effective solution to the overcrowding issue. The Emergency Nurse Practitioner indicates a faster pathway in selected patients with certain characteristics. This model translates into a reduction in waiting times while maintaining the same quality of care.
Aim: To evaluate the potential benefits for patients of the implementation of the See and Treat model within the Emergency Department.
Materials and Methods: Using the GIPSE system, all Emergency Department entries from 2019 have been selected. Minor codes in the triage phase have been considered, as well as those potentially falling within the See and Treat protocol. Each included case has been associated to a See and Treat diagnosis. The waiting time and the time spent in the Emergency Department were derived from the data collected.
Results: 9.41% of the sample is eligible for the See and Treat method, with an average waiting time of one hour and peaks of almost 4 hours for white codes. The application of the See and Treat model to the population covered by our study would reduce the waiting times at the Emergency Department by 6.99%, reduce the simultaneous presence of users on the Emergency Department by 8.88% and reduce the stay for other minor codes by 4.38%.
Discussion: The percentage of patients treatable in the See and Treat system (11%) is in line with the Tuscany trial but statistically lower than the international context (from 63% to 90%). The results obtained from this study showed the significant impact that the See and Treat model could have on reducing overcrowding, positively affecting both users and staff.
Keywords: See and Treat; Emergency Department; overcrowding; advanced nursing skills.
INTRODUCTION
Overcrowding of the Emergency Department (ED) is currently one of the most important problems related to the organisation of emergency health services [1]. In the last decade, the decrease in the number of public and private hospital facilities [2], the growth of the population, the increase in frail patients [3,4] and the population that is not included in the health registry [5], the lack of knowledge of alternative services and the citizen’s belief that they will find a quick solution to a real or perceived problem in the ER [6] have had negative repercussions both on waiting and intervention times, and on the ability of the emergency system to provide adequate solutions to users. All this has burdened the National Health System in terms of quality and efficiency of services [7] also due to a reduction in the number of beds in the ordinary departments and lack of investment in the national network [8].
See and Treat was devised in England in the 1980s to provide an effective response to overcrowding [2]. The figure in charge of this role is the Emergency Nurse Practitioner, who in addition to establishing the usual priorities, indicates a faster professional pathway where patients selected for minor health problems are assessed and treated immediately [9]. The nursing staff operates independently on the basis of protocols that include the possibility of requesting specific tests and prescriptions for drugs, according to current legislation [10]. Studies in the literature show how the introduction of this figure reduces waiting times and overcrowding of the ER [1,11] while guaranteeing the same quality of care [12]. The Emergency Nurse Practitioner is present on a large scale in Northern Europe where nurses with advanced skills play a central role in the See and Treat model, with direct responsibility for the procedures carried out according to certain pre-established protocols [9,13].
In Italy, the See and Treat model has been applied in the Tuscany Region, [14] which, since 2010, has decided to engage in an experimentation project to carry out a profound organisational renewal of emergency departments; this experimentation has resulted in an improvement in the efficiency of ERs, has optimised the management of less critical cases, has reduced waiting times, has improved staff morale, reducing the aggressiveness of users and using nursing and medical resources more appropriately [15,16]. To date, Tuscany represents the only region in which a See and Treat model has been implemented in the safe treatment and discharge of users who access the ER for minor problems, thanks to a theoretical-practical training course for a total of 180 hours (organisational, operational and relational sections) together with work experience in the emergency room of at least 3 years [16].
Objective of the study
The objective of this study is to evaluate the potential benefits for patients accessing the ED of San Camillo-Forlanini Hospital, Rome, in the event of implementation by the Lazio Region of the See and Treat model.
MATERIALS AND METHODS
Sampling and Eligibility
In this paper, with the authorisation of the Health Management of the San Camillo-Forlanini Hospital in Rome, all the accesses to the Emergency Department during the year 2019 considered as minor codes in the triage phase and that potentially fell within the protocols defined by the Tuscany Region for See and Treat [14] were selected, initially by colour code (in force in 2019) and subsequently stratified according a triage statement by operators trained for this activity. Men and women over the age of 16, registered between 1 January 2019 and 31 December 2019, were included. Patients with minor codes (white and green codes) and who had the following items coded in the GIPSE (Emergency Department Information Management) system as their main triage issue were included: trauma or burns; other symptoms and disorders; dyspnoea; intoxication; urological symptoms and disorders; abdominal pain; other nervous system symptoms; allergic reaction; acute neurological syndrome; rhythm disorder; dermatological syndromes or disorders; non-traumatic haemorrhage; arterial hypertension; ENT syndromes and disorders; psychomotor agitation; chest pain and ophthalmological symptoms or disorders. Patients waiting for a visit who absconded from the ED due to waiting were also included as they contributed to the overcrowding figure. Patients with major codes (Red and Yellow) were excluded. Some problems defined in Tuscany Region Resolution [14], which did not congruently adhere to the admission procedures for patients of the San Camillo-Forlanini Hospital Emergency Department, such as paediatric and gynaecological patients, which belong to specific and separate pathways, were excluded.
Tools
The cases under study were identified by means of the GIPSE programme and subsequently collected in a spreadsheet; the division was made in chronological order, by work shift (morning, afternoon and night) using the inclusion and exclusion criteria described above. Each case included was associated with a See and Treat Diagnosis. Information such as age, gender, nationality, triage problem, colour code, date and time of admission, date and time of chart opening, date and time of discharge, access mode, day of the week, discharge to home or outpatient clinic or patient absent on call, triage statement and discharge medical diagnosis were coded. By comparing the admission, history-taking and discharge times, two further parameters were derived from those in our possession: waiting time and length of stay in the emergency department (data not present in GIPSE). The same methodology was subsequently applied to all ineligible patients in the See and Treat pathway to assess for differences.
Ethical Considerations
The study was authorised on 10 March 2021 by the Medical Directorate of San Camillo – Forlanini Hospital. No formal approval by the Local Ethics Committee was required for this study. All data were collected in aggregate form, and the researchers acted in accordance with the ethical considerations of the Declaration of Helsinki.
Statistical Analysis
Data on continuous variables (age, waiting time and time spent in the department) are presented in mean ± SD (Standard Deviation) or median (Q1: 25th centile – Q3: 75th centile); while categorical variables are presented as absolute frequency (n) and percentages (%).
The associations between categorical variables were evaluated through the c2 test; while the difference between two proportions was tested by the z test between two proportions.
The normality/symmetry of the continuous variables (age, waiting time and time spent in the department) compared to the groups (white vs. green, weekdays vs. holidays, females vs. males, Italians vs. foreigners, age classes: ≤48 vs. >48 years) was tested with the Shapiro-Wilk test, the Quantile-Quantile chart control and the verification of the presence of asymmetry and kurtosis.
The comparison between the above-mentioned groups and the continuous variables was tested using the Mann-Whitney test (absence of normality/symmetry); while the Kruskal-Wallis test (absence of normality of the residuals) was used to compare the days of the week and the work shift with respect to the continuous variables (age, waiting time and time spent in the department), the subsequent post-hoc analysis was performed using the Games-Howell method (due to absence of homoschedasticity).
All analyses were performed using SAS v.9.4 and JMP PRO v. 17 software (Institute Inc., Cary, NC, USA). A p-value < 0.05 was considered statistically significant.
RESULTS
The period under study was between 01/01/2019 and 31/12/2019; from the analysis of 29019 ED files divided into three shifts (morning, afternoon and night), 2731 patients eligible for See and Treat were selected, equal to 9.41% of the sample. Table 1 summarises the general data of patients eligible for See and Treat and those in the emergency department.
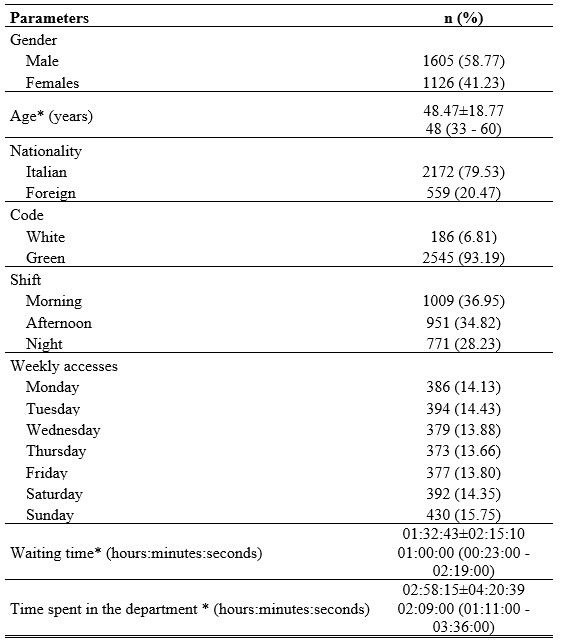
*data presented both as mean±SD and as median (Q1: 25th centile – Q3: 75th centile)
Table 1. Socio-demographic and emergency department characteristics
Analysis by colour code shows that 93.2% (n=2545) of patients were assigned a green code, while the rest were assigned a white code, without differences in the assignment of the colour code between males and females (c2 test, p=0.57) and between age and colour code (Mann-Whitney test, p=0.70); Users assigned a White code waited a median time of 01hr48’:30” more than the green codes (Mann-Whitney test, p<0.0001) and spent 01hr:24’:00” longer in the emergency department than the green codes (Mann-Whitney test, p<0.0001), as shown in table 2.
The majority of users were male at 58.8% (n=1605), the median age of patients was 48 years (Q1: 33 – Q3: 60 years), while the mean was 48.47±18.77 years. The median age of females was 49 years (Q1: 35 – Q3: 62 years), while the mean was 49.93±19.11 years. The median age of males was 47 years (Q1: 32 – Q3: 59), while the mean was 47.45±18.46 years (comparison Females vs. Males: Mann-Whitney test, p=0.001), with a more representative age group in the under-48 age group (52.18%) compared to those older than 48 years (47.82%) (z-test for two proportions, p=0.001).
Gender is associated with age group with a cut-off of 48 years (£48 years – Female/Male: 555 (38.95)/870 (61.05) vs. >48 years – Female/Male: 571 (43.72)/735 (56.28), c2 test, p=0.01). The waiting time after triage before the compilation of the medical history is not affected by either age group or gender (Mann-Whitney test, p=0.71 and p=0.055, respectively).
Gender does not affect the time spent in the emergency department (Mann-Whitney test, p=0.99), while there is an increase in the median time spent in the ED in patients over 48 years of 12 minutes (Mann-Whitney test, p=0.001), a data item highlighted in table 2.
79.5% of users were Italian while 20.5% of the sample came from other countries. Foreign nationality (table 2) affects waiting time, increasing it by a median of 27 minutes (Mann-Whitney test, p<0.0001) and time spent in the ED is increased by a median of 26 minutes (Mann-Whitney test, p<0.0001).
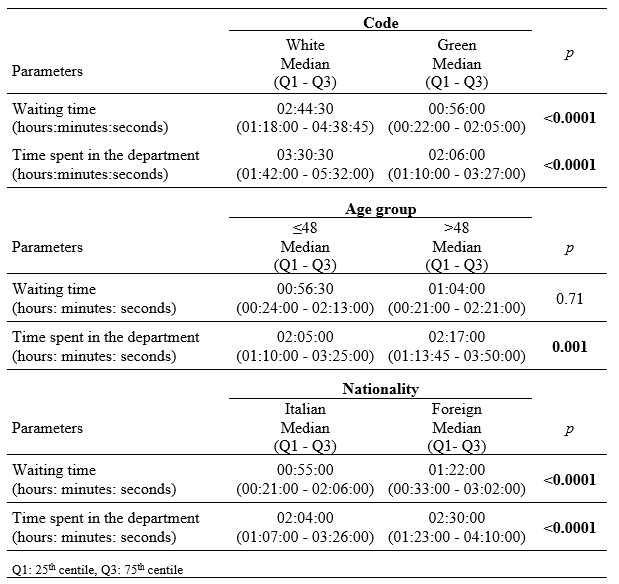
Table 2. Difference of waiting time and time spent in the department with respect to code, age group and nationality.
Accesses during the different days of the week were homogeneous except for a peak of influx on Sundays (Figure 1); however, no differences were found between access on weekdays versus holidays with gender (c2 test , p=0.94), age (Mann-Whitney test, p=0.80), waiting time (Mann-Whitney test, p=0.38) and time spent in the ED (Mann-Whitney test, p=0.10). Accesses in the various months of the year were uniform except for the month of January where there was a greater influx equal to 10.9% of the total.
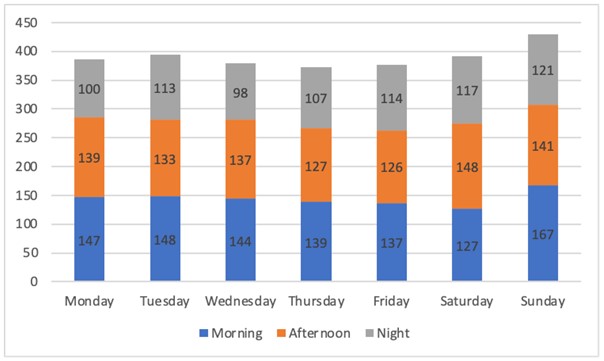
Figure 1. Accesses by day of the week and by shift
The analysis of accesses conducted with respect to work shifts (morning: 07:00 – 13:30, afternoon 13:30 – 19:50, night 19:50 – 07:00) showed a greater influx in the morning shift (36.9%) followed by the afternoon shift (34.8%) while the remaining 28.2% of the patients included came in during the night shift (c2 test, p=0.02) (Figure 1).
The post-hoc analysis (table 3) shows that the median age of patients tends to be higher in the morning shift compared to the afternoon shift (Kruskal-Wallis test and Games-Howell test, p<0.0001) and the night shift (Games-Howell test, p<0.0001). The median waiting time is 22 minutes longer in the morning shift than in the afternoon shift (Kruskal-Wallis test and Games-Howell test, p<0.0001) and 25 minutes longer than in the night shift (Kruskal-Wallis test and Games-Howell test, p<0.0001). The median time spent in the ED is 12 minutes shorter in the morning shift compared to the afternoon shift (Kruskal-Wallis test and Games-Howell test, p=0.001) and 8 minutes longer in the afternoon shift compared to the night shift (Kruskal-Wallis test and Games-Howell test, p=0.003).

Table 3. Differences between the variables indicated and the shift
By dividing patients by the categories defined by the model proposed by the Tuscany region [10], 57.7% of the sample came to the ED for trauma-related problems and 12% for musculoskeletal problems; small wounds, manageable through the See and Treat model were detected in 27.8% of cases. 81.1% of the patients completed the course of treatment while the rate of leaving the ED without receiving any treatment was found to be 16.2%. Among these users, about one in four (23.5%) had been assigned a white code. Of the selected patients, 18.5% did not need an estimation of days of illness, while 64% of them had a prognosis of 1 to 7 days; 36.4% of the sample were scheduled for a follow-up appointment in outpatient facilities. Excluding from our study population the patients eligible for See and Treat (thus creating a parallel pathway for 9.41% of the patients attending the ED) would have led to an average reduction in waiting times at the ED of 6.99%; the simultaneous presence of users in the ED would have decreased on average from 84.14 to 76.5 with a decrease of 8.88%. By freeing up resources, it would have been possible to provide each patient with a minor code, not included in the See and Treat pathway, with 19 minutes more of hospital care, thus achieving a reduction in the length of stay in the ED for minor codes of 4.38%.
DISCUSSION
The objective of this study was to evaluate the potential benefits for patients attending the ED of the San Camillo-Forlanini Hospital in Rome if the See and Treat model had been implemented by the Lazio Region. The results obtained showed that the percentage of patients treatable through the See and Treat regimen in our study (9.4%) is in line with that of the Tuscany trial where 11% of the patients in the sample fell into this category [16]. However, these data are not in line with the international literature, which shows that the use of the See and Treat model increases the percentage of patients seen from 63% to 90% [1]. This difference could be attributed to the fact that, in Italy, the figure of the Emergency Nurse Practitioner is not recognised [17], consequently the nurse specialised in first aid interventions, thus defined by the Tuscany region after participation in the pre-established training course to provide care in the See and Treat model [14] has less professional autonomy and can treat a limited number of issues [18,19]. In the study presented, the frequency of green codes is significantly higher (93.2%) than that of white codes, which by definition are considered inappropriate in an emergency department [20]. This figure is consistent with that of the 2010 Nati study, which described the management of white and green codes in the Emergency Department, by general practitioners, which reported 88.9% of green codes compared to 11.1% of white codes [21]. Of the patients selected, a considerable portion, 20.5%, was of foreign origin, a figure greater than the results of other studies carried out in Italy where the number of accesses to the ED by foreign citizens is 13% [22]; they waited longer than Italians both in terms of admission to the EDand their stay there. This figure can be linked to the difficulty of accessing health services for foreigners, who come to the ED to solve their health problems [21]. The mean age of the sample (48.5 years) was found to be in line with the study of Nati et al. where the age of the selected patients was 48.3 years [21]; patients over 48 years of age had a longer stay in the ED, probably due to comorbidities, which, among other things, can exclude (as per protocol) some of them from the See and Treat pathway (52.18% of patients under 48 years of age and 47.82% of patients over this age); this conclusion has not emerged in other studies, however. The Tuscan model includes a See and Treat clinic operating 7 days a week from 8 a.m. to 8 p.m. [14]. Our study showed that there is a uniformity of accesses in different months and on different days of the week. These data differ from the study performed by Fiorentini et al. in 2013 where the “Monday effect” and a general greater number of inappropriate accesses coinciding with the summer months were highlighted [23]. Fundamental to the organisation of this pathway is the data on patient accesses in the various shifts; the data that emerged (morning shift 36.9%, afternoon shift 34.8% and night shift 28.2%) is comparable to that of the study carried out by Fiorentini et al. where the distribution by time bracket of patients with minor codes was uniform, with peaks in the morning hours and a gradual reduction in accesses in the remaining part of the day [23]. The greater influx in the morning hours generates an overcrowding of the ED in the afternoon, which is reduced in the night shift as a result of fewer admissions. 57.7% of the patients in our study went to the ED for trauma-type problems (minor contusions of the limbs, uncomplicated hand and foot trauma, wounds, abrasions, superficial fingertip avulsion, insect bites and removal of stitches), while in the Tuscany trial the results showed that patients with these problems accounted for 70% of the sample analysed; specifically, the most frequent “See and Treat diagnosis” in our research was “wounds” with 27.8%, followed by “trauma of the fingers and toes” with 14.3%. The number of wounds appears to be higher than that of the study conducted by Righi in 2020, where patients with wounds accounted for only 18.2% [24]. Finally, the use of See and Treat would reduce the mean waiting times of the general user for minor codes by 6.99% and the time spent in the ED by 4.38%. The data from the Tuscany region show reductions of 46.4% in waiting times and 22.2% in the time spent in the ED [25]; these differences are probably attributable to the different conditions in which See and Treat was applied in Tuscany.
CONCLUSIONS
The results of this study showed the significant impact that the See and Treat pathway could have on reducing overcrowding. Every month in the ED, 2418 patients with minor codes accessed the department with a simultaneous average presence of 84.14 patients, 7.48 of whom were eligible for the See and Treat pathway. The implementation of a See and Treat pathway could result in an 8.88% reduction in overall average attendances, bringing benefits such as reducing the average ED attendance to 76.5 patients per day. Reducing overcrowding would have a positive impact on both the users (delays in care, reduction in violence towards staff, reduction in legal disputes, reduction in the rate of abandonment of the ED and greater satisfaction in the care received) and the staff (reduction in errors, reduction in sentinel events, reduction in job stress, greater job satisfaction, and fewer delays in patient transfers) [7]. However, See and Treat is not the only solution to the problem of overcrowding, also considering that to date there are no studies in the literature that demonstrate the economic benefits of one model compared to another [9]. Other models include the Minor Injuries Units (MIUs), departments dedicated to certain minor emergencies with waiting times usually shorter than those in the Emergency Department, or the Fast Track model where, following Triage, the nurse independently and after assessing and ascertaining the user’s health needs sends them directly to the appropriate specialist if they have a minor pathology clearly suited to treatment by a single specialist. [18,19,26]. To conclude, a state-of-the-art model such as See and Treat applied in a large emergency department would significantly reduce the phenomenon of overcrowding by reducing waiting times, time spent in the ED and the total number of patients present in the department as well as reducing the number of voluntary abscondment from the ED. The development of greater nursing skills can contribute to the management of a See and Treat pathway with the ultimate aim of improving patient outcomes.
Limitations of the study
The fact that the study is a single-centre study is the main limitation of this paper; moreover, it was decided to analyse data from a period prior to the COVID-19 pandemic as it temporarily changed the pattern of access to the Emergency Department.
Possible Funding
This research did not receive any form of funding
Conflicts of interest
The authors declare that they have no conflicts of interest associated with this study
Contributions of the authors
Design: Riccardo Venditti and Anna Rita Marucci. Data acquisition, analysis or interpretation: Riccardo Venditti, Antonio Romanelli, Anna Rita Marucci, Flavio Marti. Statistical analysis: Giuseppe Campagna. Critical review of the article: Anna Rita Marucci, Flavio Marti, Roberto Latina, Lucia Mitello, Antonello Pucci, Lucia Mauro.
REFERENCES
- Jeyaraman MM, Alder RN, Copstein L, Al-Yousif N, Suss R, Zarychanski R, et al. Impact of employing primary healthcare professionals in emergency department triage on patient flow outcomes: a systematic review and meta-analysis. BMJ Open. 20 aprile 2022;12(4):e052850.
- Polello L, Boscolo Anzoletti A. See and Treat: ambulatorio per i codici minori come soluzione al sovraffollamento del Pronto Soccorso. L’Infermiere. 2015;2:28–31.
- Vetrano D. La Mappa della fragilità in Italia [Internet]. 2022. Disponibile su: https://www.italialongeva.it/wp-content/uploads/2022/04/indagine-2022_italialongeva.pdf
- ISTAT, curatore. Gli anziani e la loro domanda sociale e sanitaria [Internet]. 2021. Disponibile su: https://www.istat.it/it/files//2021/06/rapporto_commissione_anziani.pdf
- Ministero dell’Interno. Sbarchi e accoglienza dei migranti [Internet]. 2022. Disponibile su: https://www.interno.gov.it/sites/default/files/2022-12/cruscotto_statistico_giornaliero_21-12-2022.pdf
- Langiano T, Romagnoli C, Traversa G. Misura dell’Appropriatezza [Internet]. Ministero della Salute; 2007 [citato 15 giugno 2022]. Disponibile su: http://www.mattoni.salute.gov.it/mattoni/documenti/Documento_riepilogativo_Comitato_Scientifico.pdf
- Rastelli G, Cavazza M, Cervellin G. Sovraffollamento in Pronto Soccorso: Analisi del fenomeno e proposte di gestione. Emerg Care J. 2010;2(VI):25–35.
- Ministero della Salute. Annuario Statistico del Servizio Sanitario Nazionale [Internet]. 2020. Disponibile su: https://www.salute.gov.it/portale/documentazione/p6_2_2_1.jsp?lingua=italiano&id=3245
- Trisyani Y, Windsor C. Expanding knowledge and roles for authority and practice boundaries of Emergency Department nurses: a grounded theory study. Int J Qual Stud Health Well-Being. dicembre 2019;14(1):1563429.
- Hoyt KS, Evans DD, Wilbeck J, Ramirez E, Agan D, Tyler D, et al. Appraisal of the emergency nurse practitioner specialty role. J Am Assoc Nurse Pract. ottobre 2018;30(10):551–9.
- Lyons M, Brown R, Wears R. Factors that affect the flow of patients through triage. Emerg Med J EMJ. febbraio 2007;24(2):78–85.
- Levati S, Capitoni E. L’impatto del ruolo delle Emergency Nurse Practitioners nella gestione clinica dei pazienti nel contesto di un Dipartimento di Emergenza Urgenza nel Regno Unito. Prof Inferm. 30 aprile 2014;65(2).
- Dwyer T, Craswell A, Browne M. Predictive factors of the general public’s willingness to be seen and seek treatment from a nurse practitioner in Australia: a cross-sectional national survey. Hum Resour Health. 17 febbraio 2021;19(1):21.
