COVID-19 Vaccines Side Effects Among Iraqi people In Kurdistan Region: A cross-sectional study
Rebar Yahya Abdullah1*, Arazoo Issa Tahir2, Dlkhosh Shamal Ramadhan3, Zuhair Rushdi Mustafa4, Kawther Mohammed Galary5
1 MSc. (Maternity and Community Health Nursing Department, College of Nursing, University of Duhok,Kurdistan,Iraq).
2 MSc (Nursing Department, Bardarash Technical Institute, Duhok Polytechnic University, Kurdistan,Iraq).
3 MSc (Maternity and Community health nursing Department, College of Nursing, University of Duhok, Kurdistan, Iraq)
4PhD (Adult Nursing Department, College of Nursing, University of Duhok, Kurdistan, Iraq).
5 MSc (Maternity and Community Health Nursing Department, College of Nursing, University of Duhok, Kurdistan, Iraq).
*Corresponding Author: Rebar Yahya Abdullah, Maternity and Community Health Nursing Department, College of Nursing, University of Duhok, Kurdistan, Iraq.
E-mail: rebar.abdullah@uod.ac
Cita questo articolo
ABSTRACT
Background: Communities around the world have expressed concern about the safety and side effects of SARS-CoV-2 vaccines. The adverse effects of the Covid-19 vaccines played a critical role in public trust in the vaccines. The current study aimed to provide evidence on the side effects of the BNT163b2 mRNA COVID-19 vaccine (Pfizer-BioNTech®); ChAdOx1 nCoV-19 vaccine (AstraZeneca®); BBIBP-CorVvaccine (Sinopharm®) COVID-19 vaccines.
Material and Methods: A cross-sectional study design was performed from April 26th, 2021, to June 3rd, 2021. Convenience sampling was used to select respondents; face validity was performed to the mandatory multiple-choice items questionnaire to cover the respondent’s demographic characteristics, coronavirus-19 related anamneses, and the side effect duration of coronavirus-19 vaccines, the data were analyzed by using descriptive statistics.
Results: The 588 participants enrolled in the current study. ChAdOx1 nCoV-19 vaccine received 49.7%, followed by BNT163b2 mRNA COVID-19 vaccine and BBIBP-CorV (39.5% and 10.9%). The most common complaint was headache (61.2%), followed by vaccine injection site discomfort (58.8%), fatigue (49.7%), fever (48.3%), muscle discomfort (42.9%), and approximately (10.5% and 10.2%) had injection site swelling and nausea, respectively. Most of those surveyed had post-vaccine symptoms for one to two days (25.2%), (41%), and only a small percentage (3.7%) experienced them for over one month. ChAdOx1 nCoV-19 vaccine handled 53% of the side effects, followed by BNT163b2 mRNA COVID-19 vaccine (42%) and BBIBP-CorV vaccines (5%).
Conclusion: Prevalence of various local and systemic vaccines side effects, such as headache, fever, and pain at the injection site, was observed. Almost all participants had mild symptoms and were well-tolerated .AstraZeneca® vaccine has the most side effects, followed by the Pfizer® vaccine, and the Sinopharm® vaccine has the least. More independent studies on vaccination safety and public awareness are critical to improving public trust in vaccines.
Keywords: COVID-19; Vaccines; Side effects; Prevalence; Cross-sectional design.
INTRODUCTION
Millions of people around the world were infected by the Coronavirus Disease-2019 (COVID-19) within three months, until World Health Organization declared it as a pandemic on March 11, 2020 [1]. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is a coronavirus that belongs to the Coronaviridae family's Sarbecovirus subgenus, and a non-segmented positive-sense Ribonucleic acid (RNA) virus encompasses it [2]. Older individuals are at an increased risk of being infected with the SARS-CoV-2 [3]. Most vaccine options target the spike (S) protein. It is the principal target of neutralizing antibodies. It helps to neutralize antibodies to prevent the Angiotensin Converting Enzyme-2 (ACE2) receptor binding motif (RBM) from engaging with the host cell [4, 5]. The vaccine development for COVID-19 prevention has grown into a struggle between viruses and humans, which has made it more complicated, along with the discovery of other related strains. Many platforms are attempting to grow, with Deoxyribonucleic acid (DNA) and RNA-based platform showing the most promise [6]. Several countries have entered the vaccine development battle, hastening the clinical trial phase and attempting to produce an efficient and safe vaccine against COVID-19 [7]. The COVID-19 vaccines have been studied in large, randomized-controlled studies with people of all ages, genders, nationalities, and individuals with known medical disorders. Across all demographics, the vaccines have shown a high level of effectiveness and are safe and efficacious in patients with various underlying diseases [8]. According to a recent national study [9], the side effects of the COVID-19 vaccine were the most common reason for vaccine hesitancy among the population in the United Kingdom (U.K.). This finding was confirmed in the context of COVID-19 vaccinations, as fear of side effects has been cited as the primary reason for healthcare workers and students in Poland refusing to accept the Covid-19 vaccine [10, 11]. Vaccines are not completely free of side effects or complications [26], headache, nausea, pain, redness, and swelling are early adverse effects of vaccines that must be expected when taking vaccines [27]. Furthermore, conditions like blood clotting were suggested to be caused by the administration of COVID-19 vaccines from Pfizer, Moderna, and AstraZeneca. [28,29].The present study aimed to determine the prevalence of side effects of the COVID-19 vaccine among vaccinated people in the Kurdistan Region, Iraq.
MATERIALS AND METHODS
Study design
The study was conducted using a cross-sectional design from April 26th to June 3rd, 2021, in the Kurdistan region, Iraq.
Samples and sampling
An Internet-based study in the Kurdistan region of Iraq recruited to enroll a sample size of 588 people from people who had been vaccinated with one of the following vaccines: BBIBP-CorV, ChAdOx1 nCoV-19 vaccine, and BNT163b2 mRNA COVID-19 vaccines. However, illiterate and old age individuals were interviewed directly by authors to increase the sample representation. The individuals were invited by using invitation links in Viber™, Facebook™, and WhatsApp™ groups by using a non-random convenience sampling method. A Google™ form document was utilized to host and deliver the questions to responders. The inclusion criteria were participants who received one of the three mentioned COVID-19 vaccines and either received the first or second dose of the vaccine.
Instruments of the study
The self-administered questionnaire of the present study, composed of nine mandatory multiple-choice items, has been adapted from previous studies and World Health Organization data [12, 13]. The questionnaire was divided into four parts: the first part included demographic data, including gender, age, and profession; the second part dealt with COVID-19 history, including COVID-19 previous infection, type and dose of COVID-9 vaccines, and medical history like having any chronic disease; the third part included the side effects and side effect duration of COVID-19 vaccines.
Statistical analysis
The descriptive statistics were performed to determine the study variables; age, gender, occupation, and the data that related to the COVID-19 vaccine. The current study used SPSS version 23 for the descriptive statistics.
RESULTS
588 participants in the study. Nearly two-thirds of participants were males (64.3%); their mean age was 41.5 years and ranged between 18 and 65 years. Most of the participants were healthcare workers (31.3%), government employees (25.2%), jobless (19), students (18), and self-employed (6.5%), as shown in Table 1.
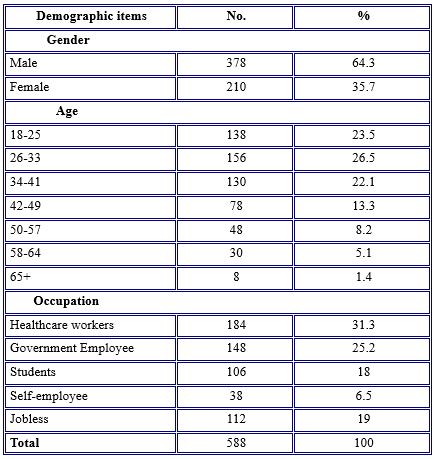
Table 1. Demographic Characteristics of study participants
According to some questions stated in Table 2, nearly half (46.3%) of the participants did not infect before taking the vaccine. About (40.8%) reported that they were infected with COVID-19 previously. Compared with a tiny percentage (12.9%) having the vaccine without knowing whether they were infected with the COVID-19 virus or not.
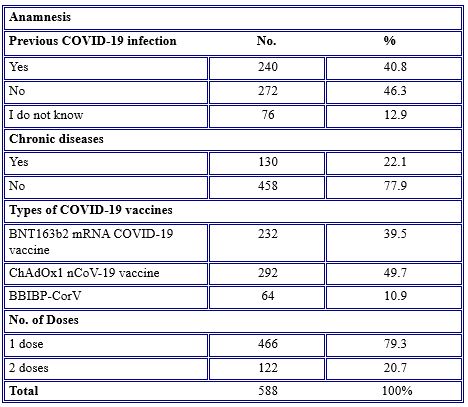
Table 2. COVID-19 vaccines related anamnesis
Regarding chronic diseases among the participants who had the COVID-19 vaccine, over three-quarters (77.9%) had no chronic diseases. The most common types of vaccines received by the participants were ChAdOx1 nCoV-19 vaccine (49.7%), followed by BNT163b2 mRNA COVID-19 vaccine and BBIBP-CorV (39.5% and 10.9%). Regarding the number of vaccine doses gained, over three-quarters (79.3%) of participants had a single dose of vaccine at the time of the study.
Regarding the response of the participants toward COVID-19 side effects, they reported having at least one side effect after the COVID-19 vaccine job. The most common side effects among the study population (61.2%) were headaches, followed by vaccine injection site pain (58.8%), fatigue (49.7%), fever (48.3%), muscle pain (42.9%), and nearly the same percentage (10.5% and 10.2%) complained of injection site swelling and nausea, respectively. Rarely (0.3% and 0.7%) reported mouth ulcers and tonsillitis, side effects of the vaccine, as noted in Table 3.
Table 3. Prevalence of COVID-19 vaccine side effects among study participants
Table 4 shows that, for the duration of the occurrence of side effects, the vast majority (41.5%) of the participants had post-vaccination side effects for about two days, while 25.2% had them for one day, and 10.9% of the individuals complained about side effects for three days. 3.7% of them had a longer duration of side effects for over one month.
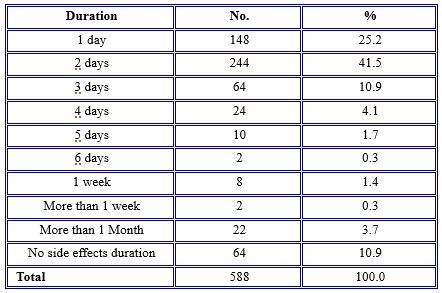
Table 4. The duration of side effects of COVID-19 vaccines
Regarding side effect prevalence with different age groups, symptoms were more common among the younger age groups ranging from 18 to 57 years old. Symptoms were much less severe in older age groups (58–64), with no noticeable side effects observed in participants older than 60 years old. Headache was more common in the age group 34-41 years old (14.2%); injection site pain was more common in the age group 26-33 years old (16.6%); fatigue was more common in the age group 34-41 years old (13.2%) as in Table 5.
Concerning the occurrence of side effects among BNT163b2 mRNA COVID-19 vaccine, ChAdOx1 nCoV-19 vaccine, and BBIBP-CorV vaccines, the vast majority (53%) of the side effects were because of ChAdOx1 nCoV-19 vaccine, followed by BNT163b2 mRNA COVID-19 vaccine (42%), BBIBP-CorV vaccines (5%) were safer than BNT163b2 mRNA COVID-19 vaccine and ChAdOx1 nCoV-19 vaccine vaccines in that almost all side effects occurred among vaccinated individuals.
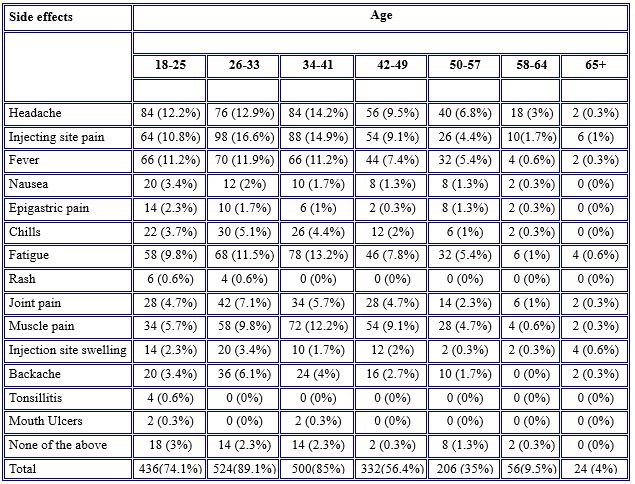
Table 5. Prevalence of the side effects of COVID-19 vaccines among age groups
Some side effects such as nausea, epigastric pain, chills, injection site swelling, backaches, tonsillitis, and mouth ulcers have not occurred at all. Only a few participants (43.7%, 28.1%, 21.9%, and 18.7%, respectively) experienced injection site pain, fatigue, headache, and fever after receiving the BBIBP-CorV vaccine.
Most of the symptoms were observable in those who received the ChAdOx1 nCoV-19 vaccine and BNT163b2 mRNA COVID-19 vaccine vaccines, although symptoms were more common in individuals vaccinated with ChAdOx1 nCoV-19 vaccine. Common side effects between BNT163b2 mRNA COVID-19 vaccine and ChAdOx1 nCoV-19 vaccine were headache (69 % versus 63.7 %), injection site pain (56.8 % versus 63.6 %), fever (42.2 % versus 59.5 %), fatigue (56.8 % versus 48.6%), and muscle pain (44.8 versus 47.9 %) as shown in Table 6.
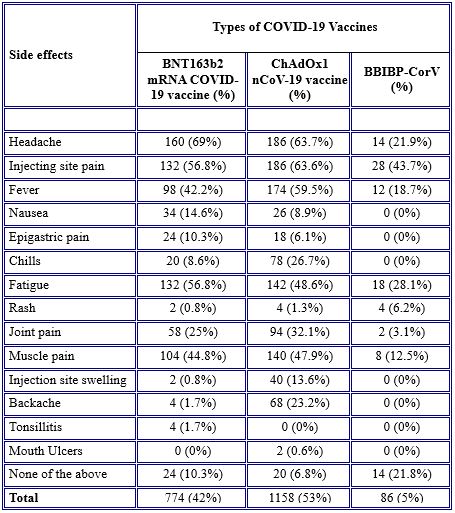
Table 6. Occurrence of side effects between vaccines
DISCUSSION
During the pandemic of COVID-19, the World Health Organization recommended that all nations strive to maintain population immunization. Although legislation and policies in this region are different, they still emphasize people at risk of coronavirus disease, such as healthcare workers, the elderly, and patients with chronic conditions [14]. Thus, the results of the current study showed that most of the participants (31.3%) were healthcare workers (males 64.3%), and most of them (46.3%) did not affect COVID-19. A similar study was conducted in India, which stated that, according to government regulations, the vaccine was initially administered to healthcare personnel in both government and private hospitals throughout India [15]. Correspondingly, in the US, priority is given mainly to all healthcare workers, then individuals who have an underlying condition, and after that to all essential service workers and older adults [16].
Because of the speed of COVID-19 vaccine manufacturing, concerns among the public have emerged about the safety of these new vaccines. No serious safety problems were reported [17]. Overall, COVID-19 vaccines are safe and will protect the community from developing severe COVID-19 disease and dying from COVID-19. BNT163b2 mRNA COVID-19 vaccine is an mRNA-based vaccine, ChAdOx1 nCoV-19 vaccine is an Adenovirus vaccine, and BBIBP-CorV is a vaccine [18]. According to the research, COVID-19 vaccination adverse effects are characterized as either local or systemic reactions, with severity ranging from mild to moderate [19]. The mRNA-based vaccines such as BNT163b2 mRNA COVID-19 vaccine have the highest level of side effects reported, except for diarrhea and arthralgia [20]. Since some of the vaccinated individuals in the current study received the mRNA-based vaccines, they were not free from side effects. No serious events associated with the COVID-19 vaccines, such as vaccine-induced immune thrombotic thrombocytopenia reported. However, most of the side effects were common and non-life-threatening. The side effects were systematic and local. The systemic reactions were headache (61.2%), fatigue (49.7%), fever (48.3%), muscle pain (42.9%), joint pain (26.2%), backache (18.4%), chills (16.7%), nausea (10.2%), epigastric pain (7.1%), and rash (1.7%), whereas the local reactions were injection site pain and injection site swelling (50.8%) and (10.5%), respectively. The rarest side effects were tonsillitis (0.7%) and mouth ulcers (0.3%). These findings are in line with those reported in the literature and reported by the Food and Drug Administration (FDA), which are: injection site pain, fatigue, headache, fever, chills, muscle pain, and joint pain are common side effects of COVID-19 vaccines [21, 15]. Similar findings were observed in the Czech Republic where the most common side effects among vaccinated individuals were injection site pain, fatigue, headache, muscle pain, and feeling unwell [12]. Also, a retrospective cross-sectional study was conducted among Saudi residents to study the side effects of the BNT163b2 mRNA COVID-19 vaccine. The study found that the most common symptoms were injection site pain, fever, headaches, flu-like symptoms, and tiredness. Less common side effects were tachycardia, generalized body aches, shortness of breath, joint pain, chills, and drowsiness. Rare side effects were tenderness, lymph node swelling, and Bell’s palsy [22]. In contrast to our study, in a systematic review study, the most common side effects were arthralgia (20). Mild to moderate side effects are experienced by vaccinated individuals. They are signs that the immune system of the body is responding to the vaccine and building protection against the COVID-19 virus (23/24). Also, in the present study, we found that the duration of post-vaccination side effects varied among participants. The majority (41.5%) were complaining about the side effects for two days, whereas 25.2% had side effects for one day, and 10% for three days. Only 3.7% had long-duration side effects for over one month. These findings follow the current studies which state that most of the side effects occur within the next 3 days after vaccination [15]. Also, similar findings were reported by Riad et al., [12]. They found that the duration of general side effects following the vaccine was mainly one day (45.1%) or three days (35.8%), and only 1.4% of them had lasted over a month.
Also, it is important to highlight that the prevalence of side effects was higher among younger individuals (> 49 years old) and almost no noticeable side effects occurred among older participants (60 years old). These findings are consistent with those published by the FDA, which found that injection site pain, weariness, headache, and muscle soreness were more common in the 55-year-old group than in the > 55-year-old group [21, 15]. Also, the same findings reported among the Czech Republic and Saudi residents, respectively [12], reported that younger adults 43 years old were more frequently affected by side effects, and [22] concluded that the frequency of side effects was higher in individuals younger than 60 years of age, except for injection site pain, which was more frequent among those 60 years old.
Concerning the comparison of the occurrence of side effects between BNT163b2 mRNA COVID-19 vaccine, ChAdOx1 nCoV-19 vaccine, and BBIBP-CorV vaccines, the findings of the present study revealed that there were substantial variations between these vaccines in the presence of side effects. The majority (53%) of side effects were because of ChAdOx1 nCoV-19 vaccine, followed by BNT163b2 mRNA COVID-19 vaccine (42%) except for headache, nausea, epigastric pain, fatigue, and tonsillitis which were more sever in BNT163b2 mRNA COVID-19 vaccine than ChAdOx1 nCoV-19 vaccine. The current study found BBIBP-CorV vaccine was safer than BNT163b2 mRNA COVID-19 vaccine and ChAdOx1 nCoV-19 vaccine vaccines in all side effects that occurred among vaccinated individuals. This finding is supported by a systematic review and meta-analysis of randomized control trials (RCTs), which revealed that those who received mRNA-based vaccines had higher rates of side effects in reactogenicity [20]. The same findings were documented in Jordan. 2213 individuals received BBIBP-CorV, ChAdOx1 nCoV-19 vaccine, BNT163b2 mRNA COVID-19 vaccine, and other vaccines. They found that those who received the ChAdOx1 nCoV-19 vaccine reported the most abundant post-vaccination symptoms, while most of those who received the BBIBP-CorV vaccine were free from symptoms [23]. Another study was conducted to assess the symptoms following the COVID-19 vaccine among residents in India. 5396 people responded to the survey. The findings revealed that the frequency of experiencing symptoms following the BBIBP-CorV vaccine was less (24.4%) compared to BNT163b2 mRNA COVID-19 vaccine 70.7% [25]. As seen, the BBIBP-CorV vaccine has few side effects compared to other vaccines.
CONCLUSIONS
The most common side effect of the BNT163b2 mRNA COVID-19 vaccine, ChAdOx1 nCoV-19 vaccine, and BBIBP-CorV among the vaccinated population of the current study was headaches, injection site pain, injecting site swelling, fatigue, fever, muscle pain, joint pain, backache, chills, nausea, epigastric pain, and rash. These side effects were consistent with the data reported in the literature. Most of these side effects were mild, and no serious incidents were documented. Symptoms were more common in younger people. Although data reported in the literature showed that mRNA-based vaccines such as BNT163b2 mRNA COVID-19 vaccine had higher side effects, However, the current study found that the ChAdOx1 nCoV-19 vaccine, which is an adenovirus-based vaccine, had more side effects than other vaccines, and the BBIBP-CorV vaccine had the lowest side effects compared to the ChAdOx1 nCoV-19 vaccine and BNT163b2 mRNA COVID-19 vaccine vaccines.
Limitations
The limitation of the current study is that it was difficult to measure the severity of the side effects because the study is a survey-based technique. Thus some side effects needed to be measured by using instruments or tools, for instance, measuring body temperature by the thermometer to know the severity of fever, and using a pain scale to measure headache, joint pain, and muscle pain. Also it is prone to selective bias as it is internet based study, not everyone has equal chance to be included in the study. Further studies needs to be done with more representative samples concerning COVID-19 intention.
Conflict of interest
The authors have no conflict of interest to declare.
Funding
The current study was not funded by any financial resources.
Ethics
The present study was carried out in accordance with the Helsinki Declaration”. Study approval was obtained by written authorization of the Ethics Committee of the College of Nursing at Duhok University. The approval is without a serial number and verbal informed consent has been obtained from each participant before participation in the current study.
Acknowledgments
We would like to extend our appreciation to all respondents who took part in this online survey. We highly appreciated their time and effort.
REFERENCES
- World Health Organization. Novel Coronavirus (2019-nCoV) SITUATION REPORT - https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200121-sitrep-1-2019-ncov.pdf. .
- Zhuo Zhou , Lili Ren , Li Zhang , Jiaxin Zhong , Yan Xiao , Zhilong Jia et alHeightened innate immune responses in the respiratory tract of COVID-19 patients. Cell Host Microbe .2020; 27, 883-890.e2.
- Centers for Disease Control and Prevention. COVID-19 information page (https://www.cdc.gov/coronavirus/2019 -ncov/index.html).
- Addetia A, Crawford KHD, Dingens A, Zhu H, Roychoudhury P, Huang ML, Jerome KR, Bloom JD, Greninger AL. Neutralizing Antibodies Correlate with Protection from SARS-CoV-2 in Humans during a Fishery Vessel Outbreak with a High Attack Rate. J Clin Microbiol. 2020 Oct 21;58(11):e02107-20. doi: 10.1128/JCM.02107-20. PMID: 32826322; PMCID: PMC7587101.
- Thompson, C. P., Grayson, N. E., Paton, R. S., Bolton, J. S., Lourenço, J., Penman, B. S., Lee, L. N., Odon, V., Mongkolsapaya, J., Chinnakannan, S., Dejnirattisai, W., Edmans, M., Fyfe, A., Imlach, C., Kooblall, K., Lim, N., Liu, C., López-Camacho, C., McInally, C., ... Girvan, M.. Detection of neutralising antibodies to SARS-CoV-2 to determine population exposure in Scottish blood donors between March and May 2020. Eurosurveillance, 25(42). https://doi.org/10.2807/1560-7917.ES.2020.25.42.2000685
- Lurie N, Saville M, Hatchett R, Halton J. Developing Covid-19 vaccines at pandemic speed. New England Journal of Medicine..2020; 21;382(21):1969-73.
- Caddy S. Developing a vaccine for covid-19. BMJ 2020;369:m1790 doi: 10.1136/bmj.m1790
- World Health Organization. . Safety of covid-19 vaccines. https://www.who.int/news-room/feature-stories/detail/safety-of-covid-19-vaccines.2020.
- Luyten, J.; Bruyneel, L.; van Hoek, A.J. Assessing vaccine hesitancy in the UK population using a generalized vaccine hesitancy survey instrument. 2019;37, 2494–2501. [CrossRef] [PubMed] .
- Szmyd, B.; Bartoszek, A.; Karuga, F.F.; Staniecka, K.; Błaszczyk, M.; Radek, M. Medical Students and SARS-CoV-2 Vaccination: Attitude and Behaviors. 2021; 9, 128. [CrossRef].
- Szmyd, B.; Karuga, F.F.; Bartoszek, A.; Staniecka, K.; Siwecka, N.; Bartoszek, A.; Błaszczyk, M.; Radek, M. Attitude and Behaviors towards SARS-CoV-2 Vaccination among Healthcare Workers: A Cross-Sectional Study from Poland. Vaccines 2021, 9, 218. https://doi.org/10.3390/vaccines9030218
- Riad, A.; Pokorná, A.; Attia, S.; Klugarová, J.; Košˇcík, M.; Klugar, M.Prevalence of COVID-19 Vaccine Side Effects among HealthcareWorkers in the Czech Republic. Clin. Med., 10, 1428. https://doi.org/ .2021;10.3390/jcm10071428.
- World Health Organization. . Side Effects of COVID-19 Vaccines. https://www.who.int/news-room/feature-stories/detail/side-effects-of-covid-19-vaccines.2021
- World Health Organization. Guidance on routine immunization services during COVID-19 pandemic in the WHO European region: World Health Organization. Regional Office for Europe.2020.
- Das, L., Meghana, A., Paul, P., & Ghosh, S. Are We Ready For Covid–19 Vaccines?–A General Side Effects Overview. Journal of Current Medical Research and Opinion.2021; 4(02).
- Barnabas, R. V., & Wald, A. A public health COVID-19 vaccination strategy to maximize the health gains for every single vaccine dose: American College of Physicians.2021.
- Gee, J. First month of COVID-19 vaccine safety monitoring—United States, December 14, 2020–January 13, 2021. Morbidity and mortality weekly report. 2021; 70.
- Wise, J. Covid-19: European countries suspend use of Oxford-AstraZeneca vaccine after reports of blood clots: British Medical Journal Publishing Group.2021.
- Oliver, S.E.; Gargano, J.W.; Marin, M.; Wallace, M.; Curran, K.G.; Chamberland, M.; McClung, N.; Campos-Outcalt, D.; Morgan, R.L.; Mbaeyi, S. The Advisory Committee on Immunization Practices’ Interim Recommendation for Use of Moderna COVID-19 Vaccine-United States, December 2020. Morb. Mortal. Wkly. Rep.2021, 5152, 1653–1656. [Google Scholar] [CrossRef]
- Pormohammad A, Zarei M, Ghorbani S, Mohammadi M, Razizadeh MH, Turner DL, Turner RJ. Efficacy and Safety of COVID-19 Vaccines: A Systematic Review and Meta-Analysis of Randomized Clinical Trials. 2021; 9(5):467. https://doi.org/10.3390/vaccines9050467.
- Centres for Diseases Control and Prevention. Local Reactions, Systemic Reactions, Adverse Events, and Serious Adverse Events: Pfizer-BioNTech COVID-19 Vaccine. Retrieved 5 June, from https://cdc.gov/vaccines/covid-19/info-by-product/pfizer/reactogenicity.html.2021.
- El-Shitany, N. A., Harakeh, S., Badr-Eldin, S. M., Bagher, A. M., Eid, B., Almukadi, H., Sindi, N. Minor to Moderate Side Effects of Pfizer-BioNTech COVID-19 Vaccine Among Saudi Residents: A Retrospective Cross-Sectional Study. International journal of general medicine.2021;14, 1389.
- Hatmal MM, Al-Hatamleh MAI, Olaimat AN, Hatmal M, Alhaj-Qasem DM, Olaimat TM, Mohamud R. Side Effects and Perceptions Following COVID-19 Vaccination in Jordan: A Randomized, Cross-Sectional Study Implementing Machine Learning for Predicting Severity of Side Effects. 2021; 9(6):556. https://doi.org/10.3390/vaccines9060556
- World Health Organization. Side Effects of COVID-19 Vaccines. Retrieved 4 June, 2021, from https://who.int/news-room/feature-stories/detail/side-effects-of-covid-19-vaccines.2021
- Jayadevan, R., Shenoy, R. S., & Anithadevi, T. Survey of symptoms following COVID-19 vaccination in India. medRxiv.2021.
- Kimmel SR. Vaccine adverse events: separating myth from reality. Am Fam Physician. 2002;66(11):2113–20.
- Center for Disease Control and Prevention. Reactions and adverse events of the pfizer-BioNTech COVID-19 vaccine | CDC [Internet]. Centers Dis Control Prev. 2020 [accessed 2021 May 30]. https://www.cdc.gov/vaccines/covid-19/info-by-product/pfi zer/reactogenicity.html
- Lee E, Cines DB, Gernsheimer T, Kessler C, Michel M, Tarantino MD, Semple JW, Arnold DM, Godeau B, Lambert MP, et al. Thrombocytopenia following Pfizer and moderna SARS-CoV-2 vaccination. Am J Hematol. [Internet]. 2021 [accessed. 2021 Aug 31];96:534–37. /pmc/articles/PMC8014568/ .
- European Medicines Agency. AstraZeneca’s COVID-19 vaccine: EMA finds possible link to very rare cases of unusual blood clots with low blood platelets [Internet]; 2020 [accessed 2021 May 30].
The questionnaire
(COVID-19 Vaccines Side Effects Among Iraqi people In Kurdistan Region)
Dears the aim of this survey is to determine the (Prevalence of Covid-19 Vaccines side effects). We are grateful for filling in this survey from you and your family who got vaccinated. I would like to assure you that your answers will remain confidential and your personal details are not required. Also, your answers will be on online systems only.
- Age
18_25
26_33
34_41
42_49
50_57
57_64
65 and more
- Gender
Male
Female
- Occupation
Health care workers
Employee Government
Student
Own Job
Jobless
- Do you have any chronic disease?
Yes
No
- Did you infected with Covid-19 before?
Yes
No
I don't know
- Which Covid-19 Vaccine you took it?
Sinopharm
Astrazenea
Pfizer
- How many Doses you got it?
1 dose
2 doses
- Select the vaccine side effects that occurred with you
Headache
Vaccine injection site pain
Fever
Nausea
Epigastric pain
Chills
Joint pain
Muscles pain
Fatigue
Injection site swelling
Allergy
Backache
Tonalities
Mouth Ulcers
No one
- Duration of side effects of Covid-19 Vaccines
1 day
2 days
3 days
4 days
5 days
6 days
1 week
More than 1 week
More than 1 month
No duration
![]() This work is licensed under a Creative Commons
This work is licensed under a Creative Commons
Attribution-NonCommercial-NoDerivatives 4.0 International License.
Analysis of Determinants of Factors Related to the Performance of Non-Communicable Diseases Development Post Cadres in Kendari City: Cross Sectional Study
Saida, Rahmawati*, Wa Ode Syahrani Hajri
Department of Nursing, Medical of Faculty, Halu Oleo of University, Kendari, Indonesia
* Corresponding author: Rahmawati, Kampus Hijau Bumi Tridharma, Anduonohu, Kec. Kambu, Kota Kendari, Sulawesi Tenggara 93232, Indonesia, Orcid : https://orcid.org/0000-0002-6826-5393. Email: saida@uho.ac.id
Cita questo articolo
Abstract
Introduction: Non-communicable diseases (NCDs) are diseases that are not caused by bacterial infection and are the main cause of death in the world. The increase in NCDs cases also occurred in Southeast Sulawesi Province (Indonesia), including Kendari City. The purpose of this study was to analyze the determinants of proxies related to the performance of Integrated Non-Communicable Diseases Development Post (INCDDP) cadres in Kendari City, Indonesia.
Materials and Methods: A cross-sectional study carried out in Kendari City, Southeast Sulawesi Province (Indonesia), with a population of all INCDDP cadres in the working area of PHC Abeli, Lepo-Lepo, and Perumnas. The sample consisted of 56 responders. Data were analyzed univariate and bivariate statistics, using the chi-square test. Multivariate using logistic regression.
Results: The results of the research on the performance of INCDDP cadres were awards (p = 0.079), cadre training history (p = 0.031), infrastructure (p = 1.0) and knowledge (p = 0.007). The factor most related to the performance of INCDDP cadres was cadre knowledge (p = 0.019) with the coefficient of determination (R2) = 27.4%.
Conclusion: Cadre performance is related to awards, cadre training history, infrastructure and cadre knowledge. The most related factor to INCDDP cadre performance is cadre knowledge.
Keywords: Health-Cadres, Non-Commnicable Diseases, Performance, Health Services
Introduction
Non-communicable diseases (NCDs) have become an enormous public health problem, especially in Indonesia [1]. It is marked by a shift in disease patterns which is often referred to as an epidemiological transition characterized by increased mortality and morbidity due to NCDs such as stroke, heart disease and diabetes mellitus [2].
NCDs account for 41 million deaths each year, equivalent to 71% of all deaths globally [3]. The 2018 Basic Health Research (BHR) results show an increase in the prevalence of NCDs compared to the 2013 BHR results [4]. NCDs cases in Southeast Sulawesi in 2018 were still relatively high [4,5]. In 2019, the number of hypertension sufferers in Kendari city was 13,807 cases, and DM patients were 2876 cases [6].
The high number of NCDs cases in Kendari City requires severe treatment by increasing the Public Health Center (PHC) role through the Integrated Non-Communicable Diseases Development Post (INCDDP), significantly expanding the part of cadres in the context of preventing and controlling NCDs. INCDDP is a form of community participation in activities for early detection, monitoring, and early follow-up of NCDs risk factors independently [7], routinely, integrated, and continuously [8]. The high number of PTM cases in Kendari City (Indonesia) requires serious handling by increasing the role of the Puskesmas through the Integrated Non-Communicable Disease Development Post (INCDDP), significantly expanding the role of cadres in the context of preventing and controlling PTM. INCDDP is a form of community participation in activities for early detection, monitoring, and early follow-up of PTM risk factors independently [7], routinely, integrated, and continuously [8].
In improving the skills of cadres, it is necessary to support the development of health workers, especially community nurses [9]. One of the intervention strategies that can be applied as community nurses as educators or educators is to provide health education to high-risk community groups and health cadres and change public health behavior. Following this research, nurses are expected to be able to empower cadres by increasing the knowledge and skills of cadres as mover in the community. One of the ways to increase knowledge and skills is through community-based education programs. This is intended to improve the quality of cadres in providing counseling and management to patients and families of NCDs patients, as well as the community [10–12].
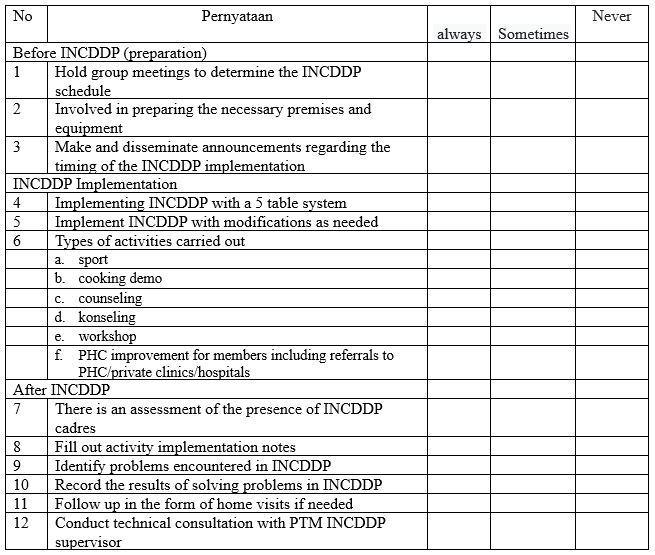
The role of INCDDP cadres is as an implementer of NCDs risk factor control for the surrounding community. The functions of cadres are as coordinator of INCDDP implementation, community mobilizer to participate in INCDDP, monitoring of measurement of NCDs risk factors, counsellor for INCDDP participants, recorder of results of INCDDP activities [13].
