TRANSFORMATIVE LEADERSHIP AND JOB SATISFACTION IN THE NURSING PROFESSION: A NARRATIVE REVIEW
Carla Rizzo 1, Flavio Marti 2, Luca Perrozzi 3*, Lucia Mauro 4
- Complex Anesthesia, Resuscitation and Intensive Care Unit, IRCCS Hospital Physiotherapy Institutes, Rome (Italy).
- Department of Health Professions AO San Camillo Forlanini, Master's Degree Course in Nursing and Midwifery Sciences, “Sapienza” University of Rome, San Camillo section, Rome (Italy).
- Accident and Emergency and Specialist Surgery Department, A.O. San Camillo Forlanini, Rome (Italy).
- Department of Surgical Sciences, Elective Surgery Block, A.O. San Camillo Forlanini, Rome (Italy).
*Corresponding Author: Luca Perrozzi, Department of Accident and Emergency and Specialist Surgery, Azienda Ospedaliera San Camillo Forlanini, C.ne Gianicolense 87, 00159 Rome (Italy). Email: lucaperrozzi@yahoo.it
Cite this article
ABSTRACT
Introduction: Healthcare organisations require optimal leadership to achieve goals and deliver high-quality services. Leadership is the ability to influence employee behaviour and beliefs and is an essential element of a successful organisation. Improving job satisfaction is a key objective in addressing the challenges related to achieving and maintaining quality standards, ensuring patient satisfaction and staff retention. Similarly, transformational leadership has positive effects on nurses' job satisfaction and promotes organisational wellbeing in the workplace.
Objective: The purpose of the review is to describe transformational leadership and job satisfaction in the nursing profession through a narrative revision.
Materials and methods: The bibliographic research was carried out between September 2022 and March 2024 by consulting databases such as PubMed, CINAHL, and PsycInfo, with time limits of 12 years and Italian and English language filters. All items deemed relevant have been stored and managed with the Zotero IT platform.
Results: 16 studies were examined: 1 comparative study, 5 descriptive correlational studies, 1 meta-analysis, 1 systematic review, 4 cross-sectional studies, 2 mixed method studies and 2 unspecified studies. The results of this study are consistent with transformational leadership theory, which highlights the leader's role in providing employees with supportive work environments that result in higher levels of job satisfaction and efficiency.
Conclusions: The skills of a transformative leader, such as the ability to listen, provide support, and promote fairness and recognition, are fundamental to increasing nurses' job satisfaction and sustaining environments with a high level of quality of care. Healthcare managers must protect the quality of work undertaken by staff, implementing strategies that can improve nurses' working conditions.
Keywords: Transformational Leadership; Job Satisfaction; Nurse; Work environment.
INTRODUCTION
Healthcare organisations are social systems in which human resources are the most important factor for the delivery of health care. Such organisations require optimal leadership to achieve goals and deliver high-quality services [1,2]. Leadership is the ability to influence employee attitudes and beliefs and is an essential element of successful and efficient organisations [3,4]. The current challenges of the health system require the presence of flexible and efficient managers [5] because the complexity of nurses' tasks requires complex leadership skills [6]. A wide range of studies have described the favourable outcomes of positive leadership, in particular, the transformational leadership style [7–9]. Transformational leadership motivates problem-solving and intellectual stimulation by influencing staff engagement in the organisation's mission. Such leaders stimulate nurses to use problem-solving strategies and provide patient care autonomously and responsibly [10]. Certain studies suggest that transformative leaders have positive effects on the wellbeing and job satisfaction of healthcare workers [4,11]. In addition, transformational leadership transforms nurses' goals and values for the benefit of the nursing profession [12] and work organisation and promotes team communication and collaboration, the work environment and organisational culture [13].
Work satisfaction, defined as “a pleasant emotional state that derives from the judgment of one's work or work experience” [14], is extremely important both for nursing managers and wellbeing of nurses in the workplace. Improving job satisfaction is a key objective in addressing the challenges related to achieving and maintaining quality standards, ensuring patient satisfaction and staff retention [15,16].
The more satisfied employees are, the more motivated they are to work and the greater the possibility of achieving the objectives, with an increase in productivity and quality. Job satisfaction cannot be overlooked if improving work performance is a priority of the organisation [17].
As part of the study, the authors described transformational leadership and staff job satisfaction, with the aim of synthesising the evidence that describes these aspects in the nursing profession.
Transformational leadership theorists indicate that leaders use socialised power to elevate and empower subordinates and provide the resources needed to achieve more than they thought possible in their work. Intrinsic motivation strategies support nursing autonomy, competence and relationship with others in the context of a mutually supportive environment to foster social and personal development at the service of the organisation's vision, mission, values, aims and objectives. In this way, subordinate nursing staff enjoy satisfaction in overcoming work challenges.
Nursing leaders must be proactive in recognising and addressing the job satisfaction needs of direct care nursing staff in order to maintain high-quality staff as well as the quality of patient care and healthcare environments [18].
Objective of the study
The purpose of the review is to describe transformational leadership and job satisfaction in the nursing profession through a narrative revision of the literature.
MATERIALS AND METHODS
The bibliographic research was carried out from 1 September 2022 to 31 March 2024 by consulting the following databases: PubMed, Cinhal, and PsycInfo, with time limits of 10 years and Italian and English language filters. The research question was formulated according to the PICO method, as shown in Table 1.
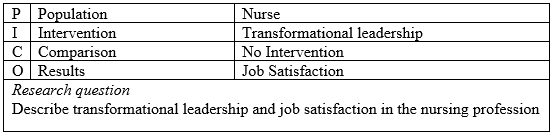
Table 1. Research question formulated according to the PICO method
The following keywords were used: “transformational leadership”, “job satisfaction”, and “nurse*”. Within the study, all the articles that dealt with transformational leadership and job satisfaction in the nursing profession with a time limit of 12 years (from January 2012 to March 2024) were included in English and Italian. All articles written in other languages were excluded.
RESULTS
During the bibliographic research, the search string generated a listing of 223 articles on 3 different databases (PubMed, Cinhal, and PsycInfo) (figure 1).
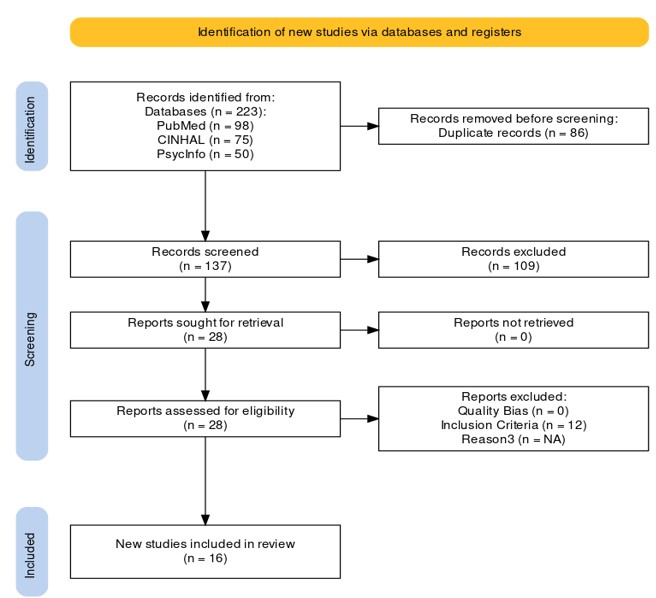
Figure 1. “PRISMA Statement” flowchart[19].
All items were managed using the Zotero IT platform. After the duplicates were removed, 137 articles remained. Selection by title and by abstract led to the exclusion of 109 articles. For the subsequent critical analysis, the 28 articles were read and evaluated in their entirety to identify and understand the content. On reading the full texts, 12 articles were discarded because they failed to comply with the inclusion criteria. A total of 16 studies were evaluated, broken down as follows: 1 comparative study, 5 descriptive correlational studies, 1 meta-analysis, 1 systematic review, 4 cross-sectional studies, 2 mixed method studies, 2 unspecified studies (see Table 2). Fifteen articles were published in English and one in Italian.
Evaluation of the quality of the studies
The articles were selected and evaluated using the checklists from “JBI Critical Appraisal Tools” [20]. A total of 16 articles were reviewed. To classify the studies in terms of quality, the overall score was calculated based on the number of "yes" answers. The included studies had at least 6 out of 10 of the items included in the checklists chosen by the authors of this study.
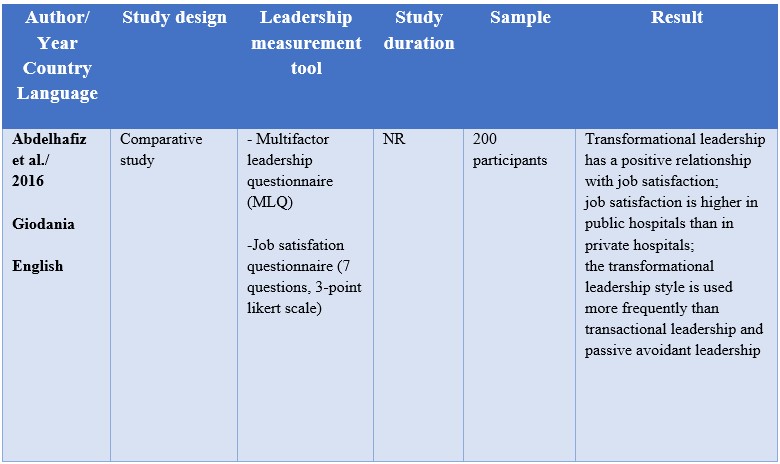
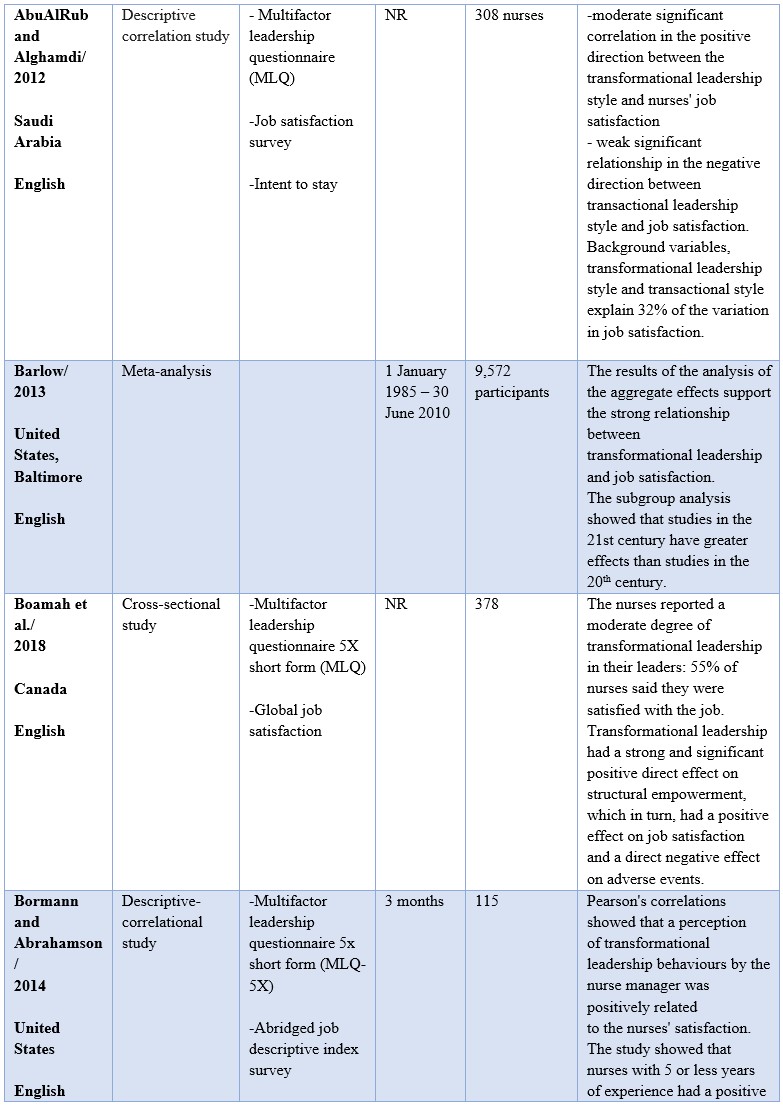
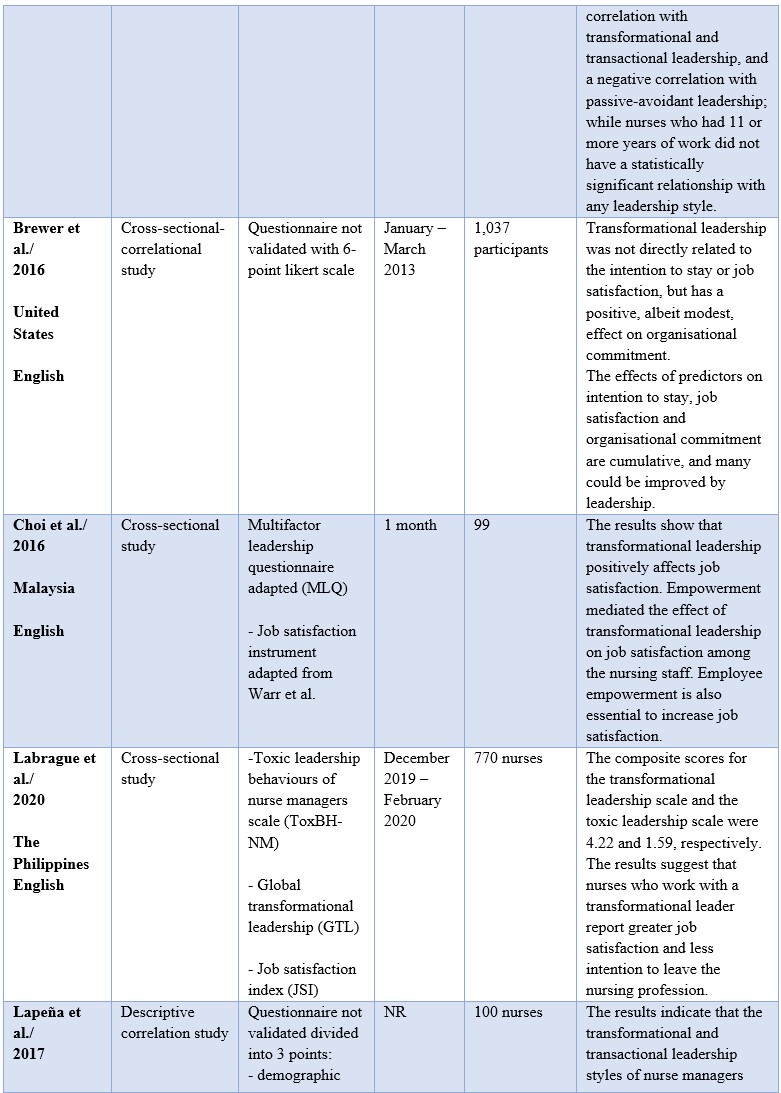
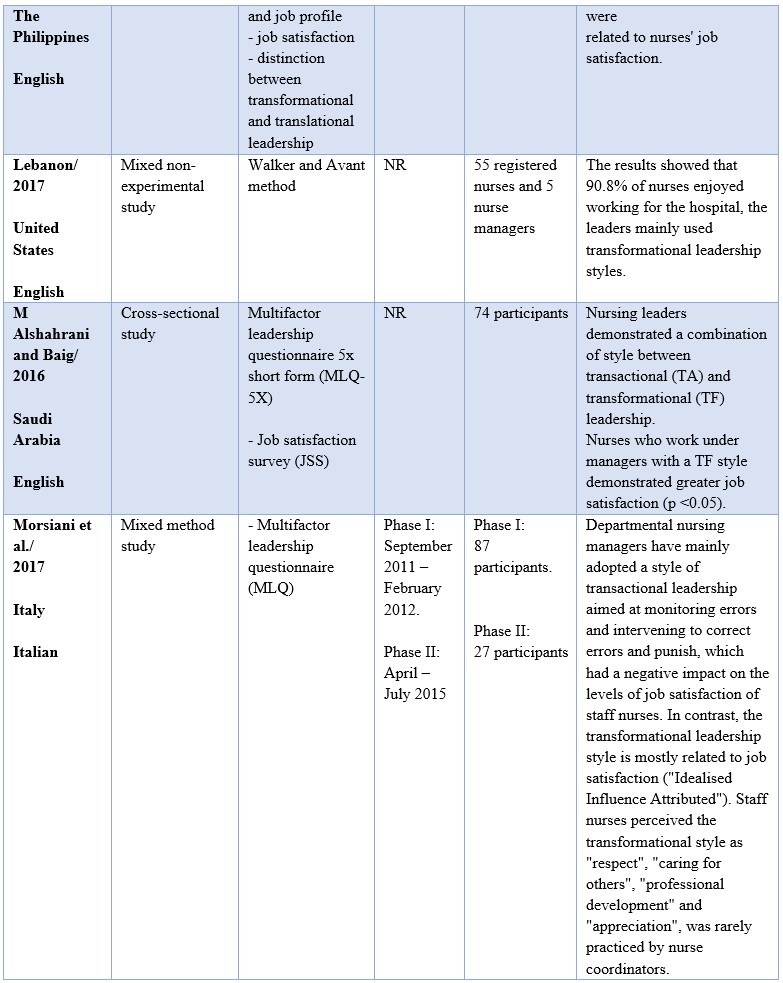
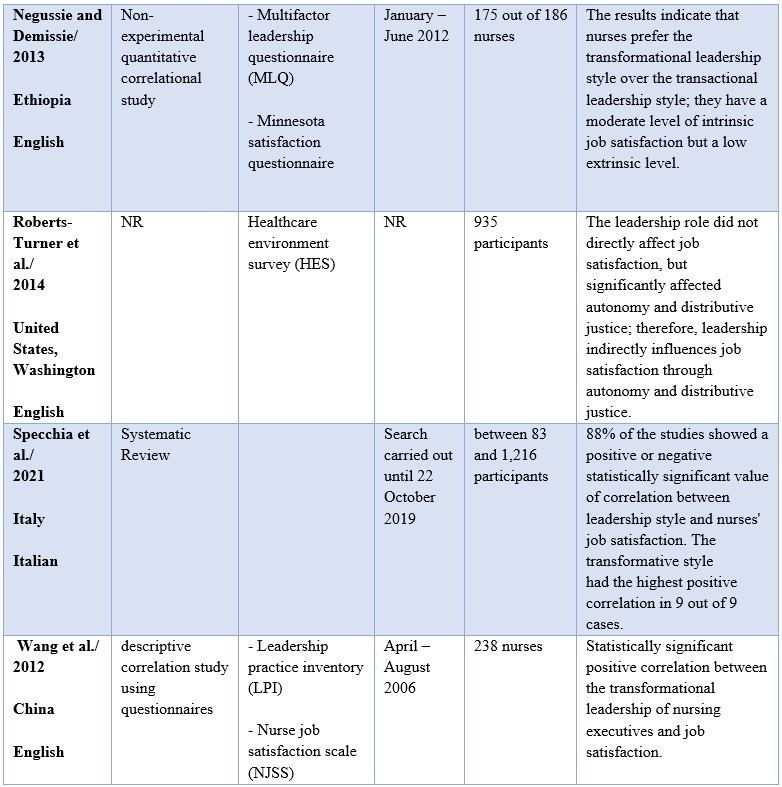
Table 2. Summary of results
DISCUSSION
The literature considered demonstrates that the transformational leadership style can positively influence job satisfaction in most of the included studies, regardless of the sample, the country, or the type of study chosen [21–34]. Only two studies do not describe a positive link between the variables analysed [35,36].
The results of this review highlight that the characteristics of a transformative leader – such as listening, support, fairness and recognition – are fundamental to increasing nurses' job satisfaction and creating environments with superior quality of care.
For example, the results of the systematic review by Specchia [31] and AbuAlRub and Alghamdi [34] emphasise that leaders who adopt a transformative style promote greater job satisfaction among nursing staff than those who adopt a transactional style. In fact, transformational leadership shows a significant and moderate correlation with job satisfaction (r = 0.45, p < 0.001), while transactional leadership shows a weak significant relationship with job satisfaction (r = -0.14, p < 0.01)[34]. In fact, the strength of transformational leaders is that they dedicate time to teaching and coaching nurses, focus on developing and improving their strengths, and provide advice for their professional and personal development [31].
These results are consistent with previous studies by Al-Hussami [37] and Bass [38]. These studies support the idea that nurses who worked with leaders who showed transformational leadership styles were more satisfied. In fact, these leaders taught and trained nurses, providing advice for professional development, treating them as individuals, listening to their concerns, and promoting their personal development[39].
Another issue concerns the correlation between transformational leadership, job satisfaction and the intention to leave work. For example, Labrague's study [26] shows how the transformational leadership of nursing executives influences nurses' job satisfaction and their intention to leave the profession despite the demographic characteristics (age, sex, sentimental situation, full time). Specifically, it differentiates toxic leadership from transformational leadership. Toxic leadership is significantly correlated with dissatisfaction at work (r = -0.19, p <0.001), absenteeism (r = 0.23, p < 0.001), psychological distress (r = 0.09, p < 0.05), organisational turnover intention (r = 0.11, p < 0.01) and professional turnover intention (r = 0.14, p < 0.001). Instead, transformational leadership is significantly related to job satisfaction (r = 0.37, p < 0.001), absenteeism (r = -0.13, p < 0.001) and the intention of organisational turnover (r = -0.08, p < 0.05). This underlines how important it is to educate leaders and nurse managers within healthcare facilities and develop behaviours that help and support staff. Indeed, maintaining a quality working environment has a significant impact on the retention of nurses and decreases the intention to leave the profession or nurse turnover.
In contrast, the results of the study by AbuAlRub and Alghamdi [34] indicate that the relationship between the transformational leadership style and the level of intention to stay at work was not statistically significant (r = 0.08, p = 0.14), so the transformational leadership style had no effect on the intention to stay at work.
Even if the results regarding intention to leave the profession are mixed, transformational leadership can provide supportive work environments that result in higher levels of job satisfaction and effectiveness [39]. In fact, by strengthening solid relationships with staff, transformational leaders understand the needs of nurses, they encourage staff to develop skills and autonomy in order to empower them to act.
The studies by Bohaman [23] and Choi [25] analysed the role that structural empowerment has in the relationship between job satisfaction and the transformational leadership style. Structural empowerment, in line with other previous research, [40–42] influences job satisfaction, organisational commitment[41], work commitment[43], lower levels of burnout and work stress [41] and turnover intentions[41,44]. This is due to the characteristics of the transformational leader, such as the ability to listen, inspire staff and stimulate individual and group skills. We can therefore state from these studies [23,25] that empowerment has a positive influence on job satisfaction.
In the study by Borman and Abrahamson [24], it emerged that nurses who worked for 5 or fewer years within the hospital had a statistically positive correlation with transformational and transactional leadership, while nurses who worked for 11 or more years did not have any type of significant relationship with any leadership style. For those who worked for 5 or fewer years, job satisfaction was mainly related to promotion opportunities, while for nursing staff of 11 or more years it had a stronger correlation for supervision. Therefore, leaders must understand the needs of their employees based on individual differences and their work experience.
The studies by McVicar and Laschinger [35,36] did not find a direct correlation between transformational leadership and job satisfaction. Roberts and Turner [36] highlighted how autonomy and distributive justice positively affect job satisfaction (0.503, p < 0.001; 0.272, p < 0.001). Within the study, the authors emphasise that autonomy represents a characteristic of transformational leadership, and distributive justice represents transactional leadership. It follows that, even if a direct relationship between the variables considered has not been found, autonomy represents one of the fundamental characteristics of the transformational leadership style. This implies that an increase in autonomy and distributive justice would increase job satisfaction.
Conversely, according to Brewer,[35] transformational leadership was not a significant predictor of job satisfaction. The variables with positive significant coefficients related to job satisfaction were organisational commitment, autonomy, tutor support and promotional opportunities. Considering job satisfaction as a dependent variable, a nurse who goes from a low organisational commitment value to a very high organisational commitment value is 12.6% more likely to be satisfied.
The Barlow meta-analysis [22] showed a very strong relationship between transformational leadership and job satisfaction: the aggregate result of the studies generated by the estimates of the size of the effect are more incisive and representative than the outcomes of individual studies examined. The study shows how transformational leaders stimulate and empower nurses to provide the resources needed to achieve greater results. In fact, staff intrinsic motivation strategies support autonomy, competence, and nursing relationships to create a mutually supportive work environment that promotes social and individual development at the service of the organisation's mission, values, and goals. In addition, the results report that the relationship between transformational leadership/job satisfaction has strengthened over time. The subgroup analysis showed that studies in the 21st century have stronger effects than studies in the 20th century. This can be explained by the identification of the Magnet design health and nursing excellence programmes, which notably increased in the 21st century [22]. Therefore, strategies must be implemented within hospitals today to increase the job satisfaction of nurses by assessing staff satisfaction on an annual basis and improving working conditions.
Another result to consider concerns the difference reported in various studies within the Barlow meta-analysis [45–47] between the greater satisfaction detected by nurses in indirect or mixed care (nurse administrators, specialised nurses) compared to staff engaged in direct care (ward nurses). This can be explained by the great shortage of nurses that is being experienced worldwide, which leads to greater workloads, work stress, burnout, intentions to leave the profession and turnovers that strongly affect job satisfaction. This is why nursing leaders are fundamental in order to understand and recognise the needs of their staff, to maintain a high quality of work, as direct care provides essential services for patients.
A study conducted in Italy by Morsiani[29] engaged focus groups to identify the main characteristics of a leader in relation to the achievement of satisfaction:
- Professional recognition. Job satisfaction depends on professional recognition, that is, giving value to the work of a nurse and expressing appreciation for the work of the staff.
- Fairness. Nursing leaders must adopt the same behaviour, be honest with all staff members and be objective about mistakes at work.
- Care of the individual. If a leader supports and listens to their staff, the latter will be more likely to experience job satisfaction. Often, the role of nurses, especially in Italy, is not recognised at a social and economic level. The first in the field who must defend the profession are precisely the leaders who must lead the profession to its emancipation, while maintaining relationships with other professionals. In fact, it is not a war between professions but an endeavour to enhance the value of the nursing profession.
- Support. Globally, the shortage of nurses impacts patient care, as the same care result must be achieved in the same time and with fewer human and material resources. Leaders should not put themselves on a different plane than nurses but should be present in the ward and help them in case of need. In addition, being present in the department is an opportunity to check the work of the staff and recognise what the errors may be within the care path and look for strategies to improve it.
- Listening. Being present also means knowing how to listen and understand the needs of the staff, such as shift scheduling and the difficulties encountered at work.
- Staff appreciation. The nursing manager must promote staff development by seeking to improve nurses, both individually and as a group. Training, feedback, and refresher courses are crucial tools to ensure that staff have greater autonomy and responsibility.
- Team development. Another important issue is teamwork. This study revealed the extent to which staff did not feel part of a work group. Teamwork is essential to ensuring collaboration, compensating for others' inadequacies, and sharing common goals and strategies to achieve patient satisfaction.
Therefore, there is scope for future studies employing a more rigorous research approach that would establish causal links between the variables considered and the appropriateness of generalising the results.
CONCLUSIONS
The review found that transformational leadership can have a positive influence on nursing job satisfaction levels. Therefore, nursing leadership assumes a fundamental role in influencing the perception that nurses have of their organisation. A leadership style that promotes nurses' autonomy, support, and empowerment can improve job satisfaction, organisational commitment, and nurses' intention to remain in their position while reducing emotional exhaustion [6]. This means that transformational leaders, through their stimulating and motivating behaviour, can induce changes in the psychological states of workers within organisations. In addition, some studies have shown how the adoption of the transformational leadership style can indirectly influence job satisfaction through the development and strengthening of nurses' sense of empowerment [23,25]. Within healthcare organisations, leadership plays a key role in providing effective and efficient care and translates into positive outcomes for professionals, patients and the work environment. It is therefore necessary to identify and fill the current gaps in the skills and abilities of nursing leaders through educational activities in institutions, underlining the importance of a two-way communication process and mutual trust between managers and nursing staff. The purpose of the review was to offer an overview of a current topic, as both job satisfaction and transformational leadership are two fundamental issues for the creation of a healthy and efficient work environment. Despite the fact that leadership quality and job satisfaction can be assessed using proven and generalizable measurement tools, few studies adopt such methods, and they thus fail to draw conclusions from the relationship between pertinent variables. For the future, the authors suggest conducting studies that can correlate transformational leadership and job satisfaction to obtain more generalizable results because these issues are based much more on empirical experience than on robust scientific evidence.
Limitations of the study
Although the research met the objective of this study, the review has limitations. For example, one of the limitations of a narrative review concerns the methodology itself; whereas a systematic review has a clear and obligatory a priori methodology, the narrative review approach lacks a research protocol. Another limitation is the interpretation bias of the results, which can bring to light only a part of the chosen topic. To confirm what has been described in this review, other studies are needed that can obtain certain, reproducible and generalizable results. In addition, the results that emerged from the other studies were evaluated by means of self-assessment questionnaires, which are frequently associated with response bias.
Funding
This study did not receive any form of funding.
Conflict of interest
The authors declare that they have no conflicts of interest associated with this study.
REFERENCES
[1] Huber D. Leadership and Nursing Care Management. 3rd ed. Saunders Elsevier, Philadelphia PA: 2006.
[2] Frisicale EM, Grossi A, Ccacciatore P, Carini E, Villani L, Pezzullo AM, et al. The need of leadership in managing healthcare and policy-making - G. Ital. Health Technol. Assess. 2019.
[3] Cleary M, Horsfall J, Jackson D, Muthulakshmi P, Hunt GE. Recent graduate nurse views of nursing, work and leadership. J Clin Nurs 2013;22:2904–11. https://doi.org/10.1111/jocn.12230.
[4] Mannix J, Wilkes L, Daly J. ‘Watching an artist at work’: aesthetic leadership in clinical nursing workplaces. J Clin Nurs 2015;24:3511–8. https://doi.org/10.1111/jocn.12956.
[5] Casida J, Parker J. Staff nurse perceptions of nurse manager leadership styles and outcomes: Nurse manager leadership styles and outcomes. J Nurs Manag 2011;19:478–86. https://doi.org/10.1111/j.1365-2834.2011.01252.x.
[6] Laschinger HKS, Wong CA, Cummings GG, Grau AL. Resonant leadership and workplace empowerment: the value of positive organizational cultures in reducing workplace incivility. Nurs Econ 2014;32:5–15, 44; quiz 16.
[7] Al-Yami M, Galdas P, Watson R. Leadership style and organisational commitment among nursing staff in Saudi Arabia. J Nurs Manag 2018;26:531–9. https://doi.org/10.1111/jonm.12578.
[8] Cummings GG, Tate K, Lee S, Wong CA, Paananen T, Micaroni SPM, et al. Leadership styles and outcome patterns for the nursing workforce and work environment: A systematic review. Int J Nurs Stud 2018;85:19–60. https://doi.org/10.1016/j.ijnurstu.2018.04.016.
[9] Umrani WA, Afsar B. How transformational leadership impacts innovative work behaviour among nurses. Br J Healthc Manag 2019;25:1–16. https://doi.org/10.12968/bjhc.2018.0069.
[10] Madathil R, Heck NC, Schuldberg D. Burnout in Psychiatric Nursing: Examining the Interplay of Autonomy, Leadership Style, and Depressive Symptoms. Arch Psychiatr Nurs 2014;28:160–6. https://doi.org/10.1016/j.apnu.2014.01.002.
[11] Robbins B, Davidhizar R. Transformational Leadership in Health Care Today. Health Care Manag 2020;39:117–21. https://doi.org/10.1097/HCM.0000000000000296.
[12] Lievens I, Vlerick P. Transformational leadership and safety performance among nurses: the mediating role of knowledge-related job characteristics. J Adv Nurs 2014;70:651–61. https://doi.org/10.1111/jan.12229.
[13] Spies LA, Gray J, Opollo JG, Mbalinda S, Nabirye R, Asher CA. Transformational leadership as a framework for nurse education about hypertension in Uganda. Nurse Educ Today 2018;64:172–4. https://doi.org/10.1016/j.nedt.2018.02.009.
[14] Locke EA. “Job satisfaction reconsidered”: Reconsidered. Am Psychol 1978;33:854–5. https://doi.org/10.1037/0003-066X.33.9.854.
[15] De Simone S, Planta A, Cicotto G. Il ruolo delle capacità agentiche nelle intenzioni di turnover del personale infermieristico 2018.
[16] Khamisa N, Oldenburg B, Peltzer K, Ilic D. Work related stress, burnout, job satisfaction and general health of nurses. Int J Environ Res Public Health 2015;12:652–66. https://doi.org/10.3390/ijerph120100652.
[17] Yang F-H, Wu M, Chang C-C, Chien Y. Elucidating the Relationships among Transformational Leadership, Job Satisfaction, Commitment Foci and Commitment Bases in the Public Sector. Public Pers Manag 2011;40:265–78. https://doi.org/10.1177/009102601104000306.
[18] Aiken LH, Clarke SP, Sloane DM, Lake ET, Cheney T. Effects of hospital care environment on patient mortality and nurse outcomes. J Nurs Adm 2008;38:223–9. https://doi.org/10.1097/01.NNA.0000312773.42352.d7.
[19] Haddaway NR, Page MJ, Pritchard CC, McGuinness LA. PRISMA2020: An R package and Shiny app for producing PRISMA 2020-compliant flow diagrams, with interactivity for optimised digital transparency and Open Synthesis. Campbell Syst Rev 2022;18:e1230. https://doi.org/10.1002/cl2.1230.
[20] Munn Z, Barker TH, Moola S, Tufanaru C, Stern C, McArthur A, et al. Methodological quality of case series studies: an introduction to the JBI critical appraisal tool. JBI Database Syst Rev Implement Rep 2019;Publish Ahead of Print. https://doi.org/10.11124/JBISRIR-D-19-00099.
[21] Abdelhafiz IM, Alloubani AM, Almatari M. Impact of leadership styles adopted by head nurses on job satisfaction: a comparative study between governmental and private hospitals in Jordan. J Nurs Manag 2016;24:384–92. https://doi.org/10.1111/jonm.12333.
[22] Barlow KM. A Meta-Analysis of Transformational Leadership and Subordinate Nursing Personnel Organizational Commitment, Job Satisfaction, and Turnover Intentions. University of Maryland, Baltimore, 2013.
[23] Boamah SA, Spence Laschinger HK, Wong C, Clarke S. Effect of transformational leadership on job satisfaction and patient safety outcomes. Nurs Outlook 2018;66:180–9. https://doi.org/10.1016/j.outlook.2017.10.004.
[24] Borman e Abrahason. Do staff nurse perceptions of nurse leadership behaviors influence staff nurse job satisfaction? The case of a hospital applying for Magnet® designation. J Nurs Adm 2014;44:219–25. https://doi.org/10.1097/NNA.0000000000000053.
[25] Choi SL, Goh CF, Adam MBH, Tan OK. Transformational leadership, empowerment, and job satisfaction: the mediating role of employee empowerment. Hum Resour Health 2016;14:73. https://doi.org/10.1186/s12960-016-0171-2.
[26] Labrague LJ, Nwafor CE, Tsaras K. Influence of toxic and transformational leadership practices on nurses’ job satisfaction, job stress, absenteeism and turnover intention: A cross-sectional study. J Nurs Manag 2020;28:1104–13. https://doi.org/10.1111/jonm.13053.
[27] Lapeña LFR, Tuppal CP, Loo BGK, Abe KHC. Transformational and Transactional Leadership Styles of Nurse Managers and Job Satisfaction among Filipino Nurses: A Pilot Study. Nurse Media J Nurs 2017;7:65–78.
[28] Libano MC. Registered Nurse Job Satisfaction and Nursing Leadership. Regist Nurse Job Satisf Nurs Leadersh 2017:1–1.
[29] Morsiani G, Bagnasco A, Sasso L. How staff nurses perceive the impact of nurse managers’ leadership style in terms of job satisfaction: a mixed method study. J Nurs Manag 2017;25:119–28. https://doi.org/10.1111/jonm.12448.
[30] Negussie N, Demissie A. Relationship between leadership styles of nurse managers and nurses’ job satisfaction in Jimma University Specialized Hospital. Ethiop J Health Sci 2013;23:49–58.
[31] Specchia ML, Cozzolino MR, Carini E, Di Pilla A, Galletti C, Ricciardi W, et al. Leadership Styles and Nurses’ Job Satisfaction. Results of a Systematic Review. Int J Environ Res Public Health 2021;18. https://doi.org/10.3390/ijerph18041552.
[32] Wang X, Chontawan R, Nantsupawat R. Transformational leadership: effect on the job satisfaction of Registered Nurses in a hospital in China. J Adv Nurs John Wiley Sons Inc 2012;68:444–51. https://doi.org/10.1111/j.1365-2648.2011.05762.x.
[33] Alshahrani FM, Baig LA. Effect of Leadership Styles on Job Satisfaction Among Critical Care Nurses in Aseer, Saudi Arabia. J Coll Physicians Surg--Pak JCPSP 2016;26:366–70.
[34] AbuAlRub RF, Alghamdi MG. The impact of leadership styles on nurses’ satisfaction and intention to stay among Saudi nurses. J Nurs Manag 2012;20:668–78. https://doi.org/10.1111/j.1365-2834.2011.01320.x.
[35] Brewer CS, Kovner CT, Djukic M, Fatehi F, Greene W, Chacko TP, et al. Impact of transformational leadership on nurse work outcomes. J Adv Nurs 2016;72:2879–93. https://doi.org/10.1111/jan.13055.
[36] Roberts-Turner R, Hinds PS, Nelson J, Pryor J, Robinson NC, Wang J. Effects of leadership characteristics on pediatric registered nurses’ job satisfaction. Pediatr Nurs 2014;40:236–41, 256.
[37] Al-Hussami M. Study of nurses’ job satisfaction: The relationship to organizational commitment, perceived organizational support, transactional leadership, transformational leadership, and level of education. Eur J Sci Res 2008;22:286–95.
[38] Bass BM, Avolio BJ. Developing Transformational Leadership: 1992 and Beyond. J Eur Ind Train 1990;14. https://doi.org/10.1108/03090599010135122.
[39] Bass BM, Avolio BJ. Multifactor leadership questionnaire: Manual and sample set (3rd ed.). 3rd ed. 2004.
[40] Lautizi M, Laschinger HKS, Ravazzolo S. Workplace empowerment, job satisfaction and job stress among Italian mental health nurses: an exploratory study. J Nurs Manag 2009;17:446–52. https://doi.org/10.1111/j.1365-2834.2009.00984.x.
[41] Spence Laschinger HK, Finegan J, Wilk P. Context Matters: The Impact of Unit Leadership and Empowerment on Nurses’ Organizational Commitment. JONA J Nurs Adm 2009;39:228–35. https://doi.org/10.1097/NNA.0b013e3181a23d2b.
[42] Pineau Stam LM, Spence Laschinger HK, Regan S, Wong CA. The influence of personal and workplace resources on new graduate nurses’ job satisfaction. J Nurs Manag 2015;23:190–9. https://doi.org/10.1111/jonm.12113.
[43] Boamah S, Laschinger H. Engaging new nurses: the role of psychological capital and workplace empowerment. J Res Nurs 2015;20:265–77. https://doi.org/10.1177/1744987114527302.
[44] Cai C, Zhou Z. Structural empowerment, job satisfaction, and turnover intention of Chinese clinical nurses. Nurs Health Sci 2009;11:397–403. https://doi.org/10.1111/j.1442-2018.2009.00470.x.
[45] Tellez M. Work satisfaction among California registered nurses: a longitudinal comparative analysis. Nurs Econ 2012;30:73–81.
[46] Çelik S, Hisar F. The influence of the professionalism behaviour of nurses working in health institutions on job satisfaction: Professionalism behaviour of nurses. Int J Nurs Pract 2012;18:180–7. https://doi.org/10.1111/j.1440-172X.2012.02019.x.
[47] Ingersoll GL, Olsan T, Drew-Cates J, DeVinney BC, Davies J. Nurses’ Job Satisfaction, Organizational Commitment, and Career Intent: JONA J Nurs Adm 2002;32:250–63. https://doi.org/10.1097/00005110-200205000-00005.
![]() This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Patients’ preferences, feelings, and benefits on Music-Based Intervention: A Pilot Study in COVID-19 Hospitalization
Alessio Pesce 1, Francesca Lantieri 2
- Department of Internal Medicine, Local Health Authority ASL2, Savona (Italy)
- Department of Health Science, Biostatistics Unit, University of Genoa, (Italy)
* Corresponding author: Dr. Alessio Pesce, Department of Internal Medicine, Local Health Authority ASL2, Savona (Italy), Piazza Sandro Pertini n. 10, 17100 Savona, Italy.
Email: alessio.pesce@uniupo.it, ORCID: https://orcid.org/0000-0003-2702-4101
Cite this article
ABSTRACT
Introduction: COVID-19 patients survive in isolation with stringent measures of infection containment, leading to anxiety, fear, stress, loneliness, and depression. Music is recognized as useful to promote multiple health outcomes, including anxiolytic effects, pain-relieving, and relaxing effects that favour well-being and social interaction in healthcare settings.
Objective: This study aimed to determine the impact of a pre-recorded music-based intervention on the music perception in hospitalized COVID-19 patients. Music appreciation, evoked emotions, and self-reported effects were explored and compared before and after music-based intervention, also considering the gender of the patients.
Methods: This prospective study consisted of a pre-recorded music-based intervention administered to 272 patients hospitalized for COVID-19 by piping the music into rooms of inpatient medical area. Pre-recorded musical pieces of were selected by a music therapist considering specific formal and parametric characteristics, with the purposes of distraction, entertainment, relaxation, and emotional support. The patients’ opinions were collected using an ad hoc self-report questionnaire and a short data survey that followed the Consolidated Framework for Implementation Research (CFIR) guidelines.
Results: Music resulted to be the preferred entertainment activity during hospitalization by 84.6% of patients, with 96.6% of them expecting a positive effect and a very high grade of usefulness attributed to music before hospitalization and even higher afterwards. The music intervention significantly changed the patients’ perception of music from everyday life to hospitalization (p<0.0001). It proved successful in evoking pleasure and fun, which raised from 18.4% of everyday life to 41.1% during hospitalization. The usefulness of listening music to alleviate unpleasant feelings including anxiety, fear, loneliness, and low mood in COVID-19 disease, had a significant increase from 22.5% to 60.0% after the music intervention.
Conclusion: Music-based intervention, directed according to reference frameworks, provides self-reported social and emotional support in hospitalized patients for COVID-19.
Keywords: Covid-19, music therapy, emotions, hospitalization, music medicine
INTRODUCTION
Music represents an interdisciplinary topic, transversal to medicine and the human sciences. It constitutes a non-pharmacological intervention aimed at multiple health outcomes, including anxiolytic, pain-relieving, and relaxing effects that promote well-being, sleep quality and social interaction in healthcare settings [1-7]. Hospitalized patients with COVID-19 survive in isolation with stringent infection containment measures, which lead to anxiety, fear, stress, loneliness, and depression, even to the point of evoking obsessive thoughts; in the most severe cases they compromise the prognosis, increasing mortality and adverse events. Music-based interventions, therefore, can also be used in psycho-social need in COVID-19 patients [1]. To date, research protocols are available in the hypothesis that music can reduce anxiety, depression or improve the quality of life in COVID-19 patients [8]. Therefore, studies to explore patients’ perspectives and determine the effects of music-based intervention during hospitalization are needed to provide scientific evidence. Some authors [9] remark how essential the compatibility of musical pieces with people’s preferences is and how these may vary depending on expectations at a specific moment, health conditions, or the healthcare environment. A crucial aspect in music-based interventions is the proper selection of musical pieces. Listening to specific types/genres of favorite music or sounds is likely to have an emotional impact based on patients’ clinical conditions. Systematic reviews show that patients’ music background and listening habits have been drastically underestimated, reported in only 7.7% of the studies conducted [10]. Only about 25% of studies have explored patient feedback on musical [10]. Personality plasticity, cognitive-affective components [11] and the clinical conditions of patients, especially respiratory system efficiency and symptom aggravation, show a close correlation with music preferences [9], stated even before COVID-19 disease. Therefore, it is crucial to explore the in-patients’ music preferences, the utility that listening to music might have for them, and their feelings also in relation to COVID-19 before starting a music-based intervention. This knowledge would allow health and music professionals to personalize the intervention and be able to demonstrate important correlations between habitual musical preferences and attitudes with those experienced by the patient as a result of listening to music. The literature generally admits methodological weaknesses in music-based interventions [10,12]. There is a lack of scientific rigor in music selection, in the involvement of music experts, and in reporting and describing the music pieces used [12]. Furthermore, music has rarely been selected to achieve specific effects according to the reference frameworks [10,12]. The opportunity to identify music mechanisms of action would allow researchers to advance beyond basic questions about efficacy and begin to answer questions about how, why, and for whom an intervention works [12]. For these reasons, we applied a music-based intervention to in-patients affected by COVID-19 after pre-inquiring their music preferences and have administered a questionnaire to investigate their appreciation for music both before and after the intervention. The music-based intervention was selected by a music therapist and integrated according to guidelines and [13] a consolidated framework [14].
Objective
This study aimed to determine the impact of a pre-recorded music-based intervention on the music perception in hospitalized COVID-19 patients. Music appreciation, evoked emotions, and self-reported effects were explored and compared before and after the music-based intervention, also considering the gender of the patients.
MATERIALS AND METHODS
Sample Recruitment and Clinical Setting
All adult patients with COVID19 admitted to the COVID-19 inpatient medical area of the Italian hospital Santa Maria Misericordia (Local Health Authority ASL2, Savona), between May 18, 2020 and February 18, 2022 were recruited. The inclusion criteria were age 18 years or older, ability to understand, write and speak Italian, and written consent to the study. Patients with severe hearing and visual deficits, and with alterations of the state of consciousness, as assessed by the medical-nursing staff, were excluded. No exclusion criteria based on covid severity were applied. According to Italian rules at that period, no COVID-19 patient received visits from friends or family members during hospitalization. The study was conducted in accordance with the 1964 Helsinki Declaration and was approved by the Ethics Committee (May 18, 2020 – Protocol Number 10459); informed consent was obtained from all participants included in the study.
Study Design
This prospective study consisted of a pre-recorded music-based intervention and the administration of a questionnaire aimed at determining the perception of music in patients hospitalised for COVID-19, and their point of view on music listening in terms of their attitude toward music and the set of sensation associated to listening the music, during hospitalization, before and after the music intervention. Patients, upon their acceptance to participate in the study, were received an ad hoc self-report questionnaire and a short data survey, both in paper form. The questionnaire included 15 pre-treatment questions regarding the patients’ attitude toward music in their everyday life and in the hospital setting and 3 post-treatment questions to be answered after the music treatment. The patients were instructed to fill in in only the pre-intervention questions before the music treatment and to complete the rest of the forms only after the music intervention. The afternoon following admission, a single 90-minute length music-based intervention was introduced in the in-patient rooms via piped music. On the same day, following the musical presentation, the two data sheets were collected. Patients who agreed to participate to the study but refused the music-based intervention due to their choice or clinical worsening, were still invited to fill in Q1-Q15 and short data record at their convenience or after the improvement of their health conditions (Figure 1).

