Rosyati Pastuty1*, Elita Vasra1, Gustiana2
1Department of Midwifery, Health Polytechnic of Palembang, Indonesia
2Department of Midwifery, Health Polytechnic of Aceh, Indonesia
* Corresponding author:
Rosyati Pastuty, Jl. Inspektur Yazid, Sekip Jaya, Kec. Kemuning, Kota Palembang, Sumatera Selatan 30114, Indonesia, Orcid: https://orcid.org/0000-0003-0804-2291
Email: rrosyatipastuty@gmail.com
Cite this article
ABSTRACT
Background: Postpartum depression is a life-threatening mental health disorder and occurs in 10-15% of women. “Globally, the incidence of postpartum depression reaches 10-15%. There are few reports in countries such as Malta, Malaysia, Austria, Denmark and Singapore. While in other countries such as Brazil, South Africa, Taiwan, Korea, Italy, and Costa Rica, symptoms of postpartum depression are reported to be quite high”. “Based the criteria of the Diagnostic and Statistical Manual of Mental Disorders, fourth edition (DSM-IV) and the Edinburgh Postnatal Depression Scale (EPDS). Audio hypnotherapy, which is the provision of positive suggestions delivered through MP3, is a method to reduce the level of postpartum depression. This study aims to determine the effectiveness of audio hypnotherapy in reducing postpartum depression during the new normal.
Materials and Methods: This quasi-experimental study used a pretest-posttest design involving 60 postpartum mothers with a history of normal delivery at 2 Midwife’s clinics in Palembang City and 1 Midwife’s clinic in Aceh. Postpartum depression levels were assessed using the Edinburgh Postnatal Depression Scale (EPDS). Data analysis used Paired Samples Test to determine differences in postpartum depression levels before and after listening to Hypnotherapy audio.
Results: There was a decrease in postpartum mothers’ depression level after listening to hypnotherapy audio for ± 2 weeks. Depression incidence before giving audio hypnotherapy has a mean value = 11.15, while after giving audio hypnotherapy, it increases to 8.90, with P-value <0.05.
Conclusion: Audio hypnotherapy therapy has proven to be effective in reducing the incidence of depression in postpartum mothers.
Keywords: Audio Hypnotherapy, depression, Post-partum mother
INTRODUCTION
Antepartum Depression (APD) and Postpartum Depression (PPD), are disorders characterized by mood swings during pregnancy and after childbirth, which have a negative impact on the physical and mental health of mothers and children [1,2]. Melville et al [3] in their study reported that prevalence rates ranged from 4.8% to 18.4% for mild depression, and from 5.1% to 12.7% for severe depression.
Globally, the incidence of postpartum depression reaches 10-15%. There are few reports in countries such as Malta, Malaysia, Austria, Denmark and Singapore. While in other countries such as Brazil, South Africa, Taiwan, Korea, Italy, and Costa Rica, symptoms of postpartum depression are reported to be quite high. A study in India, involving 359 primiparous mothers, reported an 11% incidence of postpartum depression [4,5].
Approximately 70% of new mothers have mild depressive symptoms which generally peak in the 2 to 5 days after delivery. These symptoms usually begin to subside spontaneously within 2 weeks, but if not detected immediately and treatment is delayed, it can develop into postpartum depression [6].
Most pregnant women who face the birth process experience feelings of anxiety, even depression. Factors causing postpartum depression consist of biological factors, characteristics and background of the mother. Levels of the hormones estrogen (estradiol and estriol), progesterone, prolactin, cortisol which increase and decrease too quickly or too slowly are biological factors that cause postpartum depression [7]. The greater the decrease in estrogen and progesterone levels after childbirth, the greater the tendency for a woman to experience depression in the first 10 days after giving birth [8]. The estrogen and progesterone exert a suppressive effect on the activity of the monoamine oxidase enzyme. This enzyme can inactivate both noradrenaline and serotonin, which play a role in mood and depression. Estradiol and estriol are the active forms of estrogen formed by the placenta. Estradiol functions to strengthen the function of neurotransmitters by increasing the synthesis and reducing the breakdown of serotonin. Therefore, theoretically the decrease in estradiol levels due to childbirth plays a role in causing postpartum depression [2,6,9,10]. Biological causative factors are difficult and rarely measured in terms of maternal depressive symptoms [11]. Other factors that influence maternal depressive symptoms described in several studies include interpersonal variables (neural disorders, poor life experiences), social variables (marital dissatisfaction, lack of social support), and clinical variables related to pregnancy (risk in current pregnancy, problems with previous pregnancy) [12].
