Venditti Riccardo1, Marti Flavio2*, Latina Roberto3, Mitello Lucia2, Romanelli Antonio1,
Pucci Antonello1, Mauro Lucia4, Campagna Giuseppe5 and Marucci Anna Rita2
1.Emergency Department Acceptance and Clinical Area, San Camillo-Forlanini Hospital, Rome
2.Department of Health Professions, San Camillo-Forlanini Hospital, Rome
3.PROMISE Department, University of Palermo, Palermo
4.Department of Surgical Sciences, San Camillo-Forlanini Hospital, Rome
5.Department of Medical-Surgical Sciences and Translational Medicine, “La Sapienza” University of Rome, Rome
* Corresponding Author: Flavio Marti. Department of Health Professions, Educational Director Postgraduate Degree in Nursing and Midwifery Sciences, Sapienza University of Rome, San Camillo Forlanini Hospital, C.ne Gianicolense 87, 00159 Rome (Italy). E-mail: flavio.marti@uniroma1.it
Cite this article
ABSTRACT
Introduction: To date, Emergency Department overcrowding represents one of the most important problems regarding the organisation of emergency healthcare. See and Treat was devised in England around the 1980s to provide an effective solution to the overcrowding issue. The Emergency Nurse Practitioner indicates a faster pathway in selected patients with certain characteristics. This model translates into a reduction in waiting times while maintaining the same quality of care.
Aim: To evaluate the potential benefits for patients of the implementation of the See and Treat model within the Emergency Department.
Materials and Methods: Using the GIPSE system, all Emergency Department entries from 2019 have been selected. Minor codes in the triage phase have been considered, as well as those potentially falling within the See and Treat protocol. Each included case has been associated to a See and Treat diagnosis. The waiting time and the time spent in the Emergency Department were derived from the data collected.
Results: 9.41% of the sample is eligible for the See and Treat method, with an average waiting time of one hour and peaks of almost 4 hours for white codes. The application of the See and Treat model to the population covered by our study would reduce the waiting times at the Emergency Department by 6.99%, reduce the simultaneous presence of users on the Emergency Department by 8.88% and reduce the stay for other minor codes by 4.38%.
Discussion: The percentage of patients treatable in the See and Treat system (11%) is in line with the Tuscany trial but statistically lower than the international context (from 63% to 90%). The results obtained from this study showed the significant impact that the See and Treat model could have on reducing overcrowding, positively affecting both users and staff.
Keywords: See and Treat; Emergency Department; overcrowding; advanced nursing skills.
INTRODUCTION
Overcrowding of the Emergency Department (ED) is currently one of the most important problems related to the organisation of emergency health services [1]. In the last decade, the decrease in the number of public and private hospital facilities [2], the growth of the population, the increase in frail patients [3,4] and the population that is not included in the health registry [5], the lack of knowledge of alternative services and the citizen’s belief that they will find a quick solution to a real or perceived problem in the ER [6] have had negative repercussions both on waiting and intervention times, and on the ability of the emergency system to provide adequate solutions to users. All this has burdened the National Health System in terms of quality and efficiency of services [7] also due to a reduction in the number of beds in the ordinary departments and lack of investment in the national network [8].
See and Treat was devised in England in the 1980s to provide an effective response to overcrowding [2]. The figure in charge of this role is the Emergency Nurse Practitioner, who in addition to establishing the usual priorities, indicates a faster professional pathway where patients selected for minor health problems are assessed and treated immediately [9]. The nursing staff operates independently on the basis of protocols that include the possibility of requesting specific tests and prescriptions for drugs, according to current legislation [10]. Studies in the literature show how the introduction of this figure reduces waiting times and overcrowding of the ER [1,11] while guaranteeing the same quality of care [12]. The Emergency Nurse Practitioner is present on a large scale in Northern Europe where nurses with advanced skills play a central role in the See and Treat model, with direct responsibility for the procedures carried out according to certain pre-established protocols [9,13].