There are still many problems in service at INCDDP related to the capacity of cadres. In theory, three factors affect a person's performance: individual elements consisting of abilities and expertise, background, and demographics. The second is psychological factors consisting of perceptions, attitudes, learning and motivation. The last is organizational factors, namely resources, leadership, rewards, structure and job design. These three factors can be classified into intrinsic factors, while extrinsic factors include political, economic and social factors [14].
The results of previous studies stated a relationship between cadre performance with attitudes, motivation, rewards, job design, and there was no relationship between HR and the role of stakeholders [15]. It is in line with other research states that the support of health cadres and family support by using INCDDP in the Ballaparang working area of Makassar City [16]. Kendari City has 15 PHCs, 13 of which have INCDDP. INCDDP cadres have a very big role in the prevention and early detection of risk factors for NCDs in the community [6].
The purpose of this study was to analyze the factors related to the performance of INCDDP cadres in Kendari City (Indonesia).
Materials and Methods
Trial design
This type of research is an observational analytic with a cross-sectional design to analyze the determinants of the proxy factors related to the performance of INCDDP cadres in Kendari City (Indonesia).
Participants
This research was carried out in October 2021 at 3 (three) Puskesmas in Kendari City (Indonesia) consisting of Abeli, Lepo-Lepo, and Perumnas Health Centers involving 56 INCDDP cadres with criteria including cadres who were present at the time of the study, cadres with active status participating in Integrated Non-Communicable Diseases Development Post (INCDDP) activities, while the inactive Cadres are expelled.
Intervention
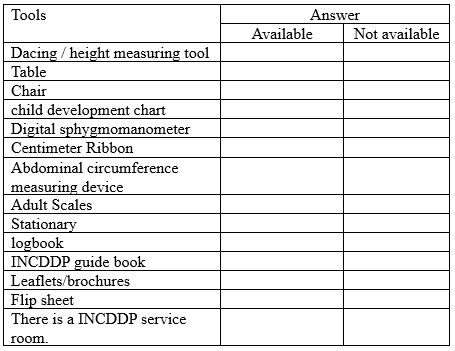
The dependent variable in this study is the performance of cadres with the objective criteria of "good" and "bad". While the independent variables are cadre training, infrastructure, knowledge, awards with "good" and "less" objective criteria. Collecting data on cadre performance variables using a questionnaire, and cadre training variables, infrastructure, knowledge, awards, also using questionnaires. on each variable, consisting of 10 questions with an alternative scoring as follows: if the respondent answers yes then it is given a score of 1 and if the respondent answers no it is given a score of zero. All questionnaires in this study used previous research questionnaires that had been tested for validity and reliability. The questionnaire received an award from the Kiting PR research. et al, [15], questionnaire of knowledge, training and infrastructure adoption from Handayani RO. et al, research [17].
Outcomes
Knowing the performance of cadres, training history, rewards, infrastructure, and knowledge.
Sample size
The number of participants in this study was 56 people. The age of the sample in this study was between 26-67 years, all of whom were female because all Integrated Non-Communicable Diseases Development Post (INCDDP) cadres were female. The sampling method in this study was total sampling because the number of Integrated Non-Communicable Diseases Development Post (INCDDP) candidates was very small.
Statistical analysis
Data are presented as numbers and percentages for categorical variables. Continuous data were expressed as mean ± standard deviation (SD) or median with Interquartile Range (IQR). The bivariate analysis uses the chi-square test, and multivariate uses logistic regression. Logistic regression test is used because the data scale used is categorical or binomial. in the multivariate test, there is R2 or R square also referred to as the coefficient of determination which explains how far the dependent data can be explained by independent data. All tests with p-value (p)<0.05 were considered significant. Statistical analysis was performed using the SPSS version 16.0 application.
Ethical Consideration
No economic incentives were offered or provided for participation in this study. The study was performed in accordance with the ethical considerations of the Helsinki Declaration. This study obtained ethical feasibility under the Health Research Ethics Committee of the College of Medicine, Halu Oleo University, number: 183/UN29.17.1.3/ETIK/2021.
Result
The distribution of the characteristics of the results of this study is showed in Table 1:
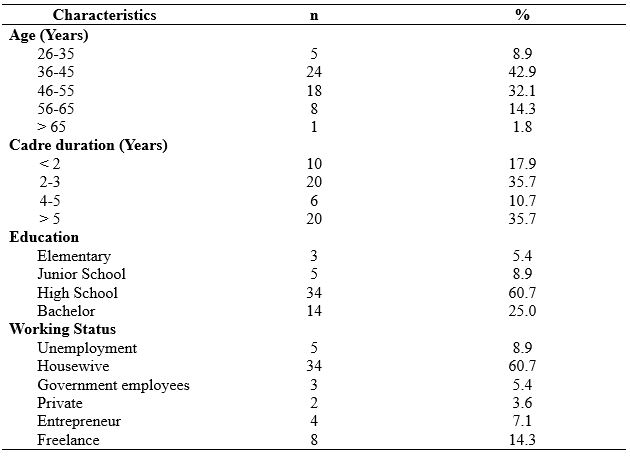
Table 1. Frequency Distribution Based on Characteristics of Respondents
Table 1 shows the frequency distribution of 56 respondents based on age characteristics, primarily aged 36-45 years as many as 24 (42.9%), the highest length of being a cadre is 2-3 years, and > 5 years each is 20 (35.7%), the highest level of education is high school graduates as many as 34 (60.7%). The most elevated employment status is as a housewife as much as 34 (60.7%).
The distribution of research variables is presented in table 2. Table 2 shows the frequency, distribution by knowledge, perception of vulnerability, and compliance, there were 29 cadres (52.8%) who performed well, 26 cadres (46.4%) had attended training, 45 cadres (80.4%) stated that they had received awards, there were 48 cadres (85.7%) who indicated that infrastructure facilities were not available. Meet the minimum requirements, and 36 cadres (64.3%) have good knowledge.
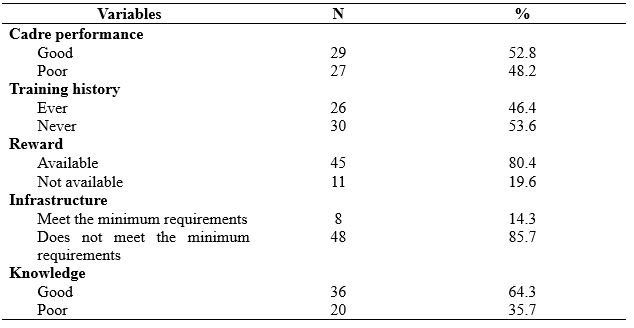
Table 2. Frequency Distribution by Knowledge, perception of vulnerability, and compliance
The distribution of the relationship between research variables can be presented in the following table 3:
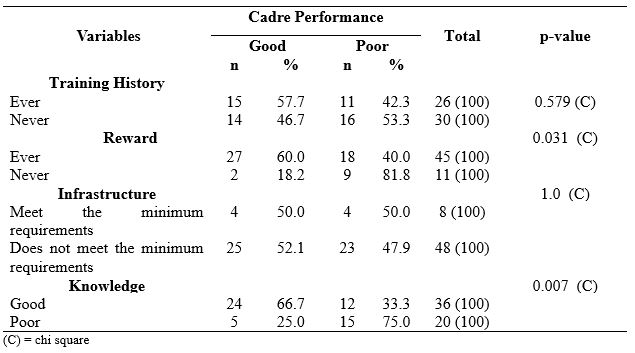
Table 3. Relationship between variables
Table 3 shows that of the 26 respondents who have a good training history, there are 15 cadres (57.7%) who perform well and 11 cadres (42.3%) who perform poorly, then from 30 respondents who have a history of lack of training, there are 16 cadres (53.3%). Underperforming and 14 cadres (46.7%) performed well. The chi-square test showed a p = 0.579, indicating no significant relationship between training history and the performance of INCDDP cadres.
Forty-five respondents assessed the availability of the award, as many as 27 cadres (60.0%) with good performance and 18 cadres (40.0%) with less performance. Then from 11 respondents who assessed that the award did not exist, nine cadres (81.8%) with poor performance and two cadres (18.2%) performed well. The chi-square test shows the p = 0.031, indicating a significant relationship between rewards and the implementation of INCDDP cadres.
Eight respondents assessed the minimum requirements of infrastructure, four cadres (50.0%) with good performance and four cadres (50.0%) with poor performance. Of the 48 respondents who assessed that the infrastructure did not meet the minimum requirements, 23 cadres (47.9%) underperforming and 25 cadres (52.1%) performed well. The chi-square test shows that the p = 1.0 indicates no significant relationship between infrastructure and the performance of INCDDP cadres.
Of the 36 respondents who have good knowledge, there are 24 cadres (66.7%) with good performance and 24 cadres (33.3%) with poor performance; then from 20 respondents who have less knowledge, there are 15 cadres (75.0%) with poor performance and five cadres (25.0 %) perform well. The chi-square test showed a p = 0.007, indicating a significant relationship between knowledge and performance of INCDDP cadres.
Multivariate data analysis using logistic regression test is presented in table 4.
The results of the multivariate analysis showed that the Wald value of the knowledge variable was the largest with a significant value (p = 0.090).
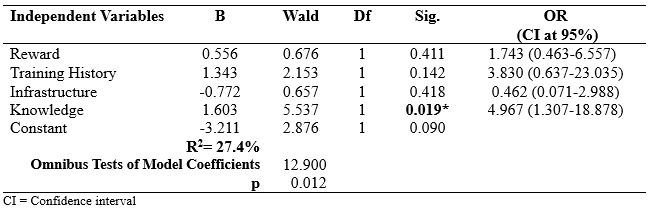
Table 4. Multivariate Analysis of INCDDP Cadre Performance
The value of R2 = 27.4% indicates that this model can explain the effect variable (INCDDP cadre performance) of 27.4%, while 72.6% is influenced by other variables not examined.
The value of chi square = 12,900 with sig. 0.012 in Degree of Feedom 4 the value of chi square table = 9.49. it can be seen that the p value < 0.05, so it can be ascertained that the addition of the independent variable has a real effect on the model, in other words other models are declared FIT
Discussion
1.Reward
The purpose of this study was to analyze the factors related to the performance of INCDDP cadres in Kendari City (Indonesia). The existence of cadres should receive fair and sincere recognition and appreciation [18]. Recognition of the existence of cadres from cadre coaches in the sub-district needs to be realized by prioritizing free health services and the presence of cadre uniforms [19]. The hierarchy of human needs starts from primary needs (physiological needs and safety needs) to be dominant until these needs are felt to be sufficiently fulfilled [20].
Appreciation for the work done is a desire from selfish needs, manifested in praise, gifts (in the form of money or not), announced to his co-workers [21]. Therefore, giving awards for cadre loyalty will be very helpful to maintain the activeness of Posbindu cadres; giving tasks that are not boring with praise, completing attributes while on duty will increase cadre performance [22].
In this study, it was found that of the overall respondents, more than half had received awards from the government through the Puskesmas or the Kendari city health office. Indeed, this greatly influenced the motivation of Posbindu cadres in working. It is statistically proven that cadres who have a history of receiving awards tend to perform well and vice versa.
It is stated that usually, a person will feel mistreated if the treatment is seen as a dangerous thing. In working life, this perception is associated with various things, namely incentives and the number of hours worked [23]. The provision of incentives is a basic payment to motivate employees to be more advanced in work with more excellent skills and responsibilities [24]. Incentives are one type of award that is associated with work performance [25].
The award should be given to human resources, in this case, Posbindu PTM cadres who perform well to increase the spirit of work. Other cadres will see and will encourage other cadres to work better so that performance improves. Therefore, the performance of PTM Posbindu cadres will significantly increase if awards are given to their human resources.
In line with the findings of Renate Pah Kiting [15] stated that there is a relationship between rewards and performance (p=0.013 OR=10.400). Furthermore, Renate et al. said that cadres who received awards ten times would have the opportunity to have better performance compared to cadres who did not accept awards.
2.Training
The commitment of cadres to the responsibilities and functions of the INCDDP program in the Anambas Islands is quite good. It is evidenced by the continued implementation of the INCDDP program even though it is still constrained by several problems such as limited tools and materials and has never received special training. Therefore, support and commitment from cadres are very vital in the implementation of the INCDDP program. In the results of his research, it is stated by [26] that INCDDP cadres who always consistently run INCDDP with or without training will motivate other cadres to take an active role and try to help active cadres with what has been exemplified.
In this study, only a few respondents had ever been sent to receive training, although some of the cadres who had attended the training section stated that they were not under the assignment field at INCDDP. This condition will undoubtedly affect cadres' performance where when doing work. They do not look professional due to their lack of knowledge.
There is a difference in the proportion of cadres who received training and whose performance was considered "good" compared to cadres whose performance was "good" but did not receive training. The result shows that the more often cadres attend training, the better their performance [27]. Cadre training is carried out to increase the knowledge and skills of cadres. It will be achieved if the training section is carried out correctly. Puspasari A stated that the quality of cadre training is a factor causing cadres' low knowledge and skills level in carrying out their roles and duties. Therefore, training activities should be carried out regularly with a distance that is not too long.
The training should always start with the importance of an INCDDP cadre's goals so that interest and strong desire to make decisions and take action in implementing PTM Posbindu activities arise. It is expected that cadres will work with higher motivation and feel satisfied with their work so that it has a direct impact on increasing performance [28].
3.Infrastructure
Not all of the INCDDP in the working area of the PHC have complete kits; it requires them to use alternate tools at implementation. The Posbindu kit contains tools for checking blood sugar, cholesterol, uric acid, measuring height and then a body fat analyzer. Digital devices have never been calibrated, and this, of course, has fatal consequences in calculating the inspection results. Based on the inspection, the digital sphygmomanometer is broken, which give abnormal results in measurement.
Regarding the damaged digital INCDDP equipment, it is also following the research of Astuti et al. [29] that the number of NCDs INCDDP equipment is damaged/error. These tools include; body fat scale analyzer, measuring blood sugar and measuring total cholesterol. Likewise, research by Pranandari et al. [30] concluded that the infrastructure for the NCDs Posbindu in Banguntapan District, Bantul Regency for examining NCDs risk factors in the form of examination strips was not sufficient. Nova Silviyani's research [31] states that the statistical results obtained a p of 0.05 = (0.05), so it can be noted that there is no significant relationship between infrastructure and Posbindu performance.
In motivating the work, it should provide suitable facilities and infrastructure to carry out tasks. However, as complained by the cadre coach at the Kendari City District level, inadequate facilities and infrastructure such as tables, chairs, scales, stationery and especially the Posbindu place will hinder the performance of Posbindu cadres [32].
Posbindu activities will not be able to run correctly if adequate facilities do not support them. The provision of work facilities is that the work facilities provided must be sufficient and follow the duties and functions. Moreover, it must be implemented and available at the right time and place. Therefore, Posbindu facilities are everything that can support the implementation of Posbindu activities such as a fixed place or location, routine funds for giving additional food (PMT), the necessary tools, for example, kitchenware, KMS, tables, chairs, register books and others [33].
4.Knowledge
Knowledge of health cadres is an essential factor in supporting the ability of cadres to provide services. This study shows that several cadres have a low level of knowledge. There needs to be an effort to increase the knowledge of cadres, where one of the steps that can be taken is to provide health education and training to health cadres [34],[35].
Cadre knowledge is the extent to which cadres understand their duties and roles in INCDDP activities, including preparation before implementation, during implementation and after the implementation of INCDDP for the elderly. Knowledge of health cadres about INCDDP services is obtained from the information they obtain both from official sources, meaning from the health office that fosters them, from informal sources, and activities aimed at increasing cadre knowledge such as training, seminars and so on [36].
It is evident from the results of statistical tests that there is a relationship between knowledge and the performance of Posbindu cadres in the working area of the Puskesmas in Kendari City. Hence, there is a tendency for cadres who have an excellent ability to do their jobs well.
It is in line with research [37] which examines the relationship between knowledge and length of work with the skills of cadres in assessing the growth curve of toddlers at the Posyandu, Tegalsari Village, Candisari District, Semarang City. This study shows that the level of knowledge of cadres about the growth curve of toddlers is primarily adequate, where one of the factors related to this knowledge is the level of education of cadres, most of whom are in high school.
We assume the level of education of cadres varies from elementary school to high school level. This level of schooling dramatically affects the attitude and ability of cadres in capturing information conveyed by officers both when training and visits to INCDDP.
5.Multivariate test results
In Table 4, there is a significant positive correlation between the Performance and Knowledge of INCDDP Cadres (OR=4.987; p=0.019). it can be explained that after going through a simultaneous test between the performance of cadres and all independent variables (knowledge, training, infrastructure, and awards) it was found that only the knowledge of cadres was significant while the other 3 variables were not significant. Knowledge of cadres dominates the motivation of cadres to improve their performance, so even though infrastructure is available, if cadres do not have knowledge of what to do, then cadres' performance tends to be poor.
Implications of research results for nursing and clinical practice is to be valuable information for health service providers, especially community health centers to maximize the performance of nurses in assisting cadres when providing services to the community.
Conclusion
Cadre performance is related to awards, cadre training history, infrastructure and cadre knowledge. The most related factor to INCDDP cadre performance is cadre knowledge.
There is a need to increase advocacy to the legislative body regarding the importance of getting more budget for PHC and the need to improve health funds budgeted through the Regional Revenue and Expenditure Budget (APBD) to support the implementation of services and the need to formulate regulatory policies to tackle financing for cadres immediately. It is necessary to carry out periodic training for cadres, and it is hoped that INCDDP cadres will continue to explore knowledge and experience to improve performance in the implementation of INCDDP activities and always be positive in every action carried out at INCDDP and need to improve and improve facilities and infrastructure to meet basic service needs.
Limitations of Study
The limitations of this study include the very limited number of subjects, and this research only involves one region or 1 region so the results may be different when compared to other regions or regions in Indonesia.
Acknowledgement
We would like to thank the Chairperson of the research institute and community service who have supported this research.
Funding statement
This research did not receive any specific grant from funding agencies in the public, commercial, or not for profit sectors.
Competing interests statement
There are no competing interests for this study.
References
- Kemenkes RI. Rencana Aksi Nasional Penyakit Tidak Menular 2015-2019. Kementerian Kesehatan RI. Jakarta; 2017.
- World Health Organization (WHO). Global status report on noncommunicable diseases. World Health Organization. Italia; 2010. 176 p.
- WHO. Noncommunicable diseases. World Health Organization; 2018.
- Kementerian Kesehatan Republik Indonesia. Riset Kesehatan Dasar. Jakarta: Balitbangkes RI; 2018. Available from: https://kesmas.kemkes.go.id/assets/upload/dir_519d41d8cd98f00/files/Hasil-riskesdas-2018_1274.pdf “Accessed December 21,2021”
- Dinas Kesehatan Provinsi Sulawesi Tenggara. Profil Kesehatan Propinsi Sulawesi Tenggara. Kendari: Bidang P2PL Dinas Kesehatan Prov. Sultra; 2020. Available from: https://farmalkes.kemkes.go.id/ufaqs/dinas-kesehatan-provinsi-sulawesi-tenggara/“Accessed December 28,2021”
- Dinas Kesehatan Kota Kendari. Profil Dinas Kesehatan Kota Kendari. Kendari: Bidang P2PL Dinas Kesehatan Kota Kendari; 2019. Available from: https://siasiksehat.kendarikota.go.id/profil-kesehatan-kota-kendari/“Accessed December 21,2021”
- Dinkes Kabupaten Demak. Kegiatan Posbindu PTM. Demak; 2018. Available from: https://dinkes.demakkab.go.id/download/“Accessed December 21,2021”
- Kemenkes RI. Petunjuk Teknis Pos Pembinaan Terpadu Penyakit Tidak Menular (POSBINDU PTM). In Jakarta: Direktorat Jenderal Pengendalian Penyakit dan Penyehatan Lingkungan Direktorat Pengendalian Penyakit Tidak Menular; 2012.
- Iriarte‐Roteta A, Lopez‐Dicastillo O, Mujika A, Ruiz‐Zaldibar C, Hernantes N, Bermejo‐Martins E, et al. Nurses’ role in health promotion and prevention: A critical interpretive synthesis. Journal of Clinical Nursing. 2020;29(21–22):3937–49.
- Halcomb E, Williams A, Ashley C, McInnes S, Stephen C, Calma K, et al. The support needs of Australian primary health care nurses during the COVID‐19 pandemic. Journal of nursing management. 2020;28(7):1553–60.
- Halcomb E, McInnes S, Williams A, Ashley C, James S, Fernandez R, et al. The experiences of primary healthcare nurses during the COVID‐19 pandemic in Australia. Journal of Nursing Scholarship. 2020;52(5):553–63.
- Blay N, Sousa MS, Rowles M, Murray‐Parahi P. The community nurse in Australia. Who are they? A rapid systematic review. Journal of nursing management. 2021;
- Kementerian Kesehatan RI. Modul Pelatihan Posbindu PTM. Jakarta: Direktorat PPTM, Direktorat Jenderal PP dan PL; 2013.
- Andriani K, Bisri RS MS. Analisis Faktor Faktor Yang Mempengaruhi Kinerja Tenaga Kesehatan Pada Penerapan Program Keluarga Sadar Gizi di Kabupaten Sukoharjo. Manajemen Bisnis Syariah. 2013;1(7).
- Kiting RP, Ilmi B, Arifin S. Faktor Yang Berhubungan Dengan Kinerja Kader Posbindu Penyakit Tidak Menular. Jurnal Berkala Kesehatan. 2017;1(2):106.
- Nasruddin NR. Faktor-faktor yang mempengaruhi pemanfaatan pos pembinaan terpadu penyakit tidak menular (POSBINDU PTM) Di Wilayah Kerja Puskesmas Ballaparang Kota Makassar Tahun 2017. Universitas Islam Negeri Alauddin Makassar; 2017. Available from: http://repositori.uin-alauddin.ac.id/6515/1/NURIZKA RAYHANA_opt.pdf.“Accessed December 28,2021”
- Handayani RO, Suryoputro A, Sriatmi A. Faktor-Faktor Yang Berhubungan Dengan Praktik Kader Dalam Pelaksanaan Posyandu Lansia di Kelurahan Sendangmulyo Kecamatan Tembalang Kota Semarang. Jurnal Kesehatan Masyarakat (Undip). 2018;6(1):81–92.
- Husniyawati YR, Wulandari RD. Analisis motivasi terhadap kinerja kader Posyandu berdasarkan teori Victor Vroom. Jurnal Administrasi Kesehatan Indonesia. 2016;4(2):126–35.
- Bunawar KMS. Hubungan Penghargaan, Tanggung Jawab, Pengawasan, Hubungan Interpersonal terhadap Motivasi Kerja Kader Posyandu di Wilayah Kerja Puskesmas Sungai Bengkal Kabupaten Tebo Tahun 2017. Scientia Journal. 2019;8(1):249–55.
- Tay L, Diener E. Needs and subjective well-being around the world. Journal of personality and social psychology. 2011;101(2):354.
- Profita AC. Beberapa faktor yang berhubungan dengan keaktifan kader posyandu di Desa Pengadegan Kabupaten Banyumas. Jurnal Administrasi Kesehatan Indonesia. 2018;6(2):68–74.
- Isaura V. Faktor-faktor yang berhubungan dengan kinerja kader posyandu di wilayah kerja Puskesmas Tarusan Kecamatan Koto XI Tarusan Kabupaten Pesisir Selatan tahun 2011. Padang: Fakultas Kedokteran Universitas Andalas (skripsi tidak diterbitkan). 2011; Available from: http://repository.unand.ac.id/17532/1/FAKTOR.pdf. “Accessed December 20,2021”
- Siagian SP. Manajemen Sumber Daya Manusia. Jakarta: Bumi Aksara; 2006.
- Bangung W. Manajemen sumber daya manusia. Bandung: erlangga. 2012;
- Larasati S. Manajemen Sumber Daya Manusia. Deepublish; 2018.
- Primiyani Y, Masrul M, Hardisman H. Analisis Pelaksanaan Program Pos Pembinaan Terpadu Penyakit Tidak Menular di Kota Solok. Jurnal Kesehatan Andalas. 2019;8(2):399.
- Puspasari A. Faktor-faktor yang mempengaruhi kinerja kader posyandu dikota Sabang Provinsi Nanggroe Aceh Darussalam. Skripsi. Institut Pertanian Bogor; 2002. Available from: https://repository.ipb.ac.id/handle/123456789/14771. “Accessed December 20,2021”
- Handarsari E, Syamsianah A, Astuti R. Peningkatan Pengetahuan dan Ketrampilan Kader Posyandu di Kelurahan Purwosari Kecamatan Mijen Kota Semarang. In: PROSIDING SEMINAR NASIONAL & INTERNASIONAL. 2015. Available from: https://jurnal.unimus.ac.id/index.php/psn12012010/article/view/1646. “Accessed December 25,2021”
- Astuti ED, Prasetyowati I, Ariyanto Y. Gambaran Proses Kegiatan Pos Pembinaan Terpadu Penyakit Tidak Menular di Puskesmas Sempu Kabupaten Banyuwangi (The Description of Activity Process for the Integrated Development Post of Non-Communicable Disease (IDP of NCD) at Sempu Public Health Centre i. Pustaka Kesehatan. 2016;4(1):160–7.
- Pranandari LL, Arso SP, Fatmasari EY. Analisis implementasi program pos pembinaan terpadu penyakit tidak menular (posbindu PTM) di Kecamatan Banguntapan Kabupaten Bantul. Jurnal Kesehatan Masyarakat (Undip). 2017;5(4):76–84.
- Silviyani N, Setyawati VAV. Faktor-Faktor yang Berhubungan dengan Kinerja Posyandu Lansia di Wilayah Puskesmas Miroto Semarang. Skripsi Semarang: Universitas Dian Nuswantoro. 2015; Available from: https://core.ac.uk/download/pdf/35382833.pdf. “Accessed December 2,2021”
- Syahmasa. Analisis Hubungan Faktor Demografi dan Motivasi Dengan Kinerja Kader Dalam Berperan Serta Meningkatkan Pelyanan Keperawatan Di Posyandu Wilayah Puskesmas Kecamatan Cipayung Jakarta Timur Tahun 2002. 2002. Available from: https://lib.ui.ac.id/detail?id=72143&lokasi=lokal. “Accessed December 2,2021”
- Siagian S. Teori dan Praktek Kepimpinan. Jakarta: PT. Rineka Cipta; 2003.
- Nurhidayah I, Hidayati NO, Nuraeni A. Revitalisasi Posyandu melalui Pemberdayaan Kader Kesehatan. Media Karya Kesehatan. 2019;2(2).
- Lindner JR, Dooley KE. Agricultural education competencies and progress toward a doctoral degree. Journal of Agricultural Education. 2002;43(1):57–68.
- Jayusman TAI, Widiyarta A. Efektivitas Program Pos Pembinaan Terpadu (POSBINDU) Penyakit Tidak Menular (PTM) Di Desa Anggaswangi Kecamatan Sukodono Sidoarjo. Dinamika Governance: Jurnal Ilmu Administrasi Negara. 2017;7(2).
- Syamsianah A, Winaryati E. Hubungan Pengetahuan dan Lama Kerja Dengan Ketrampilan Kader Dalam Menilai Kurva Pertumbuhan Balita di Posyandu Kelurahan Tegalsari Kecamatan Candisari Kota Semarang. Jurnal Gizi. 2013;2(1).
Appendix A
QUESTIONNAIRE
Instruction :
1. Fill in the blanks with honest answers
2. Put a tick (X) on the multiple choice answer
3. Put a tick (√ ) on the available answer choices
A. Cadre performance
B. INCDDP Cadre Training
Have you ever received training for INCDDP cadres?
a. Yes
b. No
C. Awards
1. Have you ever received an award in the form of a charter or award while being a INCDDP cadre?
a. Yes
b. No
2. Have you ever received an award in the form of funds while being a INCDDP cadre?
a. Yes
b. No
3. Do you get a uniform to carry out INCDDP activities?
a. Yes
b. No
4. Do you always receive an award if you are active in INCDDP activities?
a. Yes
b. No
D. Facilities and infrastructure
E. Knowledge
PROBLEM BASED LEARNING MODEL IN VIRTUAL ENVIRONMENT CLASS IN HEALTH: A SISTEMATIC REVIEW
Rosmaria1, Rayandra Ashar2, Muhaimin3, Herlambang4
1Department of Midwifery, Health Polytechnic of Jambi, Indonesia
2Chemistry Education Study Program, Faculty of Teacher Training and Education, Jambi University, Indonesia
3Study Programs In Chemistry Education, Faculty of Teacher Training and Education, Jambi University, Indonesia
4Medical Study Program, Faculty of Medicine, Jambi University, Indonesia
* Corresponding author: Rosmaria, Department of Midwifery, Health Polytechnic of Jambi, Indonesia. , E-mail: rosmaria.poltekkes@gmail.com
Cita questo articolo
Abstract
Background. PBL is a student-centred learning method where students determine their own learning goals from clinical-based problems. Many studies have been conducted regarding the effectiveness of PBL based on virtual classes or online classes in various fields of science. This systematic study aims to evaluate the implementation of PBL in various online learning contexts.
Methods. This systematic review was conducted using the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) statement. We include intervention studies, training, or educational strategies using PBL method focusing on any health student class, and published between 2010 to 2021. Three authors (RA, MH, HR) performed data extraction. Differences that arise are resolved by consensus, in consultation with other investigators (RS).
Results. The search returned 1,678 articles; after removing the duplicated articles, 731 articles remained, of which 721 articles were removed after screening titles and abstracts. The remaining ten articles were reviewed and checked for eligibility, so three articles were excluded. The final results were collected as many as seven articles that met the inclusion criteria.
Conclusion. Online PBL is perceived to be an effective educational strategy by lecturer. Overall, the results for PBL in online/virtual class include Positively impact the learning experience, Increase knowledge and skills, improve the learning process, Increased self-learning capacity, motivation, self-monitoring, and interpersonal communication, Improve student understanding and application of theoretical knowledge in a large classroom setting, Increased availability and acceptance, reduced interactivity.
Keywords: Problem-Based learning, Virtual, Online Class, Students
INTRODUCTION
As a modern pedagogical philosophy, Problem-Based Learning (PBL) is increasingly recognized as a critical research area in student learning and pedagogical innovation in health science education [1,2]. In contrast to teaching and learning approaches dominated by conventional lectures, inquiry-based approaches such as PBL encourage students to be actively involved in knowledge construction and develop competencies in various contexts [3]. This review focuses on PBL rather than other inquiry-based pedagogical approaches, such as discovery learning, experiential learning, and project-based learning. Given the high level of technological involvement of 21st-century learners, a new area of research is examining the emerging role of educational technology in PBL [4–6]. Therefore, this study aims to review the application of PBL in the concept of problem-based online classes. What is interesting from this review are studies investigating the effectiveness of online classes in achieving PBL-related student learning outcomes of flexible knowledge, practical problem-solving skills, independent study skills, collaborative teamwork skills, and intrinsic motivation [7,8].
The studies included in this review are studies where educational technology has been adopted to support PBL for undergraduate and postgraduate program learning. Traditional pedagogy, which is teacher-centred, class-oriented, and pressure on exams, places students passively “acceptance” state [9]. PBL is a student-centred learning method where students determine their own learning goals from clinical-based problems [10,11]. As an established approach, PBL has been reported to be suitable for use in graduate medical schools [12]. Recently, PBL has become a subject of considerable interest in postgraduate education. PBL can cultivate postgraduate leadership, teamwork, communication, and problem-solving skills, which are helpful for lifelong learning and facilitate postgraduates to take responsibility for their learning.
The online PBL format has been piloted with varying degrees of success, and although the PBL approach is beneficial for students in various disciplines, the results associated with this strategy are inconclusive in nursing education [13]. One such study compared conventional classroom-based strategies with problem-based asynchronous learning for part-time public health students. The development of web-based technology has resulted in new ways to implement PBL in large classrooms [14]. New teaching methods facilitated by web-based technologies have been applied in nursing education using web-based PBL methods with promising effects. Web-based PBL also enables better communication between teachers and students. When used with conventional PBL teaching methods, web-based PBL facilitates the development and promotion of more significant self-directed learning and innovation in nursing and other professional education systems.
Many studies have been conducted regarding the effectiveness of PBL based on virtual classes or online classes in various fields of science. It has prompted the author's interest to conduct a systematic study of this review on PBL implementation based on online classes or virtual classes. For this reason, the current study aims to evaluate the implementation of PBL in various online learning contexts.
METHODS
Review Protocol
This systematic review was conducted using the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) statement [15]. The current study tries to evaluate the application of the problem-based learning method in virtual or online learning situations from articles that have been published in the period 2010 to 2021.
Searching strategy
Relevant articles were searched and collected using Sciencedirect, Google Scholar, Proquest, Pubmed, and the Wiley Online Library, with a publication time between 2010 and 2021. The search keywords were adjusted according to the Mesh terms for health research. The keywords used vary, depending on the search engine used. In general, the keywords focus on 'Effectiveness' OR 'Effect' OR 'Evaluation' AND 'Problem-Based Learning' OR 'PBL' AND 'Online class' OR 'Virtual class' OR 'virtual meeting' AND 'web-based' OR 'social-media OR 'Online group discussion'.
Eligibility
Inclusion criteria consist of intervention studies, training, or educational strategies using PBL method focusing on any health student class in certain subjects for example Physiology, anatomy, nursing care, community health, etc. Study outcomes such as increased knowledge, attitude, skills, and/or student satisfaction. We choose only articles published in English, and in the time range 2010 to 2021. We excluded or not reviewed books, disertation, letter to editor, and systematic review study.
Study Quality
Overall articles were assessed using the NIH (National Institutes of Health) quality assessment of controlled intervention studies, for Observational Cohort and Cross-Sectional Studies, and Quality Assessment of Case-Control Studies [16].
A scoring sheet was developed to assess the research methodology and adherence to the scoring criteria for each article that met the inclusion criteria of this study. Articles with scores <30% of the criteria were classified as "poor", scores between 30 and 70% were classified as "moderate", and scores >70% were classified as "good" study quality. The articles taken are classified as moderate and "good".
Extraction and Analysis
Three authors (RA, MH, HR) performed data extraction. Differences that arise are resolved by consensus, in consultation with other investigators (RS) if an agreement is not reached. Main items extracted included: lead author/year, country, purpose of the study, method (Quasi-experimental, Randomized Controlled Trial), evaluation strategies, and results.
Titles and abstracts are screened on each database. Screening for duplicate articles is carried out using the Mendeley application. Substantive information is extracted from each article into a Microsoft Word table.
The author determined the selection of articles after being reviewed from 7 full-text articles adjusted to the inclusion and exclusion criteria. Data extraction was carried out with care. The interpretations are presented in the table by taking the critical parts of the article.
RESULTS
The search returned 1,678 articles; after removing the duplicated articles, 731 articles remained, of which 721 were removed after screening titles and abstracts. The remaining ten articles were reviewed and checked for eligibility, so three articles were excluded. The final results were collected as many as seven articles that met the inclusion criteria.
Article Characteristics
Most of the literature included is in the quantitative type with a Quasy experimental research design of five articles [13,17,18,21,22] and one each for the Randomized Controlled Trial [20], and Research & Development [19]. A total of 654 students were involved in all the studies included in this study. Included articles were published from 2010 to 2021 and conducted in five different countries, including China (n = 3) and one study in Hong Kong, Turkey, Korea, and the USA.
Areas of knowledge for the implementation of Problem-Based Learning (PBL) in online classes include Hematology [17], Dentistry [13], Nursing management [22], problem-solving skills, and communication skills [18], Division of Speech and Hearing Sciences [19], Oncology Nurses [20], bio-pharmaceutics [21].
The educational levels of participants in several articles included in this review consist of clerkship students [13], Post-graduate students [15], undergraduate students, and working nurses [18].