Figure 1. Flowchart of the study
Criteria for constructing the questionnaire
The present questionnaire was specifically constructed for this study to explore preferences, diffusion modes, utility, emotions evoked, and self-reported effects, also considering the gender, and to compare the point of view during hospitalization with what described by the patient after the music-based intervention. A preliminary questionnaire was constructed in 2013 and used for the first time on a sample of 55 patients to evaluate the point of view on habitual music listening and in hospitalization for cardiac catheterization [15]. The meaningful constructs, facade preferences and response categories that emerged from this previous study guided the initial design of the items for the present study. Based on this, an updated questionnaire was developed in 2020 following the adoption of the Consolidated Framework for Implementation Research (CFIR) to integrate a music-based intervention. According to the CFIR framework, to embody music into the hospitalization through piped music, it is necessary to explore the possibility of integrating music into the in-patient setting.
The purpose was to 1) understand the general appreciation and practical feasibility of the musical introduction, 2) explore the point of view of operators and patients to define the modalities of integration in the healthcare setting and 3) investigate listening preferences before the experimentation. To this aim, the updated questionnaire, preliminary to the present one, was submitted to all the 33 healthcare professionals and to a limited sample of 25 patients before the start of the experimentation. They were asked to give their opinion on the questionnaire and fill in two short surveys to assess the overall comprehensibility of the questionnaire and collect the suggestions from patients and health professionals, aimed at improving the form and content of the questionnaire. Based on scientific evidence from the literature [1-7,10,12], the frameworks on music selection, and the suggestions that had emerged from patients and operators in the preliminary investigation, the final questionnaire was declined and then submitted to the different sample of 267 patients of the present study, together with the short survey. The final questionnaire, specifically constructed for this study, consists of 18 questions. The questionnaire is structured in two sections, the first, pre-intervention, with the aim of exploring the patient’s habitual (8 questions, T0) and hospitalization perceptions (7 questions, T1) and the second to explore the patient’s experience after the music-based intervention (3 questions, T2). For questions 1 to 18 the participants can choose one of the predefined answers that best describes his or her point of view, with the possibility, for eleven of these questions, to enter open answers different from the predefined ones. Socio-demographic data (nationality, sex) were collected by the short data survey that was administered by a separate sheet and that include the overall evaluation of the questionnaire by the participant. This short survey also includes the pre-post opinions about the music intervention through 5 Point Likert Scale Questions (1: strongly disagree, 2: disagree, 3: neither agree nor disagree, 4: agree, 5: strongly agree).
Intervention
A pre-recorded music-based intervention was developed in the pre-experimental phase when the preliminary version of the questionnaire was developed. During this phase, musical genres of patients’ preference on admission were explored. A music therapist structured an intervention based on the opinions of 25 patients. The music-based experimentation was designed using specific theoretical frameworks for music selection [10] and reporting intervention quality guidelines [13]. Pre-recorded pieces of music were selected considering specific formal and parametric characteristics with the purposes of distraction, entertainment, relaxation, and emotional support. The selection criteria, declined through the intervention reporting checklists by Robb SL et al. [13] reported on the Equator Network are detailed in Table 1. The piped music was transmitted into the single room of patient participating to the study via a player and an amplifier located in a workstation isolated from the COVID-19 wards. Ceiling speakers were used to prevent contamination through portable music players/earphones and in consideration of the poor management of portable devices or musical instruments due to medical ventilation devices.


Table 1. Music-Based Intervention
Statistical Analysis
Categorical data are reported as counts (N) and percentages (%) with 95% confidence intervals (95%CI, binomial exact calculation). We applied the Cramer’s V test to investigate if the usually preferred genre of music (classical, Italian, foreign language, etc.) correlated with the preferences during hospitalization (Q3 vs Q13). Categorical variants were compared by Chi-square test or by Fisher’s exact test when more appropriate. In particular, the Fisher’s exact test was applied to explore if the emotional effects (relaxation, happiness, crave, etc.) were different between what expected in usual settings and what was expected during hospitalization (Q8 vs Q17). The Fisher exact test was also used to compare if patients enjoyed music and the reasons why they listened to music (the utility of the music in terms of kind of sensations achieved: amusement, relief, etc.) in the three settings: usual life vs what expected during hospitalization vs what actually felt during hospitalization (Q1 vs Q14 vs Q16, and Q7 vs Q12 vs Q18, respectively). These tests were confirmed by the Cochrane Q test to compare more than two groups for a binary outcome when considering only the two categorical “yes” or “no” answers. Also, the differences between females and males were investigated through the Fisher’s exact test, as well as the association between the genre of music preferred during the hospitalization and the emotional effect and the utility in terms of sensation achievement. Finally, the level of appreciation of music measured by the Likert questions was compared before and after the music intervention by the Wilcoxon test, while the correlation was estimated by Spearman’s rho; the differences between males and females were tested by the Mann-Whitney test. All tests were two tailed and considered significant with p-value (p) <0.05. Data were analyzed using 24.0 SPSS Software.
RESULTS
Analyzed Sample and Baseline patients’ characteristics
Two hundred and seventy-two patients met the eligibility criteria, however five refused to participate in the study, declining the proposal because they did not want to answer the questions on the questionnaire. Among the participating patients, two refused the music-based intervention after answering the first questions of the questionnaire; one due to clinical aggravation and the other due to the need for rest. The flowchart of the study is depicted in Figure 1. Patients were mostly Italian (94.4%), 59.6% were males. For 95.1% of the participants, the questionnaire had a good (66.8%) or complete intelligibility (28.3%). Only 4.9% believed that the questions were fairly comprehensible. Answers regarding the usual everyday life are described in Table 2 (Q1-Q8). Usually, patients listened to music to get a pleasant distraction (69.7%) or to relieve from negative feelings (22.5%) and what achieved from listening to music was relax (41.6%) or leisure (18.4%).


Table 2. Habitual listening to music
Preferences specific to the hospitalization
Most of patients at the time of hospitalization would have preferred listen to music (84.6%) rather than other activities such as reading, watching TV, etc. Accordingly, the patients declared they would like to listen to music during hospitalization (95.5%), granting that it would have a positive effect on them (96.6%), mainly through piped music (93.3%), and without any distinction in administration time (85.4%) (Table 3 Q9-Q15). The genre of music habitually listened highly correlated with the one desired during hospitalization (Cramer’s V = 0.928, p<0.0001), with only 6 patients preferring a genre of music different from the one usually preferred.


Table 3. Views on music listening during hospitalization.
Perceptions experienced after music-based intervention
Answers given after the music treatment are reported in comparison with answers given before the treatment (Table 4). Patients who appreciated listening to music increased from 93.6% of the everyday life, to 95.5% in their perception of hospitalization, and up to 98.5% after hospitalization (Q1, Q14 and Q16), although the latter percentage is slightly inflated by the fact that two patients who didn’t habitually like music refused the music treatment and therefore did not answer to the post treatment questions (Table 4). These differences reached the statistical significance when comparing “yes” vs “I do not know” across the three periods (the only two “no” answers were missing at the post treatment, Cochran’s Q= 13.0, df=2, p=0.0015). According to the high percentage of patients declaring that they liked music, the degree of usefulness attributed to music was very high both before and after hospitalization (median= 4 in both, on a score from 1 to 5) (Table 4). There were high and significant correlations between the two (Spearman’s rho=0.631, p<0.0001) and difference between the two periods did not reach the statistical significance (Wilcoxon Signed Ranks Test Z = -1.821, p=0.0687), although 23 patients gave a score below 4 before hospitalization (8.6%, two patients scored 1, one scored 2 and 20 scored 3), who reduced to only 9 patients giving a score of 3 (3.4%). The emotional effects usually conveyed by music were significantly different from those conveyed during hospitalization (Q8 vs Q17, p<0.0001), with happiness falling from 17.2% to 8.7% and excitement from 9.4% to 0, while amusement/entertainment raised from 18.4% to 41.1% (Table 4). Also, the reasons why the patients listened to music changed from the usual habits to the idea the patients had about hospitalization and to what they have actually perceived during the hospitalization (Q7 vs Q12 vs Q18, p<0.0001): pleasant distraction went from 69.7% to 55.8% to 38.7%, while relief went from 22.5% to 35.2% to 60.0% (Table 4). Only 80 patients chose the same reasons for the three periods, mostly (90.0%) desired music for pleasant distraction.


Table 4. Perceptions experienced after music-based intervention.
Not surprisingly, the music treatment was appreciated especially by the patients who preferred listening to music rather than other activities such as reading, watching TV, etc.: all the 266 patients that had declared they would have liked listening to music appreciated the treatment, while 4 patients out of 39 that would have rather preferred other entertainment activities were then not sure about the music treatment (p<0.0001). However, the patients who preferred other activities were mainly satisfied by the music treatment. Finally, there were some differences between males and females (Table 5). In particular, males tended to habitually listen to music more than females (96.2% vs 88.0%, p=0.0161) and through different playback sources (p<0.0001), in particular males preferred radio and females preferred television. Females usually tended to listen to music more to get a pleasant distraction, achieving relaxing sensations while males more to get relief from negative feelings (p<0.0001), achieving leisure (p<0.0001). Of note the answers specific to hospitalization showed, at opposite, that females were more expecting to get relief, while males were more expecting to get a pleasant distraction (p<0.0001), a trend confirmed at the post treatment evaluation (p<0.0001).
Females rated the utility of listening to music slightly less than males as for their hospitalization expectance (p=0.0330, Mann-Whitney test), but without any difference at the post treatment evaluation, when at opposite their appreciation was even higher than those by males, although not significantly different (Table 5).