In Italy, the See and Treat model has been applied in the Tuscany Region, [14] which, since 2010, has decided to engage in an experimentation project to carry out a profound organisational renewal of emergency departments; this experimentation has resulted in an improvement in the efficiency of ERs, has optimised the management of less critical cases, has reduced waiting times, has improved staff morale, reducing the aggressiveness of users and using nursing and medical resources more appropriately [15,16]. To date, Tuscany represents the only region in which a See and Treat model has been implemented in the safe treatment and discharge of users who access the ER for minor problems, thanks to a theoretical-practical training course for a total of 180 hours (organisational, operational and relational sections) together with work experience in the emergency room of at least 3 years [16].
Objective of the study
The objective of this study is to evaluate the potential benefits for patients accessing the ED of San Camillo-Forlanini Hospital, Rome, in the event of implementation by the Lazio Region of the See and Treat model.
MATERIALS AND METHODS
Sampling and Eligibility
In this paper, with the authorisation of the Health Management of the San Camillo-Forlanini Hospital in Rome, all the accesses to the Emergency Department during the year 2019 considered as minor codes in the triage phase and that potentially fell within the protocols defined by the Tuscany Region for See and Treat [14] were selected, initially by colour code (in force in 2019) and subsequently stratified according a triage statement by operators trained for this activity. Men and women over the age of 16, registered between 1 January 2019 and 31 December 2019, were included. Patients with minor codes (white and green codes) and who had the following items coded in the GIPSE (Emergency Department Information Management) system as their main triage issue were included: trauma or burns; other symptoms and disorders; dyspnoea; intoxication; urological symptoms and disorders; abdominal pain; other nervous system symptoms; allergic reaction; acute neurological syndrome; rhythm disorder; dermatological syndromes or disorders; non-traumatic haemorrhage; arterial hypertension; ENT syndromes and disorders; psychomotor agitation; chest pain and ophthalmological symptoms or disorders. Patients waiting for a visit who absconded from the ED due to waiting were also included as they contributed to the overcrowding figure. Patients with major codes (Red and Yellow) were excluded. Some problems defined in Tuscany Region Resolution [14], which did not congruently adhere to the admission procedures for patients of the San Camillo-Forlanini Hospital Emergency Department, such as paediatric and gynaecological patients, which belong to specific and separate pathways, were excluded.
Tools
The cases under study were identified by means of the GIPSE programme and subsequently collected in a spreadsheet; the division was made in chronological order, by work shift (morning, afternoon and night) using the inclusion and exclusion criteria described above. Each case included was associated with a See and Treat Diagnosis. Information such as age, gender, nationality, triage problem, colour code, date and time of admission, date and time of chart opening, date and time of discharge, access mode, day of the week, discharge to home or outpatient clinic or patient absent on call, triage statement and discharge medical diagnosis were coded. By comparing the admission, history-taking and discharge times, two further parameters were derived from those in our possession: waiting time and length of stay in the emergency department (data not present in GIPSE). The same methodology was subsequently applied to all ineligible patients in the See and Treat pathway to assess for differences.
Ethical Considerations
The study was authorised on 10 March 2021 by the Medical Directorate of San Camillo – Forlanini Hospital. No formal approval by the Local Ethics Committee was required for this study. All data were collected in aggregate form, and the researchers acted in accordance with the ethical considerations of the Declaration of Helsinki.
Statistical Analysis
Data on continuous variables (age, waiting time and time spent in the department) are presented in mean ± SD (Standard Deviation) or median (Q1: 25th centile – Q3: 75th centile); while categorical variables are presented as absolute frequency (n) and percentages (%).
The associations between categorical variables were evaluated through the c2 test; while the difference between two proportions was tested by the z test between two proportions.
The normality/symmetry of the continuous variables (age, waiting time and time spent in the department) compared to the groups (white vs. green, weekdays vs. holidays, females vs. males, Italians vs. foreigners, age classes: ≤48 vs. >48 years) was tested with the Shapiro-Wilk test, the Quantile-Quantile chart control and the verification of the presence of asymmetry and kurtosis.
The comparison between the above-mentioned groups and the continuous variables was tested using the Mann-Whitney test (absence of normality/symmetry); while the Kruskal-Wallis test (absence of normality of the residuals) was used to compare the days of the week and the work shift with respect to the continuous variables (age, waiting time and time spent in the department), the subsequent post-hoc analysis was performed using the Games-Howell method (due to absence of homoschedasticity).