- Giunta Regionale Toscana. Progetto di sperimentazione del modello See and Treat in pronto soccorso – revisione. Delibera n 449 mar 31, 2010.
- Brebner JA, Ruddick-Bracken H, Norman JN, Page JG. The nurse practitioner: management of minor trauma. Accid Emerg Nurs. gennaio 1996;4(1):43–6.
- Rosselli A, Becattini G, Cappugi M, C Francois, Ruggeri M. See & Treat. Protocolli medico-infermieristici: la sperimentazione toscana nei pronto soccorso. Firenze: Giunti; 2015. 38 p.
- Bornaccioni C, Coltella A, Pompi E, Sansoni J. Accessi non urgenti nel Dipartimento di Emergenza (D.E.) e ruoli dell’infermiere. Una revisione narrativa della letteratura. Prof Inferm. 10 novembre 2014;67(3).
- Bambi S, Giusti M, Becattini G. See & Treat in pronto soccorso: dal medico all’infermiere con competenze avanzate. Una revisione della letteratura. Assist Inferm E Ric. 2008;27(3).
- Radice C, Ghinaglia M, Doneda R, Bollini G. «See and Treat» in the Emergency Department: legal aspects and professional nursing responsibility. Prof Inferm. 2013;66(3):175–81.
- Lamanna C, Trastulli E. Accessi impropri al Pronto Soccorso e H24. Riv Soc Ital Med Gen. 2012;4:27–8.
- Nati G, Ialongo A, Fucito G, D’Angelo E, de Lucia L, Valente F, et al. Il management dei codici bianchi e verdi da parte dei medici di medicina generale in un Pronto Soccorso di Roma: lo studio MAPS. Riv Soc Ital Med Gen. 2010;3:18–22.
- Bongiovanni A, Canepari F, Ferraris P, Negri P, Pitisano C. Accessi dei cittadini stranieri al Pronto Soccorso dell’Azienda Ospedaliera SS. Antonio e Bigio e C. Arrigo di Alessandria (anni 2011 – 2012). Work Pap Public Health. 15 giugno 2013;2(1).
- Fiorentini G, Lippi Bruni M, Mammi I, Ugolini C. Valutazione dell’impatto prodotto nelle Regioni monitorate per la riduzione degli accessi impropri in Pronto soccorso. Quad Monit. 2013;32:87–108.
- Righi L, Jasmine L, Ronchese F, Trapassi S. Le urgenze minori in pronto soccorso: analisi del percorso See and Treat all’interno del Presidio Ospedaliero Misericordia di Grosseto. novembre 2020;64:1–3.
- Rosselli A, Francois C, Massai D, Becattini G, Paffetti M, Ruggeri M, et al. Risultati della sperimentazione del See and Treat. Toscana Medica. 2011;29(9):17–9.
- Lindner G, Woitok BK. Emergency department overcrowding : Analysis and strategies to manage an international phenomenon. Wien Klin Wochenschr. marzo 2021;133(5–6):229–33.
ANALYSIS OF PSYCHOSOCIAL STATUS AND QUALITY OF LIFE IN THE ELDERLY WITH OSTEOARTHRITIS DURING THE COVID-19 PANDEMIC: A CROSS SECTIONAL STUDY
Mohd Syukri1*, Dewi Masyitah1, Mashudi1, Lailatul Fadilah2
1. Department of Nursing, Health Polytechnic, Ministry of Health Jambi, Indonesia
2. Department of Nursing, Health Polytechnic, Ministry of Health Banten, Indonesia
* Corresponding author: Mohd Syukri, Jl. Dr. Tazar, Buluran Kenali, Kec. Telanaipura, Kota Jambi, Jambi 36361, Indonesia, Orcid: https://orcid.org/0000-0003-2061-5531
Email: syukrimuh290@gmail.com
ABSTRACT
Introduction: Along with increasing age, there will also be an increasing tendency to get sick and have physical limitations (disabilities) due to a drastic decline in physical abilities. These conditions are the leading cause of high mortality and morbidity in the elderly, especially during the Covid-19 pandemic. The current study aims to analyze the relationship between psychosocial status and the quality of life of the elderly with osteoarthritis during the Covid-19 pandemic.
Materials and Methods: This cross-sectional study was located at a nursing home in Jambi, involving 351 randomly selected participants. Measure the psychosocial status of the elderly using the Indonesian version of the Self Reporting Questionnaire (SRQ) and the quality of life using the Indonesian version of the World Health Organization Quality of Life-Old (WHOQOL – OLD) questionnaire.
Results: Most elderly have a good quality of life, as many as 229 (65.1%), while a poor quality of life, as many as 30 people (8.5%). In the psychosocial variables, most respondents did not experience mental health disorders, as many as 260 people (74.1%). The Mann-Whitney test showed a significant relationship between Quality of Life and Psychosocial Status, in particular we obserbed in subjects without mental disorders in comparison to subjects with mental disorders a better quality of life, i.e. the elderly who do not suffer from mental disorders will show a tendency for a good quality of life.
Conclusions: Psychosocial status related to quality of life in the elderly with osteoarthritis during the Covid-19 pandemic. The elderly who do not suffer from mental disorders will show a tendency for a good quality of life.
Keywords: Elderly; Covid-19; Psychosocial; Quality of life
INTRODUCTION
Qualified elderly are elderly who, through the aging process, remain healthy and optimal physically, socially, and mentally to remain prosperous throughout life and participate in improving the quality of life as members of society [1,2]—osteoarthritis in the elderly results in limitations in carrying out daily activities independently. A study revealed that 2.6% of the elderly experienced total dependence, 1.2% with moderate support, and 96.3% with mild reliance [3]. Dependence, coupled with lifestyle changes, is one of the factors causing stress in the elderly [4,5].
The elderly with osteoarthritis who experience stress tend to experience sadness, and the body becomes weak, with reduced appetite and interest in all things [6,7]. As a result, they will experience delays in treatment, especially in the second year of the Covid-19 pandemic, where there is a statistical increase in cases in various parts of the world, including some areas in Indonesia, where the elderly are a group that is vulnerable to infection. The number of deaths continues to increase, especially in the elderly group [8–10]. If this condition is allowed to drag on, it will trigger depression. In addition, the elderly will find it difficult to motivate themselves to recover. The adaptation process that must undertake to all the changes experienced makes the elderly vulnerable to psychological disorders such as unstable emotional conditions, depression, or anxiety, and it may reduce the quality of life of the elderly [11,12].
Crisis in the elderly can be expressed as a condition of psychosocial disorders with characteristics including dependence on others, isolating themselves, or withdrawing from social activities for various reasons. The reasons include undergoing retirement, severe and prolonged illness, the death of a spouse, and undergoing health protocols during the Covid-19 period, where everyone must keep their distance and isolate themselves [6,13]. For the elderly, changing roles in the family, socio-economic, and social community resulted in setbacks in adapting to the new environment and interacting with the social environment [11,14].
Quality of life is a strategic issue that reflects the condition of the elderly in enjoying the rest of their life and preparing to die peacefully. Therefore, factors affecting the quality of life of the elderly should be accommodated by the elderly, families, and health providers [15,16]. One of the health service providers on the first line is the Public Health Center (PHC). PHC as a health service provider and acting as a center for community health development in its working area should develop health programs based on problems that develop in the community [17,18].
Psychological factors, as assessed by the Geriatric Depression Scale, and sociodemographic characteristics, such as marital status, income and leisure activities, had an impact on quality of life [19]. Other studies show that apart from social demographic factors, social organization and social support affect the quality of life of the elderly [20], and the ability to perform daily routine activities is the strongest predictor [21]. In addition to the aforementioned factors, it is necessary to explore the effects of the psychosocial status of the elderly during the Covid-19 pandemic because the elderly are prone to depression. Preliminary research shows an increase in depression, post-traumatic anxiety, and adjustment disorders in the elderly, and the risk of suicide increases sharply. Stress can also lower the body's immunity, worsening the condition of the elderly who are already physically weak. Patients with a previous psychiatric disorder will tend to experience worsening [3,20].
The elderly group is very vulnerable to contracting Covid-19, plus declining physical health conditions are increasingly impacting the decline in the quality of life of the elderly, increasing mortality rates in the elderly group. For this reason, it is necessary to survey psychosocial health status, response, and quality of life during the Covid-19 pandemic. This study explores the psychosocial problems of the elderly with osteoarthritis during the Covid-19 pandemic.
MATERIALS AND METHODS
Study design
The type of research is analytic observational using the research design is cross sectional study.
Study Population
This study was conducted at the Jambi Nursing Home involving 351 randomly selected participants with the following sample criteria including age 55 years, living in Jambi Nursing Home for at least one year.
Instruments
Psychosocial status was measured using the Indonesian version of the Self-Reporting Questionnaire (SRQ), which consisted of 29 questions about the respondent's condition during the last 30 days [21]. The Indonesian version of the SRQ-20 has 5 dimensions, namely energy, cognitive, depression, physiology, and anxiety. The YES answers to items 1 to 20 (symptoms of neurosis) indicated a psychological problem, and item number 21 meant using a psychoactive substance. One YES answer from items 22 to 24 (psychotic symptoms) indicates a severe problem and needs further treatment. One YES answer to items 25-29 indicates the presence of symptoms of PTSD (Post Traumatic Stress Disorder).
Psychosocial status was categorized into suffering and not suffering from mental disorders. A mental disorder is declared if at least 5 neurotic symptoms are found or there is at least 1 psychotic or PTSD (Post Traumatic Stress Disorder) symptom on the Self-Reporting Questionnaire (SRQ). Meanwhile, it is declared not suffering from mental disorders if there are only 4 items of neurotic symptoms and there are no psychotic symptoms or PTSD (Post Traumatic Stress Disorder) symptom on the Self-Reporting Questionnaire (SRQ). The variable “Psychosocial status” assigning the scores: 1 = suffering and 0 = not suffering for mental disorders.
Measurement of quality of life used the Indonesian version of the World Health Organization Quality of Life-Old (WHOQOL – OLD) questionnaire, which contains the respondents' living conditions in the last four weeks consisting of 26 questions [22]. The variable “Quality of Life”, assigning the scores: 1 = poor, 2= moderate, 3 = good, and 4 = very good for each subject.
The Indonesian version of the World Health Organization Quality of Life-Old (WHOQOL – OLD) questionnaire consists of the Herth Hope Index, Perceived Social Support from Friends (PSS-Fr), Perceived Social Support from Family (PSS-Fa) [22]. The Indonesian version of the WHOQOL-BREFF questionnaire has been tested for validity and reliability by Priastana et al. [22] with a rcount value (0.361) and a Cronbach Alpha value = 0.965, so researchers do not need to test the validity and reliability again.
Sample size
The number of samples involved was 351 participants who were randomly selected from the population. Calculating the number of samples is determined using the Slovin formula [23], where from 2.880 people in the population, d = 0.05, the number of samples is 351.
Ethical Consideration
No economic incentives were offered or provided for participation in this study. The study protocol matched the Declaration of Helsinki ethical guidelines for clinical studies. This research has been approved by the Health Research Ethics Commission of the Health Polytechnic of the Jambi Ministry of Health with the number LB.02.06/2/111/2022.
Statistical analysis
Data are presented as number and percentage for categorical variables, and continuous data expressed as the mean ± standard deviation (SD) or median with Interquartile Range (IQR). The results of data normality analysis using the Kolmogorov Smirnov test showed that the data were not normally distributed. We found the relationship between Quality of Life and Mental disorders using the Mann–Whitney test (ordinal data vs dichotomous).
We considered all tests with P-value< 0.05 as significant. The statistical analysis was performed by SPSS software version 16.0.
RESULTS
The distribution of the characteristics of the research respondents is presented in table 1.

Table 1. Distribution of the Respondents characteristics
Table 1 show that most respondents were 55-64 years, as many as 186 (53%). Most sexes are male, with as many as 225 (64.1%) respondents. Most respondents had a high school education, with 227 (64.7%).
Table 2 shows that most elderly have a good quality of life, as many as 229 (65.1%), while a poor quality of life, as many as 30 people (8.5%).
In the psychosocial variables, most respondents did not experience mental health disorders, as many as 260 people (74.1%).
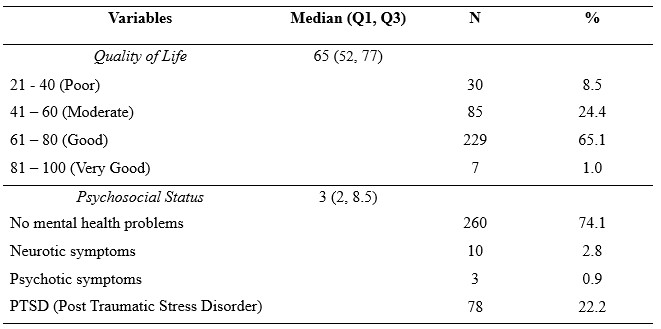
Table 2. Distribution of study variables
Table 3 shows that of the 91 respondents who do have mental disorders, there are 46 respondents with a moderate quality of life category. Of the 260 respondents with not mental disorders, there are 218 respondents have a good quality of life category
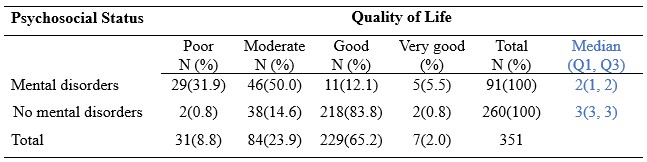
Table 3. Relationship between Psychosocial Status and Quality of Life in the Elderly
The Mann-Whitney test showed a significant relationship between Quality of Life and Psychosocial Status, in particular we obserbed in subjects without mental disorders in comparison to subjects with mental disorders a better quality of life (median: 3 vs 2, p<0.0001), i.e. the elderly who do not suffer from mental disorders will show a tendency for a good quality of life.
DISCUSSION
Elderly stress arises from anxiety about various diseases, including Covid-19. The current study aims to analyze the relationship between psychosocial conditions and the quality of life of the elderly with osteoarthritis during the Covid-19 pandemic.
The results of this study reported that on the psychosocial variables of the elderly, most of the elderly did not experience mental health disorders, as many as 260 people (74.1%) and the elderly and around 25.9% of the elderly experienced mental disorders ranging from PTSD (Post Traumatic Stress Disorder), neurotic and psychotic. Mental disorders experienced by the elderly include the elderly avoiding interacting with other people, decreasing interest in routine activities, always remembering the impact of Covid-19 and feeling disturbed, lack of appetite, not sleeping well, and feeling anxious. Symptoms of this health disorder significantly interfere with the quality of life of the elderly [24].
Anxiety, as a symptom of stress in the elderly in the Covid-19 pandemic situation, should receive support from spouses and family members by being willing to listen to the complaints of the elderly, being able and having time always to be near and accompany the elderly. Elderly family members are also responsible and act as friends of the elderly in dealing with their day-to-day. Likewise, in elderly stress, there is family support to maintain health by supporting the health of the elderly [25].
The increasing number of Covid-19 cases harms everyone's mentality, especially the elderly. SARS-CoV-2 is highly contagious. Even some cases develop into respiratory failure, which will progress to death. Deterioration of the patient's condition is more common in the elderly and those with previous co morbidities (hypertension, diabetes, heart disease) [26,27]. The elderly group (elderly) has physical and psychological weaknesses during the Covid-19 pandemic. About 20% of deaths with Covid-19 in China are over 60 years old [28].
The effects of quarantine are loneliness, sadness, and prolonged stress. Preliminary research suggests an increase in depression, post-traumatic stress, adjustment disorders in the elderly, and the risk of suicide [29]. Stress lowers immunity. This situation can worsen the condition of the elderly, who are already physically weak. Patients with previous psychiatric conditions will tend to experience worsening, one of which is the problem of osteoarthritis [30].
The main problem often experienced by the elderly with osteoarthritis is joint pain. Pain will increase when doing activities, which limits a person's activities. The decrease in physical activity will affect the patient's daily life activities and the quality of his life. A further consequence of osteoarthritis is decreased functional activity, especially difficulty rising to a sitting position, walking, and going up and down stairs [31,32]. The elderly with osteoarthritis will experience joint and muscle dysfunction, so they will experience limited movement, decreased strength, and muscle balance. About 18% experience difficulties and limitations in activities, loss of function of work capacity, and decreased quality of life [33,34].
According to Hong's study [35], the elderly with osteoarthritis have a poorer quality of life than the elderly without osteoarthritis. This condition is associated with decreased physical function due to joint inflammation caused by joint damage. Therefore, it is highly recommended that families take care of the mental health of the elderly during Covid-19 so that it does not affect their physical health. Maintaining the mental health of the elderly during the Covid-19 pandemic requires assistance from all parties. Families, health workers, the government, and the elderly must cooperate. In addition, the knowledge, attitude, and behavior of the elderly need to be improved to deal with the Covid-19 pandemic. Adaptation and survival are the keys to overcoming this pandemic condition [29].
The primary strategy is to ensure that the elderly always maintain physical distance, wash their hands, use masks, eat nutritious foods, and do light exercise [36,37]. Other activities that can be done indoors, such as reading books, painting, or watching movies, can still be done. Explanations should be given as concisely as possible to the elderly. If the elderly understand, they will feel safe and peaceful and improve their quality of life. Social relations with family and friends must still be carried out through communication tools. Emotional support is crucial for the elderly who live alone. They are prone to anxiety and confusion during this uncertain period [9,38].
Visits to the doctor should be replaced with telemedicine. Patients can consult via Whatsapp, telephone, short message, Zoom, or any application. All planned surgeries should be postponed, such as cataracts, hernias, and kneecap replacements [38]. Any redundant information about Covid-19 should be reduced to prevent panic and misunderstanding. Information should focus on preventive measures, not on myths alone. Health information, updates about Covid-19, and psychological consultations should be provided by telephone or online by the government [30,39]. Although the elderly may appear weak from the outside, the family must try to give them a sense of freedom, respect, and genuine care. The elderly must still be involved in decision-making [40].
The World Health Organization (WHO) emphasizes the importance of psychosocial needs for the elderly [38]. The government is expected to provide basic needs for the elderly, especially those less well off financially and psychologically. The items that is important to prepare including food, medicines, and disinfectants. The need for security is essential and should not be ignored [41].
The strength of this study is that the two questionnaires used, namely the Self Reporting Questionnaire (SRQ) and the World Health Organization Quality of Life-Old (WHOQOL – OLD) questionnaire, have used the Indonesian version of the questionnaire to reduce research bias.
CONCLUSION
Psychosocial status related to quality of life in the elderly with osteoarthritis during the Covid-19 pandemic. The elderly who do not suffer from mental disorders will show a tendency for a good quality of life.
LIMITATIONS
The research location only involves 1 place so that it cannot compare the results of similar studies in different populations, so in the future research must be carried out involving several regions. Another limitation is the cross-sectional research design because it only measures the current condition of the variables, so it can cause research results to be biased.
FUNDING STATEMENT
This research did not receive any specific grant from funding agencies in the public, commercial, or not for profit sectors.
COMPETING INTERESTS STATEMENT
There are no competing interests for this study.
AUTHORS’ CONTRIBUTION
All authors equally contributed to preparing this article.
REFERENCES
- do Nascimento RJ, Barbosa Filho VC, Rech CR, Brasil RB, Junior RC, Streit IA, et al. Changes in Health-Related Quality of Life and Physical Activity Among Older Adults in the First-Wave COVID-19 Outbreak: A Longitudinal Analysis. Journal of Aging and Physical Activity. 2021;30(3):389–96.
- Ragni E, Mangiavini L, Viganò M, Brini AT, Peretti GM, Banfi G, et al. Management of Osteoarthritis During the COVID‐19 Pandemic. Clinical Pharmacology & Therapeutics. 2020;108(4):719–29.
- Pramono YS, Yuniarti Y, Anggraini L. Hubungan Derajat Insomnia Dengan Pemenuhan Kebutuhan Activity Of Daily Living Pada Lansia Di Panti Sosial Budi Sejahtera Banjarbaru 2019. Dinamika Kesehatan: Jurnal Kebidanan dan Keperawatan. 2019;10(2):916–27.
- Lábadi B, Arató N, Budai T, Inhóf O, Stecina DT, Sík A, et al. Psychological well-being and coping strategies of elderly people during the COVID-19 pandemic in Hungary. Aging & Mental Health. 2022;26(3):570–7.
- Nimitha KJ, Singh B, Srivastava RN, Kumar R. SYMPOSIUM Health Related Quality Of Life And Depression In Older Adults With Knee Osteoarthritis Pain-Cross-Sectional Telephonic Survey In Covid 19 Pandemic. Indian journal of psychiatry. 2022;64(Suppl 3):S634.
- Giacalone A, Rocco G, Ruberti E. Physical health and psychosocial considerations during the COVID-19 outbreak. Psychosomatics. 2020;61(6):851–2.
- Dubey S, Biswas P, Ghosh R, Chatterjee S, Dubey MJ, Chatterjee S, et al. Psychosocial impact of COVID-19. Diabetes & Metabolic Syndrome: clinical research & reviews. 2020;14(5):779–88.
- Onder G, Rezza G, Brusaferro S. Case-fatality rate and characteristics of patients dying in relation to COVID-19 in Italy. Jama. 2020;323(18):1775–6.
- Lee K, Jeong G-C, Yim J. Consideration of the psychological and mental health of the elderly during COVID-19: A theoretical review. International journal of environmental research and public health. 2020;17(21):8098.
- Akat M, Karataş K. Psychological effects of COVID-19 pandemic on society and its reflections on education. Electronic Turkish Studies. 2020;15(4).
- Min Fui W, Abdul Majid H, Ismail R, Su TT, Maw Pin T, Said MA. Psychosocial factors associated with mental health and quality of life during the COVID-19 pandemic among low-income urban dwellers in Peninsular Malaysia. PloS one. 2022;17(8):e0264886.
- Bidzan-Bluma I, Bidzan M, Jurek P, Bidzan L, Knietzsch J, Stueck M, et al. A Polish and German population study of quality of life, well-being, and life satisfaction in older adults during the COVID-19 pandemic. Frontiers in psychiatry. 2020;11:585813.
- Wiraini TP, Zukhra RM, Hasneli Y. Hubungan Dukungan Keluarga Dengan Kualitas Hidup Lansia Pada Masa COVID-19. Health Care: Jurnal Kesehatan. 2021;10(1):44–53.
- Muliani R, Jayanti TN, Dirgahayu I, Safarudin I, Anri A. Psychosocial Support in Increasing COVID-19 and Mental Health in The Elderly. JCES (Journal of Character Education Society). 2021;4(1):135–47.
- Zulka AN, Suryaningsih Y, Wulandari PNM, Putri DA. Evaluasi Manajemen Penyakit dan Psychological Well Being Lansia di Masa Pandemi Covid 19. The Indonesian Journal of Health Science. 2022;14(1):84–91.
- Juwita R. Meningkatkan Kualitas Hidup Lansia Pasca Pandemi Covid 19. Jurnal Mitra Prima. 2022;4(2).
- Rayani D, Purqoti DNS. Kecemasan Keluarga Lansia Terhadap Berita Hoax Dimasa Pandemi COVID-19. Realita: Jurnal Bimbingan dan Konseling. 2020;5(1).
- Syahruddin S. Kebugaran Jasmani Bagi Lansia Saat Pandemi Covid-19. JUARA: Jurnal Olahraga. 2020;5(2):232–9.
- Alexandre T da S, Cordeiro RC, Ramos LR. Factors associated to quality of life in active elderly. Revista de saude publica. 2009;43:613–21.
- Guida C, Carpentieri G. Quality of life in the urban environment and primary health services for the elderly during the Covid-19 pandemic: An application to the city of Milan (Italy). Cities. 2021;110:103038.
- Idaiani S, Suryaputri IY, Mubasyiroh R, Indrawati L, Darmayanti I. Validity of the Self Reporting Questionnaire-20 for Depression Based on National Health Survey. 2021;
- Priastana IKA, Kusumaningtiyas DPH. Quality of Life in The Elderly Viewed from Hope, Friend Support, and Family Support. STRADA Jurnal Ilmiah Kesehatan. 2020;9(2):1670–5.