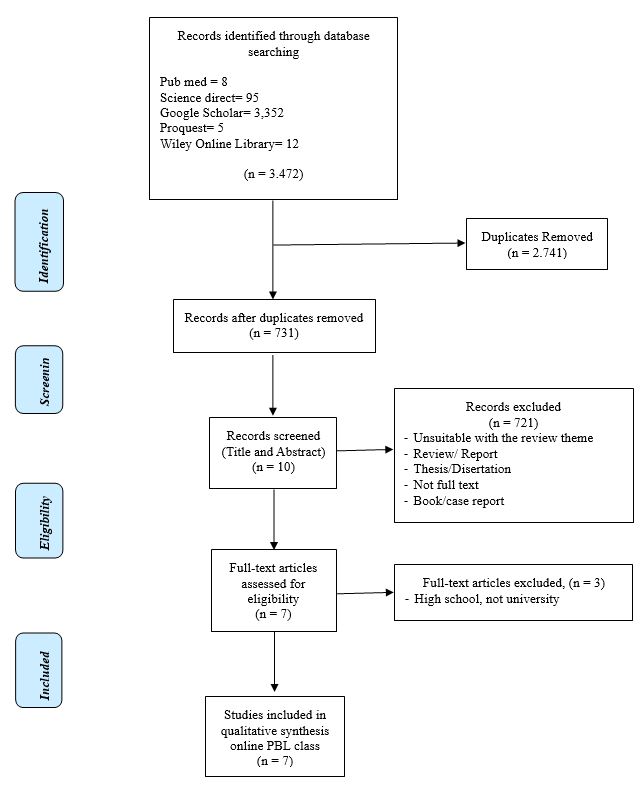
Figure 1. PRISMA Flowchart literature search
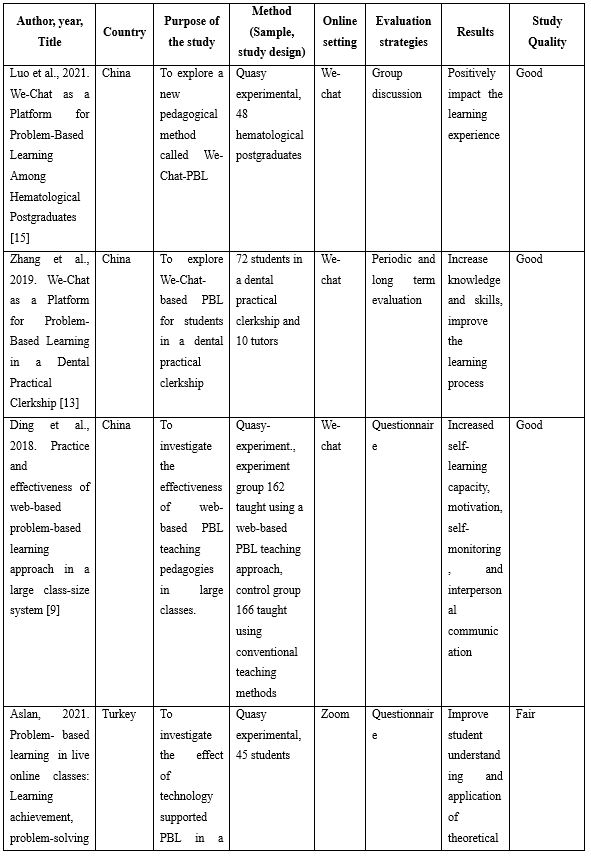
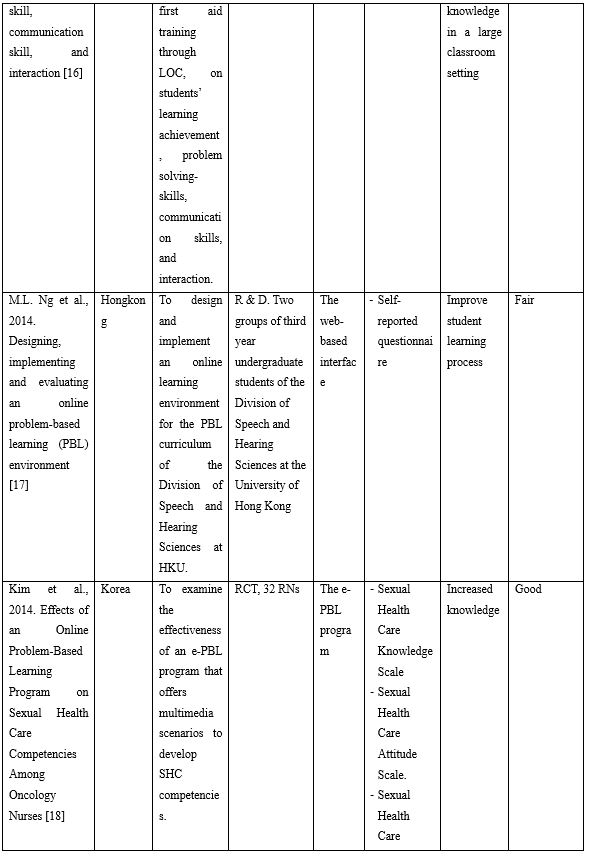
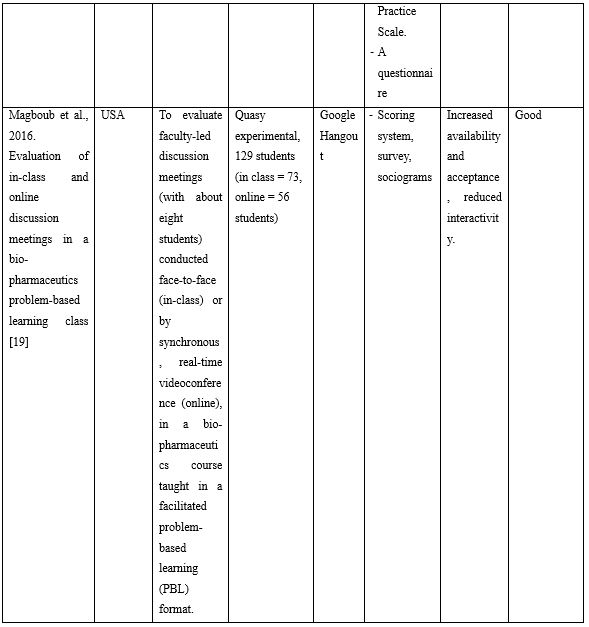
Table1. Critical data extraction from included articles
Online settings
The online class system used is varied, such as We-chat social media used in three studies conducted in China with results showing that this strategy provides an increase in the learning experience, increases student knowledge, and interpersonal communication [13,17,22]. Two studies conducted in the same year, namely 2014 in Hong Kong and Korea, used a web-based interface to form Adobe Connect and the e-PBL program. In carrying out the study, authors combined several other internet-based communication channels such as e-mail, and social media as a forum to discuss the assigned tasks where it improvises the learning process and can increase students' knowledge [19,20]. Meanwhile, a study in the USA used the Google Hangout application to discuss the tasks of the Problem-Based Learning program; this is considered the most accessible medium to use where this application is available on every gadget or smart phone. Through those media may increased availability and acceptance, but unfortunately reduced interactivity [21]. The application that is currently most often used is "Zoom" Aslan conducted a study that tried to investigate the effect of using this application in the PBL model on the problem-solving skills, communication skills, and interactions of 45 students involved in his studies. Zoom PBL improves student understanding and application of theoretical knowledge in a large classroom setting [18].
The entire study was conducted to assess the effect of implementing the PBL method in online classes. Some studies even compare with conventional methods or face-to-face [21]; [20]. Meanwhile, the study conducted by [18] tried to compare the online class with the PBL approach with the online class teacher-based methods. Three studies using We-chat applications in China aimed to assess the effectiveness of online class-based PBL using We-chat, but each has a different field of knowledge for its application [13,17,22].
DISCUSSION
The articles reviewed in this systematic review generally show the implementation of PBL methods in online classes. In some cases, this method can reduce cognitive load and allow students to learn in complex domains [18,20].
The We Chat-based PBL mode conducted by [17] is designed to support postgraduate students' abilities in haematology courses, including those related to clinical reasoning, team skills, and meta-cognition. This online PBL model has succeeded in eliminating the physical and temporal limitations of traditional PBL, as has been implemented so far [17]. Similar results were also obtained in another study that used We-Chat as a medium in the implementation of PBL, where this method succeeded in removing the physical and temporal limitations of traditional PBL in dental registrars. We-chat is very common and familiar in China, so this application is the primary choice for people to socialize in cyberspace. This method also ensures the time required and quality of PBL, expands the means of acquiring knowledge, and increases efficiency in problem-solving. As a modern pedagogical philosophy, the importance of PBL is increasingly recognized in student learning and innovation in medical education [1]. Many educators have tried to improve traditional PBL by modifying instruction. Therefore, other PBL modes such as tutors PBL, 3C3R Modified PBL, and Hybrid PBL have emerged in PBL teaching [13,23,24]. However, compared to traditional PBL, WeChat-PBL has several advantages that take PBL to a higher level [13,22].
M.L. Ng and colleagues used Adobe Connect to implement online tutorials to embody the Problem-Based Learning model for students. Users, namely students, can open any web browser to connect to Adobe Connect. All PBL sessions ran smoothly, without significant delays in audio or serious interruptions in video transmission. Students stated that Adobe Connect was smooth, easy to install and worked well with their home internet connection. The students agreed that the system met the requirements for online tutorials. The study also concludes that the pedagogical effectiveness associated with online PBL does not differ from traditional PBL for students in later years with the curriculum well integrated into the PBL process. Through online PBL, students enjoy PBL more and save a lot of travel time [19]. Thus, online PBL appears to be the way forward when time and place requirements cannot be met or when weather or other conditions do not allow for regular meetings or the current situation, namely the Covid-19 pandemic.
The e-PBL program that is trying to be developed in Korea shows that this program is very useful, especially for Oncology nurses. Online learning allows participants to interact with each other regardless of time and place restrictions and presents complex data in an accessible way that is fun and easy to learn. This program is highly expected to be integrated into continuing education for nurses. when PBL is delivered in online groups, students can play an active role in solving problems through the use of case studies and online discussions. Tutors participate in online discussions by contributing questions and comments, and provide timely feedback to encourage collaboration and topic-focused discussion [20].
The challenges of online education include technological capabilities, student acceptance of technology, and the ability of lecturers to adapt to new roles and to acquire new instructional skills [25]. The survey results in research in the USA show that technology is not a barrier for students. However, almost half of the students in the class indicated that they preferred discussion in class to online. Many students get lower online discussion learning scores than in class meetings [5]. PBL discussion meetings may be held online due to the increased availability and acceptance of technology but may lead to reduced interaction and participation. This suggests that online discussions require facilitators to encourage and stimulate student participation and active student-student interaction which may differ from the approach used for face-to-face class discussions [5].
The current reviews corresponds to the findings from other reviews focusing on the effectiveness of DPBL (Digital Problem Based Learning) in improving health professionals’ knowledge, skills, attitudes, and satisfaction [1],[26]. These reviews explores more the differentiation between DPBL and traditional PBL [26]. In current review, we found few evidence that show the effectiveness of PBL in virtual environment similar with traditional PBL. Jin & Bridges reviews stated more on the hardware used in PBL, while our review mostly used software or application which commonly can be accessed using android technology in mobile phone.
CONCLUSION
This systematic review shows the implementation of various PBL-based online classroom technologies. Overall, the results for PBL in virtual class include Positively impact the learning experience, Increase knowledge and skills, improve the learning process, Increased self-learning capacity, motivation, self-monitoring, and interpersonal communication, Improve student understanding and application of theoretical knowledge in a large classroom setting, Increased availability and acceptance, reduced interactivity.
LIMITATION
The systematic preparation of this review cannot be separated from efforts to collect relevant articles completely and comprehensively discussing issues related to the theme of implementing the PBL model in online classes. The author does not collect enough relevant articles due to the accessibility of relevant articles in the database that the author cannot do, besides the language that the author limits to English articles only. In the end, we were unable to carry out further analysis (meta-analysis) because the number of articles included in this study did not meet the requirements (very few).
Funding statement
This research did not receive any specific grant from funding agencies in the public, commercial, or not for profit sectors.
Competing interests statement
There are no competing interests for this study.
REFERENCES
- Jin J, Bridges SM. Educational technologies in problem-based learning in health sciences education: a systematic review. Journal of medical internet research. 2014;16(12):e251.
- Zabit MNM. Problem-based learning on students critical thinking skills in teaching business education in Malaysia: A literature review. American Journal of Business Education (AJBE). 2010;3(6):19–32.
- Prosser M, Sze D. Problem-based learning: Student learning experiences and outcomes. Clinical linguistics & phonetics. 2014;28(1–2):131–42.
- Bridges S, Botelho M, Green JL, Chau ACM. Multimodality in problem-based learning (PBL): An interactional ethnography. In: Problem-based learning in clinical education. Springer; 2012. p. 99–120.
- Bridges SM, Green J, Botelho MG, Tsang PCS. Blended learning and PBL: An interactional ethnographic approach to understanding knowledge construction in-situ. Essential readings in problem-based learning: Exploring and extending the legacy of Howard S Barrows. 2015;107–30.
- Lu J, Bridges S, Hmelo-Silver C. Problem-based learning. The Cambridge handbook of the learning sciences. 2014;298–318.
- Hmelo-Silver CE. Problem-based learning: What and how do students learn? Educational psychology review. 2004;16(3):235–66.
- Hmelo-Silver CE, Barrows HS. Goals and strategies of a problem-based learning facilitator. Interdisciplinary journal of problem-based learning. 2006;1(1):4.
- Matsuka Y, Nakajima R, Miki H, Kimura A, Kanyama M, Minakuchi H, et al. A problem‐based learning tutorial for dental students regarding elderly residents in a nursing home in Japan. Journal of dental education. 2012;76(12):1580–8.
- Aldayel AA, Alali AO, Altuwaim AA, Alhussain HA, Aljasser KA, Abdulrahman KA Bin, et al. Problem-based learning: medical students’ perception toward their educational environment at Al-Imam Mohammad Ibn Saud Islamic University. Advances in medical education and practice. 2019;10:95.
- Rui Z, Rong-Zheng Y, Hong-Yu Q, Jing Z, Xue-Hong W, Chuan Z. Preliminary investigation into application of problem-based learning in the practical teaching of diagnostics. Advances in medical education and practice. 2015;6:223.
- Doherty-Restrepo J, Odai M, Harris M, Yam T, Potteiger K, Montalvo A. Students’ perception of peer and faculty debriefing facilitators following simulation-based education. Journal of allied health. 2018;47(2):107–12.
- Yan Q, Ma L, Zhu L, Zhang W. Learning effectiveness and satisfaction of international medical students: Introducing a Hybrid–PBL curriculum in biochemistry. Biochemistry and Molecular Biology Education. 2017;45(4):336–42.
- Liu L, Du X, Zhang Z, Zhou J. Effect of problem-based learning in pharmacology education: A meta-analysis. Studies in Educational Evaluation. 2019;60:43–58.
- Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS medicine. 2009;6(7):e1000097.
- Health NI of. Quality assessment tool for observational cohort and cross-sectional studies. 2014.
- Luo P, Pang W, Wang Y, Liu M, Zhou S, Liu S, et al. WeChat as a Platform for Problem-Based Learning Among Hematological Postgraduates: Feasibility and Acceptability Study. Journal of Medical Internet Research. 2021;23(5):e16463.
- Aslan A. Problem-based learning in live online classes: Learning achievement, problem-solving skill, communication skill, and interaction. Computers & Education. 2021;171:104237.
- Ng ML, Bridges S, Law SP, Whitehill T. Designing, implementing and evaluating an online problem-based learning (PBL) environment–A pilot study. Clinical linguistics & phonetics. 2014;28(1–2):117–30.
- Kim J-H, Shin J-S. Effects of an online problem-based learning program on sexual health care competencies among oncology nurses: a pilot study. The Journal of Continuing Education in Nursing. 2014;45(9):393–401.
- El-Magboub A, Haworth IS, Sutch BT, Romero RM. Evaluation of in-class and online discussion meetings in a biopharmaceutics problem-based learning class. Currents in Pharmacy Teaching and Learning. 2016;8(6):811–20.
- Ma X, Pan Y-J, Chen F, Ding X, Tseng S-P. A constructive problem-based course design for internet of things. In: International Conference on Smart Vehicular Technology, Transportation, Communication and Applications. Springer; 2017. p. 397–402.
- Kaliyadan F, Amri M, Dhufiri M, Amin TT, Khan MA. Effectiveness of a modified tutorless problem‐based learning method in dermatology–a pilot study. Journal of the European Academy of Dermatology and Venereology. 2012;26(1):111–3.
- Xue H, Qian J, Wang L, Yuan X, Chen Y, Wu W, et al. 3C3R modified PBL pediatric teaching of Chinese medical students. PloS one. 2013;8(5):e63412.
- Barrot JS, Llenares II, Del Rosario LS. Students’ online learning challenges during the pandemic and how they cope with them: The case of the Philippines. Education and Information Technologies. 2021;1–18.
- Kyaw BM, Saxena N, Posadzki P, Vseteckova J, Nikolaou CK, George PP, et al. Virtual reality for health professions education: systematic review and meta-analysis by the digital health education collaboration. Journal of medical Internet research. 2019;21(1):e12959.
![]() This work is licensed under a Creative Commons
This work is licensed under a Creative Commons
Attribution-NonCommercial-NoDerivatives 4.0 International License.
VIDEO-BASED INTERVENTION ON THE KNOWLEDGE OF BREAST-MILK SUPPORT GROUP IN SEMBUBUK VILLAGE, MUARO JAMBI REGENCY: A PRE-EXPERIMENT STUDY
Yuli Suryanti1*, Damris Muhammad2, M. Naswir3, Guspianto2
1Department of Midwifery, Health Polytechnic of Jambi, Indonesia
2Department of Environmental Engineering, Jambi University, Indonesia
3Department of Chemistry, Jambi University, Indonesia
4Department of Public Health, Jambi University, Indonesia
* Corresponding author: Yuli Suryanti, Department of Midwifery, Health Polytechnic of Jambi, Indonesia, Jalan Prof DR GA Siwabessy No.42. Buluran Kenali, Kec. Telanaipura, Kota Jambi,.36122, Phone : +62 813-6635-9359, E-mail: suryantiyuli03@gmail.com
Cita questo articolo
Abstract
Introduction: Breast milk is the best food for babies because it contains nutrients to support growth and development. The achievement rate of exclusive breastfeeding in ASIA countries has not yet reached the expected target. The coverage of exclusive breastfeeding in Jambi Province in 2018 was 59.36%. The success of exclusive breastfeeding is not only influenced by the mother's physical and mental readiness to breastfeed. Still, it is also influenced by support from health workers and the family. The study aimed to determine the effect of counseling using breastfeeding video on grandmothers' knowledge as breastfeeding support in Sembubuk Village, Muaro Jambi Regency.
Methods: This type of pre-experimental research using the One Group Pretest-Posttest design, which saw 40 grandmothers of the Breast Milk Support Group members, was carried out from June 2020 to July 2021. Respondents answer the questionnaires to complete the data collection. The intervention carried out in this study was the provision of counseling using video media about breastfeeding. Data were analyzed through univariate and bivariate using the Wilcoxon test.
Results: The results showed the p-value = 0.0001, which means that breastfeeding video affects grandmothers' knowledge in breastfeeding support groups in Sembubuk village, Muaro Jambi District.
Conslusion: The results of this study are expected to increase public knowledge and insight regarding the importance of breastfeeding for infant health so that positive behavior is formed in breastfeeding, providing additional appropriate information to advance understanding of breastfeeding support groups about breastfeeding.
Keywords: Exclusive breastfeeding, health education, Knowledge, Video-based
Introduction
Breast milk has been an optimal food source for babies due to its rich nutrients for growth and development [1–3]. The benefits of breast milk will be optimal if it is given regularly from birth with the correct breastfeeding position, breastfeeding at the baby's desire (on demand), and offered exclusively [4–6]. In Indonesia, exclusive breastfeeding for 6 (six) months has been stipulated in the Decree of the Minister of Health No. 450/Menkes/SK/IV/20042 [7].
The achievement target of exclusive breastfeeding in Indonesia is 75% [8], while globally, it is 70% [9]. Exclusive breastfeeding in ASIA countries is far from the achievement target [10]. Exclusive breastfeeding coverage for infants under 6 months is 15% in Thailand, 40% in China, Indonesia 42%, India 46%, Mongolia 66% [11]. Based on this percentage, Indonesia has the third position of lowest breastfeeding coverage compared to other ASIA countries [12]. The issue is related to the number of mothers who do not like exclusive breastfeeding, where almost 9 out of 10 mothers have breastfed [13]. Still, only 49.8% gave exclusive breastfeeding for six months [14,15]. The low coverage of exclusive breastfeeding impacts the quality of life of the next generation and the national economy [16–18]. The number of mothers who have breastfed in Indonesia is already high at 90%, but those who give exclusively for six months are still low (20%) [19,20]. The coverage of exclusive breastfeeding in 2018 in Jambi Province was 59.36%, while the target for the province was 61%. Merangin Regency is the only district with the highest achievement of exclusive breastfeeding with 88.75%. In comparison, the lowest is Tanjung Jabung Barat Regency at 30.91%, and Muaro Jambi Regency with the 3rd rank of 64.54% [21]. Penyengat Olak, one of the sub-districts in Muaro Jambi Regency, consists of 8 villages. Sembubuk village is the only village with the lowest breastfeeding coverage; based on the survey results, the number of infants aged 0-2 years old in Sembubuk was 71 people, and the number of infants 0-6 months was 40 people. The Penyengat Olak Health Center targets exclusive breastfeeding of 65% [22].
Infants, who get insufficient breastfed until the first six months of life, are at risk of developing diarrhea [23,24]. Meanwhile, complementary foods such as formula milk also increase the risk of diarrhea, resulting in malnutrition because the nutritional content in formula milk is not sufficient to meet baby needs. Lack of breastfeeding causes babies to be malnourished [25,26]. Malnutrition will decrease the quality of human resources, such as failure of physical growth, mental and intellectual development, lowering productivity, increasing morbidity and mortality. Breast milk benefits both mother and fetus, and it also appears to reduce the chances of getting leukemia, lymphoma, diabetes, and asthma as the child grows older [27].
The success of exclusive breastfeeding is not only influenced by the mother's physical and mental readiness but is also influenced by support factors from both health workers and family [28]. Research by Nankuda et al. [29], in rural areas in Uganda proves that peer support in the form of visits and providing support can be more readily accepted in the breastfeeding mother community. Mothers feel happy to have a peer counselor who can help them with various problems during breastfeeding [30]. To improve and support the process of exclusive breastfeeding for mothers, forming a breastfeeding support group can be an option [31]. The Breast Milk Support Group is a forum for breastfeeding mothers to give and receive technical, moral, and emotional support by exchanging experiences and discussing maternal and child health, especially breastfeeding and nutrition [32]. Those are facilitated or guided by breast milk motivators. It is considered to cause behavioral changes in society. One of these behavioral changes can be seen in the mother's breastfeeding belief [33]. Bekti and colleagues [7], in their study on the Effectiveness of Exclusive Breastfeeding Support Groups (EBSG) toward Exclusive Breastfeeding Behavior, found that the majority of the groups with exclusive EBSG support (86.4%) gave exclusive breastfeeding. In comparison, there is only a tiny part (31.8%) of exclusively breastfed in the leaflet group. The formation of breastfeeding support groups affects entire breastfeeding behavior (p-value 0.001).
The involvement of grandmothers who support breastfeeding is essential because grandmothers play a vital role in the family. Grandmothers can influence decisions in the family, whether the mother should breastfeed a newborn baby or not. This condition is almost evenly spread throughout Indonesia [34,35]. Other research in the Ayeyarwaddy Region in Myanmar found that one of the primary barriers to exclusive breastfeeding was that mothers, husbands, and grandmothers believed exclusive breastfeeding was insufficient for babies and solid foods and water were necessary [36]. Supporting EBSG activities, a counseling program is needed to increase grandmother's knowledge about the importance of exclusive breastfeeding. Counseling is effective using a variety of media. It depends on the learning component, such as the use of media. Engaging media will provide confidence to accelerate affective and psychomotor cognitive changes [37]. One of the media in counseling is video. Video is a modern interactive medium by times (advancement of science and technology) because it can be seen and heard. Messages delivered are more efficient because moving images can communicate messages quickly and naturally [38].
Video media has advantages in providing good visualization to facilitate absorbing knowledge. Video is included in audio-visual media because it involves the sense of hearing and the importance of sight [38].
This study aims to determine the effect of video media on breastfeeding knowledge of breastfeeding support groups in Sembubuk Village, Muaro Jambi Regency.
Methods
Trial design
This study establishes a pre-experiment with the One Group Pretest-Posttest approach, aiming to determine the Effect of Video Media on Breastfeeding on Knowledge of Breastfeeding Supporting Grandmothers Group in Sembubuk Village, Muaro Jambi Regency.
Participants
The population in this study were EBSG members totaling 40 people, selected randomly and consecutively according to our inclusion criteria. This study was conducted in June 2021.
Inclusion and Exclusion Criteria
Grandmothers who live with nursing mothers, while grandmothers who do not understand Indonesian are excluded
Intervention
The data was collected by filling out a questionnaire by the respondents. The intervention that will be carried out in this study is the provision of counseling using video media about breastfeeding. The research team made Breastfeeding videos are made. This video is 15 minutes long which contains the understanding of breastfeeding, the benefits of breastfeeding, the correct way to breastfeed, the recommended breastfeeding time, the duration of breastfeeding. video screening was held at the conference hall in Sembubuk Village, Muaro Jambi Regency
The knowledge questionnaire consists of 15 questions about breastfeeding. If the mother who supports breastfeeding is correct, she is given a score of 1, while if the answer is wrong, she is given a 0. The objective criteria for the variable are good and imperfect knowledge. Cut-off criteria are good and less, using a median value of 8. Good criteria, if the total answer score is 8-15, while the criteria are less if the total answer score is 1-7.
This questionnaire contains the definition of breastfeeding, benefits for mothers and babies; baby satisfied signs, the content of breast milk, the age of breastfeeding, breastfeeding manner, the actions after breastfed, when the baby is breastfed for the first time, the meaning of colostrum, the age of giving. Complementary feeding, grandmother's understanding of breastfeeding, frequency of breastfeeding in a day. The questionnaire used has been validated and declared valid and reliable. Determine the validity of the questions by using the product-moment test. If the coefficient between each item and the total item is equal to or above 0.3, the item is declared valid. Still, if the correlation value is below 0.3, the item is declared invalid. While the correlation is 0.7, the item provides a sufficient level of reliability; otherwise, if the correlation value is below 0.7, the item is said to be less reliable—determination of reliable items using Spearman Rho test [39]. The instrument test was carried out on ten breastfeeding mothers with the results. From the 15 questions asked, two questions had a validity index value of <0.3, so they had to be corrected, and two questions correlated 0.7, so they had to be updated again.
Questionnaires were distributed to grandmothers in Sembubuk village, Muaro Jambi district, Indonesia. After the researcher carried out data collection, the researcher then compiled the data, processed and analyzed the data. Female researcher aged 35-50 years with qualified health research experience.
Outcomes
The research outcome is in the form of information about the influence of video media on the knowledge of breastfeeding mothers
Sample size
This study involved 40 participants, namely grandmothers who support breastfeeding, where these grandmothers will be given education in the form of breastfeeding videos and then evaluate the knowledge of the grandmothers.
Ethical Consideration
No economic incentives were offered or provided for participation in this study. The study was performed in accordance with the ethical considerations of the Helsinki Declaration. This study obtained ethical feasibility under the Health Research Ethics Commission of the Ministry of Health, Jambi, and registration number: LB.03.02./3.5/140/2021.
Statistical analysis
Data are presented as numbers and percentages for categorical variables. Continuous data were expressed as mean ± standard deviation (SD) or median with Interquartile Range (IQR). Then proceed with bivariate analysis using the Wilcoxon test. The Wilcoxon test was used to determine the effect of counseling using breastfeeding video on the knowledge of breast milk supportive groups. All tests with p-value (p)<0.05 were considered significant. Statistical analysis was performed using the SPSS version 16.0 application.
Results
The characteristics of respondents in this study include age, education level, and occupation. The following is the frequency distribution of the respondents' characteristics in this study:
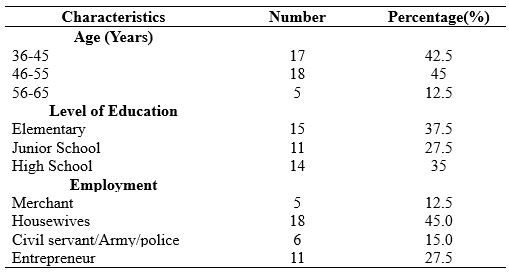
Table 1. Frequency Distribution of Respondents Characteristics
In Table 1 it is known that most of the respondents with an age range of 46-55 years are 18 respondents (45%), and there are no respondents aged <25 years. most of the respondents with elementary education are 15 respondents (37.5%). Most types of work are housewives as many as 18 respondents (45.0). Knowledge of breastfeeding support groups before and after being given an intervention using video media about breastfeeding underwent univariate analysis.
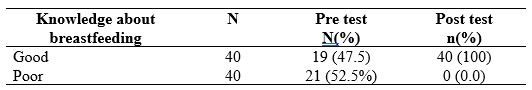
Table 2. Distribution of Knowledge Frequency of Breastfeeding Support Groups Before and after Video Media About Breastfeeding
Table 2 shows that of the 40 respondents who knew the breastfeeding grandmother group before being given video media about breastfeeding, 19 respondents (47.5%) had good knowledge, and 21 respondents (52.5%) had poor knowledge. Then it changed after counseling using video media, namely 40 respondents (100%) had good knowledge.
The effect of breastfeeding counseling using video media on the knowledge of the grandmothers of the support group can be seen in the following table:
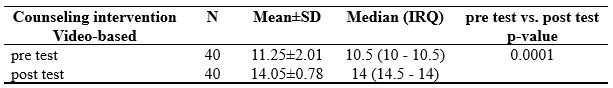
Table 3. The Effect of Video Breastfeeding on Knowledge of Breastfeeding Supporting Group
Table 3 shows an increase between before and after being given video media about breastfeeding with statistical test results obtained p-value = 0.0001 <0.05. This statistical test indicates an effect of video media on breastfeeding on the knowledge of the breastfeeding support grandmother group in Sembubuk village, Muaro Jambi District.
Discussion
The description of the knowledge of the breastfeeding grandmother group before (pre-test) the video-based intervention was rated at a minimum of 5, and the maximum value of the ability of the breastfeeding support grandmother group before being given video-based intervention was 15. The average value of the knowledge value of the breastfeeding support grandmother group before being given an intervention using media the video is 11.25.
The current study revealed respondents knowledge which appears inadequate regarding breastfeeding. Respondents indicated some of their ignorance about the economic benefits of breastfeeding for mother and baby, baby signs of enough breast milk, the nutrients in breast milk, exclusive breastfeeding time, breastfeeding manner, activities after breastfeeding, the right time to provide breast milk, breast milk for the first time, Breastfeeding in infants, the role of colostrum, timing of additional food and drink, sources of information, and frequency of breastfeeding in a day.
The description of support groups' breastfeeding knowledge in Sembubuk Village after (post-test) intervention reaches a minimum score of 13, a maximum value of 15 and a median value of 14.00. After being given a video-based intervention, nearly all of the questions can be answered by respondents. It shows an increase in the knowledge of the breastfeeding support grandmother group. The questionnaire correctly answers statements about the nutritional contained in breast milk, such as carbohydrates, proteins, fats, minerals and vitamins. The following information is regarding the correct way of breastfeeding. Washing hands, cleaning the mother's breasts, removing a little milk and then smearing it on the nipple and the surrounding areola, inserting the nipple and making sure the baby sucks the entire dark area of the breast and not just the nipple. The following statement is about when a baby should be given his first breast milk immediately after birth or a maximum of 1 hour after birth. The results are in line with the previous study [7] regarding the Effectiveness of Exclusive Breastfeeding Support Groups on Exclusive Breastfeeding Behavior, where the group with exclusive Breast Milk Support mainly (86.4%) gave exclusive breastfeeding, while the group with leaflet intervention only a tiny proportion (31.8%) of exclusively breastfeeding. The formation of breastfeeding support groups affects exclusive-breastfeeding behavior (p-value 0.001).
Another study by Fatiyani & Ani [40] regarding the Formation and Implementation of Breastfeeding Support Groups in the Work Area of the Rejosari Health Center, Tenayan Raya Pekanbaru, in 2019 found the formation of a Breastfeeding Support Group (BSG) "Bintang with Sirih Adat." Increase knowledge of Exclusive Breastfeeding Support Groups mothers on Early Breastfeeding Initiation (IMD) material from an average of 60 to 80. Knowledge of Exclusive Breastfeeding Support Groups mothers on breastfeeding material from an average of 70 to 90.4. The provision of Exclusive Breastfeeding Support Groups mothers' skills in providing IEC was 83.75.
The BSG in Penyengat Olak is the Breastfeeding Supporting Grandmother Group (BSGG), an association or community whose members consist of grandmothers who work in breastfeeding support groups. This group of grandmothers who support breastfeeding is followed by prospective grandmothers/grandmothers aged 34-65 years, established in 2019. The activity was carried out at the Penyengat Olak Health Center with several briefings and providing materials using leaflet media by a team of health workers about the importance of exclusive breastfeeding during breastfeeding. Six months, and continued breastfeeding for up to 2 years.
BSGG can assist in counseling activities and increase the coverage of exclusive breastfeeding in Sembubuk village, Muaro Jambi District. The reason for choosing grandmothers as a supporter of breastfeeding is related to the role of parents. Both in-laws and grandmothers significantly influence exclusive breastfeeding, such as the recommendation to give complementary foods (MPASI) too early, usually because the baby is fussy even though he has been given breast milk or formula milk. In addition, a grandmother is a person who is more experienced in taking care of babies because grandmothers already have this experience so that they can be an example or role model for young mothers. Although mothers know that giving MP-ASI too early can interfere with the baby's health, they think that parents, whether in-laws or grandmothers, are considered to learn better ways to take care of children because they are deemed to have experience and understand better in taking care of children [41].
Conclusion
There is an increase in BSGG knowledge after being given video-based counselling, with statistical test results obtained p-value = 0.0001, which means that video media's effect on breastfeeding on BSG knowledge in Sembubuk village Muaro Jambi District.
This intervention can be used as an effort to improve the quality of health services and health promotion as well as add information and insight for health workers at the Penyengat Olak Health Center, especially in Sembubuk Village, where breastfeeding coverage is the lowest in the work area of the Penyengat Olak Health Center of 7 other villages.
Limitations of Study
The limitations of this study include the very limited number of samples and the research only involves one province in Indonesia.
Acknowledgement
We would like to express our gratitude to the director of the Midwifery Department of Jambi health polytechnic who has supported this research.
Funding statement
This research did not receive any specific grant from funding agencies in the public, commercial, or not for profit sectors.
Competing interests statement
There are no competing interests for this study.
References
- Kusnan A, Binekada IMC, Usman AN. The proxy determinant of complementary feeding of the breastfed child delivery in less than 6 months old infant in the fishing community of Buton tribe. Enfermeria clinica. 2020;30:544–7.
- Ku C, Chow SKY. Factors influencing the practice of exclusive breastfeeding among Hong Kong Chinese women: a questionnaire survey. Journal of clinical nursing. 2010;19(17‐18):2434–45.
- Kridis WB, Mnif A, Khmiri S, Toumi N, ... Self-medication with herbal medicine and breast cancer survival: a prospective monocentric study. Journal of Cancer … [Internet]. 2021; Available from: https://link.springer.com/article/10.1007/s00432-021-03600-y
- Arsin AA, Sirajuddin S, Syafar M. The effect of education lactation on breastfeeding behavior infant 0-6 months in Kendari Indonesia. Public Health of Indonesia. 2016;2(2):100–11.
- Tan KL. Factors associated with exclusive breastfeeding among infants under six months of age in peninsular Malaysia. International breastfeeding journal. 2011;6(1):1–7.
- La Aga, Erwin AL. Cakupan dan Determinan Pemberian ASI Ekslusif di Pemukiman Kumuh Dalam Perkotaan di Kecamatan Tallo Kota Makassar. Majalah Kesehatan FKUB. 2019;6(1):44–55.
- Yuniyanti B. Efektivitas Kelompok Pendukung ASI (KP-ASI) Eksklusif terhadap Perilaku Pemberian ASI Eksklusif. Jurnal Ilmiah Bidan. 2017;2(1):48–54.