Table 5. Gender Differences to questionnaire responses
DISCUSSION
This pilot study aimed to determine the impact of a pre-recorded music-based intervention on music perception in patients hospitalized for COVID-19. This study, in line with others [16], describes an almost total appreciation for music in everyday life. The COVID-19 patients included in this study liked music even more in the perspective of hospitalization, with a further increase in the overall liking after the music-based intervention. Particularly, this observation emerged in females with a 99.1% of appreciation and a reduction from 6.5% to 0.9% of undecided/negative answers after the treatment. This implies that the musical listening confirmed and exceeded the usual expectations towards music, particularly in females, who showed a slightly lower preference for music than males in their habitual life. This observation provides support for the importance of music presence during hospitalization and potential benefits in COVID-19 patients. This study also shows that habitual preferences are closely related to those in the in-patient setting and should therefore be considered in order to direct music-based interventions [10,12-14]. The preference for Italian pop music reflects the cultural and musical background of the participants, considering their Italian origins and the high average age. Regardless of the usual musical medium, and in line with other studies [22], participants preferred piped music in the in-patient setting, while only 0.7% and 4.9% of them liked live music or music via earphones, respectively. It is conceivable that piped music represents a socially accepted medium in the care setting and that live music may represent an unrealistic novelty, especially given the restrictions and isolation during hospitalization. However, it must also be considered that the use of medical devices such as masks or helmets for ventilation makes it difficult or impossible to set up a system of music diffusion via earphones. Likewise, there are further complications in the hygienic handling of diffusion devices/music instruments in a COVID-19 environment, which must ensure minimal contamination of surfaces by microorganisms [23]. These limitations might have mitigated, in fact, the clear preference for piped music. The habitual listening to music was shown to find its place in numerous daily life activities (during free time, sports, or work). Similarly, the patients were willing to enjoy music at any time during hospitalization, being the preferred entertainment activity in hospital compared to other proposals, such as reading, watching TV, or taking drugs to relax. This may suggest the possibility to extend music not only to the in-patient rooms but also to the corridors, to the rooms used for clinical care services, and to the common spaces. The experimental intervention impacted the perception of the effects attributed to music. Feelings of pleasure and enjoyment were experienced by more than double the participants compared to the usual condition. Not surprisingly given the patients’ situation, happiness and joy decrease from 17.2% to 8.7% and the exciting/energizing effect was not perceived by anyone post-intervention. Similarly, the reasons that motivated the patients to listen to music were significantly different between everyday life, the hospitalization perspective, and the post intervention. The usefulness of listening music to alleviate unpleasant feelings including anxiety, fear, loneliness, and low mood had a significant increase after the music intervention. Furthermore, the degree of usefulness experienced with the intervention was greater than that usually perceived, even if the very high level of appreciation already in everyday life did not allow us to detect a statistically significant increase. No participant experienced little or no benefit from the intervention. The pre-recorded music was specifically designed according to general patient preferences and frameworks for entertainment and mood improvement, considering the need for emotional support in disease. In the literature, for example, it has been widely demonstrated that musical rhythms between 60 and 80 bpm or the use of musical instruments that are tuned to A432(Hz) can assist physical and emotional relaxation with a decrease in sympathetic nervous system activity, thus decreasing adrenergic activity, neuromuscular arousal, cardiovascular and respiratory rhythms, tension, metabolic rate, gastric acidity, motility, and sweat gland activity [10]. In this study, in line with findings in the literature, the effects of music listening can be traced back to the rationale with which the music was selected [10]. In fact, music selected to promote distraction, relaxation, entertainment and emotional support predominantly elicited relaxation and pleasure, recognised to distract, and alleviate unpleasant feelings such as anxiety, fear and stress. To confirm this, sadness, melancholy, love, nostalgia, and pride were evoked to a limited extent by listening to music. These findings support the directionality of the music-based intervention according to specific frameworks. Scientific rigour in music selection, the involvement of music experts, and the use of reporting guidelines can determine specific listener-perceived effects and allow for adequate replicability of the intervention. These data are in line with other studies that suggest that music-based intervention induced greater satisfaction and compliance in the patient pathway [18]. Awareness and recognition of the usefulness of music by the patient can in fact mitigate the decision-making processes of care and self-care. Structural changes can improve the environment and even encourage interaction between operators and patients [24]. However, economic, and organizational aspects must be considered in order to integrate this kind of service. In this study, the design of a piped intervention based on pre-recorded music tracks, according to scientific frameworks, required limited costs for the music setting by a professional and the copyright licenses, given that the in-patient area already had ceiling-mounted audio diffusion media. Also considering that the use of the music playback devices avoided any risk of infection from contamination, the safety of the intervention, in addition to the cost-effectiveness, was evident. Other studies have already amply demonstrated the benefits in terms of cost-effectiveness in multiple contexts and with different music playing methods [25,26].
CONCLUSION
This pilot study explored in-patients’ preferences, utility that comes from music, usages, and expectation from the effect of music in COVID-19 patients, before and after music-based intervention, and was carried out in response to a lack of studies in the literature and methodological weaknesses of publications. In this study, music was the most welcome activity during the hospitalization. The experimental intervention, directed according to reference frameworks, significantly impacted on the utility, on the evoked emotions, and on the self-reported effects of music during hospitalization for COVID-19. This result provides support for the intervention with pre-recorded music as an integrated standard in treatment protocols to meet the need for social and emotional support in hospitalized patients for COVID-19 and possibly in similar settings of hospitalization in isolation.
Limitations
It was not possible to recruit patients younger than forty years of age. This made it impossible to evidence some generational differences between the participants. A similar consideration regards the lack of heterogeneous in nationality. In addition, participants could not enjoy parental visits during their hospital stay due to COVID-19 restrictions, limiting the comparison with the more general situation of parental social support. Other clinical variables such as anxiety levels, loneliness in the healthcare relationship [27,28], psycho-physical distress and respiratory complications, which could have impacted the perception of the music experienced, were not considered. In the literature, there is ample evidence that patients with high levels of anxiety and distress obtained greater benefit from music [1,3,6,18,29-32], so although the aim of this study was not to measure changes in health outcomes, a correlation between high levels of psycho-physical distress on admission and musical perceptions related to the need to alleviate unpleasant feelings is likely. Preferences, beliefs, and attitudes towards the different genre of music, also in the context of socio-demographic characteristics should lead future study. The catchiness, use of melody, rhythm, and ease to understand of lyrics should be explored as well. Future randomised controlled trials using the same framework should be considered, to determine its effects on healthcare outcomes in multiple populations with similar needs for social and emotional support. The appropriate use of music may also be aimed at improving recovery time and reducing the need for medication to treat COVID19-induced psycho-physical distress [1,33,34]. Hopefully future studies will consider patients’ perceptions as a crucial factor in determining the specific psychophysical effects of music. Based on this knowledge it will be possible to structure, implement and systematically replicate music in healthcare environment.
Funding statement
This research did not receive any specific grant from funding agencies in the public, commercial, or not for profit sectors.
Conflict of interest
The authors report no conflict of interest.
Authors’ contribution
Dr. Alessio Pesce: Conceptualization, Methodology, Writing- Original draft preparation, Visualization, Investigation, Validation, Writing- Reviewing and Editing.
Department of Internal Medicine, Local Health Authority ASL2, Savona (Italy), Piazza Sandro Pertini n. 10, 17100 Savona, Italy. Tel: +39 340 7114674. E-mail: alessio.pesce@uniupo.it; ORCID: https://orcid.org/0000-0003-2702-4101
Dr. Francesca Lantieri: Software, Data curation, Visualization, Investigation, Supervision, Validation, Writing- Reviewing and Editing.
Department of Health Science, Biostatistics Unit, University of Genoa, Italy, via Pastore 1, 16132 Genova, Italy. E-mail: f.lantieri@unige.it; ORCID: https://orcid.org/0000-0002-8923-0165
Acknowledgements
We want to thank the staff of the Internal Medicine department at the dedicated Covid-19 hospital in Albenga, and Dr. Letizia Ceravolo for revising the English-language manuscript.
REFERENCES
- Chen X, Li H, Zheng X, Huang J. Effects of music therapy on COVID-19 patients’ anxiety, depression, and life quality: A protocol for systematic review and meta-analysis. Medicine (Baltimore). 2021 Jul 2;100(26): e26419. doi: 10.1097/MD.0000000000026419.
- Bradt J, Dileo C, Myers-Coffman K, Biondo J. Music interventions for improving psychological and physical outcomes in people with cancer. Cochrane Database Syst Rev. 2021 Oct 12;10(10):CD006911. doi: 10.1002/14651858.CD006911.pub4.
- Kakar E, Billar RJ, van Rosmalen J, Klimek M, Takkenberg JJM, Jeekel J. Music intervention to relieve anxiety and pain in adults undergoing cardiac surgery: a systematic review and meta-analysis. Open Heart. 2021 Jan;8(1):e001474. doi: 10.1136/openhrt-2020-001474.
- Boster JB, Spitzley AM, Castle TW, Jewell AR, Corso CL, McCarthy JW. Music Improves Social and Participation Outcomes for Individuals With Communication Disorders: A Systematic Review. J Music Ther. 2021 Mar 16;58(1):12-42. doi: 10.1093/jmt/thaa015.
- Cheng J, Zhang H, Bao H, Hong H. Music-based interventions for pain relief in patients undergoing hemodialysis: A PRISMA-compliant systematic review and meta-analysis. Medicine (Baltimore). 2021 Jan 15;100(2):e24102. doi: 10.1097/MD.0000000000024102.
- Gauba A, Ramachandra MN, Saraogi M, Geraghty R, Hameed BMZ, Abumarzouk O, Somani BK. Music reduces patient-reported pain and anxiety and should be routinely offered during flexible cystoscopy: Outcomes of a systematic review. Arab J Urol. 2021 Mar 3;19(4):480-487. doi: 10.1080/2090598X.2021.1894814.
- Kakar E, Venema E, Jeekel J, Klimek M, van der Jagt M. Music intervention for sleep quality in critically ill and surgical patients: a meta-analysis. BMJ Open. 2021 May 10;11(5):e042510. doi: 10.1136/bmjopen-2020-042510.
- Chen X, Li H, Zheng X, Huang J. Effects of music therapy on COVID-19 patients’ anxiety, depression, and life quality: A protocol for systematic review and meta-analysis. Medicine (Baltimore). 2021 Jul 2;100(26):e26419. doi: 10.1097/MD.0000000000026419.
- Sliwka A, Pilinski R, Przybyszowski M, Pieniazek M, Marciniak K, Wloch T, Sladek K, Bochenek G, Nowobilski R. The influence of asthma severity on patients’ music preferences: Hints for music therapists. Complement Ther Clin Pract. 2018 Nov;33:177-183. doi: 10.1016/j.ctcp.2018.10.005.
- Williams C, Hine T. An investigation into the use of recorded music as a surgical intervention: A systematic, critical review of methodologies used in recent adult controlled trials. Complement Ther Med. 2018 Apr;37:110-126. doi: 10.1016/j.ctim.2018.02.002.
- Greenberg DM, Baron-Cohen S, Stillwell DJ, Kosinski M, Rentfrow PJ. Musical Preferences are Linked to Cognitive Styles. PLoS One. 2015 Jul 22;10(7):e0131151. doi: 10.1371/journal.pone.0131151.
- (1) Robb SL, Hanson-Abromeit D, May L, Hernandez-Ruiz E, Allison M, Beloat A, Daugherty S, Kurtz R, Ott A, Oyedele OO, Polasik S, Rager A, Rifkin J, Wolf E. Reporting quality of music intervention research in healthcare: A systematic review. Complement Ther Med. 2018 Jun;38:24-41. doi: 10.1016/j.ctim.2018.02.008.
- (2) Robb SL, Burns DS, Carpenter JS. Reporting Guidelines for Music-based Interventions. Music Med. 2011 Oct;3(4):271-279. doi: 10.1177/1943862111420539.
- Carter JE, Pyati S, Kanach FA, Maxwell AMW, Belden CM, Shea CM, Van de Ven T, Thompson J, Hoenig H, Raghunathan K. Implementation of Perioperative Music Using the Consolidated Framework for Implementation Research. Anesth Analg. 2018 Sep;127(3):623-631. doi: 10.1213/ANE.0000000000003565.
- Pesce A. Music before undergoing cardiac catheterisation between preference and reality. A pilot study. Prof Inferm. 2021 Oct-Dec;74(4):272. doi: 10.7429/pi.2021.744272a.
- Cabedo-Mas A, Arriaga-Sanz C, Moliner-Miravet L. Uses and Perceptions of Music in Times of COVID-19: A Spanish Population Survey. Front Psychol. 2021 Jan 12;11:606180. doi: 10.3389/fpsyg.2020.606180.
- Alter DA, O’Sullivan M, Oh PI, Redelmeier DA, Marzolini S, Liu R, Forhan M, Silver M, Goodman JM, Bartel LR. Synchronized personalized music audio-playlists to improve adherence to physical activity among patients participating in a structured exercise program: a proof-of-principle feasibility study. Sports Med Open. 2015;1(1):23. doi: 10.1186/s40798-015-0017-9.
- Jayakar JP, Alter DA. Music for anxiety reduction in patients undergoing cardiac catheterization: A systematic review and meta-analysis of randomized controlled trials. Complement Ther Clin Pract. 2017 Aug;28:122-130. doi: 10.1016/j.ctcp.2017.05.011.
- Bradt J, Dileo C. Music interventions for mechanically ventilated patients. Cochrane Database Syst Rev. 2014;2014(12):CD006902. doi: 10.1002/14651858.CD006902.
- Makama JG, Ameh EA, Eguma SA. Music in the operating theatre: opinions of staff and patients of a Nigerian teaching hospital. Afr Health Sci. 2010 Dec;10(4):386-9.
- Graff V, Wingfield P, Adams D, Rabinowitz T. An Investigation of Patient Preferences for Music Played Before Electroconvulsive Therapy. J ECT. 2016 Sep;32(3):192-6. doi: 10.1097/YCT.0000000000000315.
- Lee KC, Chao YH, Yiin JJ, Chiang PY, Chao YF. Effectiveness of different music-playing devices for reducing preoperative anxiety: a clinical control study. Int J Nurs Stud. 2011 Oct;48(10):1180-7. doi: 10.1016/j.ijnurstu.2011.04.001.
- Folsom S, Christie AJ, Cohen L, Lopez G. Implementing Telehealth Music Therapy Services in an Integrative Oncology Setting: A Case Series. Integr Cancer Ther. 2021 Jan-Dec;20:15347354211053647. doi: 10.1177/15347354211053647.
- Drahota A, Ward D, Mackenzie H, Stores R, Higgins B, Gal D, Dean TP. Sensory environment on health-related outcomes of hospital patients. Cochrane Database Syst Rev. 2012 Mar 14;2012(3):CD005315. doi: 10.1002/14651858.CD005315.
- Chlan LL, Heiderscheit A, Skaar DJ, Neidecker MV. Economic Evaluation of a Patient-Directed Music Intervention for ICU Patients Receiving Mechanical Ventilatory Support. Crit Care Med. 2018 Sep;46(9):1430-1435. doi: 10.1097/CCM.0000000000003199.
- DeLoach Walworth D. Procedural-support music therapy in the healthcare setting: a cost-effectiveness analysis. J Pediatr Nurs. 2005 Aug;20(4):276-84. doi: 10.1016/j.pedn.2005.02.016.
- Pesce, A. Solitudine nella relazione di cura: un concetto dimenticato tra i fondamenti di cura. L’infermiere, (2020) 1–7
- Karhe L, Kaunonen M, Koivisto AM. Loneliness in Professional Caring Relationships, Health, and Recovery. Clin Nurs Res. 2018 Feb;27(2):213-234. doi: 10.1177/1054773816676580.
- Bradt J, Dileo C, Shim M. Music interventions for preoperative anxiety. Cochrane Database Syst Rev. 2013 Jun 6;2013(6):CD006908. doi: 10.1002/14651858.CD006908.
- Kühlmann AYR, de Rooij A, Kroese LF, van Dijk M, Hunink MGM, Jeekel J. Meta-analysis evaluating music interventions for anxiety and pain in surgery. Br J Surg. 2018 Jun;105(7):773-783. doi: 10.1002/bjs.10853.
- Walter S, Gruss S, Neidlinger J, Stross I, Hann A, Wagner M, Seufferlein T, Walter B. Evaluation of an Objective Measurement Tool for Stress Level Reduction by Individually Chosen Music During Colonoscopy-Results From the Study “ColoRelaxTone”. Front Med (Lausanne). 2020 Sep 15;7:525. doi: 10.3389/fmed.2020.00525.
- Monsalve-Duarte S, Betancourt-Zapata W, Suarez-Cañon N, Maya R, Salgado-Vasco A, Prieto-Garces S, Marín-Sánchez J, Gómez-Ortega V, Valderrama M, Ettenberger M. Music therapy and music medicine interventions with adult burn patients: A systematic review and meta-analysis. Burns. 2022 May;48(3):510-521. doi: 10.1016/j.burns.2021.11.002.
- Raglio A. Therapeutic Use of Music in Hospitals: A Possible Intervention Model. Am J Med Qual. 2019 Nov/Dec;34(6):618-620. doi: 10.1177/1062860619850318.
- Biondi Situmorang DD. Music Therapy for the Treatment of Patients With COVID-19: Psychopathological Problems Intervention and Well-Being Improvement. Infect Dis Clin Pract (Baltim Md). 2021 May;29(3):e198. doi: 10.1097/IPC.0000000000000999.
![]() This work is licensed under a Creative Commons
This work is licensed under a Creative Commons
Attribution-NonCommercial-NoDerivatives 4.0 International License.
Effectiveness of nursing intervention in short-term hospitalization for patients suffered from borderline personality disorder and self-harm. A narrative literature review
Antonino Calabrò1, Federica Ilari2, Lorenzo Rizzo3, Alessia Lezzi4, Simone Zacchino4, Pierluigi
Lezzi5, Giovanni Maria Scupola6, Marta Fanton7, Roberto Lupo6, Elsa Vitale8*
- Psychiatry Unit, Nuovo Ospedale Degli Infermi, Biella, Italia
- Department of Translational Medicine, University of Eastern Piedmont, Biella, Italy
- Eating Disorders Cente, Villa Eèa Cooperative Città Azzurra, Bolzano, Italy
- Associazione Nazionale Italiana Tumori, Lecce, Italy
- Neurology Unit, Vito Fazzi Hospital, Local Health Authority (ASL) Lecce, Italy
- Department of Emergency Medicine, San Giuseppe da Copertino Hospital, Local Health Authority Lecce, Italy
- Azienda ospedaliera nazionale SS. Antonio e Biagio e Cesare Arrigo, S.C. Cardiologia, Alessandria, Italy
- Department of Mental Health, Local Health Authority (ASL) Bari, Italy
*Corresponding Author: Elsa Vitale, Department of Mental Health, Local Health Authority (ASL) Bari, Italy. E-mail: vitaleelsa@libero.it; ORCID: 0000-0002-9738-3479.
Cite this article
ABSTRACT
Introduction: Personality disorder sufferers with severe self-harm and experience long psychiatric hospitalizations have complex mental health conditions and are at risk of suicide. When the symptoms of emotional instability are combined with self-harm, the resulting crisis often becomes difficult for patients and caregivers to manage. To improve care during these crises, the Dutch Multidisciplinary Guideline for Personality Disorders designates “brief admission” (BA) hospitalizations as an ameliorative intervention.
Objective: To describe the effectiveness of short hospitalization nursing care for people with borderline personality disorder and who practice self-harm, compared to ordinary hospitalization.
Methods: A narrative review was conducted through the Embase and CINAHL databases, the selected articles had to answer the following research questions: “what are the observable benefits of short-term hospitalization on patients with borderline personality disorder?”; and “what are the benefits compared to short hospitalization operators?”.
Results: Seven studies were selected. The results show that BA was perceived as an effective nursing intervention, which promoted the patient’s self-determination and self-care. This helped increase confidence in daily life and allowed people to maintain their daily routines, work, and relationships by decreasing long hospitalizations and increasing patient compliance. There has also been benefit from the staff, who report an improvement in work quality.
Conclusions: This type of hospitalization has developed in Northern European states. BA has never been tested in the Italian healthcare sector. It would be appropriate and desirable, given the results obtained, to experiment with this procedure also in Italy to obtain specific feedback regarding the relationship of short-term hospitalization with our National Health Service. It is hoped that this research can be a stimulus in this sense.
Keywords: Borderline Personality Disorder, Nursing Management, Brief Admission, Patient Experiences, Self-Harm, Short-term hospitalization.
INTRODUCTION
Borderline Personality Disorder (BPD) is the most common personality disorder observed in clinical settings and within societies around the world. This disorder is characterized by various elements: a set of unstable and changing interpersonal relationships; emotional instability which often manifests itself with sudden attacks of anger; poor impulse control associated with self-harm; identity disorders [1]. The prevalence of people with borderline personality disorder in general and clinical psychiatric populations is approximately 4% and 20%, respectively. Approximately 75% of patients with borderline personality disorder attempt suicide and 10% succeed in their attempt [2]. Self-harm is part of the signs and symptoms of BPD and is the act of harming oneself voluntarily but without a conscious or declared suicidal intention (non-suicidal self-harm ANS) [3].
It is a very common phenomenon widespread especially among young people, in fact, it is also a major health care problem among both outpatient psychiatric patients and those in hospital care, with incidence rates of 55% and 65%, respectively. When the subject with BPD practices recurrent acts of self-harm, it is due to his inability to express his own internal suffering, he attacks his own body because he has the impression that by doing so, he will calm down. This becomes difficult to manage both for the patients themselves but above all for the healthcare personnel who deal with them [2]. Patients with borderline personality disorder are followed in both outpatient and hospital settings. Treatment typically begins with community services with day care and individual and/or group psychotherapy, depending on the individual [4].
When the behavior of these individuals becomes dangerous to their health, treatment may sometimes be necessary. interruption of outpatient treatment, preferring hospitalization in a psychiatric ward to ensure good protection for the patient. However, unplanned or long-term hospitalization for these patients without a clear treatment structure is very often associated with clinical and functional decompensation [5]. Hospitalization has been shown to have limited value, with often a failure to eradicate ideas. aimed at anti-conservative actions, with the development of possible negative side effects such as the beginning of a period of regression and the continuous need for repeated hospitalizations over time [6].
The Dutch Multidisciplinary Guideline for Personality Disorders [7] recommends short-term hospitalization as a treatment and crisis management approach for people with borderline personality disorder. Similarly, the National Institute for Health and Clinical Excellence (NICE) Clinical Guideline [8] for patients with borderline personality disorder mentions the development of autonomy and the promotion of individual choice as key factors for this type of treatment. Patients should be actively involved in finding solutions to their problems even during a crisis, as this allows them to gain experience in managing the crisis and to develop a certain autonomy regarding the decisions to be made at that moment [4].
Early hospitalizations and preventive interventions have made it possible to positively change the subsequent clinical course of individuals with borderline personality disorder. It was soon noticed that preventive psychiatric hospitalizations for such patients led to significantly greater agreement between healthcare professionals and patients on the treatment they would have liked to undertake and thanks to this type of intervention many patients who took part experienced the control over one’s own care. Following this model, to support patients with borderline personality disorder, a specific crisis intervention called “brief admission” (short hospitalization or BA) was developed [2]. With the advent of the new diagnostic and statistical manual in 2014 (DSM V), the new perspectives of this disease have also changed, and therefore also the treatments. Since then a new path has been started, therefore few review studies have been found one of these is by Helleman et,[4] al. who subsequently conducted the experiments that were introduced. With this article we want to raise awareness and bring out new perspectives for the treatment of this pathology
Purpose
To describe the effectiveness of short hospitalization nursing care for people with borderline personality disorder and who practice self-harm, compared to ordinary hospitalization.
MATERIALS AND METHODS
On the day 04/11/2023 with the support of the staff of Biomedical Library Foundation in Biella, Italy, a bibliographic search was conducted within the Embase and CINAHL Complete databases.
Search strategy and keywords used
A narrative review of the literature [9] was conducted following the methodology reported in the ‘Scale for the Assessment of Narrative Review Articles’ (SANRA) [10]. The following research questions were formulated:
- What are the benefits of short hospitalization for patients suffering from BPD?
- What are the benefits compared to short-term hospitalization operators?
To conduct the literature search, a research question was previously outlined using the P.I.O. framework (Table 1), search strings were subsequently created on biomedical databases such as Embase and CINAHL, using the Boolean operators “AND” and “OR” to interconnect the following keywords: Borderline Personality Disorder, Emotionally unstable personality disorder, Injuries, Self-Inflicted, short hospitalization, brief hospital, Nursing Staff, Hospital, Nursing Outcomes, Nursing Management.
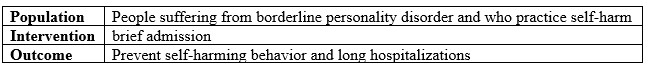
Table 1. The PIO methodology assessment.
Inclusion and Exclusion criteria
All original studies, attributable to primary resources, relevant to the research question illustrated were included. Only references written in English published in the last 15 years were taken into consideration.
However, secondary studies were excluded. Also excluded were all those references such as collections of abstracts, oral dissertations, and those quotes for which it was not possible to find the written “full text” version through the library circuit of the “Virtual Library for Health – Piedmont” (BVS – P).
Literature selection method: From the results of the searches carried out on the databases, a total of 128 bibliographical references were included. The results obtained were analyzed by two evaluators independently, by title and abstract, to identify relevant articles. The selected studies were found in full text format, read critically and the relevant ones were included in the review.
Extrapolated variables; the following data were extrapolated from the included studies: title, authors; study design; study context; mode; results and conclusions and listed in chronological order.
RESULTS
The bibliographic search revealed 128 references, of which 24 in CINAHL Complete and 104 in Embase. After a selection by reading the title and abstract, 96 articles were excluded. The articles initially included were 32; after removing the double 18s, 15 full text articles remained. The results were analyzed by two evaluators independently and read critically; after removing secondary studies, 7 articles were selected, respectively: 5 articles in Embase and 2 articles in CINAHL Complete.
Study selected
Below are the synoptic table 2 summarizing the selected articles.
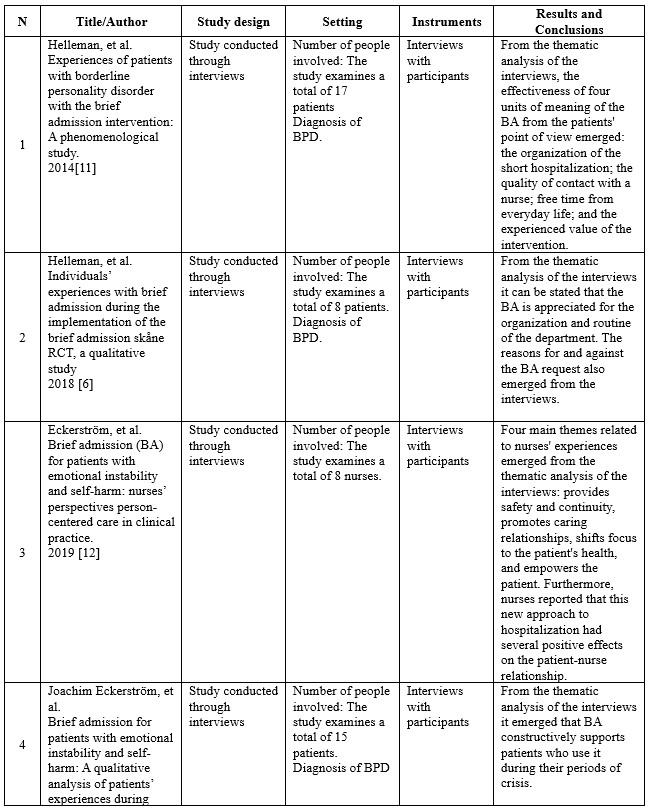
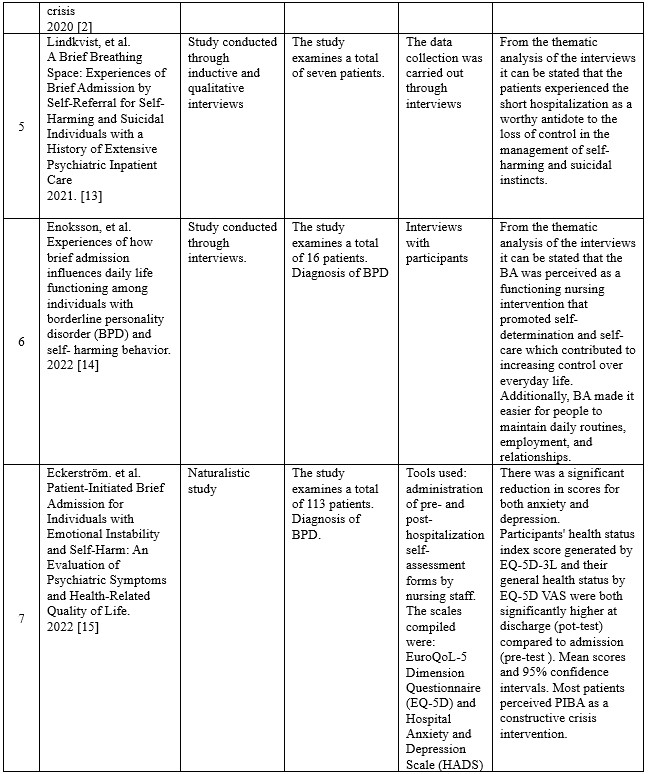
Table 2. Studies selected in the present review.
Study description
The first article is a study conducted through interviews, using Giorgi’s descriptive phenomenological methodology: Experiences of patients with borderline personality disorder with the brief admission intervention: A phenomenological study; published in International Journal of Mental Health Nursing in March 2014 [11]. The researchers’ overall objective was to describe the lived experiences of patients diagnosed with borderline personality disorder during the brief admission. A total of seventeen patients participated in the present study, which was conducted between January 2011 and August 2012. Patients were included according to the following criteria: individuals receiving public mental health services in the Netherlands; sufficient understanding of the Dutch language; diagnosis of borderline personality disorder according to the Diagnostic and Statistical Manual of Mental Disorders-IV (DSM-IV) criteria; ability to sustain an interview; prior experience with brief admission; neither age nor gender were considered. Instead, patients who met the following criteria were excluded: substance abuse; persons who presented fear that the interview would be recorded. Data were collected through interviews lasting between 45 and 75 minutes each, structured following a common pattern and based on clinical experience and a review of relevant Helleman literature. Data saturation was reached when no new meaning units were mentioned after interviews were conducted with 15 participants. Interviews with participants were audio recorded and transcribed verbatim. The meaning units in the transcripts were then identified and analyzed to reveal current problems and patterns following the steps described by Giorgi. Thematic analysis of the interviews revealed the effectiveness of four units of meaning of short hospitalization from the patients’ perspective: the organization of the short hospitalization; the quality of contact with a nurse; the regaining of free time in daily life; and the personal value this type of intervention acquired for patients. These units of meaning formed the essential structure of the experience. Patients also reported that the quality of contact with a nurse is the most important thing. Nurses should therefore be aware of the meaning and value of their relationship with patients with borderline personality disorder considering the strong interpersonal hypersensitivity of such individuals.
The second article is an interview study focusing on qualitative analysis of patients’ experiences: Individuals’ experiences with brief admission during the implementation of the brief admission skåne RCT, a qualitative study; published in Nordic Journal of Psychiatry Nordic [6]. The researchers’ overall objective was to detect possible limitations and strengths of brief admission and what were the reasons for requiring or conversely not requiring this type of admission. A total of 8 patients participated in the present study. Patients were included according to the following criteria: meeting at least three criteria for a diagnosis of borderline personality disorder; having been admitted to a psychiatric hospital for acute care for at least seven days or having presented to a psychiatric emergency room at least three times in the past six months; having recently performed acts of self-harm and/or recurrent suicide attempts; and age ≥18 years to 60 years. In contrast, patients were excluded if they met the following criteria: no regular contact with outpatient psychiatric services; somatic disorder or need for medication management that contributes significantly to the inclusion criteria (e.g., if self-harm occurs only during episodes of hypoglycemia in a diabetic person or in someone with substance-induced psychosis); homeless persons.
Data were collected through interviews conducted at the Lund psychiatric clinic, their duration was between 20 and 45 minutes each, and all interviews were conducted following a common pattern. The interviews with the participants were audio-recorded and transcribed verbatim. The units of meaning in the transcripts were then identified and analyzed to reveal current problems and patterns. From the thematic analysis of the interviews, it can be stated that the elements of short hospitalization most valued by the participants were the organization and routine of the ward. This is contrasted with the statements of some patients who reported that they had problems with some negative attitudes of the staff. Regarding the reasons reported for requesting short hospitalization, effective prevention of impulses aimed at self-harm, ending social isolation, creating a daily routine, and having an alternative to excessively long hospitalizations and mandatory hospitalizations emerged. Reasons for not requesting short hospitalization, on the other hand, are fear of rejection and difficulty in deciding the degree of severity of personal problems.
The third article is an interview study focused on qualitative analysis of nurses’ experiences: Brief admission (BA) for patients with emotional instability and self-harm: nurses’ perspectives person-centered care in clinical practice; published in International Journal of Qualitative Studies on Health and Well-being [12]. The researchers’ overall objective was to describe the experiences of nurses working with BA related to patients with emotional instability and self-harm. A total of 8 nurses participated in the present study. Purposive sampling was used to recruit participants. The only criterion that was followed to include the nurses was that they worked, during day shifts, within the selected psychiatric clinic, in the ward where the short hospitalization was taking place. Interviews with participants were audio recorded and transcribed verbatim. Units of meaning in the transcripts were then identified and analyzed to reveal current problems and patterns. Thematic analysis of the interviews revealed four main themes related to nurses’ experiences: providing safety and continuity, promoting relationship as caring time, shifting the focus to inpatient health, and empowering the patient. In addition, nurses reported that this new approach to hospitalization had several positive effects.
The fourth article is an interview study focusing on qualitative analysis of patients’ experiences: Brief admission for patients with emotional instability and self-harm: A qualitative analysis of patients’ experiences during crisis; published in International Journal of Mental Health Nursing [2]. The researchers’ overall goal was to answer the following research questions: what are patients’ experiences during brief admission? What do patients think are the key components of ‘brief admission? What improvements are considered relevant by patients? Purposive sampling was used to recruit participants, starting with contact with those who had most used short admission. A total of fifteen patients participated in the present study. Patients were included according to the following criteria: possessing a documented clinical history of emotional instability (mainly problems with emotion regulation and impulse control, borderline personality disorder); prior experience with brief admission; whether the patient had recently performed acts of self-harm and/or recurrent suicide attempts; neither age nor gender were taken into account. Instead, patients who had a primary diagnosis of psychotic disorder or depressive disorder were excluded.
Data were collected through interviews conducted at participants’ outpatient units, their duration ranged from 13 to 51 minutes each (mean = 31 minutes), and all interviews were conducted following a common pattern and structured based on a review of previous research. Interviews with participants were audio recorded and transcribed verbatim. The units of meaning in the transcripts were then identified and analyzed to reveal current problems and patterns following the steps described by Giorgi. Thematic analysis of the interviews revealed four themes related to patients’ experiences: “it is a break when life gets difficult”; “it is comforting to know that there is help”; “it encourages taking personal responsibility”; and “it is helpful to see problems from a different perspective.” Four themes also described key components: “a clear treatment plan,” “a smooth admission procedure,” “a friendly and welcoming approach from staff,” and “daily conversations.” Finally, three themes described areas for improvement: “feeling guilty for requesting short hospitalization,” “room occupancy problems,” and “differences in staff competence.” Overall, the results indicate that short hospitalization constructively supports patients with emotional instability and self-harm during a period of crisis.
The fifth article is a study conducted through inductive and qualitative interviews, uses hermeneutic phenomenological methodology and is inspired by Ricoeur’s theory of interpretation: A Brief Breathing Space: Experiences of Brief Admission by Self-Referral for Self-Harming and Suicidal Individuals with a History of Extensive Psychiatric Inpatient Care; published in Issues Ment Health Nurse [13]. The overall goal of the researchers was to detect the main characteristics as well as pre-expectations and reflections on potential improvements and adaptations of short hospitalization through patients’ personal experiences during their BA. A total of seven patients participated in the present study. Patients were included if they had met the following two criteria: prior experience of short admission; having been admitted to a hospital ward for psychiatric care for at least one hundred and eighty days in the 365 days prior to short admission.
Data collection was carried out through interviews conducted at patients’ homes or within psychiatric clinics in Helsingborg, Lund or Malmo between September and October 2018. All interviews were conducted following a common pattern. Interviews with participants were audio recorded and transcribed verbatim. The units of meaning in the transcripts were then identified and analyzed to reveal current problems and patterns. From the thematic analysis of the interviews, it can be said that the patients experienced the short hospitalization as a worthy antidote to the loss of control in dealing with self-injurious and suicidal instincts; moreover, the relief of not being continually interviewed reduced to some extent the negative feelings of fear in seeking help and care from health care personnel. Contrast this, however, with the statements of some patients who reported how brief hospitalization could offer the help and protection needed in times of mild crisis, but how it was of little help in the face of a more severe crisis.
The sixth article is a study conducted through interviews, using the descriptive qualitative method: Experiences of how brief admission influences daily life functioning among individuals with borderline personality disorder (BPD) and self-harming behavior; published in Journal of Clinical Nursing [14].
The researchers’ overall goal was to explore the experiences of how brief admission affects daily life functioning among individuals with borderline personality disorder and self-injurious behavior. Purposive sampling was used to recruit participants. A total of sixteen patients participated in the present study, which was conducted between November 2020 and January 2021. Patients were included according to the following criteria: diagnosis of borderline personality disorder; experience of brief hospitalization; whether the patient had recently performed acts of self-harm; neither age nor gender were considered. Instead, patients who met the following criteria were excluded: being admitted to a hospital at that time. Data collection was carried out through interviews conducted at the location chosen by each participant, their duration was between 15 and 90 minutes each, and all interviews were structured and conducted following a common pattern.
Data saturation was reached when no new meaning units were mentioned after interviews were conducted with 13 participants. Interviews with participants were audio recorded and transcribed verbatim. The meaning units in the transcripts were then identified and analyzed to reveal current problems and patterns. From the thematic analysis of the interviews, it can be stated that short hospitalization was perceived as a functioning nursing intervention that promoted self-determination and self-care, helping to increase control over one’s everyday life. In addition, short hospitalization made it easier for people to create or maintain a daily routine, employment and social relationships.
The seventh article is a naturalistic study with repeated measures (pre-test and post-test): Patient-Initiated Brief Admission for Individuals with Emotional Instability and Self-Harm: An Evaluation of Psychiatric Symptoms and Health-Related Quality of Life; published in Issues in Mental Health Nursing. Aim was to evaluate how symptoms of anxiety, depression and health-related quality of life (HRQoL) change after patient-initiated brief admission (PIBA), in patients in crisis with increased risk of self-harm. One hundred and thirteen patients were recruited from a Stockholm psychiatric clinic between 2016 and 2020. Upon admission and discharge, patients completed the Hospital Anxiety and Depression Scale (HADS) and the EuroQoL-5 Dimension Questionnaire (EQ-5D). Two outpatient psychiatric clinics and two psychiatric hospital departments in Stockholm specializing in BPD and anxiety disorders were involved initially.
During the 4-year intervention period (2016-2020), a reorganization was performed, and four additional outpatient units were included. By minimizing exclusion criteria and involving only inpatient and outpatient adult psychiatric units specializing in BPD, our patient sample is considered representative of the patient population of these units. One of the units had two patient rooms dedicated to PIBA, while the other unit had one room dedicated to PIBA. Inclusion criteria were as follows: (1) clinical history and current symptomatology of emotional instability (mainly problems with emotion regulation and impulse control) and a history of self-harm and (2) at least one previous period of inpatient care. Of the 145 patients who had PIBA contracts during the intervention period, 113 (78%) gave oral and written informed consent to participate in the study. The results obtained among the 113 patients with PIBA contracts, 57% (n = 64) used PIBA at least once during the study period.
There was a significant decrease in symptoms of anxiety and depression, as reflected in the HADS score, after the first hospitalization, with a medium effect size. Significant reductions in both anxiety and depression symptoms were also observed after subsequent hospitalizations. Combining the two subscales of the HADS, the results showed a large effect (d = 0.75) on the total burden of psychiatric symptoms. This result was confirmed in the analysis of the EQ-5D dimension “anxiety/depression,” with a large reduction (d = 0.72) in symptoms. The HRQoL of the participants increased significantly, with a large effect as measured by the EQ-5D VAS and a mean effect as measured by the EQ-5D index. and analysis of each dimension of the EQ-5D index showed that only the “Anxiety/depression” dimension was significantly decreased (except for “Habitual Activities” in the third admission to PIBA). This specific EQ-5D result was consistent with the changes in anxiety and depression symptoms in the HADS.
The potential reasons for the absent effect on the “Mobility” and “Self-care” dimensions could be due to low levels of symptomatic load in these areas. Moreover, they were not the primary indication for PIBA. The decrease in the “Habitual Activities” dimension was not significant for the first, second, and fourth admissions to PIBA. This could be an area for improvement and show the need to further educate health care providers on helping patients with behavior activation and helping self-help regarding initiating their daily activities. Almost all participants (95.2%) described PIBA as a constructive intervention. The importance of getting quick help when psychiatric symptoms worsen. The results of this study also reported high ratings (M = 9.02 out of 10) regarding the approach from staff, which aligns with previous studies of PIBA [11,12] in which a friendly and welcoming attitude from health care providers was described.
Based on this, our hypothesis is that PIBA is cost-effective and efficient in terms of utilization. The overall purpose of PIBA is to provide a patient-initiated time-out in a safe environment when a crisis is imminent, the patients in this study, in which most had been diagnosed with a disorder that was previously considered “difficult to treat”, stated that PIBA fulfills its stated purpose.
DISCUSSION
The objective of this review was to describe published studies on the effectiveness of short hospitalization nursing care for people with borderline personality disorder and who practice self-harm, six studies were identified of which 6 are qualitative [2,6,11–14] and one quantitative [15].
The thematic strengths found by the patients are summarized in these 4 macro areas identified by Helleman [6] and common to other authors: were: 1 Structure and routine, 2 Positive staff attitudes, 3 The experience of self and 4 Negative staff attitudes.
- Structure and routine: Patients reported value in knowing that a BA was available to them and experienced it as helpful in regaining basic sleep and eating routines, getting respite from the demands at home, and creating meaning safety. The fact that they could be sure that there would be daily conversations reportedly created a feeling of safety. Even just knowing that BA was a possibility was mentioned as something important, even if it wasn’t used. The reported perception was that the BA had prevented them from self-harming and attempting suicide. However, self-harm treatment was not perceived as the focus of BA. Rather, BA’s role was to meet basic needs by providing “rest from real life” by letting go of daily duties or overthinking to do something.
- Positive attitudes from staff: Patients also reported positive attitudes from staff. A warm welcome at the start of the BA is “more important than people think”. The experience of being listened to, taken seriously and feeling responsible for their health was perceived as building their confidence. The operators ensured daily conversations, which led to feelings of greater safety.
- The experience of the self: main objective of the BA, during admission the responsibility for managing current crises is in the hands of the participants themselves. This was mostly described as a positive experience: patients were able to take control of their situation, self-determine (taking medications not from nurses but self-managed), keep personal items, sense of independence and integrity, all in one protected environment where discussion is always possible.
- Weaknesses noted by patients were linked to: From the staff as lack of knowledge about BA, negative attitudes about BA expressed in front of patients, which created an unwelcome and unsafe feeling and lack of time. Lack of time was another factor. This made them feel rejected, which in turn increased distress and negative thoughts.
Organizationally: Mixing BA with acute hospitalizations was a challenge for patients in BA when they found themselves relatively stable compared to other hospitalized patients. This led to worries about irritating others, feelings of guilt for trying to use BA preventively. It has been noted that having only one room, within an acute ward, undermines the entire purpose of the BA as the risk of being left alone during the crisis and without support from providers is very high.
The quantitative study by Eckerström [15] analyzes the aspects of anxiety/depression and quality of life through two scales, the first Hospital Anxiety and Depression Scale (HADS) and the second EuroQoL-5 Dimension Questionnaire (EQ-5D). The data collected validates those of previous studies for anxiety and depression, a significant decrease in symptoms of anxiety and depression, as reflected in the HADS score, after the first hospitalization. Significant reductions in anxiety and depression symptoms were also observed after subsequent hospitalizations. Combining the two subscales of the HADS, the results showed a large effect (d = 0.75) on total psychiatric symptom burden. This result was confirmed in the analysis of the EQ-5D dimension “anxiety/depression”, with a large reduction (d = 0.72) in symptoms. These findings match the results of a previous study, which included 15 patient respondents who reported that BA helped them overcome suicidal thoughts, depressive symptoms, and emotional distress [12]. The quality-of-life results highlight that nearly all participants (95.2%) described BA as a constructive intervention, the importance of receiving rapid help when psychiatric symptoms worsen. The results of this study also reported high ratings regarding the staff approach. Patients who have experienced both BA and regular hospital care describe the latter as old-fashioned, as patients have to wait until they get worse to receive treatment and demonstrate their need for help with self-harm as already demonstrated by Lindkvist’s study [13].
In reference to the second research question “What are the benefits compared to short-term hospitalization operators?” Eckerström’s study [12] aims to describe the experiences of nurses working with BA in relation to patients with emotional instability and self-harm, through interviews. The data that emerged also confirms from the nurses some data already collected by the patients from a care perspective such as: provides safety and continuity; direct access to the patient, without going through official channels Emergency, urgency and acceptance department (DEA), Mental Health Center (CSM) has improved communication between operators and patients, reducing misunderstandings that sometimes arise when communications are filtered through different nurses and doctors. Know what you both expect from the contract.
Furthermore, nurses described their new responsibility as challenging because they had to support patients with nursing interventions rather than medications or monitoring alone. In this sense the improvement of the patient-nurse relationship leads to a greater understanding of the person behind the patient, which was mostly described in a positive way.
Promoting person-centered care led to a demonstration of nurses’ confidence in their patients’ abilities fostered a positive relationship in which patients began to act more constructively, leading to mutual respect and a more balanced relationship. However, such in-depth reporting was painful because it became too close to the patients. BA gave nurses the mandate and the possibility to focus on nursing care, making the best use of those concepts of empathy that belong to us.
CONCLUSIONS
The objective of this review was to describe published studies on the effectiveness of short hospitalization nursing care for people with borderline personality disorder and who practice self-harm. Considering what was assessed in the discussions, we can affirm that short hospitalization is the best nursing intervention in terms of effectiveness and results obtained in the treatment of the population taken into consideration. The aspects of greatest interest that have the best outcomes are: quality of the patient-nurse relationship, the regaining of free time in daily life, the awareness of support for quality and duration of care, the management of self-harming and suicidal instincts, the promotion of self-determination and self-care, the maintenance of valid social relationships in the family and in the working world, the increase in the perception of security.
Undoubtedly within our review we took into consideration the critical issues that emerged such as: organizational factors, patients in BA admitted to emergency facilities, lack of staff training.
Nurses should therefore be aware of the meaning and value of their relationship with patients suffering from borderline personality disorder considering the strong interpersonal hypersensitivity of such subjects.
Short-term hospitalization was born and developed within the psychiatric wards and healthcare facilities of Northern European states, where nowadays it very often represents the most used treatment for the care of people with borderline personality disorder, as well as all the complications that this diagnosis brings. As regards the situation in our country, however, there are no studies that deal with this topic. In Italy, in fact, short hospitalization has never been experimented with, despite the effectiveness demonstrated by the results obtained from this treatment. Given the modest number of studies that we have analyzed for this type of hospitalization, it would be appropriate and desirable to experiment with this procedure also in Italy to have specific feedback regarding the relationship of short hospitalization with our National Health Service.
It is considered appropriate to continue and stimulate research into this topic, given the few studies on this subject present in the literature, as the topic we have discussed is one with a strong social impact.
Strengths and limitations
The strengths of the study are: original argument on a developing topic which has demonstrated excellent results, from the research carried out the presence of only one revision carried out by Helleman 2014 at the beginning of the process, 2014 subsequently no other revisions were found. It is believed to be an important contribution for the scientific community to be able to make known a patient-centered care model and consequently to be able to implement it in other contexts as well.
The limits are specific to narrative reviews: poor reproducibility of the research, little specificity.
Furthermore, the study was self-financed which led to a search of a few databases and the possibility of downloading full texts.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest.
Author Contributions
All Authors equally contributed.
Acknowledgments
Authors thank all the staff of Biomedical Library Foundation in Biella, Italy.
REFERENCES
[1] American Psychiatric Association. DSM-5 Manuale diagnostico e statistico dei disturbi mentali. Quinta. Milano: Raffaello Cortina Editore; 2014.
[2] Eckerström J, Flyckt L, Carlborg A, Jayaram‐Lindström N, Perseius K. Brief admission for patients with emotional instability and self‐harm: A qualitative analysis of patients’ experiences during crisis. Int J Ment Health Nurs 2020;29:962–71. https://doi.org/10.1111/inm.12736.
[3] Hawton K, Saunders KEA, O’Connor RC. Self-harm and suicide in adolescents. Lancet Lond Engl 2012;379:2373–82. https://doi.org/10.1016/S0140-6736(12)60322-5.
[4] Helleman M, Goossens PJJ, Kaasenbrood A, Van Achterberg T. Evidence Base and Components of Brief Admission as an Intervention for Patients With Borderline Personality Disorder: A Review of the Literature: Evidence Base and Components of Brief Admission as an Intervention for Patients With Borderline Personality Disorder. Perspect Psychiatr Care 2014;50:65–75. https://doi.org/10.1111/ppc.12023.
[5] Liljedahl SI, Helleman M, Daukantaité D, Westrin Å, Westling S. A standardized crisis management model for self-harming and suicidal individuals with three or more diagnostic criteria of borderline personality disorder: The Brief Admission Skåne randomized controlled trial protocol (BASRCT). BMC Psychiatry 2017;17:220. https://doi.org/10.1186/s12888-017-1371-6.
[6] Helleman M, Lundh L-G, Liljedahl SI, Daukantaité D, Westling S. Individuals’ experiences with brief admission during the implementation of the brief admission skåne RCT, a qualitative study. Nord J Psychiatry 2018;72:380–6. https://doi.org/10.1080/08039488.2018.1467966.
[7] Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M. Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ 2008:a1655. https://doi.org/10.1136/bmj.a1655.
[8] NICE. Borderline Personality Disorder: Treatment and Management. Leicester (UK): British Psychological Society (UK); 2009.
[9] Grant MJ, Booth A. A typology of reviews: an analysis of 14 review types and associated methodologies. Health Inf Libr J 2009;26:91–108. https://doi.org/10.1111/j.1471-1842.2009.00848.x.
[10] Baethge C, Goldbeck-Wood S, Mertens S. SANRA-a scale for the quality assessment of narrative review articles. Res Integr Peer Rev 2019;4:5. https://doi.org/10.1186/s41073-019-0064-8.
[11] Helleman M, Goossens PJJ, Kaasenbrood A, van Achterberg T. Experiences of patients with borderline personality disorder with the brief admission intervention: a phenomenological study. Int J Ment Health Nurs 2014;23:442–50. https://doi.org/10.1111/inm.12074.
[12] Eckerström J, Allenius E, Helleman M, Flyckt L, Perseius K-I, Omerov P. Brief admission (BA) for patients with emotional instability and self-harm: nurses’ perspectives – person-centred care in clinical practice. Int J Qual Stud Health Well-Being 2019;14:1667133. https://doi.org/10.1080/17482631.2019.1667133.
[13] Lindkvist R-M, Westling S, Liljedahl SI, Landgren K. A Brief Breathing Space: Experiences of Brief Admission by Self-Referral for Self-Harming and Suicidal Individuals with a History of Extensive Psychiatric Inpatient Care. Issues Ment Health Nurs 2021;42:172–82. https://doi.org/10.1080/01612840.2020.1789787.
[14] Enoksson M, Hultsjö S, Wärdig RE, Strömberg S. Experiences of how brief admission influences daily life functioning among individuals with borderline personality disorder (BPD) and self‐harming behaviour. J Clin Nurs 2022;31:2910–20. https://doi.org/10.1111/jocn.16118.
[15] Eckerström J, Carlborg A, Flyckt L, Jayaram-Lindström N. Patient-Initiated Brief Admission for Individuals with Emotional Instability and Self-Harm: An Evaluation of Psychiatric Symptoms and Health-Related Quality of Life. Issues Ment Health Nurs 2022;43:593–602. https://doi.org/10.1080/01612840.2021.2018530.
![]() This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Online Learning Method in COVID-19 Pandemic: The Perspectives, Opportunities, and Challenges of Nursing Students in Aceh, Indonesia: An Exploratory Descriptive Study
Cut Husna1, Riski Amalia1*, Ahyana1
1 Department of Medical and Surgical Nursing, Faculty of Nursing, Universitas Syiah Kuala, Banda Aceh, Indonesia, 23111.
Corresponding author: Ns. Riski Amalia, S.Kep., M.Kep. Teungku Tanoh Abee Street, Kopelma Darussalam, Universitas Syiah Kuala, Banda Aceh, Indonesia, 23111. Orcid: https://orcid.org/0000-0002-3004-0455. Email: riskiamalia@usk.ac.id.
Cite this article
ABSTRACT
Introduction: The Covid-19 virus pandemic caused a significant impact on communities’ life and their activities throughout the world. The Covid-19 pandemic also had a significant effect on the education system in Indonesia and requires all teaching and learning activities for students to be carried out by virtual or online learning method.
Aim: This study was to explore online learning methods’ perceptions, opportunities, and challenges in the COVID-19 pandemic among nursing students.
Method: A descriptive explorative study was implemented with a cross-sectional design. The study was conducted on 276 nursing students in Aceh, Indonesia. The data were collected using a 5-point Likert scale and the standardized Online Learning Perception Scale (OLPS) and Opportunities and Challenges Online Learning (OCOL) questionnaires. The reliability test of the questionnaires were indicated by Cronbach alphas of 0.89 and 0.90, respectively.
Result: The study results showed that 50.4% of the nursing students have positive perceptions about the online learning method, 51.4% of the students believe that online learning offers high opportunities, and 50.4% of students think that the online learning method is highly challenging. It showed more than 50% of the students have significant on the positive perceptions, high opportunities, and challenges in learning method.
Conclusion: The positive perception, high opportunities, and challenges towards online learning methods among nursing students is the result of a study that proved the benefits of online learning methods which can be used as an alternative for students to achieve learning goals, especially during the COVID-19 pandemic. Positive perceptions from students towards online learning methods can be encouragement and strength for one of the online-based learning methods and could also be proven by the high opportunities and challenges students in this online learning method.
Keywords: Perception, opportunities, challenges, students, online learning
INTRODUCTION
The COVID-19 outbreak in December 2019 has significantly impacted communities’ life and activities. The SARS-CoV 2 causes COVID-19 has become an epidemic and causes the foremost crucial number of deaths worldwide. The COVID-19 generated more than 80% of infected people developed mild to moderate illness with symptoms such as fever, dry cough, fatigue, and severe symptoms such as chest pain, loss of speech, and shortness of breath, and recover without hospitalization [1]. It has also impacted all aspects of human life globally, including economic, education, health, medical needs and services, and social crises [2].
The impact of the COVID-19 pandemic on education is also prominent. The government policy to carry out physical and social distancing as a health protocol required by the World Health Organization has mandated that all teaching and learning activities carried out at home (school from home) [2]. The health protocol intended to minimize physical contact to break out the virus’s chain. Learning media through distance learning with online media (in-network) is a method used to achieve learning competencies during this pandemic [3].
Online learning that has been widely applied for years is back in the spotlight during the COVID-19 pandemic. Before the pandemic, e-learning had not received much attention due to the perception that face-to-face learning was more effective than online methods. The COVID-19 pandemic has made swift changes and forced the learning system to be online to reduce the gaps due to the lockdown situations [4-7]. They aimed to achieve student competencies through critical thinking, creative thinking, collaboration, and communication. Critical thinking directs students to solve problems in the learning process. Creativity thinking is having high creativity and reasoning and seeing a situation from various sides or perspectives, changing textual learning to be contextual using multiple sources in society. Then, collaboration is an activity to work together in their future lives, and finally, communication means conveying ideas and thoughts quickly, clearly, and effectively [8]. The online learning method needs determination and ability from the user, including the students must be perspicuity, dependability, stimulation, attractiveness, and usability and innovation. The study also proved that stimulation and attractiveness is an online learning method that significantly affects students’ satisfaction during the COVID-19 pandemic [9].
Furthermore, an online class-based curriculum is more flexible and convenient for students. The use of online learning platforms in teaching and learning was more effective and efficient; however, some challenges may occur in online learning, especially in the practice of lab skills [5,7]. Online learning also offers some opportunities for the students. The students could access appropriate and accessible data and information, master the use of information and technology tools, access education anywhere, seek and learn new knowledge virtually through textbooks and print media that affect the role of lecturers in delivering learning materials [4].
Based on the primary sources conducted with several students of the Faculty of Nursing, Universitas Syiah Kuala, Banda Aceh, Indonesia, as an area severely damaged during the 2004 tsunami with the condition of being very prone to natural disasters unstable geographical conditions. The students explained that the online learning method is beneficial in time management, transportation costs, and autonomy in the learning process. However, some students dominantly showed that they were confused in the laboratory skills conducted online and preferred face-to-face laboratory learning, experienced boredom, and sometimes lacked concentration during the online learning process. Furthermore, other students mentioned that the opportunities in the online learning methods might develop creative ideas, such as making learning media; video, role play, demonstration, leaflet, booklet, and several other assignments. It also motivated them to self-learn by accessing digital learning resources, enhancing their discussion skills, and using online meeting platforms, such as Zoom meeting applications and Google classroom. The challenges during online learning include the lack of internet connection, application systems, electrical power, computers or android devices, and environmental factors. This online learning challenge is supported by Gumede & Badriparsad [11] mentioned that there are concerns about the transition from face-to-face lectures to online learning systems and the need to adapt adequately to online learning methods such as devices and data availability. The objective of the study was to explore three parts about online learning methods among nursing students: Perceptions, opportunities, and challenges in the COVID-19 pandemic.
METHOD
Study Design
This study design was a descriptive explorative to explore the perceptions, opportunities, and challenges of the online learning method in the COVID-19 pandemic in nursing students.
Population and Sample
This study was conducted from September to October 2020. The populations were all the nursing students at the Faculty of Nursing, Universitas Syiah Kuala, Banda Aceh, Indonesia who had been studying from years of 2016-2019 (year of academic entry) at both the academic and professional education stages. The sampling method was consecutive sampling totalling 276 students.
Instruments
The perception questionnaire used was the standardized Online Learning Perception Scale (OLPS) from Wei & Chou (2020), and Opportunities and Challenges Online Learning (OCOL) questionnaires. The reliability test of the questionnaires using Cronbach alpha of 0.90 and 0.89, respectively. The researchers developed Opportunities and Challenges Online Learning (OCOL) questionnaires based on a literature review. It was validated for face validity and content validity using content validity index (relevance, clarity, and brevity) by three experts from the Faculty of Nursing at Universitas Syiah Kuala, Banda Aceh, and fulfilled the validity test requirements. For the face validity aimed to investigate the cultural relevance, understanding of meaning, logical flow, grammar, and composition of the newly developed items [1]. The OLPS and OCOL questionnaires consisted of 5-points Likert scale: strongly agree (5), agree (4), doubtful (3), disagree (2), strongly disagree (1). The OPLS consisted of 23 positive statements and the OCOL questionnaires (opportunities and challenges online learning method) consisted of 24 positive statements. The binary categories have been decided by using mean score for OPLS into 2 categories: positive and negative peceptions. Morever, the OCOL questionnaire also divided into 2 categories: high and low opportunities and challenges online learning method.
Data Collection
The preparatory stage of data collection includes completing the administration process and approval from the Dean of the Faculty of Nursing at Universitas Syiah Kuala, Banda Aceh, Indonesia. The researcher collected the data by recruiting the eligible respondents: all students of the class 2016-2019 (four batches) in the academic and professional stages using online learning in the COVID-19 pandemic. The data is kept confidential by coding the respondents. The respondents signed the written informed consent form using an online platform. Next, the respondents who agreed to involve in this study were sent a link to fill out the online questionnaires. The questionnaire was checked for completeness. The researchers would like to thank the respondents who have participated in the study.
Data Analysis
Descriptive analysis in this study uses the mean, standard deviation, frequency, and percentage of perceptions, opportunities, and challenges of online learning methods for nursing students. Data were analyzed using the statistical package Statistical Program for Social version 23.0 (IBBM Corp., Armonk, New York, USA).
Ethical consideration
This study is consistent with the Declaration of Helsinki. The study has been approved by the local Ethics Committee in Indonesia (Research Code: 113003080620; Decision Date: July 21, 2020).
RESULTS
The population in this study was both the nursing students of academic and nurses’ profession stages of Faculty of Nursing, totally 667 students. By using consecutive sampling, 276 students were conducted in this study. The results of this study consisted of demographic data of the respondents, perceptions about online learning, and opportunities, and challenges online learning method in COVID-19 pandemic are explained as follow (Table 1, 2, 3, 4)

Table 1. Characteristics of the respondents (n = 276)
Table 1 showed the average age of the respondents was 20.44, with a standard deviation of 1.56. The majority of respondents were female (91.7%).
Then, most respondents had only been studied for a year or started in 2019 (27.5%), and 94.2% of the respondents had online learning experiences. The biggest obstacle in online learning methods was internet access (25.1%).
Perceptions, opportunities, and challenges online learning method in COVID-19 Pandemic
Student’ perception, opportunities, and challenges about online learning method among nursing students in Faculty of Nursing are shown in Table 2.

Table 2. Perceptions, opportunities, and challenges of nursing students about online learning method in COVID-19 pandemic (n = 276)
Table 2 showed 50.4% of respondents have positive perceptions of online learning in COVID-19, 51.4% believe that online learning methods offer high opportunities, and 50.4% think that online learning is highly challenging.
The details of each item for OPLS and OCOL questionnaires were presented in Tables 3, 4, and 5 as follow:

Table 3. Online Learning Perception Scale (OLPS) of nursing students about online learning method in COVID-19 pandemic (n = 276).

Table 4. The opportunities of nursing students about online learning method in COVID-19 pandemic (n = 276).