All analyses were performed using SAS v.9.4 and JMP PRO v. 17 software (Institute Inc., Cary, NC, USA). A p-value < 0.05 was considered statistically significant.
RESULTS
The period under study was between 01/01/2019 and 31/12/2019; from the analysis of 29019 ED files divided into three shifts (morning, afternoon and night), 2731 patients eligible for See and Treat were selected, equal to 9.41% of the sample. Table 1 summarises the general data of patients eligible for See and Treat and those in the emergency department.
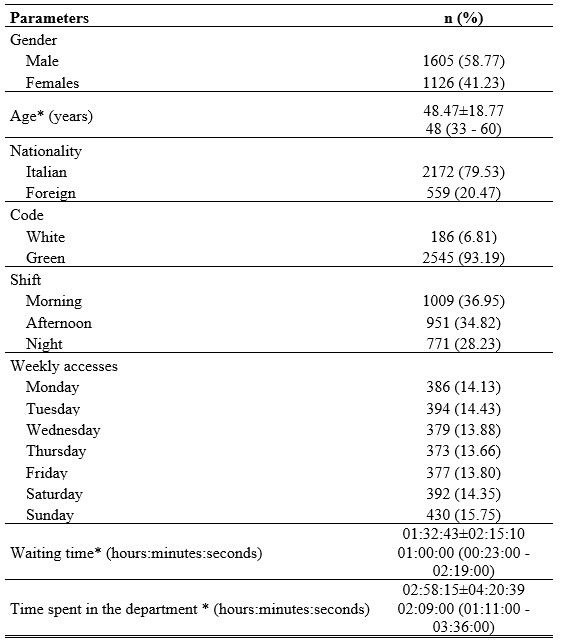
*data presented both as mean±SD and as median (Q1: 25th centile – Q3: 75th centile)
Table 1. Socio-demographic and emergency department characteristics
Analysis by colour code shows that 93.2% (n=2545) of patients were assigned a green code, while the rest were assigned a white code, without differences in the assignment of the colour code between males and females (c2 test, p=0.57) and between age and colour code (Mann-Whitney test, p=0.70); Users assigned a White code waited a median time of 01hr48’:30” more than the green codes (Mann-Whitney test, p<0.0001) and spent 01hr:24’:00” longer in the emergency department than the green codes (Mann-Whitney test, p<0.0001), as shown in table 2.
The majority of users were male at 58.8% (n=1605), the median age of patients was 48 years (Q1: 33 – Q3: 60 years), while the mean was 48.47±18.77 years. The median age of females was 49 years (Q1: 35 – Q3: 62 years), while the mean was 49.93±19.11 years. The median age of males was 47 years (Q1: 32 – Q3: 59), while the mean was 47.45±18.46 years (comparison Females vs. Males: Mann-Whitney test, p=0.001), with a more representative age group in the under-48 age group (52.18%) compared to those older than 48 years (47.82%) (z-test for two proportions, p=0.001).
Gender is associated with age group with a cut-off of 48 years (£48 years – Female/Male: 555 (38.95)/870 (61.05) vs. >48 years – Female/Male: 571 (43.72)/735 (56.28), c2 test, p=0.01). The waiting time after triage before the compilation of the medical history is not affected by either age group or gender (Mann-Whitney test, p=0.71 and p=0.055, respectively).
Gender does not affect the time spent in the emergency department (Mann-Whitney test, p=0.99), while there is an increase in the median time spent in the ED in patients over 48 years of 12 minutes (Mann-Whitney test, p=0.001), a data item highlighted in table 2.
79.5% of users were Italian while 20.5% of the sample came from other countries. Foreign nationality (table 2) affects waiting time, increasing it by a median of 27 minutes (Mann-Whitney test, p<0.0001) and time spent in the ED is increased by a median of 26 minutes (Mann-Whitney test, p<0.0001).