- Kemenkes Republik Indonesia. Profil Kesehatan Indonesia tahun 2020. Pusdatin. Jakarta; 2020.
- World Health Organization. Global Breastfeeding Scorecard, 2019 [Internet]. 11 Februari 20219. 2020. p. 4. Available from: https://apps.who.int/iris/bitstream/handle/10665/326049/WHO-NMH-NHD-19.22-eng.pdf
- Danso J. Examining the practice of exclusive breastfeeding among professional working mothers in Kumasi metropolis of Ghana. International journal of nursing. 2014;1(1):11–24.
- Oktavianto E, Setyaningrum H, Timiyatun E. Dukungan Nenek Berhubungan Erat Dengan Keberhasilan ASI Eksklusif. Surya Medika: Jurnal Ilmiah Ilmu Keperawatan Dan Ilmu Kesehatan Masyarakat. 2018;13(2).
- Aryeetey R, Dykes F. Global implications of the new WHO and UNICEF implementation guidance on the revised Baby‐Friendly Hospital Initiative. Maternal & child nutrition. 2018;14(3):e12637.
- Kementerian Kesehatan RI. Laporan Riskesdas 2018. Laporan Nasional Riskesdas 2018. 2018;
- Aoyagi S-S, Tsuchiya KJ. Does maternal postpartum depression affect children’s developmental outcomes? Journal of Obstetrics and Gynaecology Research [Internet]. 2019 Sep 18;45(9):1809–20. Available from: https://onlinelibrary.wiley.com/doi/abs/10.1111/jog.14064
- Emerson JA, Tol W, Caulfield LE, Doocy S. Maternal Psychological Distress and Perceived Impact on Child Feeding Practices in South Kivu, DR Congo. Food and Nutrition Bulletin [Internet]. 2017 Jun 19;38(3):319–37. Available from: https://doi.org/10.1177/0379572117714385
- Jacobson SW, Chiodo LM, Jacobson JL. Breastfeeding effects on intelligence quotient in 4-and 11-year-old children. Pediatrics. 1999;103(5):e71–e71.
- Fonseca ALM, Albernaz EP, Kaufmann CC, Neves IH, de Figueiredo VLM. Impact of breastfeeding on the intelligence quotient of eight-year-old children. Jornal de Pediatria (Versão em Português). 2013;89(4):346–53.
- Bernard JY, Armand M, Peyre H, Garcia C, Forhan A, De Agostini M, et al. Breastfeeding, polyunsaturated fatty acid levels in colostrum and child intelligence quotient at age 5-6 years. The Journal of Pediatrics. 2017;183:43–50.
- Widyastutik O, Nursya D. Kelompok Nenek ASI sebagai Empowerment Kader ASI di Kelurahan Mariana Pontianak. BULETIN AL-RIBAATH. 2019;15(2):30–5.
- Mulyadi. Faktor-Faktor yang Berhubungan dengan Pemberian ASI Eksklusif Pada Keluarga Miskin di Puskesmas Tebas Kecamatan Tebas Kabupaten Sambas. Skripsi thesis, Fakultas Ilmu Kesehatan. Universitas Muhammadiyah Pontianak; 2014.
- Department of Health Jambi Province. Profile Health Department of Health Jambi Province [Internet]. Jambi, Indonesia; 2018. Available from: http://dinkes.jambiprov.go.id/file/informasi_publik/MTYxNTE2NDQyOA_Wkt1615164428_XtLnBkZg.pdf
- Penyengat Olak Health Center. Health Profil of Penyengat Olak Health Center [Internet]. Jambi, Indonesia; 2020. Available from: https://pkmpenyengatolak.muarojambikab.go.id/
- Lamberti LM, Walker CLF, Noiman A, Victora C, Black RE. Breastfeeding and the risk for diarrhea morbidity and mortality. BMC public health. 2011;11(3):1–12.
- Hanieh S, Ha TT, Simpson JA, Thuy TT, Khuong NC, Thoang DD, et al. Exclusive breast feeding in early infancy reduces the risk of inpatient admission for diarrhea and suspected pneumonia in rural Vietnam: a prospective cohort study. BMC Public Health. 2015;15(1):1–10.
- Martin CR, Ling P-R, Blackburn GL. Review of infant feeding: key features of breast milk and infant formula. Nutrients. 2016;8(5):279.
- Raheem RA, Binns CW, Chih HJ. Protective effects of breastfeeding against acute respiratory tract infections and diarrhoea: Findings of a cohort study. Journal of paediatrics and child health. 2017;53(3):271–6.
- Nadeem J, Nadeem A, Sarwar MH, Sarwar M. Breastfeeding Benefit from Mom Gives the Gift of a Lifetime to the Baby for Healthy Future. American Journal of Food Science and Health. 2017;3(5):95–101.
- Mulyani S, Subiyanto AA, Anantanyu S, Respati SH, Wiboworini B. Motivation as Mediator between Family Support to the Readiness of Pregnant Woman in Exclusive Breastfeeding. International Journal of Public Health. 2017;6(2):197–202.
- Nankunda J, Tumwine JK, Nankabirwa V, Tylleskär T. “ She would sit with me”: mothers’ experiences of individual peer support for exclusive breastfeeding in Uganda. International breastfeeding journal. 2010;5(1):1–13.
- Wati NH, Muniroh L. Pengaruh Kelompok Pendukung Air Susu Ibu (KP-ASI) Terhadap Perilaku Pemberian ASI Eksklusif dan Status Gizi Bayi 6-12 Bulan. Media Gizi Indonesia. 2018;13(1):33–40.
- Fitriani F, Syahputri VN. Pembentukan KP–ASI (Kelompok Pendukung ASI) Dalam Mewujudkan Kadarsie (Keluarga Sadar ASI Eksklusif) Di Wilayah Kerja Puskesmas Meurebo Kabupaten Aceh Barat. LOGISTA-Jurnal Ilmiah Pengabdian kepada Masyarakat. 2019;3(1):9–16.
- Abeng AT, Hardiyanti L. Pengaruh Kelompok Pendukung ASI (KP-ASI) Terhadap Self Efficacy Ibu Menyusui di Desa Borong Pa’lala Kabupaten Gowa. Bina Generasi: Jurnal Kesehatan. 2020;12(1):42–8.
- Karuniawati N, Masnilawati A, Saputri LH. Pengaruh Niat Ibu, Kondisi Masa Nifas, Kelancaran Produksi ASI terhadap Keputusan untuk Menyusui. Window of Midwifery Journal. 2020;1–13.
- Amalia D, Hardiani RS, Sulistyorini L. Perbedaan Dukungan Nenek dalam Keluarga Extended Family pada Pemberian ASI Eksklusif dan Tidak Eksklusif di Wilayah Kerja Puskesmas Arjasa Kabupaten Jember (The Differences of Grandmother Support in Extended Family on Exclusive and Non-Exclusive Breastfee. Pustaka Kesehatan. 2018;6(1):153–60.
- Nugroho R, Waryana W, Aritonang I. Peran Nenek dalam Peningkatan Cakupan ASI Eksklusif di Desa Bangunjiwo Kasihan Bantul. JURNAL NUTRISIA. 2017;19(1):68–78.
- Thet MM, Khaing EE, Diamond-Smith N, Sudhinaraset M, Oo S, Aung T. Barriers to exclusive breastfeeding in the Ayeyarwaddy Region in Myanmar: Qualitative findings from mothers, grandmothers, and husbands. Appetite. 2016;96:62–9.
- Kapti RE, Rustina Y, Widyatuti W. Efektifitas audiovisual sebagai media penyuluhan kesehatan terhadap peningkatan pengetahuan dan sikap ibu dalam tatalaksana balita dengan diare di dua rumah sakit kota Malang. Jurnal Ilmu Keperawatan: Journal of Nursing Science. 2013;1(1):53–60.
- Imran FA, Hasnah H. Pengaruh Penyuluhan Kesehatan Melalui Media Video Terhadap Peningkatan Pengetahuan Remaja Putri Tentang Dampak Abortus Provokatus Kriminalis Di Kelas X SMAN 2 Gowa. Jurnal Kesehatan. 2020;10(2):61–7.
- Sugiyono. Metode Penelitian Kuantitatif, Kualitatif, dan R&D. Bandung: Alfabeta; 2017.
- Alyensi F. Pembentukan dan Pelaksanaan Kelompok Pendukung ASI (KP ASI) di RW 2 Kelurahan Sialang Sakti Wilayah Kerja PUSKESMAS Rejosari Kecamatan Tenayan Raya Pekanbaru Tahun 2019. Dinamisia: Jurnal Pengabdian Kepada Masyarakat. 2019;3(2):299–304.
- Suryati, Sari, Oktavianto E. Praktek Pemberian Makanan Pendamping ASI Dini Ditinjau dari Peran Nenek. Jurnal Kesehatan Global. 2020;12(4; Desember 2020):757–66.
![]() This work is licensed under a Creative Commons. Attribution-NonCommercial-NoDerivatives 4.0 International License.
This work is licensed under a Creative Commons. Attribution-NonCommercial-NoDerivatives 4.0 International License.
THE EFFECT OF EMOTIONAL DEMONSTRATION METHODS AND VIDEO LEARNING ON HAND WASHING ON KNOWLEDGE AND SKILLS OF HOUSEWIVES
Winda Triana1*, Ervon Verza 1, Pahrur Razi 1
- Department Of Health Promotion, Health Polytechnic of Jambi, Indonesia
* Corresponding author: Winda Triana, Jl. Prof DR GA Siwabessy No.42, Buluran Kenali, Kec. Telanaipura, Kota Jambi, Jambi 36122 Department of Midwifery, Health Polytechnic of Jambi, Indonesia. Orcid : https://orcid.org/0000-0003-0574-7915. Email: trianawinda146@gmail.com
Cita questo articolo
Abstract
Introduction: Efforts to prevent the transmission of infectious diseases through hands can be prevented by washing hands. It is especially emphasized on mothers with toddlers. However, many mothers do not know how to wash their hands using soap correctly and adequately. This study aims to analyze the effect of the emotional demonstration method and video media on how to wash hands on the knowledge and skills of homemakers.
Materials and Methods: This research is a quasi-experimental method, with a two-group design pretest-posttest approach involving 40 participants, conducted in September-October 2020 in Penyengat Olak Village. The research sample was divided into two groups, 20 participants received the emo demo method, and 20 other participants received videos.
Results: The results showed an increase in mothers' knowledge and skills after receiving an education using the emotional demonstration method and video media and statistically showed significant results (<0.05).
Conclusion: Therefore, this educational media is highly recommended as a method of educating the public about good and correct hand washing
Keyword: Wash-hands, Education media, Emotional demonstration, video learning, knowledge, skill
Introduction
The hand is the easiest part of the body as an intermediary for entering germs in the body [1,2]. Therefore, hand hygiene can reduce morbidity and mortality due to infections spread by the fecal-oral route and person-to-person contacts, such as diarrhea and upper respiratory tract infections. Information about this is widely known, but the habit of washing hands with soap is still not optimal [3,4]. Most people already know the importance of washing hands with soap, but there are still few (only 5%) washing hands properly in practice. Most people think that washing hands with water is enough to prevent disease. This perception is undoubtedly wrong because water cannot kill germs/bacteria on hands [5]. Handwashing with proper soap reduces the risk of developing diseases such as diarrhea and can reduce the risk of diarrhea among children five years and under by up to 45% [6].
The lack of public awareness, especially mothers who have pre-school children, in implementing washing hands with soap is the effect of lack of understanding. Therefore, the form of intervention that can improve community compliance, especially homemakers, can be done by giving examples to mothers through demonstrations or showing videos [7]. Emotional Demonstration (Emo Demo) is one of the public education methods developed by the Global Alliance for Improved Nutrition (GAIN) through a new approach that refers to the Behavior Centered Design (BCD) theory [8]. BCD was initiated by the Environmental Health Group of the London School of Hygiene and Tropical Medicine (LSHTM) [9]. BCD was developed based on evolutionary principles and environmental psychology and a way to plan and test imaginative and provocative behavior change interventions. BCD theory holds that behavior can only change in response to something new, challenging, surprising, or interesting. This Emo Demo method uses imaginative and provocative ways to achieve behavior change in public health [10].
Emo Demo is a communication strategy in behavior change that incorporates Behavior Communication Change (BCC), an interactive process between individuals, groups, or communities to develop communication strategies to achieve positive behavior change. Behavior Communication Definition (BCD) is a communication process that utilizes individual psychological constructions involving feelings, needs, and thoughts. It is one of the methods that is being widespread and gaining attention [11]. The success and effectiveness of using Emo Demo have been proven in implementation in several areas. These results encourage the need for the introduction of this method in other areas of health education. The Emo Demo method, in addition to providing health information, also uploads the subject's emotions so that the subject will be encouraged to make behavioral changes [12,13].
Another method that can be used is learning videos on how to wash hands properly and correctly. Video media has become an integral part of both desktop and laptop computers. The latest development of video media as a digital device is its ability to display images and sound simultaneously with a high level of clarity. It is known as picture and sound in high definition format. The rapid development of video technology, both software, and hardware, has given this media its advantages to be used as a learning medium [14].
The learning video program differs from other video programs regarding the objectives to be achieved [15,16]. The instructional video program has more specific objectives when compared to the objectives to be achieved in the entertainment video program. This program is usually proposed to support learning activities for specific audience groups to achieve specific competencies [17,18].
Lack of proper handwashing practice causes bacteria to enter the body quickly because hands are a medium for rapid transfer/exchange. Therefore, this study aims to analyze the effect of the Emotional Demonstration Method and video media on How to Wash Hands on the knowledge and skills of homemakers in Penyengat Olak Village.
Methods
Trial design
This research is a quasi-experimental study using two groups of pretest-posttest design
Participants
This study involved 40 participants who were divided into 2 groups and was carried out in September-October 2020 in Penyengat Olak Village. The study involved housewives who were randomly selected with the inclusion criteria of mothers who had never participated in a study with the same theme, mothers who were under or equal to 35 years of age, while mothers who had hand skin disease were not included.
Intervention
The study sample was divided into two groups, 20 participants received the emo demo method, and another 20 participants received videos. a video on how to wash hands with soap made by the researcher himself, as well as a demonstration on how to wash hands by the researcher.
The research variable is the mother's knowledge and skills. Before the intervention was given, the researcher first measured the level of knowledge and skills of the mother/participant (pre-test), then after the intervention was given the researcher again measured the level of knowledge and skills of the mother. /participant (post-test). The knowledge and skills questionnaires each consist of 15 questions with correct and incorrect answer choices. If the mother answered correctly, she was given a score of 1 and if the answer was wrong, she was given a score of 0. Both of these questionnaires used the Guttman scale.
Researchers have done a lot of research in the health sector and have compiled a lot of questionnaires so that the questionnaires in this study have been prepared by the researchers themselves. Before the research was conducted, the questionnaire was tested on 10 mothers and the results showed that there were 2 questions that had to be replaced because they were invalid.
Outcomes
This study compares the knowledge and skills of mothers in washing hands using soap after being given an intervention in the form of emo demos and videos
Sample size
This study involved 40 participants who were divided into 2 groups
Ethical Consideration
No economic incentives were offered or provided for participation in this study. The study was performed in accordance with the ethical considerations of the Helsinki Declaration. This study obtained ethical feasibility under the Health Research Ethics Commission of the Ministry of Health, Jambi, and registration number: LB.02.06/2/151/2020.
Statistical analysis
Data are presented as numbers and percentages for categorical variables. Continuous data were expressed as mean ± standard deviation (SD) or median with Interquartile Range (IQR). Then proceed with bivariate analysis using the Wilcoxon test. The Wilcoxon test was used to determine the effect of the emo demo and video intervention on knowledge and skills. All tests with p-value (p)<0.05 were considered significant. Statistical analysis was performed using the SPSS version 16.0 application.
Results
The characteristics of respondents in this study include age, education level, and occupation. The following is the frequency distribution of the respondents' characteristics in this study:

Table 1. Frequency Distribution of Respondents Characteristics
In Table 1 it is known that all participants in the study were women, most of the respondents with an age range of 26-30 years were 19 respondents (47.5%). most of the respondents have high school education as many as 17 respondents (42.5%). Most types of work are housewives as many as 21 respondents (52.5%).
Participants' knowledge before and after being given emo demos and videos can be presented in the following table,

Table 2. Frequency Distribution Knowledge about hand washing with soap Before and After intervention
Table 2 shows that participants' level of knowledge before giving the intervention using the emo demo method or video media was higher in the less category. However, after being given the material, participants' level of knowledge increased higher in the "good" category than in the "poor" category.
Participants' skills before and after being given emo demos and videos presented in the following table:

Table 3. Frequency Distribution Skills about hand washing with soap Before and After intervention
Table 3 shows that participants' skills before giving the intervention using the emo demo method or video media were higher in the poor category, but after the intervention, the participants' skills increased higher in the good category than the poor category.
The effects of emo demo and video media interventions on participants' knowledge and skills are presented in the following table:

Table 4. Effects of emo demo and video media interventions on participants' knowledge and skills
Table 4 shows the effect of providing emo demo and video media interventions on participants' knowledge and skills with a p-value < 0.05.
Discussion
Based on the study results, it was known that before the intervention, their level of knowledge and skills on how to wash their hands correctly and adequately was very low. It may be influenced by the low level of education and low access of homemakers to the media; the subordinate role of health workers also influences it in providing information and education to the public.
In line with previous research by Padila [19] at Aisyiyah 1 Kindergarten, Bengkulu City, it was found that before the intervention was given, most of them received the first-star category as many as 27 people (90%), while the number of respondents after the intervention was mostly increased in ability and received the fourth-star category. totaled 23 people (76.7 %). Likewise, Nidiyah's research [20] at RA Raisul Anwar Kedung Rejoso, Kota Anyar District, Probolinggo Regency, found a change in knowledge after obtaining material through demonstration media (emo demo) how to wash hands in 7 steps.
The results of this study reject the null hypothesis regarding the effect of the emotional demonstration method and video media on how to wash hands on the knowledge and skills of homemakers. The result is in line with Nidiyah's research [20] which states that the emo demo method increases children's knowledge, behavior, and habits to wash their hands properly and well. Fermi Avissa [21] also found that the demonstration method was more effective in increasing the knowledge and skills of handwashing in preschool children at Flamboyan Platuk Kindergarten Surabaya. Indah Lastari's research [22] found differences in health education skills through demonstrations and learning videos of the washing skill with the hand-soap method in PAUD. The way of learning through a demonstration method is suitableto be applied on preschool children because this demonstration method makes students receive a clear perception from direct observation. Students obtain practical experiences to develop their proficiency and skill.
Through the demonstration method of hand washing, mothers can directly practice the appropriate intervention that has been given. Skills that are trained with repeated practice will become habitual or automatic [23]. A suitable respondent's knowledge then impacts the actions taken by respondents with good criteria as well. Health education interventions with demonstration and video methods cause homemakers to be skilled in washing their hands to prevent various diseases related to hand hygiene, especially when feeding children when eating [24].
This research is very important to be carried out, especially during the COVID-19 pandemic, where everyone is required to practice hand washing before and after contact with other people, and according to the researcher, washing hands in 7 steps is very effective in preventing transmission of the COVID-19 virus [25–27].
In the current pandemic, the best way to prevent infection is to avoid exposure to the virus that causes it. Prevention of transmission can be done in daily life practices, such as washing hands using soap and running water, the behavior of people who have not practiced clean and healthy lifestyles, especially washing hands with soap can increase the risk of contracting COVID-19. For the community, it is very important to carry out clean and healthy living behavior in the form of washing hands to prevent COVID-19 in the current pandemic era even though COVID-19 can be prevented as recommended by the government to reduce the increase in COVID-19 cases, especially in Indonesia [10].
In general, the results of the study found that the knowledge and skills of respondents increased after the intervention, although there were some respondents that did not change after being given education through emo demo media and video media, this was probably due to their poor memory.
Conclusion
Health education using the demonstration method has been proven to increase knowledge and skills in washing hands, especially for homemakers, so it is highly recommended that health workers provide education on how to wash hands to apply the emo demo and video methods.
Limitations of Study
The limitations of this study include the very limited number of samples, and this study only involves one country, namely Indonesia, so the results may be different when comparing the effects of emo demo and video interventions on mothers in European countries.
Acknowledgement
We would like to thank the director of the Department of Health Promotion, Jambi Health Polytechnic for supporting this research.
Funding statement
This research did not receive any specific grant from funding agencies in the public, commercial, or not for profit sectors.
Competing interests statement
There are no competing interests for this study.
References
- Park J-H, Cheong H-K, Son D-Y, Kim S-U, Ha C-M. Perceptions and behaviors related to hand hygiene for the prevention of H1N1 influenza transmission among Korean university students during the peak pandemic period. BMC infectious diseases. 2010;10(1):1–8.
- Zivich PN, Gancz AS, Aiello AE. Effect of hand hygiene on infectious diseases in the office workplace: A systematic review. American journal of infection control. 2018;46(4):448–55.
- Fesharaki MG, Rahmati-Najarkolaei F, Aghamiri Z, Mohamadian M. Hand-washing compliance rate and the influencing factors. Archives of Clinical Infectious Diseases. 2014;9(4).
- Ataee RA, Ataee MH, Tavana AM, Salesi M. Bacteriological aspects of hand washing: A key for health promotion and infections control. International journal of preventive medicine. 2017;8.
- Tulak GT, Ramadhan S, Musrifah A. Edukasi perilaku cuci tangan pakai sabun pada siswa untuk pencegahan transmisi penyakit. JMM (Jurnal Masyarakat Mandiri). 2020;4(1):37.
- Kemenkes RI. Hasil utama RISKESDAS 2018 [Internet]. Kementerian Kesehatan Badan Penelitian dan Pengembangan Kesehatan. Jakarta; 2018. Available from: https://kesmas.kemkes.go.id/assets/upload/dir_519d41d8cd98f00/files/Hasil-riskesdas-2018_1274.pdf
- Sianipar HF, Sijabat A. Demonstrasi Pentingnya Cuci Tangan Pakai Sabun Untuk Mencegah Pertumbuhan Mikroba. Jurnal Altifani Penelitian Dan Pengabdian Kepada Masyarakat. 2021;1(1):18–21.
- Ridwan M, Ningsih VR, Sari P. Pendekatan Emotional Demonstration Dalam Upaya Peningkatan Praktek Perilaku Hidup Bersih dan Sehat Suku Anak Dalam di Desa Pelakar Jaya. Jurnal Salam Sehat Masyarakat (JSSM). 2020;2(1):42–8.
- Tidwell JB, Chipungu J, Bosomprah S, Aunger R, Curtis V, Chilengi R. Effect of a behaviour change intervention on the quality of peri-urban sanitation in Lusaka, Zambia: a randomised controlled trial. The Lancet Planetary Health. 2019;3(4):e187–96.
- Syafrudin, O, Apriyatmoko, R R. Perbedaan Praktik Cuci Tangan Pakai Sabun Untuk Pencegahan Penyebaran Virus Corona Sebelum dan Sesudah Diberikan Pendidikan Kesehatan Dengan Metode Emotional Demonstration Pada Remaja di Kelurahan Ngempon Kecamatan Bergas. PhD Thesis. Universitas Ngudi Waluyo Universitas Ngudi Waluyo; 2021. S1_010117A089_Artikel - rizal olief.pdf (unw.ac.id)
- Wilbur J, Bright T, Mahon T, Hameed S, Torondel B, Mulwafu W, et al. Developing behaviour change interventions for improving access to health and hygiene for people with disabilities: two case studies from Nepal and Malawi. International journal of environmental research and public health. 2018;15(12):2746.
- Aunger R, Curtis V. Behaviour Centred Design: towards an applied science of behaviour change. Health psychology review. 2016;10(4):425–46.
- Amareta DI, Ardianto ET. Peningkatan praktik cuci tangan pakai sabun pada anak usia sekolah dengan metoda emo demo. Sanitasi: Jurnal Kesehatan Lingkungan. 2017;9(2):88–93.
- Putri SF, Putri DASR, Santi IN. Vidio Animasi Prilaku Hidup Bersih Sehat sebagai Media Pendidikan Masyarakat di Masa New Normal. Jurnal Karinov. 2020;3(3):201–7.
- Rosita A, Dahrizal D, Lestari W. Metode Emo Demo Meningkatkan Pengetahuan dan Sikap Cuci Tangan Pakai Sabun (CTPS) pada Anak Usia Sekolah. Jurnal Keperawatan Raflesia. 2021;3(2):11–22.
- Birawida AB, Selomo M, Mallongi A, Adilah D, Suriah S. Effectiveness of Emotional Demonstration Method in Counseling Handwashing with Soap in Small Islands of Makassar. 2019. http://eprints.eudl.eu/id/eprint/6871/1/eai.26-10-2018.2288563.pdf
- Kristanto A. Pengembangan Model Media Video Pembelajaran Mata Kuliah Pengembangan Media Video/Tv Program Studi Teknologi Pendidikan Fakultas Ilmu Pendidikan Universitas Negeri Surabaya. PhD Thesis. UNS (Sebelas Maret University); 2011. https://digilib.uns.ac.id/dokumen/download/18119/NDQzMDk=/Pengembangan-Model-Media-Video-Pembelajaran-Mata-Kuliah-Pengembangan-Media-VideoTv-Program-Studi-Teknologi-Pendidikan-Fakultas-Ilmu-Pendidikan-Universitas-Negeri-Surabaya-Binder1.pdf
- Falahudin I. Pemanfaatan media dalam pembelajaran. Jurnal Lingkar Widyaiswara. 2014;1(4):104–17.
- Padila P, Andri J, Harsismanto J, Andrianto MB, Admaja RD. Pembelajaran Cuci Tangan Tujuh Langkah melalui Metode Demonstrasi pada Anak Usia Dini. Journal of Telenursing (JOTING). 2020;2(2):112–8.
- Wahid H. Metode Emo Demo dan Metode Bermain Puzzle Terhadap Cara Mencuci Tangan Pada Anak Prasekolah. 2019;7(1):35–44.
- Avissa F, Nursalam N, Ulfiana E. Efektivitas Pendidikan Kesehatan Metode Demonstrasi Dan Metode Ceramah Dengan Media Booklet Terhadap Perubahan Pengetahuan Dan Tindakan Mencuci Tangan Pada Anak Prasekolah. Fundamental and Management Nursing Journal. 2012;1(1):59–66.
- Lestari I, Krisnanto PD, Fitriana LB. The Difference of Health Education Through Demonstration and Singing Video Methods on Hand-Washing Soap Skill in Preschool Children. Jurnal Keperawatan Respati Yogyakarta. 2020;7(2):72–6.
- Bowen A, Ma H, Ou J, Billhimer W, Long T, Mintz E, et al. A cluster-randomized controlled trial evaluating the effect of a handwashing-promotion program in Chinese primary schools. The American journal of tropical medicine and hygiene. 2007;76(6):1166–73.
- Ali MM, Verrill L, Zhang Y. Self-reported hand washing behaviors and foodborne illness: a propensity score matching approach. Journal of Food Protection. 2014;77(3):352–8.
- Wardhani DK, Susilorini MR, Angghita LJ, Ismail A. Edukasi Pencegahan Penularan COVID-19 Pada Anak Usia Dini Melalui Media Pembelajaran Audio Visual. Jurnal Abdidas. 2020;1(3):131–6.
- Karo MB. Perilaku hidup bersih dan sehat (PHBS) strategi pencegahan penyebaran Virus Covid-19. In: Prosiding Seminar Nasional Hardiknas. 2020. vol. 1, pp. 1–4.
- Sinaga LRV, Munthe SA, Bangun HA. Sosialisasi perilaku cuci tangan pakai sabun di desa sawo sebagai-bentuk kepedulian terhadap masyarakat ditengah mewabahnya virus covid-19. Jurnal Abdimas Mutiara. 2020;1(2):19–28.
![]() This work is licensed under a Creative Commons
This work is licensed under a Creative Commons
Attribution-NonCommercial-NoDerivatives 4.0 International License.
THE EFFECTIVENESS OF THE DEMONSTRATION METHOD AND AUDIO-VISUAL METHOD ON ADOLESCENT KNOWLEDGE ABOUT BREAST SELF-EXAMINATION
Titik Hindriati*, Nurmisih, Diniyati, Rosmaria
Department of Midwifery, Health Polytechnic of Jambi, Indonesia
* Corresponding author: Titik Hindriati, Department of Midwifery, Health Polytechnic of Jambi, Indonesia, Jalan Prof DR GA Siwabessy No.42. Buluran Kenali, Kec. Telanaipura, Kota Jambi, 36122, Phone : +62 852-6970-1226, E-mail: titikpoltekkes@gmail.com
Cita questo articolo
Abstract
Introduction: Breast cancer is the most frequent type of cancer in women, and it is one of the major causes of mortality. Efforts should be made to prevent breast cancer by using the breast self-examination (BSE) method of early diagnosis. This study aims to determine the effectiveness of the demonstration and audio visual methods on adolescent knowledge about breast self-examination at SMA Pertiwi 1 Jambi City, Indonesia.
Methods. This study is a quasi-experimental study using a two-group pretest-posttest design at the private high school Pertiwi 1 Jambi City, involving 122 participants divided into two groups. Group 1 consisted of 61 participants given BSE material by demonstration, while group 2 consisted of 61 participants given material using audio-visual media. Data processing in this study used univariate and bivariate analysis, and the statistical test used was the Wilcoxon test.
Results. The results showed that there was an increase in students' knowledge about BSE after the demonstration with p-value < 0.0001, and displayed audio-visually with p-value < 0.0001.
Conslusion: demonstration and audiovisual methods proved effective in increasing adolescent knowledge about breast self-examination at at SMA Pertiwi 1 Jambi City, Indonesia.
Keywords: breast self-examination, knowledge, cancer, demonstration, audio visual
Introduction
The breast is one of the crucial organs for women because apart from being a tool for breastfeeding, it is also a symbol of beauty [1–3]. Because its vital existence makes a woman feel worried if the breast is abnormal; the most feared abnormality is malignancy or cancer [4]. Breast cancer is a condition in which cells have lost their usual control and mechanism, resulting in irregular, fast and uncontrolled growth in breast tissue [5,6].
According to the Breast Cancer Management Organization and the World Health Organization, by 2030, cancer in the world will increase 300%, and the majority occur in developing countries, including Indonesia [7].
Breast cancer is second cancer with the highest prevalence compared to other cancer in Indonesia in 2013, namely breast cancer, by 0.5% or around 61,682 patients in Indonesia. The prevalence of breast cancer incidence in Jambi Province was approximately 0.6% or about 977 cases in 2013 [8].
Based on data from the Jambi Provincial Health Office, in 2014, the number of patients who have breast cancer reached 38 (55%) people, and in 2015 the number of cases of breast cancer patients was 15 (22%) people. The age group in patients who have breast cancer starts from 14 years to 64 years. The data shows that the age at which breast cancer is susceptible is from the age of 24 years to the age of 64 years, and it occurs mainly in women. In 2016 it was found that breast cancer patients were only 14 years old; this could make it possible that all women can suffer breast cancer, both married and unmarried [9].
Only a tiny proportion of women perform the breast self-examination (BSE) [10]. It is estimated that only 25% to 30% of women perform regular monthly breast self-exams. Whereas, the level of sensitivity to detect breast cancer is about 20-30%. Almost 85% of lumps are found by sufferers independently through proper examination [11]. Breast self-examination is the first step. If breast cancer can be detected early and treated appropriately, the cure rate will be higher (80-90%). 85% of sufferers detect breast abnormalities [8]. If this examination becomes a routine and regular habit, it can detect more breast cancer early. Although this method is cheap, safe, repeatable and straightforward, only about 15-30% of women use it [12–14].
Breast exam (BSE) can be applied to young women who experience change physical and secondary sexual development that is, puberty breast enlargement occurs between the ages of 12-13 years [15]. Benefits of breast examination alone on teenage girls for early detection of tumors or lump in the breast [16–18].
Better breast self-examination carried out during menstruation, i.e 7-10 days from the first day of menstruation with consideration at that time the influence of the hormones estrogen and Progesterone is very low and at the same time it’s deep breast gland tissue no edema or not swell so much easier feel for tumors or abnormalities [19,20].
The results of the interviews in the initial survey at the Pertiwi 1 Private High School in Jambi City to 8 students stated that they did not know about BSE. Allegedly due to lack of information on reproductive health, especially BSE. One method of providing information is by delivering a demonstration using audio-visual.
This study aims to determine the effectiveness of the demonstration and audio visual methods on adolescent knowledge about BSE at SMA Pertiwi 1 Jambi City, Indonesia.
Methods
Design
This study is a quasi-experimental study using a two-group pretest-posttest design
Participants
The study was conducted at Pertiwi 1 Private High School Jambi City involving 122 female students with inclusion criteria ranging from 16-19 years of age, while adolescents under 16 years of age and not present at the time of the study were not included in the study.
Intervention
51 years old researcher, works as a lecturer at one of the universities in Indonesia, actively conducts research and writes a special book on midwifery. Group 1 consisted of 61 female participants (F) with an age range of 16-19 years, who were given BSE material by means of a demonstration, while group 2 consisted of 61 participants who were given material using audio-visual media. Before the BSE material, students’ knowledge was first measured using a questionnaire, then after the material was given, it was continued with an evaluation of the students’ level of knowledge about BSE (post-test).
The knowledge questionnaire consisted of 20 questions containing students’ knowledge about breast self-examination. If students answer correctly, they are given a score of 1, while if students answer incorrectly, they are given a score of 0. The objective criteria for the knowledge variable are good and bad. Good, if the total score of student answers is 11-20, while the criteria is less, if the total score of student answers is 1-10. The questionnaire used has been validated and declared valid and reliable. Determine the validity of the questions using the product moment test. If the coefficient between the items and the total items is equal to or above 0.3 then the item is declared valid, but if the correlation value is below 0.3 then the item is declared invalid. While the correlation is 0.7, it is said that the item provides a sufficient level of reliability, on the contrary, if the correlation value is below 0.7, it is said that the item is less reliable. Determining reliable question items using the Spearman Rho test [21]. The instrument test was carried out on 15 adolescents with the results, of the 20 submitted there were 4 questions that had a validity index value <0.3 so they had to be corrected and 3 questions had a correlation below 0.7 so they had to be corrected again.
Questionnaires were distributed to students at Pertiwi 1 Private High School Jambi City, Indonesia. After the data collection was carried out by the researcher, the researcher then compiled the data, processing and analyzing the data.
Outcomes
To determine the effectiveness of learning using demonstration and audio visual methods
Sample size
This study involved 122 participants who were divided into two groups defined in random way, and namely group 1 and group 2 both composed of 61 female participants.
Ethical Consideration
No economic incentives were offered or provided for participation in this study. The study was performed in accordance with the ethical considerations of the Helsinki Declaration. This study obtained ethical feasibility under the Health Research Ethics Commission of the Ministry of Health, Jambi, and registration number: LB.03.02./3.5/130/2021.
Statistical analysis
Data are presented as numbers and percentages for categorical variables. Continuous data were expressed as mean ± standard deviation (SD) or median with Inter Quartile Range (IQR). Then proceed with bivariate analysis using the Wilcoxon test. The Wilcoxon test was used to determine the effect of counselling using breastfeeding video on the knowledge of breast milk supporting group. All tests with p-value (p)<0.05 were considered significant. Statistical analysis was performed using the SPSS version 16.0 application.
Results
As for the characteristics of the respondents can be presented in the following table :
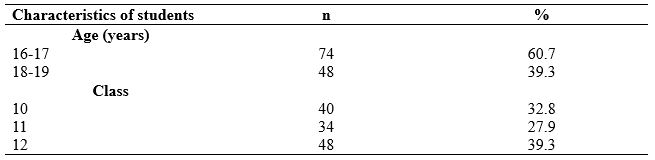
Table 1. Characteristics of research respondents in high school
The highest respondent's age characteristic is the range of 16-17 years as much as 60.7%, then the most students occupy class 12
Students' knowledge about breast self-examination before and after giving the material using demonstration and audio-visual methods is presented in the following table:
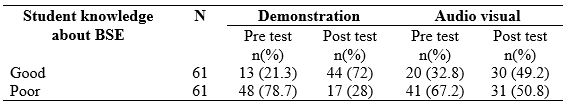
Table 2. Frequency distribution of students' knowledge about BSE
Table 2, shows that students' knowledge about breast self-examination before giving the demonstration group was higher in the poor than in the excellent category. After the demonstration, students' learning was higher in the superb class than in the fewer categories. Meanwhile, students' knowledge before audio-visual material was higher in the lower category than the excellent category. After giving the material, the same changes occurred for both classes.