- Sugiyono. Metode penelitian pendidikan pendekatan kuantitatif, kualitatif dan R&D. Alfabeta; 2013.
- Widyaningrum DA, Umam FN. Pengaruh Nyeri Sendi Terhadap Kualitas Tidur dan Kualitas Hidup Pada Lansia Penderita Osteoartritis. Jurnal Keperawatan. 2020;13(2):7.
- Intarti WD, Savitri NPH. Manfaat Relaksasi Yoga Dan Swedish Massage Terhadap Stress Lansia Saat Pandemi Covid-19. Jurnal Bina Cipta Husada. 2021;17(1):96–112.
- Banerjee D. ‘Age and ageism in COVID-19’: Elderly mental health-care vulnerabilities and needs. Asian journal of psychiatry. 2020;51:102154.
- Jing Z, Li J, Wang Y, Ding L, Tang X, Feng Y, et al. The mediating effect of psychological distress on cognitive function and physical frailty among the elderly: evidence from rural Shandong, China. Journal of affective disorders. 2020;268:88–94.
- Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. jama. 2020;323(13):1239–42.
- Perrotta F, Corbi G, Mazzeo G, Boccia M, Aronne L, D’Agnano V, et al. COVID-19 and the elderly: insights into pathogenesis and clinical decision-making. Aging clinical and experimental research. 2020;32(8):1599–608.
- Armitage R, Nellums LB. COVID-19 and the consequences of isolating the elderly. The Lancet Public Health. 2020;5(5):e256.
- Peat G, McCarney R, Croft P. Knee pain and osteoarthritis in older adults: a review of community burden and current use of primary health care. Annals of the rheumatic diseases. 2001;60(2):91–7.
- Jakobsson ULF, Hallberg IR. Pain and quality of life among older people with rheumatoid arthritis and/or osteoarthritis: a literature review. Journal of clinical nursing. 2002;11(4):430–43.
- Neogi T. The epidemiology and impact of pain in osteoarthritis. Osteoarthritis and cartilage. 2013;21(9):1145–53.
- McCaffrey R, Freeman E. Effect of music on chronic osteoarthritis pain in older people. Journal of advanced nursing. 2003;44(5):517–24.
- Hong J-Y, Han K, Shin D-H, Chun EM. Quality of life analysis and smoking correlation in symptomatic spine osteoarthritis: a nationwide health survey analysis of an elderly population with EQ-5D. PLoS One. 2016;11(3):e0151315.
- Meng H, Xu Y, Dai J, Zhang Y, Liu B, Yang H. Analyze the psychological impact of COVID-19 among the elderly population in China and make corresponding suggestions. Psychiatry research. 2020;289:112983.
- Girdhar R, Srivastava V, Sethi S. Managing mental health issues among elderly during COVID-19 pandemic. Journal of geriatric care and research. 2020;7(1):32–5.
- Banerjee D. The impact of Covid‐19 pandemic on elderly mental health. International journal of geriatric psychiatry. 2020;35(12):1466.
- Petretto DR, Pili R. Ageing and COVID-19: what is the role for elderly people? Vol. 5, Geriatrics. MDPI; 2020. p. 25.
- Liu K, Chen Y, Lin R, Han K. Clinical features of COVID-19 in elderly patients: A comparison with young and middle-aged patients. Journal of Infection. 2020;80(6):e14–8.
- Papadopoulos V, Li L, Samplaski M. Why does COVID‐19 kill more elderly men than women? Is there a role for testosterone? Andrology. 2021;9(1):65–72.
![]() This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Cardiopulmonary Resuscitation (CPR) during COVID-19 Pandemic
Aprianto Daniel Pailaha1*
1 Professional Nurse Study Program, Department of Nursing, Faculty of Health Sciences, Brawijaya University, Malang, Indonesia
*Corresponding Author: Ns. Aprianto Daniel Pailaha, S.Kep., Professional Nurse Study Program, Department of Nursing, Faculty of Health Sciences, Brawijaya University, Malang, Indonesia. Email: apriantodanielpp@gmail.com
ORCHID ID: https://orcid.org/0000-0002-9456-6616
ABSTRACT
Introduction: The COVID-19 infection has a high rate of mortality and morbidity and is extremely contagious. COVID-19 has raised attention to safety issues involving healthcare workers who perform CPR. The risk of transmission produces a dilemma to perform cardiopulmonary resuscitation (CPR) within the COVID-19 pandemic. Additionally, patient and/or family preferences, as a factor associated with Do-Not-Resuscitate (DNR). This commentary wants to provide an overview or other perspectives that may be the subject of further research so that there will be evidence base practice for health workers, especially nurses in code blue situations.
Discussion: COVID-19 pandemic has clearly had a significant impact on the epidemiology and outcome of cardiac arrest in both out-of-hospital and in-hospital settings. All potential COVID-19 patients should be offered the advantage of CPR by attempting to revive them after taking all required safety precautions, and the patient should only be confirmed dead after CPR has been performed. Provision of further information regarding CPR to patients and/or families for consideration, including the advantages and disadvantages of CPR, before making a final decision regarding the administration of CPR. COVID-19 patients with a poor prognosis might benefit from Do-Not-Resuscitate (DNR) but this is causes dilemmas in nursing profession.
Conclusion: Although the survival rate for COVID-19 patients is poor, it is anticipated that CPR attempts will still be performed during the COVID-19 pandemic by following several guidelines. COVID-19 patients with a poor prognosis might benefit from Do-Not-Resuscitate (DNR) if the patient and/or family who are accountable provide their approval and everything is in order. As a nurse, we must respect the decisions that patients or families make because it is their right and their authority.
Keywords: CPR; Cardiac Arrest; DNR; COVID-19; Nursing
INTRODUCTION
The COVID-19 pandemic is extremely challenging health care systems worldwide and increasing principal ethical issues, especially concerning a prospect need for health care in the context of scarce resources and crisis capacity. Cardiac arrest is defined as the sudden cessation of cardiac mechanical activity, confirmed by the absence of signs of circulation. Lack of blood flow to the brain and other vital organs can cause loss of consciousness, powerlessness, or death if not treated properly [1]. Cardiac arrest is associated with pneumonia in COVID-19 patients, myocardial injury has a poor percentage of outcomes, whereas other Cardiovascular Disease (CVD) cases without myocardial injury are relatively vulnerable [1,2]. The COVID-19 patients may experience respiratory dysfunction and a subsequent change in tissue oxygenation that directly affects the cardiovascular system and results in serious issues including myocarditis, myocardial injuries, acute myocardial infarction, heart failure, cardiac dysrhythmia, and thromboembolism [3]. COVID-19 infection has a high mortality and morbidity rate and is highly contagious. COVID-19 has raised attention to safety issues involving healthcare workers attempting CPR. Among the several aerosol-producing procedures performed on patients, CPR is strongly associated with a variety of aerosol-generating procedures, including chest compression, positive pressure ventilation, and the respiratory tract maneuver. This will trigger extremely concerned about being infected with COVID-19 because considering that the COVID-19 virus is very dangerous for vulnerable populations.
Several inpatients experiencing cardiac arrest are administered cardiopulmonary resuscitation (CPR), provided advance instructions are available or the patient has a documented Do-Not-Resuscitate (DNR) status [4]. Despite the fact that attitudes regarding CPR have changed due to the COVID-19 pandemic, the majority of respondents reported that they would be prepared to do CPR if they encountered a cardiac arrest incident. Notably, independent of usual circumstances, people are more inclined to perform CPR without mouth-to-mouth resuscitation. There were other factors that affected CPR during the COVID-19 pandemic, however the two of that had been determined to be of considerable increasing significance were the fear of contracting COVID-19 and the fear of spreading COVID-19 to others, which were assessed at 78% and 29%, respectively [5,6]. This is a separate consideration for health workers, especially nurses in implementing CPR in cases of cardiac arrest during the COVID-19 pandemic.
When a new pandemic begins, the infection in healthcare facilities spreads easily. In April 2020, as many as 22,073 cases of COVID-19 among healthcare professionals were reported to the WHO. On February 2020, there were 1716 healthcare professionals in China who had contracted SARS-CoV-2. As many as 3300 people were infected as of early March, and at least 22 of them died in China. As of March 2020, about 2600 people were infected in Italy, and 13 of them had died [7]. When performing CPR during the COVID-19 pandemic, there are several factors that need to be considered carefully to ensure the safety of the rescuers, the patients, and the surroundings. The purpose of writing comments on this article is to provide an opinion regarding the administration of CPR in cardiac arrest in patients with COVID-19 or during this COVID-19 pandemic.
The resuscitation guidelines, in force considering 2015, have consequently been adapted to this new situation, e.g., for Basic Life Support (BLS), mouth-to-mouth ventilation in addition to chest compression are encouraged to bystanders. For Advanced Life Support (ALS), bag-masks or Supraglottic Airway (SGA) ventilation are considered appropriate options to tracheal intubation [8]. Recently, updates have been issued, considerably with the aid of using the International Liaison Committee on Resuscitation (ILCOR), European Resuscitation Council (ERC), and the American Heart Association (AHA). Briefly, the principle modifications advise that lay rescuers have to consider chest compressions only, except for children, and all life support providers must use PPE all through resuscitation and favor early tracheal intubation to minimize aerosols.
The risk of transmission of the SARS-CoV-2 virus to initial responders performing cardiopulmonary resuscitation (CPR) produce a dilemmas to manage CPR within the COVID-19 pandemic. A better knowledge of this could enable identification of which individuals are less likely to benefit from CPR, and inform discussion of a Do Not Resuscitate (DNR). This aims to provide an overview or other perspectives that may be the subject of further research so that there will be evidence base practice for health workers, especially nurses in code blue situations.
DISCUSSION
1. CPR and COVID-19 Additional Considerations
The new regulations for performing high-quality CPR during the COVID-19 pandemic have been introduced to lower the risk of COVID-19 transmission. In order, the American Heart Association (AHA), European Resuscitation Council (ERC), International Liaison Committee on Resuscitation (ILCOR), and other resuscitation associations have been released a modification guidelines or recommendations for the COVID-19 pandemic concerns into account [9-11]. Several modification and recommendation implemented since the COVID-19 pandemic:
1) International Liaison Committee on Resuscitation (ILCOR)
Treatment recommendations from ILCOR for performing CPR to address cardiac arrest problems in patients with COVID-19 [12].
a) Cardiopulmonary resuscitation and chest compressions may produce aerosol.
b) Rescuers consider public-access defibrillation and compression-only.
c) Rescuers who are committed, competent, and trained may choose to give children rescue breaths in addition to chest compressions (good practice statement).
d) Should wear personal protection equipment during resuscitation
e) Rescuers consider defibrillation before donning aerosol-generating personal protection equipment.
2) European Resuscitation Council (ERC)
The following new recommendation of Basic Life Support (BLS) are advised by the European Resuscitation Council for patients with confirmed or suspected COVID-19 [12,13].
a) Should have prior training in appropriate use of PPE
b) Consider to compression-only CPR if bag-mask ventilation is difficult or not available
c) Use a high-efficiency particulate air (HEPA) filter during bag-mask ventilation
d) Use two hands to hold the mask and the person doing compressions can squeeze the bag when they pause after 30 compressions
e) Use PPE (surgical mask, eye protection, apron, and gloves) before defibrillation because not an aerosol-generating procedure
3) American Heart Association (AHA)
The American Heart Association (AHA) introduced new recommendation for Basic Life Support (BLS) in COVID-19 patients both in‑and out‑of‑hospital cardiac arrest [13].
a) Significantly reduce the risk of infection with vaccination and boosters.
b) CPR is considered to be an aerosol-generating procedure (AGP) such as hest compressions, defibrillation, bag-valve-mask (BVM) ventilation, intubation, and positive pressure ventilation.
c) Should wear PPE such as N95 mask, gloves, gown, eye protection, positive pressure ventilation.
d) PPE must be donned before performing components of resuscitation.
If patients have any signs and symptoms, bystanders should give defibrillation only and without chest compression unless they have PPE. As a result, the estimated death rates for CPR are extremely low, and the use of barriers such as PPE was strongly recommended to reduce the risk of COVID-19 transmission. Cardiopulmonary Resuscitation (CPR) attempts such as chest compression only and defibrillation only as procedures with an increased risk of COVID-19 transmission. Tracheal intubation and mouth-to-mouth or mouth-to-mask ventilation were associated with a high risk of COVID-19 transmission. Although previous research has shown that compression-only CPR is as effective as combined compressions and ventilations, this could not be the case for COVID-19 patients because they suffer from primary respiratory failure.
The European Resuscitation Council (ERC) COVID-19 guidelines encourage continuing resuscitation efforts for cardiac arrests that occur both inside and outside of hospitals while also attempting to reduce risk to the person providing treatment. The COVID-19 guidelines focus specifically on patients with COVID-19. Those providing treatment should conduct a dynamic risk assessment, which may include current COVID-19 prevalence, the patient's presentation, the probability that treatment will be effective and efficient, the accessibility of personal protective equipment (PPE), and personal risks for those providing treatment [14]. The proportion of patients with shockable rhythms decreased, as did the use of automated external defibrillators. The use of supraglottic airways increased, while the rate of intubation decreased. Overall, there was a increase rates return of spontaneous circulation, survival to admission, and survival to discharge.
2. CPR Outcomes during COVID-19 Pandemic
According to recent research, in-hospital cardiac arrest (IHCA) among COVID-19 patients was 9.39%, with 9% ROSC and 2% survival to hospital discharge. Accordingly, the average rate of out-of-hospital cardiac arrest (OHCA) survival to discharge is 8.8% [15]. But among COVID-19 patients, two more investigations on both in- and out-of-hospital CA showed a 0% survival rate to hospital discharge rate [16,17]. The primary CPR success rate among COVID-19 patients was low, especially for those with asystole or bradycardia [3,18]. This harmful infection has influenced the CPR efficacy because there are additional considerations for the CPR attempt. Therefore, the COVID-19 pandemic has largely influenced CPR procedures. Apart from the various factors involved in performing CPR, another thing that must be considered is the ability and capability to perform CPR through training [19]. Participation in training such as Basic Trauma Cardiac Life Support (BTCLS) or Advanced Cardiac Life Support (ACLS) will help nurses gain more knowledge, experience, and skills when it comes to performing CPR on cardiac arrest patients.
Continuous cardiopulmonary resuscitation (CPR) training and quality control systems, such as monitoring morbidity and mortality, are also recommended [20]. Every nurse, especially those working in emergency room, needs to have the necessary training to administer first aid in accordance with protocol. As a result, nurses may feel more confident and competent to provide CPR in situations of cardiac arrest.
Data from in-hospital cardiac arrests caused by COVID-19 are less commonly reported. According to a multicenter cohort study from 68 Intensive Care Units in the United States found that 14.0% (701/5019) of patients had an in-hospital cardiac arrest, 57.1% (400/701) received CPR, and 7.0% (28/400) survived to hospital discharge with normal or mildly impaired neurological status [21]. According to data from 136 patients in China, about 113 (83.1%) of them required CPR, and ROSC occurred in 18 (13.2%) of the patients, 4 (2.9%) survived for at least 30 days, and one patient had a favorable neurological outcome at 30 days [22]. COVID-19 pandemic has clearly had a significant impact on the epidemiology and outcome of cardiac arrest in both out-of-hospital and in-hospital settings.
3. Nursing Decision-Making
Nursing is patient-centered care. A nursing profession requires to follow an ethical code, which allowed to provide great nursing care. Therefore, the nursing profession intends to maintain and improve health care in society. The key point is that a lower survival rate in CPR was reported at the start of the COVID-19 pandemic compared to previous years. All intervention decisions must involve informed and involved patients and/or families, according to national and institutional policy [23]. However, patient and/or family preferences, as a factor associated with Do-Not-Resuscitate (DNR). Provision of further information regarding CPR to patients and/or families for consideration, including the advantages and disadvantages of CPR, before making a final decision regarding the administration of CPR.
It is critical for determine personal goals and preferences regarding a resuscitation attempt. The mortality rate for COVID-19 patients who seemed to be critically ill was significant and increased with age, comorbidities, and symptom severity. The AHA recommends taking these considerations into account when weighing the risk versus the benefit of initiating resuscitation. Furthermore, many different institutions have strongly advised patients with poor prognoses to consider DNR. When considering DNR, COVID-19 positivity by itself cannot be a factor except when it is accompanied by irreversible multi-organ dysfunction [16,24]. All potential COVID-19 patients should be offered the advantage of CPR by attempting to revive them after taking all required safety precautions, and the patient should only be confirmed dead after CPR has been performed. The statement emphasized the need for all professionals to consider every cardiac arrest victim who presents to the emergency room as a possible COVID-19 suspect during the pandemic and to wear the proper PPE. The CPR method should be performed with the fewest number of essential medical professionals present, ideally in a single-person room with the door closed.
It is noteworthy that CPR, in some cases, has been initiated by nurses, but the decision-making process for non-resuscitation is made by the physician and based on the discussion between the all-team members, considers not being useful the CPR maneuvers for some cases. It depends on the nurse, among other actions, the functionality of the stop cart, with availability of materials necessary for this type of assistance, technical procedures for venipuncture, preparation and administration of medications, supervision of the technical professionals of the nursing team and possible relay in resuscitation maneuvers.
4. Ethical Approaches and DNR
The reality requires reflection with a professional ethical focus on the duty of updating professionals, as provided for in the Code of Ethics for Nursing Professionals, and which determines that the patient has the right to get preserve of correct information, to be heard in their needs, and to get preserve of resolute humanized care. These conclusions are based on bioethical reflection and acknowledgement that not all nurses working in palliative care for COVID-19 patients with DNR are able to provide communication that supports this choice, either by acting in accordance with protocol or by providing nursing care without considering or updating the practice of euthanasia. In this situation, struggling to take into consideration the knowledge of those involved or neglecting to listen to the patient and family interferes with their ability to communicate effectively and their autonomy, leading to conflicts and challenges in the management of nursing care.
According to qualitative research, in Maryland there are 31 nurses who worked for COVID-19 patients in the acute care units, in depth-interview the nurse mentioned that “They really push that DNR and that’s like a part of my distress, because I know I’m very patient-family centered in my thinking…because it’s futile they tell the family this person should be DNR. They’re over 70, we’re not going to escalate care…The family has to believe whatever we tell them…so hopefully they’re right, because they don’t have a choice, the family or the patient.[25]” Knowing the DNR order causes the nurse to experience moral distress. Rather than enhancing services, prepare for end-of-life care is something that is very difficult. Of course, as a nurse, you want to do the best for patients and their families, but not in the event of a DNR, because It is the patient and family's authority. Besides, disagreement about the proper use of end-of-life care is one of the triggers of moral distress when providers encourage families to do DNR.
According to qualitative research, in Philippines there are 12 nurses who worked in COVID-19 ward of several hospitals, the nurse mentioned that “Occasionally, family members decide against intubation because they do not wish to witness their family member suffer further and add to the agony of the patient [26].” Severe symptoms of COVID-19 prompt families to put their loved ones out of the misery and sign DNR forms. In this case, nurses support symptom-free death and suffering reduction through assisting patients and families.
According to qualitative research, in United States there are 7 ICU nurses, in interview session the nurse mentioned that "Patient was a DNR or DNI maxed out on BiPAP (bilevel positive airway pressure support) and developed respiratory arrest. I, the nurse, and the intensivist thoroughly explained the situation to the family and encouraged transition to comfort care, yet the family refused. The patient suffered for another day and a half before she died. I was furious at the family and heartbroken for the patient, she deserved a more dignified death than she received [27].” The nurse was not explicit use term “moral distress” but describe about condition when they experienced moral-constraint distress because they perceived the life-sustaining treatments provided were contrary to the patient’s wishes and contributing to the patient’s suffering because they were constrained by a DNR order. Surrogate decision-making are not reflect the fully patient’s wishes.
Evidence has emerged illustrating ethical dilemmas in conducting DNR discussions during the COVID-19 pandemic [28]. Based on some of the qualitative research findings in several countries, it shows that DNR status causes moral distress due to opposition, and disagreement about DNR. Moreover, nurses have to support symptom-free death and suffering reduction for patients and their families. Additionally, nurses believe that the DNR is not in line with the patient's intentions and that the surrogate decision-making certainly does not properly represent the patient's preferences. Some of the responses given by nurses depend on the assessment of the ethics held. This can be considered valid or correct if it is based on strong evidence.
CONCLUSIONS
Even when cardiopulmonary resuscitation is administered, cardiac arrest is common in critically ill COVID-19 patients and is associated with poor survival. COVID-19 patients with a poor prognosis might benefit from Do-Not-Resuscitate (DNR) if the patient and/or family who are accountable provide their approval and everything is in order. In fact, CPR efforts are still possible if there is a chance of surviving the patient. Although the survival rate for COVID-19 patients is poor, it is anticipated that CPR attempts will still be performed during the COVID-19 pandemic by following several guidelines in order to help people COVID-19 patients to survive using the American Heart Association (AHA), European Resuscitation Council (ERC), International Liaison Committee on Resuscitation (ILCOR), and other resuscitation associations modification guidelines or recommendations for the COVID-19 pandemic. However, patient and/or family preferences, as a factor associated with Do-Not-Resuscitate (DNR) in several cardiac arrest conditions. Nursing profession have to reflection and uphold ethical as provided for in the Code of Ethics for Nursing Professionals. DNR status causes moral distress due to opposition, and disagreement. Surrogate decision-making certainly does not properly represent the patient's preferences. As nurse, we have to support symptom-free death and suffering reduction for patients and their families, and respect the decisions that patients or families make because it is their right and their authority.
CONFLICT OF INTERESTS DISCLOSURE
The author declares that there is no conflict of interests
ETHICAL APPROVAL
Not applicable
FUNDING
Not applicable
REFERENCES
- Shao F, Xu S, Ma X, et al. In-hospital cardiac arrest outcomes among patients with COVID-19 pneumonia in Wuhan, China. Resuscitation 2020;151:18–23; doi: 10.1016/j.resuscitation.2020.04.005.
- Guo T, Fan Y, Chen M, et al. Cardiovascular Implications of Fatal Outcomes of Patients With Coronavirus Disease 2019 (COVID-19). JAMA Cardiol 2020;5(7):811; doi: 10.1001/jamacardio.2020.1017.
- Goodarzi A, Khodaveisi M, Abdi A, et al. Cardiopulmonary Resuscitation Outcomes of Patients with COVID-19; a One-Year Survey. Arch Acad Emerg Med 2021;9(1); doi: 10.22037/AAEM.V9I1.1381.
- Garg H, Jha S. Cardiopulmonary Resuscitation during COVID-19 Pandemic: Outcomes, Risks, and Protective Strategies for the Healthcare Workers and Ethical Considerations. Indian Journal of Critical Care Medicine 2020;24(9):868–872; doi: 10.5005/jp-journals-10071-23544.
- AL-shiakh S, Tran QK, Caggiula A, et al. Attitudes among healthcare professionals towards cardiopulmonary resuscitation during COVID-19. Am J Emerg Med 2022;52:34–42; doi: 10.1016/j.ajem.2021.11.017.
- Chong K-M, Chen J-W, Lien W-C, et al. Attitude and behavior toward bystander cardiopulmonary resuscitation during COVID-19 outbreak. PLoS One 2021;16(6):e0252841; doi: 10.1371/journal.pone.0252841.
- Jin YH, Huang Q, Wang YY, et al. Perceived infection transmission routes, infection control practices, psychosocial changes, and management of COVID-19 infected healthcare workers in a tertiary acute care hospital in Wuhan: A cross-sectional survey. Mil Med Res 2020;7(1); doi: 10.1186/s40779-020-00254-8.
- Baert V, Jaeger D, Hubert H, et al. Assessment of changes in cardiopulmonary resuscitation practices and outcomes on 1005 victims of out-of-hospital cardiac arrest during the COVID-19 outbreak: registry-based study. Scand J Trauma Resusc Emerg Med 2020;28(1); doi: 10.1186/s13049-020-00813-x.