Table 5. The challenges of nursing students about online learning method in COVID-19 pandemic (n = 276)
DISCUSSION
This study explores the opportunities and challenges of online learning methods during the COVID-19 pandemic in nursing students. The results showed that more than half of the respondents have positive perceptions of online learning (50.4%). This finding is supported by several statement items indicating a positive impact of online education on students, namely the availability of various learning resources, available time and place, reducing pressure during exams and assessment, and increasing student creativity in creating learning media. Meanwhile, nearly half of the students show negative perceptions (49.6%) of online learning. The nursing students mentioned that online learning requires high internet data or fees, and internet access is limited for those living far from urban areas due to environmental factors and electrical powers. Besides, the interaction with lecturers and other students is minimal. They found it challenging to understand the learning delivered by lecturers and other students during activities in online education.
The finding concerning the students with negative perceptions (49.6%) on the online learning method aligns with Zhafira et al. (2020), who argued that students need to have learning methods to motivate themselves to achieve their learning goals. The online lecture system is still perceived as a breakthrough or a new paradigm in teaching and learning activities because students and lecturers do not need to attend class. They only rely on an internet connection to conduct learning activities from faraway places [13]. Furthermore, also supported by the results of the study stated that several problems in online learning method in the COVID-19 pandemic such as technological factors, mental health, time management, and the balance between life and education. The study results also reported that the students are dissatisfied with the online learning experience due to distraction and reduced focus, psychological problems, and management issues [14].
The study conducted by Khan et al [6] showed that most of the students positively perceive the online learning system in the pandemic to maintain the educational process; however, there are several challenges, such as internet quality, digital information technology literacy, and economic conditions related to internet fee. However, the study results by reported that a different view of online learning activities in terms of soft skills do not be achieved, such as the face-to-face learning method in the class. Then, a study conducted by Kulal & Nayak [16] also revealed that students feel comfortable with the online learning process with support from educators. Yet, they could not provide a traditional classroom learning atmosphere because of technical problems and lack of training, impacting the ineffectiveness of online classroom learning by educators.
The world of education around the globe must process faster adaptation in the face of the COVID-19 pandemic by switching to online learning models to accelerate opportunities in facing the era of industrial revolution 4.0 as part of digital technology transformation [17-19]. Furthermore, Gurel and Tat[16] stated that opportunity is a situation or condition relevant for an activity that is positive and fun and has advantages and forces that encourage an action to occur.
This study shows that most respondents (51.4%) believe that the online learning method offers high opportunities. The COVID-19 pandemic crisis provides opportunities for lecturers to develop pedagogical innovations and create digital-based teaching curricula. One of which is that academics could teach and guide students in accessing e-learning technology and apply techniques that could design various flexible online programs to increase students’ competence in problem-solving, critical thinking, and adaptability skills [20]. Furthermore, the previous study also mentioned that the students agree with the benefits and are very satisfied with their learning experience by using online learning methods [21]. However, the online learning method needs additional financial burden due to fully online learning, namely cost to access and cost to acquire equipment [22].
The study results also show that more than half of the students (50.4%) found the online method in the COVID-19 pandemic is highly challenging. The forms of online learning challenges faced by students during the COVID-19 pandemic were internet access (25.1%), learning interactions (21.0%), learning facilities (17.9%), learning media (14.0 %), methods (13.3%), and learning materials (8.8%). Fearnley & Malay [23] stated positive developments in students’ readiness for online learning. However, the results of Yaseen et al [25] research found challenges during online education, including concerns about the technological competence of lecturers and students, increased assignments, privacy issues, social inequality when activating videos, communication disorders due to internet network constraints, unable to assess student body language and soft-skills during the learning process, student absenteeism due to internet disconnection, ethical considerations due to increased plagiarism during assignment creation, online video skills laboratory and use of virtual laboratories not suitable as a substitute for practical demonstration. However, there are opportunities for reform in the learning process, although online learning is still not considered the best alternative to studying on campus [26].
Internet access for online-based learning is critical during the COVID-19 pandemic. The government’s policy to reduce the spread of the COVID-19 virus or COVID-19 disease through physical and social distancing has shifted the offline to online learning method. The development of information technology impacts an increasingly effective learning process using computer-based technology. Media and technology adopted as facilitation in open and distance learning are also challenge the willingness to use learning models from students’ perspectives [27]. Furthermore, in the digital era and the COVID-19 pandemic, educational institutions are increasingly promoting online learning, resulting in a shift from traditional face-to-face classes (offline) to distance learning (online) [28]. However, especially for the laboratory skills competencies, almost all the students mentioned that they are more satisfied with face-to-face than the online learning methods [29]. However, especially for the laboratory skills competencies, almost all the students mentioned that they are more satisfied with face-to-face than the online learning methods. This study results follow the statement by Muflih et al. (2021) which reported that the students expressed mixed feelings about online learning, and most of them supported face-to-face classroom learning. They are pessimistic about learning professional skills and core competencies online.
Conclusion and Recommendations
The online learning method is highly relevant and applied worldwide during the COVID-19 pandemic. The pandemic has altered the order of a community’s lives in various aspects of life, including education. The existence of physical and social distancing policy with the obligation to learn from home has required online learning. The online learning methods provide several benefits, such as reducing the risk of COVID-19 transmission, increasing information and technology (IT) mastery skills, improving time management, and motivating students to learn independently.
Meanwhile, the opportunities for online learning methods in the COVID-19 pandemic are also significant, and the nursing students believe that online learning offers them high opportunities. These opportunities include using IT facilities, improving experiences in the learning process, enhancing creativity, allowing for critical and innovative thinking, providing opportunities to access learning resources, such as e-books, e-journals, e-libraries, and e-education, and enhancing self-management skills in time management in the process of completing requirements. Furthermore, the online learning methods are also highly challenging for nursing students during the COVID-19 pandemic. The challenges are internet access, internet data or fee, learning platform facilities, electrical power, environmental problems (natural and non-natural disturbances), and time constraints.
This results study provides feedback for the policymakers to prepare feasibly and good online learning platforms, internet facilities, costs, and IT personnel who could ensure the sustainable use of this online method. The governments may improve the online learning method through increasing internet access, learning media, methods used, learning materials, learning interactions, and learning facilities.
Study Limitations
The study only focuses on a descriptive exploratory. A cross sectional design was not conducted hence it can not explore the factors associated with others several online learning methods.
Conflict of interest
The authors declare no potential conflict of interests with respect to the research, authorship, and/or publication of this article.
Funding
This research did not receive any specific grant from funding agencies.
Authors contribution
Author 1: Dr. Ns. Cut Husna, S.Kep, MNS, Nursing Lecturer at the Faculty of Nursing, Universitas Syiah Kuala, Aceh, Indonesia. Contribution type: conception, design, supervision, fundings, materials, data collection and/or processing, analysis and/or interpretation, literature review, writing, and critical review. Email: cuthusna@usk.ac.id ; ORCID: https://orcid.org/0000-0002-6283-4209
Author 2: Ns. Riski Amalia, S.Kep, M.Kep, Nursing Lecturer at the Faculty of Nursing, Universitas Syiah Kuala, Aceh, Indonesia. Contribution type: analysis and/or interpretation, literature review, writing, and critical review. Email: riskiamalia@usk.ac.id ; ORCID: https://orcid.org/0000-0002-3004-0455
Author 3: Ns. Ahyana, S.Kep, MNS, Nursing Lecturer at the Faculty of Nursing, Universitas Syiah Kuala, Aceh, Indonesia. Contribution type: conception, design, supervision, literature review, and writing. Email: ahyana@usk.ac.id ; ORCID: https://orcid.org/0000-0001-6750-5052
Acknowledgment
The author would like to thank all respondents, the Nursing Students Universitas Syiah Kuala for their willingness and fully participation in this study, also to the Institute for Research and Community Service Universitas Syiah Kuala-Darussalam; the Dean of the Faculty of Nursing, the Nursing Ethics Committee Nursing Faculty Universitas Syiah Kuala which has fully assisted and facilitated in this study.
REFERENCES
[1] T. B. Alakus and I. Turkoglu, “Comparison of deep learning approaches to predict COVID-19 infection,” Chaos Solitons Fractals, vol. 140, p. 110120, 2020, doi: 10.1016/j.chaos.2020.110120.
[2] I. Duek and D. M. Fliss, “The COVID-19 pandemic – from great challenge to unique opportunity:perspective,” Annals of Medicine and Surgery, vol. in press, pp. 1–18, 2020, doi: 10.1016/j.snb.2019.127065.
[3] Ch. D. Anugrah, “Dinamika Pembelajaran Daring Di Tengah Pandemi Covid-19.” pp. 1–3, 2020. http://beritamagelang.id/kolom/dinamika-pembelajaran-daring-di-tengah-pandemi-covid-19.
[4] A. Démuth, Perception Theories, 1st ed., no. January 2013. Trnava: Faculty of Philosophy and Arts. Trnava Univeristy in Trnava, 2013, ISBN 978-83-7490-599-2. https://ff.truni.sk/sites/default/files/publikacie/demuth_philosophical_aspects_of_the_history_of_science_1.1.pdf
[5] D. Henderson et al., “Keep calm and carry on learning: using Microsoft Teams to deliver a medical education programme during the COVID-19 pandemic,” Future Healthc J, vol. 7, no. 3, pp. e67–e70, 2020, doi: 10.7861/fhj.2020-0071.
[6] M. A. Khan, T. Kamal, A. Illiyan, and M. Asif, “School students’ perception and challenges towards online classes during covid-19 pandemic in india: An econometric analysis,” Sustainability (Switzerland), vol. 13, no. 9, 2021, doi: 10.3390/su13094786.
[7] M. V. Mahajan and R. Kalpana, “A study of students’ perception about e -learning,” vol. 5, no. 4, pp. 501–507, 2018, doi: 10.18231/2394-2126.2018.0116.
[8] Ch. D. Anugrah, “Dinamika Pembelajaran Daring Di Tengah Pandemi Covid-19.” pp. 1–3, 2020, http://beritamagelang.id/kolom/dinamika-pembelajaran-daring-di-tengah-pandemi-covid-19
[9] E. Agyeiwaah, F. Badu Baiden, E. Gamor, and F.-C. Hsu, “Determining the attributes that influence students’ online learning satisfaction during COVID-19 pandemic,” J Hosp Leis Sport Tour Educ, no. xxxx, p. 100364, 2021, doi: 10.1016/j.jhlste.2021.100364.
[10] L. Gumede and N. Badriparsad, “Online teaching and learning through the students’ eyes – Uncertainty through the COVID-19 lockdown: A qualitative case study in Gauteng province, South Africa,” Radiography, vol. 28, no. 1, pp. 193–198, 2021, doi: 10.1016/j.radi.2021.10.018.
[11] L. Gumede and N. Badriparsad, “Online teaching and learning through the students’ eyes – Uncertainty through the COVID-19 lockdown: A qualitative case study in Gauteng province, South Africa,” Radiography, vol. 28, no. 1, pp. 193–198, 2021, doi: 10.1016/j.radi.2021.10.018.
[12] N. H. Zhafira, Y. Ertika, and Chairiyaton, “Persepsi Mahasiswa Terhadap Perkuliahan Daring Sebagai Sarana Pembelajaran Selama Masa Karantina Covid-19,” Jurnal Bisnis dan Kajian Strategi Manajemen, vol. 4, pp. 37–45, 2020, ISSN: 2614-2147. http://jurnal.utu.ac.id/jbkan/article/view/1981/1454
[13] N. Adijaya, “Persepsi Mahasiswa dalam Pembelajaran Online* *Pengembangan teori dari penelitian berjudul ‘persepsi mahasiswa terhadap materi ajar pada pembelajaran online’ yang telah dipublikasi di Jurnal Eduscience Vol. 3/1,” Wanastra: Jurnal Bahasa dan Sastra, vol. 10, no. 2, pp. 105–110, 2018, doi: 10.31294/w.v10i2.3931.
[14] M. Maqableh and M. Alia, “Evaluation online learning of undergraduate students under lockdown amidst COVID-19 Pandemic: The online learning experience and students’ satisfaction,” Child Youth Serv Rev, vol. 128, no. January, p. 106160, 2021, doi: 10.1016/j.childyouth.2021.106160.
[15] A. Kulal and A. Nayak, “A study on perception of teachers and students toward online classes in Dakshina Kannada and Udupi District,” Asian Association of Open Universities Journal, vol. 15, no. 3, pp. 285–296, 2020, doi: 10.1108/aaouj-07-2020-0047.
[16] E. Gurel and M. Tat, “SWOT Analysis: A Theoretical Review,” The Journal of International Social Research, vol. 10, no. 51, pp. 994–1006, 2017, doi: http://dx.doi.org/10.17719/jisr.2017.1832.
[17] C. Liguori, Eric; Winkler, “From Offline to Online: Challenges and Opportunities for Entrepreneurship Education following the COVID-19 Pandemic,” Angewandte Chemie International Edition, 6(11), 951–952., 2020, https://doi.org/10.1177/2515127420916.
[18] T. Favale, F. Soro, M. Trevisan, I. Drago, and M. Mellia, “Campus traffic and e-Learning during COVID-19 pandemic,” Computer Networks, vol. 176, no. 1, pp. 1–9, 2020, doi: 10.1016/j.comnet.2020.107290.
[19] B. Indrawati, “Tantangan dan Peluang Pendidikan Tinggi Dalam Masa dan Pasca Pandemi Covid-19,” Jurnal Kajian Ilmiah, vol. 1, no. 1, pp. 39–48, 2020, doi: 10.31599/jki.v1i1.261.
[20] S. Dhawan, “Online Learning: A Panacea in the Time of COVID-19 Crisis,” Journal of Educational Technology Systems, vol. 49, no. 1, pp. 5–22, 2020, doi: 10.1177/0047239520934018.
[21] I. Thepwongsa, P. Sripa, R. Muthukumar, K. Jenwitheesuk, S. Virasiri, and P. Nonjui, “The effects of a newly established online learning management system: the perspectives of Thai medical students in a public medical school,” Heliyon, vol. 7, no. 10, p. e08182, 2021, doi: 10.1016/j.heliyon.2021.e08182.
[22] S. Sarosa, “ScienceDirect ScienceDirect The perceived risks The effect effect of of perceived risks and and perceived perceived cost cost on on using using online online learning by high students learning by high school students,” Procedia Comput Sci, vol. 197, no. 2021, pp. 477–483, 2022, doi: 10.1016/j.procs.2021.12.164.
[23] M. R. Fearnley and C. A. Malay, “Assessing students’ online learning readiness: Are college freshmen ready?,” Asia-Pacific Social Science Review, vol. 21, no. 3, pp. 249–259, 2021, https://www.dlsu.edu.ph/wp-content/uploads/pdf/research/journals/apssr/2021-September-vol21-3/18-Assessing-Students-Online-Learning-Readiness-Are-College-Freshmen-Ready_.pdf.
[24] H. Yaseen, A. R. Alsoud, M. Nofal, O. Abdeljaber, and A. S. Al-Adwan, “The Effects of Online Learning on Students’ Performance: A Comparison between UK and Jordanian Universities,” International Journal of Emerging Technologies in Learning, vol. 16, no. 20, pp. 4–18, 2021, doi: 10.3991/ijet.v16i20.24131.
[25] H. Yaseen, A. R. Alsoud, M. Nofal, O. Abdeljaber, and A. S. Al-Adwan, “The Effects of Online Learning on Students’ Performance: A Comparison between UK and Jordanian Universities,” International Journal of Emerging Technologies in Learning, vol. 16, no. 20, pp. 4–18, 2021, doi: 10.3991/ijet.v16i20.24131.
[26] A. Appolloni, N. Colasanti, C. Fantauzzi, G. Fiorani, and R. Frondizi, “Distance learning as a resilience strategy during covid-19: An analysis of the italian context,” Sustainability (Switzerland), vol. 13, no. 3, pp. 1–12, 2021, doi: 10.3390/su13031388.
[27] O. T. Arulogun, O. N. Akande, A. T. Akindele, and T. A. Badmus, “Survey dataset on open and distance learning students’ intention to use social media and emerging technologies for online facilitation,” Data Brief, vol. 31, no. 1, pp. 1–8, 2020, doi: 10.1016/j.dib.2020.105929.
[28] O. T. Arulogun, O. N. Akande, A. T. Akindele, and T. A. Badmus, “Survey dataset on open and distance learning students’ intention to use social media and emerging technologies for online facilitation,” Data Brief, vol. 31, no. 1, pp. 1–8, 2020, doi: 10.1016/j.dib.2020.105929.
[29] C. Dong, S. Cao, and H. Li, “Young children’s online learning during COVID-19 pandemic: Chinese parents’ beliefs and attitudes,” Child Youth Serv Rev, vol. 118, no. 1, pp. 1–9, 2020, doi: 10.1016/j.childyouth.2020.105440.
[30] S. Muflih, S. Abuhammad, S. Al-Azzam, K. H. Alzoubi, M. Muflih, and R. Karasneh, “Online learning for undergraduate health professional education during COVID-19: Jordanian medical students’ attitudes and perceptions,” Heliyon, vol. 7, no. 9, p. e08031, 2021, doi: 10.1016/j.heliyon.2021.e08031.
[31] S. Muflih, S. Abuhammad, S. Al-Azzam, K. H. Alzoubi, M. Muflih, and R. Karasneh, “Online learning for undergraduate health professional education during COVID-19: Jordanian medical students’ attitudes and perceptions,” Heliyon, vol. 7, no. 9, p. e08031, 2021, doi: 10.1016/j.heliyon.2021.e08031.
![]()
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Risk Factors for Maternal Mortality in Indonesia: Systematic Review
Dewi Nopiska Lilis1, Nesi Novita2*, Ekadewi Retnosari2
1Department Midwifery, Health Polytechnic of Jambi, Indonesia
2Department Midwifery, Health Polytechnic of Palembang, Indonesia
Corresponding author: Nesi Novita, Jalan Jenderal Sudirman KM 3,5 Nomor 1365 Samping Masjid Ash-Shofa Komplek RS Moh. Hoesin Palembang, 30114, Indonesia
ORCID: https://orcid.org/0000-0002-1572-5448
Email: nesinovita51@gmail.com
Cite this article
ABSTRACT
Background: Seventeen Sustainment Development Goals are a joint agreement from countries around the world. Maternal mortality is included in Sustainment Development Goals3, whereby in 2030, the number is expected to decrease significantly. A systematic study has yet to be conducted in Indonesia to assess the factors involved in maternal mortality. This review focuses on the question, what are the risk factors, and which ones exert the most significant influence on maternal mortality in Indonesia?
Methods: This systematic review was conducted using the Preferred Reporting Items Checklist for Systematic Review and Meta-Analysis Protocol) involving studies published between 2000 and 2021 through Embase, Scopus, Web of Science, Cochrane library, Medline, ScienceDirect, Google scholar, and Wiley Online Library, in English version. Study quality was assessed using the National Institutes of Health controlled intervention study. The risk of study bias was also assessed using The Risk of Bias in Non-randomized Studies – of Exposure tool.
Results: There are 334,105 publications were discovered at initial search. Ten articles were finally eligible for further analysis. Risk factors included in the modifiable category including Prior medical history (40% of ten studies; OR range 3.322 – 20.143), pregnancy complications (40% of ten studies; OR range 2.31 – 9.75), delivery complications (30% of ten studies; OR range 5.08 – 8.5), puerperal complications (20% of ten studies; OR 4.19 – 4.382), parity (30% of ten studies; OR 0.25 – 33.949), Birth space (20% of ten studies; OR 0.49 – 5.806), Nutritional status (20% of ten studies; OR 1.37 – 13.256), delayed referral (30% of ten studies; OR 4.01 – 7.135), living area (30% of ten studies; OR 0.989 – 7.41), number of doctors (10% of ten studies; OR 0.99), triage response time (10% of ten studies; OR 1.88), Obst. resident response time (10% of ten studies; OR 1.02), and ICU waiting time (10% of ten studies; OR 1.01). Meanwhile, the most striking non-modifiable risk factor is the mother’s age (40% of ten studies; OR 0.27 – 2.792).
Conclusion. The study describes some of the modifiable risk factors that can be used in the country’s health policies to improve the quality-of-care activities.
Keywords: Risk factors, pregnant women, maternal deaths, systematic review, Indonesia
INTRODUCTION
In 2017, around 295,000 maternal deaths occurred globally, reflecting a Maternal Mortality Ratio (MMR) of 211 per 100,000 live births in 185 countries [1]. The global MMR between 2000 and 2017 fell by an average of 2.9% per year, with the global number of maternal deaths in 2017 estimated to be 35% lower than in 2000 [2]. MMR is significantly higher in low- and middle-income countries (LMICs), with sub-Saharan Africa and southern Asia accounting for 86% of all maternal deaths [2,3]. Evidence suggests that several high-income countries (HIC) are also experiencing increases in MMR, mostly among vulnerable populations [4].
Maternal death has significant negative social and economic consequences on society, and on the health and life of families, especially in newborns, especially in conditions of socioeconomic deprivation [5–7]. The MMR is a significant public health indicator that reflects both the quality of healthcare services and the status and interests of women in their society [2]. The priority given to reducing maternal mortality is shown by its choice as one of the seventeen Sustainment Development Goals (SDGs) [8]. There is evidence that the risk of maternal mortality is closely related to pregnancy and childbirth and the low quality of health services, which needs serious attention [9]. However, little is known about time trends in the immediate postpartum 42-day period to identify when more adequate follow-up is needed to reduce mortality. A systematic review of causes of maternal death up to 2012 identified that 73% of maternal deaths were caused by direct obstetric causes, such as bleeding, hypertensive disorders, and sepsis [10]. In general, 40% to 45% of maternal deaths occur between the onset of labour and the 24 hours immediately after birth [11]. Much of this evidence focuses on LMICs where the risk of death for women during the postpartum period is significantly higher [1].
In LMICs, coverage for essential health care interventions for women (e.g., skilled birth care providers) has increased, with a global emphasis on the SDGs and support for the Every Woman Every Child (EWEC) initiative [12]. However, global estimates show lower coverage for interventions targeting the postpartum period, with a further reduction in coverage of postpartum visits for women compared to newborns [12]. Understanding when and why death and severe morbidity postpartum can influence policies and recommendations to promote high-quality health care coverage. The current WHO recommendation is for postpartum care to be provided within the first 24 hours after birth in a health facility or within 24 hours if the delivery is at home, followed by a minimum of three postpartum contacts that occur within 48 to 72 hours, between days 7 and 14, and 6 weeks after birth [1].
This study aims to systematically examine the risk factors for maternal mortality in Indonesia. This review contributes to the body of knowledge on maternal mortality, especially in the Indonesian context. This review also may inform policymakers and healthcare practitioners in Indonesia about the current state of maternal mortality, its causes, and potential interventions. Preliminary results from our review indicate that no previous systematic review has been conducted on the determinants or causes of maternal death in Indonesia. Previous review studies presented in a proceeding focused on social and cultural factors that are determinants of maternal mortality in Indonesia, where the perceptions of mothers and families are the focus of the results of the review found [13].
The implication of this review for nurses including to serve better understanding the common causes of maternal mortality which may help nurses better prepare for obstetric emergencies. This includes recognizing when immediate action is needed and responding effectively to save lives.
The review’s findings can emphasize the importance of ongoing education and training for nurses in maternal healthcare. It can lead to the development of targeted training programs focusing on maternal health and emergency response.
This review focuses on the question, what are the risk factors for maternal mortality in Indonesia?
MATERIALS AND METHODS
We conducted a systematic review following the preferred reporting items for systematic reviews and meta-analyses, the PRISMA statement version 2020 [14].
Searching strategy
Databases used in collecting relevant literature include Embase (accessed January 2023), Sciencedirect (accessed January 2023), Cochrane library (Central) (accessed March 2023), Medline (accessed April 2023), Scopus (accessed June 2023), Web of Science (accessed June 2023), Google scholar (accessed June 2023), and the Wiley Online Library (accessed June 2023). In addition, we also conducted a hand-searching through the bibliography of relevant studies.
Our search was limited to English-language studies. In supporting a more focused literature search, the PICOS statement includes maternal deaths that occur in healthcare facilities and without intervention as in experimental studies because they focus on observational studies. Studies comparing maternal outcomes with live births were also included in this review.
The defined keywords adhere to the Mesh term for health research. The keywords being used are varied because they are tailored to the search engine. The keywords focus on factors related to maternal death including pregnancy, childbirth, delivery of health care, facilities AND maternal mortality OR maternal death.
Eligibility Criteria
For the inclusion criteria, we included observational studies. Eligible studies should meet the following criteria:
- Population: pregnant women, or anyone else who can give accurate information.
- Intervention: with or without any intervention which related to the factors of maternal mortality in Indonesia.
- Comparison: results. The study must explain the analysis results regarding the relationship between existing factors and maternal mortality, regardless of whether it is significant.
- Written in English and published in peer-reviewed journals.
The exclusion criteria including all studies that reported incomplete information regarding the factors and the association, duplicate publications, systematic reviews, commentaries, and letters to editors that did not provide primary data. The pooled studies were then grouped by category including maternal characteristics, history of pregnancy and childbirth, and family characteristics.
Outcome Measures
The outcome of each study was assessed for its significance level based on the p-value, or the magnitude of the risk through the OR value. We also looked at the frequency of the most common factor in the studies reviewed. Additionally, we also examined the postpartum period, focusing on maternal deaths, to ascertain the most prevalent time of mortality.
Selection Process
Two authors (NN, ER) independently screened each record (title/abstract), and if there is confusion regarding the information in the abstract, then the author reads further in the main text. This screening process uses the benefits of Mendeley software. Disagreement between the two authors resolved through discussion the first author (DNL). Screening is done by adjusting the title, objectives, and conclusions. The screening focus was based on the inclusion criteria of this systematic review.
Data Extraction and synthesis
Two independent authors (NN, ER) conducted the extraction. The extraction items consist of First author/year, country, study design (observational design), sample size, age, determinants, and outcomes. Discrepancies among those two authors are resolved by consensus after consulting with first author (DNL) when failed to meet an agreement. The first author will recheck the extraction results to ensure completeness.
Quality of evidence
Methodologically, two authors independently assessed the article quality using tools from the National Institutes of Health (NIH) on controlled intervention studies [15]. The first author will be the final decider of the quality of the included studies. There is an assessment sheet for assessing the methodology and compliance with the inclusion criteria of this study. Scores <30% of the criteria were classified as “poor”, scores between 30 and 70% were classified as “moderate”, and scores >70% were classified as “good” study quality. We agreed to include articles that fall into the “fair” and “good” categories.
Risk of bias
Using The Risk Of Bias In Non-randomized Studies – of Exposure (ROBINS-E) tool [16]. Each bias domain in ROBINS-E is addressed using signaling questions to gather important information about the study and the analysis being assessed. Many signaling questions have answer choices of ‘Yes’, ‘Maybe yes’, ‘Probably no’, ‘No’ and ‘No information’. For these, ‘Yes’ and ‘Maybe yes’ have the same implications for risk of bias and ‘No’. ‘No’ and ‘Probably not’ have the same implications for the risk of bias; the distinction enables the user to distinguish between situations in which definitive information is available from situations in which judgments are made. Other signaling questions have different response options specific to the question, which can be used to distinguish between different risks of bias.
RESULTS
The Identified Outcomes
A systematic electronic search identified that 95,948 publications were discovered through backward searching of relevant papers. The full-text screening was conducted on 746 articles. A total of 654 articles failed to meet eligibility criteria at the full-text screening stage, and only 10 articles were finally eligible for further analysis. The search results follow the PRISMA 2020 flow diagram (Figure 1).
General Characteristics
There are ten eligible studies that included in this review (Table 1). The studies are retrospective studies regarding maternal death history based on secondary data available in healthcare facilities. More than five million participants participated in the studies included in this review, where the overall age of pregnant women analyzed was in the range of 15 to 49 years. Most of the studies use a case-control approach to be able to compare how the influence of factors related to maternal mortality in the control group [17–22]. The data sources used by the studies in this review are varied, including medical records[11,17–22], National survey [23], Interview [19,20,24,25], verbal autopsy [19,24].

Figure 1. PRISMA flow diagram for literature search





*ANC= Ante Natal Care; KMS= Kartu Menuju Sehat (Toddler health-record card); OVM= Otopsi Verbal Maternal (Maternal verbal autopsy); MMR= Maternal Mortality Rate; ICU= Intensive Care Unit; OR=Odds Ratio; CI= Confidence Interval
Table 1. Characteristics of the studies included.
Study quality assessment
Based on the results of the study quality assessment, overall the included studies were in the study quality between Moderate to High. The result of RoB assessment presented in Table 2. There are three studies with only 12 “Yes” answer indicating a Moderate quality, and the rest is with 13 “Yes” means a high quality.

*Y= yes; NR= Not reported
Table 2. Summary of Study Quality Assessment
Risk of Bias Assessment
Most of the studies included in this review are in the Some Concerns category (Baharuddin et al., 2019; Diana et al., 2020; Ikhtiar & Yasir, 2015; Iswati et al., 2020, Mawarti et al., 2017, [26]. There are four studies that are in the Low Risk of Bias category [17,18,22,23]. Following are the results of the Risk of Bias assessment using the ROBINS E Tool presented in the form of a Traffic Light plot (Figure 2).
Risk Factors of maternal mortality
Based on what was obtained in the studies collected, it is known that several factors are related to the incidence of maternal mortality in Indonesia, which are then categorized into Modifiable and Non-modifiable risk factors. Based on the compiled studies, it is evident that modifiable factors are the most significantly associated risk factors with maternal mortality rates in Indonesia (Table 3).

Figure 2. Traffic-Light Plot for Risk of Bias Result.


Table 3. Risk Factors of Maternal mortality in Indonesia
Risk factors included in the modifiable category including prior medical history (40% of ten studies; OR range 3.322 – 20.143), pregnancy complications (40% of ten studies; OR range 2.31 – 9.75), delivery complications (30% of ten studies; OR range 5.08 – 8.5), puerperal complications (20% of ten studies; OR 4.19 – 4.382), parity (30% of ten studies; OR 0.25 – 33.949), Birth space (20% of ten studies; OR 0.49 – 5.806), Nutritional status (20% of ten studies; OR 1.37 – 13.256), delayed referral (30% of ten studies; OR 4.01 – 7.135). Regarding facilities, several categories of modifiable risk factors include living area (30% of ten studies; OR 0.989 – 7.41), number of doctors (10% of ten studies; OR 0.99), triage response time (10% of ten studies; OR 1.88), Obst. resident response time (10% of ten studies; OR 1.02), and ICU waiting time (10% of ten studies; OR 1.01). Meanwhile, the most striking non-modifiable risk factor is maternal age (40% of ten studies; OR 0.27 – 2,792).
Place of the maternal mortality
Based on the ten studies included, most place of mothers death was in the health care facilities including hospitals (Astuti et al., 2017; Bazar, 2012; Noferi Kusnadi & Sulistyowati, 2019; Mawarti et al., 2017; Baharuddin et al., 2019), Public Health Center (Cameron et al., 2019; Diana et al., 2020; Ikhtiar & Yasir, 2015; Palimbo et al., 2019), and Clinic [20].
Outcome Measures
Information regarding maternal mortality, including assessment of research outcomes using medical records (Astuti et al., 2017; Bazar, 2012; Ikhtiar & Yasir, 2015; Palimbo et al., 2019; Mawarti et al., 2017; Baharuddin et al., 2019 ), National survey (Cameron et al., 2019), interview and observation (Diana et al., 2020; Ikhtiar & Yasir, 2015; Iswati et al., 2020; Kusnadi & Sulistyowati, 2019), Maternal verbal autopsy (Diana et al. al., 2020; Ikhtiar & Yasir, 2015), and Mother-Toddler health-record card (Diana et al., 2020; Iswati et al., 2020).
DISCUSSION
Maternal mortality is the result of complications during and after pregnancy and childbirth. Most of these complications develop during pregnancy and can be prevented or treated. Other complications may exist before but worsen during pregnancy, especially if not treated as part of the woman’s care. Not only that but maternal mortality can also be influenced by other factors that are indirectly related to the mother’s physique.
This review has collected scientific evidence from published studies on maternal mortality in Indonesia in the last twenty years. In this review, various variations of factors associated with the incidence of maternal mortality were found. These various factors have been tried to be classified to make it easier to understand and as a guide to overcoming this problem systematically, especially for those who have authority.
Mother-related factors
After analyzing descriptively, the results of the studies collected, factors from within the mother are the most decisive factor related to the incidence of maternal mortality. Variables included in this factor include age, level of knowledge and education, pregnancy complications, delivery complications, medical history, and nutritional status.
Obstetric complications, namely pregnancy, childbirth, and postpartum complications, are risk factors for maternal death [27]. Obstetric complications directly resulting in maternal death are as much as 75% of all maternal deaths. Medical intervention can prevent such deaths [25]. The main complications that cause almost 75% of all maternal deaths are heavy bleeding (mostly bleeding after delivery), infection (usually after delivery), high blood pressure during pregnancy (pre-eclampsia and eclampsia), complications from childbirth, and unsafe abortion [10].
In this review, it was found that complications in pregnancy were a frequent factor found in almost all the studies included in this review. Ikhtiar & Yasir stated that mothers who experience pregnancy complications would be ten times at risk of experiencing death compared to mothers who do not experience pregnancy complications [19].
The nutritional status of pregnant women is also a factor associated with maternal mortality. This condition is associated with a lack of nutritional intake during pregnancy, such as anaemia and chronic energy deficiency. Anaemia in pregnancy has been associated with higher rates of maternal mortality, perinatal mortality, premature birth, preeclampsia, low birth weight, small live birth for gestational age (SGA), and cesarean delivery [28–32].
Socio-economic-cultural factors
The factors that fall into this category based on the results of the studies included in this review include husband/family support, economic/family income status, occupational status, and referral status.
The role of the husband and family in the mother’s pregnancy is crucial because it relates to the mother’s desire to have a pregnancy check-up. In several studies conducted in countries such as Asia and Africa, husbands and families hold full power to determine what pregnant women should do because, usually, this is related to some cultural or customary rules that apply in specific regions or tribes. Husband and family’s knowledge about pregnancy and various types of problems is essential to increase as a counterweight in making a decision that might conflict with the beliefs they live by [33–36].Support from the husband while the mother is in the hospital can increase the mother’s social support. Even though the role is unclear psychologically in influencing the birth process, it was reported that physical support and feelings could speed up the process of cervical opening, minimise complications, and add to the mother’s sense of optimism [37].
Individual socioeconomic status has a robust protective effect [3,38]. According to Kusnadi and colleagues, a family income below the minimum standard has five times the risk of experiencing maternal death [26]. Lack of family income has implications for the lack of meeting family nutritional needs, costs for carrying out pregnancy checks, and costs for childbirth, including transportation costs [39,40].
Factors of health facilities and services
This category includes antenatal care, living area/residence, family planning, referral status, response time, diagnosis, laboratory test results, treatment and intervention were given, health worker-oriented, administrative/supply, transportation, and patient-oriented factors. Antenatal care (ANC) is highly recommended for pregnant women in places that carry it out according to their regions. Through ANC, various information and education related to pregnancy and childbirth preparation can be given to mothers as early as possible. Lack of knowledge about the danger signs of pregnancy often occurs due to a lack of ANC visits. Lack of ANC visits can cause harm to the mother and fetus, such as bleeding during pregnancy, because no signs of danger are detected [41].
A study in Mozambique stated that the delays in referrals for pregnant women were related to the management of the referral process, which was characterized by frequent fuel stocks running out and lack of ambulance maintenance or even no functioning in the District[42]. A study conducted by Bazar and colleagues stated that in Palembang, most of the deaths occurred within <48 hours after hospital admission, which indicates that most of the referrals were delayed or late referrals [17]. The high maternal mortality rate in Indonesia indicates the low quality of health services. It is considered impossible to reduce without an effective referral system, especially in cases with complications [43,44].
Studies in Tanzania show that more than a quarter of maternal deaths are caused by late referrals from lower care facilities to higher care facilities, long distances to facilities and poor infrastructure [45,46]. In practice, long distances to health facilities, poor communication and transportation infrastructure continue to complicate timely access to health services due to delays [38,47]. In addition, it shows a weak healthcare system that contributes to the poor management of this condition in regional and district-level hospitals. In addition, most health facilities in low- and middle-income countries cannot offer safe and effective care to women with obstetric complications due to limited resources [48,49].
CONCLUSION
Understanding the causes and contributing factors to maternal death is critical to developing interventions and funding to reduce maternal mortality. The results of this review study highlight the importance of paying attention to the causes of maternal death in Indonesia in higher proportion. In particular, maternal deaths due to pregnancy complications require special attention because these causes are responsible for half of all maternal deaths in Indonesia. This study also summarizes the results of an analysis that examines the relationship between maternal mortality and maternal characteristics as well as facilities and health services in Indonesia and shows that factors within the mother (age, level of knowledge and education, complications of pregnancy, complications of childbirth, medical history, and nutritional status), Socio-economic-cultural factors (husband/family support, economic/family income status, occupational status, and referral status), and Factors of health facilities and services (Antenatal care, living area/residence, family planning, referral status, response time, diagnosis, laboratory test results, treatment and intervention given, health worker-oriented, administrative/supply, transportation, and patient-oriented factors) are related to maternal mortality. In addition to the need for a national study to determine the factors associated with maternal mortality, specific differences in the determinants of death between districts and provinces should be considered.
LIMITS AND STRENGTH
The studies collected were small and not of high quality, so caution should be exercised in using the results of this review. However, by analyzing the factors related to maternal mortality in Indonesia, this study can become a starting point to examine further the factors frequently emerging in most studies included in this review.
Registration
This work has been archived in https://osf.io/thpfa/, DOI 10.17605/OSF.IO/THPFA
Author’s Contribution
All authors equally contributed to preparing this article.
Funding
This review did not receive financial support from any party.
Conflict of Interest
There is no conflict of interest.
REFERENCES
- World Health Organization. Trends in maternal mortality 2000 to 2017: estimates by WHO, UNICEF, UNFPA, World Bank Group and the United Nations Population Division. World Health Organization; 2019. Available from: https://www.unfpa.org/featured-publication/trends-maternal-mortality-2000-2017#:~:text=The%20global%20maternal%20mortality%20ratio%20in%202017%20is%20estimated%20at,ratio%20was%202.9%20per%20cent.
- World Health Organization. Trends in maternal mortality: 1990 to 2013 [Internet]. Estimates by WHO, UNICEF, UNFPA, The World Bank and the United Nations Population Division. 2020. Available from: https://openknowledge.worldbank.org/handle/10986/18203
- Ronsmans C, Graham WJ, group LMSS steering. Maternal mortality: who, when, where, and why. The lancet. 2006;368(9542):1189–200.
- Hoyert DL, Miniño AM. Maternal mortality in the United States: changes in coding, publication, and data release, 2018. 2020;
- Sliwa-Hahnle K, Anthony J. Late maternal deaths: a neglected responsibility. The Lancet. 2016;2072–3.
- National Research Council. The consequences of maternal morbidity and maternal mortality: report of a workshop. 2000.
- Ahmed I, Ali SM, Amenga-Etego S, Ariff S, Bahl R, Baqui AH. Alliance for Maternal and Newborn Health Improvement (AMANHI) mortality study group. Population-based rates, timing, and causes of maternal deaths, stillbirths, and neonatal deaths in south Asia and sub-Saharan Africa: a multi-country prospective cohort study Lancet Glob Health. 2018;6(12):e1297-308.
- United Nations. The seventeen Goals [Internet]. Department of Economic and Social Affairs. Sustainable Development. 2022. Available from: https://sdgs.un.org/goals
- Freedman LP, Waldman RJ, De Pinho H, Wirth ME, Chowdhury AMR, Rosenfield A. Transforming health systems to improve the lives of women and children. The Lancet. 2005;365(9463):997–1000.
- Say L, Chou D, Gemmill A, Tunçalp Ö, Moller A-B, Daniels J, et al. Global causes of maternal death: a WHO systematic analysis. The Lancet global health. 2014;2(6):e323–33.
- Baharuddin M, Amelia D, Suhowatsky S, Kusuma A, Suhargono MH, Eng B. Maternal death reviews: A retrospective case series of 90 hospital‐based maternal deaths in 11 hospitals in Indonesia. International Journal of Gynecology & Obstetrics. 2019;144:59–64.
- Requejo J, Diaz T, Park L, Chou D, Choudhury A, Guthold R, et al. Assessing coverage of interventions for reproductive, maternal, newborn, child, and adolescent health and nutrition. BMJ. 2020 Jan 27;368.
- Takaeb AEL. Exploration of Socio-Cultural Determinants of Maternal Mortality in Indonesia. In: 5th International Conference on Tourism, Economics, Accounting, Management and Social Science (TEAMS 2020). Atlantis Press; 2020. p. 482–7.
- Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. International Journal of Surgery. 2021;88:105906.
- National Heart and Blood Institute L. Study Quality Assessment Tools [https://www. nhlbi. nih. gov/health-topics/study-quality-assessment-tools]. Accessed; 2019.
- Wang WW, Zhou QX, Ma L, Feng SH, Yang ZR, Sun F, et al. Introduction of a tool to assess Risk of Bias in Non-randomized Studies-of Environmental Exposure (ROBINS-E). Zhonghua liu Xing Bing xue za zhi= Zhonghua Liuxingbingxue Zazhi. 2022;43(1):98–104.
- Bazar A. Maternal Mortality and Contributing Risk Factors. Indonesian Journal of Obstetrics and Gynecology. 2012;30(1):8-13
- Astuti SK, Aziz MA, Arya IFD. Maternal Mortality Risk Factors in Dr. Hasan Sadikin General Hospital, Bandung in 2009− 2013. International Journal of Integrated Health Sciences. 2017;5(2):52–6.
- Ikhtiar M, Yasir Y. Analysis of Maternal Mortality Determinants in Gowa District South Sulawesi Province, Indonesia. Am J Public Heal Res. 2015;3(3):113–5.
- Iswati I, Shaluhiyah Z, Agushybana F. Does Husband Affect Maternal Mortality? A Case Control Study in Indonesia. International Journal of Health, Education & Social (IJHES). 2020;3(9):59–71.
- Mawarti Y, Utarini A, Hakimi M. Maternal care quality in near miss and maternal mortality in an academic public tertiary hospital in Yogyakarta, Indonesia: a retrospective cohort study. BMC pregnancy and childbirth. 2017;17(1):1–8.
- Palimbo A, Salmah AU, Sari A. Determinant factors of maternal mortality from 2016 to 2017 a casecontrol study in Banjar regency. Indian Journal of Public Health Research and Development. 2019;10(1):1188–92.
- Cameron L, Contreras Suarez D, Cornwell K. Understanding the determinants of maternal mortality: An observational study using the Indonesian Population Census. PloS one. 2019;14(6):e0217386.
- Diana S, Wahyuni CU, Prasetyo B. Maternal complications and risk factors for mortality. Journal of Public Health Research. 2020;9(2):jphr-2020.
- Kumari K, Srivastava RK, Srivastava M, Purwar N. Maternal mortality in rural Varanasi: delays, causes, and contributing factors. Indian journal of community medicine: official publication of Indian Association of Preventive & Social Medicine. 2019;44(1):26.
- Noferi Kusnadi SHR, Sulistyowati S. Risk Factors of Maternal Death in Karanganyar, Central Java, Indonesia. Journal of Maternal and Child Health. 2019;4(6):499–506.
- Song H, Hu K, Du X, Zhang J, Zhao S. Risk factors, changes in serum inflammatory factors, and clinical prevention and control measures for puerperal infection. Journal of clinical laboratory analysis. 2020;34(3):e23047.
- Mahmood T, Rehman AU, Tserenpil G, Siddiqui F, Ahmed M, Siraj F, et al. The association between iron-deficiency anemia and adverse pregnancy outcomes: a retrospective report from Pakistan. Cureus. 2019;11(10).
- Patel M. anemia and underweight as determinants of pregnancy outcomes: cohort study in eastern rural Maharashtra. India, BMJ Open. (8):e021623.
- Vindhya J, Nath A, Murthy GVS, Metgud C, Sheeba B, Shubhashree V, et al. Prevalence and risk factors of anemia among pregnant women attending a public-sector hospital in Bangalore, South India. Journal of family medicine and primary care. 2019;8(1):37.
- Smith C. Anämie in der Schwanger-schaft begünstigt maternale und perinatale Komplikationen. Geburtsh Frauenheilk. 2020;80(03):252
- Harrison RK, Lauhon SR, Colvin ZA, McIntosh JJ. Maternal anemia and severe maternal morbidity in a US cohort. American journal of obstetrics & gynecology MFM. 2021;3(5):100395.
- Piane GM. Maternal mortality in Nigeria: a literature review. World Medical & Health Policy. 2019;11(1):83–94.
- Rahman AE, Perkins J, Islam S, Siddique AB, Moinuddin M, Anwar MR, et al. Knowledge and involvement of husbands in maternal and newborn health in rural Bangladesh. BMC pregnancy and childbirth. 2018;18(1):1–12.
- Marabele PM, Maputle MS, Ramathuba DU, Netshikweta L. Cultural factors contributing to maternal mortality rate in rural villages of Limpopo Province, South Africa. International Journal of Women’s Health. 2020;12:691.
- Teklesilasie W, Deressa W. Husbands’ involvement in antenatal care and its association with women’s utilization of skilled birth attendants in Sidama zone, Ethiopia: a prospective cohort study. BMC pregnancy and childbirth. 2018;18(1):1–10.
- Kristianingrum DY. The role of husbands in giving labor support. EMBRIO. 2021;13(1):39–45.
- Assarag B, Dujardin B, Delamou A, Meski F-Z, De Brouwere V. Determinants of maternal near-miss in Morocco: too late, too far, too sloppy? PloS one. 2015;10(1):e0116675.
- Collucci C. Brazil’s child and maternal mortality have increased against background of public spending cuts. British Medical Journal Publishing Group. 2018;362:k3583
- Hamal S. Decentralization of education in Nepal: A rein in a horse nose. Social Inquiry: Journal of Social Science Research. 2020;2(2):194–215.
- Sinambela M. Pengaruh Tingkat Kecemasan dan Mekanisme Koping Ibu Primigravida terhadap Lamanya Kala I Persalinan Spontan di Klinik Bersalin Swasta Wilayah Kerja Puskesmas Delitua Kabupaten Deli Serdang Tahun 2013. 2013; Available from: https://repositori.usu.ac.id/handle/123456789/39218
- Chavane LA, Bailey P, Loquiha O, Dgedge M, Aerts M, Temmerman M. Maternal death and delays in accessing emergency obstetric care in Mozambique. BMC Pregnancy and Childbirth. 2018;18(1):1–8.
- Geller SE, Koch AR, Garland CE, MacDonald EJ, Storey F, Lawton B. A global view of severe maternal morbidity: moving beyond maternal mortality. Reproductive health. 2018;15(1):31–43.
- Howell EA. Reducing disparities in severe maternal morbidity and mortality. Clinical obstetrics and gynecology. 2018;61(2):387.
- Maro EW, Mosha NR, Mahande MJ, Obure J, Masenga G. Ten years trend in maternal mortality at Kilimanjaro Christian Medical Center Tanzania, 2003–2012: A descriptive retrospective tertiary hospital based study. Asian Pacific Journal of Reproduction. 2016;5(3):214–20.
- Urrio TF. Maternal deaths at Songea Regional Hospital, southern Tanzania. East African medical journal. 1991;68(2):81–7.
- Hirose A, Borchert M, Cox J, Alkozai AS, Filippi V. Determinants of delays in travelling to an emergency obstetric care facility in Herat, Afghanistan: an analysis of cross-sectional survey data and spatial modelling. BMC pregnancy and childbirth. 2015;15(1):1–13.
- Pembe AB, Paulo C, D’mello BS, van Roosmalen J. Maternal mortality at Muhimbili National Hospital in Dar-es-Salaam, Tanzania in the year 2011. BMC pregnancy and childbirth. 2014;14(1):1–7.
- Mgawadere F, Unkels R, Kazembe A, van den Broek N. Factors associated with maternal mortality in Malawi: application of the three delays model. BMC pregnancy and childbirth. 2017;17(1):1–9.
![]() This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
THE POTENTIAL OF ACTIVATED CHARCOAL MADE FROM INDONESIAN JAMBI FOREST WOOD FOR HOME-USE BLEACHING TEETH
Rina Kurnianti1, Retno Dwi Sari1, Mira Sri Gumilar1*
1Department of Dental Health, Health Polytechnic of Jambi, Indonesia
* Corresponding author: Mira Sri Gumilar, Jl. KH. Agus Salim no. 9 Kota Baru Jambi city, 36128, Indonesia, ORCID: https://orcid.org/0000-0002-0029-3099
Email: gumilarmirasri@gmail.com
Phone: +6281223339230
Cite this article
ABSTRACT
Introduction: Discoloration of the teeth can occur when stains damage the surface of tooth enamel. Developing treatment of teeth discoloration has increasingly due to discoloration teeth. Activated wood charcoal is one of the natural ingredients that can be used as an alternative to chemical home-use bleaching.
Objective: The purpose of this study was to obtain the effectiveness of activated charcoal made from tembesu wood and bulian wood for home-use bleaching teeth
Materials and Methods: This experiment was conducted at two locations: the Jambi Health Polytechnic Pharmacy Laboratory and the Jambi University Laboratory. It involved 60 samples, which were divided into six groups. The samples used in this research consisted of individuals with missing permanent teeth. The tooth color was assessed using the Vita Classical Shade Guide Tool. Charcoal derived from bulian wood and tembesu wood was mixed with toothpaste at concentrations of 10%, 20%, and 30%.
Results: Our results showed a significant teeth whitening in both groups, namely Tembesu wood and Bulian. Particularly, we found that Tembesu wood, when used at concentrations of 10%, 20%, and 30%, is highly effective in teeth whitening. Specifically, at a 10% concentration of Tembesu wood, teeth whitening displayed a notable increase from day four to day 10. Meanwhile, at concentrations of 20% and 30%, teeth whitening exhibited significant improvement from day two to 10. In the case of Bulian Wood, teeth whitening was similarly effective for concentrations of 10% and 20%, with noticeable enhancement from day two to 10. For the 30% concentration, teeth whitening effectiveness increased substantially, starting from day one and continuing through day 10. Finally, no statistically significant difference between the two groups was found (p>0.05).
Discussion: Tembesu wood and bulian wood at concentrations of 10%, 20%, and 30% are effectively used for teeth whitening, and there is no statistically significant difference between the two groups (p > 0.05).
Keywords: Activated charcoal, Bleaching teeth, Tooth whitening, Whitening toothpaste
INTRODUCTION
Tin-Oo MM et al [1] study performed in Malaysia showed that most of the participants were not satisfied with the color of their teeth, and need to use substance in whitening for their teeth. Healthy white color teeth make people more confident with their appearance. This reason encourages the desire for dental services, especially in aesthetic dentistry. Developing treatment of teeth discoloration has increasingly due to discoloration teeth. This condition drives a concern among patients and clinicians to improve dental aesthetics services.
Discoloration of the teeth can occur when stains damage the surface of tooth enamel [2]. The natural color of the teeth is polychromatic which differs in each third of the tooth based on the thickness and translucency of the enamel and dentin depending on the degree of calcification [3]. The natural color of teeth is bluish white in primary teeth and grayish yellow, grayish white or yellowish white in permanent teeth [4]. Changes in the natural color of the teeth differ according to their etiology and severity. It can be classified into extrinsic and intrinsic discoloration [4].
Tooth discoloration can be treated in several ways according to the diagnosis [5]. The treatment that is commonly conducted is chemical bleaching techniques. In this treatment oxidizing material can be used as a bleaching procedure to whiten the color of teeth by applying chemicals such as hydrogen peroxide and carbamide peroxide. The use of these chemicals has side effects such as hypersensitivity, cervical resorption, and external roots on teeth.
Numerous studies have indicated that incorporating light with bleaching gels does not result in significant improvements in the effectiveness of whitening procedures [6,7]. A recent systematic review and meta-analysis found that the use of light to activate the bleaching agent did not lead to better efficiency when compared to bleaching methods without light [8].
Activated wood charcoal is one of the natural ingredients that can be used as an alternative to chemical home-use bleaching because it has a high absorption effect on stains. Activated charcoal is a carbon material that can be produced from various raw materials containing carbon. One of the raw materials that can be used for activated charcoal is wood charcoal. Activated charcoal has been widely used as an absorbent for gas purification, water purification and oil purification due to its excellent absorption properties.
Jambi has commodity of Tembesu wood and Bulian wood as a timber forest product. The eminence quality of Tembesu wood and Bulian wood are characterized by its density. Now, utilization of these woods is still for the furniture or material house building. With this study we hope this commodity can be used for dental health. Activated charcoal can be used as a material for toothpaste, teeth whitening gel and others. This study can be a potential factor to develop dental health material product with local wisdom. Accordingly, the purpose of this study was to obtain the effectiveness of activated charcoal made from Tembesu wood and activated charcoal made from Bulian wood for home-use bleaching teeth.
MATERIALS AND METHODS
This research method was experimental research that was carried out in the Pharmacy Laboratory of Health Polytechnic of Jambi and in the laboratory of the Faculty of Engineering, University of Jambi. This study involved six groups of treatment that each group consisted of ten samples.
The samples of this study were permanent lost teeth, which were taken from the dental health clinic of Department Dental Health, Health Polytechnic of Jambi. The criteria for the teeth used in this study were permanent maxillary right first incisors (11), permanent maxillary right second incisors (12), permanent maxillary left first incisors (21), and permanent maxillary left second incisors (22). The condition of the teeth must be free of caries and calculus. The teeth used in this study were dipped with a 50% solution of Arabica coffee for a duration of 6 hours a day. This treatment repeated for 10 days. Each tooth was placed in a different container and the coffee solution was changed daily. To isolate from the coffee, the teeth’s roots covered with clear nail polish. After 10 days of immersion, the teeth were removed and washed with saline and then dried. The purpose of dipping teeth to coffee was to discolor the teeth, so before treatment each tooth had the same color. The measurement of color on teeth used the Vita Classical Shade Guide Tool.
The material of activated charcoal for this study was from Bulian wood and Tembesu wood. Bulian wood and Tembesu wood were one of the forest product commodities in Jambi Province, Indonesia. This study will examine the ability of activated charcoal to whiten teeth in concentrations of 10%, 20%, and 30%.
Bulian wood and Tembesu wood were processed into charcoal at 400°C for 12 hours. After the wood has turned into charcoal, then the charcoal was ground and sieved using Retsch to get a size of 200 meshes. Furthermore, the charcoal was activated through physical activation by heating in a furnace for three hours at a temperature of 800°C. This process converted bulian wood and tembesu wood to be activated charcoal. Activated charcoal was left in a desiccator for 15 minutes.
The product of activated charcoal will be mixed with toothpaste at concentrations at 10%, 20%, and 30% both in Bulian and Tembesu wood. By this treatment, the study had six groups that were intervened. The intervention for each group consist of 10% bulian wood activated charcoal, 20% Bulian wood activated charcoal, 30% Bulian wood activated charcoal, 10% Tembesu wood activated charcoal, 20% Tembesu wood activated charcoal, and 30% Tembesu wood activated charcoal.
Treatment was done by applying toothpaste contain of activated charcoal in certain concentration to the tooth surface by brushing at a pressure of 300 to 400 N/m2 on all teeth. Tooth-brushing is done in small circular motions for 2 minutes, then allowed to stand for 10 minutes and then rinsed with running saline water. This treatment was repeated for 10 days. The data of score white tooth level measured by Vita Classical Shade Guide Tool.
Ethical considerations
This research was approved by ethics No. LB.02.06/2/98/2022 from Health Polytechnic of Jambi, Jambi Province, Indonesia.
Statistical analysis
Data were presented as numbers or percentages for categorical variables. Continuous data are expressed as the mean ± standard deviation (SD), or median with Interquartile Range (IQR). Prior to the statistical test, a data normality test was carried out using the Kolmogorov-Smirnov test which aims to assess the distribution of data in a group of data or variables, whether the data distribution is normally distributed or not. From normality test, the data had normal distribution, so the collected data analyzed using the repeated measures Anova test. If the Anova test for was significant (p<0.05) the post hoc Anova test was performed for pairwise comparison. Finally, to test the differences between Tembesu and Bulian wood, we used the independent t test.
We considered all tests with p<0.05 as significant. We analyzed all data using SPSS statistical software ver. 16.
RESULTS
The research results can be presented in the following table:

