Vincenza Giordano 1 *, Luca Cardillo 2
- Nurse with Master’s Degree in Nursing and Midwifery Sciences, AORN Antonio Cardarelli
- Nurse and Business Trainer at A.S.L Napoli 2 NORD (Hospital Santa Maria delle Grazie)
*Corresponding Author: Dr. Vincenza Giordano, Nurse with Master’s Degree in Nursing and Midwifery Sciences, AORN Antonio Cardarelli
E-mail: enza-giordano@hotmail.it
Cita questo articolo
ABSTRACT
Introduction: Fournier’s Gangrene is a severe necrotising infection that can be fatal if not recognised and treated immediately. Treatment consists of a combination of conventional therapy with a multidisciplinary approach (early diagnosis, surgical debridement, antibiotic therapy, intensive care and reconstructive surgery) and adjuvant therapy with hyperbaric oxygen therapy sessions.
Objective: To identify the role and evaluate the efficacy of hyperbaric oxygen therapy in Fournier’s gangrene.
Method: To conduct the following narrative review a research question was outlined using the PIO methodology. Subsequently, a literature review was conducted using the PubMed, Scopus and CINAHL Complete databases from December 2020 to February 2021.
Results: Eight studies emerged from the literature review showing that the use of adjuvant Hyperbaric oxygen therapy (HBOT) in combination with classical treatment has beneficial effects and enhances the efficacy of hyperbaric oxygen therapy, resulting in lower mortality rates, in contrast to the average number of hospital days spent in intensive care, which do not undergo any significant change. But in contrast to mortality, the average number of days spent in intensive care differed significantly in favour of the standard treatment group.
Conclusion: The combined effect of hyperbaric oxygen therapy with conventional therapy offers a significant advantage in the management of FG; furthermore, HBOT is associated with a significant survival advantage.
Keywords: Fournier‘s gangrene, Fournier’s disease, Hyperbaric oxygen therapy and HBOT
INTRODUCTION
Necrotising fasciitis, better known as “Fournier’s Gangrene” (FG), is a polymicrobial infection caused by aerobic and anaerobic microorganisms acting synergistically to cause severe soft tissue infection (NSTI), targeting the genital, perineal and perianal region [1,2]. The term, coined by the scholar Wilson, first appeared in the scientific world in 1952 [3]. FG is now considered a rare disease [4-6], predominantly affecting males (10 to 1 ratio) with a mean age of 50 years [4,7], with an incidence rate ranging from 0.3 to 15.5 cases per 100000 inhabitants [8,9]. It is associated with high morbidity and mortality between 3% and 67% [4]. FG has a subtle and rapid pathogenesis, so much so that some authors have divided the disease into 4 phases[5]: (i) the initial phase occurs within 24-48 hours and is associated with non-specific symptoms, such as itching, oedema, erythema and partial hardening of the affected tissues; (ii) the second phase is brief and invasive with the presence of local inflammatory manifestations; (iii) the third phase is the necrotic phase in which there is a rapid deterioration, which may evolve into septic shock, with the risk of spreading necrosis to the anterior abdominal wall and thighs; (iv) the fourth phase is one of spontaneous repair which occurs after a few months, during which epithelial regeneration and healing take place [5]. From an aetiological point of view, the bacteria responsible for this infection include group A Streptococcus as the most common monomicrobial culprit [10,11], while Escherichia coli, Bacteroides, Staphylococcus, Proteus, Streptococcus, Pseudomonas and Enterococcus are among the polymicrobial culprits [12,13]. Microorganisms have been found in the urogenital tract and in the digestive tract: the causes of bacterial presence in the urogenital tract are urethral stenosis, scrotal abscesses, orchitis, epididymitis, renal abscess, ureteral trauma, renal calculosis, bladder and penile cancer, prostate biopsy and catheterization [14,15], while the presence of bacteria in the digestive tract is found in outbreaks originating from perianal abscesses, colorectal tumours, appendicitis, acute diverticulitis, Crohn’s disease, incarcerated hernias and perforation of the rectum, particularly caused by a foreign body [16,17]. Without treatment, the process may not only rapidly spread to the abdominal wall, dorsal region, upper limbs and retroperitoneum, but also lead to sepsis, multi-organ failure and death [1,18,19]. Systemic diseases listed as risk factors for the development of FG include: diabetes mellitus, alcoholism, hypertension, obesity, smoking, immune suppressive conditions such as HIV infection, radiotherapy and chemotherapy [4,7,20-23]. In terms of semeiotics, the most frequent manifestations include pain, erythema, oedema and necrosis of the scrotum or the perianal and perineal region, often associated with fever and chills [24-26]. Other symptoms are mostly localised and include the presence of blisters, crackles, cyanosis and malodorous discharge; however, it should be emphasised that the skin manifestations are the ‘tip of the iceberg’, while the infection spreads rapidly and aggressively along deep fascial planes [27,28]. The FGSI (Fournier’s Gangrene Severity Index) scale is used to estimate the severity of Fournier’s gangrene. It uses 9 parameters: temperature, pulse, respiratory rate, sodium, potassium and creatinine levels, haematocrit, leukocytosis and bicarbonate levels. Each parameter is assigned a score from 0 to 4. A high FGSI score denotes a worse prognosis [29]. Treatment of FG includes management of sepsis according to guidelines (early diagnosis, surgical debridement, antibiotic therapy, intensive care and reconstructive surgery) [30] and hyperbaric oxygen therapy (HBOT) is highly recommended whenever possible [31].