- Kundra P, Vinayagam S. COVID-19 cardiopulmonary resuscitation: Guidelines and modifications. J Anaesthesiol Clin Pharmacol 2020;36(5):39; doi: 10.4103/joacp.JOACP_257_20.
- Chojecka D, Pytlos J, Zawadka M, et al. How to Maintain Safety and Maximize the Efficacy of Cardiopulmonary Resuscitation in COVID-19 Patients: Insights from the Recent Guidelines. J Clin Med 2021;10(23):5667; doi: 10.3390/jcm10235667.
- Fazel MF, Mohamad MHN, Sahar MA, et al. Readiness of Bystander Cardiopulmonary Resuscitation (BCPR) during the COVID-19 Pandemic: A Review. Int J Environ Res Public Health 2022;19(17):10968; doi: 10.3390/ijerph191710968.
- Nolan JP, Monsieurs KG, L.Bossaert, et al. European Resuscitation Council COVID-19 guidelines executive summary. Resuscitation 2020;153:45–55; doi: 10.1016/j.resuscitation.2020.06.001.
- Kundra P, Vinayagam S. COVID-19 Cardiopulmonary Resuscitation: Guidelines and Modifications. J Anaesthesiol Clin Pharmacol 2020;36(5):S39–S44; doi: 10.4103/joacp.JOACP_257_20.
- Perkins GD, Graesner JT, Semeraro F, et al. European Resuscitation Council Guidelines 2021: Executive summary. Resuscitation 2021;161:1–60; doi: 10.1016/j.resuscitation.2021.02.003.
- Nguyen D, Sarani N, Marshall K, et al. CODE BLUE-19: A Proposed Protocol to Mitigate COVID-19 Transmission in the Emergency Department when Receiving Out-of-hospital Cardiac Arrest Patients. Western Journal of Emergency Medicine 2020;21(6); doi: 10.5811/westjem.2020.7.48436.
- Sultanian P, Lundgren P, Strömsöe A, et al. Cardiac arrest in COVID-19: characteristics and outcomes of in- and out-of-hospital cardiac arrest. A report from the Swedish Registry for Cardiopulmonary Resuscitation. Eur Heart J 2021;42(11):1094–1106; doi: 10.1093/eurheartj/ehaa1067.
- Thapa SB, Kakar TS, Mayer C, et al. Clinical Outcomes of In-Hospital Cardiac Arrest in COVID-19. JAMA Intern Med 2021;181(2):279; doi: 10.1001/jamainternmed.2020.4796.
- Hayek SS, Brenner SK, Azam TU, et al. In-hospital cardiac arrest in critically ill patients with covid-19: multicenter cohort study. BMJ 2020;m3513; doi: 10.1136/bmj.m3513.
- Sukarwan A, Peristiowati Y, Ellina AD. The Role of Emergency Nurses in Cardiopulmonary Resuscitation (CPR) of Cardiac Arrest Patients: A Literature Review. ENDLESS : International Journal of Future Studies 2021;4(1):148–158; doi: 10.54783/endless.v4i1.53.
- Taha HS, Shaker MM, Abdelghany MM. Cardiopulmonary resuscitation during the COVID-19 pandemic: a scientific statement on CPR management protocol of Kasr Al-Ainy University Hospital is presented. The Egyptian Heart Journal 2020;72(1):73; doi: 10.1186/s43044-020-00106-9.
- Hayek SS, Brenner SK, Azam TU, et al. In-hospital cardiac arrest in critically ill patients with covid-19: multicenter cohort study. BMJ 2020;371:m3513; doi: 10.1136/bmj.m3513.
- Phattharapornjaroen P, Nimnuan W, Sanguanwit P, et al. Characteristics and outcomes of out-of-hospital cardiac arrest patients before and during the COVID-19 pandemic in Thailand. Int J Emerg Med 2022;15(1); doi: 10.1186/s12245-022-00444-2.
- Connellan D, Diffley K, McCabe J, et al. Documentation of Do-Not-Attempt-Cardiopulmonary-Resuscitation orders amid the COVID-19 pandemic. Age Ageing 2021;50(4):1048–1051; doi: 10.1093/ageing/afab075.
- Nguyen D, Sarani N, Marshall K, et al. CODE BLUE-19: A Proposed Protocol to Mitigate COVID-19 Transmission in the Emergency Department when Receiving Out-of-hospital Cardiac Arrest Patients. Western Journal of Emergency Medicine 2020;21(6); doi: 10.5811/westjem.2020.7.48436.
- Silverman HJ, Kheirbek RE, Moscou-Jackson G, et al. Moral distress in nurses caring for patients with COVID-19. Nurs Ethics 2021;28(7–8):1137–1164; doi: 10.1177/09697330211003217.
- Jimenez OJB, Trajera SM, Ching GS. Providing End-of-Life Care to COVID-19 Patients: The Lived Experiences of ICU Nurses in the Philippines. Int J Environ Res Public Health 2022;19(19); doi: 10.3390/ijerph191912953.
- Morley G, Copley DJ, Field R, et al. RESPONDER: A qualitative study of ethical issues faced by critical care nurses during the COVID-19 pandemic. J Nurs Manag 2022; doi: 10.1111/jonm.13792.
- Hanna K, Cannon J, Gabbay M, et al. End of life care in UK care homes during the COVID-19 pandemic: a qualitative study. BMC Palliat Care 2022;21(1); doi: 10.1186/s12904-022-00979-4.
![]() This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
THE EFFECTIVENESS OF AUDIO HYPNOTHERAPY IN REDUCING POSTPARTUM DEPRESSION DURING NEW NORMAL
Rosyati Pastuty1*, Elita Vasra1, Gustiana2
1Department of Midwifery, Health Polytechnic of Palembang, Indonesia
2Department of Midwifery, Health Polytechnic of Aceh, Indonesia
* Corresponding author:
Rosyati Pastuty, Jl. Inspektur Yazid, Sekip Jaya, Kec. Kemuning, Kota Palembang, Sumatera Selatan 30114, Indonesia, Orcid: https://orcid.org/0000-0003-0804-2291
Email: rrosyatipastuty@gmail.com
ABSTRACT
Background: Postpartum depression is a life-threatening mental health disorder and occurs in 10-15% of women. “Globally, the incidence of postpartum depression reaches 10-15%. There are few reports in countries such as Malta, Malaysia, Austria, Denmark and Singapore. While in other countries such as Brazil, South Africa, Taiwan, Korea, Italy, and Costa Rica, symptoms of postpartum depression are reported to be quite high”. “Based the criteria of the Diagnostic and Statistical Manual of Mental Disorders, fourth edition (DSM-IV) and the Edinburgh Postnatal Depression Scale (EPDS). Audio hypnotherapy, which is the provision of positive suggestions delivered through MP3, is a method to reduce the level of postpartum depression. This study aims to determine the effectiveness of audio hypnotherapy in reducing postpartum depression during the new normal.
Materials and Methods: This quasi-experimental study used a pretest-posttest design involving 60 postpartum mothers with a history of normal delivery at 2 Midwife's clinics in Palembang City and 1 Midwife's clinic in Aceh. Postpartum depression levels were assessed using the Edinburgh Postnatal Depression Scale (EPDS). Data analysis used Paired Samples Test to determine differences in postpartum depression levels before and after listening to Hypnotherapy audio.
Results: There was a decrease in postpartum mothers' depression level after listening to hypnotherapy audio for ± 2 weeks. Depression incidence before giving audio hypnotherapy has a mean value = 11.15, while after giving audio hypnotherapy, it increases to 8.90, with P-value <0.05.
Conclusion: Audio hypnotherapy therapy has proven to be effective in reducing the incidence of depression in postpartum mothers.
Keywords: Audio Hypnotherapy, depression, Post-partum mother
INTRODUCTION
Antepartum Depression (APD) and Postpartum Depression (PPD), are disorders characterized by mood swings during pregnancy and after childbirth, which have a negative impact on the physical and mental health of mothers and children [1,2]. Melville et al [3] in their study reported that prevalence rates ranged from 4.8% to 18.4% for mild depression, and from 5.1% to 12.7% for severe depression.
Globally, the incidence of postpartum depression reaches 10-15%. There are few reports in countries such as Malta, Malaysia, Austria, Denmark and Singapore. While in other countries such as Brazil, South Africa, Taiwan, Korea, Italy, and Costa Rica, symptoms of postpartum depression are reported to be quite high. A study in India, involving 359 primiparous mothers, reported an 11% incidence of postpartum depression [4,5].
Approximately 70% of new mothers have mild depressive symptoms which generally peak in the 2 to 5 days after delivery. These symptoms usually begin to subside spontaneously within 2 weeks, but if not detected immediately and treatment is delayed, it can develop into postpartum depression [6].
Most pregnant women who face the birth process experience feelings of anxiety, even depression. Factors causing postpartum depression consist of biological factors, characteristics and background of the mother. Levels of the hormones estrogen (estradiol and estriol), progesterone, prolactin, cortisol which increase and decrease too quickly or too slowly are biological factors that cause postpartum depression [7]. The greater the decrease in estrogen and progesterone levels after childbirth, the greater the tendency for a woman to experience depression in the first 10 days after giving birth [8]. The estrogen and progesterone exert a suppressive effect on the activity of the monoamine oxidase enzyme. This enzyme can inactivate both noradrenaline and serotonin, which play a role in mood and depression. Estradiol and estriol are the active forms of estrogen formed by the placenta. Estradiol functions to strengthen the function of neurotransmitters by increasing the synthesis and reducing the breakdown of serotonin. Therefore, theoretically the decrease in estradiol levels due to childbirth plays a role in causing postpartum depression [2,6,9,10]. Biological causative factors are difficult and rarely measured in terms of maternal depressive symptoms [11]. Other factors that influence maternal depressive symptoms described in several studies include interpersonal variables (neural disorders, poor life experiences), social variables (marital dissatisfaction, lack of social support), and clinical variables related to pregnancy (risk in current pregnancy, problems with previous pregnancy) [12].
Antepartum Depression (APD) and Postpartum Depression (PPD) together are called perinatal depression. Various diagnostic criteria with major depression occur during pregnancy or within 4 weeks after delivery [13]. Based on previous research, women with a history of high levels of stress may be at increased risk for perinatal depression [14,15].
Based on the criteria of the Diagnostic and Statistical Manual of Mental Disorders, fourth edition (DSM-IV) [16] and the Edinburgh Postnatal Depression Scale (EPDS) [17], mothers with symptoms of postpartum depression are defined by several major symptoms, including a depressed mood or decreased pleasure. These symptoms include impaired appetite, physical agitation or psychomotor slowing, weakness, decreased concentration, and suicidal ideation. Mothers also often feel insomnia even though the baby has fallen asleep. These symptoms must be present throughout the day and last for at least two weeks [3,9].
Women who experienced depression during pregnancy had seven times the risk of developing postpartum depression than women who did not have symptoms of antenatal depression. An observational study of 78 depressed women in the first trimester of pregnancy found that postpartum depression did not occur in all women who received treatment, both psychotherapy and pharmacotherapy, compared with 92% of women who were depressed and did not receive treatment. Supportive and psychological interventions are more effective when performed after delivery than when they are initiated during pregnancy [18].
Mothers with postpartum depression need extensive treatment with both pharmacological and non-pharmacological therapies. Through non-pharmacological therapy, such as psychological therapy, mothers can find the right way to deal with the symptoms of depression, deal with disorders that arise, or think positively when the situation is stressful [19,20].
There are several non-pharmacological techniques to relieve anxiety such as pregnancy exercise, distraction, biofed back, yoga, acupressure, aroma therapy, steam therapy and hypnosis. Hypnosis is a natural method used to relieve fear, panic, tension, and other pressures. Hypnosis is done by making direct contact with the subconscious, by giving suggestions in order to build various positive emotional conditions [21,22].
Khoirunnisa et al., [21] used a narrative review method to explore types of interventions for postpartum depression and found that several interventions such as music therapy [22], postpartum exercise [23], aerobic exercise [24], laughter therapy [25], cognitive behavior Therapy [26], Effleurage Massage Therapy [27], Acupressure Therapy [28], are effective in reducing postpartum depression.
Based on some of these studies provides an illustration that not many hypnotherapy interventions have been thoroughly scrutinized considering the impact of depression on postpartum mothers; we are therefore interested in analyzing the effectiveness of Audio Hypnotherapy in reducing postpartum depression, especially in the new normal period in 2021.
MATERIALS AND METHODS
Study design
This type of research is a quasi-experimental design using a pretest - posttest design.
Study Population
This research was conducted in January–December 2021 at the Teti Herawati Midwife clinic, Meli Rosita Palembang City and the Mariana Aceh Besar Indonesia, midwife clinic involving 60 participants who were randomly selected and had met the sample inclusion requirements such as being healthy after giving birth, having never received hypnotherapy audio, mentally healthy, and has a cell phone. Demographic characteristics of postpartum women collected in this study were age, education, occupation and parity.
Sample size
The number of samples involved was 60 participants who were randomly selected from the population. Calculating the number of samples is determined using the Slovin formula [29], where from 71 people in the population, d = 0.05, the number of samples is 60.
Instruments
The incidence of postpartum depression will be measured using a standardized questionnaire developed by Cox et al., the Edinburgh Postnatal Depression Scale (EPDS). This questionnaire consists of 10 questions; each has four responses with a Likert scale from 0 – 3. The maximum value is 30, and the lowest is 0. It is called experiencing depression if the score is ≥ 10. EPDS has a sensitivity of 80% and a specificity of 84.4 % [23]. Meanwhile, EPDS in Indonesian has a sensitivity of 86% and a specificity of 78% [24].
The scale shows how the mother felt during the previous week. In doubtful cases it may be useful to repeat the tool after 2 weeks. This scale is not used to detect mothers with anxiety neuroses, phobias or personality disorders [25].
Interventions
Audio hypnotherapy is giving positive suggestions or orders to the subconscious mind to change thoughts, feelings, and behaviors for the better through MP3 voice recordings sent via WhatsApp groups. In this study, hypnotherapy was carried out by selfhypnosis using standardized hypnotherapy audio recording media. The selfhypnosis method with standard hypnotherapy audio recording media for 30 minutes in stages; pre-induction (introduction, explaining goals, and building trust), filling in the informed consent sheet, explaining the use of tools, induction (the relaxation process brings the patient to the subconscious mind with Hanung techniques), deepening (trance), suggestion (giving messages with the aim of certain), and termination (slowly awakening the patient).
Before the intervention, all respondents filled out the EPDS questionnaire to determine the risk of postpartum depression. Then, respondents listened to Hypnotherapy audio for ± 30 minutes every night before going to bed for 2 weeks. After undergoing an audio Hypnotherapy intervention for 2 weeks, all respondents filled out the EPDS questionnaire to determine the risk of postpartum depression.
Ethical Consideration
Before the respondents filled out the questionnaire, the researchers first explained their informed consent about the scope of the research. Then after the prospective respondent agreed, the respondent signed an agreement to become a respondent. All data about respondents will be kept confidential and only used for research purposes.No economic incentives were offered or provided for participation in this study. The study protocol matched the Declaration of Helsinki ethical guidelines for clinical studies. This research has been approved by the Health Research Ethics Commission of the Health Polytechnic of the Palembang Ministry of Health with the number 1250/KEPK/Adm2/VIII/2021.
Statistical analysis
The statistical analysis was performed by SPSS software version 16. 0. Data are presented as number and percentage for categorical variables, and continuous data expressed as the mean ± standard deviation (SD) unless otherwise specified. The first statistical test, the McNemar test, aims to analyze differences in depression status before and after the intervention using categorical data. Before conducting the different tests, first, we tested the normality of the data using the Kolmogorov Smirnov and found the data was not normally distributed. The research data were analyzed using the Wilcoxon test. This test was performed on same data sample in two different periods where the data were not normally distributed. It is considered significant if the research variable has a P-value <0.05.
RESULTS
The characteristics of respondents in this study include age, education, employment status and parity. The following is the frequency distribution of the respondents' characteristics in this study:
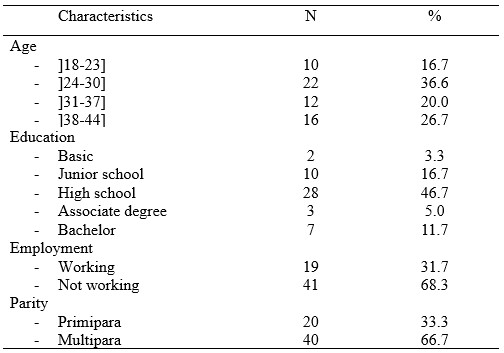
Table 1. Frequency Distribution of Respondents Characteristics
Table 1 shows that most of the mothers aged 24-30 years were 22 mothers (36.6%). The respondents' education is mostly High school as many as 28 respondents (46.7%). Most respondents did not work as many as 41 (68.3%), and multipara as many as 40 respondents (66.7%).
The results of statistical tests and the distribution of depression status before and after the intervention are presented in table 2.

Table 2. Distribution of depression incidence before and after interventions
Table 2 shows that before the intervention there were 26 depressed respondents then after the intervention there were 12 respondents. Based on the McNemar test, a p-value <0.05 was obtained, meaning that there were differences in depression status before and after the intervention.
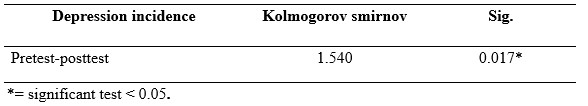
Table 3. Normality Test Results of depression incidence pretest and posttest audio hypnotherapy
Table 3 shows that the results of the Kolmogorov Smirnov statistical test obtained a P-value <0.05, so the normality is rejected. The depression incidence data at the pre-post test audio hypnotherapy not normally distributed. Therefore, the statistical difference test was tested using Wilcoxon.
The results of the audio hypnotherapy pre-post test statistics and the mean depression incidence values are presented in table 4.
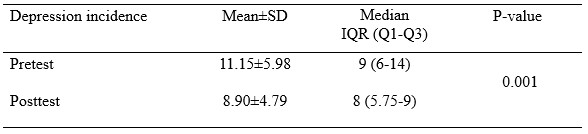
Table 4. Average Depression Incidence Pretest and Posttest Audio Hipnoterapy
Table 4 shows that depression incidence before giving audio hypnotherapy has a mean value = 11.15, while after giving audio hypnotherapy, it decreases to 8.90, with P-value <0.05.
DISCUSSION
Most pregnant women who face the birth process experience feelings of anxiety, even depression. Factors causing postpartum depression consist of biological factors, characteristics and background of the mother. Levels of the hormones estrogen (estradiol and estriol), progesterone, prolactin, cortisol which increase and decrease too quickly or too slowly are biological factors that cause postpartum depression [7]. The greater the decrease in estrogen and progesterone levels after childbirth, the greater the tendency for a woman to experience depression in the first 10 days after giving birth [8].
The estrogen and progesterone exert a suppressive effect on the activity of the monoamine oxidase enzyme. This enzyme can inactivate both noradrenaline and serotonin, which play a role in mood and depression. Estradiol and estriol are the active forms of estrogen formed by the placenta. Estradiol functions to strengthen the function of neurotransmitters by increasing the synthesis and reducing the breakdown of serotonin. Therefore, theoretically the decrease in estradiol levels due to childbirth plays a role in causing postpartum depression [9,10]. Biological causative factors are difficult and rarely measured in terms of maternal depressive symptoms [11]. Other factors that influence maternal depressive symptoms described in several studies include interpersonal variables (neural disorders, poor life experiences), social variables (marital dissatisfaction, lack of social support), and clinical variables related to pregnancy (risk in current pregnancy, problems with previous pregnancy) [12].
The results of the current study showed a decrease in the level of postpartum depression before and after listening to audio hypnotherapy. This means that listening to audio hypnotherapy can reduce the level of postpartum depression, where postpartum mothers feel comfortable, calm and relaxed after listening to audio hypnotherapy, although not every night or every day. Audio hypnotherapy is a hypnosis therapy, where respondents get positive suggestions through MP3 audio sent via cellphone. Hypnotherapy or clinical hypnosis is an integrative mind-body technique using hypnotic suggestions for specific therapeutic purposes that are identified jointly by the hypnotherapist and client [26].
The results of the Paired Samples Test analysis showed a difference in the average level of depression before and after listening to audio hypnotherapy with a significance value of P-value 0.001. For this reason, it can be concluded that audio hypnotherapy can reduce the level of depression in pregnant women, especially during the Covid-19 pandemic. The average decrease in anxiety levels of pregnant women before and after listening to audio hypnotherapy is 2.6.
Hypnotherapy has long been believed to reduce postnatal pain by giving suggestions in the form of positive commands [27]. Through the process of hypnosis, the patient is brought into a relaxed state in order to calm the autonomic nervous system and induce positive emotions that affect the patient's coping mechanisms for pain perception [28]. It stimulates positive emotions for more norepinephrine production, reduces ROS production, increases tryptophan levels, and stimulates the ventricular nucleus which functions to secrete oxytocin in the dopamine system, and subsequently plays a role in pain modulation [6,29]. A deeper hypnotic state (trance) can help activate the endorphins and encephalin system that can inhibit the production of substance P, a pain sensitizing agent in the dorsal horn of the spinal cord [30].
Some respondents experienced persistent depression despite the intervention. This condition was caused by the respondent's disobedience in carrying out audio hypnotherapy. Most of the respondents underwent audio hypnotherapy at night before going to bed. Some respondents listen when they feel uncomfortable or when they have free time. Some respondents do not run audio hypnotherapy every night.
In the future, audio hypnotherapy in order to reduce the level of depression in postpartum mothers can be an important alternative therapy besides the provision of medical drugs.
CONCLUSION
Before the intervention, there were 26 depressed respondents. Then after the intervention, there were 12 respondents. Audio hypnotherapy has been proven effective in reducing depression in postpartum mothers.
LIMITATIONS
The assessment of the level of depression in the current study is still subjective. Future research can use more real/objective measurements or combine subjective and objective scales. Furthermore, the research location only involves 3 places, therefore it cannot compare the results of similar studies in different populations.
The future research must be carried out involving several regions. This study also showed the possibility that socio-demographic factors' influence could not be controlled because the respondent's character was not matched.
FUNDING STATEMENT
This research did not receive any specific grant from funding agencies in the public, commercial, or not for profit sectors.
COMPETING INTERESTS STATEMENT
There are no competing interests for this study.
AUTHORS’ CONTRIBUTION
All authors equally contributed to preparing this article.
REFERENCES
- Field T. Prenatal depression effects on early development: a review. Infant behavior and development. 2011;34(1):1–14.
- Woods SM, Melville JL, Guo Y, Fan M-Y, Gavin A. Psychosocial stress during pregnancy. American journal of obstetrics and gynecology. 2010;202(1):61-e1.
- Melville JL, Gavin A, Guo Y, Fan M-Y, Katon WJ. Depressive disorders during pregnancy: prevalence and risk factors in a large urban sample. Obstetrics and gynecology. 2010;116(5):1064.
- Shorey S, Chee CYI, Ng ED, Chan YH, San Tam WW, Chong YS. Prevalence and incidence of postpartum depression among healthy mothers: a systematic review and meta-analysis. Journal of psychiatric research. 2018;104:235–48.
- Wang Z, Liu J, Shuai H, Cai Z, Fu X, Liu Y, et al. Mapping global prevalence of depression among postpartum women. Translational psychiatry. 2021;11(1):1–13.
- Varga K, Kekecs Z. Oxitocina y cortisol en interacción hipnótica. International Journal of Clinical and Experimental Hypnosis. 2014;62(1):111–28.
- Rizkiani I, Respati SH, Sulistyowati S, Budihastuti UR, Prasetya H. The Effect of Hypnotherapy on Serum Cortisol Levels in Post-Cesarean Patients. Journal of Maternal and Child Health. 2021;1(2549–0257):258–66.
- Yuniasti RD, Upoyo AS, Taufik A. The Effect of Hypnotherapy on Pain Intensity in Postoperative Patients: A Systematic Review. IJNP (Indonesian Journal of Nursing Practices). 2021;5(2):112–22.
- Lara MA, Navarrete L, Nieto L. Prenatal predictors of postpartum depression and postpartum depressive symptoms in Mexican mothers: a longitudinal study. Archives of women’s mental health. 2016;19(5):825–34.