Table 1. Data normality test results
Table 1 shows that the p-value is >0.05, it means all variables are normally distributed, thus the statistical test used is the parametric test.
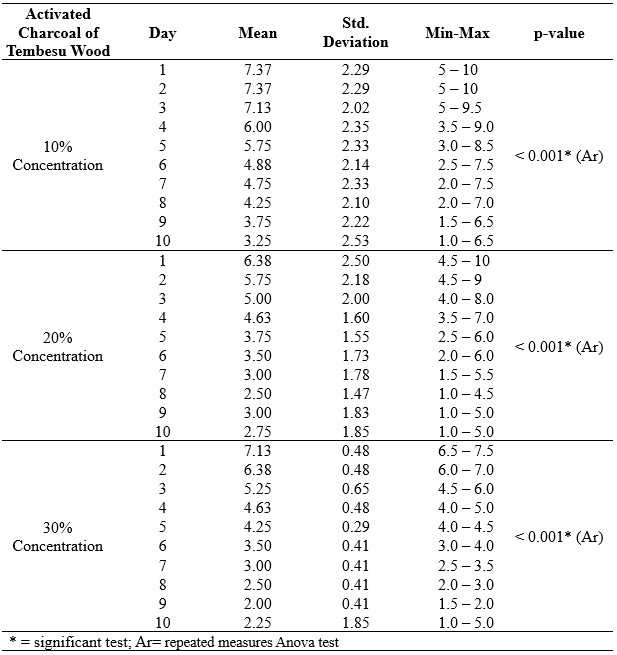
Table 2. The Results of the repeated measures Anova test for Tembesu Wood Activated Charcoal Group at 10%, 20% and 30% of concentration.
The table illustrates that the results of the tests were less than 0.001, indicating the effective utilization of tembesu wood at concentrations of 10%, 20%, and 30% for teeth whitening between 1 and 10 days of use. Specifically, by post hoc Anova test we found for the 10% concentration of tembesu wood, a noticeable enhancement in teeth whitening effectiveness from day four to day 10. Similarly, for tembesu wood concentrations of 20% and 30%, there was a significant improvement in teeth whitening efficacy from day two to day 10 (p<0.05).
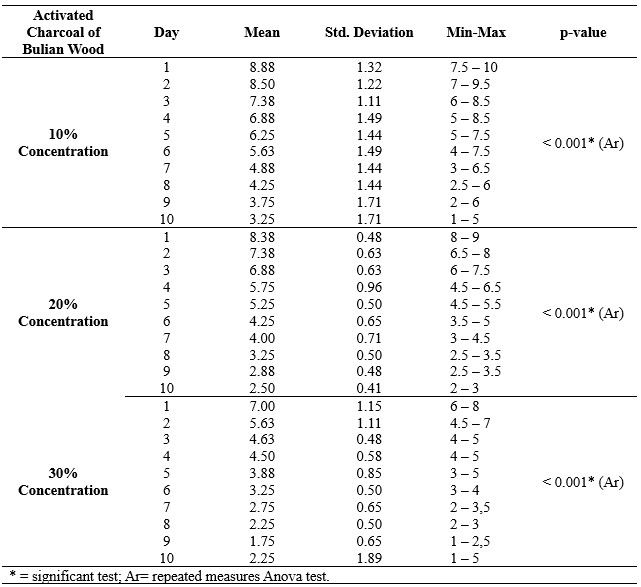
Table 3. The Results of the repeated measures Anova test for Bulian Wood Activated Charcoal Group at 10%, 20% and 30% of concentration.
The table shows that the results of the statistical tests were less than 0.05, indicating that bulian wood, when used at concentrations of 10%, 20%, and 30%, is highly effective for teeth whitening between 1 and 10 days of use. In the case of tembesu wood, by post hoc Anova test at concentrations of 10% and 20%, we found an improvement in teeth whitening effectiveness from day two to day 10. Conversely, at a concentration of 30%, teeth whitening exhibited a significant increase in effectiveness, starting from day one and extending through day 10.
In table 4, we reported the comparison between Tembesu Wood and Bulian Wood group, for each day at 10%, 20% and 30% of concentration.
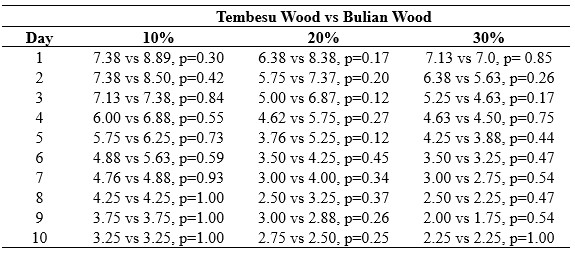
Table 4. Comparison between Activated Charcoal of Bulian Wood and Activated Charcoal of Tembesu Wood, to identify for each concentration (10%, 20%, 30%).
Table 4 shows that there is no statistically significant difference between tembesu wood and bulian wood when used at concentrations of 10%, 20%, and 30% over the course of the first ten days, as indicated by a p-value > 0.05.
DISCUSSION
Five groups in this study shown that activated charcoal could decrease the level color tooth score which was if its level decreased so the tooth was whiter. The group with the 10% concentration activated charcoal of Tembesu wood could not effectively decreased the color tooth score in ten days.
Tembesu wood and bulian wood had a different minimum effectiveness concentration and duration of use activated charcoal toothpaste. Tembesu wood was effective minimum concentration for bleaching teeth at 20% concentration. In this concentration, need 8 days to whitening the teeth. 30% Activated charcoal of Tembesu wood could whiten the teeth in two days.
Bulian wood had minimum concentration that can decrease the color tooth score at 10% concentration in eighth days. If we were using 20% concentration and 30% concentration, the effectiveness of bleaching teeth could reach in three days. The other study shown that activated charcoal toothpaste can remove stain from resin composite.
Activated charcoal is a porous solid containing 85-95% carbon, produced from carbon-containing materials such as hardwood trees and coconut shells. In medicine, activated carbon has been used for ‘universal antidote’ in cases of poisonings, as a filter aid agent, and in decolorization processes [9,10]. This advantage of activated charcoal is from their adsorptive ability. Activated wood charcoal is one of the natural ingredients that can be used as an alternative to chemical home bleaching because it has a high absorption effect on stains [11,12].
Bulian wood and Tembesu wood are wood that is widely available in Jambi Province. The eminence quality of Tembesu wood and Bulian wood are characterized by the dense of their wood. Now, utilization of that wood is still for the furniture or material house building[13]. With this study we hope this commodity can be use for dental health. Activated charcoal can using as a material for whitening toothpaste, teeth whitening gel and others. With this innovation, it can be a potential factor to develop dental health material with local wisdom [14].
Activated charcoal is a broad-spectrum agent that effectively binds to many pollutant compounds like organic, inorganic, biological and microbial. The efficiency of absorption from these substances is influenced by various factors such as pH, ionic strength of saliva, dispersion time, modification procedure, physical properties include surface area and porosity and chemical properties of activated charcoal. The advantage of activated charcoal is that it has a strong binding capacity so that when applied to the tooth surface, a significant change in the color of tooth enamel will be obtained [11,15,16].
The chemical bleaching teeth usually used carbamide peroxide, which is a combination of hydrogen peroxide and urea. The use of these chemicals has side effects such as hypersensitivity, cervical resorption, and external roots on teeth [17,18]. Another advantage is that there is no limit to consumption. When swallowed up to 100 grams will not cause any side effects. This is because activated charcoal is not absorbed by the body, but activated charcoal absorbs all dirt, oil, toxins in the digestive tract, toxins in the body, so activated charcoal is proven to be safe when it is in the mouth and in contact with the teeth within 5 minutes to perform a tooth whitening procedure [19,20].
The most important property of activated charcoal is absorption. In this case, there are several factors that affect the adsorption capacity such as porous solid, which mostly consists of free carbon elements, and each is covalently bonded. Thus, the activated charcoal surface is non-polar. In addition to composition and polarity, pore structure is also an important factor to consider. The pore structure is related to the surface area, the smaller the pores of the activated charcoal, the larger the surface area. Thus, the adsorption speed increases. To increase the adsorption speed, it is recommended to use activated charcoal that has been pulverized. The amount or dose of activated charcoal used, is also considered [21–23].
Except for whitening the teeth, brushing teeth with activated charcoal can reduce plaque. Based on the data of 2013 National Health Research reported peoples in Indonesia have a good behavior of brushing teeth with proportion was 93.8%, but its correctly was very poor that only 2.3% [24]. In this situation, the good appearance of teeth must be followed by the health of teeth. Because the good condition of teeth is good color and be spared from the diseases like caries. Good condition of teeth is dependent on people’s behaviour.
CONCLUSION
Dental nurses can actively fulfill their role in providing oral health education to effectively maintain dental health by utilizing natural materials rooted in local wisdom, such as Tembesu and Bulian wood. It is crucial for the public to recognize the significance of dental health improvement, as it is closely intertwined with one’s quality of life. Healthy teeth contribute to self-confidence and alleviate discomfort for both individuals and those around them. Dental nurses must persuade the public that attaining good dental health is attainable at a minimal cost and through straightforward methods of preparing the materials. Additionally, these research findings can serve as a foundation for the development of packaged toothpaste derived from Tembesu and Bulian wood by dental nurses.
In this study was observed that, both tembesu and bulian wood, when utilized at concentrations of 10%, 20%, and 30%, proved effective for teeth whitening, while no significant differences were observed between the two treatments (p > 0.05).
Study limitation
The limitation of this study lies in the relatively small number of samples.
Funding statement
This research did not receive any specific grant from funding agencies in the public, commercial, or not for profit sectors.
Conflict of interest
The authors report no conflict of interest.
Authors’ contribution
RIK, RDS and MSG carried out initial observations, defined problems, and conceptualized research topics, RDS, MSG developed research instruments, and collected data in the field, RIK analyzed data. RIK, MSG compiled the manuscript. All authors finalized the manuscript and approved it.
Acknowledgements
The author would like to thank all the staff of the dental health clinic of Department Dental Health, Health Polytechnic of Jambi who were involved in this research. Also to the President of Health Polytecnic of Jambi who has given permission for this research.
REFERENCES
- Tin-Oo MM, Saddki N, Hassan N. Factors influencing patient satisfaction with dental appearance and treatments they desire to improve aesthetics. BMC oral health. 2011;11(1):1–8.
- Dalrymple A, Bean E-J, Badrock TC, Weidman RA, Thissen J, Coburn S, et al. Enamel staining with e-cigarettes, tobacco heating products and modern oral nicotine products compared with cigarettes and snus: An in vitro study. Am J Dent. 2021;34(1):3–9.
- Chen H, Liu Y. Teeth. In: Advanced ceramics for dentistry. Elsevier; 2014. p. 5–21.
- Mortazavi H, Baharvand M, Khodadoustan A. Colors In Tooth Discoloration: A New Classification And Literature Review. International Journal of Clinical Dentistry. 2014;7(1).
- Rodríguez‐Martínez J, Valiente M, Sánchez‐Martín M. Tooth whitening: From the established treatments to novel approaches to prevent side effects. Journal of Esthetic and Restorative Dentistry. 2019;31(5):431–40.
- Gonçalves RS, Costa CAS, Soares DGS, Santos PH dos, Cintra LTA, Briso ALF. Effect of different light sources and enamel preconditioning on color change, H2O2 penetration, and cytotoxicity in bleached teeth. Operative dentistry. 2016;41(1):83–92.
- Maran BM, Burey A, de Paris Matos T, Loguercio AD, Reis A. In-office dental bleaching with light vs. without light: A systematic review and meta-analysis. Journal of dentistry. 2018;70:1–13.
- Maran BM, Ziegelmann PK, Burey A, de Paris Matos T, Loguercio AD, Reis A. Different light-activation systems associated with dental bleaching: a systematic review and a network meta-analysis. Clinical oral investigations. 2019;23:1499–512.
- Thakur A, Ganeshpurkar A, Jaiswal A. Charcoal in dentistry. Natural Oral Care in Dental Therapy. 2020;197–209.
- Oremosu OA, Umesi DC, Oderinu OH, Banjo SA. Dental implants as tooth replacement option among patients in government hospitals Lagos, South-West Nigeria. European Journal of Prosthodontics. 2016;4(1):7.
- Viana ÍEL, Weiss GS, Sakae LO, Niemeyer SH, Borges AB, Scaramucci T. Activated charcoal toothpastes do not increase erosive tooth wear. Journal of dentistry. 2021;109:103677.
- Epple M, Meyer F, Enax J. A critical review of modern concepts for teeth whitening. Dentistry journal. 2019;7(3):79.
- Ismail I, Habriyanto H, Badaruddin B. Strategi Pemenuhan Kelangkaan Bahan Baku Industri Kecil Mebel Kayu di Kecamatan Jambi Luar Kota Kabupaten Muaro Jambi. UIN Sulthan Thaha Saifuddin Jambi; 2021.
- Tomás DBM, Pecci-Lloret MP, Guerrero-Gironés J. Effectiveness and Abrasiveness of Activated Charcoal As A Whitening Agent: A Systematic Review of In Vitro Studies. Annals of Anatomy-Anatomischer Anzeiger. 2022;151998.
- Lestari U, Syamsurizal S, Trisna Y. The Antiplaque Efficacy and Effectiveness of Activated Charcoal Toothpaste of Elaeis guineensis in Smokers. Indonesian Journal of Pharmaceutical Science and Technology. 2021;1:75–87.
- Agrawal P, Panda S, Mishra SR. A Review On Activated Charcoal Tooth Paste. World Journal of Pharmaceutical Research. 2018;7(9):478-481.
- Siregar. Efektivitas Penggunaan Pasta Gigi Arang Aktif (Activated Charcoal) Terhadap Perubahan Warna Gigi Pada Masyarakat Kampung Belawan Bahagia Kecamatan Medan Belawan Tahun 2020. 2020;
- Ameli N, Kianvash Rad N, Nikpour F, Ghorbani R, Mohebi S. Effect of Short-and Long-term Use of Home and In-Office Bleaching with Carbamide Peroxide and Hydrogen Peroxide on Enamel Microhardness. Journal of Dentistry Indonesia. 2020;27(2):50–5.
- Alshamsi ZAN, Walke S. Utilization of Food Waste For Production of Activated Carbon. International Journal of Electrical Engineering and Technology (IJEET). 2021;12(7):88–95.
- Ajayi DM, Gbadebo SO, Adebayo GE. Perception about tooth colour and appearance among patients seen in a tertiary hospital, South-West, Nigeria. The Pan African Medical Journal. 2021;38.
- Zellner T, Prasa D, Färber E, Hoffmann-Walbeck P, Genser D, Eyer F. The use of activated charcoal to treat intoxications. Deutsches Aerzteblatt International. 2019;116(18):311.
- Toxicology AA of C, Toxicologists EA of PC and C. Position paper: single-dose activated charcoal. Clinical Toxicology. 2005;43(2):61–87.
- Mohammad-Khah A, Ansari R. Activated charcoal: preparation, characterization and applications: a review article. Int J Chem Tech Res. 2009;1(4):859–64.
- Kementrian Kesehatan RI. Laporan Nasional hasil Riskesdas 2013 [Internet]. Jakarta: Badan Penelitian dan Pengembangan kesehatan; 2013. Available from: https://pusdatin.kemkes.go.id/resources/download/general/Hasil Riskesdas 2013.pdf.Last accessed: 1 June 2022.
![]() This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
ANALYSIS OF HOSPITAL ANTIBIOTIC PRESCRIPTIONS AFTER THE IMPLEMENTATION OF STEWARDSHIP: A RETROSPECTIVE OBSERVATIONAL STUDY IN TWO HOSPITALS IN NORTH-EASTERN SICILY
Salvatore Coppolino1*, Veronica Crucitti1, Febronia Federico1,
Emanuele Leotta1, Nadia Caporlingua2
- Unità Operativa Semplice (U.O.S.) Farmacia, Presidio Ospedaliero Barone Ignazio Romeo, Messina (Italy).
- Unità Operativa Semplice (U.O.S.) Farmacia, Presidio Ospedaliero Mistretta, Messina (Italy).
* Corresponding author: Salvatore Coppolino, Dirigente Farmacista, Presidio Ospedaliero Barone Ignazio Romeo, Via Giuseppe Mazzini, 14 Patti (Me) sacoppolin@yahoo.it
Cite this article
ABSTRACT
Introduction: Antimicrobial resistance is a global problem caused by the inappropriate use of antibiotics. To combat this phenomenon, multidisciplinary antimicrobial stewardship programmes have been initiated, the primary objectives of which include improving both the level of appropriateness of prescription and clinicians’ awareness of the correct use of antibiotics.
Objective/Purpose: The objective of the work was to conduct an analysis of antibiotic consumption at hospital level to assess the appropriateness of antibiotic prescription in a number of Operational Units.
Method: From 01/01/2021 to 31/12/2022, data were extracted from the Pharmacy Operational Unit’s management software on the dispensing of antibiotics (injectable and oral use), the Defined Daily Doses, and the number of dosage units dispensed to the General Medicine, Intensive Care, General Surgery and Neurorehabilitation Operational Units of two hospitals.
Results: Total antibiotic consumption was 7,845 dosage units in 2021 and 10,182 in 2022. The comparison of the defined daily dose values (4,565,485 in 2021 and 5,079,671 in 2022) is indicative of the use of antibiotics with different dosages, with a percentage increase of 11.3%. A comparison was also made between the Defined Daily Doses/100 bed-days delivered in 2021 and the regional and national figures, yielding a significantly lower figure than these latter figures.
Conclusions: The loss of antibiotic efficacy threatens to throw healthcare systems into crisis, leading to in an increase in morbidity and mortality from infections. The implementation of antimicrobial stewardship programmes remains, at present, the best tool to harness in order to curb the phenomenon of antimicrobial resistance. There is therefore a need for increasingly specialised professionals in the field of infectious diseases. Nurses and pharmacists play a crucial role in antimicrobial stewardship programmes, as they collaborate not only in the implementation of antimicrobial guidelines, but also in the review of individual patient regimens in order to optimise treatment and in the training of healthcare personnel on the appropriate use of antimicrobials.
Keywords: antimicrobial resistance, antimicrobial stewardship, antibiotics, appropriateness of prescription
INTRODUCTION
Antimicrobial resistance is a growing global public health problem that could lead, unless action is taken, to 10 million deaths a year by 2050 [1,2].
It is a complex phenomenon with a multifactorial genesis: the increased use of antibiotics (including inappropriate use), the spread of hospital infections with antibiotic-resistant micro-organisms (and the limited control of these infections), and the increase in international travel with the consequent increased spread of strains. Many pathogens are also simultaneously resistant to several classes of antibiotics (multidrug resistance) [3].
The resistance of bacteria to antibiotics can be divided into two types: natural (or innate) resistance and acquired resistance.
Acquired resistance is the result of clonal selection due to the selective pressure exerted by the drug and can be broken down into chromosomal resistance, which accounts for about 10-15% of all resistance, and extra-chromosomal resistance, which accounts for about 90% of all resistance and is mediated by gene sequences in plasmids or transposons (mobile genetic elements) [4,5].
The mechanisms whereby microorganisms become resistant to antibiotics include the production of antibiotic-inactivating enzymes (the production of ꞵ-lactamases, for example, is one of the most widespread resistance mechanisms. The enzyme hydrolyses the ꞵ-lactam ring, a pharmacophore, resulting in the loss of activity of the molecule); altered envelope permeability; altered targeting (altering the DNA gyrase by substituting a single amino acid makes the enzyme resistant to quinolone antibiotics); active transport systems (protein-coding genes that act as efflux pumps for antibiotics) and alternative metabolic pathways.
The Italian periodic national surveillance report (AR-ISS), published in 2021 by the Istituto Superiore di Sanità, highlighted the main pathogens (Staphylococcus aureus, Streptococcus pneumoniae, Enterococcus faecalis, Enterococcus faecium, Escherichia coli, Klebsiella pneumoniae, Pseudomonas aeruginosa and Acinetobacter species) responsible for the phenomenon of antimicrobial resistance, the use of which should be closely monitored.
In 2021, 33.1% of Klebsiella pneumoniae isolates and 8.8% of Escherichia coli isolates were multi-resistant to third-generation cephalosporins, aminoglycosides and fluoroquinolones; for Pseudomonas aeruginosa, the percentage of resistance to three or more antibiotics (piperacillin/tazobactam, ceftazidime, carbapenems, aminoglycosides and fluoroquinolones) was 11.4%; a high percentage of multi-resistance (fluoroquinolones, aminoglycosides and carbapenems) (85.4%) was observed for Acinetobacter species. The national figures on carbapenem-resistant Enterobacteriaceae (CRE) infections reported as many as 2,192 cases in 2021, confirming the widespread occurrence of carbapenem-resistant Enterobacteriaceae bacteraemia in Italy, especially in hospitalised patients [6].
Inappropriate use of antibiotics is associated with unfavourable outcomes, such as death, treatment failure and adverse reactions, resulting in an increased burden of care on the healthcare system, duration of antibiotic therapy and duration of hospitalisation [7,8]. It
also promotes the selection of resistant strains and the spread of antimicrobial resistance [9,10].
In Italy, the high levels of antibiotic resistance and antibiotic consumption require urgent prevention and monitoring action. Despite the downward trend, consumption continues to be higher than the European average, both in the human and veterinary sectors, with considerable interregional variability. Furthermore, in European maps of the distribution of resistant bacteria in Europe, Italy holds, together with Greece, the record for the spread of resistant germs. One of the main causes behind the increase in resistance in Italy and worldwide is the excessive use of antibiotics, especially after the emergency linked to the COVID-19 pandemic. To combat antimicrobial resistance, so-called “Antimicrobial Stewardship” (AS) [11] programmes have been initiated. These represent a series of interventions aimed at promoting and monitoring the correct choice of antibiotic, dosage and duration of treatment to preserve the future effectiveness of these molecules in real-life everyday clinical practice [12,13].
The Antimicrobial Stewardship Team (AST) is a multidisciplinary corporate body that must include an infectious disease specialist, a hospital pharmacist, a hygiene specialist, a nurse and a clinical microbiologist [13,14].
The primary objectives are to improve the level of appropriateness of prescription and clinical and microbiological indicators, to increase awareness among healthcare professionals on the correct use of antibiotics and the prevention of care-related infections, and to reduce costs due to short- and long-term clinical complications. Each member of the AST Team must cooperate with the corporate Hospital Infection Committee (HIC) for the activities within their competence. The resolution establishing the AST must define the responsibilities and methods of cooperation with the corporate HIC. It is of paramount importance that there is no ambiguity of roles between the AST and the HIC at corporate level, and that both maintain well-defined and closely interconnected areas of activity established by each individual health authority.
At local level, the Sicily Region, with Local Government Decree no. 703 of 04/08/2020, has drawn up a regional guideline document for the organisation of corporate AS programmes, setting out the lines of action to be followed by all companies. These include the implementation of the antimicrobial stewardship corporate function and the appointment of departmental representatives for each individual Operational Unit, represented by a doctor and a nurse, increased audits and feedback on the appropriateness of prescription, the establishment of lists of high-concern antibiotics, the implementation of a structured and informed system for infectious disease consultancy, the preparation of semi-annual reports, the drafting of corporate protocols for antibiotic therapy and prophylaxis and empirical therapy in hospitalised patients, company training and impact assessments [15].
With the CRE Regional Directive (DASOE/8/21932), in implementation of the circular of the Ministry of Health no. 1479 of 17/01/2020, the Sicily Region has initiated a surveillance programme for bacteraemias caused by carbapenem-resistant Enterobacteriaceae (CRE). The Directive provides for the collection of case reports on the regional territory, data analysis, monitoring, dissemination and evolution of infections, with periodic transmission of the data to the Italian National Health Institute (Istituto Superiore di Sanità) [16].
All the actions undertaken by the Sicily Region form part of the 2020-2025 Regional Prevention Plan, which represents the main planning, prevention and health promotion tool, as it places the citizen at the centre of the interventions, accompanying them throughout all phases of life, with the aim of achieving the highest level of health. The Regional Plan envisages, by 2025, the establishment of AST in all Regional Health Authorities [17].
Objective/Purpose
The objective of the work was to conduct an analysis of the consumption of antibiotics in certain Operational Units at the “Barone Ignazio Romeo” Hospital in Patti and the “San Salvatore” Hospital in Mistretta, part of the Provincial Health Authority of Messina, to assess the appropriateness of their use per Operational Unit.
MATERIALS AND METHODS
Sampling and eligibility
A retrospective observational analysis was conducted between 01/01/2021 and 31/12/2022.
The data were obtained from the consumption of antibiotics provided by the hospital pharmacies at the hospitals concerned in the five Operational Units considered.
Tools
For the implementation of this study, paper prescription forms for injectable antibiotics and the consumption of both antibiotics administered both intravenously (i.v.) and orally (p.o.), provided by the Pharmacy Operational Units of the two hospitals in Patti and Mistretta, were considered.
The injectable antibiotic prescription form used for administration bears the patient’s initials, the required active substance, the number of vials, the dosage, the duration of treatment, and whether it is targeted treatment or empirical treatment. The data on the dispensing of antibiotics by the two Pharmacy Operational Units, both for injection and oral use, to the General Medicine, Intensive Care, General Surgery and Neurorehabilitation Operational Units of the Patti and Mistretta Hospitals, facilities belonging to the Messina Provincial Health Authority (ASP), were extracted from the corporate management software. The number of beds per single Operational Unit and per year are shown in Table 1.

Table 1. Numbers of beds in different Operational Units at Patti and Mistretta hospitals
The data were collected by the researchers and processed in aggregate form for research purposes only. All the authors who took part in the observational study are hospital pharmacists, some with twenty years of service and a PhD in Pharmaceutical Sciences. All the authors have obtained the Specialisation in Hospital Pharmacy or in Pharmacology and Clinical Toxicology. To ensure confidentiality, each patient was assigned a number. For all the antibiotics dispensed, the Defined Daily Doses (DDDs) were considered, i.e. the average doses taken daily by an adult patient, with reference to the main therapeutic indication of the drug [18] and the number of dosage units dispensed to the individual Operational Units. Consumption was calculated as DDD/100 bed-days according to the scheme used by the Italian National Observatory on the Use of Medicines (OsMed) in the national report on the use of antibiotics in Italy for the year 2021[19].
Statistical Analyses
The data have been presented as numbers and percentages for categorical variables and in terms of the arithmetic mean in the case of continuous variables. For the management of our data, the calculation of DDDs, Delta (2022-2021) and Pareto diagrams were carried out using an Excel spreadsheet. In particular, the Pareto diagram was used to understand which factors could most influence our results.
RESULTS
Total antibiotic consumption was 7,845 dosage units in 2021 and 10,182 in 2022. The comparison of the DDD values (4,565,485 in 2021 and 5,079,671 in 2022) is indicative of the use of antibiotics at different dosage strengths, as an increase in DDD corresponds to an increase in the doses administered at different dosage strengths, allowing a comparison of consumption as it is a technical tool for measuring drug prescriptions. In 2022, there was a percentage increase of 11.3%. The analysis of DDDs was carried out on 100 bed-days provided per individual Operational Unit.
For Patti Hospital (Table 2), for the General Surgery department, 485,762 DDDs were provided in 2021 and 784.869 in 2022; for General Medicine, 1,817,933 DDDs in 2021 and 2,354,803 DDDs; for Intensive Care, 598,954 DDDs in 2021 and 736.244 DDDs in 2022; while for the Operational Unit of Mistretta Hospital (Table 3), 1,249,067 were provided for the General Medicine department in 2021 and 433.301 for 2022 and for the Neurorehabilitation department, 414.488 DDDs in 2021 and 770.457 DDDs in 2022.



Table 2. Comparison of antibiotic consumption in 2021 and 2022 at Patti Hospital.

Table 3. Comparison of antibiotic consumption in 2021 and 2022 at Mistretta Hospital.
For the year 2021, the consumption of DDD/100 bed-days in the Operational Units at the two hospitals examined was compared with the regional data and with the national data based on the findings of the 2021 National Report “The use of antibiotics in Italy” produced by OsMed [20]. The DDD/100 bed-days provided in 2021 was 70.6 at national level; in the Sicily Region it was 81.6, while in the Operational Units we examined it was 44.3.
The analysis of the data shows for Patti Hospital an increase in the consumption of amoxicillin/clavulanic acid, both p.o. and i.v. (Δ%=0.47), piperacillin/tazobactam (Δ%=1.23) and levofloxacin (Δ%=0.5) in General Surgery. An increase in the use of third-generation cephalosporins (Δ%=1.68), ciprofloxacin, both p.o. and i.v. (Δ%=1.21%), gentamicin (Δ%=0.73), linezolid and (Δ%=0.2) piperacillin/tazobactam (Δ%=1.54) was observed in General Medicine. Finally, an increase in the use of third-generation cephalosporins (Δ%=0.81), ciprofloxacin (Δ%=0.2), gentamicin (Δ%=0.06) and piperacillin/tazobactam (Δ%=1.35) was also observed in Intensive Care.
For Mistretta Hospital, there was no significant difference in Δ% between 2021 and 2022, only a clear reduction in the consumption of ceftriaxone (Δ% = -6) in General Medicine and an increase in amoxicillin/clavulanic acid, both p.o. and i.v. (Δ%=0.98%), and an increase in ertapenem (Δ%=0.61%) in Neurorehabilitation. From the prescription forms viewed, it was found that empirical prescriptions correspond to 92.8%, while those based on antibiogram evaluation only account for 7.2% of total prescriptions. Parenteral Amoxicillin/Clavulanic acid is used for otitis, sinusitis and COPD (chronic obstructive pulmonary disease), Cefazoline for respiratory tract infections and peritonitis, ceftazidime for gram-negative bacteria and Pseudomonas infections and for surgical interventions; ciprofloxacin for COPD, respiratory and urinary tract infections; gentamicin as a broad-spectrum antibiotic; meropenem for staphylococcal and streptococcal infections; piperacillin/tazobactam for pneumonia; teicoplanin for resistant Staphylococcus aureus infections. Further analysis was carried out on antibiotics for injectable use that required the use of prescription forms to monitor their appropriate use. The following antibiotics were considered: ciprofloxacin, colistin, fosfomycin, imipenem/cilastatin, levofloxacin, linezolid, meropenem, teicoplanin, tigecycline and vancomycin.
A comparison between 2021 and 2022 was performed using the Pareto diagram (Figure 1 and 2).