Antepartum Depression (APD) and Postpartum Depression (PPD) together are called perinatal depression. Various diagnostic criteria with major depression occur during pregnancy or within 4 weeks after delivery [13]. Based on previous research, women with a history of high levels of stress may be at increased risk for perinatal depression [14,15].
Based on the criteria of the Diagnostic and Statistical Manual of Mental Disorders, fourth edition (DSM-IV) [16] and the Edinburgh Postnatal Depression Scale (EPDS) [17], mothers with symptoms of postpartum depression are defined by several major symptoms, including a depressed mood or decreased pleasure. These symptoms include impaired appetite, physical agitation or psychomotor slowing, weakness, decreased concentration, and suicidal ideation. Mothers also often feel insomnia even though the baby has fallen asleep. These symptoms must be present throughout the day and last for at least two weeks [3,9].
Women who experienced depression during pregnancy had seven times the risk of developing postpartum depression than women who did not have symptoms of antenatal depression. An observational study of 78 depressed women in the first trimester of pregnancy found that postpartum depression did not occur in all women who received treatment, both psychotherapy and pharmacotherapy, compared with 92% of women who were depressed and did not receive treatment. Supportive and psychological interventions are more effective when performed after delivery than when they are initiated during pregnancy [18].
Mothers with postpartum depression need extensive treatment with both pharmacological and non-pharmacological therapies. Through non-pharmacological therapy, such as psychological therapy, mothers can find the right way to deal with the symptoms of depression, deal with disorders that arise, or think positively when the situation is stressful [19,20].
There are several non-pharmacological techniques to relieve anxiety such as pregnancy exercise, distraction, biofed back, yoga, acupressure, aroma therapy, steam therapy and hypnosis. Hypnosis is a natural method used to relieve fear, panic, tension, and other pressures. Hypnosis is done by making direct contact with the subconscious, by giving suggestions in order to build various positive emotional conditions [21,22].
Khoirunnisa et al., [21] used a narrative review method to explore types of interventions for postpartum depression and found that several interventions such as music therapy [22], postpartum exercise [23], aerobic exercise [24], laughter therapy [25], cognitive behavior Therapy [26], Effleurage Massage Therapy [27], Acupressure Therapy [28], are effective in reducing postpartum depression.
Based on some of these studies provides an illustration that not many hypnotherapy interventions have been thoroughly scrutinized considering the impact of depression on postpartum mothers; we are therefore interested in analyzing the effectiveness of Audio Hypnotherapy in reducing postpartum depression, especially in the new normal period in 2021.
MATERIALS AND METHODS
Study design
This type of research is a quasi-experimental design using a pretest – posttest design.
Study Population
This research was conducted in January–December 2021 at the Teti Herawati Midwife clinic, Meli Rosita Palembang City and the Mariana Aceh Besar Indonesia, midwife clinic involving 60 participants who were randomly selected and had met the sample inclusion requirements such as being healthy after giving birth, having never received hypnotherapy audio, mentally healthy, and has a cell phone. Demographic characteristics of postpartum women collected in this study were age, education, occupation and parity.
Sample size
The number of samples involved was 60 participants who were randomly selected from the population. Calculating the number of samples is determined using the Slovin formula [29], where from 71 people in the population, d = 0.05, the number of samples is 60.