- Campbell SB, Cohn JF. Prevalence and correlates of postpartum depression in first-time mothers. Journal of abnormal psychology. 1991;100(4):594.
- Mahandaru AH, Respati SH, Sulistyowati S, Laqif A, Prasetya H. The Effect of Hypnotherapy on Postpartum Pain and Depression in Women with Post Caesarean Delivery. Indonesian Journal of Medicine. 2021;6(2):194–205.
- Millizia A, Syafridah A. The Effect of Murottal Al-Quran Therapy on Pain in Post Cesarean Surgery Patients at Abby Mother and Child Hospital, Lhokseumawe City. Arkus. 2022;8(1):198–202.
- Dørheim SK, Bondevik GT, Eberhard-Gran M, Bjorvatn B. Sleep and depression in postpartum women: a population-based study. Sleep. 2009;32(7):847–55.
- Gjerdingen DK, Yawn BP. Postpartum depression screening: importance, methods, barriers, and recommendations for practice. The Journal of the American Board of Family Medicine. 2007;20(3):280–8.
- Eberhard-Gran M, Tambs K, Opjordsmoen S, Skrondal A, Eskild A. A comparison of anxiety and depressive symptomatology in postpartum and non-postpartum mothers. Social psychiatry and psychiatric epidemiology. 2003;38(10):551–6.
- Carter MJ. Diagnostic and statistical manual of mental disorders. Therapeutic recreation journal. 2014;48(3):275.
- Cox JL, Chapman G, Murray D, Jones P. Validation of the Edinburgh Postnatal Depression Scale (EPDS) in non-postnatal women. Journal of affective disorders. 1996;39(3):185–9.
- Stewart DE, Vigod S. Postpartum depression. New England Journal of Medicine. 2016;375(22):2177–86.
- Seymour-Smith M, Cruwys T, Haslam SA, Brodribb W. Loss of group memberships predicts depression in postpartum mothers. Social psychiatry and psychiatric epidemiology. 2017;52(2):201–10.
- Patel M, Bailey RK, Jabeen S, Ali S, Barker NC, Osiezagha K. Postpartum depression: a review. Journal of health care for the poor and underserved. 2012;23(2):534–42.
- Leger J, Letourneau N. New mothers and postpartum depression: a narrative review of peer support intervention studies. Health & social care in the community. 2015;23(4):337–48.
- Howell EA, Bodnar-Deren S, Balbierz A, Loudon H, Mora PA, Zlotnick C, et al. An intervention to reduce postpartum depressive symptoms: a randomized controlled trial. Archives of women’s mental health. 2014;17(1):57–63.
- Santos IS, Matijasevich A, Tavares BF, Barros AJD, Botelho IP, Lapolli C, et al. Validation of the Edinburgh Postnatal Depression Scale (EPDS) in a sample of mothers from the 2004 Pelotas Birth Cohort Study. Cadernos de saude publica. 2007;23:2577–88.
- Nasri Z, Wibowo A, Biostatistika D, Ghozali EW, Jiwa K. Faktor determinan depresi postpartum di kabupaten Lombok Timur. Pusat Penelitian dan Pengembangan Humaniora dan Manajemen Kesehatan; 2018.
- Levis B, Negeri Z, Sun Y, Benedetti A, Thombs BD. Accuracy of the Edinburgh Postnatal Depression Scale (EPDS) for screening to detect major depression among pregnant and postpartum women: systematic review and meta-analysis of individual participant data. bmj. 2020;371.
- Mubarokah RI, Prasetya H, Respati SH. The Effectiveness of Hypnotherapy to Reduce Anxiety in Pre-Caesarean Section Women. Journal of Maternal and Child Health. 2020;5(1):12–8.
- Kendrick C, Sliwinski J, Yu Y, Johnson A, Fisher W, Kekecs Z, et al. Hypnosis for acute procedural pain: a critical review. International Journal of Clinical and Experimental Hypnosis. 2016;64(1):75–115.
- Alarcon R. Synopsis of psychiatry: Behavioral sciences and clinical psychiatry. American Journal of Psychiatry. 1992;149(7):972–4.
- Sanders VM. The beta2-adrenergic receptor on T and B lymphocytes: do we understand it yet? Brain, behavior, and immunity. 2012;26(2):195–200.
- Price, Wilson A. Patofisiologi: Konsep Klinis Proses-proses Penyakit (Pathophysiology Clinical Concepts of Disease Processes), Buku I. Penerbit Buku Kedokteran EGC; 1995.
![]() This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
THE EFFECT OF PARENTAL HOLDING ON PAIN LEVELS INFANT DURING MEASLES IMMUNIZATION: QUASI-EXPERIMENTAL STUDY
Nesi Novita1*, Ratnaningsih Dewi Astuti2, Yeni Elviani3, Emi Latifah Sukasna4
1,4Department of Midwifery, Health Polytechnic of Palembang, Indonesia
2Department of Pharmacy, Health Polytechnic of Palembang, Indonesia
3Department of Nursing, Health Polytechnic of Palembang, Indonesia
* Corresponding author: Nesi Novita: Jl. InspekturYazid, Sekip Jaya, Kec. Kemuning, Kota Palembang, Sumatera Selatan 30114, Department of Midwifery, Health Polytechnic of Palembang, Indonesia, Orcid : https://orcid.org/0000-0002-1572-5448, Email: nesinovita51@gmail.com
ABSTRACT
Background: Immunization is the most effective and efficient public health effort in preventing various dangerous diseases, one of which is measles immunization. In practice, it is very closely related to needles that can cause anxiety, pain, avoidance, and even suffering in children when visiting health services to get vaccines. Parental care is a form of non-pharmacological intervention to treat pain. The purpose of this study was to determine the effect of parental maintenance on infant pain levels during measles immunization.
Methods: Quasi-experimental research method with pretest posttest control group design. The number of samples was 42 respondents who were divided into an intervention group and a control group in the working area of the Taman Bacaan Health Center Jambi city, Indonesia. This research was carried out in May-July 2021. The instrument used is the Face, Legs, Activity, Cry and Consolability (FLACC) scale and parental holding Standard Operating Procedures (SOP). Research statistical test with paired t test and independen t test.
Results: The results obtained p-value < 0.0001 with the level of pain in infants during measles immunization in the intervention group with an average of 5.52 and a standard deviation of 0.928, while the level of pain in infants during measles immunization in the control group with an average of 8.24 and standard deviation 1.044.
Conclusion: The parental grip in the position of holding the baby facing the chest with the parents affects the baby's level of pain during measles immunization. It is hoped that parental holding can be used as an alternative during immunization so that babies are more comfortable and can reduce pain.
Keywords: Parental Holding, Pain Management, Complementary Therapy, Measles Immunization
INTRODUCTION
Immunization is a public health effort that is most effective and efficient in preventing various dangerous diseases [1,2]. The magnitude of the role of immunization has been recorded in history to save the world community from illness and even death from diseases such as smallpox, polio, tuberculosis, hepatitis B, diphtheria, including measles [3–5]. Immunization is an effort to actively generate or increase a person's immunity to disease and if exposed to the disease, he or she will not get sick or experience mild illness [6].
Immunization is a critical agenda in children’s health. The World Health Organization (WHO) has set a goal that all countries should reach 90% coverage of all vaccines by 2020. The coverage rate considerably varies among countries. Today there are still 19.4 million unvaccinated children globally. Among those children, 60% come from 10 countries, and Indonesia is on that list [7,8].
In the Indonesian Health profile, the number of diseases that can be prevented by immunization for tetanus neonatorum increased in 2019, accompanied by suspected measles which also increased from 8,429 cases in the previous year, to 8,819 suspected cases of measles. Complete basic immunization coverage for infants from the 2019 target is expected to be 95% where in 2017 it reached 80% but in 2018 it decreased to 68.75% in districts/cities [7].
Immunization, which is mostly given in the form of injections, will create new problems. Pain and trauma due to immunization injections are effects that need attention in addition to other unexpected side effects. These side effects can be one of the causes of the lack of immunization coverage [8,9]. Parents assume that repeated immunizations can make children feel pain, which in turn contributes greatly to refusal, non-adherence to schedules, and delays in immunization [10]. Anxiety and pain due to injection are complaints that are often conveyed by both parents and children due to immunization. This condition makes parents reluctant to come to health services afterwards [8,11]. More than 90% of children experience severe stress during immunization which results in parents not complying with the existing schedule. The results of studies in America show that 24% of parents and 63% of children are afraid of needles when immunizations affect 7-8% of children with incomplete immunization status [8]. Needle phobia is estimated to reach 10-20% of the population [11].
One type of non-pharmacological intervention that has been developed to treat this pain is parental holding with hug therapy. Parental holding involves close contact between parent and baby, with the baby in the parent's arms, facing each other and parallel, and there is eye contact between the two. Parental grip may reduce the response to procedures that are painful for the baby, such as exercise [9]. Parents can get the attention and attention of their babies, this is in line with the recommendations from WHO to give special attention to babies during technique. According to Sari [9] hugs from parents to their children will help the pituitary gland secrete endorphins which function to improve the immune system, improve the ability to reduce pain, besides that the baby will avoid fear, anxiety and stress. In addition, the comfortable feeling that arises due to the mother's embrace is able to make the baby's body to secrete endorphins. Endorphins can improve mood, reduce anxiety, causing muscles to relax, and calm. So that the level of pain experienced by the baby will decrease [10,11].
According to Modanloo et al. [12] vaccination for early childhood is one of the most important public health interventions therefore clinical practice guidelines recommend the use of pain management strategies for infants during vaccination. Immunization is closely related to needles that can cause anxiety, avoidance, and even distress in children during visits to health services to get vaccines [13]. Medical procedures performed using needles such as immunizations are a source of pain for children. In addition, children will also feel anxiety and fear that become trauma which will continue into adulthood [14].
Pain is a protective mechanism that alerts the body that there will be tissue damage in the body that can affect survival [15]. This procedure is a painful procedure for children especially when immunized without adopting pain management [16]. Young children have difficulty understanding pain and procedures performed by health workers. Toddlers have difficulty interpreting the pain experienced, usually the toddler responds to pain with crying or facial expressions and simple words for toddlers who are able to speak [17].
Wahyuni & Suryani [18] resulted in an average pain scale before being given parental holding was 7.8 with a standard deviation of 1.4 and a minimum - maximum value range 5.0-10.0, and the average pain scale after parental holding was given was 3.6 with a standard deviation of 1.6 and a minimum-maximum value range of 1.0-7.0. With the result that 12 respondents who received parental holding intervention experienced a decrease in pain scale by a difference of 4, and the results of the sample t test were obtained p <0.05, meaning that there is a difference in pain scale before and before being given parental holding.
Research Sri Rahyanti et al [19] in Jakarta using a randomized clinical trial method and involving 34 respondents aged 1 to 4 years who were included in the intervention group and the control group, it was found that parental holding and upright position results in significant differences in pain scores in children were compared with the group that was not given parental holding and upright position with a p-value < 0.0001.
The results of the preliminary study at the time of giving technique midwives will perform a distraction technique (guided imagery) on the baby by saying there is something interesting on the other side, hidden the syringe used and giving breast milk after the exercise.
The problem in this study was pain management in infants during immunization is still not optimal and has an impact on ongoing trauma into adulthood. Is there any effect of parental holding on the baby's pain level during measles immunization?
The purpose of the study was to carry out parental holding it would affect the level of infant assistance during measles in the work area of the Taman Bacaan Health Center Palembang. The benefits are in order to provide comfort for babies during immunization and to make standard operating procedures (SOPs) with parental holding techniques that can be applied by health workers.
METHODS
Study design
This study used quantitative research methods with a quasi-experimental design and a pre-test post-test control group design.
Study Population
The population and sample are all infants under the age of 1 year given measles immunization in the working area of Taman Bacaan Health Center conducted on May-July 2021.
Inclusion criteria consisted of infants aged 9-12 months, The baby's parents agree that their child is a respondent, and the baby's parents agree to provide parental holding. And the exclusion criteria include babies who are not directly accompanied by their parents, babies who are not directly accompanied by their parents crying and not being soothed before the injection, sick or contraindication of immunization, and parents who refuse to be respondents.
Sample size
The numbers of samples involved were 42 participants who were chosen randomly or randomly from the population. The sample was divided into an intervention group of 21 respondents in (given parental holding by hugging) and 21 respondents in the control group (held and on the lap by his mother). Calculation of the number of samples was determined using the Slovin formula [20], where from a population of 47 people, d = 0.05, the total sample was 42 people. The research population, also known as the target population in this study, was the number of toddlers aged <1 year who visited the Taman Bacaan Health Center in Jambi City, Indonesia, conducted on May-July 2021, totaling 47 people.
Instruments
The independent variable is parental holding, and the dependent variable is the level of pain in infants during measles immunization. Pain variables were measured using the FLACC Pain Assessment Tools instrument. The FLACC Behavioral Pain Scale is a pain assessment tool for children less than three years of age or with cognitive impairment. FLACC is an acronym for Face, Legs, Activity, Cray, and Consolability (face, legs, activity, crying, and controllability). The five components are totaled, and the severity of pain is determined from a score of 0-10.
The assessment consisted of facial expressions (0-2), leg movements (0-2), activity (0-2), crying (0-2), ability to be entertained (0-2). The results of the behavioral scores are: 0: No Pain, 1-3: mild pain/mild discomfort, 4-6: moderate pain and 7-10: severe pain/severe discomfort. Measurement of the pain level variable was carried out before the intervention (pre-test) and 15 minutes after the intervention (post-test).
The type of intervention in this study was parental holding by hugging (Intervention group), and held and on the lap by the mother (control group). Both of these interventions were only carried out once when the child was given measles immunization.
Ethical Consideration
Prior to the implementation of measles immunization, the researcher first asked the mother's willingness to provide informed consent. After the consent became the research sample, the baby's mother signed the informed consent. No economic incentives were offered or provided for participation in this study. The study protocol matched the Declaration of Helsinki ethical guidelines for clinical studies. This research has been approved by the Health Research Ethics Commission of the Health Polytechnic of the Jambi Ministry of Health with the number LB.02.06/2/51/2021.
Statistical analysis
Data are presented as numbers and percentages for categorical variables. Continuous data were expressed as mean ± standard deviation (SD) or median with Interquartile Range (IQR). To see the distribution of research data, the Kolmogorov Smirnov test was used. The research data is normally distributed. Then proceed with bivariate analysis using the Paired t test. The Paired t test was used to determine the effect of Parental holding on infant pain level during measles immunization. Then to analyze the differences between the intervention and control groups, using the Independent t test. All tests with p-value <0.05 were considered significant. Statistical analysis was performed using the SPSS version 16.0 application.
RESULTS
The research respondents were 42 respondents, which were divided into 21 respondents in the intervention group and 21 respondents in the control group. The general description of the frequency distribution by gender and age can be seen in the following table:
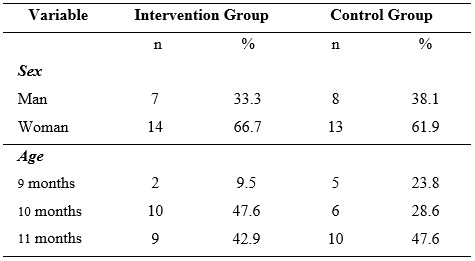
Table 1. Frequency distribution of general characteristics of the sample
Based on table 1, it is known that in the intervention group most of them were female, namely 66.7%, and in the control group most were female, namely 61.9%. While the age variable in the intervention group was mostly 10 months old, namely 47.6%, and in the control group most were 11 months old, namely 47.6%.
To find out the distribution of research data, a normality test of the data was carried out, presented in table 2.
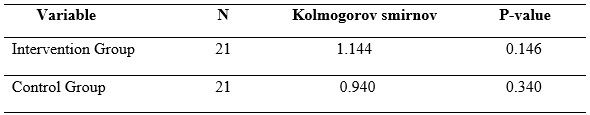
Table 2. Data normality test
Based on table 2, the research data obtained were normally distributed with p-value > 0.05.
Bivariate analysis aims to explain or describe the dependent variable, namely the level of infant pain during measles immunization in the intervention group and the control group.
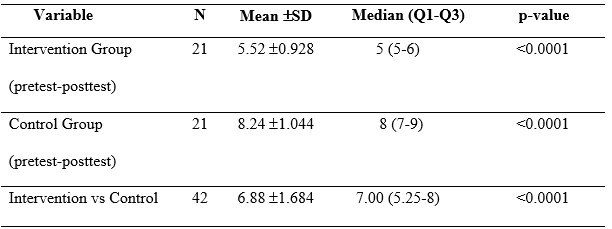
Table 3. Analysis of the effect of parental holding on infant pain levels
Based on table 3, it is known that the results of paired t test have the effect of parental holding on the baby's pain level during measles immunization with a p-value < 0.0001 . The mean value of the two groups (intervention and control) is 6.88. The result of independent t test is a p-value <0.05, it means that there is a difference in the effect of the two interventions on the pain level of infant during measles immunization.
DISCUSSION
The purpose of the study was to carry out parental holding it would affect the level of infant assistance during measles in the work area of the Taman Bacaan Health Center Palembang. In this study, the age of the respondents was between 9-11 months; based on Minister of Health regulations no. 42 of 2013 the first measles immunization was given to infants aged 9 months. Measles immunization is given in 2 doses, namely when the baby is 9 months old (as basic immunization), and when the baby is 9 months old (as basic immunization). when the child is 2 years old (as a follow-up immunization) [21]. According to Perry et al. [17] young children have difficulty understanding pain and procedures performed by health workers. Toddlers have difficulty interpreting the pain experienced, usually the toddler responds to pain with crying or facial expressions and simple words for toddlers who are able to speak. Babies have not been able to express pain with words; therefore the level of pain in infants is measured using the FLACC scale which is seen through the baby's responses in the form of behaviour, facial expressions, crying, and movements.
In this study, the observed of level pain was in infants aged 9-12 months, babies could not show the pain response, it was necessary to have skills of health workers to assess the baby’s pain level based on the FLACC scale, besides that most mothers said they were afraid to accompany the baby directly during immunization. In this study, it was stated that there was a significant decrease in the infant's pain level during measles immunization with a p-value < 0.0001 and the minimum and maximum pain values obtained from the control group (who were not given parental holding) of 7.00 and 10.00. to the minimum - maximum values in the intervention group (given parental holding) of 4.00 and 7.00.
This study is in line with research Modanloo et al. [12] which states that pain management strategies during vaccination can be carried out by holding. While in this study, parental holding is done by hugging or hugging. According to Sari [9] hugs from parents to their children will help the pituitary gland secrete endorphins which function to increase the immune system, increase the ability to reduce feelings of anxiety. In addition, the baby will avoid fear, anxiety and stress. Increased endorphins can affect mood, reduce anxiety, cause muscles to relax, and calm down, therefore, the level of pain experienced by the baby will decrease. Endorphins are natural substances produced by the body whose job is to inhibit the passage of pain sensations from the traumatized body part to the brain. Everyone's endorphin levels are different, this causes different responses to the same type of pain [22]. Besides being useful for inhibiting pain, endorphins also have other benefits, namely to regulate hormone production, reduce persistent aches and pains, and control stress [23,24]. In line with research Qiu et al. [25] which states that endorphins are endogenous opioids that are released in response to pain and increase pain inhibition when an organism is exposed to stress or painful stimuli (acute pain). In this study, painful stimuli in the form of measles immunization injections can affect the release of endorphins.
This study is in line with research Dewi et al. [26] which states that babies who given parental holding will feel a sense of love and comfort from their parents, so that the fear and anxiety they experience will be reduced because of their parents holding them. Parental hugs provide a sense of comfort and reduce pain levels in children.
In this study, the difference in the level of infant pain in the intervention group and the control group can be seen from the pain response felt by the baby, as evidenced by changes in facial expressions, grimacing, body squirming, crying, body rigidity, restlessness, to an increase in stress hormones. Parental holding involves close contact between parents and babies, with the baby in the parent's arms, facing each other and parallel, and there is eye contact between the two. Parental holding may reduce the response to procedures that are painful for the baby, such as immunizations. Parents can distract and calm their babies, this is in line with the recommendations from WHO to pay special attention to babies during immunization. When babies are immunized using injections, parental holding by hugging other forms of touch that can minimize pain, make babies feel more comfortable and good, so that it has an impact on the baby's quality of life by getting a direct touch of love from the parents [18].
Parental holding comfort to the baby and mother at the time of immunization with the injection technique, so that immunization does not have an impact on causing trauma to babies until they are adults for fear of being injected. In addition, it can be used as an alternative effort for health workers when giving immunizations to minimize level pain in infants.
Researchers would like to convey that these two interventions have been proven to reduce immunization pain in children. although in the independent t test the two interventions had differences in reducing the pain scale in immunized children. This means that the way the mother holds or hugs the child during immunization has a calming effect on the child.
The strength of this study compared to previous studies lies in the comparison of the effects of 2 different interventions on the pain scale during measles immunization in children which was not carried out in the previous study, which only used 1 intervention in the form of parental holding.
CONCLUSION
Parental holding has an effect on reducing pain in infants when given measles immunization by providing a sense of comfort, and reducing distress in infants. So that health workers can use this method as an alternative in reducing pain levels in infants when immunized. Parental holding can be used as a basis in formulating policies or standard operating procedures (SOPs) for the management of measles immunization, namely the provision of parental holding as one of the procedures in reducing pain levels in infants during immunization. With this policy, it is hoped that health workers will apply techniques to reduce pain in infants when immunized against measles.
LIMITATION OF STUDY
One of the limitations of this study is the very small sample size (a pilot study). The research location only involves one region, therefore it cannot compare the results of similar studies in different populations. In addition to these two things, the environmental conditions where the vaccination is carried out must be designed not to have little effect on the research results. Likewise, the clothing of health workers must be adapted because usually, children are treated at hospitals or trauma clinics in white clothes.
FUNDING STATEMENT
This research did not receive any specific grant from funding agencies in the public, commercial, or not for profit sectors.
CONFLICT OF INTEREST
The authors report no conflict of interest.
ACKNOWLEDGEMENT
We would like to thank the director of the Department of Midwifery and Pharmacy, Palembang Health Polytechnic for supporting this research
AUTHORS’ CONTRIBUTION
All authors equally contributed to preparing this article.
REFERENCES
1. Whitney CG, Zhou F, Singleton J, Schuchat A. Benefits from immunization during the vaccines for children program era—United States, 1994–2013. Morbidity and Mortality Weekly Report. 2014;63(16):352.
2. Doherty M, Buchy P, Standaert B, Giaquinto C, Prado-Cohrs D. Vaccine impact: Benefits for human health. Vaccine. 2016;34(52):6707–14.
3. Greenwood B. The contribution of vaccination to global health: past, present and future. Philosophical Transactions of the Royal Society B: Biological Sciences. 2014;369(1645):20130433.
4. Miller MA, Sentz JT. Vaccine-preventable diseases. 2011;
5. Ehreth J. The value of vaccination: a global perspective. Vaccine. 2003;21(27–30):4105–17.
6. Kemenkes R. Buku Ajar Imunisasi. Pusat Pendidikan dan Pelatihan Tenaga Kesehatan. 2014.
7. UNICEF WHO. Progress and challenges with achieving universal immunization coverage: 2019 estimates of National immunization coverage [Internet]. Februari 10, 2020. Geneva, Switzerland: WHO; 2019. Available from: https://www.who.int/%0Aimmunization/monitoring_surveillance/who-immuniz.pdf.
8. Hardhantyo M, Chuang Y-C. Urban-rural differences in factors associated with incomplete basic immunization among children in Indonesia: A nationwide multilevel study. Pediatrics & Neonatology. 2021;62(1):80–9.
9. Indah. Pengaruh parental holding terhadap distress anak selama prosedur insertion intravena (IV) di ruang rawat inap anak RSUD Adnan WD Payakumbuh tahun 2019. stikes perintis padang; 2019.
10. Nurlaila N, Baniyah N, Iswati N. Terapi Dekapan dapat Menurunkan Kecemasan Anak saat Pemberian Terapi Intravena. Jurnal Berita Ilmu Keperawatan. 2022;15(1):27–33.