Figure 1. Pareto diagram of injectable antibiotics under monitoring for the years 2021 and 2022.
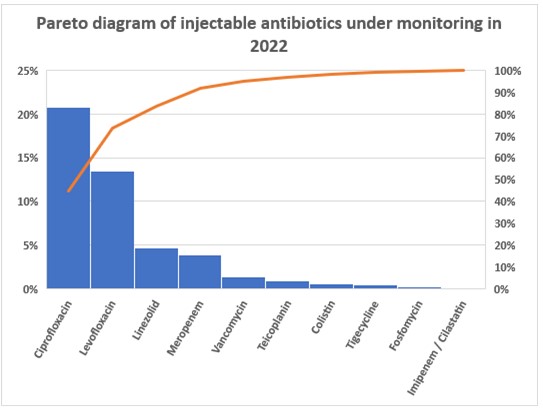
Figure 2. Pareto diagram of injectable antibiotics under monitoring for the years 2021 and 2022.
The Pareto diagrams showed that in 2022, there was a reduction in prescriptions for ciprofloxacin, levofloxacin and tigecycline. Increases were found for linezolid and meropenem. For the other antibiotics, prescriptions have remained constant or have undergone slight increases.
DISCUSSION
The analysis of paper prescription forms shows a consumption based more on empirical treatment (92.8%) than on antibiogram evaluations (7.2%), a situation that has prompted further corrective action by the AST and HIC, such as compulsory antibiograms for the antibiotics vancomycin, tigecycline, teicoplanin, meropenem, linezolid and the combination imipenem/cilastine.
Furthermore, for high-cost injectable antibiotics, such as fosfomycin or the meropenem/vaborbactam combination, a specific prescription form has been drawn up, in which certain requirements must be fulfilled by the patient to be eligible for that treatment, so that these antibiotics are reserved for cases where there are no valid treatment alternatives. Analysis of the Pareto diagrams showed that the use of the prescription form proved to be a valuable tool for improving appropriateness of prescription.
Although COVID-19 put the appropriate use of antibiotics at risk, especially in the early stages of the pandemic – for instance the improper use of azithromycin – hospital pharmacists and nursing coordinators worked hard to draw up and implement internal protocols on the use of antibiotics in Operational Units to ensure their rational use.
Hospital pharmacists and nursing coordinators play a crucial role in antimicrobial stewardship (AS) programmes, as they are involved in the development and management of antimicrobial guidelines, the review of individual patient regimens to optimise treatment, and the training of healthcare personnel on the appropriate use of antimicrobials.
The results from the cohort examined show that to ensure appropriate use and targeted treatment, thus avoiding the phenomenon of antibiotic resistance, it is necessary to isolate the bacterium responsible for the infection and carry out an antibiogram before administering certain antibiotics to hospitalised patients. Specifically, this procedure concerns vancomycin, tigecycline, teicoplanin, meropenem, linezolid, levofloxacin, the imipenem/cilastatin combination, fosfomycin, colistimethate and ciprofloxacin.
The AS strategy, which has been followed in our hospitals to date, involves a careful and thorough patient assessment, the choice of the most suitable antimicrobial to be prescribed, its administration and the monitoring of the patient once treatment has begun. This last phase includes the possibility of reducing the duration of antimicrobial treatment, converting the route of administration from intravenous to oral, modifying the dose based on any clinical conditions that might affect the patient’s pharmacokinetics, such as excretory system deficiencies, monitoring the use of the prescribed antibiotic, monitoring adherence to treatment, and informing the patient on the appropriate use of antimicrobials [21,22]. The hospital pharmacist plays a crucial role in the fight against antibiotic resistance by acting as a link between the clinician and the microbiology laboratory. This surveillance activity results in a positive effect on how antibiotics are prescribed by healthcare professionals, leading to a reduction in hospital infections.
The use of antibiotics must also be monitored in real-life everyday clinical practice. The nursing coordinator collects and reports to the hospital pharmacist any adverse reactions to antibiotics to confirm or otherwise the initial risk/benefit ratio with which the drug was marketed.
CONCLUSIONS
The effects of resistance, i.e., the inability of antibiotics, administered at therapeutic doses, to reduce survival or inhibit the replication of pathogenic bacteria, can be observed worldwide. Recently, the phenomenon has been further aggravated by their often inappropriate use.
The implementation of AS programmes in all health authorities remains, at present, the best tool to harness in order to curb the phenomenon of antimicrobial resistance.
The discovery of new molecules with antimicrobial activity capable of treating infections by multiresistant microorganisms is not an immediate tool; years of preclinical and clinical studies are required for a new molecule to be marketed. The phenomenon of antimicrobial resistance is urgent and requires an immediate solution to combat it. Increasingly more specialised figures are needed in the field of infectious diseases than just clinicians, and therefore hospital pharmacists and nursing staff must also be adequately trained to be able to give their best possible support in the battle against antimicrobial resistance.
LIMITATIONS
The work conducted is based on prescription forms and consumption data of antibiotics used by injection or orally. The work considers a limited geographical area. Lastly, a further limitation of the study is the lack of inferential analysis of our data.
Ethical considerations
No formal approval by the Local Ethics Committee was necessary for this type of study, since it is a publication concerning consumption data and aggregated data.
No economic incentives were provided for this analysis. Authorisation for the use of prescription forms was issued by the Hospital’s Medical Director, the consumption data derive from reports certified by the Corporate Management Control. The participants’ anonymity was ensured. The study was conducted in accordance with the ethical considerations of the Declaration of Helsinki.
Funding statement
This research did not receive any specific contributions from public, commercial or non-profit funding bodies.
Conflicts of interest
The authors do not report any conflicts of interest.
Contributions of the authors
All authors contributed equally to the production of this study.
REFERENCES
- Akpan, M.R., Ahmad, R., Shebl, N.A., et al. A review of quality measures for assessing the impact of antimicro- bial stewardship programs in hospitals. Antibiotics (Basel). 2016;5(1):5.
- O’Neill, J. Tackling drug-resistant infections globally: final report and recommendations. The review on antimicrobial resistance. 2016. https://amr-review.org/sites/default/files/160525_Final%20paper_with%20cover.pdf. Last accessed on July 23, 2023.
- Garau, J., Nicolau, D.P., Wullt, B., et al. Antibiotic stewardship challenges in the management of community-acquired infections for prevention of escalating antibiotic resistance. J Glob Antimicrob Resist. 2014;2(4):245–53.
- Antimicrobial resistance (AMR) Disponibile su: http://www.ecdc.europa.eu/en/activities/surveillance/EARS-Net/. Last accessed on August 19, 2023
- World Health Organization. Antimicrobial resistance Global Report on surveillance 2014. http://www.who.int. Last accessed on August 08, 2023.
- Aspetti epidemiologici in Italia Sorveglianza nazionale dell’Antibiotico-Resistenza (AR-ISS) https://www.epicentro.iss.it/antibiotico-resistenza/epidemiologia-italia. Last accessed on August 19, 2023.
- Spoorenberg, V., Hulscher, M.E, Akkermans, R.P., Geer- lings SE. Appropriate antibiotic use for patients with urinary tract infections reduces length of hospital stay. Clin Infect Dis. 2014;58(2):164–9.
- Ortega, M., Marco, F., Soriano, A., Almela M., Martinez J.A., Munoz A. et al. Epidemiology and prognostic determinants of bacteraemic catheter-acquired urinary tract infection in a single institution from 1991 to 2010. J Infect. 2013;67(4):282–7.
- Dalfino, L., Bruno, F., Colizza, S., Concia E., Novelli A., Rebecchi F.S. et al. Cost of care and antibiotic prescribing attitudes for community acquired complicated intra-abdominal infections in Italy: a retrospective study. World J Emerg Surg. 2014; 9:39.
- Magill, S.S., O’Leary, E., Janelle, S.J., Thompson D.L., Dumyati G., Nadle J. et al. Changes in Prevalence of Health Care-Associated Infections in U.S. Hospitals. N Engl J Med. 2018; 379(18):1732-1744
- Karki, T., Plachouras, D., Cassini, A., Suetens C. Burden of healthcare-associated infections in European acute care hospitals. Wiener Medizinische Wochenschrift. 2019; 169: 3–5.
- Goff, D.A., Rybak, M.J. Global antimicrobial stewardship: challenges and successes from frontlinestewards. Infect Dis Ther. 2015;4(Suppl 1):1–3.
- Society for Healthcare Epidemiology of America. Infectious dis- eases society of America, pediatric infectious diseases society. policy statement on antimicrobial stewardship by the Society for Healthcare Epidemiology of America (SHEA), the Infectious Diseases Society of America (IDSA), and the Pediatric Infectious Diseases Society (PIDS). Infect Control Hosp Epidemiol. 2012;33(4):322–7.
- Dellit, T.H., Owens, R.C., McGowan, J.E., Gerding D.N., Weinstein R.A., Burke J.P. et al. Infectious diseases society of America and the society for healthcare epidemiology of America guidelines for developing an institutional program to enhance antimicrobial stewardship. Clin Infect Dis.2007;44(2):159–77.
- European Centre for Disease Prevention and Control. Proposals for EU guidelines on the prudent use of antimicrobials in humans, 2017. https://www.ecdc.europa.eu/en/publications-data/proposals-eu-guidelines-prudent-use-antimicrobials-humans. Last accessed on July 23, 2023.
- Decreto Assessoriale n. 703 del 04/08/2020 della Regione Sicilia http://pti.regione.sicilia.it/portal/page/portal/PIR_PORTALE/PIR_LaStrutturaRegionale/PIR_AssessoratoSalute/PIR_Infoedocumenti/PIR_DecretiAssessratoSalute/PIR_DecretiAssessoriali/PIR_DecretiAssessorialianno2020/DA%20N.%20703.pdf. Last accessed on July 23, 2023.
- Direttiva Regionale CRE (DASOE/8/21932) https://www.qualitasiciliassr.it/sites/doc/cre/direttiva_cre_dasoe21392_29042021.pdf. Last accessed on July 23, 2023.
- Piano Regionale della prevenzione 2020-2025. http://www.quadernidellasalute.it/portale/prevenzione/DELIBERE_PRP_2020-2025/Sicilia/Allegato_1-PRP_23_12_2020-2025_integrato.pdf. Last accessed on July 23, 2023.
- Gli strumenti: il metodo di classificazione secondo il sistema ATC/DDD Bollettino d’informazione sui farmaci. Anno IX N. 6. http://www.agenziafarmaco.gov.it/wscs_render_attachment_by_id/111.61850.1150390484813676c.pdf?id=111.61855.1150390485109. Last accessed on August 08, 2023.
- L’uso degli antibiotici in Italia Rapporto Nazionale Anno 2021. https://www.aifa.gov.it/documents/20142/1853258/Rapporto_Antibiotici_2021.pdf Last accessed on August 08, 2023.
- Gilchrist, M., Wade, P., Ashiru-Oredope, D., Howard P., Sneddon J, Whitney L. et al. antimicrobial stewardship from policy to ptice: experiences from UK antimicrobial pharmacists. Infect Dis Ther. 2015;4(Suppl 1):51–64.
- Barlam, T.F., Cosgrove, S.E., Abbo, L.M., MacDougall C., Schuet A.N., SeptimusEJ., et al. Implementing an antibiotic stewardship pro- gram: guidelines by the infectious diseases Society of America and the society for healthcare epidemiology of America. Clin Infect Dis. 2016;62(10): e51–77.
![]() This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Increasing Diversity at the Highest Levels of Nursing: Perspectives of a Doctor of Nursing Practice Graduate
Monica Jaramillo1*
- Independent Author, Florida, US.
*Corresponding Author: Monica Jaramillo DNP, MSN/Ed., RN-NLC, CNE®n, CCRN.
Instructor, mentor, and tutor of various healthcare programs. I am not affiliated with any institution when writing and submitting this manuscript to the NSC journal for open-access publication.
Florida, US. Email: MonicaJaramilloDNP@Gmail.com
Open Researcher and Contributor ID: https://orcid.org/0009-0005-0572-4061
Cite this article
Abstract
Introduction: There is a need to increase diversity at the highest levels of education in nursing to ensure competent transcultural services for the growing multicultural population worldwide. The Doctor of Nursing Practice (DNP) is a terminal degree that significantly impacts change advocacy. This commentary includes the perspectives of an immigrant nurse in her journey to completing a doctoral degree while contributing to diversity.
Discussion: Diversity, Equity, Inclusion, and Accessibility (DEIA) positively impacts nursing and healthcare systems at many levels. It is imperative to advocate for equal services for all individuals while inspiring nurses and other healthcare professionals to further their careers by achieving advanced education degrees conducive to propelling health services forward. The author seeks to inspire nurses worldwide to continue their educational journey and encourage immigrants to believe they can do it despite their fears and hesitation.
Keywords: Diversity; Equity; Inclusion; Accessibility; DEIA; Doctor of Nursing Practice.
Introduction
Immigrant nurses can face many challenges when trying to succeed in a place away from home, and this can negatively affect their desire to return to school and achieve higher degrees of education, especially terminal degrees such as the Doctor of Nursing Practice (DNP). Individuals moving to different countries must perform under the same standards as those with inherent language and culture.[1,2] Recent literature suggests that many challenges employees, employers, students, and organizations face regularly relate to the lack of adequate cross-culturalism competencies.[3] Furthermore, professionals from different geographic areas, such as Taiwan and Mexico, report experiencing multiple challenges in succeeding in scholarly endeavors with English as an additional language.[5] Accordingly, increasing diversity at all levels of health care and the nursing profession is imperative to ensure competent transcultural services for the growing multicultural population.[4] This article aims to inspire other nurses to pursue their call for further education while adding to diversity in nursing at the doctoral level worldwide. This author is a Latin-American intensive care nurse and nurse educator who completed the DNP program in the United States despite multiple fears resulting from being an immigrant nurse and a busy young mother in another country with English as an additional language. The author shares her journey through international open access, hoping it will inspire others experiencing any dilemmas related to Diversity, Equity, Inclusion, and Accessibility (DEIA) while considering achieving advanced education degrees. This commentary article includes a discussion and a conflict of interest statement while exploring the importance of taking the first step, believing in self, and abiding by solid values.
Discussion
Taking the First Step
Coming from a country where English is not the primary language can pose a significant barrier to diverse nurses from various geographic areas since advancing their careers in a different country by increasing their education without having the full command of the new language can slow down the learning process by adding fear and intimidation. In addition, English remains the dominant language for academic projects and scientific publications worldwide.[5] At first, the author experienced hesitation in enrolling in the DNP program due to language and other barriers that could arise due to disparities. But the persistent call to serve others and the burning passion for adding to diversity while advancing her career inspired her to take the first step. That initial decision was to continue advanced education programs like the master’s degree and related certificates until reaching the highest degree in nursing without forgetting to embrace her differences as an immigrant and follow her passion for the profession and service. Since then, the author has enjoyed inspiring nurses and allied health students to put their fears aside. After overcoming all fears and limiting beliefs, the author became a role model for other nurses. As a role model for the profession, the author has ensured excellence and professionalism in clinical and academic practices while engaging in life-long learning conducive to expanding knowledge, skills, and attitudes personally and professionally. In this author’s experience, taking the first step, per their individual goals and aspirations, can initiate a cascade of events that eventually will lead to empowerment and successful decisions.
Believing in Self
Another crucial element of success in higher education degrees is to believe in and honor the self. Self-confidence is vital to ensure not only the completion of projects but also positive outcomes.[6] In this author’s experience, this means being confident in individual abilities and embracing all skills and differences. Early in her educational journey, while living in a country away from home, the author learned that having a solid and positive relationship with herself was vital to her growth and expansion. Self-reflection while exploring innovative ways to cultivate self-love and self-motivation was crucial to her drive to complete all advanced nursing education. This author has always seen herself as a person with big dreams. Still, it was not until she started trusting in her competencies and believing she could accomplish anything that she started impacting herself and others around her. All nurses, immigrants or not, worldwide must believe in their abilities and capabilities while ensuring a positive self-image and respect for their differences.
Abiding by Solid Values
Values and beliefs are also vital components of successful educational pathways. Values in the nursing profession are essential foundations to ensure safe, effective, and meaningful practices.[7,8] This author knew she needed to be true to herself while expanding her nursing knowledge and skillsets, mainly since she lives far from most of her family and support systems. Since the author’s values represent the framework influencing her decisions as a nurse and student, she needed to align all core values with her selected terminal degree. For example, her values have always helped her carry out the nursing practice with integrity while doing what is best for everyone involved. Also, one of this author’s passions is translating research evidence into all professional practices with active participation in change advocacy conducive to diversity and equal opportunities for all human beings. Therefore, she sought advanced educational programs that would lead her to give back to the nursing profession through leadership, scientific publications, and professional endeavors while engaging in cutting-edge research, evidence-based practice, and professional literacy. The author is now using all those experiences and her background as an immigrant to contribute at a grander scale to diversity in nursing while advocating for others to join similar efforts.
Inspiration
In conclusion, these personal and professional stories seek to inspire many to believe in themselves and advocate for DEIA. Overcoming the fear of being an immigrant nurse in another country wanting to achieve a terminal degree of education entitles taking the first step, believing in self, and abiding by solid core values. The author sincerely hopes nobody lets their diverse and unique talents die without exploring and sharing them with the world. People can accomplish anything they desire with hard work and determination. The world needs diversity today more than ever, considering the growth of multicultural groups, and each nurse’s unique background can signify a tremendous contribution to inclusion at all levels of the nursing profession.
Funding Statement
This research received no external funding.
Conflict of Interest Statement
The author declares no conflict of interest.
References
- Larsen R, Mangrio E, Persson K. Interpersonal communication in transcultural nursing care in India: A descriptive qualitative study. Journal of Transcultural Nursing. 2020;32(4).
- Oducado RMF, Sotelo M, Ramirez LM, Habaña M, Belo-Delariarte RG. English Language proficiency and its relationship with academic performance and the nurse licensure examination. Nurse Media Journal of Nursing. 2020;10(1).
- Comeaux E, Grummert SE, Mireles DC. A critical review of the literature on cultural competency in student affairs: Toward transformative cultural responsiveness. Journal of Diversity in Higher Education. 2021.
- McFarland MR, Wehbe-Alamah HB. Leininger’s Theory of Culture Care Diversity and Universality: An overview with a historical retrospective and a view toward the future. Journal of Transcultural Nursing. 2019;30(6).
- Hanauer DI, Sheridan CL, Englander K. Linguistic injustice in the writing of research articles in English as a second language: Data from Taiwanese and Mexican researchers. Written Communication. 2018;36(1).
- Costa RR de O, Medeiros SM de, Coutinho VRD, Mazzo A, Araújo MS de. Satisfaction and self-confidence in the learning of nursing students: Randomized clinical trial. Escola Anna Nery. 2020;24(1).
- Poorchangizi B, Borhani F, Abbaszadeh A, Mirzaee M, Farokhzadian J. The importance of professional values from nursing students’ perspective. BMC Nursing. 2019;18(1).
- Turale S, Meechamnan C, Kunaviktikul W. Challenging times: Ethics, nursing and the COVID‐19 pandemic. International Nursing Review. 2020;67(2).
![]() This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Workplace Violence Experienced by Nurses in Northern Region Hospitals of Morocco: A Cross-Sectional Study
Safae Ouma1,2, Maria Leyre Lavilla Lerma 3, Nabil Benomar3 and Nabila Rouahi4,*
1 Higher Institute of Nursing Professions and Technical Sciences, ISPITS, Boulevard Abdelkhalaq Torres, Route de Martil, 93100, Tetouan, Morocco. safaeouma21@gmail.com
2 PhD student, Faculty of Health Sciences, University of Jaen, Campus Las Lagunillas s/n, 23071 Jaén, Spain.
3 Faculty of Health Sciences, University of Jaen, Campus Las Lagunillas s/n, 23071 Jaén, Spain; llavilla@ujaen.es; nben@ujaen.es
4 Higher Institute of Nursing Professions and Technical Sciences ( ISPITS Annexe Kenitra), Route de Casablanca, 10120, Rabat, Morocco. rouahinbl@gmail.com
* Correspondence : Rouahi Nabila (Rouahi N), Professor at Higher Institute of Nursing Professions and Technical Sciences ( ISPITS Annexe Kenitra), Route de Casablanca, 10120, Rabat, Morocco.
e-mail : rouahinbl@gmail.com
Cite this article
Abstract
Background: Workplace violence (WPV) perpetrated against health professionals is a major problem in health sector. It affects health and performance of workers. The aims of this study were: 1) to assess WPV facing nurses in the northern region of Morocco and 2) to identify the related factors.
Methods: We conducted a cross-sectional study in the northern region of Morocco from October to December 2021. In total, 391 volunteer nurses working in 13 hospitals were enrolled. A self-reported questionnaire, ‘Violent Incident Form’ (VIF), was distributed to the participants. It assesses verbal and physical violence.
Results: We obtained 98% response rate and 97% of the respondent nurses faced at least one WPV episode the last year. Verbal violence is the most common type of violence. Significant factors as age of the victims (c2 = 15.34; p = 0.038) and the assaulters (c2 = 27.66; p <0.001), and mental condition of the assaulter (c2 = 28.27; p = 0.003) were obtained. According to post hoc residual z test, nurses aged between 40 and 49 and over 60 y.o were more exposed to physical violence than other groups, while the aggressors were younger aggressors (19-30 y.o.) and over 60 ; wherears significant less frequent were cases of aggressors aged between 31 and 50 y.o.
Conclusion: A high exposure of nurses to WPV in northern Moroccan hospitals is noted. The significant factors of violence obtained must be considered for the control and prevention of WPV among nurses in Moroccan hospitals.
Keywords: Morocco; nurses; hospital; verbal violence; physical violence; workplace violence; questionnaire
Introduction
The Workplace violence (WPV) is a worldwide problem within the healthcare sector. The effect of this phenomenon on the performance of an organization makes it a serious issue that we should study in all dimensions. The World Health Organization classifies workplace violence into physical and non-physical violence [1]. This publication specifies that these categories of WPV include physical assault, homicide, verbal abuse, bullying/mobbing, sexual/racial harassment, and threatening behavior. The National Institute for Occupational Safety and Health also defines it as a violent act, including physical assaults and threats of assault directed toward persons at work or on duty [2]. Other classifications, based on the relationship between the two parties involved in the incident, are also known [3, 4].
The notified incidence of violence in the health sector constitutes almost a quarter of all the incidents of WPV perpetrated in all the other sectors [5]. Consequently, WPV affects the work demand [6], the quality of healthcare, and the psychological state of the health workers [7].
In health facilities, 52.2% to 87.3% of health workers reported an experience of physical violence during their careers. Many more are threatened or exposed to verbal abuse. Patients and visitors are responsible for a great number of incidents [8]. Pich and Roche [8] confirmed that all the categories of health workers are concerned with WPV, but the highest rate of reported cases is observed among nurses and midwives in both public and private sectors and different geographic areas.
According to Cebrino et al, a worldwide bibliometric analysis reveals that the number of studies on WPV perpetrated against healthcare personnel grew between 1992 and 2019 [9]. Most reported WPV factors include psychological setting, illness of the perpetrators, miscommunication, younger nurse age, and alcohol use [10]. Chapman et al. [11] identified the predicting behaviors that must alert nurses on the occurrence of a WPV incident and then help them manage it. It was found that nurses suffer from WPV approximately two times more than physicians [12]. Despite the growing interest and the high number of studies published on WPV perpetrated against healthcare workers, this phenomenon is still underestimated. According to Kvas and Seljak, this is due to unreported cases and a large tolerance of WPV among health professionals [13].
In Morocco, non-medical health professionals represent 56% of health human resources; physicians represent 22% and administrates 22% [14]. The first category of health personnel includes Nurses (69%), Midwives (16%), Health technicians such as medical analysis laboratory and imagery personnel (11%), rehabilitation personnel (4%), and social worker (1%). According to the same document, 60% are female gender and 40% are male gender.
The first study conducted in Morocco on WPV in the healthcare sector was published in 2010 [15]. Moroccan healthcare workers are at high risk of exposure to WPV [16]. A report on the Moroccan working environment showed a higher workload and higher stress levels in the workplace [17]. Additionally, the same authors observed the absence of an ergonomic workplace, the non-availability of resources, and the ignorance of consequences of exposure to violence in the Moroccan healthcare sector. The reality is that few data are available and published on WPV in the Moroccan health sector.
For a better control and prevention of this phenomenon, it is important to know the occurrence and the factors associated with WPV perpetrated against nurses in Moroccan hospitals. To intervene and manage these incidents as quickly as possible, nurses need to be able to know and identify factors that can alert them to the possibility that a violent incident may occur [11]. This interest is in line with policies issued by Moroccan Health authorities. Additionally, Moroccan high governmental authorities and health authorities adopted laws and procedures to be applied in the case of any kind of aggression facing health professionals in their workplace. The authorities adopted this strategy during the year 2021.
The study questions are 1) What is the occurrence of the WPV in northern region hospitals of Morocco and 2) What are the factors related to WPV among nurses exposed to WPV in the hospitals of this area. Only 1 study has investigated this phenomenon in Morocco, specifically in the emergency unit of the national hospital located in Rabat city.
Objectives
The aims of this study were 1) to assess the WPV perpetrated against nurses in hospitals of the northern area of Morocco and 2) to identify the related factors.
Materials and Methods
Study area, study design and tool
We performed a cross-sectional field study. The study was conducted in a geographic area located in the north-west of Morocco (35.2630° N, 5.5617° W). Mediterranean Sea borders this area from the north and the Atlantic Ocean from the west. Rabat-Salé- Kénitra region and Fès-Meknès region border the area from the southeast and the east. A total of 12.5 million of inhabitants live in this area. The estimated number of non-medical health professionals working in the hospitals of this area was 1749.
To achieve the aims of our study, we adopted a self-reported questionnaire, Violent Incident Form (VIF). This questionnaire was initially developed by Arnetz [18], and used after that in several WPV survey studies [7, 19, 20]. The VIF assesses verbal violence and physical violence (spitting, biting, kicking, scratching/pinching, slapping/hitting punching, pushing, restraining, use of object or weapon, others). It reports also the circumstances, perpetrator, reactions and consequences of the violence. The questionnaire consists of 18 questions with binary (Yes/No) or multiple-choice responses. One section describes the characteristics of the victim and the aggressor. The other section describes the related factors of WPV experienced by nurses over the preceding 12 months.
Authorizations and ethical consideration
In accordance with the Declaration of Helsinki, we first obtained the authorization of the Regional Health Authorities and the approval of the Ethics Committee (protocol code 28/2021). Anonymous identification, data protection, and voluntary participation were ensured. Additionally, all the participants in the study gave their written agreement to participate in the survey by filling out a consent form.
Subjects, sampling, recruitment and data collection procedure
Participants were enrolled according to these inclusion criteria: being nurse and working for at least 2 years in the hospital as full-time worker. We excluded nursing students and nursing trainees. We unexpectedly visited the hospitals of the study area. The procedure to recruit the eligible subjects is the following. We went to each nurse’s supervisor in each hospital and asked him to distribute, among the eligible nurses, the pack of supports and tools of this survey. The individual pack contained the VIF questionnaire, along with a cover letter and a consent form. The sample size was estimated by Bernoulli sampling [21], according to the following formula.

We considered the central value of the prevalence interval as the representative value of the interval, i.e. 70%, IC=95%, Z-score 1.96 and a Δ=5%. In this way the minimum size was estimated equal to 323 nurses. We expanded the estimated sample up to 379 to reduce any statistical bias, due to any questionnaires not completed or with missing data. In this regard, we distributed 391 questionnaires. We recruited 387 volunteers and consenting nurses. The nurses were asked to describe the most significant WPV incident that they experienced during the 12 months preceding the study, as indicated in the VIF. Among the volunteers, 379 nurses experienced a WPV incident. They completed the questionnaire independently and anonymously. Afterwards, they deposited the completed questionnaires in a sealed box that we previously distributed in each hospital. Then, we collected the boxes 15 days after. The period of data collection lasted from October to December 2021.
Statistical analysis
We analyzed the data using the package IBM SPSS Statistics for Windows, version 21.0. Armonk, NY: IBM Corporation. Multiple responses were possible on the section of the checklist dealing with type of violence and other variables. The type of violence as dependent variable was categorized into verbal violence, physical violence (spitting, biting, kicking, scratching/pinching, slapping/hitting, punching, pushing, restraining, use of object or weapon) and Both, based on the approach of these authors [22]. Descriptive statistics were conducted to determine the characteristics of the study sample. Data were presented as frequencies and percentages. The multicomparison chi-square test was used to define significant differences among groups. Fisher’s exact test was used where the chi-square test was not appropriate. If the statistical test considering all options of responses for an item was positive (p-value <0.05), then the highest percentage value for an option was compared statistically to the sum of the percentages of all the other options, in order to point out probable triggers of WPV. Additionally, we performed a post hoc multiple chi-square test or multiple Fisher’s exact test (if the chi-square test or Fisher’s exact test were significant) to identify significantly more or less frequent categories. We applied the 2 tailed residual z test for significant variables. A value higher than +1.96 standard deviations is considered significant. The critical value is the same for each tail. All tests with p< 0.05 were considered significant.
Results
Demographic characteristics of the victims and the assaulters
We distributed the questionnaires to 391 nurses working in hospitals located in the study area. In total, 387 nurses informed the questionnaire with 98% response rate. Among the respondents, 97% of the nurses experienced at least one WPV episode during the preceding year. The demographic characteristics of the assaulted nurses and the assaulters are illustrated in Table 1.

Table 1. Demographic data of victims and WPV perpetrators in hospitals, northern region of Morocco, 2021.
Our data showed that the majority of the nurses (78%) aged less than 39 years old. The sex ratio (Male-to-Female) was 0.7. Most of the victims were females (60%), whereas most of the assaulters were male (70%). The majority of assaulters aged between 31 and 50 years old.
Violence pattern among nurses
The data on the type of violence facing nurses are presented in Table 2. The most common type of violence was verbal violence (70 %). The main forms of physical violence were Slapping/Hitting (29 %) and Kicking (26 %).

Table 2. Type of WPV facing nurses (n=379) in northern region hospitals of Morocco, 2021.
Profile of the victims and the aggressors
The data on the profile of the victims, aggressors and factors related to WPV are illustrated in Table 3.
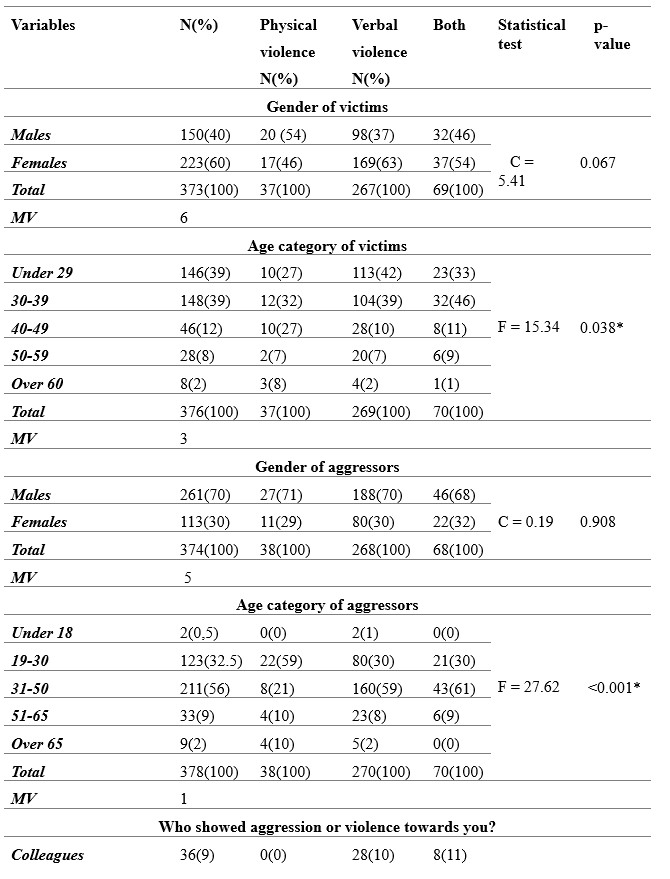