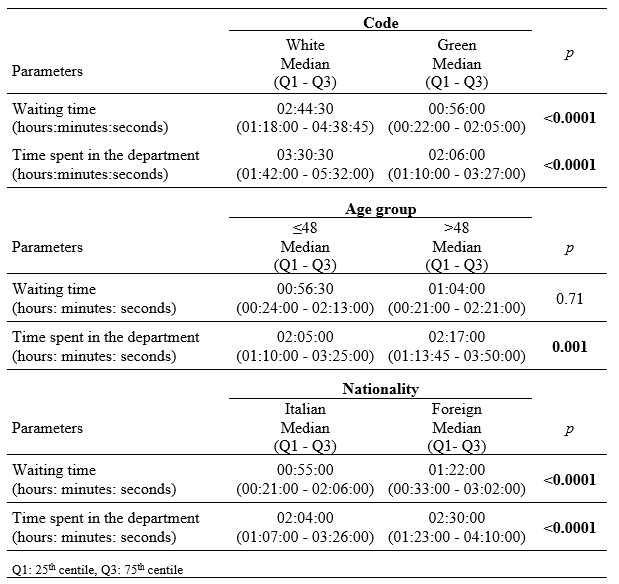
Table 2. Difference of waiting time and time spent in the department with respect to code, age group and nationality.
Accesses during the different days of the week were homogeneous except for a peak of influx on Sundays (Figure 1); however, no differences were found between access on weekdays versus holidays with gender (c2 test , p=0.94), age (Mann-Whitney test, p=0.80), waiting time (Mann-Whitney test, p=0.38) and time spent in the ED (Mann-Whitney test, p=0.10). Accesses in the various months of the year were uniform except for the month of January where there was a greater influx equal to 10.9% of the total.
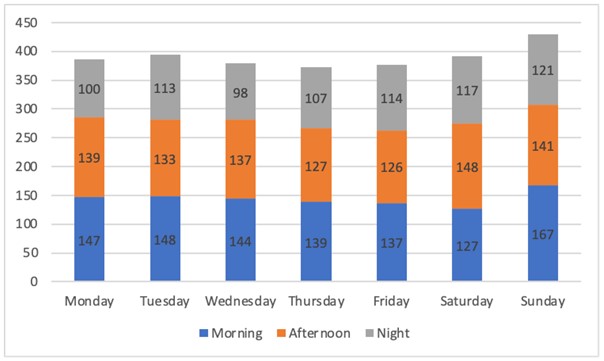
Figure 1. Accesses by day of the week and by shift
The analysis of accesses conducted with respect to work shifts (morning: 07:00 – 13:30, afternoon 13:30 – 19:50, night 19:50 – 07:00) showed a greater influx in the morning shift (36.9%) followed by the afternoon shift (34.8%) while the remaining 28.2% of the patients included came in during the night shift (c2 test, p=0.02) (Figure 1).
The post-hoc analysis (table 3) shows that the median age of patients tends to be higher in the morning shift compared to the afternoon shift (Kruskal-Wallis test and Games-Howell test, p<0.0001) and the night shift (Games-Howell test, p<0.0001). The median waiting time is 22 minutes longer in the morning shift than in the afternoon shift (Kruskal-Wallis test and Games-Howell test, p<0.0001) and 25 minutes longer than in the night shift (Kruskal-Wallis test and Games-Howell test, p<0.0001). The median time spent in the ED is 12 minutes shorter in the morning shift compared to the afternoon shift (Kruskal-Wallis test and Games-Howell test, p=0.001) and 8 minutes longer in the afternoon shift compared to the night shift (Kruskal-Wallis test and Games-Howell test, p=0.003).

Table 3. Differences between the variables indicated and the shift
By dividing patients by the categories defined by the model proposed by the Tuscany region [10], 57.7% of the sample came to the ED for trauma-related problems and 12% for musculoskeletal problems; small wounds, manageable through the See and Treat model were detected in 27.8% of cases. 81.1% of the patients completed the course of treatment while the rate of leaving the ED without receiving any treatment was found to be 16.2%. Among these users, about one in four (23.5%) had been assigned a white code. Of the selected patients, 18.5% did not need an estimation of days of illness, while 64% of them had a prognosis of 1 to 7 days; 36.4% of the sample were scheduled for a follow-up appointment in outpatient facilities. Excluding from our study population the patients eligible for See and Treat (thus creating a parallel pathway for 9.41% of the patients attending the ED) would have led to an average reduction in waiting times at the ED of 6.99%; the simultaneous presence of users in the ED would have decreased on average from 84.14 to 76.5 with a decrease of 8.88%. By freeing up resources, it would have been possible to provide each patient with a minor code, not included in the See and Treat pathway, with 19 minutes more of hospital care, thus achieving a reduction in the length of stay in the ED for minor codes of 4.38%.