Instruments
The incidence of postpartum depression will be measured using a standardized questionnaire developed by Cox et al., the Edinburgh Postnatal Depression Scale (EPDS). This questionnaire consists of 10 questions; each has four responses with a Likert scale from 0 – 3. The maximum value is 30, and the lowest is 0. It is called experiencing depression if the score is ≥ 10. EPDS has a sensitivity of 80% and a specificity of 84.4 % [23]. Meanwhile, EPDS in Indonesian has a sensitivity of 86% and a specificity of 78% [24].
The scale shows how the mother felt during the previous week. In doubtful cases it may be useful to repeat the tool after 2 weeks. This scale is not used to detect mothers with anxiety neuroses, phobias or personality disorders [25].
Interventions
Audio hypnotherapy is giving positive suggestions or orders to the subconscious mind to change thoughts, feelings, and behaviors for the better through MP3 voice recordings sent via WhatsApp groups. In this study, hypnotherapy was carried out by selfhypnosis using standardized hypnotherapy audio recording media. The selfhypnosis method with standard hypnotherapy audio recording media for 30 minutes in stages; pre-induction (introduction, explaining goals, and building trust), filling in the informed consent sheet, explaining the use of tools, induction (the relaxation process brings the patient to the subconscious mind with Hanung techniques), deepening (trance), suggestion (giving messages with the aim of certain), and termination (slowly awakening the patient).
Before the intervention, all respondents filled out the EPDS questionnaire to determine the risk of postpartum depression. Then, respondents listened to Hypnotherapy audio for ± 30 minutes every night before going to bed for 2 weeks. After undergoing an audio Hypnotherapy intervention for 2 weeks, all respondents filled out the EPDS questionnaire to determine the risk of postpartum depression.
Ethical Consideration
Before the respondents filled out the questionnaire, the researchers first explained their informed consent about the scope of the research. Then after the prospective respondent agreed, the respondent signed an agreement to become a respondent. All data about respondents will be kept confidential and only used for research purposes.No economic incentives were offered or provided for participation in this study. The study protocol matched the Declaration of Helsinki ethical guidelines for clinical studies. This research has been approved by the Health Research Ethics Commission of the Health Polytechnic of the Palembang Ministry of Health with the number 1250/KEPK/Adm2/VIII/2021.
Statistical analysis
The statistical analysis was performed by SPSS software version 16. 0. Data are presented as number and percentage for categorical variables, and continuous data expressed as the mean ± standard deviation (SD) unless otherwise specified. The first statistical test, the McNemar test, aims to analyze differences in depression status before and after the intervention using categorical data. Before conducting the different tests, first, we tested the normality of the data using the Kolmogorov Smirnov and found the data was not normally distributed. The research data were analyzed using the Wilcoxon test. This test was performed on same data sample in two different periods where the data were not normally distributed. It is considered significant if the research variable has a P-value <0.05.
RESULTS
The characteristics of respondents in this study include age, education, employment status and parity. The following is the frequency distribution of the respondents’ characteristics in this study:
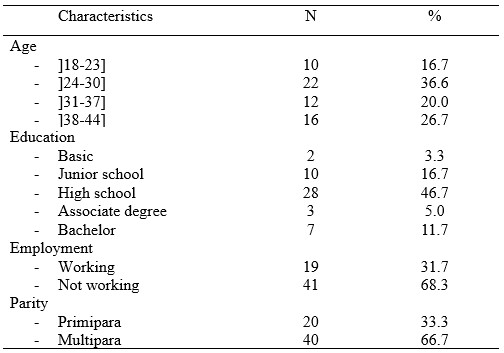
Table 1. Frequency Distribution of Respondents Characteristics
Table 1 shows that most of the mothers aged 24-30 years were 22 mothers (36.6%). The respondents’ education is mostly High school as many as 28 respondents (46.7%). Most respondents did not work as many as 41 (68.3%), and multipara as many as 40 respondents (66.7%).
The results of statistical tests and the distribution of depression status before and after the intervention are presented in table 2.

Table 2. Distribution of depression incidence before and after interventions
Table 2 shows that before the intervention there were 26 depressed respondents then after the intervention there were 12 respondents. Based on the McNemar test, a p-value <0.05 was obtained, meaning that there were differences in depression status before and after the intervention.