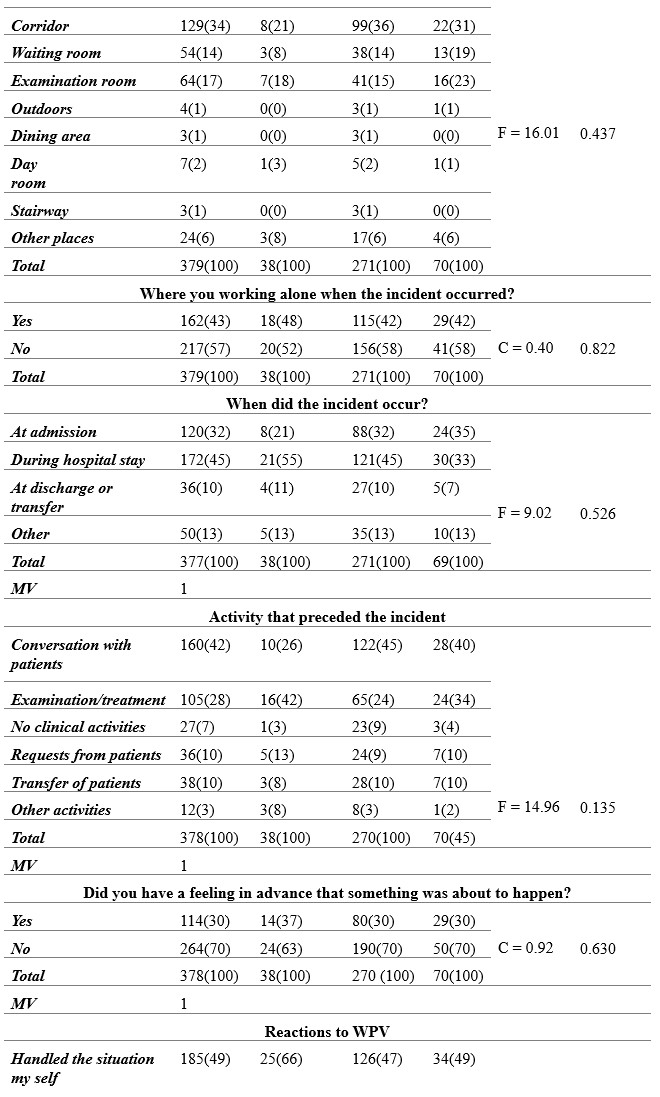
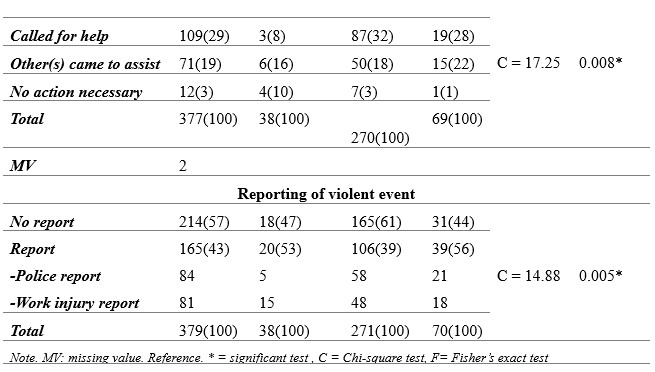
Table 3. Circumstances and factors associated with violence using VIF questionnaire among nurses, Morocco, 2021.
The data on the post hoc statistics, based on 2 tailes residual z test for significant variables previously obtained using Chi-square or Fisher tests, are reported in Table 4.
Considering the profile of the victims, our results indicated that nurses having less than 39 years old were significantly more exposed to WPV than the elders (c2 = 15.34; p = 0.038). Focusing on 40-49 and 60 or older age groups of the victims, the standardized residuals are significant for physical violence. This finding suggests a significant positive association between 40-49 (z = 2.6) and 60-older age groups (z = 2.5) and the physical violence.
Regarding the aggressors, we found that males perpetrate more violence than females. Neverthless, this result was not statistically significant. We observed that the age category of the aggressor was significantly associated with violence (c2 = 27.66; p < 0.001). The aggressors belonging to 31-50 years old age category perpetrated more WPV than other age categories. Comparing this age category to the others, we found that this interval can be considered as a trigger of WPV (p < 0.001).
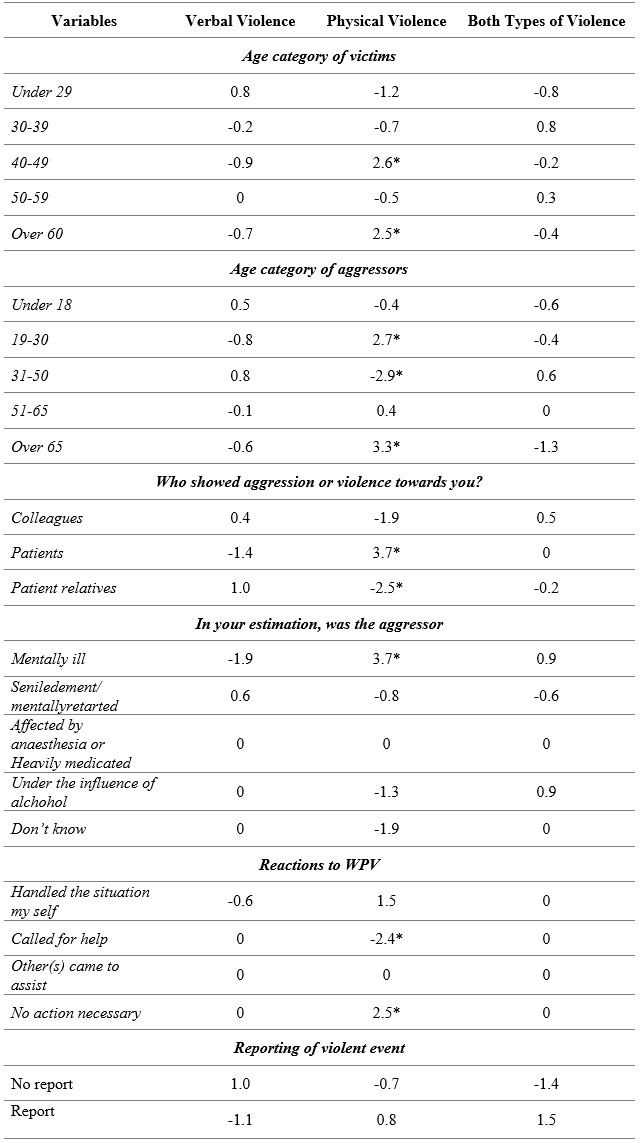
Table 4. Post hoc statistics, based on 2 tailes residual z test applied to significant risk factors of WPV experienced by nurses, Morocco 2021. Significant z values were marked with an asterisk.
Additionally, post hoc statistics based on residual standardized z test, were significant for 19-30 and over 65 age groups of the aggressors (z = 2.7 and z = 3.3 respectively) for physical violence. This result indicates a significant positive association between these age grousp and physical violence. At the opposite, we obtained a significant negative association between 31-50 age group and physical violence (z = – 2.9).
With regards to the nature of the relationship between the parties involved in the incident, the data showed that this factor was strongly and significantly associated with violence (c2 = 28.17; p < 0.001). The most frequently notified profile of the aggressor was the patient’s relatives (50%). Comparing this profile of the perpetrator to the others, we found that patient’s relatives is probably a trigger of WPV (p = 0.001). Moreover, according to post hoc statistics based on residual standardized z test, we obtained that the profile ‘Patients’ was positively associated with physical violence (z = 3.7) and ‘Patients relatives’ profile was negatively associated with physical violence (z = – 2.5).
Considering the emotional and psychological state of the aggressor, it was significantly associated with violence (c2 = 28.28; p = 0.003). Comparing the state of the aggressor ‘Mentally ill’ to the other states, we found that the mentally ill aggressor can be considered as a significant alerting factor of violence (p = 0.006). On the other hand, the standardized residual z test indicated that ‘Mentally ill’ aggressor’s state is positively associated with physical violence (z = 3.7). This finding suggest that mentally ill aggressors are more likely authors of physical violence than the aggressors with other mental and psychological disorders.
Circumstances and factors associated with WPV
Considering the circumstances of the violence, the time of violent incidents was not significantly associated with WPV. Nevertheless, we observed that aggressive episodes occurred with a high frequency throughout daily shift (68%). About the place of WPV occurrence, the corridors were the most frequently signalized place (34%) than other places. However, the result was not statistically significant. Regarding the situation if the victim was working alone or not, the frequency of violence was slightly high (57%) when the victim was not working alone.
Looking for which step during the patient journey the incidents occur mainly, we observed that most of the events occurred during the hospital stay (45%) and at admission (32 %). Nevertheless, the results were not statistically significant.
Considering the activities preceding the incident, we found that ‘Conversation with the patient’ was the most frequent (42%), followed by ‘Examination/treatment’ (28%).
Prediction, reactions and management of workplace violence
Considering the feeling in advance that something was about to happen, most of the victims (70%) responded by No. This result indicates that the great majority of the nurses were not able to identify suspicious behaviors.
Regarding the reactions to WPV, half of the victims opted for handling the situation themselves and this result was statistically significant (c2 = 17.96; p = 0.008). Comparing the option ‘Handled the situation my self’ to all the other options, we found that this option is a probable trigger of WPV (p = 0.088). Post hoc residual statistics showed a negative association of the option ‘Call for help with physical violence (z = -2.4). About the option ‘No action necessary’, residual statistics showed a positive association with physical violence. in general, the results on the reactivity of the nurses express a non-responsiveness.
Our data showed a low reporting level of the violence occurring in Moroccan hospitals. We observed that 57% of the nurses did not formally report the violence in a police report or a work injury report. This result was statistically significant (c2 = 14.9; p = 0.005). Finally, Data indicates that the most frequent negative effect of WPV on the nurses was the psychological problem (74%).
Discussion
In this study, we have explored the occurrence of workplace violence among nurses and the associated factors in northern region hospitals of Morocco. It presents the first data on occupational violence facing nurses in Morocco to our knowledge. We obtained a high exposure to WPV among nurses working in this area. This finding was similar to the data reported in these studies [6, 11, 23-28]. Moreover, comparing the WPV frequency between different studies is difficult [6, 20, 23]. This difficulty may be due to the different case definition of different categories of violence adopted by the authors, the use of different tools, and the application of different study designs. In addition, individual differences in perception of violence forms can lead to different results. Overall, verbal violence was more frequent than physical violence. In addition, Arnetz et al report that the violence pattern facing healthcare professionals is different between different health units providing different kind of healthcare [18].
Profile of the victims and the aggressors
Focusing on the age of the victims, we observed that younger nurses, i.e., under 39 years old, faced more workplace violence than elderly nurses. This finding is consistent with the literature [10, 29, 30]. We suggest the insertion of a training module on the management and prevention of WPV in the nursing academic course and the first years after employment in Moroccan health facilities.
Considering the gender of the aggressors, despite the fact that this factor was not statistically significant, but the proportion of male aggressors was very high (70%) compared to females (30%). This item was reported as a factor of violence in these studies [19, 31, 32]. Regarding the assaulter’s age, we found that it was a statistically significant factor of violence. This finding is consistent with the last cited studies.
The significantly most incriminated assaulters were the patients’ relatives. This result is supported by these studies [24, 26, 28, 32-35]. This finding may be linked to the fact that patients and their relatives have high expectations of healthcare professionals, and when they perceive that their needs are not satisfied, they may adopt aggressive attitudes [3, 36]. According to post hoc residual z test, significant statistics showed that nurses aged between 40 and 49 and over 60 y.o were more exposed to physical violence than other age categories, while the aggressors aged between (19-30 y.o.) and over 60. In addition, significant less frequent were cases of aggressors aged between 31 and 50 y.o.
These victims and aggressors age categories must be considered by the healthcare professionals in the management and the control of WPV.
Circumstances and factors associated with WPV
Despite the fact that our findings were not statistically significant, most of the incidents occurred during daily shifts. This finding is in accordance with these studies [37, 38]. Other authors obtained contradictory data [28, 32].
About WPV place, the most frequently signalized place was the corridors (35%). These data are consistent with these studies [29, 10]. The fact that the results on the circumstances were not statistically significant may be linked to the great number of the response options, the reduced number of the participants in each response option, and the limited sample size.
Prediction, reactions and management of workplace violence
Considering the feeling in advance that an incident will occur, the majority of the incidents were not expected by the nurses. This result is in accordance with the data found in the literature on the predictive factors of WPV [39]. This finding expresses a need to sensitize and inform the nurses about workplace violence. Regarding the consequences of WPV, the most negative effect was psychological problems. This result is in line with the findings of the previously cited study.
Beside this result, we obtained a low reporting of the violent incidents. This finding is in accordance with the results obtained by these authors [40, 41]. It is probably due to the lack of a notification system of WPV, the lack of information on how to report the incident, the ignorance of labor laws and rights, and the victims may believe that the reporting is useless or the act of violence is not considered a crime.
Conclusions
A high exposure of nurses to WPV in northern Moroccan hospitals is noted. Verbal violence is more predominant than physical violence. Considering the profile of the assaulters, the majority are male and the most incriminated are the patients’ families. Significant risk factors such as age of the victims and the assaulters were obtained. The mental condition of the assaulter is significantly associated to violence perpetrated against nurses. These results should alert policymakers about the violent workplace incidents committed in Moroccan hospitals. We recommend the conduction of large-scale studies to inform policymakers about the exact magnitude and factors of WPV in other hospitals and non-hospital settings in all regions of the kingdom. Then the implementation of a program on the prevention and management of WPV for nurses and other categories of healthcare professionals. Another preventive aspect is the setting of a WPV notification system in hospitals to help operative managers on time to address the factors that lead to workplace violence.
Limitations
Despite the fact that most of our findings are supported by the data published on workplace violence, our study has some limitations. The main limitation is that VIF asks about violence experienced the past year only. Another limitation about the severity of the violence is related to the fact that the VIF reports if the participant experienced a violent event or not, but the participant is not asked about how often he faced incidents during the year. Finally, since our study was conducted in the northern area only, our findings are not generalized to the whole population of nurses working in Moroccan hospitals or other healthcare facilities. In order to have representative results on the violence through all the country, further studies must be extended to a larger period of time and cover all the regions of Morocco.
Funding: This research received no external funding.
Institutional Review Board Statement: The study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Review Board (or Ethics Committee) of “Comithé d’Ethique pour la Recherche Biomédicale CERBO (protocol code 28/2021 and date of 11/10/2021).
Informed Consent Statement: Informed consent was obtained from all subjects involved in the study. Written informed consent has been obtained from the patient(s) to publish this paper.
Data Availability Statement: Data is unavailable due to privacy and national restrictions.
Conflicts of Interest: The authors declare no conflict of interest.
Author Contributions: Conceptualization, S.O (Safae Ouma); N.B (Nabil Benomar) and N.R (Nabila Rouahi); Methods, S.O; N.B and N.R; Software, S.O and N.R; Validation, S.O; N.B; M.L.LL (Maria LeyreLavilla Lerma) and N.R; Formal analysis: MLLL; Investigation, S.O; Resources, S.O; N.B and N.R; Data curation, S.O; N.R and N.R; Writing—Original draft preparation, S.O and N.R; Writing—review and editing, S.O; N.B; MLLL and N.R; Visualization, S.O; N.B; MLLL and N.R; Supervision, N.B and N.R; Project administration, N.B and N.R; Funding acquisition, None. All authors have read and agreed to the published version of the manuscript.
Acknowledgments: We would like to thank the nurses who participated in this research and staff of the hospitals who facilitated the fluent conduction of the study for their efforts in the data collection.
References
- Krug, E. G., Dahlberg, L. L., Mercy, J. A., Zwi, A. B., Lozano, R. (2002). World report on violence and health. World Health organization. https://apps.who.int/iris/handle/10665/42495.
- National Institute for Occupational Safety and Health. (2002). Violence : Occupational hazards in hospitals. http://doi.org/10.26616/NIOSHPUB2002101.
- Phillips, J. P. (2016). Workplace Violence against Health Care Workers in the United States. New England Journal of Medicine, 374(17), 1661‑1669. https://doi.org/10.1056/NEJMra1501998.
- Wassell, J. T. (2009). Workplace violence intervention effectiveness : A systematic literature review. Safety Science, 47(8), 1049‑1055. https://doi.org/10.1016/j.ssci.2008.12.001.
- Tuncel, E. K., Dundar, C., Sunter, A. T., Canbaz, S., &Peksen, Y. (2009). Violence towards primary healthcare workers in Samsun, Turkey. 18.Conference: 12th World Congress on Public Health World Health Organization
- Park, M., Cho, S.-H., & Hong, H.-J. (2015). Prevalence and Perpetrators of Workplace Violence by Nursing Unit and the Relationship Between Violence and the Perceived Work Environment : Workplace violence against nurses. Journal of Nursing Scholarship, 47(1), 87‑95. https://doi.org/10.1111/jnu.12112.
- Khalil, M., &Alameddine, M. (2020). Recruitment and retention strategies, policies, and their barriers : A narrative review in the Eastern Mediterranean Region. Health Science Reports, 3(4). https://doi.org/10.1002/hsr2.192.
- Pich, J., & Roche, M. (2020). Violence on the Job: The Experiences of Nurses and Midwives with Violence from Patients and Their Friends and Relatives. Healthcare, 8(4). 522. http://doi.org/10.3390/healthcare8040522.
- Cebrino, J., &Portero de la Cruz, S. (2020). A worldwide bibliometric analysis of published literature on workplace violence in healthcare personnel. PLOS ONE, 15(11), e0242781. https://doi.org/10.1371/journal.pone.0242781.
- Kamchuchat, C., Chongsuvivatwong, V., Oncheunjit, S., Yip, T. W., &Sangthong, R. (2008). Workplace Violence Directed at Nursing Staff at a General Hospital in Southern Thailand. Journal of Occupational Health, 50(2), 201‑207. https://doi.org/10.1539/joh.O7001.
- Chapman R, Perry L, Styles I, Combs S. Predicting patient aggression against nurses in all hospital areas. British Journal o Nursing. 2009. 18(8) : 476 – 483.
- Partridge, B.; Affleck, J. Verbal abuse and physical assault in the emergency department: Rates of violence, perceptions of safety, and attitudes towards security. Australas. Emerg. Nurs. J. 2017, 20, 139–145. [CrossRef]
- Kvas, A., & Seljak, J. (2014). Unreported workplace violence in nursing : Unreported workplace violence in nursing. International NursingReview, 61(3), 344‑351. https://doi.org/10.1111/inr.12106.
- Human Resources report of the Ministry of Health, 2016.
- Belayachi, J., Berrechid, K., Amlaiky, F., Zekraoui, A., &Abouqal, R. (2010). Violence toward physicians in emergency departments of Morocco : Prevalence, predictive factors, and psychological impact. Journal of Occupational Medicine and Toxicology, 5(1), 27. https://doi.org/10.1186/1745-6673-5-27.
- Giurgiu DL., Jeoffrion C., Roland-Lévy C, Grasset B., Brigitte Dessomme BK., Moret L., Roquelaure Y., Caubet A., Verger C., El Houssine Laraqui C., Lombrai Pl., Geraut C, and Tripodi D. 2016. Wellbeing and occupational risk perception among health care workers: a multicenter study in Morocco and France. J.Occup Med Toxicol. 2016; 11: 20. http://doi.org/10.1186/s12995-016-0110-0.
- Semlali H. (2010). The Morocco Country Case Study: Positive Practice Environments. Morocco Case Study: Health Care Environments in Morocco. Global Health Workforce Alliance, WHO, Geneva. http://www.who.int/workforcealliance/knowlege/resources/ppemorocco/en/index.html
- Arnetz JE, Arnetz BB, Söderman E. Violence toward health care workers. Prevalence and incidence at a large, regional hospital in Sweden. AAOHN J. 1998 Mar;46(3):107-14. PMID: 9582726.
- Ferri, P., Silvestri, M., Artoni, C., & Di Lorenzo, R. (2016). Workplace violence in different settings and among various health professionals in an Italian general hospital : A cross-sectional study. Psychology Research and Behavior Management, 9, 263‑275. https://doi.org/10.2147/PRBM.S114870.
- Magnavita, N., &Heponiemi, T. (2012). Violence towards health care workers in a Public Health Care Facility in Italy: A repeated cross-sectional study. BMC Health Services Research, 12(1), 108. https://doi.org/10.1186/1472-6963-12-108.
- Strand, M. M., Estimation of a population total under a “Bernoulli sampling” procedure. The American Statistician, 1979. 33(2), 81-84.
- Khalid GM, Idris UI, Jatau AI, Wada YH, Adamu Y, Ungogo MA. Assessment of occupational violence towards pharmacists at practice settings in Nigeria. Pharmacy Practice. 2020 Oct-Dec;18(4):2080. https://doi.org/10.18549/PharmPract.2020.4.20.
- Ayranci, U., Yenilmez, C., Balci, Y., &Kaptanoglu, C. (2006). Identification of Violence in Turkish Health Care Settings. Journal of Interpersonal Violence, 21(2), 276‑296. https://doi.org/10.1177/0886260505282565.
- Kitaneh, M., &Hamdan, M. (2012). Workplace violence against physicians and nurses in Palestinian public hospitals : A cross-sectional study. BMC Health Services Research, 12(1), 469. https://doi.org/10.1186/1472-6963-12-469.
- Alsaleem, S., Alsabaani, A., Alamri, R., Hadi, R., Alkhayri, M., Badawi, K., Badawi, A., Alshehri, A., & Al-Bishi, A. (2018). Violence towards healthcare workers : A study conducted in Abha City, Saudi Arabia. Journal of Family & Community Medicine, 25, 188‑193. https://doi.org/10.4103/jfcm.JFCM_170_17.
- Hamdan, M., & Abu Hamra, A. (2015). Workplace violence towards workers in the emergency departments of Palestinian hospitals : A cross-sectional study. Human Resources for Health, 13(1), 28. https://doi.org/10.1186/s12960-015-0018-2.
- Rafeea, F., AlAnsari, A., Musbah Abbas, E., Elmusharaf, K & Abu Zeid, M. (2017). Violence toward health workers in Bahrain Defense Force Royal Medical Services´ emergency department. Open Access Emergency Medicine, 9, 113‑121. https://doi.org/10.2147/OAEM.S147982.
- Zafar, W., Siddiqui, E., Ejaz, K., Shehzad, M. U., Khan, U. R., Jamali, S., &Razzak, J. A. (2013). Health Care Personnel and Workplace Violence in the Emergency Departments of a Volatile Metropolis : Results from Karachi, Pakistan. The Journal of Emergency Medicine, 45(5), 761‑772. https://doi.org/10.1016/j.jemermed.2013.04.049.
- Adib, S. M., Al-Shatti, A. K., Kamal, S., El-Gerges, N., & Al-Raqem, M. (2002). Violence against nurses in healthcare facilities in Kuwait. International Journal of Nursing Studies, 39(4), 469‑478. https://doi.org/10.1016/S0020-7489(01)00050-5.
- Alameddine, M., Mourad, Y., &Dimassi, H. (2015). A National Study on Nurses’ Exposure to Occupational Violence in Lebanon : Prevalence, Consequences and Associated Factors. PLOS ONE, 10(9), e0137105. https://doi.org/10.1371/journal.pone.0137105.
- Gerberich, S. G. (2004). An epidemiological study of the magnitude and consequences of work related violence : The Minnesota Nurses’ Study. Occupational and Environmental Medicine, 61(6), 495‑503. https://doi.org/10.1136/oem.2003.007294.
- Lei, Z., Yan, S., Jiang, H., Feng, J., Han, S., Herath, C., Shen, X., Min, R., Lv, C., & Gan, Y. (2022). Prevalence and Risk Factors of Workplace Violence Against Emergency Department Nurses in China. International Journal of Public Health, 67, 1604912. https://doi.org/10.3389/ijph.2022.1604912.
- Algwaiz, W. M. (2012). Violence exposure among health care professionals in Saudi public hospitals. Saudi Med J. 2012. 7.
- Muñoz del Carpio-Toia, A., Begazo Muñoz del Carpio, L., Mayta-Tristan, P., Alarcón-Yaquetto, D. E., & Málaga, G. (2021). Workplace Violence Against Physicians Treating COVID-19 Patients in Peru : A Cross-Sectional Study. The Joint Commission Journal on Quality and Patient Safety, 47(10), 637‑645. https://doi.org/10.1016/j.jcjq.2021.06.002.
- Sachdeva, S., Jamshed, N., Aggarwal, P., & Kashyap, S. (2019). Perception of workplace violence in the emergency department. Journal of Emergencies, Trauma, and Shock, 12(3), 179. https://doi.org/10.4103/JETS.JETS_81_18.
- Usman, N., Dominic, B., Nwankwo, B., Nmadu, A., Omole, N., & Usman, O. (2022). Violence towards health workers in the workplace : Exploratory findings in secondary healthcare facilities in Kaduna metropolis, Northern Nigeria. Babcock University Medical Journal, 5(1). https://doi.org/10.38029/babcockunivmedj.v5i1.118.
- Albashtawy, M., Al-Azzam, M., Rawashda, A., Batiha, A.-M., Bashaireh, I., &Sulaiman, M. (2015). Workplace Violence Toward Emergency Department Staff in Jordanian Hospitals : A Cross-Sectional Study. Journal of Nursing Research, 23(1), 75‑81. https://doi.org/10.1097/jnr.0000000000000075.
- Fernandes, C. M. B., Raboud, J. M., Christenson, J. M., Bouthillette, F., Bullock, L., Ouellet, L., & Moore, C. F. (2002). The effect of an education program on violence in the emergency department. Annals of Emergency Medicine, 39(1), 47‑55. https://doi.org/10.1067/mem.2002.121202.
- Alshahrani, M., Alfaisal, R., Alshahrani, K., Alotaibi, L., Alghoraibi, H., Alghamdi, E., Almusallam, L., Saffarini, Z., Alessa, S., Alwayel, F., Saffarini, L., Alrawdhan, A., Mapusao, C., Asonto, L. P., Alsulaibikh, A., &Aljumaan, M. (2021). Incidence and prevalence of violence toward health care workers in emergency departments : A multicenter cross-sectional survey. International Journal of Emergency Medicine, 14(1), 71. https://doi.org/10.1186/s12245-021-00394-1.
- Garg, R., Garg, N., Sharma, D.K., Gupta, S. (2019). Low reporting of violence against health-care workers in India in spite of high prevalence. Medical Journal Armed Forces India. 75. 211-215. doi: 10.1016/j.mjafi.2018.11.011.
- Alfuqaha O., Albawati N., Alhiary S., Alhalaiqa F., Haha M., Musa S., Shunnar O and AL Thaher Y 5. (2022). Workplace Violence among Healthcare Providers during the COVID-19 Health Emergency: A Cross-Sectional Study. Behav. Sci. 2022, 12, 106. https://doi.org/10.3390/bs12040106.
![]() This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Systems compared: Capillary glucose self-monitoring and Flash glucose monitoring system. Cross-sectional study
Francesco Saverio Auricchio¹*, Maria Russo²,
Maddalena Lettieri¹, Nicolas Craparotta¹
¹Department of Translation Medical Sciences, University Federico II, Naples.
²San Giovanni di Dio Civil Hospital of Frattamaggiore, Asl Naples 2 North, Naples.
*Corresponding author: Francesco Saverio Auricchio, Department of Translation Medical Sciences, University Federico II, Naples.
Email: francescosaverio.auricchio@unina.it

Cite this article
ABSTRACT
Introduction: In recent years, with the rapid advancement of technology, tools capable of minimising discomfort for the diabetic patient are becoming increasingly popular, thereby increasing adherence to treatment. The use of technology improves glycometabolic compensation and quality of life.
Objective: The aim of the present study is to verify, in the group using the Flash Glucose Monitoring system, improved diabetes management and satisfaction in insulin-treated patients.
Materials and Methods: A retrospective cross-sectional study was performed through the administration of the “Diabetes Treatment Satisfaction Questionnaire”. The study was performed from January to July 2019. 82 validated questionnaires were administered in the Italian version. Participants were 47 women (39 Type 1 Diabetes Mellitus and 8 Type 2 Diabetes Mellitus) and 35 men (19 Type 1 Diabetes Mellitus and 16 Type 2 Diabetes Mellitus).
Results: Results show that subjects with the Flash Glucose Monitoring system have greater satisfaction than those using the Self-Monitoring of Blood Glucose system. Patients using Flash Glucose Monitoring showed 83.9% satisfaction, while patients using Self-Monitoring of Blood Glucose showed 33.3% complete satisfaction. The average glycosylated haemoglobin of the group of subjects using Flash Glucose Monitoring was 53.2 mmol/mol, while that of subjects with self-monitoring of capillary blood glucose was 60.3 mmol/mol.
Conclusions: The adoption of new technologies has benefits for the patient that positively affect quality of life. The study showed better glycometabolic compensation in the group of patients using Flash Glucose Monitoring. Diabetes carries significant costs to public health, and prevention and improvement of care could be a primary goal for the community and health systems.
Keywords: Diabetes mellitus; Telemedicine; Technology; Flash glucose monitoring; Self-monitoring of blood glucose
INTRODUCTION
Diabetes mellitus is a chronic disease characterised by increased concentration of glucose in the blood. The vast majority of diabetes cases fall into two broad aetiopathogenic categories. In one category, Type 1 Diabetes Mellitus (DMT1), the cause is an absolute lack of insulin secretion due to an autoimmune pathological process that occurs in the pancreatic islets and/or genetic alterations. In the other category, Type 2 Diabetes Mellitus (DMT2), the cause is a combination of resistance to insulin activity and an inadequate compensatory insulin secretory response. In the latter category, a degree of hyperglycemia sufficient to cause pathological and functional alterations in various target tissues, but without clinical symptoms, may be present for a long time before diabetes is detected [1].
DMT2 is considerably the most frequent form of diabetes (it affects 90% of cases) and is typical of middle age. It emerges as a multifactorial disease that involves both genetic predisposition and multiple environmental factors [2]. In 2021, the International Diabetes Federation (IDF) estimated that 537 million were diagnosed with diabetes mellitus and predicted that this figure will reach 643 million by 2030 and 783 million by 2045. In addition, the IDF estimated that, in 2021, 541 million people had reduced glucose tolerance. The number of children and adolescents living with diabetes is constantly increasing. In 2021, more than 1.2 million children and adolescents were diagnosed with Type 1 Diabetes Mellitus.
Direct health expenditures due to diabetes are already close to $1 trillion and will exceed this figure by 2030. The 10th edition of the IDF Diabetes Atlas also shows that hyperglycaemia in pregnancy affects about one in six pregnancies. Another cause for alarm is the consistently high percentage (45%) of people with undiagnosed diabetes, which is predominantly type 2. This highlights the urgent need to improve the ability to diagnose people with diabetes, many of whom do not know they have the condition, and to provide appropriate and timely care to all people with diabetes as soon as possible [3]. One-fifth of people with type 1 diabetes are in low- and lower-middle-income countries. The residual life expectancy of a 10-year-old child diagnosed with Type 1 Diabetes Mellitus in 2021 ranged from an average of 13 years in low-income countries, to 65 years in high-income countries [4].
Diabetes therapy is often substitutive and is based on partly frequent or continuous insulin administrations. The objective of replacement therapy is to maintain blood glucose concentrations in a physiological range, trying to avoid or in any case limit both episodes of hypoglycaemia and hyperglycaemia. It is therefore necessary to continuously harmonise insulin therapy, nutrition and exercise, also taking into account the hyperglycaemic effect of stress, intercurrent diseases and, in the case of the child, even in changes in a growing body [5]. To be able to live with your diabetes, without being overwhelmed by it, you need good blood sugar control. To judge the effectiveness of the control, it is necessary to measure the reactions of the body to the treatment, even if you are not on drug therapy, but proper care is based on lifestyle changes and physical activity [6]. Through monitoring, it is possible to intervene in the most appropriate way, bringing or maintaining blood glucose levels as close as possible to the reference values [7]. The American Diabetes Association (ADA) recommends that all diabetics try by any and all means to maintain blood sugar control so as to reduce the risk of complications [8].
Diabetes, a systemic disease not to be overlooked, has chronic complications that can also be disabling and fatal. Diabetes presents macrovascular complications, including coronary heart disease, stroke, and peripheral vascular disease, and microvascular complications, such as end-stage renal disease, retinopathy, and neuropathy, along with lower limb amputations. Complications are responsible for much of the health spending associated with diabetes. There is also a growing recognition of a diverse set of causal conditions, including cancers, ageing-related outcomes (e.g. dementia), infections, and liver disease [9]. Daily monitoring of diabetes, due to frequent capillary sampling obtained by finger prick, is painful and this can make it difficult to adhere to a diabetes management plan. In recent years, thanks to the increasing number of technologies available for glycaemic monitoring and insulin administration, there has been a real revolution in the care of people with diabetes mellitus [10].
The Flash Glucose Monitoring (FGM) system avoids inconvenience to patients due to repeated capillary punctures, providing continuous measurement of blood glucose [11] through a system consisting of a small circular sensor applied to the back of the arm that, at intervals of one minute, measures glucose in the interstitial fluid, by means of a small filament inserted under the skin and held in place by a small adhesive pad. Using this circuit, the patient is able to detect blood glucose in real time, and wirelessly transmit all the information necessary to evaluate the glycaemic trend.
The purpose of this study is to look at the impact of the FGM system on glycaemic control in insulin-treated diabetic patients, verifying whether those who use the FGM system have better diabetes management, as well as a better degree of satisfaction than those who use Self-monitoring of Blood Glucose (SMBG).
MATERIALS AND METHODS
The following cross-sectional study was carried out by administering a questionnaire validated in its Italian version, found in the international literature. The Italian adaptation of the “Diabetes Treatment Satisfaction Questionnaire” (DTSQ) was used [12]. This questionnaire has been specifically designed to measure satisfaction with diabetes treatments and can be used in both patients with type 1 diabetes and those with type 2 diabetes. The level of treatment satisfaction in the two patient groups (FGM and SMBG) and the frequency of perception of episodes of hypoglycaemia and hyperglycaemia were analysed and compared. The study began in January 2019 and was completed in July of the same year. 82 questionnaires of the validated Italian version of the DTSQ were administered. The questionnaire includes 8 questions, 6 of which are added together in a single score that varies between 8 (very unsatisfied) and 36 (very satisfied). The remaining two questions, used individually, explore the perceived frequency of episodes of hypo- and hyperglycaemia [13], through an incremental score of 1 (never) to 6 (very often). We also investigated the personal characteristics of the sample (gender and age), the type of diabetes (DMT1 and DMT2), the methods of glycaemic control (SMBG and FGM) and the value of glycosylated haemoglobin (HbA1c).
The questionnaires were administered online, on Facebook™ social media and through the Google Forms™ platform, within special groups dedicated to the diabetic patient, namely Diabetica: il gruppo sul diabete tipo 1, Diabete.com, Diabetici Insieme. The survey was conducted through the use of convenience sampling. Adherence to the questionnaire was voluntary and the questionnaire was made anonymous at source. The consent to the participation and use of the data was considered acquired at the time of sending the questionnaire. The data were analysed in aggregate form. Approval by the Local Ethics Committee was not required for this type of study.
The following inclusion criteria were defined: subjects of both sexes, patients with DMT1, patients with DMT2, patients on pharmacological treatment, patients aged > 6 years. The following exclusion criteria were defined: patients aged < 6 years, patients not pharmacologically treated or patients who follow only a diet and/or physical activity.
Statistical analyses
The data collected were processed through the use of the “LibreOffice6.2™” package for descriptive statistical analysis. The same data were analysed with the statistical software “RStudio™” for the analysis of the variables under analysis. Data are presented as number and percentage for categorical variables and continuous data are expressed as mean ± standard deviation (SD), median and interquartile range (IQR). The confidence interval (CI) was calculated for mean age and HbA1c. The different variables were analysed and correlated to assess whether there were differences in diabetes management and satisfaction in the two patient groups (SMBG and FGM). The chi-squared test was performed for the two levels of satisfaction obtained in relation to the two types of treatment. The Shapiro-Wilk test was used to determine whether the variables were distributed normally and, subsequently, the non-parametric Wilcoxon-Mann-Whitney test was carried out for unpaired data, since the variables were not distributed normally. All tests with a p-value <0.05 were considered significant.
RESULTS
The sample consisted of 82 diabetic subjects, of whom 58 (70.7%) had a diagnosis of DMT1, while 24 (29.3%) had a diagnosis of DMT2.
The subjects included in the study had a variable age. The mean age was 37.5 years (95% CI: 34.1-40.9; SD=15.4). The study included the distribution of patients according to sex.
The analysis of the data showed greater participation in the completion of the questionnaire by females (47 subjects, equal to 57.3% of the sample) compared to males (35 subjects, equal to 42.7% of the sample). For the purposes of the study, patients were divided according to the type of glycaemic monitoring: SMBG and FGM. On analysing the data, it was observed, as is known, that the glycemic self-monitoring system using capillary puncture is the most widespread system.
Of the 82 subjects who participated in the study, 51 subjects used the SMBG system (62.2%) and 31 subjects (37.8%) used the FGM system. The different levels of satisfaction for the related types of monitoring were also analysed.
For the evaluation of the different levels of satisfaction, of a maximum score of 36 (sum of the maximum scores of each score), a score < 12 was considered as totally unsatisfactory, a score between 12 and 24 as partially satisfactory and finally a score between 24 and 36 as satisfactory. The scores obtained were categorised and analysed.
The results, extrapolated from the questions investigating objective data, were stratified according to gender and are reported in Table 1.

Table 1. Characteristics of 82 diabetic patients stratified by gender.
The effectiveness of diabetes treatment should not be assessed solely on the basis of HbA1c levels as it should also focus on patient-reported outcomes such as patient satisfaction, well-being and quality of life. The DTSQ was developed to assess patient satisfaction in the treatment of diabetes.
Table 2 shows the results obtained from the questionnaire.

Table 2. Summary of the percentages of responses obtained from the DTSQ questionnaire administered to 82 diabetic patients (the score for each field ranges from 1 to 6, where 1 means “very dissatisfied” and 6 means “very satisfied”).
Table 3 shows the results obtained from the DTSQ, stratified into three categories: “Satisfaction yes”, “Partial satisfaction”, “Satisfaction no”,
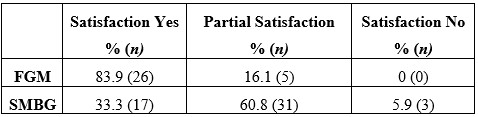
Table 3. Results obtained according to the evaluation criteria of the scale used (score < 12 = totally unsatisfactory, score between 12 and 24 = partially satisfactory, score between 24 and 36 = satisfactory).
Subjects with the FGM system show greater satisfaction than those using the SMBG system. Patients using Flash Glucose Monitoring showed 83.9% satisfaction, 16.1% partial satisfaction and 0% total dissatisfaction. Patients using capillary glucose self-monitoring, on the other hand, showed complete satisfaction for 33.3% of the sample (1 out of 3), partial satisfaction for the treatment equal to 60.8% and total dissatisfaction equal to 5.9% (Table 3).
The results obtained show that the FGM group had a dissatisfaction (satisfaction no) value of 0. The purpose of the study was to demonstrate a significant difference in satisfaction in the two different monitoring groups. The results obtained by the partially satisfied (partial satisfaction), considered as negative and not sufficient, were merged with those of the not satisfied (satisfaction no). Table 4 shows the new classification.

Table 4. Comparison between the results obtained for “satisfaction yes” and the combined results of “satisfaction no” and “partial satisfaction”
In Table 4 the results obtained for “partial satisfaction” were considered as negative values and therefore added to the values obtained for “satisfaction no”.
Table 4 shows a significant relationship between the groups and the satisfaction variable. In particular, the chi-squared test showed a significantly higher presence of satisfaction in the FGM group compared to the SMBG group (19.74, 83.9% vs 33.3%, chi-squared=19.74, p<0.0001). In other words, there is significantly greater treatment satisfaction in diabetic patients using the FGM monitoring system compared to the traditional method (SMBG). Differences in glycosylated haemoglobin were also analysed in the two patient groups. The mean glycosylated haemoglobin of the FGM group was 53.2 mmol/mol (95% CI: 49.0-57.4), while that of subjects with self-monitoring of capillary blood glucose was 60.3 mmol/mol (95% CI: 55.9-64.6).
For inferential analysis, the Wilcoxon-Mann-Whitney nonparametric test was used for two independent samples, as the data distributions were not normal. The different variables covered by the research were compared in relation to the monitoring system used by the patient (Table 5). Statistical analysis of both samples (SMBG and FGM) was performed. The samples were first analysed independently and then compared.