Hyperbaric oxygen therapy is a therapeutic approach that involves the use of 100% pressurised oxygen, which is delivered in an airtight chamber. HBOT has a bactericidal action on anaerobes and reduces the activity of endotoxins in the presence of high oxygen levels. This treatment has provided benefits such as improved neutrophil phagocytic action, fibroblast proliferation and angiogenesis, reduced oedema, absence of free radicals and increased intracellular transport of antibiotics [32,33]. Adverse effects associated with this treatment approach are relatively rare, but there are not enough studies that have investigated the role of HBOT in FG [34,35]. Among the few studies presented in literature, adverse events include barotrauma of the tympanic membrane and paranasal sinuses, the possibility of sudden onset of epileptic seizures and pulmonary and central nervous system toxicity caused by oxygen[36]. However, the use of hyperbaric oxygen therapy in the management of FG is widely discussed, sometimes even controversially, because clinical evidence regarding HBOT in these infections is scarce and of generally low quality and, moreover, the use of hyperbaric oxygen therapy is not standard of care in many centres, so much so that some authors recommend HBOT as an adjuvant treatment [37], while others do not recommend it as routine use in the management of FG [38]. This literature review aims to investigate the role that HBOT plays in Fournier’s gangrene, its effectiveness and influence on some variables. Some studies show that HBOT reduces the extent of necrosis, mortality, morbidity rates [39,40] and the need for further surgery [41]. The strength of this review is to highlight that, although oxygen therapy is a second-line treatment, in all the studies reported in this review, it still plays a decisive role in the treatment of Fournier’s gangrene, as it allows restitutio ad integrum.
Objective of the study
Identify the role and evaluate the effectiveness of hyperbaric oxygen therapy in Fournier’s gangrene.
MATERIALS AND METHODS
Study design
A narrative review of the literature was conducted using an evidence method. To conduct the review, a research question was outlined using the Population, Intervention, Outcome (PIO) methodology. The PIO specifies the population to be studied, the intervention to be implemented and the outcomes (Table 1).

Table 1. Question according to the PIO method. FG= Fournier’s gangrene
Research strategy
The research of the articles was carried out through the following databases PubMed, Scopus and CINAHL Complete in the time period from December 2020 to February 2021.
The following keywords were used:
“Fournier’s Gangrene”, “Fournier’s Disease”, “Gangrena de Fournier”, “Hyperbaric Oxygen Therapy”, “hbot”, “hyperbaric oxygen” and “oxygen therapy“.
For each MeSH term, the respective synonyms have been identified in each database. Next, advanced search terms were set up, using the Boolean operators ‘OR’ and ‘AND’ to cross terms in different combinations and make the search more specific. The only limit included is the date of publication: only articles published within the last 10 years were taken into account.
The formulation of the keywords and MeSH terms was carried out jointly by the two authors in order to comply with validity criteria and reduce search bias . Similarly, the authors also collaborated in the retrieval of articles and full-texts and their respective evaluations, to identify reports relevant to the research topic. The search terms are shown in Table 2.