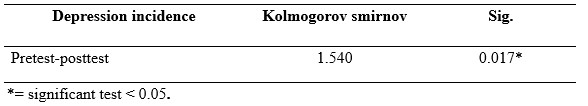
Table 3. Normality Test Results of depression incidence pretest and posttest audio hypnotherapy
Table 3 shows that the results of the Kolmogorov Smirnov statistical test obtained a P-value <0.05, so the normality is rejected. The depression incidence data at the pre-post test audio hypnotherapy not normally distributed. Therefore, the statistical difference test was tested using Wilcoxon.
The results of the audio hypnotherapy pre-post test statistics and the mean depression incidence values are presented in table 4.
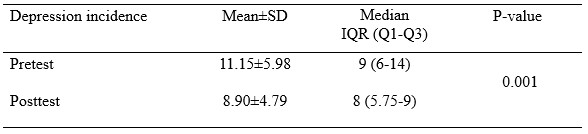
Table 4. Average Depression Incidence Pretest and Posttest Audio Hipnoterapy
Table 4 shows that depression incidence before giving audio hypnotherapy has a mean value = 11.15, while after giving audio hypnotherapy, it decreases to 8.90, with P-value <0.05.
DISCUSSION
Most pregnant women who face the birth process experience feelings of anxiety, even depression. Factors causing postpartum depression consist of biological factors, characteristics and background of the mother. Levels of the hormones estrogen (estradiol and estriol), progesterone, prolactin, cortisol which increase and decrease too quickly or too slowly are biological factors that cause postpartum depression [7]. The greater the decrease in estrogen and progesterone levels after childbirth, the greater the tendency for a woman to experience depression in the first 10 days after giving birth [8].
The estrogen and progesterone exert a suppressive effect on the activity of the monoamine oxidase enzyme. This enzyme can inactivate both noradrenaline and serotonin, which play a role in mood and depression. Estradiol and estriol are the active forms of estrogen formed by the placenta. Estradiol functions to strengthen the function of neurotransmitters by increasing the synthesis and reducing the breakdown of serotonin. Therefore, theoretically the decrease in estradiol levels due to childbirth plays a role in causing postpartum depression [9,10]. Biological causative factors are difficult and rarely measured in terms of maternal depressive symptoms [11]. Other factors that influence maternal depressive symptoms described in several studies include interpersonal variables (neural disorders, poor life experiences), social variables (marital dissatisfaction, lack of social support), and clinical variables related to pregnancy (risk in current pregnancy, problems with previous pregnancy) [12].
The results of the current study showed a decrease in the level of postpartum depression before and after listening to audio hypnotherapy. This means that listening to audio hypnotherapy can reduce the level of postpartum depression, where postpartum mothers feel comfortable, calm and relaxed after listening to audio hypnotherapy, although not every night or every day. Audio hypnotherapy is a hypnosis therapy, where respondents get positive suggestions through MP3 audio sent via cellphone. Hypnotherapy or clinical hypnosis is an integrative mind-body technique using hypnotic suggestions for specific therapeutic purposes that are identified jointly by the hypnotherapist and client [26].
The results of the Paired Samples Test analysis showed a difference in the average level of depression before and after listening to audio hypnotherapy with a significance value of P-value 0.001. For this reason, it can be concluded that audio hypnotherapy can reduce the level of depression in pregnant women, especially during the Covid-19 pandemic. The average decrease in anxiety levels of pregnant women before and after listening to audio hypnotherapy is 2.6.
Hypnotherapy has long been believed to reduce postnatal pain by giving suggestions in the form of positive commands [27]. Through the process of hypnosis, the patient is brought into a relaxed state in order to calm the autonomic nervous system and induce positive emotions that affect the patient’s coping mechanisms for pain perception [28]. It stimulates positive emotions for more norepinephrine production, reduces ROS production, increases tryptophan levels, and stimulates the ventricular nucleus which functions to secrete oxytocin in the dopamine system, and subsequently plays a role in pain modulation [6,29]. A deeper hypnotic state (trance) can help activate the endorphins and encephalin system that can inhibit the production of substance P, a pain sensitizing agent in the dorsal horn of the spinal cord [30].