Table 5. Comparison between SMBG and FGM samples, regarding the different variables considered in our study, such as Satisfaction yes, HbA1c, Hyperglycaemia, Hypoglycaemia, tot DTSQ Satisfaction.
In the study sample, as seen in the descriptive statistical analysis, there was some difference between the glycosylated haemoglobins of the two groups. This comparison parameter was analysed using the Wilcoxon-Mann-Whitney test. The test showed that the difference is statistically significant, p-value= 0.029.
Another variable under study was the analysis of the frequency of perception of episodes of both
hypoglycaemia and hyperglycaemia. The frequencies of these perceptions were compared for the two classes of patients by performing an inferential analysis. With regard to the comparison of the perception of hypoglycaemic episodes, the test did not show a statistically significant difference, p-value = 0.22. The test also showed no statistically significant significance when comparing the perception of hyperglycaemic episodes, p-value = 0.30.
Finally, the degree of patient satisfaction in relation to the type of monitoring was investigated.
As seen above during the descriptive statistical analysis, there was a significant difference in satisfaction in the two groups. Statistical inference was performed to test whether the relationship between monitoring systems and satisfaction was statistically significant. The non-parametric Wilcoxon-Mann-Whitney test was chosen for two independent samples (p-value Shapiro-Wilk test = 0.024, so the distribution is not normal).
The test showed a statistically significant difference between the two groups (p-value < 0.0001).
DISCUSSION
Based on the material found in the international scientific literature, the results obtained from the study show a good match in measuring the satisfaction of diabetic patients with blood glucose monitoring. Flash glucose monitoring allows frequent glucose checks with increased time in range and reduced time in hyper- and hypoglycaemia [14]. The use of innovative tools, capable of providing greater patient comfort, is helpful in achieving better outcomes and better management of a chronic condition such as diabetes. The Impact study showed that FGM was able, in comparison to conventional systems, to increase the frequency of monitoring (up to 15 scans per day), reduce the time spent in hypoglycaemia and result in no increase in glycosylated haemoglobin at six months. FGM decreases hypoglycaemia in patients with DMT1 by an average of 74 minutes per day, with a 38% reduction compared to the control group in the 6 a.m. to 11 p.m. time slot and a 40% reduction in the time spent in hypoglycaemia in the 11 p.m. to 6 a.m. period [15].
A retrospective study, conducted in the US, and a meta-analysis, conducted in the US and Canada, showed that, with the use of the FGM system, glycosylated haemoglobin was significantly reduced in DMT2 [16].
The FGM system tends to improve treatment satisfaction, can lead to improved glycaemic control in patients with DMT2 undergoing multi-injection therapy, without increasing the frequency of hypoglycaemia [17], improving daily glycaemic control and self-care behaviour [18].
The research included the administration of the DTSQ in order to be able to analyse possible differences between the two monitoring groups and confirmed what has been stated by the various studies in the literature. The analysed sample is not representative of the entire population of diabetics as it comes from the online patient groups only, however, the patients belong to different settings as well as to different regions. In agreement with the findings in the literature, this research has shown that the use of the FGM system improves the quality of life and satisfaction of patients and promotes their well-being. The FGM system not only benefits the patient, who has greater awareness of glucose trends throughout the day, but also benefits the physician himself, who can better monitor diabetes compensation, hypoglycaemic and hyperglycaemic load in order to make the necessary changes to drug treatment [19]. Research has shown the benefits of using innovative monitoring systems.
This system is easy to wear and, with a painless scan, allows the measurement of glucose levels in the interstitial fluids of people with diabetes mellitus, even through clothing. Each scan shows both the current glucose value and the glucose data for the last 8 hours. A trend arrow helps the patient to assess the trend of blood sugar: whether it is increasing or decreasing and at what rate. These graphs allow adult patients and parents of children with diabetes to take all the necessary steps to avoid serious glycaemic imbalances. Indeed, the FGM system avoids repetitive fingertip pricks for blood glucose measurement, which cause pain, embarrassment and discomfort to the patient, and consequently allows more frequent glucose monitoring. This allows optimal management of the disease and its complications, helping to prevent, and thus reduce, episodes of hypoglycaemia and hyperglycaemia. In this regard, an additional variable was considered in the study, which involved analysing the frequency of perception of episodes of both hypoglycaemia and hyperglycaemia for the two classes of patients by performing an inferential analysis. However, the difference was not statistically significant. In addition to the limited sample size, this is due to the problems of perception of the problem and the type of data collected (self-reported).
The burden of caring for people with diabetes is considerable and the cost grows exponentially as co-morbidities increase, with hospitalisation being the main cost factor. The FGM system promotes the self-care of patients with diabetes mellitus and can help prevent acute disease-related events such as ketoacidosis and severe hypoglycaemia, thus reducing hospitalisations. Investing resources in new technologies, and thus in treatments and devices that reduce diabetes-related events, is a cost-effective strategy and thus amounts to reducing costs for the SSN (National Health Service).
The FGM system also fits well with the recent development of new digital technologies. Thanks to these advances, while on the one hand we have witnessed the increasing development of telecommunication, enabling the user to take advantage of health services through remote communication [20], on the other hand there have been significant advances in medical and technological studies, from the combination of which Telemedicine was born. It guarantees greater continuity of care, better quality of life and savings in terms of health expenditure. This enables simple and immediate doctor-patient communication, reducing outpatient visits as well as offering personalised and effective care management. Women treated with telemedicine feel better cared for through the continuous exchange of information between doctor and patient [21]. With the use of these new tools and technologies, the aim is to achieve a more sustainable management of diabetes and a more rational and modern approach to remotely managed care. Moreover, it should not be overlooked that the use of such systems allows the concept of patient empowerment to take hold, which is fundamental in the management of chronic diseases, as it enables the patient’s active participation in the treatment decision-making process.
CONCLUSIONS
The adoption of new technologies to detect blood glucose has benefits for the patient that positively influence quality of life. The improved control of the disease, linked to increased frequency of glucose monitoring, allows the reduction of glycosylated haemoglobin levels, thus achieving improved glycometabolic control. The study showed that there was a statistically significant difference in glycosylated haemoglobins between the two groups (FGM and SMGB). Glycosylated haemoglobin provides a good indication of the amount of glucose present in the blood over the past few months and is therefore a valid test for diagnosing and monitoring diabetes and, above all, diabetes management. The use of the FGM system, as confirmed by the study, allows the improvement of the quality of life of people with diabetes mellitus as well as better management of the disease. Reducing morbidity and mortality and improving the quality of life of people with diabetes mellitus is one of the current challenges for healthcare professionals.
LIMITATIONS OF THE STUDY
Although the study conducted confirmed what is already widely found in the literature, it is not without its limitations. The limitations of the study are related to the way the questionnaire was administered and the choice of sampling, which was carried out according to a non-probabilistic method that does not give all units of the population the same probability of being part of the sample. Indeed, convenience sampling was chosen for data collection. With convenience sampling, patients are not recruited randomly, so the resulting sample is subject to bias. Further limitations are represented by the sample size, which is especially useful to allow generalisation of the results, and the administration of the questionnaire to paediatric patients and young adults up to 18 years of age. For this class of patients, 8 were aged < 18 years (9.8 % of the sample), 3 were aged < 10 years (3.7 % of the sample). It is likely that the answer to the questionnaire was provided by the parent, who therefore has a system of perception of the problem that is not the patient’s own. A further study with a larger sample size would be needed to demonstrate the statistically significant reduction between perceptions of hypoglycaemic and hyperglycaemic episodes in subjects using the FGM system compared to those using the SMGB.
FUNDING
The authors did not receive any external funding to support this research.
AUTHORS’ CONTRIBUTION
All the authors contributed to the same extent to the realisation of the research.
CONFLICT OF INTEREST
The authors declare that they have no conflicts of interest.
LEGEND ACRONYMS AND ABBREVIATIONS
ADA = American Diabetes Association; DMT1 = Type 1 Diabetes Mellitus; DMT2 = Type 2 Diabetes Mellitus; DTSQ = Diabetes Treatment Satisfaction Questionnaire; FGM = Flash Glucose Monitoring; HbA1c = Glycosylated Hemoglobin; CI = Confidence Interval; IDF = International Diabetes Federation; IQR= Interquartile Scrap; SMBG = Self-monitoring of Blood Glucose; SSN = National Health Service
REFERENCES
- American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care 2014; 37(Suppl. 1): (S81–S90)2, 1993.
- Leslie RDG. Causes of diabetes. Genetic and environmental factors. Wiley & Sons, Chicester, 1993.
- Dianna J. Magliano, Edward J. Boyko. IDF Diabetes Atlas 10th edition scientific committee. Brussels: International Diabetes Federation; 2021.
- Gabriel A Gregory, Thomas I G Robinson, Sarah E Linklater, Fei Wang, Stephen Colagiuri, Carine de Beaufort et al. Global incidence, prevalence, and mortality of type 1 diabetes in 2021 with projection to 2040: a modelling study. Lancet Diabetes Endocrinol. 2022 Oct; 10(10):741-760.
- Lo Scalzo A, Abraha I, Bonomo MA, Chiarolla E, Migliore A, Paone S et al. Flash Continuous Glucose Monitoring Systems – Rapid HTA report for diabetes subjects in insulin therapy. Agenas: Rome, 2018.
- Fox C, Kilvert A. Il diabete di tipo 2. Tutte le risposte a portata di mano. Versione italiana a cura di Edoardo Mannucci e Caterina Lamanna. Ercules Comunicazioni, 2012.
- American Diabetes Association (ADA). Standards of Medical Care in Diabetes. Diabetes Care 2018; 41, Suppl. 1, 2018.
- Implication of Diabetes Control and Complication Trial. Diabetes Care, 2004.
- Wenqi Fan, Haipeng Pang, Zhiguo Xie, Gan Huang, and Zhiguang Zhou. Circular RNAs in diabetes mellitus and its complications. Front Endocrinol (Lausanne). 2022; 13: 885650.
- Mariarosaria De Luca, Michele Modestino, Olimpia Iacono, Anna De Simone, Vincenzo Guardasole, Angelo Foglia. Advanced hybrid closed-loop: review of the current systems available in Italy for the treatment of type 1 diabetes mellitus. JAMD 2022| VOL. 25 | N° 2: 121.
- Yaron M, Roitman E, Aharon-Hananel G, Landau Z, Ganz T, Yanuv I et al. Effect of Flash Glucose Monitoring Technology on Glycemic Control and Treatment Satisfaction in Patients With Type 2 Diabetes. Diabetes Care. 2019 Apr 29.
- Nicolucci A, R Giorgino, D Cucinotta, G Zoppini, M Muggeo, S Squatrito et al. Validation of the Italian version of the WHO-Well-Being Questionnaire (WHO-WBQ) and the WHO-Diabetes Treatment Satisfaction Questionnaire (WHO-DTSQ). Diabetes Nutr Metab. 2004 Aug;17 (4):235-43.
- Nicolucci A. L’uso dei questionari sulla qualità della vita. G It Diabetol Metab ,2006.
- Timothy C Dunn, Yongjin Xu , Gary Hayter , Ramzi A Ajjan. Real-world flash glucose monitoring patterns and associations between self-monitoring frequency and glycaemic measures: A European analysis of over 60 million glucose tests. Diabetes Res Clin Pract. 2018 Mar;137:37-46.
- Bolinder J, Antuna R, Geelhoed-Duijvestijn P, Kroger J, Weitgasser R. Novel glucose-sensing technology and hypoglycaemia in type 1 diabetes: a multicentre, non-masked, randomised controlled trial. Lancet, 2016.
- Anders L Carlson, Timothy Dilon Daniel, Andrea DeSantis, Serge Jabbour, Esra Karslioglu French , Davida Kruger et al. Flash glucose monitoring in type 2 diabetes managed with basal insulin in the USA: a retrospective real-world chart review study and meta-analysis. BMJ Open diabetes Res Care. 2022 Jan; 10(1):e002590.
- Marianna Yaron, Eytan Roitman, Genya Aharon-Hananel, Zohar Landau, Tali Ganz, Ilan Yanuv et al. Effect of Flash Glucose Monitoring Technology on Glycemic Control and Treatment Satisfaction in Patients With Type 2 Diabetes. ADA Volume 42,Issue 7, 2019 July.
- Reng-Na Yan, Ting-Ting Cai1, Lan-Lan Jiang 1, Ting Jing 1, Ling Cai , Xiao-Jing Xie et al. Real-Time Flash Glucose Monitoring Had Better Effects on Daily Glycemic Control Compared With Retrospective Flash Glucose Monitoring in Patients With Type 2 Diabetes on Premix Insulin Therapy. Front Endocrinol (Lausanne).2022 Feb 10;13:832102.
- Concetta Irace, Sergio Di Molfetta. Il monitoraggio in continuo della glicemia: stato dell’arte. Aggiornamento in tema di tecnologie. Dicembre 2022| Vol 34.| N° 4.
- Michael J. Ackerman, Rosemarie Filart, Lawrence P. Burgess, Insup Lee, and Ronald K. Poropatich.Developing Next-Generation Telehealth Tools and Technologies: Patients, Systems, and Data Perspectives.Telemedicine and e-Health.Feb 2010.93 95.
- Ming W, Lucy H Mackillop, Andrew J Farmer, Lise Loerup, Katy Bartlett, Jonathan C Levy et al. Telemedicine Technologies for Diabetes in Pregnancy: A Systematic Review and Meta-Analysis J Med Internet Res 2016; 18 (11):e290.
![]() This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Healthy Nurses: Tips for Enhancing Mental, Emotional, and Spiritual Well-being
Monica Jaramillo1*
1. Independent Author, Florida, US
*Corresponding Author: Monica Jaramillo DNP, MSN/Ed., RN-NLC, CNE®n, CCRN.
Instructor, mentor, and tutor of various healthcare programs and currently not affiliated with any institution when I submitted this manuscript to the Journal. Florida, US. Email: MonicaJaramilloDNP@Gmail.com
Open Researcher and Contributor ID: https://orcid.org/0009-0005-0572-4061
Cite this article
Abstract
Introduction: Recent literature suggests a detrimental burden affecting nurses of all settings and backgrounds. Mental and emotional problems such as moral distress, burnout, compassion fatigue, depression, and severe stress are a few of the many issues nurses are experiencing worldwide. Nurses need enhanced guidance and support regarding caring for their health and well-being.
Discussion: It is imperative to advocate for healthier nurses worldwide. Nurses are experiencing several mental issues and burnout due to a lack of resilience and self-care management. All key stakeholders internationally need to aid nurses with feasible tools that promote mindfulness and improvement of self-care while ensuring stability. The key to enhancing nurses’ mental, emotional, and spiritual well-being could be to offer holistic support conducive to mind-body-spirit and physical health.
Keywords: Healthy Nurses; Holistic; Wholistic; Mental; Emotional; Spiritual; Well-being.
Introduction
Nursing is a caring and compassionate profession full of holistic practices that advocate for the health and well-being of entire communities. Unfortunately, nurses worldwide continue failing in the call to care for themselves in the same empathetic manner as they care for others.[1-3] Nurses nowadays face burnout, fatigue, depression, and severe mental problems such as moral distress and compassion fatigue, to name some of the many stressors, at an exponential rate.[1,2] Healthy nurses are associated with better care outcomes since they represent strong role models for the community and positive health and wellness advocates.[1-3] It is time to advocate more actively for our nurses’ health and well-being while providing support conducive to enhancing their mental, emotional, and spiritual well-being. This work aims to inspire change in nursing through practical advice for all stakeholders while empowering nurses to build resilience and positive self-care practices.
Healthy nurses care for their physical, emotional, spiritual, and mental health while living life to its maximum capacity. Healthy nursing professionals prioritize their well-being as much as they prioritize those they care for. These nurses represent significant advocacy to all communities as they role-model positive and empathetic self-care practices conducive to healthy and meaningful living.[3] Indeed, the health and well-being of nurses are valuable and essential concepts to cultivate to ensure positive outcomes. The importance of healthy nurses is entitled to the impact of these professionals on their communities.[1-3] Nurses are the caregivers and the image many have to look after. Many individuals from all communities around the globe follow nurses’ advice regarding healthy living, and these individuals see nurses are their exemplars of living meaningful lives.[1,2] It is time for nurses of all practice settings and levels of expertise to take a more active role in their health while using the available resources to live their lives to the fullest. Seek help in your institutions or from national and international associations. Many resources are at hand to support you in all ways that ensure the professional development and advancement of the nursing profession and the health and well-being of all nurses. One example of the multiple national resources available for nurses in the United States is the American Nurses Association (ANA). This organization represents and supports 4.3M nurses nationwide while empowering them to thrive in all aspects of their personal and professional lives.[4] The multiple initiatives ANA has established to ensure healthy nurses while ensuring a healthy country are worth exploring. In the end, it all entitles building resilience and incorporating self-care. Nurses’ resilience represents coping with unforeseen or stressful situations and returning to healthy and balanced wellness after a crisis, while self-care promotes mind and body wholeness.[5,6] This composition explores the definition and importance of healthy nurses, tips for building resilience, feasible techniques for wholistic self-care, and recommendations. This commentary includes a discussion and a conflict of interest statement.
Discussion
Resilience is the ability to withstand adversity.[5] Undoubtedly, all nurses, despite their area of expertise, face some level of difficulty and stress. Nurses must be mindful of the need to adapt to challenging situations successfully.[5,6] This author’s most remarkable experiences with resilience and mindfulness arise from clinical experiences in intensive care and the pressure of completing advanced-practice nursing degrees of education toward the terminal degree in nursing. The chaos of multiple professional and personal demands and the responsibility of caring for patients in a life-death environment is highly challenging. Still, from tough situations like this emerge great realizations. Accordingly, the scientific evidence around the globe is conclusive in suggesting that nurses worldwide need mental and emotional support to mitigate their stress and burnout.[1-3] It is imperative for nurses to improve their resilience and for all key stakeholders to support the health and well-being of nurses with tools that will enhance wholeness.[5,6] Some of the most helpful tips for building resilience in this author’s experience include using all the available resources, starting soon in the career, practicing gratitude, sparking the passion for nursing often, and taking enough time for self-care daily. In this regard, seeking help when first needed while exploring resources such as counseling, mentoring, connections, or community programs is ideal. Similarly, gratitude and purpose or passion for nursing can increase resilience. Lastly, self-care is another valuable component of resilience worth exploring separately.
Self-care is also vital for every person’s health and well-being, not just for nurses. This concept means taking care of self while ensuring both physical and mental, spiritual, and mental health in a comprehensive or wholistic manner. Now, wholistic can mean different things to different people, and the term may be unknown to many others.[7] For this author, this term means ensuring holistic practices that entitle the whole aspects of the person and caring for self comprehensively and holistically while embracing mind-body-spirit. Seeing self-care from this wholistic approach can be the key to improve not only resilience but nurses’ mental, physical, emotional, and spiritual well-being.
In this author’s experiences, feasible techniques to ensure wholistic self-care in nurses and all individuals despite their culture and background are as follows. First, be true to yourself by following your mind and heart’s desires. Advocating for your well-being first is vital, as hard as this may sound for many nurses considering our call to serve others. Follow your preferences, call to help, and continue that path with your health in mind. Second, perform regular physical activities that are attractive to you personally. This step can be as simple as taking the stairs at work instead of the elevator to have peace of mind that you are incorporating self-care into your daily practices. Third, engage in excellence groups or advocacy associations of your interest as much as possible to promote self-pride. Fourth, be an active advocate for self-care practices in your organization. For this, you may explore the available resources and recommend a practice change policy that promotes more initiatives to ensure the health and well-being of nursing staff. Lastly, do not forget to be kind to yourself and reward yourself often for your achievements.
It is imperative to ensure the health and well-being of nurses around the globe. Healthy nurses are professionals who live their lives to the fullest while inspiring the community to live healthy and meaningful lives. Ensuring nurses’ physical, mental, emotional, and spiritual well-being requires strong resilience and conscious self-care. These wholistic practices can positively impact all nurses directly while indirectly improving entire communities’ health. It is time to increase advocacy regarding nurses’ health while reminding these professionals to utilize available resources, seek help when needed, practice activities they enjoy, ensure self-care as part of their daily routines, and be kind to themselves. The author hopes to inspire all stakeholders to advocate for healthier nurses and invites further research and studies concerning this vital topic for global public health.
Funding Statement
This research received no external funding.
Conflict of Interest Statement
The author declares no conflict of interest
References
- Wand T, Glover S, Paul D. What should be the future focus of mental health nursing? Exploring the perspectives of mental health nurses, consumers, and allied health staff. International Journal of Mental Health Nursing. 2021;31(1).
- Khatatbeh H, Pakai A, Al‐Dwaikat T, et al. Nurses’ burnout and quality of life: A systematic review and critical analysis of measures used. Nursing Open. 2021;9(3).
- Rykkje L, Søvik MB, Ross L, McSherry W, Cone P, Giske T. Educational interventions and strategies for spiritual care in nursing and healthcare students and staff: A scoping review. Journal of Clinical Nursing. 2021.
- American Nurses Association. Healthy Nurse, Healthy Nation [Internet]. American Nurses Association; [cited 2023 April 18]. Available from: https://www.nursingworld.org/practice-policy/hnhn/
- Janzarik G, Wollschläger D, Wessa M, Lieb K. A group intervention to promote resilience in nursing professionals: A randomised controlled trial. International Journal of Environmental Research and Public Health. 2022;19(2):649.
- Zeb H, Arif I, Younas A. Mindful self-care practice of nurses in acute care: A multisite cross-sectional survey. Western Journal of Nursing Research. 2021;44(6):019394592110045.
- Chizhande I. No health without wholistic health: An empirical approach to mental health cultivation. Asian Journal of Research in Social Sciences and Humanities. 2022;12(4):416-424.
![]() This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
MUSIC THERAPY FOR PAIN AND ANXIETY IN HOSPITALIZED CHILDREN: A SYSTEMATIC REVIEW OF RANDOMIZED CONTROLLED TRIAL
Arvida Bar1, Monalisa2*, Netha Damayantie3, Halimah4
1,2,3,4Department of Nursing, Health Polytecnic of Jambi, Indonesia
* Corresponding author: Monalisa, Jl. Dr. Tazar, Buluran Kenali, Kec. Telanaipura, Kota Jambi, Jambi 36361, Indonesia, Orcid: https://orcid.org/0000-0002-4879-3893
Email: monalisa.poltekkes@gmail.com
Phone: +62 821-8656-3003
Cite this article
ABSTRACT
Introduction. Music has been widely recognized for its effectiveness in controlling anxiety and pain. However, in particular groups such as children, the implementation may be challenging, especially regarding the type of music selection. The aim of the study is to evaluate the music therapy efficacy on pain and anxiety management in pediatric care to improve the management of pain and anxiety in the pediatric population.
Methods. This review was written according to the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) statement. In assessing the impact of music therapy as a method of pain and anxiety management in pediatric care, a database tracking was conducted for articles publicized between 2000 and 2022. The databases used including Sciencedirect, Cochrane library, PubMed, and Wiley online library. Articles were deemed if the study subjects ranged in age from 0 to 21 years old, the intervention was live or recorded music, and the study took place in an inpatient background.
Results. 1,129 publications were discovered. In final search of literature, there are 12 articles included in this review. There is consistent and consequential evidence that music may relieve pain and anxiety in hospitalized children before and during procedures. The type of music that is widely used is classical and traditional instrumental music. In addition, there were only two studies using nursery rhymes.
Conclusion. The patient’s preference in choosing music for children enables them to determine the appropriateness of therapy. Classical music can be the main choice in applying music therapy in reducing anxiety and pain in children.
Keywords: Pediatric; music; pain; anxiety; inpatient; nurse
INTRODUCTION
Extreme anxiety may harm a child’s physical and psychological health, cause adverse postoperative outcomes that hinder recuperation, rehabilitation and reduce a child’s alliance in self-care [1–3]. Hospitalized children may experience anxiety due to daily activities, recurring convulsions, loss of control, or loneliness [4–6]. According to the current study, compelling pain and anxiety management are critical to healing [7,8]. Untreated pain and anxiety may cause diverted recovery, extended hospitalization, impaired physical growth and development, faked personality, and a lifelong nervousness of medical providers and treatments to be inducted [6,9–12].
There are multiple hindrances to implementing sufficient management of child care. Many parents and healthcare providers fear the side effects of pain and anxiety remedies [13–16]. Since 1999, the U.S. pediatric mortality rate, ages 0 to 19, has nearly tripled due to illicit prescription opioids [18]. Due to the risks and harmful effects of sole reliance on pharmacological treatments, Governments and healthcare providers are striving for alternative non-pharmacological modalities for manipulating pain and anxiety, particularly in children [19].
Music, touch, and nurse-led distraction techniques are non-pharmacological therapies currently widely used in pediatric care [20]. This therapy is effective in helping reduce the dose and duration of pain and anxiety medications and improve pain and anxiety scores; thus, nurses can continue to maintain their autonomy [21,22]. Focusing on music therapy turns out that this therapy has the potential to reduce or even eliminate the need for pharmacological therapy (18). Music also impacts human emotional and physiological responses by diverting attention from the symptoms of pain and anxiety that arise (19). The theory best known as the mechanism of pain, Gate Control, posits that pain receptors collaborate to transmit pain signals to the brain [23]; thus, distractions such as music can block specific pain pathways and reduce the amount of pain felt. Music therapy sessions allow individuals to express their pain and anxiety in healthy ways, such as through improvised songs and playing instruments [24,25]. Music has been used in clinical settings such as general practice (medical and dental) and more specialized settings such as surgery and related medical professions (such as physiotherapy and speech therapy). It is essential to recognize differences between the clinical practice of music therapists, who are certified, and the use of music by lay practitioners, who are not explicitly trained or have some background in music psychology or clinical psychology [26,27].
Previous systematic reviews of randomized controlled trial studies concluded the excellent efficacy of music therapy for children in controlling pain and anxiety when facing medical procedures. However, these studies could have clearly shown the type of music and therapy delivery method, which is still a big question [28]. Another review study found that the evidence for the effectiveness of using music to reduce dental anxiety in children is inconclusive and of limited quality [27]. The present review study aims to assess the effect of music therapy on pain and anxiety management in pediatric care to improve pain and anxiety management in the pediatric population from existing literature published from 2000 to 2022. The time-lapse choosen to updating studies in previous review. Review question including what types of music most used? What method used to deliver the music?
METHODS
Review Protocol
Following the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) 2020 guidelines, we conducted a systematic review of the literature consisting of Randomized Controlled Trials (RCTs) that apprised the effectiveness of music therapy in alleviating pain and anxiety in pediatric care [29].
Eligibility Criteria
We removed duplicates and uploaded articles to the web-based bibliography and database manager. It was then distributed to the team members, and a single reviewer initially reviewed the title and abstract. The following step was a full-text review by two reviewers. Additional reviewers were organized to deal with contentions to reach a consensus. The inclusion criteria include subjects ranged in age from 0 to 21, using live or recorded music in a hospital setting, effective or ineffective in alleviating pain and anxiety, and the full text was available in English. Articles are excluded if located in an outpatient setting, such as an emergency department or venipuncture clinic; music therapy by a music therapist; in labour or involving pregnant adolescents; during surgery or under general anaesthesia, or occurs in the neonatal intensive care unit (NICU) or pediatric intensive care unit (PICU). Babies treated in the NICU must be excluded because premature babies’ nervous systems are immature, so they respond to pain differently from full-term babies. Although not all babies treated in the NICU are premature, several articles do not always distinguish between premature and full-term babies born in the NICU. Theses or dissertations, conference articles, comments, editorial reports, and poster presentations are exempt.

Table 1. PICOS statement
Information source
A medical librarian searched a database for articles published in the previous ten years, from 2000 to 2022, in May 2022. Sciencedirect, Cochrane library, PubMed, and Wiley online library were all searched.
Search Strategy
PubMed, Sciencedirect, Wiley Online Library, and the Cochrane Library were among the databases searched. Furthermore, we also search on the list of references in the article that meet the criteria to broaden the search results further. In creating a comprehensive search strategy for each database, the following search terms were used: (1) pediatric, child, adolescent, infant, infant, toddler, adolescent, adolescent, male, female, (2) pain, tone, voice (3) anxiety (4) hospitalization, hospitalization, procedure, postoperative, surgery. A review of all included study references was also conducted. We also add filters to each database, including publication type and research design.

Table 2. Search String
Data Collection
Two authors independently screened the title and abstract to suit the inclusion criteria, if it was not clear, then they continued by reading the main text. No automation tools were used in selection literatures.
Data Extraction
To extract the required data, we followed the McMaster Critical Review Form-Quantitative Studies v. 2.0 and added some information that we think is important. The data we extracted included authors, countries, outcomes, study designs, participants, interventions, evaluation methods, and main findings. Two authors performed data extraction independently. The finalization of the extraction process was read and endorsed by the first author.
Quality of the Study
Study quality was assessed by two authors independently using the Critical Appraisal Skills Program (CASP) for the Randomized Controlled Trial [30]. This tool consists of 11 questions which are divided into four sections with the choices of Yes, No, and Can’t Tell checklist columns. We categorize the quality of studies into High, Medium, and Low. High quality studies if you have answers YES 10 – 11/11, medium quality if you have answers YES 7 – 9/11, and Low quality if answers YES ≤6/11.
Study Risk of Bias Assessment
The risk of bias or validity in the process and results of a systematic review is reflected in its methodological quality. The Cochrane Handbook 5.2.0 was used to reckon methodological quality. Two authors independently assessed the risk of bias in the included studies. In the circumstance of a disagreement, refer it to the corresponding author for arbitration. The Cochrane bias risk assessment tool was used to evaluate the risk of RCTs, which possessed random sequence generation, allocation concealment, blinding of subjects and researchers, blinding of outcome assessment, insufficient outcome data, and selective reporting.
RESULTS
Study Selection
A systematic electronic search identified that 1,129 publications were discovered through backward searching of relevant papers. The full-text screening was conducted on 783 articles. A total of 692 articles failed to meet eligibility criteria at the full-text screening stage, and only 12 articles were finally eligible for further analysis. The search results follow the PRISMA 2020 flow diagram (Fig. 1).
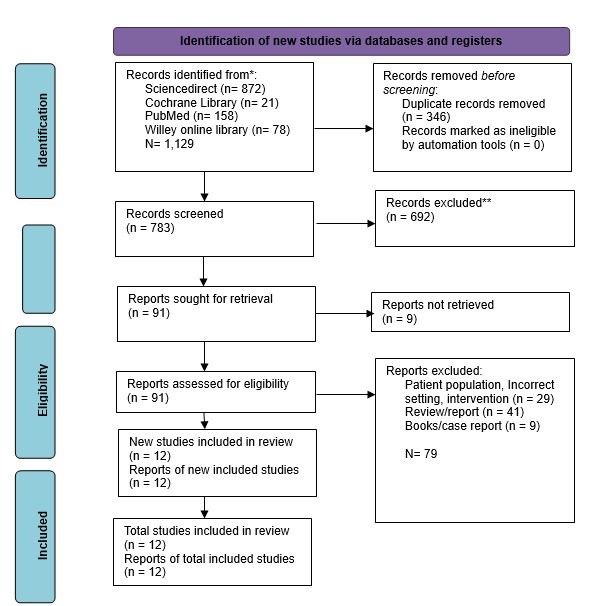
Figure 1. PRISMA flow diagram for literature search


Table 3. Characteristics of studies included.
Study Characteristics
Eleven randomized controlled trials (RCTs) and one quasi-experimental study met the inclusion criteria and was analyzed. The studies included 543 participants ranging in age from seven days to 18 years. The research was conducted in eight countries: India (8.33%, n=1) [31], Brazil (8.33%, n=1) [32], Iran (16.67%, n=2) [33,34], South Korea (8.33%, n=1) [35], the United Kingdom (UK) (8.33%, n=1) [36], Vietnam (8.33%, n=1) [37], the United States (US) (16.67%, n=2) [38,39], Turkey (8.33%, n=1) [25], and China (16.67%, n=2) [40,41].
Studies reported the implementation of music therapy before a procedure (n =5, 41.67%), during a procedure (n =4, 33.33%), after a procedure (n =6, 50%), or at any time during a hospitalization (n =2 16.67%), music-based interventions were used. The time spent listening to music ranged from 1 minute to at least 30 minutes. Most of the studies (n=7, 58.3%) used recorded music with headphones (n=7, 58.3%); one used speakers and ambient music.
The studies in the analysis scrutinized the effects of music-based interventions on pain (n=5, 41.67%) and anxiety (n=5, 41.67%). Some studies found a consequential lowering in pain scores in the music group (n=3), while others found no significant reduction (n=2). Before and during procedures, all studies conveyed a significant reduction in anxiety scores in the music group (n=5). Only one study discovered no significant lessening in anxiety scores in the music group following surgery.
Study quality
Based on the results of the study quality assessment which consisted of thirteen questions, only four studies were in the High Quality category, and eight other studies were in the Medium Quality category.

Table 4. Summary of quality assessment
Risk of Bias in Studies
Based on the bias assessment, all studies are in the low category in the Bias in measurement of the outcome domain. For overall bias, there are four studies that are in the Some Concerns category, and eight studies that are in the Low risk of bias category.

Figure 2. Traffic-light plot for RoB in individual study
Effect on Anxiety
There are eight studies [25,32,34,35,37,38,40] who analyzed the effect of music on pediatric anxiety in dealing with hospital care situations. The measurements of participants’ anxiety levels used a variety of instruments, including The Observational Scale of Behavioral Distress (OSBD), the modified Yale Preoperative Anxiety Scale (mYPAS), and The Spielberger State-Trait Anxiety Inventory (STAIC). Overall there was a significant decrease in anxiety in the studies that analyzed the effects of this music intervention.
Effect on Pain
There are nine studies [25,31,33,36–41] who analyzed the effect of music on the level of pain experienced by pediatricians. However, two studies showed insignificant results in reducing experienced pain [31,41]. The instruments used to measure pain include Wong-Baker Faces (WB-FACES), Visual Analog Scale (VAS), Numeric rating scale (NRS), and The Children’s Hospital of Eastern Ontario Pain Scale (CHEOPS).
DISCUSSION
Non-pharmacologic methods are widely used as forms of pain, fear, and vomiting control for children in the hospital setting. There are several medical procedures in the hospital that can provide an unpleasant experience, especially in Pediatric care. This review evaluated the impact of music therapy as a corroborative strategy for pain and anxiety control in hospitalized children. The publications’ central theme was statistically meaningful evidence that music can decline anxiety before and during procedures [32,34,35,37,38,40,41]. However, results concerning pain, often viewed as physiologic analogs to pain, were mixed [31,32,36–39,41]. Music-based interventions are also secure for hospitalized children, according to the evidence. Only one RCT reported any negative effects, deemed minor and mostly related to headphone affliction or no refinement in pain or anxiety scores [37].
It is crucial to explore patient factors that contributed to music interventions’ success in employing this review’s findings. Several studies have emphasized the importance of patient discretion in deciding on music for children [32,37,39,41]. Researchers have allowed two-year-olds to choose the type of music they want to listen to in several research studies [37,39,41]. According to one study, this sovereignty contributed to lower pain and anxiety levels in music groups [37]. In another study, subjects were reluctant to listen to researcher-selected music, resulting in significant sample loss [32]. It reflects a broader healthcare shift towards patient-centered care over the past decades, recognizing the importance of patient preferences in achieving positive health outcomes[24]. Music-based interventions deliver tangible ways for children to partake directly in care giving and manage challenging situations.
It is also important to regard the kit for implementing musical interventions. There is a high reliance on pre-recorded audio delivered through headphones. It exemplifies the viability and cost-effectiveness of music interventions in the hospital. The costs associated with the equipment needed to play music are relatively affordable, and several previous studies suggest that nurses may execute interventions without formal internship [32,35,37,39,41].
Music treatment is unassailable, affordable, and uncomplicated to learn, and hospital nurses can use it efficiently [42]. Music in nursing practice can be used unattended or in concurrence with other methods, such as jaw relaxation [43] and therapist guidance [44]; it can be used in a variety of sets, circumstances, and people for a miscellany of pursuits [43–47]. According to studies, 20-90 minutes of music therapy is an adequate remedy time. The following types of music were played: Sedative music [48], researcher-supplied music and subject-preferred music, smoothing music, and easy-listening music are all examples of sedative [46].
Music therapy may activate the natural analgesia in the human body that leads to alleviating pain, known as Endorphine [49]. Endorphine is a neuro hormone provoking pleasant sensations. The pain will be relieved along with parasympathetic system activation, which leads to the relaxation of the body. Aside from feel-good chemicals, nor-adrenaline and serotonin contribute enormously to pain relief via attenuated transmission of the brain’s descending impulse. The descending control system is a sensory neuron fiber that runs from the midbrain (precisely the peri-aqueductal gray matter) to the inter-neuronal inhibitory system [50–52]. The system will remain active in response to the stimulus of soft music, which inhibits the transmission of the pain stimulus. Music therapy has been shown to stimulate the axons or nerve fibers on the ascending tracts of RAS neurons (Reticular Activating System). The stimulus is transmitted to the cerebral cortex, limbic system, and corpus callosum through the autonomous nervous and neuro-endocrine systems. When one is immersed in soft music, the limbic system is aroused, causing it to secrete phenylethylamine (neuroamin), which controls impulse and mood emotion. Music stimulates the parasympathetic nervous system to work on the sympathetic nerves, causing the switch to alpha-type brain waves to yield soothing outcomes on the autonomic nervous system [53–55].
The physiological justification backs up the study’s finding that music therapy has a positive effect on reducing or relieving anxiety and pain in children. Nurses ought to employ a combination of pharmacologic and non-pharmacologic interventions to relieve pain and avoid the medication’s unwanted side effects [56]. It lays the hypothetical underpinnings for skillful or qualified nurses to gain new knowledge of other methods effective in relieving pain and anxiety, such as the use of music therapy, in health-care facilities. It echoes the assertion made by Huang, Good, and Zauszniewski [48] that music therapy is one of the interventional techniques that has concrete proof nursing theories to proficiently alleviate anxiety and pain.
Indeed although all considerations included in this integrator writing survey are of tall or great quality, it is conceivable that the comes about might have been impacted by pondering confinements. For case, a few ponder utilized a little test measure or did not incorporate a test estimate calculation. Test estimate was famous when evaluating the quality of each article. In expansion, most things did not dazzle the analysts, spectators, or members. Even though blinding in the investigation is critical to play down any conceivable inclination, it is troublesome to do so with music-based mediations, especially live music.
Two studies used an invalidated pain or anxiety scale in the study population, which was highlighted when appraising the precision of each article [37,41]. Because pain and anxiety are subjective, they are challenging to assess. Standardized pain and anxiety scales are used by providers to assess pain and anxiety, especially in nonverbal or nonresponsive patients. CHEOPS, FACES, FPS-R, NRS, and VAS pain scales were used in the studies. The m-YPAS and STAIC anxiety scales were used in the studies. While there are numerous pain and anxiety scales available, a validated and user-friendly pain or anxiety scale may not always be obtainable or ubiquitously used for the workforce being ascertained.
A wide age range of participants was used in multiple studies. From infancy to adolescence, children’s emotions, personalities, behavior, and speech will grow and develop. The way children react to stimuli like pain and anxiety will vary based on their developmental stage and age. Despite the fact that the studies only looked at children aged 0 to 18, the use of such a wide age range of individuals makes the reliability analysis of the findings questionable.
LIMITATION
In our search for full-text articles, we only collected 12 articles due to the limited access we faced, which prevented us from further exploring the magnitude of the effect of music therapy on pain and anxiety in children in the form of a meta-analysis. Some of the studies we include are also in the Some Concern category, so using the results of this study requires caution. However, we believe that nurses can apply music therapy autonomously in managing pain and anxiety in children as a form of nursing implementation and improving the quality of care.
CONCLUSION
For children in the hospital, pain, and anxiety often come to them in various incredibly invasive medical procedures. Music therapy can be the first choice for nurses to offer children with minimal side effects and is friendly to children’s conditions. Physiologically, music therapy can trigger natural analgesics in the body through neurohormones that have a calming effect. Based on studies that apply music therapy, the type of music generally used in classical music is delivered through headphones. Future studies can further examine how music therapy influences chronic pain conditions in children.
Conflict of Interests
There is no conflict of interest.
Ethical Approval
Ethics approval Ethical approval will not be required because this study will retrieve and synthesize data from already published studies.
Acknowledgments
We would like to express our gratitude to all parties, particularly the director of Health Polytechnic of Jambi.
Author’s Contribution
All authors equally contributed to preparing this article.
Funding/Support
This research did not receive any specific grant from funding agencies in the public, commercial, or not for profit sectors.
REFERENCES
- van der Heijden MJE, Jeekel J, Rode H, Cox S, van Rosmalen J, Hunink MGM, et al. Can live music therapy reduce distress and pain in children with burns after wound care procedures? A randomized controlled trial. Burns. 2018;44(4):823–33.
- Anggerainy SW, Wanda D, Nurhaeni N. Music therapy and story telling: Nursing interventions to improve sleep in hospitalized children. Comprehensive child and adolescent nursing. 2019;42(sup1):82–9.
- Zhu X, Haegele JA, Healy S. Movement and mental health: Behavioral correlates of anxiety and depression among children of 6–17 years old in the US. Mental Health and Physical Activity. 2019;16:60–5.
- Gomes GLL, Fernandes M das GM, Nóbrega MML da. Hospitalization anxiety in children: conceptual analysis. Revista brasileira de enfermagem. 2016;69:940–5.
- Li WHC, Chung JOK, Ho KY, Kwok BMC. Play interventions to reduce anxiety and negative emotions in hospitalized children. BMC pediatrics. 2016;16(1):1–9.
- Delvecchio E, Salcuni S, Lis A, Germani A, Di Riso D. Hospitalized children: anxiety, coping strategies, and pretend play. Frontiers in public health. 2019;7:250.
- Gogoularadja A, Bakshi SS. A Randomized study on the efficacy of music therapy on pain and anxiety in nasal septal surgery. International Archives of Otorhinolaryngology. 2020;24:232–6.
- Cırık V, Efe E. THE EFFECT OF MUSIC THERAPY IN CHILDREN’S HEALTH. Journal of Educational & Instructional Studies in the World. 2018;8(2).
- Chow CHT, Van Lieshout RJ, Schmidt LA, Dobson KG, Buckley N. Systematic review: audiovisual interventions for reducing preoperative anxiety in children undergoing elective surgery. Journal of pediatric psychology. 2016;41(2):182–203.
- Lerwick JL. Minimizing pediatric healthcare-induced anxiety and trauma. World journal of clinical pediatrics. 2016;5(2):143.
- Fronk E, Billick SB. Pre-operative anxiety in pediatric surgery patients: Multiple case study analysis with literature review. Psychiatric Quarterly. 2020;91(4):1439–51.
- Johnson AA, Berry A, Bradley M, Daniell JA, Lugo C, Schaum-Comegys K, et al. Examining the effects of music-based interventions on pain and anxiety in hospitalized children: An integrative review. Journal of Pediatric Nursing. 2021;60:71–6.
- Bawa M, Mahajan JK, Aggerwal N, Sundaram J, Rao KLN. Barriers to pediatric pain management in children undergoing surgery: A survey of health care providers. Journal of Pain & Palliative Care Pharmacotherapy. 2015;29(4):353–8.
- Katende G, Mugabi B. Comforting strategies and perceived barriers to pediatric pain management during IV line insertion procedure in Uganda’s national referral hospital: A descriptive study. BMC pediatrics. 2015;15(1):1–8.
- Greenfield K, Carter B, Harrop E, Jassal S, Bayliss MJ, Renton K, et al. Healthcare professionals’ experiences of the barriers and facilitators to pediatric pain management in the community at end-of-life: a qualitative interview study. Journal of Pain and Symptom Management. 2022;63(1):98–105.
- Sabeti F, Mohammadpour M, Pouraboli B, Tahmasebi M, Hasanpour M. Health Care Providers’ experiences of the non-pharmacological pain and anxiety management and its barriers in the Pediatric Intensive Care Units. Journal of Pediatric Nursing. 2021;60:e110–6.
- Rudd RA, Aleshire N, Zibbell JE, Gladden RM. Increases in drug and opioid overdose deaths—United States, 2000–2014. Morbidity and mortality weekly report. 2016;64(50 & 51):1378–82.
- Gaither JR, Shabanova V, Leventhal JM. US national trends in pediatric deaths from prescription and illicit opioids, 1999-2016. JAMA network open. 2018;1(8):e186558–e186558.
- Bizzio R, Cianelli R, Villegas N, Hooshmand M, Robinson M, Hires KA, et al. Exploring non-pharmacological management among anesthesia providers to reduce preoperative distress in children. Journal of pediatric nursing. 2020;50:105–12.
- Giordano F, Zanchi B, De Leonardis F, Rutigliano C, Esposito F, Brienza N, et al. The influence of music therapy on preoperative anxiety in pediatric oncology patients undergoing invasive procedures. The Arts in Psychotherapy. 2020;68:101649.
- Uggla L, Bonde L, Hammar U, Wrangsjö B, Gustafsson B. Music therapy supported the health‐related quality of life for children undergoing haematopoietic stem cell transplants. Acta paediatrica. 2018;107(11):1986–94.
- Mondanaro JF, Sara GA, Thachil R, Pranjić M, Rossetti A, Sim GE, et al. The effects of clinical music therapy on resiliency in adults undergoing infusion: a randomized, controlled trial. Journal of Pain and Symptom Management. 2021;61(6):1099–108.
- Melzack R, Wall PD. Pain Mechanisms: A New Theory: A gate control system modulates sensory input from the skin before it evokes pain perception and response. Science. 1965;150(3699):971–9.
- Finnerty R. Music therapy as an intervention for pain perception. Anglia Ruskin University, Cambridge, England. 2006;
- Bulut M, Alemdar DK, Bulut A, Şalcı G. The effect of music therapy, hand massage, and kaleidoscope usage on postoperative nausea and vomiting, pain, fear, and stress in children: A randomized controlled trial. Journal of Perianesthesia Nursing. 2020;35(6):649–57.
- Stegemann M. therapy and other music-based interventions in pediatric health care: An overview. Medicines;
- Ainscough SL, Windsor L, Tahmassebi JF. A review of the effect of music on dental anxiety in children. European Archives of Paediatric Dentistry. 2019;20(1):23–6.
- Klassen JA, Liang Y, Tjosvold L, Klassen TP, Hartling L. Music for pain and anxiety in children undergoing medical procedures: a systematic review of randomized controlled trials. Ambulatory pediatrics. 2008;8(2):117–28.
- Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. International Journal of Surgery. 2021;88:105906.
- Programme CAS. CASP randomised controlled trial checklist. 2018.
- Balan R, Bavdekar SB, Jadhav S. Can Indian classical instrumental music reduce pain felt during venepuncture? The Indian Journal of Pediatrics. 2009;76(5):469–73.
- Franzoi MAH, Goulart CB, Lara EO, Martins G. Music listening for anxiety relief in children in the preoperative period: a randomized clinical trial. Revista latino-americana de enfermagem. 2016;24.
- Sabzevari A, Kianifar H, Jafari SA, Saeidi M, Ahanchian H, Kiani MA, et al. The effect of music on pain and vital signs of children before and after endoscopy. Electronic physician. 2017;9(7):4801.
- Kazemi S, Ghazimoghaddam K, Besharat S, Kashani L. Music and anxiety in hospitalized children. Journal of Clinical and Diagnostic Research. 2012;6(1):94–6.
- Kim SJ, Oh YJ, Kim KJ, Kwak Y-L, Na S. The effect of recorded maternal voice on perioperative anxiety and emergence in children. Anaesthesia and intensive care. 2010;38(6):1064–9.
- Longhi E, Pickett N, Hargreaves DJ. Wellbeing and hospitalized children: can music help? Psychology of music. 2015;43(2):188–96.
- Nguyen TN, Nilsson S, Hellström A-L, Bengtson A. Music therapy to reduce pain and anxiety in children with cancer undergoing lumbar puncture: a randomized clinical trial. Journal of Pediatric Oncology Nursing. 2010;27(3):146–55.
- Noguchi LK. The effect of music versus nonmusic on behavioral signs of distress and self-report of pain in pediatric injection patients. Journal of Music Therapy. 2006;43(1):16–38.
- Suresh S, De Oliveira GS, Suresh S. The effect of audio therapy to treat postoperative pain in children undergoing major surgery: a randomized controlled trial. Pediatric Surgery International. 2015;31(2):197–201.
- Liu Y, Petrini MA. Effects of music therapy on pain, anxiety, and vital signs in patients after thoracic surgery. Complementary therapies in medicine. 2015;23(5):714–8.
- Yu H, Liu Y, Li S, Ma X. Effects of music on anxiety and pain in children with cerebral palsy receiving acupuncture: A randomized controlled trial. International Journal of Nursing Studies. 2009;46(11):1423–30.
- Wang C-F, Sun Y-L, Zang H-X. Music therapy improves sleep quality in acute and chronic sleep disorders: A meta-analysis of 10 randomized studies. International journal of nursing studies. 2014;51(1):51–62.
- Good M, Anderson GC, Ahn S, Cong X, Stanton‐Hicks M. Relaxation and music reduce pain following intestinal surgery. Research in nursing & health. 2005;28(3):240–51.
- Gutgsell KJ, Schluchter M, Margevicius S, DeGolia PA, McLaughlin B, Harris M, et al. Music therapy reduces pain in palliative care patients: a randomized controlled trial. Journal of pain and symptom management. 2013;45(5):822–31.
- Chaput-McGovern J, Silverman MJ. Effects of music therapy with patients on a post-surgical oncology unit: A pilot study determining maintenance of immediate gains. The Arts in Psychotherapy. 2012;39(5):417–22.
- Allred KD, Byers JF, Sole M Lou. The effect of music on postoperative pain and anxiety. Pain Management Nursing. 2010;11(1):15–25.
- Wurjatmiko AT. The effects of music therapy intervention on the pain and anxiety levels of cancer patient: A systematic review. International Journal of Nursing Education. 2019;11(4):14–8.
- Huang S-T, Good M, Zauszniewski JA. The effectiveness of music in relieving pain in cancer patients: a randomized controlled trial. International journal of nursing studies. 2010;47(11):1354–62.
- Aktaş YY, Karabulut N. The use of cold therapy, music therapy and lidocaine spray for reducing pain and anxiety following chest tube removal. Complementary therapies in clinical practice. 2019;34:179–84.
- Cowen R, Stasiowska MK, Laycock H, Bantel C. Assessing pain objectively: the use of physiological markers. Anaesthesia. 2015;70(7):828–47.
- McInnis PM, Braund TA, Chua ZK, Kozlowska K. Stress-system activation in children with chronic pain: a focus for clinical intervention. Clinical Child Psychology and Psychiatry. 2020;25(1):78–97.
- Wei Y, Liang Y, Lin H, Dai Y, Yao S. Autonomic nervous system and inflammation interaction in endometriosis-associated pain. Journal of Neuroinflammation. 2020;17(1):1–24.
- Riganello F, Cortese MD, Arcuri F, Quintieri M, Dolce G. How can music influence the autonomic nervous system response in patients with severe disorder of consciousness? Frontiers in neuroscience. 2015;9:461.
- Akimoto K, Hu A, Yamaguchi T, Kobayashi H. Effect of 528 Hz music on the endocrine system and autonomic nervous system. Health. 2018;10(09):1159.
- Yamashita K, Kibe T, Ohno S, Kohjitani A, Sugimura M. The effects of music listening during extraction of the impacted mandibular third molar on the autonomic nervous system and psychological state. Journal of Oral and Maxillofacial Surgery. 2019;77(6):1153-e1.
- Yaban ZS. Usage of non-pharmacologic methods on postoperative pain management by nurses: Sample of turkey. International Journal of Caring Sciences. 2019;12(1):529–41.
![]() This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.