The effect of giving the method using demonstration and audio-visual techniques on students' knowledge about breast self-examination is presented in the following table:
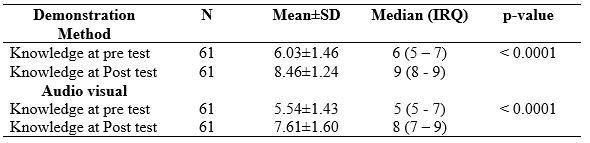
Table 3. The effect of giving material using demonstration and audio-visual methods on students' knowledge
Table 3 shows the increase in students' knowledge about breast self-examination after demonstration with p-value < 0.0001. as well as shown audio visually with a p-value < 0.0001.
Discussion
Prior to the application of the demonstration method and the audio-visual group, data was obtained that a small number of respondents had good knowledge of BSE. Meanwhile, more than half of the respondents have poor knowledge. This is because students have never received information about breast cancer and BSE examinations at school.
After giving the material using the demonstration method, there was an increase in students' knowledge about BSE. Most of the respondents had good knowledge about understanding, examination, standard nipple colour and the purpose of BSE, and only a small number of respondents had less knowledge about BSE.
After giving the material using audio-visual media, there was an increase in respondents' knowledge after the audio-visual about BSE; that is, most of the respondents had good knowledge. Using video media has a more significant impact on health education; it relies on hearing and vision from the target; it is interesting; the messages are delivered quickly and efficiently and can develop the mind and develop the imagination of young women. The video can clarify the pictures and the steps of the importance of the BSE examination. In the process of giving it, the respondent not only hears the sound, but the respondent will see directly and the steps of the breast self-examination.
Based on the results of research by [22], the demonstration method through demonstration activities has proven to be more effective in increasing young women's knowledge to perform BSE techniques. It is also supported by research by [23] that there is a relationship between knowledge, attitudes and BSE actions through demonstrations to detect breast cancer early in female students at the Faculty of Public Health. This result is also supported by the research of [13], which suggests that the demonstration method is proven to be more effective in increasing knowledge through learning media on BSE skills. A similar thing was reported by [13], who researched SMA 1 Sumber, Indonesia students who found an increase in student's knowledge after being given information using demonstrations and media in the form of videos.
The counselling was carried out to increase the respondent's knowledge about BSE. There was material about BSE in the counselling, which was packaged in an attractive video format and demonstrated by conducting a demonstration to obtain information directly. In addition, in the counselling process, answers are also held so that respondents who do not understand the material about BSE can now ask questions, and the respondents can understand the information [18,24,25].
The current research is to improve health education about reproductive health, especially breast health of a young woman in the research location. Knowledge of breast self-examination (BSE) is essential to be known and understood by a young woman [26].
Conclusion
The use of demonstration methods and audio-visual media in learning is considered adequate to increase students' knowledge about breast self-examination for students of SMAN Pertiwi 1 Jambi city. It is hoped that the high school will provide information about BSE in adolescent girls to detect early symptoms of breast cancer.
Limitations of Study
The limitations of this study include, in addition to the relatively small number of participants, the type of quasi-experimental research does not do randomization
Acknowledgement
We would like to express our gratitude to the director of the Midwifery Department of Jambi health polytechnic who has supported this research.
Funding statement
This research did not receive any specific grant from funding agencies in the public, commercial, or not for profit sectors.
Competing interests statement
There are no competing interests for this study.
References
- Sukartini T, Sari YIP. Women with breast cancer living with one breast after a mastectomy. Central European Journal of Nursing and Midwifery. 2021;12(2):366–75.
- Guilford K, McKinley E, Turner L. Breast cancer knowledge, beliefs, and screening behaviors of college women: application of the health belief model. American Journal of Health Education. 2017;48(4):256–63.
- Chee HL, Rashidah S, Shamsuddin K, Intan O. Factors related to the practice of breast self examination (BSE) and Pap smear screening among Malaysian women workers in selected electronics factories. BMC women’s health. 2003;3(1):1–11.
- Filippi MK, Ndikum-Moffor F, Braiuca SL, Goodman T, Hammer TL, James AS, et al. Breast cancer screening perceptions among American Indian women under age 40. Journal of Cancer Education. 2013;28(3):535–40.
- Yadav AR, Mohite SK. Cancer-A silent killer: An overview. Asian Journal of Pharmaceutical Research. 2020;10(3):213–6.
- Madkhali NA, Santin O, Noble H, Reid J. Understanding breast health awareness in an Arabic culture: qualitative study protocol. Journal of advanced nursing. 2016;72(9):2226–37.
- Setiyaningrum KD, Maliya A. Hubungan Dukungan Keluarga terhadap Kualitas Hidup Pasien Kanker Payudara yang Menjalani Kemoterapi di Rumah Sakit Umum Daerah dr. Moewardi Surakarta. Universitas Muhammadiyah Surakarta; 2018.
- Kemenkes RI. Hasil utama RISKESDAS 2018 [Internet]. Kementerian Kesehatan Badan Penelitian dan Pengembangan Kesehatan. Jakarta; 2018. Available from: https://kesmas.kemkes.go.id/assets/upload/dir_519d41d8cd98f00/files/Hasil-riskesdas-2018_1274.pdf
- Dinkes Kota Jambi. Profil Kesehatan Kota Jambi. Jambi; 2018.
- Mahfouz AA, Hassanein MHA, Nahar S, Farheen A, Gaballah II, Mohamed A, et al. Breast cancer knowledge and related behaviors among women in Abha city, southwestern Saudi Arabia. Journal of Cancer Education. 2013;28(3):516–20.
- Artanty NW. Lima Menit Kenali Payudara. CV Andi: Yogyakarta. 2011.
- Olfah Y, Mendri NK, Badi’ah A. Kanker Payudara dan SADARI. Jakarta: Nuha Medika. 2013;
- Aeni N, Yuhandini DS. Pengaruh Pendidikan Kesehatan dengan media video dan metode demonstrasi terhadap pengetahuan sadari. Care: Jurnal Ilmiah Ilmu Kesehatan. 2018;6(2):162–74.
- Olii N, Abdul NA. The Influence of Booklets and Videos on the Ability to Practice Breast Self Examination in Students of High School 4 Gorontalo. Indian Journal of Forensic Medicine & Toxicology. 2021;15(2).
- Wulandari F, Ayu SM. Hubungan tingkat pengetahuan dan sikap dengan perilaku pemeriksaan payudara sendiri (sadari) mahasiswi. In: Prosiding Seminar Nasional IKAKESMADA “Peran Tenaga Kesehatan dalam Pelaksanaan SDGs.” Fakultas Kesehatan Masyarakat Universitas Ahmad Dahlan; 2017. p. 137–44.
- Harford JB. Breast-cancer early detection in low-income and middle-income countries: do what you can versus one size fits all. The lancet oncology. 2011;12(3):306–12.
- Weiss NS. Breast cancer mortality in relation to clinical breast examination and breast self‐examination. The Breast Journal. 2003;9:S86–9.
- Noer RM, Purba NH, Suryadartiwi W. Edukasi Sadari (Pemeriksaan Payudara Sendiri) Sebagai Deteksi Dini Pencegahan Kanker Payudara Pada Remaja Putri. JMM (Jurnal Masyarakat Mandiri). 2021;5(2):651–62.
- McPherson K, Steel C, Dixon JM. ABC of breast diseases: breast cancer—epidemiology, risk factors, and genetics. BMJ: British Medical Journal. 2000;321(7261):624.
- Monticciolo DL, Newell MS, Moy L, Niell B, Monsees B, Sickles EA. Breast cancer screening in women at higher-than-average risk: recommendations from the ACR. Journal of the American College of Radiology. 2018;15(3):408–14.
- Sugiyono. Metode Penelitian Kuantitatif, Kualitatif dan R&D. Bandung: PT Alfabet; 2016.
- Handayani S, Sudarmiati S. Pengetahuan remaja putri tentang cara melakukan SADARI. Jurnal Keperawatan Diponegoro. 2012;1(1):93–100.
- Amila A, Sinuraya E, Gulo ARB. Edukasi Sadari (Pemeriksaan Payudara Sendiri) Untuk Deteksi Dini Kanker Payudara Pada Siswi SMA Medan. Jurnal Abdimas Mutiara. 2020;1(2):29–40.
- Sadoh AE, Osime C, Nwaneri DU, Ogboghodo BC, Eregie CO, Oviawe O. Improving knowledge about breast cancer and breast self examination in female Nigerian adolescents using peer education: a pre-post interventional study. BMC women’s health. 2021;21(1):1–9.
- Yuslikhah AM, Wijayanti Y, Rustiana ER. the Effectiveness of Health Education Method on Early Detection Carcinoma Mammae in Teenage Girls of Madrasah Aliyah in Mijen Sub-District. Public Health Perspective Journal. 2019;4(2).
- Dadzi R, Adam A. Assessment of knowledge and practice of breast self-examination among reproductive age women in Akatsi South district of Volta region of Ghana. PloS one. 2019;14(12):e0226925.
![]() This work is licensed under a Creative Commons
This work is licensed under a Creative Commons
Attribution-NonCommercial-NoDerivatives 4.0 International License.
THE EFFECT OF ACUPRESSUR THERAPY IN REDUCING NAUSEA AND VOMITING PREGNANT WOMEN TRIMESTER I : QUASI-EXPERIMENTAL STUDY
Suryani, Ika Murtiyarini*, Yuli Suryanti, Misnanda
Department of Midwifery, Health Polytechnic of Jambi, Indonesia
* Corresponding author: Ika Murtiyarini, Department of Midwifery, Health Polytechnic of Jambi, Indonesia, Jalan Prof DR GA Siwabessy No.42. Buluran Kenali, Kec. Telanaipura, Kota Jambi, .36122. E-mail: ikamurtiyarini.poltekkes@gmail.com
Cita questo articolo
Abstract
Introduction. Nausea and vomiting are the most common symptoms experienced by pregnant women in the first trimester, and these symptoms are experienced by 70-85% of women. Nausea and vomiting are often experienced by pregnant women, especially in the first trimester, affecting about 50-80% of pregnant women. Management of nausea and vomiting in pregnancy consists of pharmacological and non-pharmacological. This study aims to analyze the effect of acupressure therapy on nausea and vomiting.
Methods. This type of research is a quasi-experimental design using a two-group pre-post design involving 30 first trimester pregnant women who experience nausea and vomiting selected by purposive sampling. The criteria for the participants were gestational age at 10-16 weeks and maternal age at 20-35 years (productive age), while mothers taking nausea and vomiting drugs were excluded from this study. Data analysis used the Wilcoxon test and Mann-Withney test.
Results. a significant decrease group with p-value <0.05. Based on the Mann Whitney test, it was found that the p-value for the pre in the frequency of moderat nausea and vomiting scores before and after acupressure in the intervention -test (<0.0001), and the post-test was 0.55, post test scores showed no difference between the two study groups.
Conslusion. The study shows encouraging signs about reducing the frequency of nausea and vomiting in first-trimester pregnant women, so this therapy can be used as an alternative intervention for pregnant women who experience nausea and vomiting.
Keywords: Acupressure, Nausea Vomiting, Pregnant Women, Non-pharmacological Therapy
Introduction
Pregnancy is fertilization or joining of spermatozoa and ovum, so nidation or implantation occurs [1]. According to the international calendar, from the time of fertilization until the birth of the baby, pregnancy will generally last 40 weeks or ten months [2,3]. The signs and symptoms of pregnancy include nausea without vomiting, micturition disorders, and fatigue [4]. Nausea occurs due to increased hormone estrogen and chorionic gonadotropin hormone (HCG) in the serum [5]. The physiological changes of this hormone increase are not yet apparent, perhaps due to stimulation of the central nervous system or gastric emptying that is not optimal [6]. A study in Indonesia revealed that pregnant women with nausea and vomiting reached 14.8% of all pregnancies. Complaints of nausea and vomiting occur in 60-80% of primigravida and 40-60% of multiple pregnancies [7]. The coverage of First Prenatal Visits in Jambi Province reached 10-15% of the 73,096 pregnant women in 2018 [8]. According to the Jambi City Health Office data, the number of pregnant women who had a First Prenatal Visit in Jambi City was 76,681 (74.9%) [8]. If nausea and vomiting in pregnancy do not treat immediately, it will impair fetal growth, fetal death and congenital abnormalities. The consequences for the mother are dehydration, acid-base balance disorders, and potassium deficiency [9]. Management of nausea and vomiting in pregnancy consists of pharmacological and non-pharmacological. Diet settings, emotional support and acupressure are options in non-pharmacological therapy which effective as an intervention to treat nausea [10]. Acupressure is a healing technique by pressing and massaging certain body parts to re-activate the energy balance in the mother's body due to adaptation to changes during pregnancy. Acupressure, especially at the pericardial point, can achieve balance in the mother's body [11]. In treating nausea and vomiting in pregnancy, acupressure carries out three fingers above the middle of the inner wrist and four fingers below the kneecap on the outer edge of the shinbone [12]. Acupressure is found to be effective in reducing nausea and vomiting through the mechanism of increasing beta endorphins. This substance is one of the natural anti-emetics that can reduce the vomiting stimulus in the CTZ (Chemoreceptor Trigger Zone) and the vomiting center which in turn can reduce nausea and vomiting [12].
A meta-analysis of acupuncture in pediatric tonsillectomy revealed that the number of patients with Postoperative Nausea and Vomiting was significantly reduced with acupuncture compared to the control group, with a risk ratio of 0.77 (95% confidence interval: 0.63–0.94, p < 0.05) [13]. A study in the Maternity and Child Hospital in Istanbul reported that acupressure would appear to be effective in symptom control, and alleviation and placebo effects in reducing the symptoms of nausea and vomiting during pregnancy [14]. Previous studies have not mapped the characteristics of nausea and vomiting severity in pregnant women. Therefore, in this study, we analyzed the effect of acupressure therapy in reducing moderate nausea and vomiting in the working area of the Talang Banjar Health Center, Jambi City.
Methods
Design
This study uses a two group with pretest-posttest design where the design provides a pretest before being treated and a posttest after being treated in each group [15]. This quasy-experimental study used two group with pretest-posttest design.
Participants
The criteria for the participants were gestational age at 10-16 weeks and maternal age at 20-35 years (productive age), while mothers taking nausea and vomiting drugs were excluded from this study.
Intervention
Acupressure therapy performs for three days for each pregnant woman. First, measurements of maternal nausea and vomiting provide, then acupressure therapy was performed. Massage performed on three fingers above the wrist in a circular motion and on four fingers below the kneecap on the outer edge of the shin, given emphasis as much as 30 times. This therapy conducts for 5 minutes every morning. At the end of the 4th-day therapy session, maternal nausea and vomiting measured. The interpretation of the results of the PUQE measurement is severe, if the score is ≥13, moderate if the score is 7-12, and mild if the score is ≤6. The measurement of nausea and vomiting used Pregnancy Unique Quantification of Emesis and Nausea (PUQE). The Pregnancy-Unique Quantification of Emesis and Nausea (PUQE) scoring system instrument is a research instrument developed by Koren et al. [16] and validated by Koren et al. [17].
Outcomes
The outcome of the study is that pregnant women are expected to show a decrease in the frequency of nausea and vomiting
Sample size
Involving 30 first trimester pregnant women who were divided into 2 groups, 15 pregnant women experienced moderate nausea and vomiting (score 7-10) and 15 pregnant women experienced moderate nausea and vomiting (score 10-12).
Randomisation (Sequence generation, Allocation etc)
The selection of research samples was carried out at simple random
Blinding
The included samples were selected blindly
Ethical Consideration
No economic incentives were offered or provided for participation in this study. The study was performed in accordance with the ethical considerations of the Helsinki Declaration. This study obtained ethical feasibility under the Health Research Ethics Commission of the Ministry of Health, Jambi, and registration number: LB.02.06/2/54/2020.
Statistical analysis
There are 2 data analyses used, namely univariate analysis to describe the characteristics of pregnant women (age, education level, and occupation of pregnant women) and a description of the frequency of nausea and vomiting before and after the intervention. Data are presented as numbers and percentages for categorical variables. Continuous data are expressed as the mean ± standard deviation (SD), or median with Interquartile Range (IQR). Then proceed with bivariate analysis using the Wilcoxon test and the Mann Whitney test. The Wilcoxon test was used to determine the effect of acupressure therapy on reducing nausea and vomiting in each study group, while the Mann Whitney test was used to determine differences in nausea and vomiting between the two study groups. All tests with p-value (p)<0.05 were considered significant. Statistical analysis performed using the SPSS app version 16.0.
Results
The characteristics of respondents in this study include age, education level, occupation, gestational age, and parity.
The following is a table of the frequency distribution of the characteristics of the respondents in this study:

Table 1. Frequency Distribution of Respondents' Characteristics
Table 1 shows that most of the respondents in Group 2 aged 20-30 years were 14 people (93.3%), and respondents aged 30-40 years were 1 (6.7%) people. The majority of respondents in group 1, as many as 13 (86.7%), have high education, namely high school graduates or more (college), and as many as two people (13.3%) have low education (< high school). At work, most of the respondents in Group 1 are housewives; 9 (60%) and 1 (6.7%) respondents were traders and entrepreneurs. At gestational age, most of the respondents in group 1 had a gestational age of 9-12 weeks, namely 9 (60%), and as many as 6 (40%) respondents had a gestational age of 5-8 weeks. In the parity aspect, some respondents in group 2 had parity > 1, namely 12 (80%) respondents and 3 (20%) had parity 1.
The results of measuring nausea and vomiting in the Group 1 and Group 2 prior to acupressure therapy using the PUQE scale can be seen in the following table:

Table 2. Results of the PUQE Scale for Respondents in the Group 1 and Group 2 Before and After Acupressure in First Trimester Pregnant Women
Table 2 shows, Group 1, as many as 6 (40%) respondents with a score of 9, 4 (26.7%) respondents had a score of 10, 3 (20%) respondents had a score of 7, and 2 (13.3%) respondents had score 8. After acupressure therapy, the nausea and vomiting score scale decreased to 13 (86.7%) in the last 24 hours experiencing nausea and vomiting with a score of 6 (mild nausea and vomiting), and as many as 2 (13.3%) respondents in The last 24 hours experienced vomiting with a score of 5 (mild nausea and vomiting). Group 2, 9 (60%) respondents experienced nausea and vomiting with a score of 10 in the last 24 hours, 5 (33.3%) respondents experienced nausea and vomiting in the previous 24 hours with a score of 11, and 1 (6.7%) respondents experienced nausea with a score of 12 in the last 24 hours. After doing acupressure therapy, 14 (93.3%) respondents got a PUQE score of 6 and 1 (6.7%) respondents got a score of 5.
The condition of nausea and vomiting before and after the acupressure technique in group 1 and Group 2 can be seen in the table below:

Table 3. Frequency distribution of Group 1 and Group 2 before and after acupressure therapies
Table 3 shows a significant decrease in the frequency of nausea and vomiting scores in both groups before and after acupressure in the intervention group with p-value <0.05. Based on the Mann Whitney test, it was found that the p-value for the pre-test (<0.0001), and the post-test was 0.55, the post-test value showed no difference between the two research groups.
Discussion
The result of study showed that patients in the treatment group, who were given acupressure therapy after day 3, had less severity of nausea, frequency of vomiting and the level of intensity of discomfort felt from nausea, when compared to the condition of nausea and vomiting on the first day before treatment. Previous research conducted by O’Brien B [18], Werntoft E [19], and Tara F [20] showed that have reported a reduction in the intensity of nausea and vomiting discomfort during the first trimester of pregnancy.
In group 1, before giving acupressure therapy, the average value of nausea and vomiting was 8.73 and it decreased very significantly after giving acupressure therapy to 5.87, meaning that there was a decrease of 2.86 points. The same thing was shown by group 2 after acupressure therapy experienced a significant decrease of 4.57 points. The results of this study indicate that acupressure therapy is very effective in reducing nausea and vomiting, especially for pregnant women in the 1st trimester.
The results of the current study have shown the ability of acupressure to significantly reduce acute nausea and vomiting scores in respondents who experience acute nausea and vomiting, so it can be concluded that acupressure is an effective intervention in reducing nausea in pregnant women. This finding is in accordance with previous findings which stated that acupressure is one of the appropriate measures in the management of nausea and vomiting due to pregnancy [11].
In a study conducted in Turkey by Gürkan ÖC [14], it was shown that in subjects undergoing at Neiguan (PC6) acupoint acupressure between days 4–6, there was less severity of nausea, frequency of vomiting, and feeling of discomfort after nausea. Another study by Markose MT [21] showed that the frequency of vomiting, nausea, and retching, as well as the discomfort caused by nausea and vomiting were significantly lower in the at Neiguan (PC6) acupoint pressure treatment group than in the control group under drug therapy. In line with the research of Mojgan Naeimi Rad et al [22] involving 80 first trimester pregnant women concluded that acupressure on KID21 point is more effective than sham acupressure in reduction of nausea and vomiting in pregnancy.
15 respondents experienced nausea and vomiting at a score of 10-12 and after being given acupressure, the score decreased to 5-6, from 15 respondents experienced nausea and vomiting a score of 7-10, after receiving acupressure therapy, the score for nausea and vomiting decreased to a score of 5-6. In group 1, the decrease was lower than in group 2. The cause could be due to stress factors, so that even though acupressure therapy has been given, the frequency of nausea and vomiting can increase again [23]. Psychological factors are factors that are triggered from the surrounding environment such as work or family problems that make pregnant women stressed, because stress can interfere with the hormonal system of the gastric organs in controlling gastric acid secretion so that stomach acid can increase and cause nausea and vomiting [24,25].
In line with the research of Pirimoglu ZM, et al [26] that pregnant women suffering from hyperemesis gravidarum were identified as 80% afraid of losing their jobs, afraid of getting pregnant again in the future, experiencing psychiatric symptoms such as depression and anxiety. Based on this research, that acupressure therapy is ideally applied to mothers who suffer from emesis or nausea and vomiting on a mild or moderate scale, and as an alternative therapy in reducing nausea and vomiting, especially pregnant women who have a fear of the side effects of medical treatment therapy, such as doubts of the effect of the drug on fetal defects in the womb.
The results of data analysis using the Mann Whitney test to determine differences in nausea and vomiting before (pre) acupressure therapy in the two study groups and differences in nausea and vomiting after (post) acupressure therapy in the two study groups showed that the pre-test of the two study groups had a p-value of 0.0001, which means that there is a difference in the point of nausea and vomiting of the two study groups before acupressure therapy, but after acupressure therapy there is no difference in the scale of nausea and vomiting in the two study groups (p-value = 0.55). there was no significant difference based on the results of statistical data analysis in the two groups after acupressure therapy was most likely strongly influenced by the same type of intervention given to both study groups.
The main limitation of this study is the absence of controlling for other factors that can affect the frequency of nausea and vomiting such as stress, and the type of food consumed by pregnant women, so it is very likely that the variable data measured are less accurate.
Conclusion
Acupressure therapy is the choice of pregnant women and is more enjoyable than medical treatment because in addition to being easy and cheap, it is also effective in reducing the frequency of nausea and vomiting in first trimester pregnant women.
Limitations
The limitations of this study include a very small sample and the pattern or type of food of pregnant women that was not controlled during the study
Acknowledgement
We would like to express our gratitude to the director of the Midwifery Department of Jambi health polytechnic who has supported this research.
Funding statement
This research did not receive any specific grant from funding agencies in the public, commercial, or not for profit sectors.
Competing interests statement
There are no competing interests for this study.
References
- Retnowati Y, Yulianti I, Ariyanti R. Pengantar Asuhan Kehamilan. Thesis Commons; 2020.
- Tyastuti S. Asuhan kebidanan kehamilan. Pusdik SDM Kesehatan; 2016.
- Hatini EE. Asuhan Kebidanan Kehamilan. WINEKA MEDIA; 2019.
- Bai G, Korfage IJ, Groen EH, Jaddoe VW V, Mautner E, Raat H. Associations between nausea, vomiting, fatigue and health-related quality of life of women in early pregnancy: the generation R study. PloS one. 2016;11(11):e0166133.
- Horan C. Physiologic changes. In: Obstetric Evidence-Based Guidelines. CRC Press; 2012. p. 47–60.
- Chortatos A. Nausea and vomiting in pregnancy and the impact upon dietary intakes and birth outcomes–a study performed in the Norwegian Mother and child cohort study. 2011.
- Kemenkes RI. Hasil utama RISKESDAS 2018. Jakarta: Kementerian Kesehatan Badan Penelitian dan Pengembangan Kesehatan. Jakarta; 2018.
- Dinkes Kota Jambi. Profil Kesehatan Kota Jambi. Jambi; 2018.
- Anita A, Aprina A, Aryani R. Perbedaan Mual dan Muntah Ibu Hamil Trimester I yang Diberikan Ekstrak Jahe dan Ekstrak Daun Mint. Jurnal Kesehatan. 2018;9(2):253–61.
- Runiari N, Imaningrum PMA. P emberian A kupresurdi T i k P6 Terhadap Intensitas Mual Muntah pada Ibu H amil. B ali: J urusan K eperawatan Poltekkes Denpasar. 2012;
- Handayani N, Khairiyatul RKA. Pengaruh Akupresur Terhadap Penurunan Mual Dan Muntah Pada Ibu Hamil Di Praktek Mandiri Bidan Sidoarjo. EMBRIO. 2019;11(2):102–9.
- Syarif H. Pengaruh terapi akupresur terhadap mual muntah akut akibat kemoterapi pada pasien kanker; a randomized clinical trial. Idea Nursing Journal. 2011;2(2):137–42.
- Sadri B, Nematullahi M, Shahrami R. The effect of acupressure on reducing nausea and vomiting after adenotonsillectomy. Journal of Iran University of Medical Sciences. 2006;13(53):121–6.
- Gürkan ÖC, Arslan H. Effect of acupressure on nausea and vomiting during pregnancy. Complementary Therapies in Clinical Practice. 2008;14(1):46–52.
- Sumantri H. Metodologi penelitian kesehatan. Jakarta: Prenada Media; 2015.
- Koren G, Boskovic R, Hard M, Maltepe C, Navioz Y, Einarson A. Motherisk—PUQE (pregnancy-unique quantification of emesis and nausea) scoring system for nausea and vomiting of pregnancy. American journal of obstetrics and gynecology. 2002;186(5):S228–31.
- Koren G, Piwko C, Ahn E, Boskovic R, Maltepe C, Einarson A, et al. Validation studies of the Pregnancy Unique-Quantification of Emesis (PUQE) scores. Journal of Obstetrics and Gynaecology. 2005;25(3):241–4.
- O’Brien B, Relyea MJ, Taerum T. Efficacy of P6 acupressure in the treatment of nausea and vomiting during pregnancy. American journal of obstetrics and gynecology. 1996;174(2):708–15.
- Werntoft E, Dykes A-K. Effect of acupressure on nausea and vomiting during pregnancy. A randomized, placebo-controlled, pilot study. The Journal of reproductive medicine. 2001;46(9):835–9.
- Tara F, Bahrami-Taghanaki H, Ghalandarabad MA, Zand-Kargar Z, Azizi H, Esmaily H, et al. The effect of acupressure on the severity of nausea, vomiting, and retching in pregnant women: a randomized controlled trial. Complementary medicine research. 2020;27(4):252–9.
- Markose MT, Ramanathan K, Vijayakumar J. Reduction of nausea, vomiting, and dry retches with P6 acupressure during pregnancy. International journal of gynaecology and obstetrics. 2004;85(2):168–9.
- Rad MN, Lamyian M, Heshmat R, Jaafarabadi MA, Yazdani S. A randomized clinical trial of the efficacy of KID21 point (Youmen) acupressure on nausea and vomiting of pregnancy. Iranian Red Crescent Medical Journal. 2012;14(11):697.
- Şimşek Y, Çelik Ö, Yılmaz E, Karaer A, Yıldırım E, Yoloğlu S. Assessment of anxiety and depression levels of pregnant women with hyperemesis gravidarum in a case-control study. Journal of the Turkish German Gynecological Association. 2012;13(1):32.
- Runiari N. Nursing care for clients with hyperemesis gravidarum: application of nursing concepts and theories. Jakarta: Salemba Medika. 2010.
- Christodoulou-Smith J, Gold JI, Romero R, Goodwin TM, MacGibbon KW, Mullin PM, et al. Posttraumatic stress symptoms following pregnancy complicated by hyperemesis gravidarum. The journal of Maternal-Fetal & Neonatal Medicine. 2011;24(11):1307–11.
- Pirimoglu ZM, Guzelmeric K, Alpay B, Balcik O, Unal O, Turan MC. Psychological factors of hyperemesis gravidarum by using the SCL-90-R questionnaire. Clinical & Experimental Obstetrics & Gynecology. 2010;37(1):56.
THE EFFECT OF YOGA ON STRESS LEVEL OF PREGNANT WOMEN IN TRIMESTER III IN PRIVATE MIDWIVES IN JAMBI CITY
Ika Murtiyarini, Imelda*, Yuli Suryanti, Rosmaria
Department of Midwifery, Health Polytechnic of Jambi, Indonesia
* Corresponding author: Imelda, Department of Midwifery, Health Polytechnic of Jambi, Indonesia, Email: imelda.poltekkesjambi@gmail.com
Cita questo articolo
ABSTRACT
Introduction: Prenatal stress is often encountered but is rarely recognized and is considered not to affect pregnancy. Pregnancy has the potential to cause morbidity during pregnancy. In a study in Indonesia, 64.4% of pregnant women experienced severe stress and were at risk of causing preterm labour. One of the preventive measures during pregnancy to improve the health condition of the mother and baby is yoga. Prenatal yoga can prepare pregnant women physically, mentally, and spiritually to play a role in the delivery process.
Materials and Methods: The current study is a quantitative study with a pre-experimental design with one group pretest-posttest without control to determine the effect of prenatal yoga on stress levels of pregnant women in the private midwives of Jambi City in 2020. The study population was 86 pregnant women; by purposive sampling, 30 pregnant women were taken. The time of the study was from March to November 2020. The data analysis used was univariate analysis and bivariate analysis with the Wilcoxon test.
Results: In the initial assessment, most pregnant women experienced moderate stress levels; after prenatal yoga, most pregnant women experienced mild and average stress levels. Wilcoxon test results show that prenatal yoga has an effect on stress levels of pregnant women with a p-value of 0.0001 (<0.05).
Conclusion: Prenatal yoga is effective for reducing stress in third-trimester pregnant women.
Keywords: Stress, pregnant women, Prenatal yoga, Depression Anxiety and Stress Scale (DASS)
INTRODUCTION
Pregnancy is a process that starts from the meeting of sperm and ovum in a woman's uterus or by another name, namely fertilization or conception, to form a zygote which then implants into the uterus and develops into a baby [1–3]. Sometimes, pregnancy has a stressful impact on pregnant women. Prenatal stress is almost expected in all pregnant women, especially in primigravida [4]. This stress can be caused by external factors (external stressors) or from within (internal stressors) pregnant women. Stress is an uncomfortable condition (dysphoric) defined as an imbalance of pregnant women to feel able or resist various changes in the adaptation process of their pregnancy [5,6].
Psychosocial studies of stress during pregnancy conducted on Asian, African, and white races found that 6% of pregnant women experienced mild stress, 78% experienced severe stress, and 16% did not experience stress at all [7]. Pregnancy stress is significantly caused by economic hardship, household problems, physical violence, medical problems, busyness, work, and a pregnancy history with complications [8].
Prenatal stress is often but is rarely recognized and is thought not to affect pregnancy [9]. A Canadian study showed that pregnant women experienced low levels of psychosocial stress and 6% of high levels of stress. Pregnant women in Spain, 30% have a lower chance of experiencing stress, while in Indonesia, 64.4% of pregnant women experience severe stress and can give birth prematurely [10].
Stress in pregnancy has the potential to cause morbidity during pregnancy [11]. Complications arise from prenatal stress, such as preterm delivery caused by the placenta, increased corticotrophin-releasing hormone (CRH), and progesterone in stressful conditions [12]. In addition, in early pregnancy, stress and a decrease in progesterone can cause abortion, progesterone which is calming and slows gastric motility as a trigger for hyper emesis gravidarum to Low Birth Weight (LBW). This impact proves that the mother's mental state can affect the mother's health during pregnancy and the baby's growth and development in the next period of life [13,14].
DASS-42 is an assessment of stress scale that can be used in the stress assessment of pregnant women [15]. DASS-42 has been used to identify stress in Hispanic, American, British, Australian and Indonesian populations. Assessment items in DASS-42 include emotional states, communication barriers and physical disturbances felt by pregnant women. Measurement of stress levels using the DASS-42 score can reflect the state of prenatal stress as a predisposing factor for pregnancy complications [16,17].
Maintaining the health of the mother and fetus during pregnancy can be done by exercising in the morning, static cycling, aerobics, water exercise, dancing, and yoga. Some pregnancy exercise methods that can be an option include yoga, pilates, Kegels, hypnotherapy [18]. Prenatal yoga is effective for pregnant women to achieve comfort during pregnancy even until the delivery process. Prenatal yoga is a skill to cultivate the mind in a comprehensive personality development technique that includes physical, psychological and spiritual. This prenatal yoga includes various relaxations, adjusting breathing postures and meditation done by pregnant women every day [19].
Several studies have shown that yoga positively affects pregnant women, significantly reducing stress levels and back pain [20,21]. Another study conducted by Rahma [22] showed an increase in sleep quality in pregnant women after prenatal yoga. Another study conducted by Mediarti et al. [23] showed differences in the complaints of pregnant women before and after prenatal yoga, including back pain, insomnia, leg cramps and anxiety.
Based on the results of several studies that have been carried out showing the benefits of implementing prenatal yoga in reducing stress during pregnancy, but no research focuses on primigravida pregnant women; therefore, we tried to conduct this research on third-trimester pregnant women in the independent practice of midwives in Jambi City, Indonesia.
MATERIALS AND METHODS
This pre-experimental study consisted of a pre-test and post-test without a control group design involving 30 third trimester primiparous pregnant women in independent practice of midwives (PMB) Jambi City, Indonesia, which was carried out from March to November 2020. The implementation of intervention was carried out in PMB Jambi City, carried out by researchers assisted by midwives et PMB and enumerators, after asking participants' consent and participants agreed by signing a certificate. The criteria for participants who were included in the study were primiparous mothers and third trimester, while mothers who were not healthy at the time of the study were not included in the study. The sample has been selected using purposive sampling, namely the technique of selecting samples based on the researcher's considerations.
The prenatal yoga intervention was given by a certified midwife as a prenatal yoga instructor, with the first procedure (1) the mother doing warm-up movements, (2) doing the Uttkatasana movement, (3) doing the Vrkasasana movement, (4) doing the Adhatasana movement, (5) perform the Virabadhanasana movement, (6) perform the Utitatrikonasana movement, (7) perform the Anjeneyasana movement, (8) perform the Utkatakonasana movement, (9) perform the Malasana movement, (10) perform the Supta Baddha Konasana movement, (11) perform the Savasana movement, and Finally, take a deep breath from the nose 5-8 times.
Treatment is carried out once a week for two weeks with duration of 1-2 hours per session. The implementation of treatment complies with health protocols during the covid-19 pandemic, including washing hands, disinfecting mats, and not doing yoga in groups. The assessment of stress levels both pre and post prenatal yoga was carried out at PMB Jambi City, Indonesia by researchers assisted by enumerators.
