Antonio Brusini.1
- Nurse in Sports Medicine, AUSL Modena, Alma Mater Studiorum university tutor, Bologna
Corresponding author: Brusini A., nurse in Sports Medicine at AUSL Modena, master’s degree in “Management of Sport and Motor Activities”. Email: antoniobrusini87@outlook.it
Cita questo articolo
ABSTRACT
Introduction: The prevention of occupational accidents in the sphere of occupational health and safety is an important issue in the Italian work setting; health workers, and especially nurses, are continually exposed to the risk of work-related accidents, which can affect the quality of care provided.
Aim: The aim of this review is to investigate the nurse’s perceived level of preparedness with regard to occupational safety.
Methods: A narrative review of the literature was conducted using some of the main databases such as PubMed, CINAHL and Cochrane.
Results: The studies analysed show that Italian nurses have little knowledge about occupational health and safety legislation.
Conclusions: Establishing specific postgraduate training events and identifying specific legislation for healthcare personnel could represent essential steps towards implementing this specific knowledge.
Keywords: Prevention; Training; Nurses; Healthcare workers
Introduction
Occupational safety has always been a central issue in the Italian working environment [1]: in 2019, 641,638 accidents at work were reported by December 2019 (640,723 in 2018), 100,905 of these took place on the journey between home and workplace (98,446 in 2018) and 540,733 in the workplace (542,277 in 2018), with 1089 fatal accidents at work (1133 in 2018) [2].
A key area for safeguarding workers, including nurses, is training, which is a useful tool for working safely [3]. Indeed, the risk of injury has increased during the COVID-19 pandemic period (131,090 reports of injuries due to COVID-19 infection in the workplace in 2020 [4]). Fewer accidents would lead to reduced expenditure, related to the cost of treatment, lost working days and replacement of the injured worker. In the UK, for example, in the 2011–12 season, there was a quantifiable loss of 10.4 million working days and a consequent reduction in productivity linked to work-related stress injuries.
The specific high-risk topics to be covered during the course include accident risks; general mechanical risks; general electrical risks; machinery; equipment; falls from height; explosion risks; chemical risks; mists, oils, fumes, vapours, dusts; labelling; carcinogenic risks; biological risks; physical risks; noise; vibration; radiation; microclimate and lighting; display screens; PPE; work organisation; working environments; work-related stress; manual handling of loads; handling of goods (lifting equipment, means of transport); signposting; emergencies; safety procedures with reference to the specific risk profile (high in this case); escape and fire procedures; organisational procedures for first aid; accidents and near misses; other risks. Any further training is at the discretion of the employer, who may decide to give his or her staff additional training [6,7].
Objective
The aim of this study is to investigate, through a narrative review of the literature, nurses’ knowledge of occupational safety.
Methods
PubMed, CINAHL and Cochrane databases were used as a search medium, and all databases were searched on 28/02/2021 for the set of keywords: ‘occupational’, ‘health’, ‘safety’, ‘nurse’, without Boolean operators between them. No time limit was given to the research, and only English-language sources were taken into account.
This search yielded 422 results on the Cochrane database (using the ‘all text’ filter); the same search yielded 2418 results on the Pubmed database and 631 results on CINAHL; of these, 3 articles could not be traced (2 on PubMed and 1 on CINAHL). Only studies that discussed the topic of occupational health and safety training and that had carried out a survey in the form of a questionnaire or other methods on training or nurses’ perceptions of training in their workplaces were included. Studies involving an education or training programme for nurses who had carried out a survey of subject knowledge prior to the intervention then performed in the study were also taken into account. The selected studies were carried out on a nursing population or included nurses among other professions in the sample. The outcomes to be studied were the survey responses of the studies on the level of preparedness in the field of occupational safety and, if not reported in quantitative terms, the authors’ considerations.
Results
Articles concerning the figure of the ‘Occupational Health Nurse/Nursing’ were excluded (Table 1), as it is a figure that specifically deals with occupational health and safety but is not present in Italy, as were repeat sources. After reading the title, 22 sources on Cochrane, 515 on PubMed and 80 on CINAHL were retained.
All articles other than primary studies were excluded. After reading the abstract and the article, 10 articles were selected (1 on Cochrane and Pubmed, 5 on Pubmed and CINAHL, 4 on Pubmed only). Duplicate results were skimmed after the results selection. 2 results concern nurses together with other health professionals, 1 result involves nurses and nursing managers.
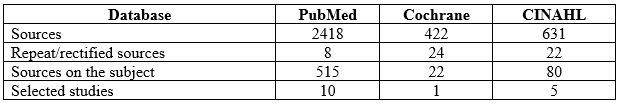
Table 1: Databases consulted, sources found and selected
The detailed procedure used in the selection of articles is presented as a flow chart in Figure 1.

Figure 1. Diagram showing the stages of the review and article selection
Table 2 shows the studies classified by author, year, health personnel involved in the study, method, number of participants and results.
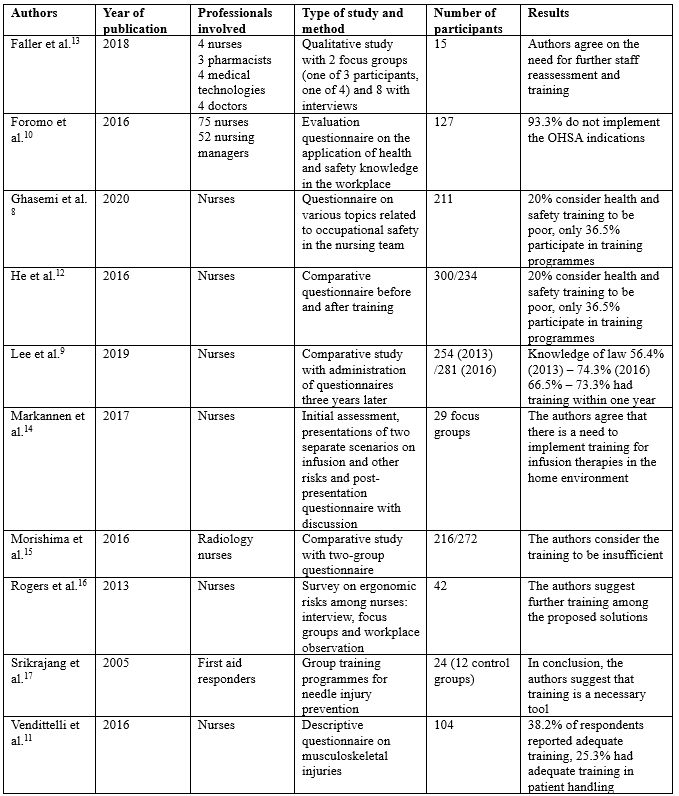
Table 2: Citations on training for nurses and healthcare professionals in the literature found, in alphabetical order by the author. OHSA ‘Occupational Health and Safety Act’, MAPO Movimentazione Assistita Pazienti Ospedalieri (Assisted Handling of Hospital Patients)
Ghasemi [8] conducted a study surveying 211 nurses by asking questions on various topics related to teamwork safety (nurse relationships, accumulated fatigue, communication with physiatrists, supervisor attitude, nursing unit conditions, error reporting, and nursing training), finding that 20% of respondents considered health and safety training to be poor, and only 36.5% participated in occupational safety training programmes. Lee [9] surveyed knowledge of the law that came out in California in 2012 on patient handling, one year (2013) and three years (2016) later, finding 56.4% of nurses in 2013 and 74.3% of nurses in 2016 were familiar with the current law, with those figures changing to 66.5% and 73.3% respectively for nurses who had received training in patient handling within the past year. Foromo [10] administered an evaluation questionnaire to 75 nurses and 52 ‘nursing managers’ asking whether health and safety regulations were implemented in the workplace and found that 93.3% were not implementing the correct instructions. Vendittelli [11] administered an online questionnaire with scales of 1 to 5 (and the optional possibility to write comments) to 104 nurses who graduated between 2011 and 2014 (offered to 435 in total, with only 104 participating), marking demographics, training (and incidence) in occupational safety, including in mobility procedures, and general nursing training, with only 38.2% stating that they had received adequate training specific to their operating unit, and only 25.3% stating that they had adequate time for training in patient handling. He [12] administered a comparative questionnaire between two groups, before and after a training programme on the topic of HIV/AIDS, and the awareness of HIV/AIDS-related knowledge improved significantly after the training (correct answers increased from 67.9% to 82.34%, on risk perception from 54.4% to 66.6%).
Faller [13] conducted a qualitative study with various healthcare professionals using instruments such as interviews and focus group discussions on some focal points (experience of accidents at work, implementations, barriers and strategies to improve safety), and eight groups with semi-structured interviews, and indicated the genuine need for further training and investigation of staff competences in the field of safety. Markannen [14] worked mainly on prevention in infusion practice, presenting possible working situations in focus groups, with pre- and post-intervention evaluation questionnaires, and agreeing on the need to implement training in home care. Morishima [15] administered a questionnaire to two groups of health professionals, one in 2008 and one in 2010, on the subject of radiation: whether there are different types (24.5% responded positively in 2008 and 40.3% in 2010), about the external protection procedure (17.6% and 26.7% positive responses respectively), the correct distance to the machine (31.5% and 41.5%) and the correct position of the dosimeter (60.8% and 55.1%). Rogers [16] conducted an investigation into the ergonomic risks of the nursing profession through focus groups, interviews and workplace observations of 42 registered nurses in five hospitals in North Carolina, finding training to be one of the main tools in preventing ergonomic risks. Finally, Srikrajang [17] conducted a study on a group of 24 emergency and laboratory health workers (including a control group of 12), demonstrating improvements with the use of training tools in preventing needlestick injuries.
Discussion
The literature review identified few sources, most agreeing that participants in the various studies show structural deficiencies in occupational health and safety training, calling for thorough training interventions. The results show that a significant number of nurses are not familiar with their state’s occupational health and safety legislation, and there are many nurses who are not familiar with risk factors and how to work as safely as possible. In fact, the pandemic period, as pointed out by Giorgi [18], highlighted a particular situation for care staff with consequent stress due both to the working conditions resulting from a higher-than-normal workload due to the emergency both in terms of working hours and in terms of working conditions (overload of patients and the continuous use of personal protective equipment (PPE) to which they were not accustomed, except in very few departments, greater emotional involvement) and to the condition that in some settings was already present before the pandemic. Moreover, there is continuous exposure to biological risk due to possible contagion between patient and operator and between operators, no longer represented almost exclusively by contact with biological liquids, although as shown by Maida [19], there is still a need for training also in this type of risk. The COVID-19 pandemic, therefore, exaggerated the possibility of an accident at work, without any clear preparation for the event. The lack of training on the correct handling of the equipment, and the impossibility of training during the lockdown period, led to a substantial change in the training offer in the field of occupational health and safety, with an increase in online portals. The example of FadinMed (https://www.fadinmed.it/) was necessary, as it offered courses, together with the Ministry’s portals, useful for training on the use of PPE during a pandemic.
A possible improvement in an Italian perspective for nurses would be the conferral of the management of training topics on occupational health and safety by the professional order (for each health category, it is compulsory to be registered; nurses must be registered with the Professional Order of Nurses, FNOPI): in the case of nurses, it could also give indications based on the work task (therefore, after a risk assessment per department and per health figure). To give a practical example, a nurse who has a higher rate of patient handling (with a high MAPO index, a rating scale for patient handling risk, above 1.51), must be trained to do so as safely as possible, and not at the discretion of the employer, but as a matter of obligation (although indications with MAPO indexes above 1.51 and especially 5 strongly recommend further training) [20].
It must also be said that the FNOPI already has a programme of courses (including in occupational health and safety training under COVID-19). However, if the use of CME has been made compulsory (the training credits for post-basic training, a quota of 150 for the three-year period, and at least 25 per year), the topics and courses to be followed still remain the choice of the professional. Therefore, a differentiation of the type of courses to be carried out in addition to the statutory ones would be necessary according to the task and location of work (Kim [21] in his study investigated 1672 nurses of childbearing age on the subject of radiation risks and found that 50.3% had not received training, and only 25.1% had received it regularly), to be included in the category of CME, and more control in the private sector. In addition, it would be appropriate to standardise the subjects of biohazard and clinical risk (and the use of PPE), given the current pandemic situation, and to organise refresher training more frequently. Also, at university level, well before the career stage, there should be a greater emphasis worldwide on occupational safety [22,23], following the American example as shown by Whitaker [24], where occupational safety and health courses are taught in more than 80% of American universities and nursing schools.
Finally, it is also necessary to run courses that encourage healthcare personnel to implement healthy lifestyles and proper management of work-related stress: sport and a positive approach to leisure time, which can be combined with family life, can help to properly manage work-related stress and reduce the risk of burnout [25]. This article explores an important open question, that of the safety of the worker (in this case, the nurse), his or her level of preparedness, and how we can work to improve it. This is an issue that is not given much consideration in Italy, and in the future, it is hoped that more studies will be carried out in this regard.
Conclusions
It is necessary to evaluate the occupational health and safety system for nurses and in universities, in order to have better-prepared professionals in the world of work in the health sector, by implementing training systems and creating a continuous survey of nurses’ knowledge, by frequently administering tools such as questionnaires and other evaluation systems, thereby inviting nurses to continue studying the topic after their basic training. In addition, the training system must also be consolidated at the university level, which is the true starting point of a nurse’s career. It is extremely important to consider that, along with training, work should also be undertaken on non-individual measures to reduce accidents (continuous research into collective protection systems and a continuous supply of increasingly high-quality PPE are examples of this), and more responsibility should be given to Prevention and Protection Service Managers, supervisors and nursing coordinators, for example, and greater collaboration with universities, with an annual update of the Nursing Guidelines and Procedures, and to work on an individual level on considerations that improve the quality of work and life outside the healthcare working environment, inviting companies to take an interest in the personal situation of employees and to help them to fulfil the concept of health as defined by the WHO in 1948 (“a state of complete physical, mental and social well-being”). In addition, there is a need for improved mechanisms in university curricula and postgraduate training (in terms of frequency and content).
Limitations of the Study
The limitations of the study are represented by the selection of considerably diverse samples: the possibility of researching any studies of a national nature, which are not currently present in the international literature, would have focused the research by giving a more precise overview of our country, together with the use of other databases and with the aid of grey literature. The data may be subject to bias as it does not include feedback from institutional channels, and is based on data in databases from doctors and health professionals in different countries. ISTAT data may be out of date and obsolete, in addition to the difficulty in distinguishing between accidents in the different health sectors.
Funding statement
This research did not receive any form of funding.
Conflicts of Interest
The author declares that he/she has no conflicts of interest associated with this study.
REFERENCES
- Ruggiero N, Magna B, Cornaggia N, Rosa AM, Ferrero O, et al., Effectiveness of Health and Safety at Work Services (PSAL) in reducing occupational injuries in Lombardy Region, Med Lav. 2018 Feb 20;109(2):110-124 DOI:23749/mdl.v109i2.6472
- ISTAT data, URL:https://dati.inail.it/opendata/default/Qualidati/index.html
- Gagliardi D, Marinaccio A, Valenti A, Iavicoli S, Occupational safety and health in Europe: lessons from the past, challenges and opportunities for the future, Ind Health. 2012;50(1):7-11
- INAIL, Coronavirus emergency, 131,000 work-related infections reported to INAIL, Report, 22/01/2021, URL:https://www.inail.it/cs/internet/comunicazione/news-ed-eventi/news/news-denunce-contagi-covid-31-dicembre-2020.html
- European Agency for Safety & Health at Work EU-OHSA, Calculating the cost of work-related stress and psychosocial risks in the workplace – Literature overview), 2014, doi:10.2802/20493
- Legislative Decree no. 81 of 9 April 2008, ‘Consolidated Act on Occupational Health and Safety”, Implementation of Article 1 of Law no. 123 of 3 August 2007 on the protection of health and safety in the workplace, (published in the Official Gazette no. 101 of 30 April 2008 – Suppl. Ordinary Supplement no. 108)
- Permanent Conference for relations between the State, the Regions and the Autonomous Provinces of Trento and Bolzano, 21 December 2011, Agreement between the Minister of Labour and Social Policy, the Minister of Health, the Regions and the Autonomous Provinces of Trento and Bolzano for worker training, pursuant to Article 37, paragraph 2, of Legislative Decree 9 April 2008, no. 81 (published in the Official Gazette General Series no. 8 of 11/02/2012)
- Ghasemi F, Aghaei H, Askaripoor T, Ghamari F, Analysis of occupational accidents among nurses working in hospitals based on safety climate and safety performance: a Bayesian network analysis, Int J Occup Saf Ergon. 2020 Jul 14;1-7
- Lee S-J, Lee JH, Harrison R, Impact of California’s safe patient handling legislation on musculoskeletal injury prevention among nurses, Am J Ind Med. 2019 Jan;62(1):50-58
- Foromo MR, Chabeli M, Satekge MM, Survey on the implementation of the Occupational Health and Safety Act at an academic hospital in Johannesburg, Curationis. 2016 Sep 28;39(1):e1-e10
- Vendittelli D, Penprase B, Pittiglio L, Musculoskeletal Injury Prevention for New Nurses, Workplace Health Saf. 2016 Dec;64(12):573-585
- He L, Lu Z, Huang J, Zhou Y, Huang J, et al., An Integrated Intervention for Increasing Clinical Nurses’ Knowledge of HIV/AIDS-Related Occupational Safety, Int J Environ Res Public Health. 2016 Nov 7;13(11):1094
- Faller EM, Miskam NB, Pereira A, Exploratory Study on Occupational Health Hazards among Health Care Workers in the Philippines, Ann Glob Health. 2018 Aug 31;84(3):338-341
- Markkanen P, Galligan C, Quinn M, Safety Risks Among Home Infusion Nurses and Other Home Health Care Providers, J Infus Nurs. Jul/Aug 2017;40(4):215-223
- Morashima Y, Chida K, Katahira Y, Seto H, Chiba H, Tabayashi K, Need for radiation safety education for interventional cardiology staff, especially nurses, Acta Cardiol. 2016 Apr;71(2):151-5
- Rogers B, Buckheit K, Ostendorf J, Ergonomics and nursing in hospital environments, Workplace Health Saf. 2013 Oct;61(10):429-39
- Srikrajang J, Pochamarn C, Chittreecheur J, Apisarnthanarak A, Danchaivijitr S, Effectiveness of education and problem solving work group on nursing practices to prevent needlestick and sharp injury, J Med Assoc Thai. 2005 Dec;88 Suppl 10:S115-9
- Giorgi G, Lecca LI, Alessio F, Finstad GL, Bondanini G, et al., COVID-19-Related Mental Health Effects in the Workplace: A Narrative Review, Int J Environ Res Public Health. 2020 Oct 27;17(21):7857
- Maida CM, Aprea L, Calamusa G, Campisi F, Favaro D, et al., Blood and body fluids exposure of healthcare workers in a university hospital of Palermo, Italy: a fourteen years long surveillance, Ann Ig. 2020 Sep 29;32(6). doi: 10.7416/ai.2020.2380
- Cantarella C, Stucchi G, Menoni O, Cairoli S, Manno R, et al., MAPO Method to Assess the Risk of Patient Manual Handling in Hospital Wards: A Validation Study, Hum Factors. 2020 Nov;62(7):1141-1149
- Kim O, Sun Kim M, Jung Jang H, Lee H, Kang Y, et al., Radiation safety education and compliance with safety procedures-The Korea Nurses’ Health Study, J Clin Nurs. 2018 Jul;27(13-14):2650-2660
- McCullagh MC, Berry P, A Safe and Healthful Work Environment: Development and Testing of an Undergraduate Occupational Health Nursing Curriculum, Workplace Health Saf. 2015 Aug;63(8):328-32
- Jahangiri M, Malakoutikhah M, Choobineh A, Zare A, Nurses’ uncertainty about medical gloves safety during the COVID-19 pandemic, J Healthc Qual Res. 2021 Apr 27;S2603-6479(21)00037-3. doi: 10.1016/j.jhqr.2021.03.009
- Whitaker S, Wynn P, Williams N, Occupational health teaching for pre registration nursing students, Nurse Educ Today. 2002 Feb;22(2):152-8
- Vitale E, Cesano E, Germini F, Prevalence of Burnout among Italian Nurses: a descriptive study, Acta Biomed. 2020 Sep 7;91(4):e2020117. doi: 10.23750/abm.v91i4.9008