11. Utario Y, Rustina Y, Efendi D. Family Centered Care Intervention Effectively Reduces Parental Anxiety in Perinatology Ward. Dunia Keperawatan: Jurnal Keperawatan dan Kesehatan. 2021;9(1):143–51.
12. Modanloo S, Stacey D, Dunn S, Choueiry J, Harrison D. Parent resources for early childhood vaccination: An online environmental scan. Vaccine. 2019;37(51).
13. Harrington JW, Logan S, Harwell C, Gardner J, Swingle J, McGuire E, et al. Effective analgesia using physical interventions for infant immunizations. Pediatrics. 2012;129(5).
14. Canbulat Şahiner N, Inal S, Sevim Akbay A. The Effect of Combined Stimulation of External Cold and Vibration During Immunization on Pain and Anxiety Levels in Children. Journal of Perianesthesia Nursing. 2015;30(3).
15. Sherwood. Fisiologi Manusia: Dari Sel Ke Sistem. 8th ed. Jakarta: Jakarta. EGC; 2012.
16. Özdemir FK, Tüfekci FG. The effect of using musical mobiles on reducing pain in infants during vaccination. Journal of Research in Medical Sciences. 2012;17(7).
17. Perry AG, Potter PA, Ostendorf WR. Clinical Nursing Skills & Techniques. Elsevier. 2014.
18. Wahyuni F, Suryani U. Efektifitas Terapi Mendekap Dan Terapi Musik Dalam Menurunkan Skala Nyeri Pada Bayi Saat Dilakukan Imunisasi Campak. Jurnal Ilmiah Keperawatan Sai Betik. 2021;16(1):13–23.
19. Sri Rahyanti NM, Nurhaeni N, Wanda D. Could a Certain Sitting Position Reduce the Pain Experienced by a Child? The Benefits of Parental Holding and an Upright Position. Comprehensive Child and Adolescent Nursing. 2017;40.
20. Sugiyono D. Metode penelitian pendidikan pendekatan kuantitatif, kualitatif dan R&D. Alfabeta; 2013.
21. Kemenkes R. Peraturan Menteri Kesehatan Republik Indonesia No. 42 Tahun 2013. 2013.
22. Mawaddah E, Rusmini R, Ningsih MU, Mardiatun M. Penerapan Konsep Atraumatic Care Saat Pemasangan Infus dan Venipunktur pada Anak. Jurnal Keperawatan Terpadu (Integrated Nursing Journal). 2021;3(1):17–27.
23. Khasanah NN, Astuti IT. Teknik Distraksi Guided Imagery sebagai Alternatif Manajemen Nyeri pada Anak saat Pemasangan Infus. Jurnal Kesehatan. 2017;8(3):326–30.
24. Hafizzanovian H, Oktariana D, Apriansyah MA, Yuniza Y. peluang terjadinya immunization stress-related response (isrr) selama program vaksinasi covid-19. Jurnal Kedokteran dan Kesehatan: Publikasi Ilmiah Fakultas Kedokteran Universitas Sriwijaya. 2021;8(3):211–22.
25. Qiu J, Jiang Y fei, Li F, Tong Q hong, Rong H, Cheng R. Effect of combined music and touch intervention on pain response and β-endorphin and cortisol concentrations in late preterm infants. BMC Pediatrics. 2017;17(1).
26. Dewi TS, Mardiah W, Rukmasari EA. Respon dan Pengelolaan Nyeri Pada Bayi Saat Imunisasi Pentabio di Wilayah Kerja Puskesmas Haurpanggung. In: Proceeding Seminar Nasional Keperawatan. 2020. p. 116–21.
![]() This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
THE EFFECT OF VIRTUAL EDUCATION ON THE KNOWLEDGE OF POSTPARTUM MOTHERS ABOUT BREASTFEEDING DURING THE COVID-19 PANDEMIC: QUASI-EXPERIMENTAL DESIGN
Imelda, Atika Fadhilah Danaz Nasution*, Ika Murtiarini, Rosmaria, Diniaty
Department of Midwifery, Health Polytechnic of Jambi, Indonesia
Corresponding author: Atika Fadhilah Danaz Nasution, Jl. Prof DR GA Siwabessy No.42, Buluran Kenali, Kec. Telanaipura, Kota Jambi, Jambi 36122, Indonesia.
Orcid: https://orcid.org/0000-0002-4181-8621; Email: atikapoltekkes@gmail.com
Abstract
Introduction: Postpartum mothers and newborns are a group that is vulnerable to COVID-19. Due to the COVID-19 pandemic, access to essential services such as breastfeeding counseling in hospitals, health clinics, and home visits has been disrupted. Postpartum mothers will immediately breastfeed. Therefore there is a need for knowledge, appropriate information, and support to provide breast milk, especially during the COVID-19 pandemic. This study aims to analyze the effect of virtual counseling on the knowledge of postpartum mothers during the COVID-19 pandemic at the Delima Midwife Clinic in Jambi City.
Materials and Methods: The current study utilized a quasi-experimental design with one group design pretest-posttest approach. This research was conducted in January-October 2021 and involved 75 postpartum mothers. This study using the zoom app. and questionnaire. Data analysis using Wilcoxon statistical test.
Results: The results showed an increase in knowledge where before being given virtual education, most of the respondents' knowledge was in the Poor category, as much as 80% (mean 6.18). After the intervention, the knowledge of most respondents in the Good category was 46.7% (mean 12.15) with P-value <0.05.
Conclusion: The study concludes that virtual counseling significantly affects the knowledge of postpartum mothers about breastfeeding during the COVID-19 pandemic.
Keywords: Postpartum Mothers, Breastfeeding, COVID-19 pandemic, Counseling, Virtual.
INTRODUCTION
Coronavirus Disease 2019 (COVID-19) is an infectious disease caused by Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2). SARS-CoV-2 is a new type of coronavirus that has never been previously identified in humans [1,2]. There are at least two types of coronaviruses known to cause diseases that can cause severe symptoms, such as Middle East Respiratory Syndrome (MERS) and Severe Acute Respiratory Syndrome (SARS) [3]. The average incubation period is 5-6 days, with the most prolonged incubation period being 14 days. In severe cases of COVID-19, it can cause pneumonia, acute respiratory syndrome, kidney failure, and even death [4,5].
The spread of COVID-19 has reached almost all provinces in Indonesia, with the number of cases and deaths increasing. This condition impacts the political, economic, social, cultural, defense and security aspects, as well as the welfare of the people in Indonesia [6]. Indonesia reported its first case of COVID-19 on March 2, 2020, and the number continues to grow until now. The data on confirmed cases of COVID-19 in Indonesia as of October 21, 2021, were 4.237.834 people, 143.120 people died, and patients who had recovered were 4.079.120 people [7]. Meanwhile, in Jambi Province, COVID-19 cases increased sharply. As of October 3, 2021, the Jambi Provincial Government recorded 29.616 positive confirmed cases of COVID-19, 768 people died, and 28.476 people recovered [8].
Postpartum mothers and newborns are a group that is vulnerable to the COVID-19 virus [9,10]. During the COVID-19 pandemic, access to essential services such as breastfeeding counseling in hospitals, health clinics, and home visits has been disrupted [11,12]. The amount of inaccurate information and news circulating about the safety of breastfeeding has reduced the number of breastfeeding mothers because mothers are afraid of transmitting diseases to their babies even though this is the most appropriate moment to provide the best intake for babies through breastfeeding. After all, breast milk contains immune substances which protect children from infections and chronic diseases and reduces the chances of suffering from health problems later in life. The Covid-19 virus has never been found in breast milk [13,14].
Social restrictions during the COVID-19 pandemic require staying at home so that continuous care cannot be carried out, both health workers to make visits and mothers and babies to check their health status at the nearest health service. The impact of this situation can cause stress and worry for postpartum mothers who are still adapting to breastfeeding activities. Breastfeeding mothers need to continue to get support in the form of assistance to overcome problems during the breastfeeding process [2,15].
The current state of the COVID-19 pandemic has made it difficult for postpartum mothers to get information and consult face-to-face due to the strict rules of physical distancing. This condition resulted in a decrease in the number of visits by postpartum mothers to health workers. The limitations of accessing information on exclusive breastfeeding from health workers can be overcome by providing health promotions delivered via Telemedia, where postpartum mothers can communicate virtually and see some presentation materials and videos of good and correct breastfeeding techniques [16,17].
Health promotion through Telemedia/online is expected to increase the knowledge of postpartum mothers about exclusive breastfeeding and sound and correct breastfeeding techniques. This online learning for postpartum mothers is expected to help postpartum mothers to obtain information and consult during the COVID-19 pandemic.
This study aims to examine the effect of Virtual Counseling on Postpartum Mother's Knowledge of Breastfeeding during the Covid-19 Pandemic at the Delima Midwife Clinic in Jambi City.
Method
Trial design
The current study utilized quasi-experimental design with one group design pretest-posttest approach.
Participants
This research was conducted in January-October 2021 and involved 75 postpartum mothers who were randomly selected and met the sample inclusion requirements, such as breastfeeding mothers, mothers who have never participated in counseling activities about breastfeeding, and who have the Zoom app.
Intervention
The research variable is the knowledge of postpartum mothers. Before the intervention was given, the researcher first measured the level of knowledge of postpartum mothers (pre-test). After being given the intervention, the researcher again measured the level of knowledge of postpartum mothers (post-test). In this study, the intervention model provided was virtual education about breastfeeding, which was carried out once for 1 hour, i.e., 45 minutes of material delivery and 15 minutes of discussion). In this study, researchers explain the principles of breastfeeding, including the correct way of breastfeeding. The researcher presented the material with a poster or picture of the correct breastfeeding technique.
The knowledge questionnaire consists of 33 questions with correct and incorrect answer choices. If the postpartum mother answered correctly, she was given a score of 1; if the answer was wrong, she was given a score of 0. The range of scores obtained was between 0-33. The questionnaire used the Guttman scale. The contents of the postpartum mother's knowledge questionnaire included the benefits of breastfeeding, breastfeeding techniques, breastfeeding positions, correct breastfeeding steps, duration and frequency of breastfeeding, milk release, milk storage, breast care, nutrition during breastfeeding, and problems in breastfeeding.
The Guttman scale has an important feature where it is a cumulative scale and only measures one dimension of a multidimensional variable; therefore, this scale is dimensionless. The data obtained are interval data or dichotomous ratios (two alternatives) [18].
Researchers did not try out the knowledge questionnaire because this questionnaire was adopted from Nalsalisa's study [19]. The results of the validity test obtained a p-value <0.05 on 33 questions. For the reliability test, this questionnaire is reliable because the value of r count> r table is reliable.
The researcher has worked as a lecturer and researcher for 10-15 years and has Master and Doctoral degrees. The researcher has done much research in the health sector and has compiled many questionnaires, so the researcher prepared a questionnaire for this study. Before the research was conducted, the questionnaire was tested on ten postpartum mothers, and the results indicated that two questions had to be replaced because they were invalid.
Outcomes
This study has produced a description of the knowledge of postpartum mothers before and after virtual educational interventions and the effect of virtual education interventions on postpartum mothers' knowledge.
Sample size
75 postpartum mothers who have been calculated using the Slovin formula at a precision (d) = 0.1, the total population is 307 people. The study population, also known as the target population in this study, is the number of postpartum mothers who visited the Delima Midwife Clinic, Jambi City, Indonesia, in 2020, totaling 307 people.
Ethical Consideration
No economic incentives were offered or provided for participation in this study. In this study, because the subject was still a minor so the researcher had asked for and obtained parental consent so that their child could participate in the study. The study was performed in accordance with the ethical considerations of the Helsinki Declaration. This study obtained ethical feasibility under the Health Research Ethics Commission of the Ministry of Health, Jambi, and registration number: LB.02.06/2/161/2021.
Statistical analysis
Data are presented as numbers and percentages for categorical variables. Continuous data were expressed as mean ± standard deviation (SD) or median with Interquartile Range (IQR). To see the distribution of research data, the Kolmogorov Smirnov test was used. Then proceed with bivariate analysis using the Wilcoxon test. All tests with p-value (p)<0.05 were considered significant. Statistical analysis was performed using the SPSS version 16.0 application.
RESULTS
The characteristics of respondents in this study include age, education, employment status and parity. The following is the frequency distribution of the respondents' characteristics in this study:

Table 1. Frequency Distribution of Respondents Characteristics
The majority of respondents are in the age range of 32-38, have high school education, do not work and have multiparous status.
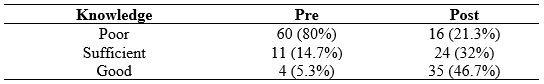
Table 2. Distribution of knowledge before and after interventions
Most of the respondents' knowledge before the intervention was in the Poor category, as much as 80%. After the intervention, the knowledge of postpartum mothers was mainly in the Good category, as much as 46.7%.
Table 3 shows that the Kolmogorov Smirnov statistical test results obtained a significant value of knowledge at the pretest and posttest virtual education, each less than 0.05.

Table 3. Normality Test Results of Knowledge pretest and posttest virtual education
The knowledge data at the pretest and posttest virtual education not normally distributed. Therefore, the statistical difference test was tested using Wilcoxon (Table 4)

Table 4. Average Knowledge Pretest and Posttest Virtual Education
Table 4 shows that knowledge before giving virtual education has a mean value = 6.18, while after giving virtual education, it increases to 12.15, with P-value <0.05.
DISCUSSION
Postpartum conditions cause a partial decrease in immunity due to physiological changes during pregnancy, making postpartum women more susceptible to viral infections. Therefore, the COVID-19 pandemic will likely cause severe consequences for postpartum mothers. Social distancing measures are effective in reducing disease transmission. It also applies to postpartum mothers to limit themselves to not being exposed to the outside environment, let alone traveling to pandemic areas [20,21]. The risk of postpartum mothers being infected with COVID-19 is one of them when visiting a postnatal check-up at a midwifery clinic or hospital, so mothers must increase their vigilance by continuing to be disciplined in the use of PPE [21,22]. Postpartum mothers can limit visits to obstetric clinics or hospitals by conducting online consultations, actively self-checking for signs and dangers during pregnancy, and only making visits when things are worrying. This study aims to analyze the effect of virtual education on postpartum mothers' knowledge about breastfeeding [13,23]. Based on the univariate analysis, it is known that most of the respondents have less knowledge (80%), and a small portion (5.7%) have good knowledge. Health promotion cannot be separated from activities or efforts to convey health messages to communities, groups, or individuals.
There are still many mothers who say that mothers who are confirmed positive for COVID-19 cannot breastfeed their babies directly. The world Health organization still recommends that mothers continue breastfeeding their babies but must follow hygiene procedures. SARS-CoV-2 has not been detected in mothers with suspected or confirmed COVID-19, and there is no evidence that the virus is transmitted through breast milk [22,24].
Postpartum mothers who have good knowledge increased to 42% after counseling. The mean value of knowledge before counseling was done was 6.18, then after virtual counseling, there was an increase in the mean value of postpartum mothers' knowledge about breastfeeding to 12.15.
There is an increase in knowledge of breastfeeding mothers about breastfeeding during the COVID-19 pandemic. It is hoped that changes in behavior will occur, such as giving exclusive breastfeeding to their babies because concerns about transmission of COVID-19 through breast milk have been answered, namely that it is not proven to transmit COVID-19, and breastfeeding mothers can also provide breast milk exclusively with due observance of health protocols. Thus, even though the baby is in a pandemic, the baby's needs are still met with the mother giving exclusive breastfeeding even though the mother is still working and can still provide exclusive breastfeeding [25].
The statistical test results obtained a P value < 0.05, so it can be concluded that virtual counseling affects postpartum mothers' knowledge about breastfeeding during the COVID-19 pandemic. Silalahi's research (2012) reported differences in the level of knowledge of postpartum mothers after being given counseling. There was an effect of counseling on exclusive breastfeeding on mothers' knowledge about exclusive breastfeeding.
This finding strengthens the previous finding that reported that knowledge for the intervention group obtained a mean value of 58.89. In contrast, the control group obtained a mean value of 45.47, with P-value = 0.012, meaning that counseling affects the knowledge of postpartum mothers in the Timbusseng Village Work Area, Pattallassang District, Kab. Gowa [26].
Extension activities can be carried out with two-way communication where the communicator (extension) provides the communicant opportunity to provide feedback on the material. This interactive discussion on two-way communication is expected to trigger the desired behavior change. This health education's success is determined by the material presented and the interpersonal relationships between communicators and communicants [16,27]. An indicator of the success of extension that can be measured quickly is the similarity of meaning or understanding of what is conveyed by the communicator and accepted by the communicant [24,28].
Virtual counseling media is an alternative for health workers to consult postpartum mothers during the COVID-19 pandemic to reduce the risk of spreading COVID-19 disease, which can endanger pregnant women and neonates. The Good knowledge of the mother determines the correct breastfeeding technique. Good knowledge about the importance of breastfeeding and ways to breastfeed will form a positive attitude, and then correct breastfeeding behavior will occur [24,29].
CONCLUSION
Virtual counseling has a significant effect on the knowledge of postpartum mothers about breastfeeding during the COVID-19 pandemic.
STUDY LIMITATIONS
There are limitations to the number of research samples, and samples only come from one location; therefore, the results of this study cannot be differentiated from samples or participants with different characters in other locations. Future research must involve many samples, and research locations must also be heterogeneous.
FUNDING STATEMENT
This research did not receive any specific grant from funding agencies in the public, commercial, or not for profit sectors.
CONFLICT OF INTEREST
The authors report no conflict of interest.
AUTHORS’ CONTRIBUTION
All authors equally contributed to preparing this article.
ACKNOWLEDGEMENT
We would like to thank the director of the Department of Midwifery, Health Polytechnic of Jambi, Indonesia for supporting this research.
REFERENCES
1. Palmquist AEL, Parry KC, Wouk K, Lawless GC, Smith JL, Smetana AR, et al. Ready, Set, BABY live virtual prenatal breastfeeding education for COVID-19. Journal of Human Lactation. 2020;36(4):614–8.
2. Nguyen PH, Kim SS, Nguyen TT, Hajeebhoy N, Tran LM, Alayon S, et al. Exposure to mass media and interpersonal counseling has additive effects on exclusive breastfeeding and its psychosocial determinants among Vietnamese mothers. Maternal & child nutrition. 2016;12(4):713–25.
3. Shu Y, He H, Shi X, Lei Y, Li J. Coronavirus disease‑2019. World Academy of Sciences Journal. 2021;3(2):1.
4. World Health Organization. The Corona Virus Disease 2019 (COVID-19). 2020;
5. Kumar D, Malviya R, Sharma PK. Corona virus: a review of COVID-19. EJMO. 2020;4(1):8–25.
6. Yamali FR, Putri RN. Dampak covid-19 terhadap ekonomi indonesia. Ekonomis: Journal of Economics and Business. 2020;4(2):384–8.
7. Kompas.com. UPDATE 21 Oktober: 143.120 Orang di Indonesia Meninggal akibat Covid-19 [Internet]. 21 Oktober 2021. 2021. Available from: https://nasional.kompas.com/read/2021/10/21/18281271/update-21-oktober-143120-orang-di-indonesia-meninggal-akibat-covid-19
8. Analisis TP&, PENANGANAN S, Provinsi C-19, Jambi. Pemetaan Risiko Covid-19 Kabupaten/Kota di Provinsi Jambi [Internet]. 3 Oktober 2021. 2021. Available from: https://corona.jambiprov.go.id/v2/files/zonasi/Pemetaan Risiko_3 Oktober 2021.pdf
9. Liu H, Wang L-L, Zhao S-J, Kwak-Kim J, Mor G, Liao A-H. Why are pregnant women susceptible to COVID-19? An immunological viewpoint. Journal of reproductive immunology. 2020;139:103122.
10. Barrero-Castillero A, Beam KS, Bernardini LB, Ramos EGC, Davenport PE, Duncan AR, et al. COVID-19: neonatal–perinatal perspectives. Journal of Perinatology. 2021;41(5):940–51.
11. Schindler-Ruwisch J, Phillips KE. Breastfeeding during a pandemic: The influence of COVID-19 on lactation services in the Northeastern United States. Journal of Human Lactation. 2021;37(2):260–8.
12. Sikorski J, Renfrew MJ, Pindoria S, Wade A. Support for breastfeeding mothers: a systematic review. Paediatric and perinatal epidemiology. 2003;17(4):407–17.
13. Singh AP, Kumar VHS, Panda S. Supporting Breastfeeding in 2021 and Beyond—Lessons from the Pandemic. Pediatric Reports. 2021;13(2):289–301.
14. Theurich MA, McCool-Myers M, Koletzko B. Supporting breastfeeding of small, sick and preterm neonates. In: Seminars in Perinatology. Elsevier; 2021. p. 151387.
15. Lima ACMACC, Chaves AFL, Oliveira MG de, Lima SAFCC, Machado MMT, Oriá MOB. Breastfeeding consultancy during the COVID-19 pandemic: experience report. Escola Anna Nery. 2020;24.
16. Haider R, Ashworth A, Kabir I, Huttly SRA. Effect of community-based peer counsellors on exclusive breastfeeding practices in Dhaka, Bangladesh: a randomised controlled trial. The lancet. 2000;356(9242):1643–7.
17. Haider R, Kabir I, Huttly SRA, Ashworth A. Training peer counselors to promote and support exclusive breastfeeding in Bangladesh. Journal of Human Lactation. 2002;18(1):7–12.
18. Sugiyono D. Metode penelitian pendidikan pendekatan kuantitatif, kualitatif dan R&D. 2013;
19. Nalsalisa J. Pengaruh Konseling Laktasi terhadap Breasfeeding Self-Efficacy pada Ibu Menyusui di Wilayah Kerja Puskesmas Sungai Mandau Tahun 2020. Universitas Pahlawan Tuanku Tambusai; 2020.
20. Giacalone A, Rocco G, Ruberti E. Physical health and psychosocial considerations during the COVID-19 outbreak. Psychosomatics. 2020;61(6):851–2.
21. Dubey S, Biswas P, Ghosh R, Chatterjee S, Dubey MJ, Chatterjee S, et al. Psychosocial impact of COVID-19. Diabetes & Metabolic Syndrome: clinical research & reviews. 2020;14(5):779–88.
22. Ceulemans M, Verbakel JY, Van Calsteren K, Eerdekens A, Allegaert K, Foulon V. SARS-CoV-2 infections and impact of the COVID-19 pandemic in pregnancy and breastfeeding: Results from an observational study in primary care in Belgium. International journal of environmental research and public health. 2020;17(18):6766.
23. Wilson JC. Using social media for breastfeeding support. Nursing for Women’s Health. 2020;24(5):332–43.
24. Anderson AK, Damio G, Young S, Chapman DJ, Pérez-Escamilla R. A randomized trial assessing the efficacy of peer counseling on exclusive breastfeeding in a predominantly Latina low-income community. Archives of Pediatrics & Adolescent Medicine. 2005;159(9):836–41.
25. Rochmawati R, Kusmintarti A, Fary V, Elfaristo L, Pembayun EL, Hayuningsih S, et al. Meningkatkan Kapasitas Ibu Menyusui Melalui Penyuluhan Kesehatan Mengenai Pemberian ASI Eksklusif Selama Masa Pandemi COVID-19. Sasambo: Jurnal Abdimas (Journal of Community Service). 2021;3(2):76–82.
26. Syahrir S, Alam S. Faktor-Faktor yang Berhubungan dengan Teknik Menyusui pada Ibu di Puskesmas Pattallassang Kabupaten Takalar. Al-Sihah: The Public Health Science Journal. 2016;8(2):130–8.
27. Graffy J, Taylor J. What information, advice, and support do women want with breastfeeding? Birth. 2005;32(3):179–86.
28. Anandita MYR. Penyuluhan Kesehatan Melalui Telemedia Pada Ibu Hamil tentang Mempersiapkan Pemberian ASI Eksklusif. Jurnal Pengabdian Masyarakat Bakti Parahita (p-ISSN-2747-2094). 2020;1(01).