This stress level was measured using the Depression Anxiety Stress Scale 42 (DASS 42) (Lovibond, 1995) both before and after the implementation of prenatal yoga. Psychometric anxiety stress scale of the Depression Anxiety stress scale 42 (DASS 42) consists of 42 question items, which include 3 subvariables including 1) physical 2) emotional/psychological 3) behavior. According to Lovibond (1995) cited by Crawford & Henry (2003) in their journal entitled "DASS: Normative data & latent structure in large non-clinical sample". DASS has a discrimant validity level and has a reliability of 0.91 which is processed based on Cronbach's Alpha assessment, so that the stress questionnaire is not tested for reliability because the questionnaire has been applied internationally. The stress level on the DASS 42 instrument (lovibond, 1995) is classified into five levels, namely Normal, score: 0 – 7; Mild, score: 8-9; Medium, 10-14; Severe, score: 15-19; Very severe, score: ≥ 20.
No economic incentives were offered or provided for participation in this study. The study was performed in accordance with the ethical considerations of the Helsinki Declaration. Ethical eligibility was obtained from the Health Research Ethics Commission of the Ministry of Health, Jambi, No. LB.02.06/2/140/2020.
Statistical Analysis
Data were analyzed using univariate analysis to obtain a frequency distribution based on each variable studied and bivariate analysis to determine the effect of prenatal yoga on stress levels of pregnant women. Data are presented as numbers and percentages for categorical variables. Continuous data are expressed as the mean ± standard deviation (SD), or median with Interquartile Range (IQR). Wilcoxon’s test was used to evaluating repeated measurements of the same objects using them as their own control. The test was carried out on 2 groups of related samples, the measurement scale was ordinal data. All tests with p-value (p)<0.05 were considered significant. Statistical analysis performed using the SPSS app version 16.0.
RESULTS
The results of the univariate analysis, which aims to determine the frequency of each variable studied, can be seen in the following table:
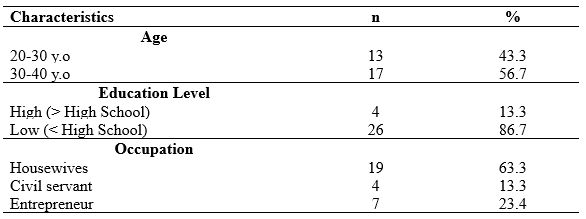
Table 1. Frequency Distribution of Respondents' Characteristics
Table 1 shows that most respondents in group aged 20-30 years amounted to 13 people (43.3%), and respondents aged 30-40 years amounted to 17 (56.7%) people. Majority of respondents' education level is low education as much as 86.7%, and the dominant occupation of respondents is housewives as much as 63.3%.
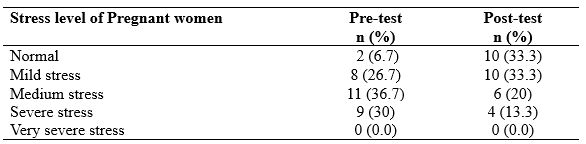
Table 2. Distribution of stress levels of pregnant women before and after prenatal yoga
Table 2 show that 11 (36.7%) respondents experienced medium stress during pregnancy, 10 (33.3%) respondents experienced mild stress levels and did not experience stress after prenatal yoga.
This analysis aims to determine the effect on variables using the Wilcoxon test, which can be seen in Table 3 below:
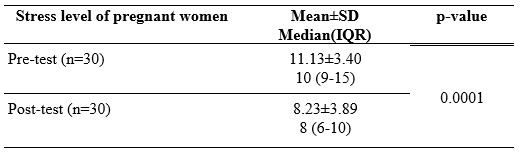
Table 3. The effect of prenatal yoga on the stress level of pregnant women in private midwives in Jambi City.
The analysis of the influence of prenatal yoga on the stress level of pregnant women in private midwives obtained a p-value = 0.0001 (p <0.05). These test results show that prenatal yoga affects the stress level of pregnant women in private midwives in Jambi City.
DISCUSSION
Anxiety in maternity mothers is related to the length of labour which results in complications in childbirth. One of the causes of prolonged labour is the stress response, and this ranks at the top among other causes [24].
Based on the study results, it is known that there are three categories of stress levels experienced by pregnant women during pregnancy. Stress is the body's reaction to situations that cause pressure, change, emotional tension, and others. Stress is universal; that is, all people can feel it, but the way it is expressed is different. According to individual characteristics, the response is different for each person. Stress in pregnant women harms themselves and their babies. Moreover, if the stress is ongoing and chronic, it can have implications for recurring anxiety, frustration, or fear that has been suffered for a long time and can have adverse health effects.
Before prenatal yoga, most pregnant women experienced moderate stress. Many things can affect this incident, for example, worrying about the baby, not deciding where to give birth, doubting the family's economic capacity. Prenatal stress often occurs only rarely recognized and considered not very important during pregnancy. Based on the study results, it is known that 64.4% of pregnant women in Indonesia experience severe stress.
Prenatal yoga is one way that can be done to relax pregnant women so that it can reduce stress levels in pregnant women. Based on the study results, it is known that there is a decrease in stress levels after prenatal yoga. Most of the stress levels of pregnant women drop to mild stress and even become routine.
Yoga affects the hypothalamus to suppress the secretion of CRH, which will affect the anterior lobe of the pituitary gland to suppress the release of the hormone ACTH so that the production of adrenal hormones and cortisol decreases and orders the anterior lobe of the pituitary gland to secrete endorphins. Yoga will inhibit the increase in sympathetic nerves so that the number of hormones that cause body deregulation can be reduced. The parasympathetic nervous system signals to influence catecholamine release. As a result, there is a decrease in heart rate, breathing rhythm, blood pressure, muscle tension, metabolic rate, and the production of hormones that cause anxiety or stress [25].
Based on the respondents' stress levels before and after prenatal yoga, there was a significant decrease with the median pre-test stress value decreasing from 10 to 8 after the post-test, p=0.0001. The results of this test indicate the influence of prenatal yoga on the stress levels of pregnant women. Several previous studies showed that yoga had a positive effect on pregnant women, namely reducing stress levels and back pain [20]. Another study conducted by Rahma [22] showed an increase in sleep quality in pregnant women after prenatal yoga.
The application of prenatal yoga, which is one way to ensure the condition of the mother and fetus in a healthy and comfortable condition during pregnancy, is appropriate [26,27]. Yoga is a combination of stretching, breathing, postures, and meditation that promotes health and spiritual growth in the practitioner. This prenatal yoga includes various relaxations, adjusting breathing postures and meditation done by pregnant women every day [28].
One experimental study at a prenatal clinic in Taipei found that prenatal yoga significantly reduced pregnant women's stress and improved their immune function. Attractive value from this study is the finding of higher immunoglobulin A (p < 0.001) in the intervention group than in the control group [29].
CONCLUSIONS
Prenatal yoga is effective for reducing stress in pregnant women in the third trimester. The variable for reducing stress levels is strongly influenced by the ability of pregnant women to control their thoughts so that the decrease in stress as a result of prenatal yoga varies in pregnant women
Study Limitations
The lack of control in this study is a limitation, so it cannot compare the intervention group who was given yoga practice and not yoga. In addition, other limitations of this study are No multicenter study, limited geographical area, small sample size.
Funding statement
This research did not receive any specific grant from funding agencies in the public, commercial, or not for profit sectors.
Competing interests statement
There are no competing interests for this study.
REFERENCES
- Nugroho T, Warnaliza D. Buku Ajar Askeb 1 Kehamilan. Nuha Medika; 2014.
- Van den Bergh BRH, van den Heuvel MI, Lahti M, Braeken M, de Rooij SR, Entringer S, et al. Prenatal developmental origins of behavior and mental health: The influence of maternal stress in pregnancy. Neuroscience & Biobehavioral Reviews. 2020;117:26–64.
- Boekhorst MGBM, Muskens L, Hulsbosch LP, Van Deun K, Bergink V, Pop VJM, et al. The COVID-19 outbreak increases maternal stress during pregnancy, but not the risk for postpartum depression. Archives of Women’s Mental Health. 2021;1–7.
- Sun S, Yang M, Zhang J, Zhou X, Jia G, Yu X. Family support for pregnant women with foetal abnormality requiring pregnancy termination in China. Health & social care in the community. 2020;28(3):1020–9.
- Woods SM, Melville JL, Guo Y, Fan M-Y, Gavin A. Psychosocial stress during pregnancy. American journal of obstetrics and gynecology. 2010;202(1):61-e1.
- Sarmita S, Nurdin S, Fattah AH. Gambaran Kecemasan Ibu Hamil Di Wilayah Kerja Puskesmas Cabenge Kabupaten Soppeng. Jurnal Pendidikan Keperawatan dan Kebidanan. 2021;1(1):20–6.
- Diane M. Korelasi Kadar Progesteron dan Kortisol Dengan Skor DASS-42 Pada Ibu Hamil Trimester 1. Universitas Andalas; 2017.
- Redshaw M, Henderson J. Fathers’ engagement in pregnancy and childbirth: evidence from a national survey. BMC pregnancy and childbirth. 2013 Mar;13:70.
- Cottrell EC, Seckl J. Prenatal stress, glucocorticoids and the programming of adult disease. Frontiers in behavioral neuroscience. 2009;3:19.
- Palmeira P, Quinello C, Silveira-Lessa AL, Zago CA, Carneiro-Sampaio M. IgG placental transfer in healthy and pathological pregnancies. Clinical and Developmental Immunology. 2012;2012.
- Sicherer SH, Wood RA, Stablein D, Lindblad R, Burks AW, Liu AH, et al. Maternal consumption of peanut during pregnancy is associated with peanut sensitization in atopic infants. Journal of Allergy and Clinical Immunology. 2010;126(6):1191–7.
- Woods‐Giscombé CL, Lobel M, Crandell JL. The impact of miscarriage and parity on patterns of maternal distress in pregnancy. Research in nursing & health. 2010;33(4):316–28.
- Johnson M, Campbell F, Messina J, Preston L, Woods HB, Goyder E. Weight management during pregnancy: a systematic review of qualitative evidence. Midwifery. 2013;29(12):1287–96.
- Brummelte S, Galea LAM. Depression during pregnancy and postpartum: contribution of stress and ovarian hormones. Progress in Neuro-Psychopharmacology and Biological Psychiatry. 2010;34(5):766–76.
- Lovibond PF, Lovibond SH. The structure of negative emotional states: Comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behaviour research and therapy. 1995;33(3):335–43.
- Crawford DM, Trotter EC, Hartshorn KJS, Whitbeck LB. Pregnancy and mental health of young homeless women. American Journal of Orthopsychiatry. 2011;81(2):173.
- Dong X, Qu Z, Liu F, Jiang X, Wang Y, Chui CHK, et al. Depression and its risk factors among pregnant women in 2008 Sichuan earthquake area and non-earthquake struck area in China. Journal of affective disorders. 2013;151(2):566–72.
- Krisnadi SR. Sinopsis yoga untuk kehamilan: sehat, bahagia dan penuh makna. Larasati, P, & Wibowo, A(2012) Pengaruh Keikutsertaan Senam Hamil Terhadap Kecemasan Primigravida Trimester Ketiga dalam Menghadapi Persalinan Skripsi, Universitas Airlangga, Fakultas Kesehatan Masyarakat, Surabaya. 2010;
- Amalia R, Syamsuddin S, Idris I, Limoa E, Pelupessy N, Syam A. The Effectiveness of Prenatal Gentle Yoga on the Recovery of Anxiety Level and Norepinephrine Level in Pregnant Women Aged 35 Years Old. International Journal of Health and Medical Sciences. 3(1):79–85.
- Field T, Diego M, Delgado J, Medina L. Yoga and social support reduce prenatal depression, anxiety and cortisol. Journal of bodywork and movement therapies. 2013;17(4):397–403.
- Battle CL, Uebelacker LA, Magee SR, Sutton KA, Miller IW. Potential for prenatal yoga to serve as an intervention to treat depression during pregnancy. Women’s Health Issues. 2015;25(2):134–41.
- Rahma FN. Hubungan Senam Yoga Terhadap Peningkatan Kualitas Tidur Pada Ibu Hamil Trimester III. Universitas Muhammadiyah Surakarta; 2014.
- Mediarti D, Sulaiman S, Rosnani R, Jawiah J. Pengaruh yoga antenatal terhadap pengurangan keluhan ibu hamil trimester III. Jurnal kedokteran dan kesehatan. 2014;1(1):181691.
- Hayati F, Herman RB, Agus M. Perbedaan tingkat kecemasan ibu bersalin di puskesmas dengan di bidan praktik mandiri dan hubungannya dengan lama persalinan. Jurnal Kesehatan Andalas. 2018;6(3):564–71.
- Vijayalakshmi P, Madanmohan BAB, Patil A, Babu K. Modulation of stress induced by isometric handgrip test in hypertensive patients following yogic relaxation training. Indian J Physiol Pharmacol. 2004;48(1):59–64.
- Chuntharapat S, Petpichetchian W, Hatthakit U. Yoga during pregnancy: effects on maternal comfort, labor pain and birth outcomes. Complementary therapies in clinical practice. 2008;14(2):105–15.
- Sun Y-C, Hung Y-C, Chang Y, Kuo S-C. Effects of a prenatal yoga programme on the discomforts of pregnancy and maternal childbirth self-efficacy in Taiwan. Midwifery. 2010;26(6):e31–6.
- Jahdi F, Sheikhan F, Haghani H, Sharifi B, Ghaseminejad A, Khodarahmian M, et al. Yoga during pregnancy: The effects on labor pain and delivery outcomes (A randomized controlled trial). Complementary therapies in clinical practice. 2017;27:1–4.
- Chen P-J, Yang L, Chou C-C, Li C-C, Chang Y-C, Liaw J-J. Effects of prenatal yoga on women’s stress and immune function across pregnancy: A randomized controlled trial. Complementary Therapies in Medicine. 2017;31:109–17.
DIFFERENCES IN THE QUALITY OF VACCINES STORED IN COOLER BOXES COMPARED TO HOUSEHOLD REFRIGERATORS
Herinawati1*, Atikah Fadhilah Danaz Nasution1, Lia Artika Sari1, Iksaruddin2
1Midwifery Department, Health Polytechnic of the Ministry of Health, 36128 Jambi, Indonesia
2Department of Health Promotion, Health Polytechnic of Jambi, 36128, Indonesia
Corresponding Author: Herinawati, herinawati.poltekkes@gmail.com, Jl. Prof DR GA Siwabessy No.42, Buluran Kenali, Kec. Telanaipura, Kota Jambi, 36122
Cita questo articolo
ABSTRACT
Background: The inappropriate temperature of vaccine storage may cause vaccine damage leading to degrading or even dispelling the vaccine’s quality. This research aims to reveal the difference of vaccine’s quality stored in the cooler box compared to the household refrigerator with vaccine only and the difference of vaccine’s quality stored in the cooler box compared to the household refrigerator with vaccine stored along with food and beverage
Methods: The research design uses an experimental study with a post-test-only control group design. The research was conducted at two independent practice midwives in Antapani Sub-district and the Faculty of Mechanical and Aerospace Engineering Bandung Institute of Technology from November to December 2015. The research object used eight types of vaccine (Hepatitis B, BCG, DPT-HB-Hib, Polio, Measles, DT, Td, and TT) with 72 vaccine vials divided into 3 vaccine storage units. The data analysis uses the chi-square test.
Results: The results of the research show that there are statistically significant differences between the vaccine’s quality stored using a cooler box compared to a household refrigerator with vaccine only and the vaccine’s quality stored using a cooler box compared to a household refrigerator with vaccine stored along with food and beverage with the value of p<0,05.
Conclusion: It is concluded that there are differences of the vaccine’s quality stored using cooler box compared to a household refrigerator with vaccine only and also different vaccine’s quality stored using cooler box compared to a household refrigerator with vaccine stored along with food and beverage
Keywords: Cooler box, household refrigerator, vaccine quality
INTRODUCTION
Vaccines are biological preparations to increase immunity against several diseases[1]. Immunization will be effective if the vaccine is distributed evenly with well-maintained quality. The quality of the vaccine is influenced by the time of distribution because the life of the vaccine is very limited and requires special treatment. For this reason, the cold chain must be adequate as a guarantee of vaccine quality [2]. The vaccine cold chain system is a series of storage and transportation processes using various equipment accordingly to ensure the quality of the vaccine from the factory to the patient [3].
The Minister of Health Regulation Number 12 of 2017 concerning the Implementation of Immunization has standardized a vaccine storage temperature of 2 to 8ºC for freeze sensitive vaccines (not frozen), and at a temperature of -15 to -25 C for heat sensitive vaccines. Currently, only polio vaccine still requires storage at temperatures below 0°C. A number of vaccines, such as Hepatitis B, DPT-HB-Hib, IPV, DT, Td will potentially be damaged if exposed to freezing temperatures. Meanwhile, the Polio, BCG, and Measles vaccines will potentially be damaged if exposed to hot temperatures. However, in general, vaccines will spoil if exposed to direct sunlight. In general, the cold chain consists of refrigerators and freezers to store vaccines, and thermos (vaccine carriers) to bring vaccines to immunization services, especially for activities outside the building/field [4]. Annually, more than 1.4 million children in the world die from various diseases, which should be avoided by immunization. Several infectious diseases that are included in the Disease Preventable by Immunization include: diphtheria, tetanus, hepatitis B, meningitis, pneumonia, polio, pertussis, and measles. Children who have been immunized will be protected from these dangerous diseases, which can cause disability or death[5,6]. Immunization for infants is called basic immunization, while immunization for primary school-age children and women of childbearing age is called advanced immunization. Vaccines for routine immunization in infants include: hepatitis B, BCG, polio, DPT, and measles. At school age: Diphtheria Tetanus (DT), Diphtheria Tetanus (Td). Immunization of women of childbearing age is given tetanus toxoid[7]. Incompatibility of the vaccine storage temperature with the standard, resulting in damage to the vaccine which means lowering the quality of the vaccine [8].Vaccine quality cannot be improved even if it is stored again at the right temperature. Defective vaccines must be destroyed, because it cannot induce immunity in the body through immunization, in fact itmayaffect Post Immunization Adverse Events (AEFI) to the target. Household refrigerators are designed to store food and drink, it is not recommended to store vaccines. At the district and immunization service units, most household refrigerators are used to store vaccines. Research conducted in Tunisia on 10 household refrigerators found that many household refrigerators found problems with freezing and high temperatures, making it a risk for vaccine storage[9]. Cooler box, a new tool made by ITB students, is an innovation in the medical field that utilizes technology to store vaccines, uses electricity and has a stable temperature (+4.63oC)[10]. Cooler Box’s ability to store vaccines is measured through a vaccine vial monitor (VVM). All vaccines in the immunization program are equipped with VVM, which is an indicator attached to each vaccine vial to monitor vaccines during transit and storage. The combined effects of time and temperature provide information about heat exposure and potency.
In Indonesia, there are still a number of deaths from Immunization Preventable Diseases (PD3I), including tuberculosis (TB) and measles [11]. In 2013 West Java Province achieved the highest measles immunization coverage in Indonesia at 95.8%, with the incidence of measles at 1,910 cases, occurring in the immunized group as many as 562 cases (34%). Measles Extraordinary Events (KLB) occurred in West Java as many as 18 outbreaks with 205 cases [11]. Another disease that is included in PD3I, and is still high in West Java is tuberculosis with a total of 61,721 people (306 patients aged <12 years)[11]. The city of Bandung is the center of the province of West Java and has 73 health centers (30 UPTs and 34 networks). In 2013 UPT Griya Antapani had 31 cases of measles and increased in 2014 to 33 cases of measles. Other diseases that are included in PD3I are at UPT Griya Antapani, namely tuberculosis [11].
The success of the immunization program cannot be determined only by the high coverage rate, but also by the reduction in cases and outbreaks of PD3I as an indicator of increasing service quality. [12]. Several studies have revealed that outbreaks can be caused by low immunization coverage or due to low vaccine quality caused by poor vaccine cold chain management [13,14].
Based on the existing problems, we tested a tool that had been developed by ITB students and was an innovation for storing vaccines. Trials by storing vaccines for 4 weeks in cooler boxes, household refrigerators filled with vaccines, and household refrigerators filled with vaccines with food and drinks. Furthermore, a vaccine vial monitor (VVM) was assessed to determine the quality of the vaccine.
METHODS
This experiment uses the Post test only control group design approach. The research group consisted of two groups including vaccines stored in household refrigerators and vaccines stored in cooler boxes. The study was conducted at 2 independent midwife clinics in Antapani sub-district and the FTMD ITB laboratory from November to December 2015. The object of the study used 8 types of vaccines (Hepatitis B, BCG, DPT-HB-Hib, polio, measles, DT, Td and TT) with a total sample of 72 vaccine vials which were divided into 3 vaccine storage devices: cooler box, refrigerator filled only with vaccines and household refrigerator filled with food and drinks.
Collecting research data by recording the temperature of household refrigerators and refrigerators, researchers make visits to the midwife's clinic 2 times a day, in the morning at 09.00-11.00 and in the afternoon at 17.00-19.00. Recording the cooler box temperature in the FTMD ITB laboratory, in the morning at 8.00-10.00 and in the afternoon at 15.00-17.00 after one month of vaccine quality assessment (VVM). The temperature of the cooler box and refrigerator is set (+20C)-(+8oC).
The limits for the condition indicators of the vial monitor vaccine (VVM) are detailed in the following Table 1.
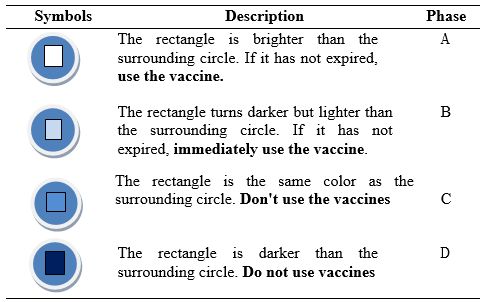
Table 1. Various vaccine vial monitor (VVM) conditions
The study was performed in accordance with the ethical considerations of the Helsinki Declaration. The Health Research Ethics Commission of the Faculty of Medicine, Padjadjaran University has given clearance approval with certificate number 694/UN6.C1.3.2/KEPK/PN2015. The ethical aspects of this study consider in detail the place of research to be used.
Statistical analysis
Data are presented as numbers and percentages for categorical variables. Continuous data are expressed as the mean ± standard deviation (SD), or median with Interquartile Range (IQR). In the case of categorical variables, the chi-square test is performed to test the difference between the two independent samples. All tests with p-value (p) <0.05 were considered significant. Statistical analysis was performed using SPSS app version 16.0.
RESULTS
The 8 types of vaccines used include Hepatitis B, BCG, polio, DPT-HB-Hib, measles, TT, DT and Td. Vaccines are stored for one month using three vaccine storage devices which are placed in different places, including a cooler box in the FTMD ITB laboratory, a household refrigerator and a refrigerator containing only vaccines at the midwife's clinic. The results showed a statistically significant difference in vaccine quality (VVM) using a cooler box compared to a household refrigerator containing vaccines, food, and beverages (p<0.05) (Table 2).
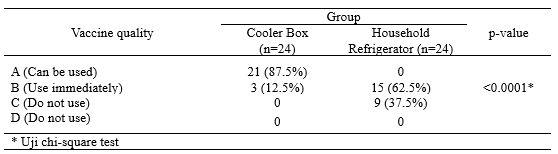
Table 2. Differences in the Quality of Vaccines stored in Cooler Boxes Compared to Household Refrigerators
The results also showed a statistically significant difference in the quality of the vaccine (VVM) stored in a cooler box compared to a refrigerator containing only vaccine (p<0.05) (Table 3).
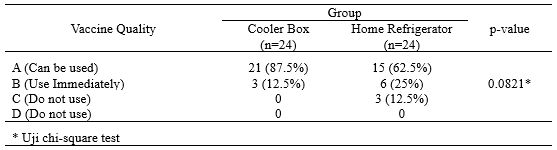
Table 3. Differences in the Quality of Vaccines Stored in Cooler Boxes Compared to Home Refrigerators containing Vaccines
The temperature fluctuations in the cooler box during the morning and afternoon inspections can be seen in Figure 1. Descriptively there is a difference in the temperature of the cooler box, where in the afternoon it is higher than in the morning. up to 7.30C.
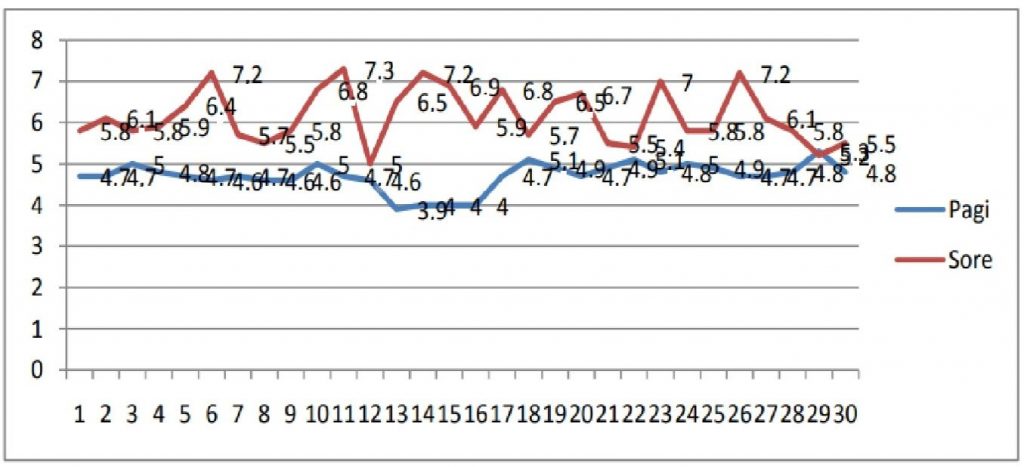
Figure 1. Vaccine Temperature Chart Stored in Cooler Box
The temperature fluctuations in the household refrigerator during the morning and afternoon inspection can be seen in Figure 2. Descriptively there is a difference in the temperature of the household refrigerator, which is higher in the afternoon than in the morning. The highest household refrigerator temperature in the morning is 11.7oC and in the afternoon it reaches 18.1oC.
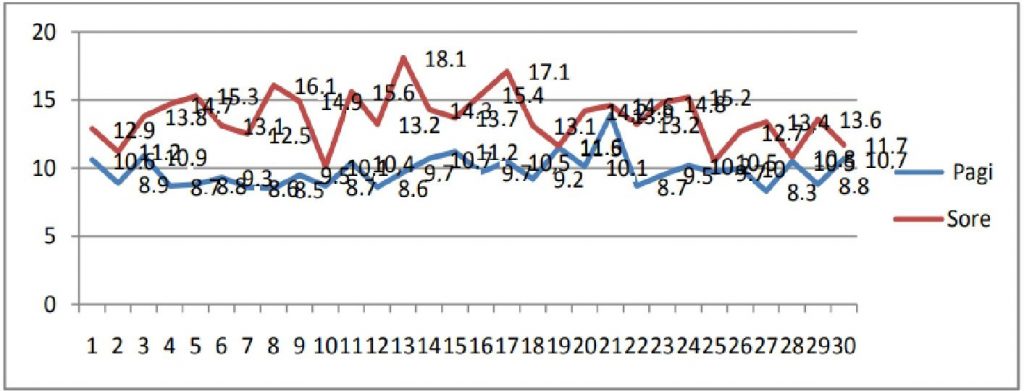
Figure 2. Graph of Vaccine Temperature Stored in Household Refrigerators
Temperature fluctuations in the refrigerator containing only vaccines in the morning and afternoon examinations can be seen in Figure 3, where descriptively there is a difference in temperature in the refrigerator containing only vaccines, which is higher in the afternoon than in the morning. The temperature of the refrigerator containing the vaccine only in the morning is 7.1oC and in the afternoon it reaches 13.1oC.
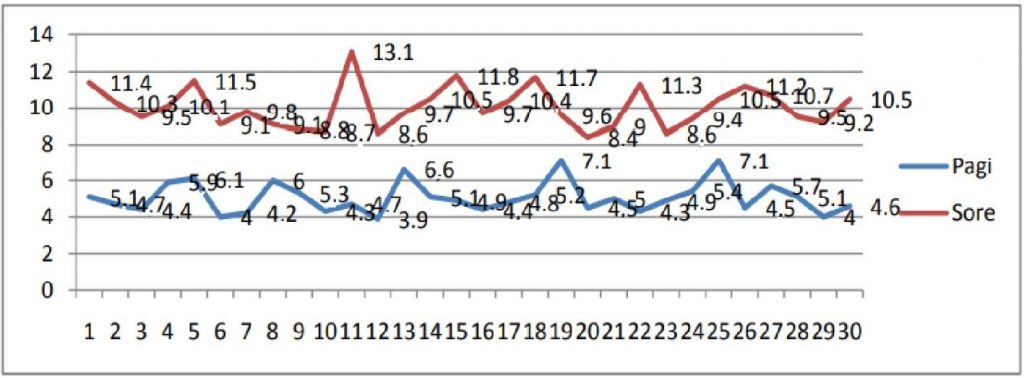
Figure 3. Vaccine Temperature Chart Stored in the Refrigerator Only Contains Vaccine
DISCUSSIONS
Vaccines have certain characteristics and require a special cold chain since they are produced in the factory until they are used in health care units. Deviations from the storage of vaccines from existing provisions can result in damage to the vaccine so that it reduces or even eliminates the quality of the vaccine, resulting in no immunity. Monitoring of vaccine storage temperatures is crucial in establishing vaccine viability. Vaccine is a biological product that is sensitive to temperature, exposure to heat will shorten the shelf life of the vaccine. Vaccine quality depends on the cold chain, with a defined temperature range from (+2oC)-(+8oC) during transport and storage [7]. Vaccine vial monitors (VVM) are used to assess whether the vaccine has ever been exposed to temperatures above the allowable limits, it is said to be VVM A or VVM B conditions. must be used immediately. The condition of VVM C or VVM D if the color of the rectangular box is the same or darker than the circle and its surroundings, then the vaccine has been exposed to temperatures above the permissible limit, the vaccine should not be used.
The results of this study revealed a significant difference in the quality of vaccines (VVM) stored in cooler boxes compared to household refrigerators (p=0.001). WHO and the Indonesian Ministry of Health do not recommend household refrigerators for vaccine storage because they are not designed to maintain a temperature (+2oC)-(+8oC) as the temperature range used to store vaccines, this is due to the rapid changes in warm temperatures when fridge door opened [15].
In accordance with the recommendations of WHO and the Indonesian Ministry of Health, it is not allowed to store food, drinks, medicines, or other objects in the vaccine refrigerator, it will disrupt temperature stability because it is often opened Any refrigerator or freezer used for vaccine storage should be dedicated only to vaccine storage without any food and drink mixes. The results of trials conducted by WHO, showed that a refrigerator or freezer for storing vaccines that is often opened can cause the refrigerator temperature to be unstable because warm air flows into the refrigerator every time the refrigerator door is opened and results in food and beverage spills and contamination [6,16]. WHO and the Indonesian Ministry of Health have recommended monitoring the temperature of the vaccine storage area twice a day, in the morning and evening before taking the vaccine. The refrigerator door should not be opened for more than one minute at a time when the vaccine is taken (avoid opening the refrigerator door too often as possible). Research conducted by WHO shows that frequently opening the refrigerator door can cause temperature instability and excessive exposure to light [15]. Several studies have found poor knowledge and practice in administering immunization vaccines in primary care centers, also found a lack of attitudes and behavior of midwives in administering vaccines according to established standards. The behavior of midwives in vaccine management is strongly influenced by the level of knowledge of the midwife about vaccines and their management. The quality of immunization is closely related to how the vaccine is handled and treated, and the maintenance of the cold chain. Vaccine management is part of the quality of service. Indicators of good vaccine management quality are indicated by maintained vaccine temperature (+2)-(+8)oC, no vaccine found with VVM C or VVM D[17]. Research in Bandung City showed that midwives had low knowledge of vaccine storage, some midwives showed a negative attitude towards vaccine storage and most respondents did not practice vaccine storage according to standards. Research in the city of Bogor found that most of the vaccines stored in the midwife clinic at the same time as placing food such as fruits, cakes, eggs, meat and vegetables, and beverages, and it was found that most of the vaccines were in VVM C and VVM D[18]. The current study found that the vaccine quality in the cooler box was better than the household refrigerator containing only vaccine (p<0.05) where there was a significant difference, this was related to the temperature in the cooler box where the vaccine was stored according to the standard (+2oC)-(+8oC) while the household refrigerator filled with vaccines did not meet the standard, the temperature (> 8oC) was found in the afternoon recording. These results are consistent with several previous studies, such as in Kelantan Malaysia found 73.5% of household refrigerators found that the temperature was more than 8oC.17 Studies in Thailand and Cameroon also showed high warm temperatures in vaccine storage using household refrigerators[19,20], and a study in Semarang City found that 52.2% of household refrigerator temperatures had a temperature > 8oC [21]. Thus, the results of the current study are in line with previous studies where the results of household refrigerator temperatures are more than 8oC. Several things related to higher refrigerator temperatures or unstable refrigerator temperatures, including the refrigerator door not closing tightly, this usually occurs because the rubber door on the refrigerator door is uneven or torn so that the cold air inside the refrigerator exchanges with air outside the refrigerator. As a result, low temperatures in the refrigerator are difficult to achieve or there is a refrigerant or freon leak in the refrigerant system which results in disruption of the cooling process because there is no refrigerant as a medium for heat transfer from inside the refrigerator to outside the refrigerator [16]. These results indicate that the polio vaccine stored in the cooler box is in VVM B (the vaccine is immediately used) while in the household refrigerator the contents of the vaccine are in VVM C [22]. Polio vaccine is stable for 6 months if stored at (+2oC)-(+8oC), and stable for 2 years if stored at (-15oC)-(-25oC). The polio vaccine does not contain preservatives, stabilizers, and adjuvants. Preservatives are used to prevent bacterial and/or fungal contamination (contamination) of bacteria and/or fungi into vaccines. Stabilizers are added in vaccine production to ensure vaccines are subject to extreme conditions or changing environmental conditions, such as heat, light, humidity, and acidity. Adjuvant are substances used to enhance the immune response of a vaccine, optimize immune system-stimulating cells, reduce the number of antigens used in a vaccine and reduce the frequency of administration [23].
The BCG vaccine is derived from live attenuated bacteria and the measles vaccine is derived from a live attenuated virus. Storage of BCG vaccine at a temperature (-15oC)-(-25oC)or at a temperature (+2oC)-(+8oC) there is no difference, BCG vaccine is stable for 1 year. Measles vaccine is derived from live attenuated virus, measles vaccine is stored at (-15oC)-(-25oC)or at (+2oC)-(+8oC) temperature there is no difference, measles vaccine is stable for 2 years[6].
Similar to polio vaccine, BCG vaccine and measles vaccine do not contain preservatives, stabilizers and adjuvants. Preservatives are used to prevent bacterial and/or fungal contamination (contamination) of vaccines. Stabilizers are added in vaccine production to ensure vaccines are subjected to extreme conditions or changing environmental conditions, such as heat, light, humidity, and acidity[24]. Adjuvants are substances used to enhance the immune response of a vaccine, optimize immune system-stimulating cells, reduce the number of antigens used in a vaccine and reduce the frequency of administration[25]. In addition, the vaccine is also light sensitive and the tinted glass vial has been shown to minimize potency loss[26].
The current study revealed that high temperatures (>8oC) in vaccine storage using household refrigerators containing only vaccines can cause changes in VVM in polio, BCG, and measles vaccines. The polio vaccine was obtained with VVM C while the BCG and measles vaccines with VVM B this was related to the use of VVM 2 in the polio vaccine (low stability) while the BCG vaccine and measles vaccine used VVM 14 (medium stability)[5].
In this study, it was found that there was no difference between the quality of the vaccine stored in the cooler box and the home refrigerator containing the vaccine because the quality of the vaccine was safe and maintained in the refrigerator. The reason is that the home refrigerator containing the vaccine is not opened often, and this is what distinguishes the vaccine from being stored in a refrigerator containing food ingredients, because it is often opened so that the temperature in the refrigerator becomes high or more than 8oC.
Based on research at the National Institute of Standards and Technology (NIST) Gaithersburg Thermal Studies Laboratory found a way to maintain cold temperatures in household refrigerators that lose cold temperatures due to frequent openings or as a result of lights, namely inserting ice bottles in household refrigerators which has an impact on prolonging time cold in the fridge. Thermal ballast usage is a practical and effective strategy for mitigating the negative impact of power outage events[27].