DISCUSSION
The objective of this study was to evaluate the potential benefits for patients attending the ED of the San Camillo-Forlanini Hospital in Rome if the See and Treat model had been implemented by the Lazio Region. The results obtained showed that the percentage of patients treatable through the See and Treat regimen in our study (9.4%) is in line with that of the Tuscany trial where 11% of the patients in the sample fell into this category [16]. However, these data are not in line with the international literature, which shows that the use of the See and Treat model increases the percentage of patients seen from 63% to 90% [1]. This difference could be attributed to the fact that, in Italy, the figure of the Emergency Nurse Practitioner is not recognised [17], consequently the nurse specialised in first aid interventions, thus defined by the Tuscany region after participation in the pre-established training course to provide care in the See and Treat model [14] has less professional autonomy and can treat a limited number of issues [18,19]. In the study presented, the frequency of green codes is significantly higher (93.2%) than that of white codes, which by definition are considered inappropriate in an emergency department [20]. This figure is consistent with that of the 2010 Nati study, which described the management of white and green codes in the Emergency Department, by general practitioners, which reported 88.9% of green codes compared to 11.1% of white codes [21]. Of the patients selected, a considerable portion, 20.5%, was of foreign origin, a figure greater than the results of other studies carried out in Italy where the number of accesses to the ED by foreign citizens is 13% [22]; they waited longer than Italians both in terms of admission to the EDand their stay there. This figure can be linked to the difficulty of accessing health services for foreigners, who come to the ED to solve their health problems [21]. The mean age of the sample (48.5 years) was found to be in line with the study of Nati et al. where the age of the selected patients was 48.3 years [21]; patients over 48 years of age had a longer stay in the ED, probably due to comorbidities, which, among other things, can exclude (as per protocol) some of them from the See and Treat pathway (52.18% of patients under 48 years of age and 47.82% of patients over this age); this conclusion has not emerged in other studies, however. The Tuscan model includes a See and Treat clinic operating 7 days a week from 8 a.m. to 8 p.m. [14]. Our study showed that there is a uniformity of accesses in different months and on different days of the week. These data differ from the study performed by Fiorentini et al. in 2013 where the “Monday effect” and a general greater number of inappropriate accesses coinciding with the summer months were highlighted [23]. Fundamental to the organisation of this pathway is the data on patient accesses in the various shifts; the data that emerged (morning shift 36.9%, afternoon shift 34.8% and night shift 28.2%) is comparable to that of the study carried out by Fiorentini et al. where the distribution by time bracket of patients with minor codes was uniform, with peaks in the morning hours and a gradual reduction in accesses in the remaining part of the day [23]. The greater influx in the morning hours generates an overcrowding of the ED in the afternoon, which is reduced in the night shift as a result of fewer admissions. 57.7% of the patients in our study went to the ED for trauma-type problems (minor contusions of the limbs, uncomplicated hand and foot trauma, wounds, abrasions, superficial fingertip avulsion, insect bites and removal of stitches), while in the Tuscany trial the results showed that patients with these problems accounted for 70% of the sample analysed; specifically, the most frequent “See and Treat diagnosis” in our research was “wounds” with 27.8%, followed by “trauma of the fingers and toes” with 14.3%. The number of wounds appears to be higher than that of the study conducted by Righi in 2020, where patients with wounds accounted for only 18.2% [24]. Finally, the use of See and Treat would reduce the mean waiting times of the general user for minor codes by 6.99% and the time spent in the ED by 4.38%. The data from the Tuscany region show reductions of 46.4% in waiting times and 22.2% in the time spent in the ED [25]; these differences are probably attributable to the different conditions in which See and Treat was applied in Tuscany.
CONCLUSIONS
The results of this study showed the significant impact that the See and Treat pathway could have on reducing overcrowding. Every month in the ED, 2418 patients with minor codes accessed the department with a simultaneous average presence of 84.14 patients, 7.48 of whom were eligible for the See and Treat pathway. The implementation of a See and Treat pathway could result in an 8.88% reduction in overall average attendances, bringing benefits such as reducing the average ED attendance to 76.5 patients per day. Reducing overcrowding would have a positive impact on both the users (delays in care, reduction in violence towards staff, reduction in legal disputes, reduction in the rate of abandonment of the ED and greater satisfaction in the care received) and the staff (reduction in errors, reduction in sentinel events, reduction in job stress, greater job satisfaction, and fewer delays in patient transfers) [7]. However, See and Treat is not the only solution to the problem of overcrowding, also considering that to date there are no studies in the literature that demonstrate the economic benefits of one model compared to another [9]. Other models include the Minor Injuries Units (MIUs), departments dedicated to certain minor emergencies with waiting times usually shorter than those in the Emergency Department, or the Fast Track model where, following Triage, the nurse independently and after assessing and ascertaining the user’s health needs sends them directly to the appropriate specialist if they have a minor pathology clearly suited to treatment by a single specialist. [18,19,26]. To conclude, a state-of-the-art model such as See and Treat applied in a large emergency department would significantly reduce the phenomenon of overcrowding by reducing waiting times, time spent in the ED and the total number of patients present in the department as well as reducing the number of voluntary abscondment from the ED. The development of greater nursing skills can contribute to the management of a See and Treat pathway with the ultimate aim of improving patient outcomes.
Limitations of the study
The fact that the study is a single-centre study is the main limitation of this paper; moreover, it was decided to analyse data from a period prior to the COVID-19 pandemic as it temporarily changed the pattern of access to the Emergency Department.
Possible Funding
This research did not receive any form of funding
Conflicts of interest
The authors declare that they have no conflicts of interest associated with this study
Contributions of the authors
Design: Riccardo Venditti and Anna Rita Marucci. Data acquisition, analysis or interpretation: Riccardo Venditti, Antonio Romanelli, Anna Rita Marucci, Flavio Marti. Statistical analysis: Giuseppe Campagna. Critical review of the article: Anna Rita Marucci, Flavio Marti, Roberto Latina, Lucia Mitello, Antonello Pucci, Lucia Mauro.
REFERENCES
- Jeyaraman MM, Alder RN, Copstein L, Al-Yousif N, Suss R, Zarychanski R, et al. Impact of employing primary healthcare professionals in emergency department triage on patient flow outcomes: a systematic review and meta-analysis. BMJ Open. 20 aprile 2022;12(4):e052850.
- Polello L, Boscolo Anzoletti A. See and Treat: ambulatorio per i codici minori come soluzione al sovraffollamento del Pronto Soccorso. L’Infermiere. 2015;2:28–31.
- Vetrano D. La Mappa della fragilità in Italia [Internet]. 2022. Disponibile su: https://www.italialongeva.it/wp-content/uploads/2022/04/indagine-2022_italialongeva.pdf
- ISTAT, curatore. Gli anziani e la loro domanda sociale e sanitaria [Internet]. 2021. Disponibile su: https://www.istat.it/it/files//2021/06/rapporto_commissione_anziani.pdf
- Ministero dell’Interno. Sbarchi e accoglienza dei migranti [Internet]. 2022. Disponibile su: https://www.interno.gov.it/sites/default/files/2022-12/cruscotto_statistico_giornaliero_21-12-2022.pdf
- Langiano T, Romagnoli C, Traversa G. Misura dell’Appropriatezza [Internet]. Ministero della Salute; 2007 [citato 15 giugno 2022]. Disponibile su: http://www.mattoni.salute.gov.it/mattoni/documenti/Documento_riepilogativo_Comitato_Scientifico.pdf
- Rastelli G, Cavazza M, Cervellin G. Sovraffollamento in Pronto Soccorso: Analisi del fenomeno e proposte di gestione. Emerg Care J. 2010;2(VI):25–35.
- Ministero della Salute. Annuario Statistico del Servizio Sanitario Nazionale [Internet]. 2020. Disponibile su: https://www.salute.gov.it/portale/documentazione/p6_2_2_1.jsp?lingua=italiano&id=3245
- Trisyani Y, Windsor C. Expanding knowledge and roles for authority and practice boundaries of Emergency Department nurses: a grounded theory study. Int J Qual Stud Health Well-Being. dicembre 2019;14(1):1563429.
- Hoyt KS, Evans DD, Wilbeck J, Ramirez E, Agan D, Tyler D, et al. Appraisal of the emergency nurse practitioner specialty role. J Am Assoc Nurse Pract. ottobre 2018;30(10):551–9.
- Lyons M, Brown R, Wears R. Factors that affect the flow of patients through triage. Emerg Med J EMJ. febbraio 2007;24(2):78–85.
- Levati S, Capitoni E. L’impatto del ruolo delle Emergency Nurse Practitioners nella gestione clinica dei pazienti nel contesto di un Dipartimento di Emergenza Urgenza nel Regno Unito. Prof Inferm. 30 aprile 2014;65(2).
- Dwyer T, Craswell A, Browne M. Predictive factors of the general public’s willingness to be seen and seek treatment from a nurse practitioner in Australia: a cross-sectional national survey. Hum Resour Health. 17 febbraio 2021;19(1):21.
- Giunta Regionale Toscana. Progetto di sperimentazione del modello See and Treat in pronto soccorso – revisione. Delibera n 449 mar 31, 2010.
- Brebner JA, Ruddick-Bracken H, Norman JN, Page JG. The nurse practitioner: management of minor trauma. Accid Emerg Nurs. gennaio 1996;4(1):43–6.
- Rosselli A, Becattini G, Cappugi M, C Francois, Ruggeri M. See & Treat. Protocolli medico-infermieristici: la sperimentazione toscana nei pronto soccorso. Firenze: Giunti; 2015. 38 p.
- Bornaccioni C, Coltella A, Pompi E, Sansoni J. Accessi non urgenti nel Dipartimento di Emergenza (D.E.) e ruoli dell’infermiere. Una revisione narrativa della letteratura. Prof Inferm. 10 novembre 2014;67(3).
- Bambi S, Giusti M, Becattini G. See & Treat in pronto soccorso: dal medico all’infermiere con competenze avanzate. Una revisione della letteratura. Assist Inferm E Ric. 2008;27(3).
- Radice C, Ghinaglia M, Doneda R, Bollini G. «See and Treat» in the Emergency Department: legal aspects and professional nursing responsibility. Prof Inferm. 2013;66(3):175–81.
- Lamanna C, Trastulli E. Accessi impropri al Pronto Soccorso e H24. Riv Soc Ital Med Gen. 2012;4:27–8.
- Nati G, Ialongo A, Fucito G, D’Angelo E, de Lucia L, Valente F, et al. Il management dei codici bianchi e verdi da parte dei medici di medicina generale in un Pronto Soccorso di Roma: lo studio MAPS. Riv Soc Ital Med Gen. 2010;3:18–22.
- Bongiovanni A, Canepari F, Ferraris P, Negri P, Pitisano C. Accessi dei cittadini stranieri al Pronto Soccorso dell’Azienda Ospedaliera SS. Antonio e Bigio e C. Arrigo di Alessandria (anni 2011 – 2012). Work Pap Public Health. 15 giugno 2013;2(1).
- Fiorentini G, Lippi Bruni M, Mammi I, Ugolini C. Valutazione dell’impatto prodotto nelle Regioni monitorate per la riduzione degli accessi impropri in Pronto soccorso. Quad Monit. 2013;32:87–108.
- Righi L, Jasmine L, Ronchese F, Trapassi S. Le urgenze minori in pronto soccorso: analisi del percorso See and Treat all’interno del Presidio Ospedaliero Misericordia di Grosseto. novembre 2020;64:1–3.
- Rosselli A, Francois C, Massai D, Becattini G, Paffetti M, Ruggeri M, et al. Risultati della sperimentazione del See and Treat. Toscana Medica. 2011;29(9):17–9.
- Lindner G, Woitok BK. Emergency department overcrowding : Analysis and strategies to manage an international phenomenon. Wien Klin Wochenschr. marzo 2021;133(5–6):229–33.