29. Aidam BA, Perez-Escamilla R, Lartey A. Lactation counseling increases exclusive breast-feeding rates in Ghana. The Journal of nutrition. 2005;135(7):1691–5.
![]() This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
The Effectiveness of Electric Toothbrushes and Conventional Toothbrushes in Reducing Plaque Scores on School-Aged Children with Mental Impairment: Pilot Study
Rusmiati*, Rosmawati, Sri Febrianti, Andriani
Department of Dental Health, Health Polytechnic Ministry of Health Jambi, Indonesia
Corresponding author: dr. Rusmiati, Tazar Street, BuluranKenali, Kec. Telanaipura, Kota Jambi, Jambi 36361, Indonesia, Orcid :https://orcid.org/0000-0003-0913-4219, Phone: +62 823-0615-7373, Email: rusmiati.dentalpoltekkes@gmail.com
ABSTRACT
Introduction: Improving the quality of life of children is one of the goals of the health development program. The growth of children's health is not discriminated against in this scenario. All children with special needs or impairments are covered by child health services, whether at Special Schools (SS), other institutions, or in the community. This study aimed to evaluated the effectiveness of using an electric toothbrushes, compared to conventional toothbrushes, in the reduction of dental plaque score.
Methods: This study was designed as a quasi-experimental study with a pretest-posttest design. All school-aged children with mental impairment in SS Jambi City, Indonesia were included in this study. Overall, 20 children were assigned to the intervention group (n=10) and to the control group (n=10). The Personal Hygiene Performance-Modified (PHP-M) was used to examine plaque index for the assessment of dental and oral hygiene.
Results: In the pretest-posttest, mean difference values in plaque scores were statistically significant in both the intervention (19.50±3.89, p<0.009) and control (17.90±1.61, p<0.001) groups. A statistically significant reductions was showed in mean post-test plaque index (p<0.001) in the intervention group compared to the control group (14.50 ±7.83; 32.80± 13.14, respectively).
Conclusion: When compared to conventional toothbrushes, electric toothbrushes are more effective in reducing plaque scores in mentally retarded children at SS Jambi City.
Keywords: Conventional toothbrush, Electric toothbrush, Plaque score, Children, Mental impairment
INTRODUCTION
Overall health, well-being, and quality of life are all influenced by dental and oral health[1,2]. Oral health is a state of a person who is free of chronic oral diseases, facial pain, mouth and throat cancer, infections and sores, gum disease, tooth decay, tooth loss, and other diseases that impair the ability to bite, chew, smile, and talk[3].
Dental and oral health care are crucial components of comprehensive health care[4–6]. Dental and oral health indicators represent the Global Goals for Oral Health 2020. One of the technical activities of the WHO Global Oral Health Program (GOHP) is to offer advice to nations on how to build policies for preventing and promoting dental and oral illnesses[7].
Improving the quality of life of children is one of the goals of the health development program. In this situation, the development of children's health is not discriminatory, and child health services are available to all children with special needs or disabilities, regardless of whether they are in special schools (SS), other institutions, or the community[8–10].
According to the 2012 Susenas (National socio-economic survey for Indonesia), 2.45 per cent of Indonesia's population has impairments [11]. Mental retardation is one group of people with disabilities. Individuals with mental impairment are referred to as having mental retardation (mental retardation). Mental retardation, according to the American Association of Mental Deficiency (AAMD), is defined as a significant divergence from general intellectual functioning that coexists with adaptive behaviour impairments and manifests during the formative period [12].
Indahwati, et al [13] compared the dental and oral hygiene of mentally disabled and deaf students in SS-B and SS-C Tomohon City. According to the findings, mentally disabled kids had lower oral and dental hygiene than deaf students. According to Martens L et al. [14], mentally impaired children's motor abilities at the age of 12 are lower than that of normal children, and mentally disabled children have difficulties holding and using a toothbrush. Rosmawati's [15] study demonstrates that children with special needs have poor dental and oral health with an average Decay Missing Filled-Teeth (DMF-T) score of three.
Because mentally retarded children endure physical and mental development delays, such as disruptions in sensorimotor coordination, children with special needs require particular health services, one of which is children with special needs for mental retardation [16–19]. According to an interview with the principal of the State Extraordinary School 2 in Jambi City, the students at the school have a joint tooth brushing program after recess directed by the teacher and use a conventional toothbrush. However, the prevalence of dental caries remains high [20].
Brushing the teeth prevents dental caries, and the toothbrush most usually used to remove plaque is a standard toothbrush. Traditional toothbrushes need motor coordination from users, but sensorimotor skills are limited in mentally disabled youngsters.
According to some authors, manual toothbrushing entails the application of much higher pressure than the use of power brushes. Powered toothbrushes appear to be helpful in improving the oral health of physically or mentally handicapped individuals because these devices require minimal hand motion and coordination skills. Some models are designed with each bristle rotating individually and are effective plaque removers [21,22].
Considering the benefits of an electric toothbrush, it can make it easier for mentally handicapped children to clean their teeth and mentally disabled children in SS Jambi City have never used an electric toothbrush, it is vital to investigate the usefulness of conventional and electric toothbrushes in them. This study aims to evaluate the effectiveness of using an electric toothbrushes, compared to conventional toothbrushes, in the reduction of dental plaque score.
METHODS
Study design
A monocentric pilot study, with pretest-posttest design, was carried out from February to July 2022 at State Special School 2 in Jambi City, Indonesia.
Sample size
The minimum sample size required for this study was calculated using the G*Power program, considering effect size of 0.82, α-value of 0.05, power of 0.80, and sample group ratio of 1 [23]. In public health research, the value of sample size strength is at least 80%, therefore, we choose an effect size of 82% (lowest).
Participants
Eligible subject were selected according to the following inclusion criteria: all children in SS Jambi, diagnosed with mild mental retardation [24], aged 10-16 years, Dental caries index ≥ 6.6, unkempt teeth, Dental plaque score 1, bracesless. Children with moderate and severe mental retardation who were unwilling and under ten years old, Dental caries index < 6.6, Dental plaque score > 1, kempt teeth, braces and were excluded. Overall, 20 children participated in the study and were split into Intervention (n=10) and Control groups (n=10) which were randomly defined.
Intervention
After enrollment, participants were randomly assigned into a control group (n=10), in which they used a conventional toothbrush, and in the intervention group (n=10), in which they used an electric toothbrush. In both groups, the dental plaque score was evaluated at baseline (T0) and after seven days (T1). On the day 7th (T1), all participants were advised to brush their teeth and not eat food for 30 minutes before the oral health examination was conducted. All participants were instructed to brush their teeth in the morning after getting up, lunch, and dinner using the same toothpaste for both study groups. The DMF-T index is an index to assess dental and oral health status in terms of permanent dental caries [25,26]. The DMF-T index is an assessment of the total number of teeth or surfaces that are Decayed/Carious (D), Missing (M), and Filling (F) for everyone. The severity of dental caries at the age of 12 years or older is categorized into five categories, including very low severity with a DMF-T value of 0.0 – 1.0. Then the low severity level with a DMF-T value of 1.2 -2.6. Moderate severity with a DMF-T value of 2.7 – 4.4. And a high severity level with a DMF-T value of 4.5 – 6.5, and a very high severity level with a DMF-T value of ≥ 6.6
Outcomes
Disclosing solution was used to carry out the procedure for measuring plaque scores. It works by putting a disclosing solution on the subject’s tooth surface and recording the findings. Dental and oral hygiene was assessed using PHP-M (Personal Hygiene Performance-Modified). The assessment begins by making imaginary lines on the teeth to form 5 imaginary lines. The lingual and labial surfaces of the teeth were examined. If a plaque was observed in one area, it was given a score of 1. Otherwise, a score of 0 or a sign was provided (-). Plaque assessment findings were calculated by summing each plaque on each tooth surface, resulting in a plaque score for each tooth ranging from 0-to 10. Plaque scores for all teeth can range from 0 to 60, with 0-20 indicating good criteria, 21-40 indicating moderate criteria, and 41-60 indicating poor criteria.
Ethical Consideration
In this study, parents of the children had given their consent to the study. Before carrying out data collection, the researcher first took care of ethical permission. The authors state that this study followed all ethical clearance processes and was approved by the health research ethics committee of Jambi University Faculty of Medicine and Health Sciences, with number: LB.02.06/2/04/2022.
Statistical methods
For categorical variables, data were presented as numbers or percentages. The mean, standard deviation (SD), or median with Interquartile Range are used to express continuous data (IQR). Before the statistical test was carried out, the data normality test was first carried out using Shapiro Wilk test.
The non-parametric test used was Wilxocon to assess pre vs post conventional groups, while the Mann Whitney test was used to assess pre vs pre both study groups. The non-parametric tests were used for non normal data. The Paired T-Test was employed in data analysis to see if there was a difference in mean plaque scores before and after using a traditional toothbrush versus an electric toothbrush. The difference in plaque scores before and after treatment between the conventional toothbrush group and the electric toothbrush group was investigated using the independent T-Test. All tests with a p-value (p) of less than 0.05 were deemed significant. The SPSS version 16.0 application was used for statistical analysis.
RESULTS
Participants characteristics
The general characteristics of children, as shown in Table 1:
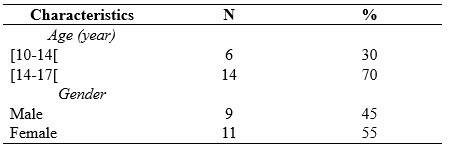
Table 1. Characteristics of childrens
The results of research on childrens with mental retardation SS Jambi City, as shown in Table 2:
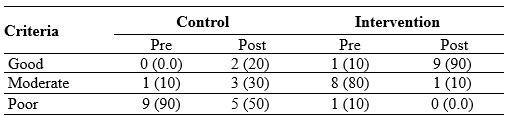
Table 2. Frequency Distribution of Plaque Score Criteria Based on PHP-M Index
Table 2 shows that before brushing their teeth, the criteria for plaque scores of children were one child (10%) with moderate criteria and nine children (90%) with poor criteria. After brushing their teeth, the criteria for plaque scores of children were two children (20%) with good criteria, three children (30%) with moderate criteria, and five children (50%) with poor criteria.
Before brushing their teeth with an electric toothbrush, the plaque score of children was eight children (80%) with moderate criteria, one child (10%) with good criteria, and one child (10%) with poor criteria. After brushing their teeth, the plaque score of nine children (90%) with good criteria and one child (10%) with moderate criteria.

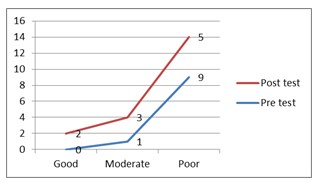
Figure 1. Plaque score criteria for control Figure 2. Plaque score criteria for intervention
group children group children
Because the sample size was less than 50 children, the Shapiro Wilk test was employed to determine the normality of the data. The sample size in this study was 20 children, as shown in Table 3:
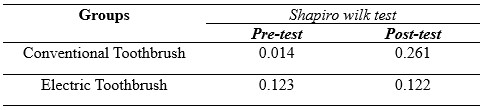
Table 3. Normality Test Results of Plaque Score Data for Children with Mental Requirements in SS Jambi City
The non-parametric test will be continued since the pre-test results in the conventional toothbrush group had an aberrant distribution of 0.014<0.05, and the post-test data were typically distributed at 0.261 > 0.05, as shown in table 3. In the meantime, the results in the electric toothbrush group were normally distributed, with a pre-test of 0.123 > 0.05 and a post-test of 0.122 > 0.05, respectively, followed by a parametric test.

Table 4. Test of the Effectiveness of Using Conventional Toothbrushes and Electric Toothbrush on Decreasing Plaque Scores in SS Jambi City
Table 4 shows that the mean score of plaque before brushing teeth is 52.30, whereas the mean score of children's plaque drops to 32.80 after brushing, indicating a 19.50 decrease in the mean value. The p-value for the paired data effectiveness test is < 0.009, indicating that using a conventional toothbrush to reduce plaque scores in mentally disabled children at SLBN 2 Jambi City is thriving. The mean score of plaque before cleaning teeth is 32.40, that the mean score of children's plaque falls to 14.50 after brushing, and that the mean value decreases by 17.90. The findings of the paired data effectiveness test show that the p-value is < 0.001, indicating that using an electric toothbrush to reduce plaque scores in mentally disabled children in SS Jambi City is beneficial.
The mean post-test value for the conventional toothbrush group is 32.80, while the electric toothbrush group is 14.50, with a P-Value of < 0.001. It indicates the difference in plaque score reduction effectiveness between conventional and electric toothbrushes in mentally disabled children.
The use of electric toothbrushes is more effective in reducing plaque scores in mentally retarded children at SS Jambi City, based on this description.
DISCUSSION
The current study is based on the theoretical basis of the physical condition of children with mental retardation. It has been known that children with mental disorders have mobility limitations, specifically in their extremities. This situation raises question marks about their ability to brush their teeth. Some studies have proven that mentally impaired children's motor abilities are lower than normal children, and mentally disabled children have difficulties holding and using a toothbrush. Children with special needs have poor dental and oral health with an average Decay Missing Filled-Teeth (DMF-T). So in this study, we evaluated the effectiveness of using an electric toothbrushes, compared to conventional toothbrushes, in the reduction of dental plaque score.
We reported that the use of conventional toothbrushes helped lower plaque scores in children with mental retardation in SS Jambi. These findings are in line with research conducted by Sitepu et al. [27] that using soft toothbrushes reduces plaque scores in mentally disabled children and a study conducted by Basith et al. [28] on 40 kids with Down syndrome in India. They observed manual or conventional toothbrushes to eliminate plaque and reduce gingivitis in children with Down syndrome for two months in each group.
In this study, it was also found that electric toothbrushes reduced the number of plaque scores in mentally disabled children in SS Jambi. Electric toothbrushes are effective in reducing OHI-S rates in children with Down syndrome, according to research conducted by Az Zahra et al. [29] and research conducted by Vandana et al. [30] on 30 people with mental problems who were observed for 45 days showed that brushing teeth with an electric toothbrush can reduce the number of mycobacteria in the oral cavity of mentally disabled children.
Plaque removal is the most critical activity for maintaining good teeth and oral health. The most popular tool for eliminating supra-gingival plaque is a toothbrush. However, most people do not clean their teeth correctly, and there is still a lot of plaque on the surface of their teeth [31].
Although electric toothbrushes are more expensive, because of the numerous designs and colors, they are thought to be more effective in raising the interest of mentally challenged youngsters in brushing their teeth. Electric toothbrushes are also good teeth cleaning equipment for preventing biofilm or plaque from forming on the surface of the teeth [32].
After brushing their teeth with an electronic toothbrush, the growing criteria for plaque scores in youngsters improve. This is due to the fact that the movement utilized in electric toothbrushes is better and more successful in reaching all parts of the mouth, as it is a systematic movement [33].
Mentally retarded children usually have difficulty in imitating the way of brushing their teeth that has been shown because their fine motor development is worse than normal children in general. Furthermore, mentally retarded children's eye and hand coordination is severely impaired. As a result, the child will have difficulties with fine motor movements, which will prevent the youngster from executing actions that demand concentration and complex hand movements [34]. Electric toothbrushes are more effective for intellectually impaired youngsters because of this. Because electric toothbrushes move automatically and children can feel the proper vibration to massage the gum and gingival area, they are a good choice for youngsters. As a result, using an electric toothbrush is more efficient and effective [29].
Although the results of this study have reported that electric toothbrushes are very suitable for use by children with mental retardation, the role of parents is highly expected. Parents or companions are required to take a more active role in encouraging mentally challenged youngsters to clean their teeth twice a day, in the morning after breakfast and at night before bed. We really hope that in the future the production of electric toothbrushes will be further improved at a price that can be affordable by all circles of society.
Based on the results of this study, we strongly recommend the use of an electric toothbrush, especially for students with mental retardation.
CONCLUSION
When compared to electric toothbrushes, electric toothbrushes are more effective in reducing plaque scores in mentally retarded children at SS Jambi City.
Study Limitations
One of the limitations of this study is the very small sample size (a pilot study), we collected data at only one center in Indonesia, which may limit the generalizability of our results to the larger population, so that in the future it is necessary to conduct similar studies in a larger population. Another limitation of the study was that the genders were not matched in the second group, which may have influenced the study results.
Authors’ contribution
All authors equally contributed to preparing this article.
Acknowledgement
We express our gratitude to the director Director of Health Polytechnic, Ministry of Health Jambi, Indonesia for its support for the implementation of this research
Funding
This research received funding from the Development and Empowerment of Human Resources in Public Health (BPPSDMK) Indonesia
Conflict Of Interest
The authors declare that there was no conflict of interest in this research.
REFERENCES
1. Van der Weijden GA, Timmerman MF, Nijboer A, Lie MA, Van der Velden U. A comparative study of electric toothbrushes for the effectiveness of plaque removal in relation to toothbrushing duration: Timerstudy. Journal of clinical periodontology. 1993;20(7):476–81.
2. Zahra AAA, Audrey NW, Ichyana DS, Saskianti T, Pradopo S, Nelwan SC, et al. Effectiveness of the Use of Manual and Electric Toothbrushes and the Effect of Educational Brushing Teeth with Video Animation on OHI-S Children with Down syndrome. Indonesian Journal of Dental Medicine. 2021;4(1):6–10.
3. WHO. Oral Health [Internet]. World Health Organization. 2018. Available from: https://www.who.int/news-room/fact-sheets/detail/oral-health
4. Govindaraju L, Gurunathan D. Effectiveness of Chewable Tooth Brush in Children-A Prospective Clinical Study. Journal of clinical and diagnostic research: JCDR. 2017;11(3):ZC31.
5. Deery C, Heanue M, Deacon S, Robinson PG, Walmsley AD, Worthington H, et al. The effectiveness of manual versus powered toothbrushes for dental health: a systematic review. Journal of Dentistry. 2004;32(3):197–211.
6. Davidovich E, Shafir S, Shay B, Zini A. Plaque removal by a powered toothbrush versus a manual toothbrush in children: A systematic review and meta-analysis. Pediatric Dentistry. 2020;42(4):280–7.
7. Kementerian Kesehatan Republik Indonesia. Pedoman Paket Dasar Pelayanan Kesehatan Gigi dan Mulut di Puskesmas. Jakarta; 2012.
8. Kementerian Kesehatan RI. Pedoman Pelayanan Kesehatan Anak di Sekolah Luar Biasa (SLB) Bagi Petugas Kesehatan. Jakarta; 2010.
9. Ganesh M, Shah S, Parikh D, Choudhary P, Bhaskar V. The effectiveness of a musical toothbrush for dental plaque removal: A comparative study. Journal of Indian Society of Pedodontics and Preventive Dentistry. 2012;30(2):139.
10. Aass AM, Gjermo P. Comparison of oral hygiene efficacy of one manual and two electric toothbrushes. Acta Odontologica Scandinavica. 2000;58(4):166–70.
11. Badan Pusat Statistik. SURVEI SOSIAL EKONOMI NASIONAL 2012 [Internet]. 2012. Available from: https://sirusa.bps.go.id/sirusa/index.php/kuesioner/202
12. Grossman HJ, Begab MJ. Classification in mental retardation. Washington, DC: Amer Assn on Intellectual & Devel; 1983.
13. Indahwati V, Mantik MFJ, Gunawan PN. Perbandingan Status Kebersihan Gigi dan Mulutpada Anak Berkebutuhan Khusus SLB-B dan SLB-C Kota Tomohon. e-GIGI. 2015;3(2).
14. Martens L, Marks L, Goffin G, Gizani S, Vinckier F, Declerck D. Oral hygiene in 12‐year‐old disabled children in Flanders, Belgium, related to manual dexterity. Community dentistry and oral epidemiology. 2000;28(1):73–80.
15. Rosmawati R, Surayah S. Status Kesehatan Gigi Dan Mulut Pada Anak Berkebutuhan Khusus Penyandang Cacat Fisik Di SLB Prof. Dr. Sri Soedewi Sofwan, SH JAMBI. JURNAL BAHANA KESEHATAN MASYARAKAT (BAHANA OF JOURNAL PUBLIC HEALTH). 2018;2(1).
16. Carina C, Panjaitan M, Anastasia I, Adhana A. Perbedaan efektivitas sikat gigi elektrik dengan sikat gigi manual dalam penurunan indeks plak pada anak-anak tunanetra. Prima Journal of Oral and Dental Sciences. 2020;3(2):33–8.
17. Pasyah F. Gambaran Kekerasan Bulu Sikat Gigi Terhadap Penurunan Debris Indeks Pada Siswa/i Kelas VIII-1 SMPN 3 Perbaungan Kec. Perbaungan kab. Serdang Bedagai. Poltekkes Kemenkes Medan; 2019.
18. Ichyana D. Efektifitas Sikat Gigi Manual Dan Sikat Gigi Elektrik Terhadap Skor Ohi-S Anak Down Syndrome [Internet]. Universitas Airlangga; 2019. Available from: https://repository.unair.ac.id/93229/
19. Hasanuddin SH. Efektivitas Pendidikan Kesehatan Menggunakan Media Video Dengan Media Cerita Bergambar Terhadap Keterampilan Menggosok Gigi Anak Usia Prasekolah. Universitas Islam Negeri Alauddin Makassar; 2018.
20. Department of Health Jambi Province. Profile Health Department of Health Jambi Province [Internet]. Jambi, Indonesia; 2020. Available from: http://dinkes.jambiprov.go.id/file/informasi_publik/MTYxNTE2NDQyOA_Wkt1615164428_XtLnBkZg.pdf
21. Vorwerk L, Ghassemi A, Hooper W, Patel V, Milleman J, Milleman K. Comparative plaque removal efficacy of a new powered toothbrush and a manual toothbrush. J clin dent. 2016;27(3):76–9.
22. García‐Carrillo A, Jover A, Plá R, Martorell A, Sota C, Gómez‐Moreno G, et al. Manual versus sonic powered toothbrushing in patients with intellectual disability: a cluster‐randomized clinical trial. Journal of Clinical Periodontology. 2016;43(8):684–93.
23. Faul F, Erdfelder E, Lang A-G, Buchner A. G* Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behavior research methods. 2007;39(2):175–91.
24. Association AP. American Psychiatric Association: Diagnosti c and Statistical Manual of Mental Disorders, Arlington. 2013.
25. Jaime RA, Carvalho TS, Bonini GC, Imparato JCP, Mendes FM. Oral health education program on dental caries incidence for school children. Journal of clinical pediatric dentistry. 2015;39(3):277–83.
26. Hariyani N, Soebekti RH, Setyowati D, Bramantoro T, Palupi LS, Putriana E. Factors influencing the severity of dental caries among Indonesian children with autism spectrum disorder–a pilot study. Clinical, cosmetic and investigational dentistry. 2019;11:227.
27. Sitepu DT, Edi IS, Hidayati S. Penurunan Indeks Plak Gigi Ditinjau Dari Penggunaan Sikat Gigi Hard, Medium, Dan Soft. Jurnal Ilmiah Keperawatan Gigi. 2021;2(2):1–6.
28. Basith A, Monica, Biir. Comparative Evaluation of Effectiveness of Manual and Electric Tooth Brush (Oral - B) in Elimination of Dental Plaque and Gingivitis. 2019;4(March):45–50.
29. Az Zahra AA, Audrey NW, Ichyana DS, Saskianti T, Pradopo S, Nelwan SC, et al. Effectiveness of the Use of Manual and Electric Toothbrushes and the Effect of Educational Brushing Teeth with Video Animation on OHI-S Children with Down syndrome. Indonesian Journal of Dental Medicine. 2021;4(1):6.
30. Vandana KL, Tatuskar PV, Valavalka NN. A Comparative Evaluation Of Manual And Powereed Brushing On Oral Health And Microbial Of Mentallu Challenged Induvidual. 2020;(May):113–8.
31. Bahammam S, Chen CY, Ishida Y, Hayashi A, Ikeda Y, Ishii H, et al. Electric and manual oral hygiene routines affect plaque index score differently. International Journal of Environmental Research and Public Health. 2021;18(24).