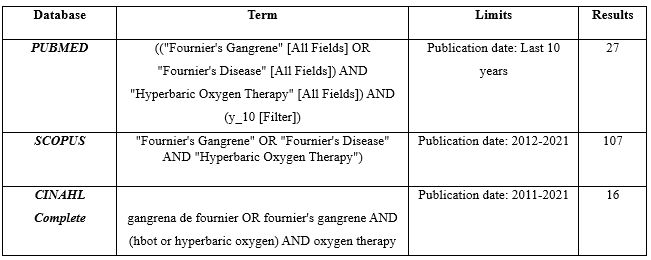
Table 2. Search terms
Inclusion and exclusion criteria
The following criteria were set for the search. We included (a) primary studies; (b) studies carried out on the adult population of both sexes; (c) studies published in the past 10 years. We excluded: (A) secondary studies; (b) editor’s reviews and / or letters to the editor; (c) studies with subjects under the age of 18; (d) studies in which the role of hyperbaric oxygen therapy was not fully exposed. The detailed procedure used in the selection of articles is presented below in the form of a flow chart shown in Figure 1.
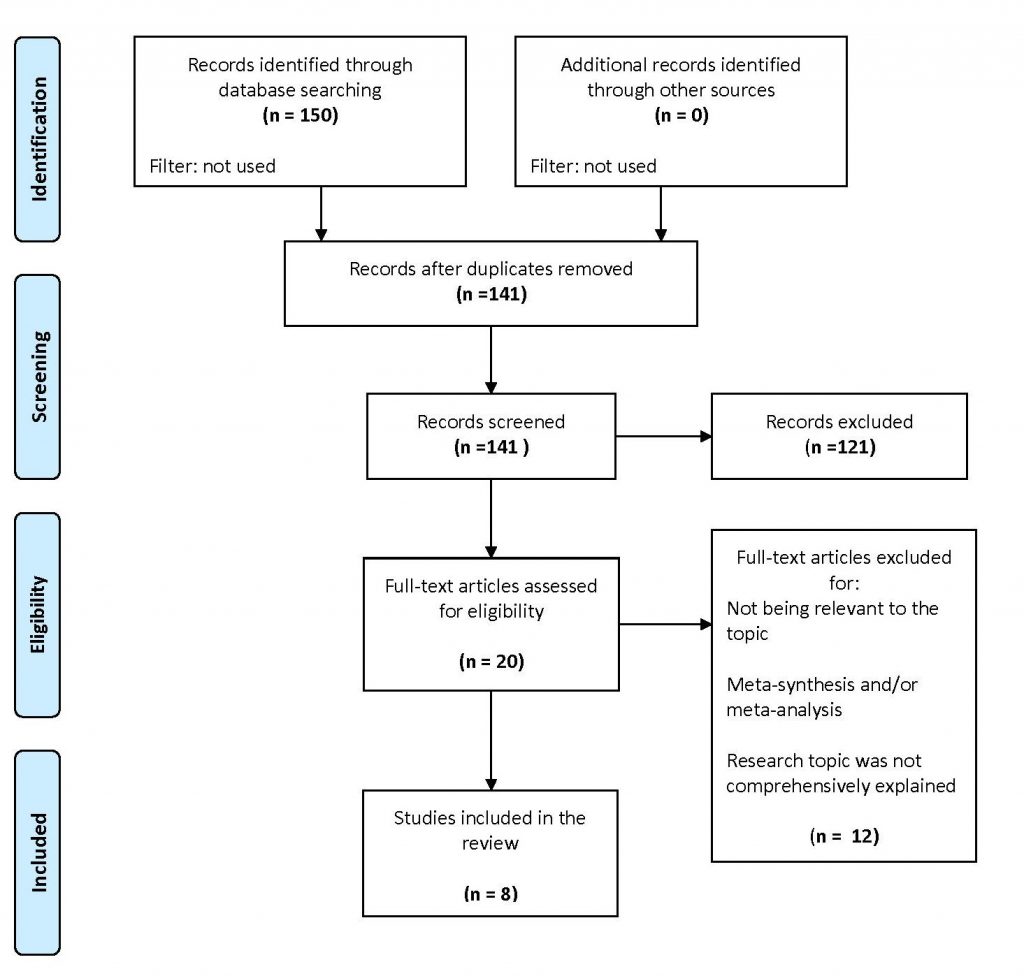
Figure 1. PRISMA Flow Diagram of the literature review
Our search strategy yielded a total of 150 preliminary stage articles (27 on Pubmed ,107 on Scopus and 16 on CINAHL Complete). 9 duplicate articles were excluded. The remaining 141 were assessed by title and abstract, 121 were discarded because they were not relevant to the objective or inconsistent with the inclusion criteria. Of the 20 remaining articles, after reading the full-text, 12 records were discarded as they were secondary studies or not relevant to the research question. 8 articles were included in the review after a full evaluation of the text. The two authors independently conducted the literature review and no discrepancies emerged between the evaluators.
RESULTS
Eight studies relevant to our question emerged and Table 3 summarises their characteristics and results. Fournier’s Gangrene is a severe necrotising infection that can be fatal if not detected and treated immediately. Treatment consists of a combination of conventional therapy with a multidisciplinary approach (early diagnosis, surgical debridement, antibiotic therapy, intensive care and reconstructive surgery) and adjuvant therapy with hyperbaric oxygen therapy sessions. This is confirmed in the articles that follow. A retrospective study [42] has shown that the use of adjuvant HBOT, in combination with classic treatment is associated with reduced mortality: this percentage was lower in the group treated with HBOT than in the control group treated with the standard approach ( 3.7% vs 28.8%). This finding is further confirmed in other studies [43,44]: in the retrospective, multicentre observational study by Anheusera et al. [44], mortality in patients treated with HBOT was 0% vs. 4.4% mortality for patients not receiving adjuvant treatment. In the latter study, as opposed to mortality, a variable on which it is important to pay attention was the average days spent in intensive care, which differed significantly in favour of the standard treatment group. In fact, the frequency of wound debridement and hospital stay were significantly higher in the hyperbaric oxygen therapy group (13 vs 5 debridements and 40 vs 22 days). However, the latter contrasts with a retrospective, multicentre study present in the literature [45], in which the variables of length of hospital stay, direct costs of hospital stay, complications and mortality in the three FG classes (minor, moderate and major), regardless of treatment, were not significantly different. In contrast, subjects receiving adjuvant therapy with HBOT had a lower rate of complications (45% vs. 66%) and deaths (4% vs. 23). In a retrospective analysis of 60 patients, first treated with broad-spectrum antibiotics and then undergoing surgery within 24 hours of admission, it was observed that fasciotomy alone was an insufficient treatment and that in many patients debridement was necessary (average of 3.1 debridements), combined with early diagnosis, intensive care and in some cases colostomy, with the addition of hyperbaric oxygen therapy sessions, which demonstrated an increase in survival [46]. In this study, 12 patients were treated with HBOT, with a survival rate of 100% (12/12 patients), compared to 66.7% (32/48) of patients who did not undergo HBOT. In addition, hyperbaric oxygen therapy, as shown in Chao et al’s case-control study [29] of 28 subjects, reduces infection rates and improves prognosis, although the most effective method for FG remains surgical treatment. However, due to the depth of the retroperitoneal space, the presence of large cavities and soft tissue, the lesions are diffuse and it is often difficult to completely debride the necrotic tissue during surgery. Therefore in such conditions, hyperbaric oxygen therapy used as an adjunct to standard therapy can reduce debridement sessions and times, shorten the length of drainage tube use, reduce healing time and improve the prognosis process of FG. In this study, as in previous studies, the experimental group had a lower mortality rate than the non-HBOT control group (12.5% vs. 33.3%). These findings are supported by two studies: a retrospective and descriptive study conducted by accessing the medical records of 34 FG patients who underwent HBOT from 1989 to 2014 [47] and a single-center, case-control study involving 341 subjects, which described the potential benefits of HBOT in FG from a pathophysiological perspective (inflammation, modulation of reperfusion injury and facilitation of wound healing), with respective reduction in mortality [48].
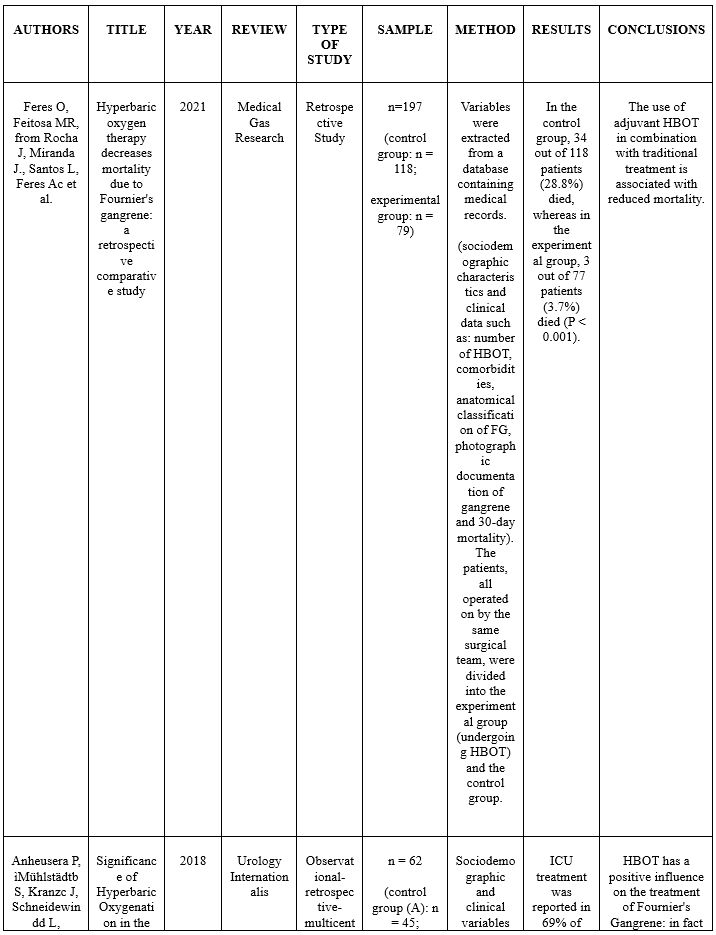
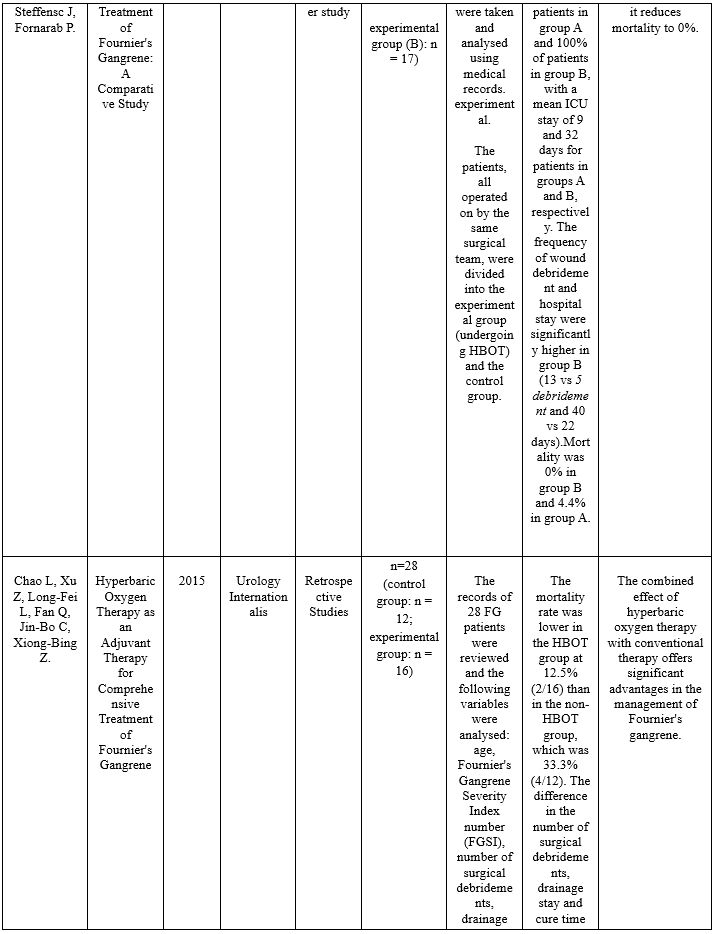
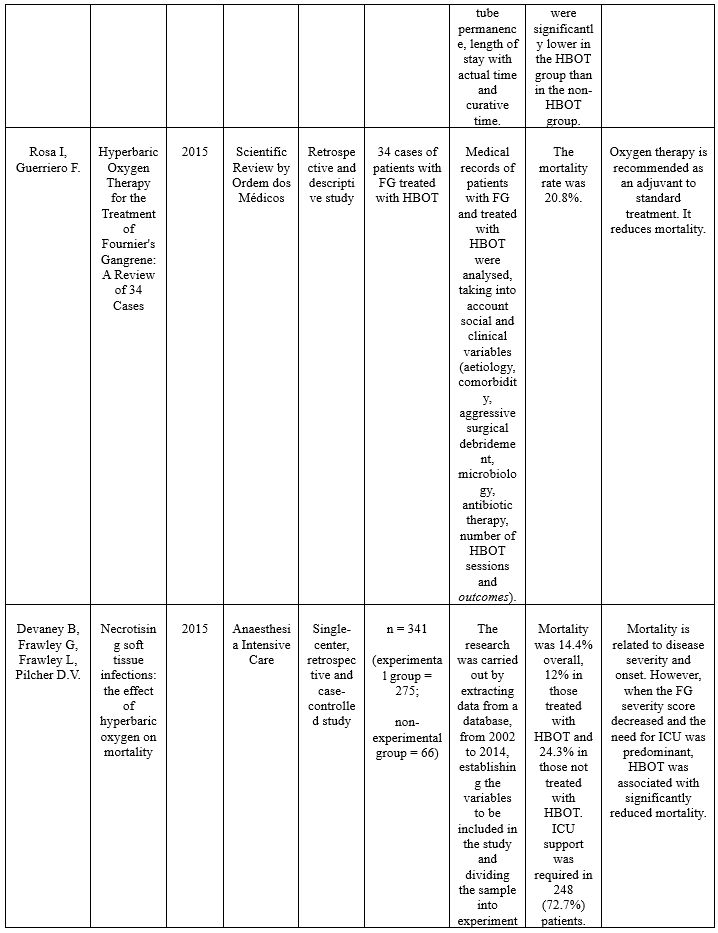
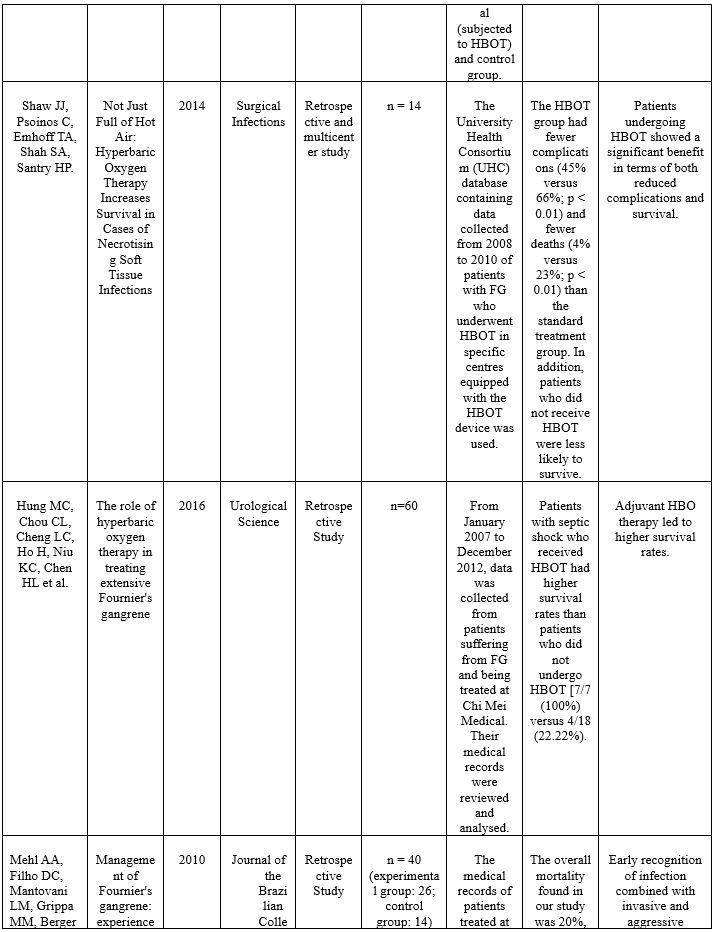
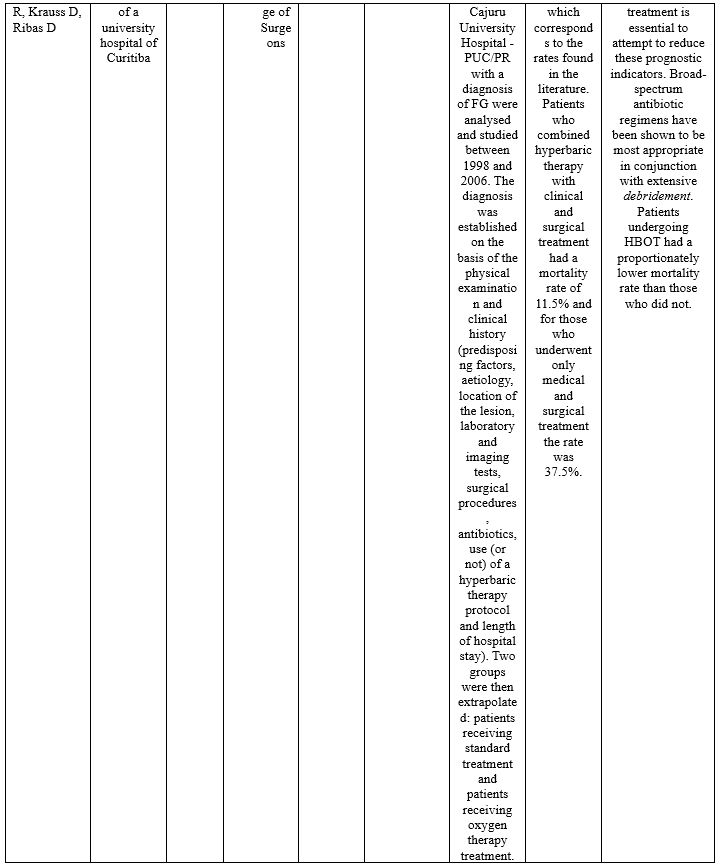
Table 3. Analysis of the studies included within the review.
DISCUSSION
The aim of the review was to identify the role and assess the effectiveness of hyperbaric oxygen therapy in Fournier’s Gangrene. From the studies analysed, it is clear that the primary treatment of Fournier’s Gangrene uses a multidisciplinary approach based on conventional therapy (early diagnosis, surgical debridement , antibiotic therapy, intensive care and reconstructive surgery). In recent years, hyperbaric oxygen therapy has shown to have an adjuvant role in the treatment of FG, but at the same time a decisive one, as it has allowed a return ad integrum with or without surgery. In fact, due to the depth of the retroperitoneal space, the large cavities and non-linear tissue, and the diffuse lesions, it is often difficult to define and carry out a complete debridement of the necrotic tissue during surgery, so that tissue hypoxia