CONCLUSIONS
There is a difference in the quality of vaccines stored in cooler boxes compared to household refrigerators. There is a difference in quality that is stored in a cooler box compared to a refrigerator containing only vaccines. Finally, the correct cold chain for the good conservation of vaccines must always be maintained according to the indications of the manufacturers
LIMITATION OF STUDY
The limitation of this study is the small sample size
CONFLICT OF INTEREST
The authors have no conflict of interest.
FUNDING STATEMENT
The author(s) received no financial support for the research, authorship, and/or publication of this article.
REFERENCES
- Pollard AJ, Bijker EM. A guide to vaccinology: from basic principles to new developments. Nature Reviews Immunology [Internet]. 2021;21(2):83–100. Available from: https://doi.org/10.1038/s41577-020-00479-7
- Yuniar Y, Syaripuddin M, Sasanti R, Susyanty AL. Sistem Manajemen dan Persediaan Vaksin di Dua Provinsi Indonesia. Indonesian Bulletin of Health Research. 2014;42(2):108–21.
- Centres for Diseases Control and Prevention. Vaccine Storage and Handling Tollkit. the U.S. Department of Health and Human Services (DHHS). the U.S. Department of Health and Human Services (DHHS); 2021. 493–493 p.
- Kemkes. Peraturan menteri kesehatan republik indonesia Nomor 12 tahun 2017 Tentang Penyelenggaraan imunisasi. Jakarta; 2017.
- WHO. Cold chain, vaccines and safe-injection equipment management. In: Department of Immunization VaB. Geneva: Department of Immunization, Vaccines and Biologicals; 2008.
- UNICEF. Handbook for Vaccine & Cold Chain. Department of Health & Family Welfare. India: Ministry of Health and Family Welfare; 2010.
- WHO. Temperature sensitivity of vaccines ed: Immunization. Vaccines and Biologicals; 2006.
- Chojnacky M, Miller W, Ripple D, Strouse G. Thermal Analysis of Refrigeration Systems Used for Vaccine Storage. America: Department of Commerce Gary Locke, Secretary; 2009.
- WHO. PATH. Domestic Refrigerators for Vaccine Storage in Tunisia Conclusion and Recommendations. USA: Vaccines and Biologicals; 2012.
- Anggita Y. Perancangan, Pembuatan, dan Pengujian Pengembangan Berpendingin Termoelektrik. Bandung: ITB; 2015.
- Dinkes. Profil Kesehatan Provinsi Jawa Barat Tahun 2013. Bandung: Dinas Kesehatan Kota Bandung; 2013.
- Kemenkes RI. Riset Kesehatan dasar Tahun 2013. Jakarta: Kementerian Kesehatan Republik Indonesia; 2013.
- Mishra A, Mishra S, Lahariya C, Jain P, Bhadoriya R, Shrivastav D. Practical observations from an epidemiological investigation of a measles outbreak in a district of India. Indian J Community Med. 2009;34(2):117–21.
- Thakur J, Ratho R, Bhatia S, Grover R, Issaivanan M, Ahmed B. Measles outbreak in a Periurban area of Chandigarh: need for improving vaccine coverage and strengthening surveillance. Indian J Pediatr. 2002;69(1):33–7.
- WHO. Annual Cold Chain Management Guide and Record. New Zealand: Ministry of Health; 2012.
- Wilsdon C. How Do Refrigerators Work? New York: ience in the Real World; 2010.
- Nurjanti S. Hubungan Tingkat Pengetahuan Bidan Tentang Imunisasi Dengan Perilaku Pengelolaan Vaksin Di Bidan Praktek Swasta Se-Wilayah Ranting Tengah Bantul Yogyakarta. Jurnal Kesehatan. 2010;1(1).
- Astuti M. Pengaruh Pengetahuan dan Kelengkapan Peralatan Rantai Dingin Terhadap Kualitas Pengelolaan vaksin Oleh Bidan Praktik Mandiri di Kota Bogor. Universitas Padjadjaran; 2013.
- Techathawat S, Varinsathien P, Rasdjarmrearnsook A, Tharmaphornpilas P. Exposure to heat and freezing in the vaccine cold chain in Thailand. Vaccine. 2007;25(7):1328–33.
- Yakum M, Ateudjieu J, Walter E, Watcho P. accine storage and cold chain monitoring in the North West region of Cameroon: a cross sectional study. BMC Res Notes. 2015;8(1):145.
- Kristini TD, Purwanti A, Udiyono. Faktor-Faktor Risiko Kualitas Pengelolaan Vaksin Yang Buruk Di Unit Pelayanan Swasta (Studi Kasus di Kota Semarang). Jurnal Kesehatan Masyarakat. 2008;3(2).
- WHO. Making use of Vaccine Vial Monitors. Geneva: Biologicals DoVa; 2000.
- Rahuh G, Suyitno H, Hadinegoro S, Kartasasmita C, Ismoedijanto, Soedjatmiko. Pedoman Imunisasi Di Indonesia. Jakarta: Badan Penerbit Ikatan Dokter Indonesia; 2014.
- Gomez PL, Robinson JM, Rogalewicz JA. Vaccine manufacturing. Vaccines. 2013;44.
- Mohan T, Verma P, Rao DN. Novel adjuvants & delivery vehicles for vaccines development: a road ahead. The Indian journal of medical research. 2013;138(5):779.
- World Health Organization. Temperature Sensitivity of Vaccines. CH-1211 Geneva 27, Switzerland: Department of Immunization, Vaccines and Biologicals; 2006.
- Chojnacky M, Rodriguez AL. Effect of thermal ballast loading on temperature stability of domestic refrigerators used for vaccine storage. PloS one. 2020;15(7):e0235777.
THE CHILDBIRTH UTILIZATION IN HEALTH FACILITIES IN THE WORKING AREA OF SUNGAI LOKAN PHC TANJUNG JABUNG TIMUR REGENCY: A CROSS SECTIONAL STUDY
Lia Artika Sari1*, Yuli Suryanti1, Enny Susilawati1
- Department of Midwifery, Health Polytechnic of Jambi, Indonesia
* Corresponding author: Lia Artika Sari, Department of Midwifery, Health Polytechnic of Jambi, Indonesia, liaartikasari57@gmail.com
Cita questo articolo
ABSTRACT
Introduction: The low number of deliveries assisted by midwives or health workers is an indicator of the low utilization of health facilities by mothers in labor. This study analyzes the factors related to the utilization of childbirth in health facilities in the Sungai Lokan Community Health Center Work Area, Tanjung Jabung Timur Regency.
Materials and Methods: This research is an analytic observational using a cross-sectional approach involving 74 participants. The research was conducted from January to July 2019 in the Sungai Lokan Health Center Work Area, Tanjung Jabung Timur Regency.
Results: The results showed that the factor of the utilization of childbirth in health facilities was related to family culture (p = 0.0001) and family support (p = 0.003), while the service access factor was not related (p = 0.364).
Conclusion: The role of health workers in socializing the importance of utilizing health facilities as a place of delivery is significant in reducing maternal mortality
Keywords: Health Facilities, Family Culture, Family Support, Access To Services
INTRODUCTION
Maternal Mortality Rate (MMR) is one indicator of success in maternal health programs. MMR is a recapitulation of maternal deaths during pregnancy, childbirth, and the puerperium due to pregnancy, delivery, and postpartum problems or their management per 100,000 live births. Reducing maternal mortality due to complications of pregnancy and childbirth is one of the eight targets of the Millennium Development Goals (MDGs) [1]. Family planning, especially for postpartum mothers and unmet need groups, integrated reproductive health services; strengthened village midwives' function, strengthened the referral system, and reduced financial barriers [2,3].
The achievement of the Millennium Development Goals (MDGs) health workforce target needs to receive support from service providers who are health service providers who have a major role in achieving health development goals [4]. Health workers are also providers of health services to patients in accordance with their professional authority to make optimal health efforts. Midwife is one of the non-medical health workers in accordance with their competence and authority to provide midwifery services which are an integral part of health services [5,6]. Every day, some 7,000 babies die in the first month of life. In 2019, an estimated 2.4 million newborns died worldwide. High Maternal Mortality Rate (MMR) and Infant mortality (IMR) is caused by complications in pregnancy and labor [7]. More in the MDG's target on MMR, as stated in the Roadmap to Accelerate Achievement of the Millennium Development Goals in Indonesia, is to reduce from 228 per 100,000 live births in 2007 to 102 per 100,000 live births in 2015. Coverage of deliveries by health workers in health care facilities in Indonesia based on data from the Profile Indonesian Health in 2017 amounted to 5,078,636 with deliveries assisted by health workers totaling 4,222,506 (83.14%). In 2019, 90.95% of deliveries were assisted by health workers. Meanwhile, pregnant women who underwent childbirth assisted by health workers in health care facilities were 88.75% [1]. Thus, around 2.2% of deliveries are assisted by health workers but are not carried out in health care facilities. The coverage of deliveries in Jambi Province based on Indonesia's health profile data in 2017 was 69,774, with deliveries assisted by health workers at health facilities totaling 25,387 (76.37%) [8]. The government targets 85% of deliveries to be carried out in health care facilities. For this reason, the government seeks to improve the quality of quality health care facilities. It is a matter of being available and affordable [9]. The current condition, Puskesmas, as a primary health service facility owned by the government, already exists in every sub-district; it is just that it is still not evenly distributed so that it is less accessible to the public [10]. As a state administrator, the government is obliged to ensure equity and quality of health services for the community. Physically, equitable distribution of health services can be interpreted as affordability in topographical, demographic, and geographical aspects. Physical topographical affordability is the proximity of the population settlements to health service facilities. Affordability in the demographic aspect means that the Puskesmas can accommodate and serve the health needs of the entire population in the work area [9,11,12]. Another critical factor is the public's misconception about the competence of traditional birth attendants that they are birth attendants that are safe, inexpensive, and able to provide services that health workers cannot provide. It is exacerbated by the absence of family support, especially mothers or mothers-in-law to take advantage of health facilities as a place to give birth.
Several previous studies found that delivery coverage at health facilities was influenced by accessibility factors [13], family support [14,15], mothers knowledge [16]. The results of the study [17] show that one of the causes of neonatal death, in addition to the distance of access to health facilities, is also influenced by birth attendants, namely giving birth to a traditional birth attendant with a risk of causing neonatal death by 12.4 times compared to not giving birth to a traditional birth attendant.
Tanjung Jabung Timur Regency, Indonesia has 17 Health centers, with the number of deliveries in 2018 totaling 4,069, with deliveries assisted by health workers in health facilities totaling 1,512 (37.16%). Specifically, Sungai Lokan Village has one main health center and one secondary Health center with total deliveries in 2018 of 29.58%, namely out of 71 deliveries, health workers assisted only 21 deliveries in health facilities [18]. The low number of deliveries assisted by midwives or health workers is an indicator of the low utilization of health facilities by mothers in labor.
Based on the existing phenomena, we tried to examine the factors related to the utilization of childbirth in health facilities in the Sungai Lokan Community Health Center Work Area, Tanjung Jabung Timur Regency”.
MATERIALS AND METHODS
The research design is a cross-sectional survey. Data collection was carried out by the research team assisted by two midwives from January to July 2019 in the Sungai Lokan Health Center Work Area, Tanjung Jabung Timur Regency. The research population was all mothers who gave birth in the Sungai Lokan Public Health Center, Tanjung Jabung Timur Regency, with a sample of 74 mothers who gave birth and at the same time as respondents who were selected by total sampling with inclusion criteria, namely the mother's place of residence is accessible, the mother is in good health, the mother who lives at home with her in-laws while the mother who does not live at home with her in-laws was excluded from the study. Before the research was carried out, the researcher first asked the mother's consent as a prospective respondent, after the mother signed the consent letter to become a respondent, then the researcher conducted interviews using a questionnaire. The research questionnaire consisted of a questionnaire on Utilization of childbirth in health care facilities consisting of 10 questions, a family culture questionnaire consisting of 10 questions, family support consisting of 10 questions, and an Access to the service questionnaire consisting of 10 questions. when the questionnaire was distributed, the mother was accompanied by a member of the researcher until the questionnaire was completed by the mother.
The study was performed in accordance with the ethical considerations of the Helsinki Declaration. No economic incentives were offered or provided for participation in this study. Ethical eligibility is obtained from the Health Research Ethics Commission of the Health Polytechnic, Jambi Ministry of Health with the number: LB.02.06 / 2/110/2019.
Statistical analysis
Data are presented as numbers and percentages for categorical variables. Continuous data are expressed as the mean ± standard deviation (SD), or median with Interquartile Range (IQR). The chi-square test and Fishers exact test were performed to evaluate significant differences of proportions or percentages between two independent groups. Particularly Fishers exact test was used where the chi-square test was not appropriate. The variables measured were adequate delivery facilities as the dependent variable and family culture, family support, and access to services as independent variables. All tests with p-value (p) < 0.05 were considered significant. Statistical analysis was performed using SPSS app version 16.0.
RESULTS
The research results are then presented in the form of distribution tables and cross-tabulations and then narrated. The following will present research data on research variables, as follows:

Table 1. Frequency distribution of research variables in the working area of Sungai Lokan Public Health Center, Tanjung Jabung Timur Regency.
Table 1 shows that of the 74 respondents, most (71.6%) of respondents will not use health facilities, most (62.2%) of respondents with unsupportive culture, most (58.1%) of respondents do not. Most of them received support from their families (77.0%) were close to the place of service.

Table 2. Results of the analysis of the relationship between the utilization of childbirth in health care facilities with a family culture, family support, and access to services in the working area of
the Sungai Lokan Community Health Center, Tanjung Jabung Timur Regency
In Table 2, it can be seen from 46 respondents with a culture that does not support there are 40 people (87.0%) respondents who will not use health facilities. Meanwhile, out of 28 respondents with a supportive culture, 15 people (53.6%) will use health facilities. The results of statistical tests using the chi-square test obtained a value of p = 0.0001 (p <0.05), meaning that there is a socio-cultural relationship with the use of delivery services in health facilities. Respondents who do not receive family support have 39 people (90.7%) respondents who will not use health facilities. Meanwhile, of the 31 respondents who received family support, 17 (54.8%) respondents would use health facilities. The results of statistical tests using the chi-square test obtained a value of p = 0.003 (p <0.05), meaning that there is a relationship between family support and delivery services in health facilities. Of the 17 respondents with long distances to the four health facilities, 14 (82.4%) respondents would not use the health facilities. Meanwhile, out of 57 respondents with proximity to health facilities, 39 (68.4%) respondents would not use health facilities. The statistical test results using the Fisher Exact test obtained a value of p = 0.364 (p> 0.05), meaning that there is no relationship between distance to the place of service and the utilization of delivery services in health facilities.
DISCUSSION
The question components in family culture variables include the habits of family members to give birth still choose a traditional birth attendant as a birth attendant. In this study it was found that the role of traditional birth attendants was very central and became the family's choice as birth attendants. family habits in giving birth to traditional birth attendants that have been carried out for generations. This has become a culture not only for the respondent's family but also for most of the people in the study area and Indonesia in general. Cultural factors have a very big influence in the selection of birth attendants. Moreover, in rural areas, the position of traditional birth attendants is more respectable, their position is higher than that of midwives, so that from examinations, delivery assistance to postpartum care, many ask for help from traditional birth attendants.
Based on the research results on the socio-cultural community in the working area of the Sungai Lokan Public Health Centre, when approaching delivery, they choose to give birth at home, in addition to being hereditary, because they feel comfortable giving birth at their own home. Some dukuns accompany mothers during childbirth, and some even choose to give birth to be assisted by shamans alone. They also think that their previous children born with the help of a dukun are no different from those who are now being helped by a midwife, apart from feeling comfortable giving birth at their own home because they feel ashamed and reluctant to give birth in a health facility.
The limited use of the national language is also one of the difficulties for the community to communicate with health workers, most of who are not from the local area. So that communication difficulties also make people more comfortable giving birth at their own home and choosing a shaman to help the delivery process. It is in line with Yeni Aryani's research [19], which found that statistical tests showed a relationship between culture and the choice of place of delivery (p = 0.028). The results of the OR (Odds Ratio) of 3.162 indicate that mothers who receive support from culture have a 3.162 times greater chance of choosing a place of delivery in a health facility compared to mothers who do not receive support from culture. In line with research in Rural Uganda which states that for both men and women in the village, the cultural behaviour patterns of the community have the most substantial impact on birth choices [20]. A woman's relationship with her partner and family is also a factor in whether the mother will use health facilities for the birth process or not. In the family role variable, one component of the question in the questionnaire is the husband's role in determining the choice of place to give birth. The husband's role is very dominant in this study determining the place of delivery for the mother. The husband is the head of the household in a family, so the rules in the household should have deliberation with the husband. Therefore, how important is the role of the husband and family in making decisions for choosing the place of delivery. Based on this and previous studies, husband/family support can influence respondents to use health facilities as a place of delivery. It is due to the husband's/family's lack of knowledge about the importance of using health facilities, especially for childbirth due to lack of knowledge of Husband/family regarding the importance of health utilization and the advantages of giving birth in health facilities. Based on the research results from 74 respondents, most of the respondents did not receive support from their families in the working area of Sungai Lokan Public Health Centre, Tanjung Jabung Timur Regency, with a p-value <0.05. In line with previous research at Puskesmas XIII Koto Kampar, obtained p-value (0.010 < 0.05), this means that there is a socio-cultural influence with the selection of birth attendants [21].
The results of this study are also in line with previous research in the working area of the Muara Ancalong Health Centre, Kutai Timur Regency, which found that family support affected the choice of place of delivery with a p-value of 0.019, namely husband and parents, this indicates that the influence of the closest family is considerable on respondents' decision making in choosing a place to give birth [21]. Another study in Kenya showed that family support in the form of funds was associated with the utilization of childbirth in health facilities [22]. The distance from a mother's house to a health facility is closely related to transportation costs and the time it takes to reach it. The closer the distance of a mother's house to a health facility is, the cheaper the costs. Accessibility based on geographical dimensions is related to time and space, which is believed to shape access to health services significantly. If these obstacles are overcome, someone will still think to decide whether the distance is an obstacle. A study states that the low utilization of health services is due to the existence of barriers for the community in accessing preventive, curative, and promotive health services [13].
Based on the study results, from 74 respondents, most of the respondents were close to the place of service in the working area of Sungai Lokan Public Health Center, Tanjung Jabung Timur Regency. It will undoubtedly increase pregnant women's access to give birth to health facilities, but in reality, this condition is very contrary to the respondent's decision not to use health facilities as a place to give birth.
This study indicates that there is no significant relationship between a mother's access to health facilities and the choice of place of delivery. According to the researcher's assumptions, this occurs because people travel long distances by using transportation to get to the garden. Affordability is based on the perception of distance and the presence or absence of private or public vehicles to reach the nearest health facility. Respondents who choose delivery assistance by traditional birth attendants are generally people whose homes are closer to the traditional birth attendant, while respondents who choose birth assistance by midwives need more time to get services because of the longer distance.
Unlike previous research in the work area of the Kawangu Health Centre, the utilization of childbirth in health facilities was influenced by the ability to access health services (p < 0.001) [16]. In this study, transportation limitations with high costs and poor road structures caused pregnant women to prefer to give birth. The difference in the results of this study is that the ability to access services in our study is already high because the distance from pregnant women's homes to the PHC is very close and does not cost a lot, even though the dominant mother decides to be more comfortable giving birth at home.
Conclusions
Most of the respondents did not use health facilities in the working area of Sungai Lokan Health Centre, Tanjung Jabung Timur Regency. Utilization of delivery services in health facilities in the working area of Sungai Lokan Public Health Center, Tanjung Jabung Timur Regency, is related to family culture and family support, while access to services is not related.
Limitation
In this study, there are limitations such as the presence of some areas that cannot be reached by the research team so they cannot participate in the study. Then in this study using a cross-sectional design so that the information obtained by researchers is only limited to data when the research is conducted.
Funding statement
This research did not receive any specific grant from funding agencies in the public, commercial, or not for profit sectors.
Competing interests statement
There are no competing interests for this study.
REFERENCES
- Kemenkes RI. Hasil utama RISKESDAS 2018. Jakarta: Kementerian Kesehatan Badan Penelitian dan Pengembangan Kesehatan. Jakarta; 2018.
- Paul VK, Sachdev HS, Mavalankar D, Ramachandran P, Sankar MJ, Bhandari N, et al. Reproductive health, and child health and nutrition in India: meeting the challenge. The Lancet. 2011;377(9762):332–49.
- Lule E, Ramana GN V, Ooman N, Epp J, Huntington D, Rosen JE. Achieving the millennium development goal of improving maternal health: determinants, interventions and challenges. 2005;
- Tangcharoensathien V, Mills A, Palu T. Accelerating health equity: the key role of universal health coverage in the Sustainable Development Goals. BMC medicine. 2015;13(1):1–5.
- Mansoor GF, Hashemy P, Gohar F, Wood ME, Ayoubi SF, Todd CS. Midwifery retention and coverage and impact on service utilisation in Afghanistan. Midwifery. 2013;29(10):1088–94.
- ten Hoope-Bender P, de Bernis L, Campbell J, Downe S, Fauveau V, Fogstad H, et al. Improvement of maternal and newborn health through midwifery. The Lancet. 2014;384(9949):1226–35.
- Unicef. Newborn and maternal mortality snapshot [Internet]. 2019. Available from: https://www.unicef.org/health/maternal-and-newborn-health
- Dinkes Kota Jambi. Profil Kesehatan Kota Jambi. Jambi; 2018.
- Laksono AD, Mubasyiroh R, Laksmiarti R, Suharmiati EN, Sukoco NE. Aksesibilitas Pelayanan Kesehatan di Indonesia. Yogyakarta: PT Kanisius. 2016.
- Izati ARM. Trend Cakupan Kunjungan Ibu Hamil (K4) Dan Pertolongan Persalinan Oleh tenaga Kesehatan Di Propinsi Jawa Timur. Jurnal Ilmiah Kesehatan Media Husada. 2018;7(1):1–10.
- Senewe FP, Elsi E. Descriptive Analysis to environment health in less development, borderlands, archipelagoes and remote areas (DTPK-T). Media Litbangkes. 2014;24(3):153–60.
- Agustina R, Dartanto T, Sitompul R, Susiloretni KA, Achadi EL, Taher A, et al. Universal health coverage in Indonesia: concept, progress, and challenges. The Lancet. 2019;393(10166):75–102.
- Laksono AD, Sandra C. Analisis Ekologi Persalinan di Fasilitas Pelayanan Kesehatan di Indonesia. Buletin Penelitian Sistem Kesehatan. 2020;23(1):1–9.
- Suci CM. Hubungan Pengetahuan Ibu Dan Dukungan Keluarga Dengan Pemilihan Penolong Persalinan di Wilayah Kerja Puskesmas Pintu Padang Kabupaten Pasaman. Universitas Andalas; 2019.
- Fahriani M, Sitorus E. Hubungan Sikap Ibu Bersalin Dan Dukungan Keluarga Dengan Pemilihan Penolong Persalinan di Wilayah Kerja Puskesmas Nibung Kabupaten Musi Rawas Utara. An-Nadaa: Jurnal Kesehatan Masyarakat. 2020;6(1).
- Adriana N, Wulandari LPL, Duarsa DP, Adriana N, Wulandari LPL, Duarsa DP. Akses pelayanan kesehatan berhubungan dengan pemanfaatan fasilitas persalinan yang memadai di Puskesmas Kawangu. Public Health and Preventive Medicine Archive. 2014;2(2):175–80.
- Kusnan A, Rangki L. Faktor determinan proksi kejadian kematian neonatus di wilayah kerja Dinas Kesehatan Kabupaten Buton Utara. Berita Kedokteran Masyarakat. 2019;35(4):131–8.
- Lokan PDS. Profil Kesehatan Desa Sungai Lokan. 2018.
- Aryani Y, Islaeni I. Hubungan Dukungan Suami dan Budaya Dengan Pemilihan Tempat Persalinan. SEAJOM: The Southeast Asia Journal of Midwifery. 2018;4(1):8–14.
- Dantas JAR, Singh D, Lample M. Factors affecting utilization of health facilities for labour and childbirth: a case study from rural Uganda. BMC Pregnancy and Childbirth [Internet]. 2020;20(1):39. Available from: https://doi.org/10.1186/s12884-019-2674-z
- Nurhapipa N, Seprina Z. Factors Affecting in Choosing the Birth Mother in Health Care Delivery XIII Koto Kampar I. Jurnal Kesehatan Komunitas. 2015;2(6):283–8.
- Kawakatsu Y, Sugishita T, Oruenjo K, Wakhule S, Kibosia K, Were E, et al. Determinants of health facility utilization for childbirth in rural western Kenya: cross-sectional study. BMC pregnancy and childbirth. 2014;14(1):1–10.
DETERMINANTS OF BREASTFEEDING EXCLUSIVE IN THE WORKING AREA OF RUMBIA HEALTH CENTER, BOMBANA REGENCY: A CROSS SECTIONAL STUDY
Asnidawati1, Wa Ode Salma2*, Adius Kusnan3
- Public Health of Faculty, Haluoleo University, Kendari, Indonesia
- Nutrition department, Public Health of Faculty, Haluoleo University, Kendari, Indonesia
- Nursing department, Medical of Faculty, Haluoleo University, Kendari, Indonesia
* Corresponding Author: Wa Ode Salma, waode.salma@uho.ac.id, Nutrition department, Public Health of Faculty, Haluoleo University, Kendari, Indonesia
Cita questo articolo
ABSTRACT
Background: Breast’s milk is an excellent food for the growth and development of infants. The United Nations Children's Funds (UNICEF) and the World Health Organization (WHO) recommend that children only be exclusively breastfed for six months and continued until two years. This study analyzes the effect of family support, health workers, and socio-culture on exclusive breastfeeding in the working area of the Rumbia Health Center, Rumbia District, Bombana Regency.
Methods: This study involved 86 mothers who had babies aged 0-6 months who were registered and domiciled in the working area of the Rumbia Health Center spread over 4 Kelurahan and 1 Village, which were selected by purposive sampling using a cross-sectional design from February to April 2021. Data analysis using odds ratio (OR) and logistic regression at significance level < 0.05.
Results: The largest age group in the range of 20-35 years, as many as 68 people (79.1%), undergraduate as many as 32 people (37.2%), and income above Rp. 2.552.014, - / month as many as 60 people (69.8%). The results showed an effect of family support on exclusive breastfeeding (p = 0.002<0.05). There is no influence of socio-cultural factors on exclusive breastfeeding (p = 0.282>0.05) and the results of multivariate analysis of the most dominant variables associated with exclusive breastfeeding in the working area of Rumbia Health Center District Rumbia Bombana Regency is supported by health workers with an OR = 9.199 (p-value = 0.039<0.05).
Conclusions: This study concludes that the support of health workers plays a very important role in exclusive breastfeeding to infants aged six months, which can impact improving the health of toddlers.
Keywords: Determinant, breastfeeding exclusive, toddler, mother
INTRODUCTION
Breast milk is an ideal food for infant growth and development [1,2]. The United Nations Children's Funds (UNICEF) and the World Health Organization (WHO) recommend that children be breastfed exclusively for six months and continued until two years. Global research reports in 2018 showed that the rate of exclusive breastfeeding was quite low, only 41 percent [3]. Meanwhile, in Indonesia, data from the Basic Health Research (RISKESDAS) in 2018 showed that the rate of exclusive breastfeeding was only 37 percent [4]. It is known that the rate of exclusive breastfeeding is still low globally, and it is possible that in Indonesia, the coverage rate of exclusive breastfeeding is below 37% due to the consequences of the Covid-19 pandemic [5].
The study results in 19 developing countries show that socio-cultural factors such as maternal beliefs and other people are significantly strong barriers to exclusive breastfeeding [6–8]. Another study reported that in general, mothers know about breastfeeding, and the majority of respondents (97.3%) had breastfed their babies, 56.5% of them started within one hour after delivery, and 74.1% only gave exclusive breastfeeding until a mean age of 4 months and 30.7% had bottle-fed [9].
The importance of appropriate breastfeeding practices for the healthy growth and development of infants and children has been presented in various policy documents, and guidelines have been set on how to practice exclusive breastfeeding [10]. Social support is widely recognized as influencing the practice of breastfeeding exclusively for six months and continuing to breastfeed for at least two years [11,12]. In addition, health care worker supporting interventions have been shown to increase the rate of exclusive breastfeeding in many developing countries [13,14].
The coverage of achieving exclusive breastfeeding in 2017 in Southeast Sulawesi province for infants 0-6 months was 55.56%, and the coverage of achieving exclusive breastfeeding in 2018 increased by 72%. Although it increased from the previous year, it was not significant and still far from the national target (80%) and the target for Southeast Sulawesi Province (85%). Fluctuating achievements indicate that the exclusive breastfeeding improvement program is not standardized by related technical programs [15]. The working area of the Rumbia Health Center is 40.74%. It is still far from the target set, 50% [16].
The coverage of exclusive breastfeeding in the working area of the Rumbia Health Center has continued to decline over the last three years. It is known that the results of data observations at the Rumbia Health Center showed that data related to mothers who brought their babies to come to the Posyandu in March 2020 recorded only 63 babies and 14 babies who received exclusive breastfeeding while 49 babies were not exclusive. Still far from the expected target of 108 infants (aged 0-6 months). It means that only about 22% of babies get exclusive breastfeeding, and 78% of babies do not get exclusive breastfeeding.
The outbreak of the covid-19 virus has greatly impacted health services, especially Posyandu services in the working area of the Bombana district office, since it was announced that there were residents in Bombana Regency who were confirmed on Covid-19. Overall, Posyandu services at the Rumbia Health Center and other health centers in Bombana Regency are no longer organize the Integrated health service from April to May 2020; therefore, services, data collection, and counseling related to exclusive breastfeeding are not well controlled.
Based on the available scientific data and evidence, this research was conducted to find out how to the influence of family support, health workers, and socio-culture on exclusive breastfeeding in the working area of the Bombana District Health Office, especially at the Rumbia Health Center.
METHODS
Study design
This type of research is analytic observational using a cross sectional design with a purposive sampling technique, so that each participant in this study was selected based on the researcher's considerations.
Participants Sampling
This study involved 86 mothers who had babies aged 0-6 months who were registered and domiciled in the working area of the Rumbia Health Center spread over 4 Kelurahan and 1 Village
Procedure Inclusion and exclusion criteria
To control the quality of research data, the researchers conducted an initial screening by setting sample criteria. The sample inclusion criteria were mothers who had babies aged 0-6 months, mothers who did not experience psychosomatic disorders, while babies who were sick during the study and were born with low birth weight were excluded from the study.
Instruments
In this study involved 3 variables, namely family support, Healthcare worker support and Social-Culture. All variables in this study were measured using a questionnaire which was prepared by the researcher himself by taking into account relevant reference sources [17–19] and had been tested and declared valid and reliable.
Statistical Analysis
Data are presented as numbers and percentages for categorical variables. Continuous data are expressed as the mean ± standard deviation (SD), or median with Interquartile Range (IQR). Data analysis in this study used the Odds Ratio (OR) test to determine the factors associated with breastfeeding exclusivity and multivariate analysis used logistic regression to determine the determinants of breastfeeding exclusivity. The results of the p-value will be the basis for the independent variables to be included in the logistic regression test if p < 0.30, while the dependent variable in the study was the provision of Breastfeeding Exclusive, which was measured using a questionnaire. All tests with p-value (p) < 0.05 were considered significant. Statistical analysis was performed using SPSS app version 16.0.
Ethical consideration
All participants in this study have signed a letter of willingness to participate in the study. No economic incentives were offered or provided for participation in this study. The study was performed in accordance with the ethical considerations of the Helsinki Declaration. This research has been approved by the Haluoleo University Health Research Ethics Commission numbered: 21/KEPK-IAKMI/III/2021.
RESULTS
In the results of this study, the characteristics of the mother, distribution of research variables, results of bivariate and multivariate analysis are presented. The distribution of respondents' characteristics can be seen in the following Table 1:
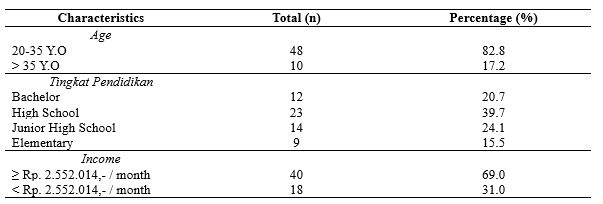
Table 1. Distribution of Respondents’ characteristics
Table 1 informs the largest age group in the range of 20-35 years, as many as 48 people (82.8%), high school as many as 23 people (39.7%), and income above Rp. 2.552.014, - / month as many as 40 people (69.0%).
Table 2 shows the distribution of the dominant study variables consisting of 50 people (58.1%) receiving family support, 67 mothers who received support from health workers (77.9%), and 79 mothers with good socio-culture. (91.9%). There is an effect of family support (p=0.002) and Healthcare worker support (p=0.004) on exclusive breast-feed. There is no influence of socio-cultural factors on the exclusive breastfeeding (p = 0.282).
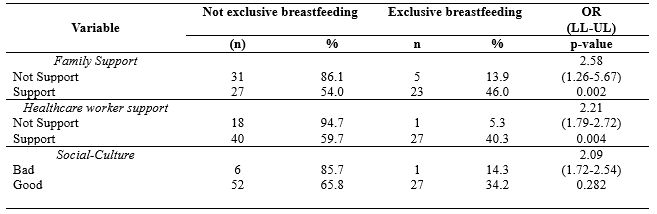
Table 2. Distribution of Study variable
Table 3 shows that after all independent variables were analyzed multivariate with logistic regression, the results obtained that the support of health workers had the greatest OR, namely 4.350 at 95% Cl with a lower limit value of 1.114 and an upper limit value of 75.974 because the confidence interval range was not. Including a value of 1 means that health workers support exclusive breastfeeding in the Work Area of the Rumbia Health Center, Rumbia District, Bombana Regency.
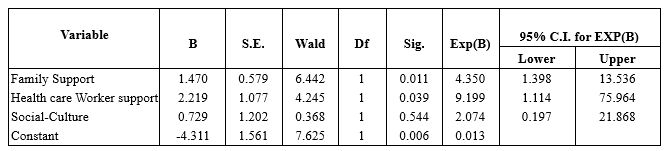
Table 3. Multivariate Analysis
DISCUSSION
- The Effect of Family Support on Exclusive Breastfeeding
The study results found that there was an effect of family support on exclusive breastfeeding in the working area of the Rumbia Health Center, Rumbia District, Bombana Regency. The results of this study are supported by several previous studies that state that exclusive breastfeeding success is closely related to family support, especially husbands and grandmothers of toddlers [20–22].
A mother needs support from the family in providing exclusive breastfeeding; support from the family will affect the mother's decision to give exclusive breastfeeding [23]. The success in providing exclusive breastfeeding by mothers is very dependent on the environment, one of which is the husband or family. If mothers get support from the surrounding environment, mothers can comfortably provide exclusive breastfeeding and take care of their children while working at home. Support or support from other people or closest people, both family support and support from health workers, is very important in the success or failure of breastfeeding [24]. The greater support to continue breastfeeding, it makes the greater the ability to continue breastfeeding. Husband and family support is very influential; a mother who lacks her husband, mother, sister, or even being scared, is influenced to switch to formula milk [25].
The success factor of exclusive breastfeeding, in addition to knowledge, to be cleared, is accompanied by the mother's own will. The role of health workers is very influential on the mother in the process of exclusive breastfeeding. The success of exclusive breastfeeding cannot be separated from family support because the family is the closest person who can encourage mothers to continue giving exclusive breastfeeding and the surrounding culture that encourages exclusive breastfeeding [26].
Family, apart from being a supporting factor, is also as retarder factor. The mother's desire to give exclusive breastfeeding should have been discussed with the family, especially people who will live with the mother when the baby is born, for example, husband, mother, mother-in-law long before the baby is born or at least during the pregnancy phase [27]. In still to families regarding the importance of breastfeeding, how to give exclusive breastfeeding and what support they can provide. It is important, because in some cases, a mother's failure to provide exclusive breastfeeding is precisely because of a misunderstanding from the family, for example, being given water, so the baby does not turn yellow, or adding a baby with formula milk because the baby cries and thinks the baby is still hungry and hungry. At that time, the baby's mother had difficulty refusing or resisting because the one who gave it was the mother-in-law and her biological mother. This event will be minimized when the mother and family have good breastfeeding knowledge and a strong agreement and commitment to supporting mothers in exclusive breastfeeding.
- The Effect of Health Worker Support on Exclusive Breastfeeding
The study results found that there was an effect of the support of health workers on exclusive breastfeeding in the working area of the Rumbia Health Center, Rumbia District, Bombana Regency. Furthermore, the results of the multivariate analysis of this study found that the most dominant variable influencing exclusive breastfeeding in the working area of the Rumbia Health Center, Rumbia District, Bombana Regency, was the support of health workers with an OR value of 9.633.
According to the theory, the support of officers is very helpful, where the support of officers has a big influence on exclusive breastfeeding [22]. A health worker is responsible for health workers who provide health services to individuals, families, and communities. If health workers actively socialize with the community, they can change traditions or habits that can slowly harm health, such as providing complementary foods to infants before six months [28]. Thus, the public will know and understand more about traditional practices that can be detrimental to health so that they will change their behavior and mindset towards what they know from the health worker [29]. The encouragement of health workers can influence respondents to have a high intention of giving exclusive breastfeeding to their babies. The success of breastfeeding mothers requires health workers, especially perinatal service workers such as midwives who are trained and understand the ins and outs of the breastfeeding process. They are the first to help mothers give birth to give breast milk to babies. The role of health workers is the beginning of the mother's success or failure in exclusive breastfeeding. Knowledge, attitudes, and actions of health workers such as midwives are the determinants of the readiness of officers in managing breastfeeding mothers with lactation management (lactation management) so that the implementation of exclusive breastfeeding increases.
This study is in line with previous studies concluding that there is a relationship between the support of health workers and exclusive breastfeeding (p-value = 0.0001) with a PR of 2.48, meaning that mothers who receive support from midwives have a 2.48 times greater chance of breastfeeding independently—exclusively compared to mothers who received less support from the midwife [28]. Furthermore, in line with other research in South Tomohon, it shows a relationship between the support of health workers in exclusive breastfeeding for six months in the Pangolombian Community Health Center, South Tomohon District, p-value = 0.008 [30].
- The Influence of Socio-Cultural Factors on Exclusive Breastfeeding
The results showed no influence of socio-cultural factors on exclusive breastfeeding in the working area of the Rumbia Health Center, Rumbia District, Bombana Regency. Breastfeeding cannot be separated from the cultural order. Every breastfeeding from mother to child will be related to the social culture that exists in the community. Behavior is formed by habits that are colored by social culture. Everyone is always exposed and touched by environmental habits and is influenced by the community, either directly or indirectly. Behavior that habits and beliefs have shaped about exclusive breastfeeding will impact the mother's desire to give exclusive breastfeeding to children. This socio-cultural will affect the success of exclusive breastfeeding; respondents who have good socio-cultural categories will show success in exclusive breastfeeding. The good social culture indicates it in providing exclusive breastfeeding, as many as 27 people (34.2%) and those who do not give exclusive breastfeeding, as many as 52 people (65.8%) while out of 7 respondents with poor socio-culture giving exclusive breastfeeding, one person (14.3%) and who did not give exclusive breastfeeding were six people (85.7%). The beliefs and traditions that exist in the community lead to the community's mindset on the actions taken to respond to something. Beliefs that exist in society are very important in shaping a person's behavior.
A study conducted [31] in Athens, Greece, found that the breastfeeding process is often not determined by biological factors but is mainly based on habits, traditions, and behaviors in society. Tradition is a social behavior where the behavior is passed down from generation to generation by going through socialization. A tradition determines the values and morals of society because tradition contains rules according to the community about what should be done.
Habits are carried out from generation to generation and carried out by the community, the judge, and assumes that it is the most correct and good thing [32]. The mother's beliefs and desires to imitate the mother's intention to breastfeed her baby. The respondent's intention to do exclusive breastfeeding is influenced by the mother's own beliefs and beliefs [33]. Logically, the existence of a tradition in Rumbia District regarding breastfeeding is closely related to the mother's intentions and expectations regarding exclusive breastfeeding success. Traditions and beliefs develop a pattern to lead people's behavior to do things under the traditions and beliefs that exist in their environment, such as colostrum contained in breast milk are not good and dangerous for babies, special teas or liquids are needed by babies before breastfeeding, and babies will experience a lack of nutrients for growth if only given breast milk [34].
Unfulfilled breast milk needs will cause malnutrition in children—some dietary restrictions at certain times and certain types of food that should not be eaten while breastfeeding. The lack of knowledge of mothers about nutrition and their beliefs causes nutritional problems for their children and impacts the body's defense against infection and delays in growth and development [35]. Interventions promoting behavior change should focus on dispelling less than optimal beliefs and practices into beliefs to build positive breastfeeding practices, involving family support (partners and other family members) as they are an important source of information about breastfeeding [36,37]. Changing people's habits and beliefs is not an easy task, so the role of health workers is very much needed to carry out activities to increase exclusive breastfeeding programs. Guidelines for increasing exclusive breastfeeding programs cannot be separated from the reproductive process of mothers after giving birth, which is expected to change the behavior of people who initially do not believe in the benefits and benefits of breastfeeding to believe and slowly leave the culture and tradition of giving additional food to infants aged 0-6 months. which can interfere with health [38].
The development of community and religious leaders is an important strategy for the health workforce because people tend to obey the directions of trusted people around their environment than people outside their environment. Community empowerment about the importance of exclusive breastfeeding for babies is known by all levels of society, which is expected to provide support and motivation for breastfeeding mothers and can automatically improve reproductive health.
CONCLUSIONS
The success of the Breastfeeding exclusive program is strongly influenced by various factors such as family support such as husbands and grandmothers of toddlers, as well as support from health workers through promotional programs when mothers of toddlers visit health care facilities, as well as socio-cultural factors that are believed by the family such as the existence of dietary restrictions for babies of a certain age, babies born must be given sweet food immediately, at a certain age babies must be given food in traditional events.
This study suggests the importance of the role of health workers in providing a good understanding to families about the benefits of exclusive breastfeeding until the baby is 6 months old.
Limitations study's
In this study, there are limitations such as the presence of some areas that cannot be reached by the research team so they cannot participate in the study. Then in this study using a cross-sectional design so that the information obtained by researchers is only limited to data when the research is conducted.
Clinical implications of research
The results of this study can be the basis for health workers in maximizing the role of the family in supporting mothers to provide exclusive breastfeeding to infants and paying attention to the socio-cultural background of the family, especially mothers in providing interventions in the field, especially regarding exclusive breastfeeding.
ACKNOWLEDGEMENT
We would like to express our gratitude to several parties who have provided support for our research. To the chief of the Poltekkes Jambi in her support in providing suggestions and input for the development of this research, and to mothers who have actively participated as respondents in this research.
FUNDING STATEMENT
This research did not receive any specific grant from funding agencies in the public, commercial, or not for profit sectors.
CONFLICT OF INTEREST
The author(s) declares no conflict of interest.
REFERENCES
- Meier PP, Patel AL, Bigger HR, Rossman B, Engstrom JL. Supporting breastfeeding in the neonatal intensive care unit: Rush Mother’s Milk Club as a case study of evidence-based care. Pediatric Clinics. 2013;60(1):209–26.
- Piemontese P, Liotto N, Mallardi D, Roggero P, Puricelli V, Giannì ML, et al. The effect of human milk on modulating the quality of growth in preterm infants. Frontiers in pediatrics. 2018;6:291.
- Osibogun OO, Olufunlayo TF, Oyibo SO. Knowledge, attitude and support for exclusive breastfeeding among bankers in Mainland Local Government in Lagos State, Nigeria. International breastfeeding journal. 2018;13(1):1–7.
- Kementerian Kesehatan. Profil Kesehatan Indonesia. Jakarta: Depkes RI; 2018.
- Unicef. Breastfeeding: a mother’s gift, for every child. Unicef; 2018.
- Balogun OO, Dagvadorj A, Anigo KM, Ota E, Sasaki S. Factors influencing breastfeeding exclusivity during the first 6 months of life in developing countries: a quantitative and qualitative systematic review. Maternal & child nutrition. 2015;11(4):433–51.
- Nsiah-Asamoah C, Doku DT, Agblorti S. Mothers’ and Grandmothers’ misconceptions and socio-cultural factors as barriers to exclusive breastfeeding: A qualitative study involving Health Workers in two rural districts of Ghana. PloS one. 2020;15(9):e0239278.
- Henry BA, Nicolau AIO, Américo CF, Ximenes LB, Bernheim RG, Oriá MOB. Socio-Cultural factors influencing breastfeeding practices among low-income women in Fortaleza-Ceará-Brazil: a Leininger’s Sunrise Model Perspective. Enfermería Global. 2010;19:1–13.
- Akinyinka MR, Olatona FA, Oluwole EO. Breastfeeding knowledge and practices among mothers of children under 2 years of age living in a military barrack in Southwest Nigeria. International Journal of MCH and AIDS. 2016;5(1):1.
- Tampah-Naah AM, Kumi-Kyereme A, Amo-Adjei J. Maternal challenges of exclusive breastfeeding and complementary feeding in Ghana. PloS one. 2019;14(5):e0215285.
- Laugen CM, Islam N, Janssen PA. Social support and exclusive breast feeding among Canadian women. Paediatric and perinatal epidemiology. 2016;30(5):430–8.
- Casal CS, Lei A, Young SL, Tuthill EL. A critical review of instruments measuring breastfeeding attitudes, knowledge, and social support. Journal of Human Lactation. 2017;33(1):21–47.
- Boateng M. Knowledge, attitude and practice of exclusive breastfeeding among mothers in Techiman, Ghana. Itä-Suomen yliopisto; 2018.
- Imdad A, Yakoob MY, Bhutta ZA. Effect of breastfeeding promotion interventions on breastfeeding rates, with special focus on developing countries. BMC public health. 2011;11(3):1–8.
- Dinkes Propinsi Sultra. Profil Kesehatan Propinsi Sulawesi Tenggara 2019. Kendari: Bidang Data dan Informasi; 2019.
- Dinkes Kabupaten Bombana. Profil Kesehatan. Rumbia: Bidang Data dan Informasi Kab/Bombana; 2019.
- Ramadani M. Dukungan keluarga sebagai faktor dominan keberhasilan menyusui eksklusif. Media Kesehatan Masyarakat Indonesia. 2017;13(1):34–41.
- Sitohang FD, Kahar IA, Sirait A. Faktor yang Berhubungan dengan Pemberian Asi Eksklusif pada Bayi Usia 6-12 Bulan di Wilayah Kerja Puskesmas Sigalingging Kabupaten Dairi Tahun 2017. Jurnal Ilmiah Keperawatan Imelda. 2019;5(1):568–78.
- Fajar NA, Purnama DH, Destriatania S, Ningsih N. Hubungan Pemberian ASI Eksklusif dalam Prespektif Sosial Budaya di Kota Palembang. JOURNAL-JIKM: JURNAL ILMU KESEHATAN MASYARAKAT. 2018;9(3):226–34.
- Nuzulia F. Hubungan antara dukungan keluarga dengan pemberian ASI eksklusif pada bayi di Desa Bebengan Kecamatan Boja Kabupaten Kendal. Jurnal Keperawatan Maternitas. 2013;1(1).
- Ratnasari D, Paramashanti BA, Hadi H, Yugistyowati A, Astiti D, Nurhayati E. Family support and exclusive breastfeeding among Yogyakarta mothers in employment. Asia Pacific journal of clinical nutrition. 2017;26(Supplement):S31.
- Kusumayanti N, Nindya TS. Hubungan dukungan suami dengan pemberian asi eksklusif di daerah perdesaan. Media Gizi Indonesia. 2017;12(2):98–106.
- Ku C, Chow SKY. Factors influencing the practice of exclusive breastfeeding among Hong Kong Chinese women: a questionnaire survey. Journal of clinical nursing. 2010;19(17‐18):2434–45.
- La Aga, Erwin AL. Cakupan dan Determinan Pemberian ASI Eksklusif di Pemukiman Kumuh Dalam Perkotaan di Kecamatan Tallo Kota Makassar. Majalah Kesehatan FKUB. 2019;6(1):44–55.
- Novena K. Hubungan Dukungan Keluarga terhadap Keberhasilan ASI Eksklusif pada Bayi Usia 0-6 Bulan di BPM Nihayatur Rokhmah Kuningan Kabupaten Blitar. STIKes Patria Husada Blitar; 2019.
- Hety DS, Susanti IY, Adiesti F, Muhith A. Maternal Knowledge, Husband’s Support, Cultural Support and Role of Health Workers in the Exclusive Breastfeeding Program at Mojosari Health Center. In: Proceedings of the Third International Seminar on Recent Language, Literature, and Local Culture Studies. Proceedings Series Journals Search EAI; 2020.
- Deslima N, Misnaniarti M, Zulkarnain HM. Analisis Hubungan Inisisi Menyusu Dini (IMD) Terhadap Pemberian ASI Eksklusif di Wilayah Kerja Puskesmas Makrayu Kota Palembang. JUMANTIK (Jurnal Ilmiah Penelitian Kesehatan). 2019;4(1):1–14.
- Zuhrotunida. Hubungan Dukungan Tenaga Kesehatan Dengan Keberhasilan ASI Eksklusif di Puskesmas Kutabumi. IMJ (Indonesian Midwifery Journal). 2018;1(2).
- Mi’rad KA, Agushybana F, Margawati A. Study of Madurese Perception and Behavior towards Maternal Health in Jember Regency. International Journal of Multicultural and Multireligious Understanding. 2020;7(3):273–82.
- Anita, Wantania J, Korompis M. Hubungan Antara Pengetahuan Ibu, Fasilitas Pelayanan Kesehatan, Dukungan Keluarga Dan Dukungan Petugas Dengan Pemberian Asi Ekslusif 6 Bulan Di Wilayah Kerja Puskesmas Pangolombian Kecamatan Tomohon Selatan. Paradigma. 2016;4(2).
- Daglas M, Antoniou E. Cultural Views and Practices Related to Breastfeeding. Health science journal. 2012;6(2):353.
- Kusnan A, Binekada IMC, Usman AN. The proxy determinant of complementary feeding of the breastfed child delivery in less than 6 months old infant in the fishing community of Buton tribe. Enfermeria clinica. 2020;30:544–7.
- Yusrina A, Devy SR. Faktor Yang Mempengaruhi Niat Ibu Memberikan ASI Eksklusif di Kelurahan Magersari, Sidoarjo. Jurnal Promkes: The Indonesian Journal of Health Promotion and Health Education. 2016;4(1):11–21.
- Hatta GR. Pedoman Manajemen Informasi Kesehatan di sarana pelayanan kesehatan. Jakarta: Universitas Indonesia. 2008.
- Salma WO, Suhadi LOMS, Irma A, Karo M. Rendahnya Pemberian ASI Eksklusif Pada Anak Etnik Pesisir Berhubungan dengan Kejadian Penyakit Tropis. Penguatan dan Inovasi Pelayanan Kesehatan. 2019;87.
- Wanjohi M, Griffiths P, Wekesah F, Muriuki P, Muhia N, Musoke RN, et al. Sociocultural factors influencing breastfeeding practices in two slums in Nairobi, Kenya. International breastfeeding journal. 2016;12(1):1–8.
- Joseph FI, Earland J. A qualitative exploration of the sociocultural determinants of exclusive breastfeeding practices among rural mothers, North West Nigeria. International breastfeeding journal. 2019;14(1):1–11.
- Batubara NS. Pengaruh Sosial Budaya Terhadap Pemberian ASI Eksklusif di Wilayah Kerja Puskesmas Batunadua Kota Padangsidimpuan Tahun 2015. Jurnal Kesehatan Ilmiah Indonesia (Indonesian Health Scientific Journal). 2016;1(1):59–66.
Occupational Health and Safety for Nurses: Literature Review
Antonio Brusini.1
- Nurse in Sports Medicine, AUSL Modena, Alma Mater Studiorum university tutor, Bologna
Corresponding author: Brusini A., nurse in Sports Medicine at AUSL Modena, master's degree in "Management of Sport and Motor Activities". Email: antoniobrusini87@outlook.it
Cita questo articolo
ABSTRACT
Introduction: The prevention of occupational accidents in the sphere of occupational health and safety is an important issue in the Italian work setting; health workers, and especially nurses, are continually exposed to the risk of work-related accidents, which can affect the quality of care provided.
Aim: The aim of this review is to investigate the nurse's perceived level of preparedness with regard to occupational safety.
Methods: A narrative review of the literature was conducted using some of the main databases such as PubMed, CINAHL and Cochrane.
Results: The studies analysed show that Italian nurses have little knowledge about occupational health and safety legislation.
Conclusions: Establishing specific postgraduate training events and identifying specific legislation for healthcare personnel could represent essential steps towards implementing this specific knowledge.
Keywords: Prevention; Training; Nurses; Healthcare workers
Introduction
Occupational safety has always been a central issue in the Italian working environment [1]: in 2019, 641,638 accidents at work were reported by December 2019 (640,723 in 2018), 100,905 of these took place on the journey between home and workplace (98,446 in 2018) and 540,733 in the workplace (542,277 in 2018), with 1089 fatal accidents at work (1133 in 2018) [2].
A key area for safeguarding workers, including nurses, is training, which is a useful tool for working safely [3]. Indeed, the risk of injury has increased during the COVID-19 pandemic period (131,090 reports of injuries due to COVID-19 infection in the workplace in 2020 [4]). Fewer accidents would lead to reduced expenditure, related to the cost of treatment, lost working days and replacement of the injured worker. In the UK, for example, in the 2011–12 season, there was a quantifiable loss of 10.4 million working days and a consequent reduction in productivity linked to work-related stress injuries.
The specific high-risk topics to be covered during the course include accident risks; general mechanical risks; general electrical risks; machinery; equipment; falls from height; explosion risks; chemical risks; mists, oils, fumes, vapours, dusts; labelling; carcinogenic risks; biological risks; physical risks; noise; vibration; radiation; microclimate and lighting; display screens; PPE; work organisation; working environments; work-related stress; manual handling of loads; handling of goods (lifting equipment, means of transport); signposting; emergencies; safety procedures with reference to the specific risk profile (high in this case); escape and fire procedures; organisational procedures for first aid; accidents and near misses; other risks. Any further training is at the discretion of the employer, who may decide to give his or her staff additional training [6,7].
Objective
The aim of this study is to investigate, through a narrative review of the literature, nurses' knowledge of occupational safety.
Methods
PubMed, CINAHL and Cochrane databases were used as a search medium, and all databases were searched on 28/02/2021 for the set of keywords: 'occupational', 'health', 'safety', 'nurse', without Boolean operators between them. No time limit was given to the research, and only English-language sources were taken into account.
This search yielded 422 results on the Cochrane database (using the 'all text' filter); the same search yielded 2418 results on the Pubmed database and 631 results on CINAHL; of these, 3 articles could not be traced (2 on PubMed and 1 on CINAHL). Only studies that discussed the topic of occupational health and safety training and that had carried out a survey in the form of a questionnaire or other methods on training or nurses' perceptions of training in their workplaces were included. Studies involving an education or training programme for nurses who had carried out a survey of subject knowledge prior to the intervention then performed in the study were also taken into account. The selected studies were carried out on a nursing population or included nurses among other professions in the sample. The outcomes to be studied were the survey responses of the studies on the level of preparedness in the field of occupational safety and, if not reported in quantitative terms, the authors' considerations.
Results
Articles concerning the figure of the 'Occupational Health Nurse/Nursing' were excluded (Table 1), as it is a figure that specifically deals with occupational health and safety but is not present in Italy, as were repeat sources. After reading the title, 22 sources on Cochrane, 515 on PubMed and 80 on CINAHL were retained.
All articles other than primary studies were excluded. After reading the abstract and the article, 10 articles were selected (1 on Cochrane and Pubmed, 5 on Pubmed and CINAHL, 4 on Pubmed only). Duplicate results were skimmed after the results selection. 2 results concern nurses together with other health professionals, 1 result involves nurses and nursing managers.
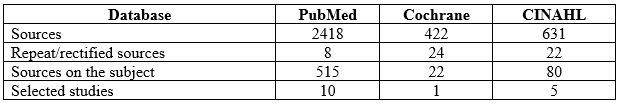
Table 1: Databases consulted, sources found and selected
The detailed procedure used in the selection of articles is presented as a flow chart in Figure 1.

Figure 1. Diagram showing the stages of the review and article selection
Table 2 shows the studies classified by author, year, health personnel involved in the study, method, number of participants and results.
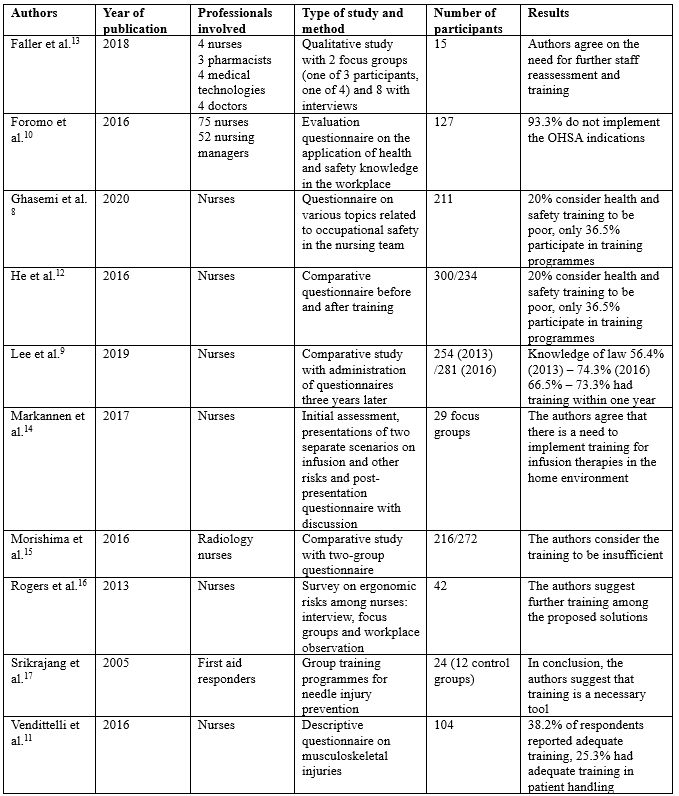
Table 2: Citations on training for nurses and healthcare professionals in the literature found, in alphabetical order by the author. OHSA 'Occupational Health and Safety Act', MAPO Movimentazione Assistita Pazienti Ospedalieri (Assisted Handling of Hospital Patients)
Ghasemi [8] conducted a study surveying 211 nurses by asking questions on various topics related to teamwork safety (nurse relationships, accumulated fatigue, communication with physiatrists, supervisor attitude, nursing unit conditions, error reporting, and nursing training), finding that 20% of respondents considered health and safety training to be poor, and only 36.5% participated in occupational safety training programmes. Lee [9] surveyed knowledge of the law that came out in California in 2012 on patient handling, one year (2013) and three years (2016) later, finding 56.4% of nurses in 2013 and 74.3% of nurses in 2016 were familiar with the current law, with those figures changing to 66.5% and 73.3% respectively for nurses who had received training in patient handling within the past year. Foromo [10] administered an evaluation questionnaire to 75 nurses and 52 'nursing managers' asking whether health and safety regulations were implemented in the workplace and found that 93.3% were not implementing the correct instructions. Vendittelli [11] administered an online questionnaire with scales of 1 to 5 (and the optional possibility to write comments) to 104 nurses who graduated between 2011 and 2014 (offered to 435 in total, with only 104 participating), marking demographics, training (and incidence) in occupational safety, including in mobility procedures, and general nursing training, with only 38.2% stating that they had received adequate training specific to their operating unit, and only 25.3% stating that they had adequate time for training in patient handling. He [12] administered a comparative questionnaire between two groups, before and after a training programme on the topic of HIV/AIDS, and the awareness of HIV/AIDS-related knowledge improved significantly after the training (correct answers increased from 67.9% to 82.34%, on risk perception from 54.4% to 66.6%).
Faller [13] conducted a qualitative study with various healthcare professionals using instruments such as interviews and focus group discussions on some focal points (experience of accidents at work, implementations, barriers and strategies to improve safety), and eight groups with semi-structured interviews, and indicated the genuine need for further training and investigation of staff competences in the field of safety. Markannen [14] worked mainly on prevention in infusion practice, presenting possible working situations in focus groups, with pre- and post-intervention evaluation questionnaires, and agreeing on the need to implement training in home care. Morishima [15] administered a questionnaire to two groups of health professionals, one in 2008 and one in 2010, on the subject of radiation: whether there are different types (24.5% responded positively in 2008 and 40.3% in 2010), about the external protection procedure (17.6% and 26.7% positive responses respectively), the correct distance to the machine (31.5% and 41.5%) and the correct position of the dosimeter (60.8% and 55.1%). Rogers [16] conducted an investigation into the ergonomic risks of the nursing profession through focus groups, interviews and workplace observations of 42 registered nurses in five hospitals in North Carolina, finding training to be one of the main tools in preventing ergonomic risks. Finally, Srikrajang [17] conducted a study on a group of 24 emergency and laboratory health workers (including a control group of 12), demonstrating improvements with the use of training tools in preventing needlestick injuries.
Discussion
The literature review identified few sources, most agreeing that participants in the various studies show structural deficiencies in occupational health and safety training, calling for thorough training interventions. The results show that a significant number of nurses are not familiar with their state's occupational health and safety legislation, and there are many nurses who are not familiar with risk factors and how to work as safely as possible. In fact, the pandemic period, as pointed out by Giorgi [18], highlighted a particular situation for care staff with consequent stress due both to the working conditions resulting from a higher-than-normal workload due to the emergency both in terms of working hours and in terms of working conditions (overload of patients and the continuous use of personal protective equipment (PPE) to which they were not accustomed, except in very few departments, greater emotional involvement) and to the condition that in some settings was already present before the pandemic. Moreover, there is continuous exposure to biological risk due to possible contagion between patient and operator and between operators, no longer represented almost exclusively by contact with biological liquids, although as shown by Maida [19], there is still a need for training also in this type of risk. The COVID-19 pandemic, therefore, exaggerated the possibility of an accident at work, without any clear preparation for the event. The lack of training on the correct handling of the equipment, and the impossibility of training during the lockdown period, led to a substantial change in the training offer in the field of occupational health and safety, with an increase in online portals. The example of FadinMed (https://www.fadinmed.it/) was necessary, as it offered courses, together with the Ministry's portals, useful for training on the use of PPE during a pandemic.
A possible improvement in an Italian perspective for nurses would be the conferral of the management of training topics on occupational health and safety by the professional order (for each health category, it is compulsory to be registered; nurses must be registered with the Professional Order of Nurses, FNOPI): in the case of nurses, it could also give indications based on the work task (therefore, after a risk assessment per department and per health figure). To give a practical example, a nurse who has a higher rate of patient handling (with a high MAPO index, a rating scale for patient handling risk, above 1.51), must be trained to do so as safely as possible, and not at the discretion of the employer, but as a matter of obligation (although indications with MAPO indexes above 1.51 and especially 5 strongly recommend further training) [20].
It must also be said that the FNOPI already has a programme of courses (including in occupational health and safety training under COVID-19). However, if the use of CME has been made compulsory (the training credits for post-basic training, a quota of 150 for the three-year period, and at least 25 per year), the topics and courses to be followed still remain the choice of the professional. Therefore, a differentiation of the type of courses to be carried out in addition to the statutory ones would be necessary according to the task and location of work (Kim [21] in his study investigated 1672 nurses of childbearing age on the subject of radiation risks and found that 50.3% had not received training, and only 25.1% had received it regularly), to be included in the category of CME, and more control in the private sector. In addition, it would be appropriate to standardise the subjects of biohazard and clinical risk (and the use of PPE), given the current pandemic situation, and to organise refresher training more frequently. Also, at university level, well before the career stage, there should be a greater emphasis worldwide on occupational safety [22,23], following the American example as shown by Whitaker [24], where occupational safety and health courses are taught in more than 80% of American universities and nursing schools.
Finally, it is also necessary to run courses that encourage healthcare personnel to implement healthy lifestyles and proper management of work-related stress: sport and a positive approach to leisure time, which can be combined with family life, can help to properly manage work-related stress and reduce the risk of burnout [25]. This article explores an important open question, that of the safety of the worker (in this case, the nurse), his or her level of preparedness, and how we can work to improve it. This is an issue that is not given much consideration in Italy, and in the future, it is hoped that more studies will be carried out in this regard.
Conclusions
It is necessary to evaluate the occupational health and safety system for nurses and in universities, in order to have better-prepared professionals in the world of work in the health sector, by implementing training systems and creating a continuous survey of nurses' knowledge, by frequently administering tools such as questionnaires and other evaluation systems, thereby inviting nurses to continue studying the topic after their basic training. In addition, the training system must also be consolidated at the university level, which is the true starting point of a nurse's career. It is extremely important to consider that, along with training, work should also be undertaken on non-individual measures to reduce accidents (continuous research into collective protection systems and a continuous supply of increasingly high-quality PPE are examples of this), and more responsibility should be given to Prevention and Protection Service Managers, supervisors and nursing coordinators, for example, and greater collaboration with universities, with an annual update of the Nursing Guidelines and Procedures, and to work on an individual level on considerations that improve the quality of work and life outside the healthcare working environment, inviting companies to take an interest in the personal situation of employees and to help them to fulfil the concept of health as defined by the WHO in 1948 ("a state of complete physical, mental and social well-being"). In addition, there is a need for improved mechanisms in university curricula and postgraduate training (in terms of frequency and content).
Limitations of the Study
The limitations of the study are represented by the selection of considerably diverse samples: the possibility of researching any studies of a national nature, which are not currently present in the international literature, would have focused the research by giving a more precise overview of our country, together with the use of other databases and with the aid of grey literature. The data may be subject to bias as it does not include feedback from institutional channels, and is based on data in databases from doctors and health professionals in different countries. ISTAT data may be out of date and obsolete, in addition to the difficulty in distinguishing between accidents in the different health sectors.
Funding statement
This research did not receive any form of funding.
Conflicts of Interest
The author declares that he/she has no conflicts of interest associated with this study.
REFERENCES
- Ruggiero N, Magna B, Cornaggia N, Rosa AM, Ferrero O, et al., Effectiveness of Health and Safety at Work Services (PSAL) in reducing occupational injuries in Lombardy Region, Med Lav. 2018 Feb 20;109(2):110-124 DOI:23749/mdl.v109i2.6472
- ISTAT data, URL:https://dati.inail.it/opendata/default/Qualidati/index.html
- Gagliardi D, Marinaccio A, Valenti A, Iavicoli S, Occupational safety and health in Europe: lessons from the past, challenges and opportunities for the future, Ind Health. 2012;50(1):7-11
- INAIL, Coronavirus emergency, 131,000 work-related infections reported to INAIL, Report, 22/01/2021, URL:https://www.inail.it/cs/internet/comunicazione/news-ed-eventi/news/news-denunce-contagi-covid-31-dicembre-2020.html
- European Agency for Safety & Health at Work EU-OHSA, Calculating the cost of work-related stress and psychosocial risks in the workplace – Literature overview), 2014, doi:10.2802/20493
- Legislative Decree no. 81 of 9 April 2008, 'Consolidated Act on Occupational Health and Safety", Implementation of Article 1 of Law no. 123 of 3 August 2007 on the protection of health and safety in the workplace, (published in the Official Gazette no. 101 of 30 April 2008 – Suppl. Ordinary Supplement no. 108)
- Permanent Conference for relations between the State, the Regions and the Autonomous Provinces of Trento and Bolzano, 21 December 2011, Agreement between the Minister of Labour and Social Policy, the Minister of Health, the Regions and the Autonomous Provinces of Trento and Bolzano for worker training, pursuant to Article 37, paragraph 2, of Legislative Decree 9 April 2008, no. 81 (published in the Official Gazette General Series no. 8 of 11/02/2012)
- Ghasemi F, Aghaei H, Askaripoor T, Ghamari F, Analysis of occupational accidents among nurses working in hospitals based on safety climate and safety performance: a Bayesian network analysis, Int J Occup Saf Ergon. 2020 Jul 14;1-7
- Lee S-J, Lee JH, Harrison R, Impact of California's safe patient handling legislation on musculoskeletal injury prevention among nurses, Am J Ind Med. 2019 Jan;62(1):50-58
- Foromo MR, Chabeli M, Satekge MM, Survey on the implementation of the Occupational Health and Safety Act at an academic hospital in Johannesburg, Curationis. 2016 Sep 28;39(1):e1-e10
- Vendittelli D, Penprase B, Pittiglio L, Musculoskeletal Injury Prevention for New Nurses, Workplace Health Saf. 2016 Dec;64(12):573-585
- He L, Lu Z, Huang J, Zhou Y, Huang J, et al., An Integrated Intervention for Increasing Clinical Nurses' Knowledge of HIV/AIDS-Related Occupational Safety, Int J Environ Res Public Health. 2016 Nov 7;13(11):1094
- Faller EM, Miskam NB, Pereira A, Exploratory Study on Occupational Health Hazards among Health Care Workers in the Philippines, Ann Glob Health. 2018 Aug 31;84(3):338-341
- Markkanen P, Galligan C, Quinn M, Safety Risks Among Home Infusion Nurses and Other Home Health Care Providers, J Infus Nurs. Jul/Aug 2017;40(4):215-223
- Morashima Y, Chida K, Katahira Y, Seto H, Chiba H, Tabayashi K, Need for radiation safety education for interventional cardiology staff, especially nurses, Acta Cardiol. 2016 Apr;71(2):151-5
- Rogers B, Buckheit K, Ostendorf J, Ergonomics and nursing in hospital environments, Workplace Health Saf. 2013 Oct;61(10):429-39
- Srikrajang J, Pochamarn C, Chittreecheur J, Apisarnthanarak A, Danchaivijitr S, Effectiveness of education and problem solving work group on nursing practices to prevent needlestick and sharp injury, J Med Assoc Thai. 2005 Dec;88 Suppl 10:S115-9
- Giorgi G, Lecca LI, Alessio F, Finstad GL, Bondanini G, et al., COVID-19-Related Mental Health Effects in the Workplace: A Narrative Review, Int J Environ Res Public Health. 2020 Oct 27;17(21):7857
- Maida CM, Aprea L, Calamusa G, Campisi F, Favaro D, et al., Blood and body fluids exposure of healthcare workers in a university hospital of Palermo, Italy: a fourteen years long surveillance, Ann Ig. 2020 Sep 29;32(6). doi: 10.7416/ai.2020.2380
- Cantarella C, Stucchi G, Menoni O, Cairoli S, Manno R, et al., MAPO Method to Assess the Risk of Patient Manual Handling in Hospital Wards: A Validation Study, Hum Factors. 2020 Nov;62(7):1141-1149
- Kim O, Sun Kim M, Jung Jang H, Lee H, Kang Y, et al., Radiation safety education and compliance with safety procedures-The Korea Nurses' Health Study, J Clin Nurs. 2018 Jul;27(13-14):2650-2660
- McCullagh MC, Berry P, A Safe and Healthful Work Environment: Development and Testing of an Undergraduate Occupational Health Nursing Curriculum, Workplace Health Saf. 2015 Aug;63(8):328-32
- Jahangiri M, Malakoutikhah M, Choobineh A, Zare A, Nurses' uncertainty about medical gloves safety during the COVID-19 pandemic, J Healthc Qual Res. 2021 Apr 27;S2603-6479(21)00037-3. doi: 10.1016/j.jhqr.2021.03.009
- Whitaker S, Wynn P, Williams N, Occupational health teaching for pre registration nursing students, Nurse Educ Today. 2002 Feb;22(2):152-8
- Vitale E, Cesano E, Germini F, Prevalence of Burnout among Italian Nurses: a descriptive study, Acta Biomed. 2020 Sep 7;91(4):e2020117. doi: 10.23750/abm.v91i4.9008