32. Silva AM, Miranda LFB, Araújo ASM, Prado Júnior RR, Mendes RF. Electric toothbrush for biofilm control in individuals with Down syndrome: A crossover randomized clinical trial. Brazilian Oral Research. 2020;34(June).
33. Rahman eddy, Ilmi MB. Perbedaan Sikat Gigi Biasa Dengan Sikat Gigi Elektrik Terhadap Penurunan Debris Indeks Pada Murid Kelas V Madrasah Diniyah islamiyah Kindaung Banjarmasin. Jurnal Kesehatan Indonesia. 2019;9(3):122–8.
34. Hakim AR. Pengaruh Motorik Kasar Anak Tunagrahita Terhadap Motorik Halus. Jurnal Ilmiah PENJAS. 2016;2(2):33–49.
![]() This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
EFFECTIVENESS OF E-BOOK APPLICATION MODEL UTERINE ATONY MANAGEMENT GUIDE AND POCKETBOOK IN IMPROVING MIDWIFE KNOWLEDGE AND SKILLS IN BASIC CARE: PRE-POST STUDY
Titik Hindriati1*, Nuraidah1, Rosmaria1, Diniyati1
1. Department of Midwifery, Health Polytechnic of Jambi, Indonesia
* Corresponding author: Titik Hindriati, Jl. Prof DR GA Siwabessy No.42, BuluranKenali, Kec. Telanaipura, Kota Jambi, Jambi 36122 Department of Midwifery, Health Polytechnic of Jambi, Indonesia. Orcid :https://orcid.org/0000-0001-7604-8068. Email: titikpoltekkes@gmail.com
Abstract
Background: Midwives are one of the main health workers at the frontline of health development to accelerate the decline in Maternal Mortality Rate (MMR) and Infant Mortality Rate (IMR). Therefore, competent and skilled midwives are needed in carrying out clinical procedures, especially in handling emergency cases of postpartum hemorrhage, with critical analysis skills. This study aims to determine the effectiveness of e-book application model uterine hypotonia management guide and pocket book in improving midwife knowledge and skills in basic care.
Method: The research design used was pre-post study, which was carried out in February-April 2021. The population and sample in this study were all midwives who provided delivery assistance at the Jambi City Health Center, totaling 64 respondents. Data analysis used the Wilcoxon and Mann-Whitney tests.
Results: In each intervention group, all variables, including knowledge and skills, are increased in both groups defined. The results showed that the educational media application of guidelines and pocketbooks on postnatal emergency management increased knowledge and skills.
Conclusion: The two study groups had a significant effect on increasing the knowledge and skills of midwives in handling postnatal emergencies due to uterine atony.
Keywords: Midwive, Emergency handling, learning media, pocket books, applications
Introduction
The role of health workers will determine the success of development programs in the health sector [1–3]. Midwives are one of the main health workers spearheading health development to accelerate the decline in Maternal Mortality Rate (MMR) and Infant Mortality Rate (IMR) [4]. For this reason, it is necessary to have midwives who have the ability and skills in clinical procedures, especially in proper management in handling emergency cases of postpartum mothers due to uterine atony with critical analytical skills [5,6].
According to the World Health Organization (WHO), the maternal mortality rate in the world in 2015 was 216 per 100,000 live births, with the highest number in developing countries, namely 239 per 100,000 live births, or 20 times higher than the maternal mortality rate in developed countries, which were only 12 per 100,000 live births [7]. Nearly 75% of all maternal deaths are caused by postpartum hemorrhage, infection (usually after delivery), high blood pressure during pregnancy (pre-eclampsia and eclampsia), and unsafe abortion [8].
Based on the 2012 Indonesian Demographic and Health Survey (IDHS), the maternal mortality rate in Indonesia is 359 per 100,000 live births. It shows a downward trend to 117 per 100,000 live births in 2017, while the Maternal Mortality Rate (MMR) target is according to the Sustainable Development Goals (SDGs) of 70 per 100,000 live births in 2030 [9]. The Maternal Mortality Rate (MMR) in Jambi city in 2018 was 18.86/100 live births, and in 2019 it increased to 46.15/100 live births, although this data is still below the national Maternal Mortality Rate (MMR). Medical factors that are direct causes of maternal death are bleeding by 42%, pregnancy poisoning (eclampsia) 13%, miscarriage (abortion) 11%, infection 10%, delayed labor / prolonged labor 9% and other causes 15% [10].
Obstetric emergencies are life-threatening health conditions that occur during pregnancy or during and after labor and birth [11,12]. The government's effort to reduce Maternal Mortality Rate (MMR) and Infant Mortality Rate (IMR) is to provide quality basic maternal and neonatal health services, namely Basic Emergency Obstetrics and Neonatal Services (PONED) at the Puskesmas. However, the maternal and neonatal emergency case services at the PONED Health Center have not been running according to the targeted expectations [13].
The high maternal and infant mortality rate can be caused by the lack of skilled midwives as health service providers, starting from pregnancy to delivery. To improve the knowledge and skills of midwives as service providers, maximum innovation is needed, including the provision of a pocketbook for handling emergency midwifery. This guideline is compiled in the form of a pocketbook equipped with an algorithm to facilitate health workers in handling emergency obstetric cases quickly. The second option can be using an android application that contains an e-book of obstetric emergency case materials, especially in the treatment of uterine atony [14,15].
In Interactive Multimedia, the stimulus appears by presenting exercises related to the material so that the midwife can respond by typing or pressing a button and then facilitated by feedback [16–19]. The existence of an attractive program display can lead to motivation so that aspects of learning readiness will also appear [20–23]. Multimedia applications can assess midwifery/psychomotor skills in basic services to detect emergency cases. Midwives as spearheads for maternal and infant health are good in theory and practice, especially for handling emergency cases. A midwife must provide quality midwifery services to prevent complications and maternal death due to complications [15,24].
The current study aims to evaluate the effectiveness of e-book application model uterine atony management guide and pocket book in improving midwife knowledge and skills in basic care.
Methods
Design
The design used is development, where this method is used to produce certain products and test the effectiveness of these products. Product testing is done by using pre-post Study.
Participants
The research respondents were 64 midwives (divided into 32 people in group 1 and 32 people in group 2) at PutriAyu Health Center and PakuanBaru Health Center who were randomly selected with the inclusion criteria of midwives who provide delivery services and have a working period of more than one year.
Intervention
The variables of this study are the knowledge and skills of the midwife who will be measured before and after the educational intervention using the application of postpartum emergency guidance due to uterine atony and pocketbooks.
The knowledge questionnaire has objective criteria of good or low, uses a Guttman scale, and consists of 15 questions with a rating range of 0-15. The variable of midwifery skill in this study was defined as the ability of the midwife to practice the procedures for handling emergency obstetrics, in this case uterine atony.
The skill questionnaire has good or poor objective criteria, uses a Guttman scale, and consists of 15 question items with an assessment range of 0-15.
The Guttman scale was used in this study because the variables used were nominal scales. The Guttman scale has an important characteristic, which is that it is a cumulative scale and measures only one dimension of a multi-dimensional variable, so that this scale has an undimensional nature. The data obtained are in the form of interval data or dichotomy ratios (two alternatives) [25].
The group 1 received an intervention providing education on using an emergency postpartum guide application due to uterine atony for seven days. The group 2 will receive an education pocketbook on handling emergency postpartum due to uterine atony for seven days. On the first day before giving the intervention, researchers measured the level of knowledge using a questionnaire in both study groups, as well as the skills of midwives were measured using a questionnaire consisting of the midwife's ability to prepare tools, prepare patients, perform actions according to procedures, evaluate patient responses to actions that have been taken. midwife, and the ability of the midwife to document the actions that have been taken.
The first stage is the research starting from determining the team, determining the development schedule, selecting and determining the scope, structure, and order of the material, determining multimedia specifications, and making storyboards. The second stage is the development stage consisting of expert validation, practitioner validation, and the implementation and evaluation stages. The third stage is the Effectiveness Test.
Blinding
In this study, 2 enumerators were used to collect research data. The previous enumerators did not know the participants because they were students who had been trained by the researcher before collecting data. The enumerators involved in this study were final year students who were about to complete their midwifery diploma, and were tasked with helping researchers collect data in the field by distributing questionnaires, however, the assessment of participants' skills was assessed by the researcher.
Statistical methods
Data were presented as numbers or percentages for categorical variables. Continuous data are expressed as the mean ± standard deviation (SD), or median with Interquartile Range (IQR). The data obtained were analyzed by univariate and bivariate, from the normality test (Kolmogorov Smirnov) obtained abnormal data so that the analysis used the Wilcoxon and Mann Whitney test. All tests with p-value (p)<0.05 were considered significant. Statistical analysis was performed using the SPSS version 16.0 application.
Ethical Consideration
Registered prospective respondents have signed an informed consent and there is no incentive to participate in the study and the anonymity of participants is guaranteed. Before carrying out data collection, the researcher first took care of ethical permission.
The authors state that this study followed all ethical clearance processes and was approved by the health research ethics committee of Ministry of Health Polytechnic of Jambi, Indonesia, and registration number: LB.02.06/2/167/2021.
Results
The results of the univariate analysis, which aims to determine the frequency of each variable studied, can be seen in the following table:
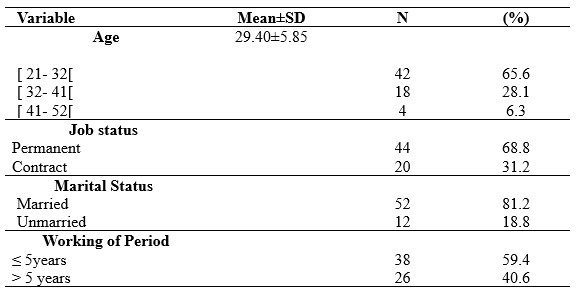
Table 1. Demographic data of participants
Table 1 shows that the dominant respondents aged 21-32 year are 41 people (65.6%), have employment status as permanent employees as many as 44 people (68.8%), 52 people are married (81.2%), and have a working period of ≤5 years as many as 38 people (59.4%).
Based on the normality test, the statistical test used in this study is non-parametric, with the results as shown in the following table:
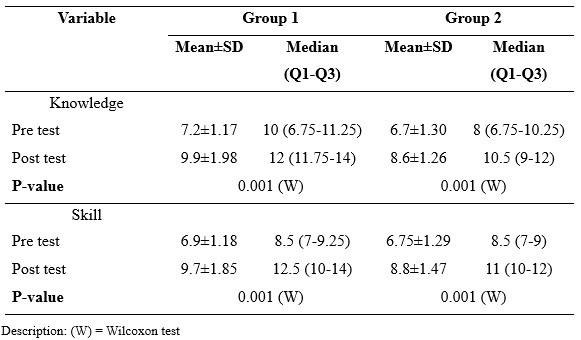
Table 2. Differences in mean values and Wilcoxon test results
Table 2 shows that in each intervention group, group 1 vs group 2, all variables, both knowledge and skills, have increased. In group 1 (e-book emergency guidance application) the median value of knowledge before intervention was 10 with a mean value of 7.2 while in group 2 (pocket book) it had a median value of 8 with a mean value of 6.7. After the intervention, group 1 (e-book emergency guidance application) had a median value of knowledge of 12 with a mean value of 9.9, while group 2 (pocket book) had a median value of 10.5 with a mean value of 8.6.
On the skill variable, in group 1 (e-book emergency guidance application) the median value before intervention was 8.5 with a mean value of 6.9 while in group 2 (pocket book) it had a median value of 8.5 with a mean value of 6.75. After the intervention, group 1 (emergency guide application e-book) had a median skill score of 12.5 with a mean value of 9.7, while group 2 (pocket book) had a median value of 11 with a mean value of 8.8.
The differences in knowledge and skills between the two study groups are presented in table 3.
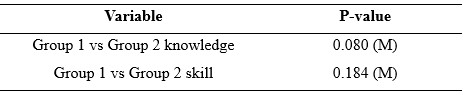
Table 3. Result of Mann Whitney test
Table 3 shows that the results of the Mann Whitney test prove that there is no difference between the two study groups in improving the knowledge and skills of midwives, in the sense that both groups (group 1 and group 2) are equally effective in improving the knowledge and skills of midwives in handling emergency obstetric cases.
Discussion
The information obtained by previous respondents strongly influences a person's level of knowledge. When the pre-test was carried out, the results obtained showed that the midwife had less knowledge before being given an android application for handling postnatal emergencies and a pocketbook. After the intervention, the respondent's knowledge increased by 71% in the group that received Android educational media. In contrast, the group that received pocketbooks in the group 2 also increased even though it was only 57%.
The Mobile Application, Education for handling postnatal emergencies, provides menus of information on handling postnatal emergencies, especially animated videos so that participants pay more attention to and master the techniques of handling postnatal emergencies.
Educational media serves to mobilize as many senses as possible to an object to facilitate the perception of the recipient of information [26]. The media will help clarify the information conveyed because it can be more interesting and interactive and overcome the limitations of space, time, and human senses. So that the information conveyed can be clearer and easier to understand according to the purpose for which it will be used [27]. Educational materials can be packaged according to the characteristics of each media used [28]. Today's cellphones not only function as a means of telecommunications but have switched functions to become androids that can do many things [29]. Mobile phones with functions like this can be known as smartphones. Smartphones can assist in medical activities, such as establishing diagnosis and therapy. From various forms of information technology and telecommunications, mobile phones are considered a suitable medium for increasing knowledge in the current developing era. The use of this smartphone is more effective than the module without the application [30,31].
Wahyuni's research [32] on the effect of smartphone applications on a person's knowledge and skills in stimulating the growth and development of toddlers shows an increase in knowledge and skills. Therefore, providing education through interesting media based on Android will make it easier for someone to stimulate independently. In addition to these researchers, other researchers state an effect of using printed media in the form of pocketbooks on increasing the knowledge of postpartum mothers. The study states that print media is the most frequently used and easy-to-reach media, for example, pocketbooks [33]. Pocket books occupy an important position in providing education because they provide clear and practical messages that allow readers to read at any time without the need for the internet to access them and are equipped with images that match the material, making it easier to understand the material [34].
Studies among various healthcare professionals reported mixed results regarding the usefulness of the e-learning, mobile learning and technology-enhanced learning. A Cochrane systematic review conducted by Vaona et al in [35] compared traditional learning with e-learning and reported that e-learning may make little or no difference in health professionals’ behaviours, skills or knowledge. A study conducted by Subhash et al, [36] among medical students reported that smartphones can be effectively used for learning. A study conducted by Snashall et al, [15] among medical students reported that medical apps can be used as an adjunct in medical education, though the evidence remains limited. Furthermore, data analysis showed that the respondent's skills increased after being given an intervention using an application for handling postnatal emergencies 43%. After being given education through a pocketbook in the group 2, the increase was lower than 21.4%. The results of the Mann-Whitney test in this study showed that there was no difference in knowledge and skills between the two study groups regarding postnatal emergency management who received the android application and the group who received a pocketbook. It shows that any media used can improve knowledge and skills because the function of the media is to help facilitate learning for students, provide a more real experience, attract greater attention from respondents because it is not boring, and all senses of respondents can be activated, attract more attention and interest of respondents in learning [37]. The most plausible reason is that the skill of midwives is higher in the group that received application media education compared to pocketbooks because the application media can be studied anytime and anywhere and displays interesting features and videos of emergency obstetric emergencies, especially uterine atony, so that midwives able to understand and remember strongly the material seen and heard [38].
Conclusion
The application model of pocket books and e-books for the management of uterine atony has been proven to be effective in improving the knowledge and skills of midwives in primary care.
Study Limitations
The limitation of this study is that this research involves a small number of samples so that this type of research is a preliminary study, and only involves a certain location, namely 1 area, so it cannot compare the results of this study to the character of the community in different locations. In the future it is necessary to conduct research on a large regional scale and the number of samples in a very large size.
Acknowledgement
We would like to express our gratitude to the director of the Midwifery Department of Jambi health polytechnic who has supported this research.
Funding statement
This research did not receive any specific grant from funding agencies in the public, commercial, or not for profit sectors.
Competing interests statement
There are no competing interests for this study.
Authors’ contribution
TH and NU were responsible for the study conception and design; RO performed the data collection; TH and DN performed the data analysis; NU, and RO were responsible for the drafting of the manuscript; TH and NU made critical revisions to the paper for important intellectual content.
References
1. Ani M, Azizah N, Rahmawati VE, Mardiah A, Febriyeni F, Astuti ED, et al. Pengantar Kebidanan. Yayasan Kita Menulis; 2021.
2. Liu A, Sullivan S, Khan M, Sachs S, Singh P. Community health workers in global health: scale and scalability. Mount Sinai Journal of Medicine: A Journal of Translational and Personalized Medicine. 2011;78(3):419–35.
3. Franco LM, Bennett S, Kanfer R. Health sector reform and public sector health worker motivation: a conceptual framework. Social science & medicine. 2002;54(8):1255–66.
4. Erawati AD, Rinayati R, Wahyuning S. Midwife roles to decline maternal mortality rate. International Journal of Public Health Science. 2020;9(1):29–33.
5. Scholes J, Endacott R, Biro M, Bulle B, Cooper S, Miles M, et al. Clinical decision-making: midwifery students’ recognition of, and response to, post partum haemorrhage in the simulation environment. BMC Pregnancy and Childbirth. 2012;12(1):1–12.
6. Maslovitz S, Barkai G, Lessing JB, Ziv A, Many A. Recurrent obstetric management mistakes identified by simulation. Obstetrics & Gynecology. 2007;109(6):1295–300.
7. Organization WH. Trends in maternal mortality: 1990-2015: estimates from WHO, UNICEF, UNFPA, World Bank Group and the United Nations Population Division. World Health Organization; 2015.
8. Organization WH. Trends in maternal mortality 2000 to 2017: estimates by WHO, UNICEF, UNFPA, World Bank Group and the United Nations Population Division. World Health Organization; 2019.
9. Kementerian Kesehatan RI. Laporan Riskesdas 2018. Laporan Nasional Riskesdas 2018. 2018.
10. BPS Provinsi Jambi. Jambi dalam angka [Internet]. 2019. Available from: https://jambi.bps.go.id/
11. Teela KC, Mullany LC, Lee CI, Poh E, Paw P, Masenior N, et al. Community-based delivery of maternal care in conflict-affected areas of eastern Burma: perspectives from lay maternal health workers. Social Science & Medicine. 2009;68(7):1332–40.
12. Susilawati E, Johari A, Marzal J, Anggereini E. Effects of Multimedia E-Books and Augmented Reality on Knowledge and Skills of Health Sciences Students: A Systematic Review. Journal of Client-Centered Nursing Care. 2022;8(2):99–110.
13. Rayfitra MR, Achmad F, Yuniarti Y. Perbandingan Tingkat Pengetahuan Bidan sebelum dan setelah Pemberian Edukasi mengenai Manajemen Kegawatdaruratan Obstetri di Puskesmas Mampu Poned Kota Bandung. 2020;
14. Sadagheyani HE, Tatari F, Raoufian H, Salimi P, Gazerani A. The effect of multimedia-based education on students’ anger management skill. Educacion Medica. 2021;22(3):149–55.
15. Snashall E, Hindocha S. The use of smartphone applications in medical education. Open Medicine Journal. 2016;3(1).
16. Tirtaningrum DA, Sriatmi A, Suryoputro A. Analisis Response Time Penatalaksanaan Rujukan Kegawatdaruratan Obstetri Ibu Hamil. Media Kesehatan Masyarakat Indonesia Universitas Hasanuddin. 2018;14(2):139–46.
17. Mustafa AR, Ramadany S, Sanusi Y, Made S, Stang S, Syarif S. Learning Media Applications for Toddler Midwifery Care about Android-Based Fine Motor Development in Improving Midwifery Students Skills. International Journal of Health and Medical Sciences. 2020;3(1):130–5.
18. Kardina I, Ramadany S, Sanusi Y, Made S, Stang S, Syarif S. Children’s Midwifery Learning Media Application About Android-based Rough Motor Development in Improving Midwifery Student Skills. International Journal of Health and Medical Sciences. 3(1):146–52.
19. Gebze DA, Perwati S. Improving problem-solving ability in physics through android-based mobile learning application. In: Journal of Physics: Conference Series. IOP Publishing; 2020. p. 12022.
20. Alwy Al-beity F, Pembe AB, Kwezi HA, Massawe SN, Hanson C, Baker U. “We do what we can do to save a woman” health workers’ perceptions of health facility readiness for management of postpartum haemorrhage. Global Health Action. 2020;13(1):1707403.
21. Ventola CL. Mobile devices and apps for health care professionals: uses and benefits. Pharmacy and Therapeutics. 2014;39(5):356.
22. Prasetyo H, Kristiyanto A, Doewes M. The Development of Android-Based Mobile Learning Media in Healthy Lifestyle Teaching Materials for Senior High School Students. International Journal of Multicultural and Multireligious Understanding. 2019;6(2):188.
23. Jesse GR. Smartphone and app usage among college students: Using smartphones effectively for social and educational needs. In: Proceedings of the EDSIG Conference. 2015.
24. Hasnah H, Triratnawati A. Penelusuran Kasus-Kasus Kegawatdaruratan Obstetri yang Berakibat Kematian Maternal: Studi kasus di RSUD Purworejo, Jawa Tengah. Makara J Heal Res. 2010;7(2):38–48.
25. Sugiyono. Metode Penelitian Kuantitatif, Kualitatif dan R&D. Bandung: PT Alfabet; 2016.
26. Gamar MM, Tati ADR. Utilization of ICT-Based Learning Media in Local History Learning. In: Journal of Physics: Conference Series. IOP Publishing; 2021. p. 12079.
27. Rohaeti EE, Bernard M, Primandhika RB. Developing interactive learning media for school level mathematics through open-ended approach aided by visual basic application for excel. Journal on Mathematics Education. 2019;10(1):59–68.
28. Puspitarini YD, Hanif M. Using Learning Media to Increase Learning Motivation in Elementary School. Anatolian Journal of Education. 2019;4(2):53–60.
29. Safitri I, Pasaribu R, Simamora SS, Lubis K. The effectiveness of android application as a student aid tool in understanding physics project assignments. Jurnal Pendidikan IPA Indonesia. 2019;8(4):512–20.
30. Hafis M, Meliasari R. Analisis Penggunaan Aplikasi pada Smartphone sebagai Media Pembelajaran. JIIP-Jurnal Ilmiah Ilmu Pendidikan. 2021;4(8):740–7.
31. Barnett J, Harricharan M, Fletcher D, Gilchrist B, Coughlan J. myPace: an integrative health platform for supporting weight loss and maintenance behaviors. IEEE journal of biomedical and health informatics. 2014;19(1):109–16.
32. Wahyuni T, Syswianti D, Hidayat DR. Uji Diagnostik Aplikasi Mother Cares (Moca) Untuk Deteksi Dini Risiko Penyimpangan Perkembangan Balita. 2019;
33. Ahmady A, Ashari AE. Efektifitas buku saku dalam meningkatkan pengetahuan pendamping ibu nifas di Kabupaten Mamuju. Jurnal Kesehatan Manarang. 2018;4(2):122–7.
34. Azadirachta FL, Sumarmi S. Pendidikan Gizi menggunakan media buku saku meningkatkan pengetahuan dan praktik konsumsi sayur dan buah pada siswa sekolah dasar. Media Gizi Indonesia. 2017;12(2):107–15.
35. Vaona A, Banzi R, Kwag KH, Rigon G, Cereda D, Pecoraro V, et al. E‐learning for health professionals. Cochrane Database of Systematic Reviews. 2018;(1).
36. Subhash TS, Bapurao TS. Perception of medical students for utility of mobile technology use in medical education. International Journal of Medicine and Public Health. 2015;5(4).
37. Stegeman CA, Zydney J. Effectiveness of multimedia instruction in health professions education compared to traditional instruction. American Dental Hygienists’ Association. 2010;84(3):130–6.
38. Ahmar H, Budi P, Ahmad M, Mustary M, Hutagaol IO. The Influence of Problem Based Learning Model Based on Midwifery First Stage of Childbirth Care Module in Improving Learning Quality. International Journal of Psychosocial Rehabilitation. 2020;24(2).
![]() This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.