and infection factors interact and in the post-operative period, poor drainage or the onset of other factors favour the spread of the disease. Therefore it becomes necessary in such conditions, to find an adjuvant therapy that can reduce the infection rates and improve the prognosis. HBOT acts as a bactericide and/or bacteriostatic against anaerobic bacteria by increasing the formation of oxygen free radicals and restores the bactericidal capacity of leukocytes in hypoxic wounds by increasing tissue oxygen tension; in addition, HBOT interacts synergistically with several antibiotics to enhance their effect and thus reduce complications that may occur. Oxygen therapy is commonly started as soon as patients are stabilised (after initial debridement) and continued until the wound is completely healed. HBOT as an adjunctive therapy may reduce debridement sessions and drainage tube time in situ; but the efficacy of hyperbaric oxygen therapy is demonstrated by the exponential decrease in mortality rates reported in all studies, even in those patients where FG is associated with critical situations such as septic shock. It is not possible, however, to conclude that HBOT has a real positive influence on the reduction of average days of hospitalisation and treatment in intensive care units and consequently on health care expenditure, as the studies in the literature are conflicting. In fact, although HBOT has potential in FG therapy, not all hospitals have or can allow the patient rapid access to hyperbaric chambers and the degree of critical illness accompanying gangrene often precludes access to oxygen therapy. Moreover, there is no established treatment protocol for HBOT and given the rarity of FG cases, it is often very difficult to carry out studies, which is why the role of hyperbaric oxygen therapy is much discussed and, at the same time, a matter of controversy. It must be said that there has not been enough studies carried out in the literature to introduce this type of therapy as a first-line treatment in the clinical routine, but only as a second-line treatment, supporting standard therapy (early diagnosis, surgical debridement, antibiotic therapy, intensive care and reconstructive surgery).
CONCLUSION
The results in the literature review suggest that the combined effect of hyperbaric oxygen therapy with conventional therapy offers a significant advantage in the management of FG and that HBOT is associated with a significant survival benefit. Multicentre studies with a larger sample size are needed to confirm these observations, but are difficult to conduct due to the rarity of FG and the limited availability of HBOT in some centres. With a better understanding of the disease and treatment experience, the management of FG could see significant developments in the future.
ABBREVIATIONS
FG (Fournier’s gangrene)
FGSI (Fournier’s Gangrene Severity Index)
HBOT (Hyperbaric oxygen therapy)
ICU (Intensive Care Unit)
PIO (Population, Intervention, Outcome)
Conflicts of interest
The authors state that they have no conflicts of interest associated with this literature review.
Funding
The authors declare that they have not received any form of funding and that the study has no financial sponsor.
REFERENCES
- Atakan, IH, Kaplan M, Kaya E, Aktoz,, & Inci, O. A life-threatening infection: Fournier’s gangrene. International Urology and Nephrology. 2002; 34: 387-392.
- Morpurgo E & Galandiuk S. Fournier’s gangrene. Surgical Clinics of North America, 2002; 82: 1213-1224.
- Wilson B. Necrotizing fasciitis. The American Journal of Surgery. 1952; 18: 416-431.
- Shyam DC & Rapsang AG. Fournier’s gangrene. Surgeon. 2013; 11: 222–232.
- Horta R, Cerqueira M, Marques M, Ferreira P, Reis J, Amarante J. Fournier’s gangrene: from urological emergency to plastic surgery. Actas Urol Esp. 2009; 33: 925–929.
- Sorensen MD, Krieger JN, Rivara FP, Broghammer JA, Klein MB, Mack CD, et al. Fournier’s gangrene: population based epidemiology and outcomes. Journal of Urology. 2009; 181: 2120-6.
- Eke N. Fournier’s gangrene: a review of 1726 cases. British Journal of Surgery. 2000; 87: 718-728.
- Khamnuan P, Chongruksut W, Jearwattanakanok K, Patumanond J, Tantraworasin A. Necrotizing fasciitis: epidemiology and clinical predictors for amputation. International Journal of General Medicine; 2015; 8: 195–202.
- Bocking N, Matsumoto CL, Loewen K, Teatero S, Marchand-Austin A, Gordon J et al. High incidence of invasive group A streptococcal infections in remote indigenous communities in northwestern Ontario, Canada. Open Forum Infectious Disease. 2016; 4: ofw243.
- Stevens DL & Bryant AE. Necrotizing soft-tissue infections. The New England Journal of Medicine, 2017; 377: 2253–2265.
- Wong CH, Chang HC, Pasupathy S, Khin LW, Tan JL, Low CO. Necrotizing fasciitis: clinical presentation, microbiology, and determinants of mortality. The Journal of Bone and Joint Surgery American. 2003; 85, (A): 1454–1460.
- Basoglu M, Ozbey I, Atamanalp S, Yildirgan MI, Aydinli B, Polat O et al. Management of Fournier’s gangrene: review of 45 cases. Surgery Today. 2007; 37 (7): 558-563.
- Nomikos IN. Necrotizing perineal infections (Fournier’s disease): old remedies for an old disease. International Journal of Colorectal Disease. 1998; 13 (1): 48–51.
- Clayton MD, Fowler JE, Sharifi R & Pearl R.K. Causes, presentation and survival of fifty-seven patients with necrotizing fasciitis of the male genitalia. Surgery, Gynecology, Obstetrics archives. 1990; 170: 49-55.
- Korkut M, Içöz G, Dayangaç M, Akgun E, Yeniay L., Erdogan, O et al. Outcome analysis in patients with Fournier’s gangrene: report of 45 cases. Disease of the Colon & Rectum. 2003; 46: 649-652.
- Murakami M, Okamura K, Hayashi M, Minoh S, Morishige I. & Hamano K. Fournier’s gangrene treated by simultaneously using colostomy and open drainage. Journal of Infection; 2006; 53; and 15-18.
- Ochiai T, Ohta K, