Imelda, Atika Fadhilah Danaz Nasution*, Ika Murtiarini, Rosmaria, Diniaty
Department of Midwifery, Health Polytechnic of Jambi, Indonesia
Corresponding author: Atika Fadhilah Danaz Nasution, Jl. Prof DR GA Siwabessy No.42, Buluran Kenali, Kec. Telanaipura, Kota Jambi, Jambi 36122, Indonesia.
Orcid: https://orcid.org/0000-0002-4181-8621; Email: atikapoltekkes@gmail.com
Cita questo articolo
Abstract
Introduction: Postpartum mothers and newborns are a group that is vulnerable to COVID-19. Due to the COVID-19 pandemic, access to essential services such as breastfeeding counseling in hospitals, health clinics, and home visits has been disrupted. Postpartum mothers will immediately breastfeed. Therefore there is a need for knowledge, appropriate information, and support to provide breast milk, especially during the COVID-19 pandemic. This study aims to analyze the effect of virtual counseling on the knowledge of postpartum mothers during the COVID-19 pandemic at the Delima Midwife Clinic in Jambi City.
Materials and Methods: The current study utilized a quasi-experimental design with one group design pretest-posttest approach. This research was conducted in January-October 2021 and involved 75 postpartum mothers. This study using the zoom app. and questionnaire. Data analysis using Wilcoxon statistical test.
Results: The results showed an increase in knowledge where before being given virtual education, most of the respondents’ knowledge was in the Poor category, as much as 80% (mean 6.18). After the intervention, the knowledge of most respondents in the Good category was 46.7% (mean 12.15) with P-value <0.05.
Conclusion: The study concludes that virtual counseling significantly affects the knowledge of postpartum mothers about breastfeeding during the COVID-19 pandemic.
Keywords: Postpartum Mothers, Breastfeeding, COVID-19 pandemic, Counseling, Virtual.
INTRODUCTION
Coronavirus Disease 2019 (COVID-19) is an infectious disease caused by Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2). SARS-CoV-2 is a new type of coronavirus that has never been previously identified in humans [1,2]. There are at least two types of coronaviruses known to cause diseases that can cause severe symptoms, such as Middle East Respiratory Syndrome (MERS) and Severe Acute Respiratory Syndrome (SARS) [3]. The average incubation period is 5-6 days, with the most prolonged incubation period being 14 days. In severe cases of COVID-19, it can cause pneumonia, acute respiratory syndrome, kidney failure, and even death [4,5].
The spread of COVID-19 has reached almost all provinces in Indonesia, with the number of cases and deaths increasing. This condition impacts the political, economic, social, cultural, defense and security aspects, as well as the welfare of the people in Indonesia [6]. Indonesia reported its first case of COVID-19 on March 2, 2020, and the number continues to grow until now. The data on confirmed cases of COVID-19 in Indonesia as of October 21, 2021, were 4.237.834 people, 143.120 people died, and patients who had recovered were 4.079.120 people [7]. Meanwhile, in Jambi Province, COVID-19 cases increased sharply. As of October 3, 2021, the Jambi Provincial Government recorded 29.616 positive confirmed cases of COVID-19, 768 people died, and 28.476 people recovered [8].
Postpartum mothers and newborns are a group that is vulnerable to the COVID-19 virus [9,10]. During the COVID-19 pandemic, access to essential services such as breastfeeding counseling in hospitals, health clinics, and home visits has been disrupted [11,12]. The amount of inaccurate information and news circulating about the safety of breastfeeding has reduced the number of breastfeeding mothers because mothers are afraid of transmitting diseases to their babies even though this is the most appropriate moment to provide the best intake for babies through breastfeeding. After all, breast milk contains immune substances which protect children from infections and chronic diseases and reduces the chances of suffering from health problems later in life. The Covid-19 virus has never been found in breast milk [13,14].
Social restrictions during the COVID-19 pandemic require staying at home so that continuous care cannot be carried out, both health workers to make visits and mothers and babies to check their health status at the nearest health service. The impact of this situation can cause stress and worry for postpartum mothers who are still adapting to breastfeeding activities. Breastfeeding mothers need to continue to get support in the form of assistance to overcome problems during the breastfeeding process [2,15].
The current state of the COVID-19 pandemic has made it difficult for postpartum mothers to get information and consult face-to-face due to the strict rules of physical distancing. This condition resulted in a decrease in the number of visits by postpartum mothers to health workers. The limitations of accessing information on exclusive breastfeeding from health workers can be overcome by providing health promotions delivered via Telemedia, where postpartum mothers can communicate virtually and see some presentation materials and videos of good and correct breastfeeding techniques [16,17].
Health promotion through Telemedia/online is expected to increase the knowledge of postpartum mothers about exclusive breastfeeding and sound and correct breastfeeding techniques. This online learning for postpartum mothers is expected to help postpartum mothers to obtain information and consult during the COVID-19 pandemic.
This study aims to examine the effect of Virtual Counseling on Postpartum Mother’s Knowledge of Breastfeeding during the Covid-19 Pandemic at the Delima Midwife Clinic in Jambi City.
Method
Trial design
The current study utilized quasi-experimental design with one group design pretest-posttest approach.
Participants
This research was conducted in January-October 2021 and involved 75 postpartum mothers who were randomly selected and met the sample inclusion requirements, such as breastfeeding mothers, mothers who have never participated in counseling activities about breastfeeding, and who have the Zoom app.
Intervention
The research variable is the knowledge of postpartum mothers. Before the intervention was given, the researcher first measured the level of knowledge of postpartum mothers (pre-test). After being given the intervention, the researcher again measured the level of knowledge of postpartum mothers (post-test). In this study, the intervention model provided was virtual education about breastfeeding, which was carried out once for 1 hour, i.e., 45 minutes of material delivery and 15 minutes of discussion). In this study, researchers explain the principles of breastfeeding, including the correct way of breastfeeding. The researcher presented the material with a poster or picture of the correct breastfeeding technique.
The knowledge questionnaire consists of 33 questions with correct and incorrect answer choices. If the postpartum mother answered correctly, she was given a score of 1; if the answer was wrong, she was given a score of 0. The range of scores obtained was between 0-33. The questionnaire used the Guttman scale. The contents of the postpartum mother’s knowledge questionnaire included the benefits of breastfeeding, breastfeeding techniques, breastfeeding positions, correct breastfeeding steps, duration and frequency of breastfeeding, milk release, milk storage, breast care, nutrition during breastfeeding, and problems in breastfeeding.
The Guttman scale has an important feature where it is a cumulative scale and only measures one dimension of a multidimensional variable; therefore, this scale is dimensionless. The data obtained are interval data or dichotomous ratios (two alternatives) [18].
Researchers did not try out the knowledge questionnaire because this questionnaire was adopted from Nalsalisa’s study [19]. The results of the validity test obtained a p-value <0.05 on 33 questions. For the reliability test, this questionnaire is reliable because the value of r count> r table is reliable.
The researcher has worked as a lecturer and researcher for 10-15 years and has Master and Doctoral degrees. The researcher has done much research in the health sector and has compiled many questionnaires, so the researcher prepared a questionnaire for this study. Before the research was conducted, the questionnaire was tested on ten postpartum mothers, and the results indicated that two questions had to be replaced because they were invalid.
Outcomes
This study has produced a description of the knowledge of postpartum mothers before and after virtual educational interventions and the effect of virtual education interventions on postpartum mothers’ knowledge.
Sample size
75 postpartum mothers who have been calculated using the Slovin formula at a precision (d) = 0.1, the total population is 307 people. The study population, also known as the target population in this study, is the number of postpartum mothers who visited the Delima Midwife Clinic, Jambi City, Indonesia, in 2020, totaling 307 people.
Ethical Consideration
No economic incentives were offered or provided for participation in this study. In this study, because the subject was still a minor so the researcher had asked for and obtained parental consent so that their child could participate in the study. The study was performed in accordance with the ethical considerations of the Helsinki Declaration. This study obtained ethical feasibility under the Health Research Ethics Commission of the Ministry of Health, Jambi, and registration number: LB.02.06/2/161/2021.
Statistical analysis
Data are presented as numbers and percentages for categorical variables. Continuous data were expressed as mean ± standard deviation (SD) or median with Interquartile Range (IQR). To see the distribution of research data, the Kolmogorov Smirnov test was used. Then proceed with bivariate analysis using the Wilcoxon test. All tests with p-value (p)<0.05 were considered significant. Statistical analysis was performed using the SPSS version 16.0 application.
RESULTS
The characteristics of respondents in this study include age, education, employment status and parity. The following is the frequency distribution of the respondents’ characteristics in this study:

Table 1. Frequency Distribution of Respondents Characteristics
The majority of respondents are in the age range of 32-38, have high school education, do not work and have multiparous status.
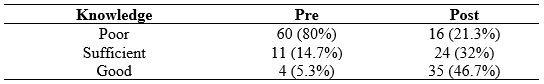
Table 2. Distribution of knowledge before and after interventions
Most of the respondents’ knowledge before the intervention was in the Poor category, as much as 80%. After the intervention, the knowledge of postpartum mothers was mainly in the Good category, as much as 46.7%.
Table 3 shows that the Kolmogorov Smirnov statistical test results obtained a significant value of knowledge at the pretest and posttest virtual education, each less than 0.05.

Table 3. Normality Test Results of Knowledge pretest and posttest virtual education
The knowledge data at the pretest and posttest virtual education not normally distributed. Therefore, the statistical difference test was tested using Wilcoxon (Table 4)

Table 4. Average Knowledge Pretest and Posttest Virtual Education
Table 4 shows that knowledge before giving virtual education has a mean value = 6.18, while after giving virtual education, it increases to 12.15, with P-value <0.05.
DISCUSSION
Postpartum conditions cause a partial decrease in immunity due to physiological changes during pregnancy, making postpartum women more susceptible to viral infections. Therefore, the COVID-19 pandemic will likely cause severe consequences for postpartum mothers. Social distancing measures are effective in reducing disease transmission. It also applies to postpartum mothers to limit themselves to not being exposed to the outside environment, let alone traveling to pandemic areas [20,21]. The risk of postpartum mothers being infected with COVID-19 is one of them when visiting a postnatal check-up at a midwifery clinic or hospital, so mothers must increase their vigilance by continuing to be disciplined in the use of PPE [21,22]. Postpartum mothers can limit visits to obstetric clinics or hospitals by conducting online consultations, actively self-checking for signs and dangers during pregnancy, and only making visits when things are worrying. This study aims to analyze the effect of virtual education on postpartum mothers’ knowledge about breastfeeding [13,23]. Based on the univariate analysis, it is known that most of the respondents have less knowledge (80%), and a small portion (5.7%) have good knowledge. Health promotion cannot be separated from activities or efforts to convey health messages to communities, groups, or individuals.
There are still many mothers who say that mothers who are confirmed positive for COVID-19 cannot breastfeed their babies directly. The world Health organization still recommends that mothers continue breastfeeding their babies but must follow hygiene procedures. SARS-CoV-2 has not been detected in mothers with suspected or confirmed COVID-19, and there is no evidence that the virus is transmitted through breast milk [22,24].
Postpartum mothers who have good knowledge increased to 42% after counseling. The mean value of knowledge before counseling was done was 6.18, then after virtual counseling, there was an increase in the mean value of postpartum mothers’ knowledge about breastfeeding to 12.15.
There is an increase in knowledge of breastfeeding mothers about breastfeeding during the COVID-19 pandemic. It is hoped that changes in behavior will occur, such as giving exclusive breastfeeding to their babies because concerns about transmission of COVID-19 through breast milk have been answered, namely that it is not proven to transmit COVID-19, and breastfeeding mothers can also provide breast milk exclusively with due observance of health protocols. Thus, even though the baby is in a pandemic, the baby’s needs are still met with the mother giving exclusive breastfeeding even though the mother is still working and can still provide exclusive breastfeeding [25].
The statistical test results obtained a P value < 0.05, so it can be concluded that virtual counseling affects postpartum mothers’ knowledge about breastfeeding during the COVID-19 pandemic. Silalahi’s research (2012) reported differences in the level of knowledge of postpartum mothers after being given counseling. There was an effect of counseling on exclusive breastfeeding on mothers’ knowledge about exclusive breastfeeding.
This finding strengthens the previous finding that reported that knowledge for the intervention group obtained a mean value of 58.89. In contrast, the control group obtained a mean value of 45.47, with P-value = 0.012, meaning that counseling affects the knowledge of postpartum mothers in the Timbusseng Village Work Area, Pattallassang District, Kab. Gowa [26].
Extension activities can be carried out with two-way communication where the communicator (extension) provides the communicant opportunity to provide feedback on the material. This interactive discussion on two-way communication is expected to trigger the desired behavior change. This health education’s success is determined by the material presented and the interpersonal relationships between communicators and communicants [16,27]. An indicator of the success of extension that can be measured quickly is the similarity of meaning or understanding of what is conveyed by the communicator and accepted by the communicant [24,28].
Virtual counseling media is an alternative for health workers to consult postpartum mothers during the COVID-19 pandemic to reduce the risk of spreading COVID-19 disease, which can endanger pregnant women and neonates. The Good knowledge of the mother determines the correct breastfeeding technique. Good knowledge about the importance of breastfeeding and ways to breastfeed will form a positive attitude, and then correct breastfeeding behavior will occur [24,29].
CONCLUSION
Virtual counseling has a significant effect on the knowledge of postpartum mothers about breastfeeding during the COVID-19 pandemic.
STUDY LIMITATIONS
There are limitations to the number of research samples, and samples only come from one location; therefore, the results of this study cannot be differentiated from samples or participants with different characters in other locations. Future research must involve many samples, and research locations must also be heterogeneous.
FUNDING STATEMENT
This research did not receive any specific grant from funding agencies in the public, commercial, or not for profit sectors.
CONFLICT OF INTEREST
The authors report no conflict of interest.
AUTHORS’ CONTRIBUTION
All authors equally contributed to preparing this article.
ACKNOWLEDGEMENT
We would like to thank the director of the Department of Midwifery, Health Polytechnic of Jambi, Indonesia for supporting this research.
REFERENCES
1. Palmquist AEL, Parry KC, Wouk K, Lawless GC, Smith JL, Smetana AR, et al. Ready, Set, BABY live virtual prenatal breastfeeding education for COVID-19. Journal of Human Lactation. 2020;36(4):614–8.
2. Nguyen PH, Kim SS, Nguyen TT, Hajeebhoy N, Tran LM, Alayon S, et al. Exposure to mass media and interpersonal counseling has additive effects on exclusive breastfeeding and its psychosocial determinants among Vietnamese mothers. Maternal & child nutrition. 2016;12(4):713–25.
3. Shu Y, He H, Shi X, Lei Y, Li J. Coronavirus disease‑2019. World Academy of Sciences Journal. 2021;3(2):1.
4. World Health Organization. The Corona Virus Disease 2019 (COVID-19). 2020;
5. Kumar D, Malviya R, Sharma PK. Corona virus: a review of COVID-19. EJMO. 2020;4(1):8–25.
6. Yamali FR, Putri RN. Dampak covid-19 terhadap ekonomi indonesia. Ekonomis: Journal of Economics and Business. 2020;4(2):384–8.
7. Kompas.com. UPDATE 21 Oktober: 143.120 Orang di Indonesia Meninggal akibat Covid-19 [Internet]. 21 Oktober 2021. 2021. Available from: https://nasional.kompas.com/read/2021/10/21/18281271/update-21-oktober-143120-orang-di-indonesia-meninggal-akibat-covid-19
8. Analisis TP&, PENANGANAN S, Provinsi C-19, Jambi. Pemetaan Risiko Covid-19 Kabupaten/Kota di Provinsi Jambi [Internet]. 3 Oktober 2021. 2021. Available from: https://corona.jambiprov.go.id/v2/files/zonasi/Pemetaan Risiko_3 Oktober 2021.pdf
9. Liu H, Wang L-L, Zhao S-J, Kwak-Kim J, Mor G, Liao A-H. Why are pregnant women susceptible to COVID-19? An immunological viewpoint. Journal of reproductive immunology. 2020;139:103122.
10. Barrero-Castillero A, Beam KS, Bernardini LB, Ramos EGC, Davenport PE, Duncan AR, et al. COVID-19: neonatal–perinatal perspectives. Journal of Perinatology. 2021;41(5):940–51.
11. Schindler-Ruwisch J, Phillips KE. Breastfeeding during a pandemic: The influence of COVID-19 on lactation services in the Northeastern United States. Journal of Human Lactation. 2021;37(2):260–8.
12. Sikorski J, Renfrew MJ, Pindoria S, Wade A. Support for breastfeeding mothers: a systematic review. Paediatric and perinatal epidemiology. 2003;17(4):407–17.
13. Singh AP, Kumar VHS, Panda S. Supporting Breastfeeding in 2021 and Beyond—Lessons from the Pandemic. Pediatric Reports. 2021;13(2):289–301.
14. Theurich MA, McCool-Myers M, Koletzko B. Supporting breastfeeding of small, sick and preterm neonates. In: Seminars in Perinatology. Elsevier; 2021. p. 151387.
15. Lima ACMACC, Chaves AFL, Oliveira MG de, Lima SAFCC, Machado MMT, Oriá MOB. Breastfeeding consultancy during the COVID-19 pandemic: experience report. Escola Anna Nery. 2020;24.
16. Haider R, Ashworth A, Kabir I, Huttly SRA. Effect of community-based peer counsellors on exclusive breastfeeding practices in Dhaka, Bangladesh: a randomised controlled trial. The lancet. 2000;356(9242):1643–7.
17. Haider R, Kabir I, Huttly SRA, Ashworth A. Training peer counselors to promote and support exclusive breastfeeding in Bangladesh. Journal of Human Lactation. 2002;18(1):7–12.
18. Sugiyono D. Metode penelitian pendidikan pendekatan kuantitatif, kualitatif dan R&D. 2013;
19. Nalsalisa J. Pengaruh Konseling Laktasi terhadap Breasfeeding Self-Efficacy pada Ibu Menyusui di Wilayah Kerja Puskesmas Sungai Mandau Tahun 2020. Universitas Pahlawan Tuanku Tambusai; 2020.
20. Giacalone A, Rocco G, Ruberti E. Physical health and psychosocial considerations during the COVID-19 outbreak. Psychosomatics. 2020;61(6):851–2.
21. Dubey S, Biswas P, Ghosh R, Chatterjee S, Dubey MJ, Chatterjee S, et al. Psychosocial impact of COVID-19. Diabetes & Metabolic Syndrome: clinical research & reviews. 2020;14(5):779–88.
22. Ceulemans M, Verbakel JY, Van Calsteren K, Eerdekens A, Allegaert K, Foulon V. SARS-CoV-2 infections and impact of the COVID-19 pandemic in pregnancy and breastfeeding: Results from an observational study in primary care in Belgium. International journal of environmental research and public health. 2020;17(18):6766.
23. Wilson JC. Using social media for breastfeeding support. Nursing for Women’s Health. 2020;24(5):332–43.
24. Anderson AK, Damio G, Young S, Chapman DJ, Pérez-Escamilla R. A randomized trial assessing the efficacy of peer counseling on exclusive breastfeeding in a predominantly Latina low-income community. Archives of Pediatrics & Adolescent Medicine. 2005;159(9):836–41.
25. Rochmawati R, Kusmintarti A, Fary V, Elfaristo L, Pembayun EL, Hayuningsih S, et al. Meningkatkan Kapasitas Ibu Menyusui Melalui Penyuluhan Kesehatan Mengenai Pemberian ASI Eksklusif Selama Masa Pandemi COVID-19. Sasambo: Jurnal Abdimas (Journal of Community Service). 2021;3(2):76–82.
26. Syahrir S, Alam S. Faktor-Faktor yang Berhubungan dengan Teknik Menyusui pada Ibu di Puskesmas Pattallassang Kabupaten Takalar. Al-Sihah: The Public Health Science Journal. 2016;8(2):130–8.
27. Graffy J, Taylor J. What information, advice, and support do women want with breastfeeding? Birth. 2005;32(3):179–86.
28. Anandita MYR. Penyuluhan Kesehatan Melalui Telemedia Pada Ibu Hamil tentang Mempersiapkan Pemberian ASI Eksklusif. Jurnal Pengabdian Masyarakat Bakti Parahita (p-ISSN-2747-2094). 2020;1(01).
29. Aidam BA, Perez-Escamilla R, Lartey A. Lactation counseling increases exclusive breast-feeding rates in Ghana. The Journal of nutrition. 2005;135(7):1691–5.
![]() This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.