Some respondents experienced persistent depression despite the intervention. This condition was caused by the respondent’s disobedience in carrying out audio hypnotherapy. Most of the respondents underwent audio hypnotherapy at night before going to bed. Some respondents listen when they feel uncomfortable or when they have free time. Some respondents do not run audio hypnotherapy every night.
In the future, audio hypnotherapy in order to reduce the level of depression in postpartum mothers can be an important alternative therapy besides the provision of medical drugs.
CONCLUSION
Before the intervention, there were 26 depressed respondents. Then after the intervention, there were 12 respondents. Audio hypnotherapy has been proven effective in reducing depression in postpartum mothers.
LIMITATIONS
The assessment of the level of depression in the current study is still subjective. Future research can use more real/objective measurements or combine subjective and objective scales. Furthermore, the research location only involves 3 places, therefore it cannot compare the results of similar studies in different populations.
The future research must be carried out involving several regions. This study also showed the possibility that socio-demographic factors’ influence could not be controlled because the respondent’s character was not matched.
FUNDING STATEMENT
This research did not receive any specific grant from funding agencies in the public, commercial, or not for profit sectors.
COMPETING INTERESTS STATEMENT
There are no competing interests for this study.
AUTHORS’ CONTRIBUTION
All authors equally contributed to preparing this article.
REFERENCES
- Field T. Prenatal depression effects on early development: a review. Infant behavior and development. 2011;34(1):1–14.
- Woods SM, Melville JL, Guo Y, Fan M-Y, Gavin A. Psychosocial stress during pregnancy. American journal of obstetrics and gynecology. 2010;202(1):61-e1.
- Melville JL, Gavin A, Guo Y, Fan M-Y, Katon WJ. Depressive disorders during pregnancy: prevalence and risk factors in a large urban sample. Obstetrics and gynecology. 2010;116(5):1064.
- Shorey S, Chee CYI, Ng ED, Chan YH, San Tam WW, Chong YS. Prevalence and incidence of postpartum depression among healthy mothers: a systematic review and meta-analysis. Journal of psychiatric research. 2018;104:235–48.
- Wang Z, Liu J, Shuai H, Cai Z, Fu X, Liu Y, et al. Mapping global prevalence of depression among postpartum women. Translational psychiatry. 2021;11(1):1–13.
- Varga K, Kekecs Z. Oxitocina y cortisol en interacción hipnótica. International Journal of Clinical and Experimental Hypnosis. 2014;62(1):111–28.
- Rizkiani I, Respati SH, Sulistyowati S, Budihastuti UR, Prasetya H. The Effect of Hypnotherapy on Serum Cortisol Levels in Post-Cesarean Patients. Journal of Maternal and Child Health. 2021;1(2549–0257):258–66.
- Yuniasti RD, Upoyo AS, Taufik A. The Effect of Hypnotherapy on Pain Intensity in Postoperative Patients: A Systematic Review. IJNP (Indonesian Journal of Nursing Practices). 2021;5(2):112–22.
- Lara MA, Navarrete L, Nieto L. Prenatal predictors of postpartum depression and postpartum depressive symptoms in Mexican mothers: a longitudinal study. Archives of women’s mental health. 2016;19(5):825–34.
- Campbell SB, Cohn JF. Prevalence and correlates of postpartum depression in first-time mothers. Journal of abnormal psychology. 1991;100(4):594.
- Mahandaru AH, Respati SH, Sulistyowati S, Laqif A, Prasetya H. The Effect of Hypnotherapy on Postpartum Pain and Depression in Women with Post Caesarean Delivery. Indonesian Journal of Medicine. 2021;6(2):194–205.
- Millizia A, Syafridah A. The Effect of Murottal Al-Quran Therapy on Pain in Post Cesarean Surgery Patients at Abby Mother and Child Hospital, Lhokseumawe City. Arkus. 2022;8(1):198–202.
- Dørheim SK, Bondevik GT, Eberhard-Gran M, Bjorvatn B. Sleep and depression in postpartum women: a population-based study. Sleep. 2009;32(7):847–55.
- Gjerdingen DK, Yawn BP. Postpartum depression screening: importance, methods, barriers, and recommendations for practice. The Journal of the American Board of Family Medicine. 2007;20(3):280–8.
- Eberhard-Gran M, Tambs K, Opjordsmoen S, Skrondal A, Eskild A. A comparison of anxiety and depressive symptomatology in postpartum and non-postpartum mothers. Social psychiatry and psychiatric epidemiology. 2003;38(10):551–6.
- Carter MJ. Diagnostic and statistical manual of mental disorders. Therapeutic recreation journal. 2014;48(3):275.
- Cox JL, Chapman G, Murray D, Jones P. Validation of the Edinburgh Postnatal Depression Scale (EPDS) in non-postnatal women. Journal of affective disorders. 1996;39(3):185–9.
- Stewart DE, Vigod S. Postpartum depression. New England Journal of Medicine. 2016;375(22):2177–86.
- Seymour-Smith M, Cruwys T, Haslam SA, Brodribb W. Loss of group memberships predicts depression in postpartum mothers. Social psychiatry and psychiatric epidemiology. 2017;52(2):201–10.
- Patel M, Bailey RK, Jabeen S, Ali S, Barker NC, Osiezagha K. Postpartum depression: a review. Journal of health care for the poor and underserved. 2012;23(2):534–42.
- Leger J, Letourneau N. New mothers and postpartum depression: a narrative review of peer support intervention studies. Health & social care in the community. 2015;23(4):337–48.
- Howell EA, Bodnar-Deren S, Balbierz A, Loudon H, Mora PA, Zlotnick C, et al. An intervention to reduce postpartum depressive symptoms: a randomized controlled trial. Archives of women’s mental health. 2014;17(1):57–63.
- Santos IS, Matijasevich A, Tavares BF, Barros AJD, Botelho IP, Lapolli C, et al. Validation of the Edinburgh Postnatal Depression Scale (EPDS) in a sample of mothers from the 2004 Pelotas Birth Cohort Study. Cadernos de saude publica. 2007;23:2577–88.
- Nasri Z, Wibowo A, Biostatistika D, Ghozali EW, Jiwa K. Faktor determinan depresi postpartum di kabupaten Lombok Timur. Pusat Penelitian dan Pengembangan Humaniora dan Manajemen Kesehatan; 2018.
- Levis B, Negeri Z, Sun Y, Benedetti A, Thombs BD. Accuracy of the Edinburgh Postnatal Depression Scale (EPDS) for screening to detect major depression among pregnant and postpartum women: systematic review and meta-analysis of individual participant data. bmj. 2020;371.
- Mubarokah RI, Prasetya H, Respati SH. The Effectiveness of Hypnotherapy to Reduce Anxiety in Pre-Caesarean Section Women. Journal of Maternal and Child Health. 2020;5(1):12–8.
- Kendrick C, Sliwinski J, Yu Y, Johnson A, Fisher W, Kekecs Z, et al. Hypnosis for acute procedural pain: a critical review. International Journal of Clinical and Experimental Hypnosis. 2016;64(1):75–115.
- Alarcon R. Synopsis of psychiatry: Behavioral sciences and clinical psychiatry. American Journal of Psychiatry. 1992;149(7):972–4.
- Sanders VM. The beta2-adrenergic receptor on T and B lymphocytes: do we understand it yet? Brain, behavior, and immunity. 2012;26(2):195–200.
- Price, Wilson A. Patofisiologi: Konsep Klinis Proses-proses Penyakit (Pathophysiology Clinical Concepts of Disease Processes), Buku I. Penerbit Buku Kedokteran EGC; 1995.
![]() This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.

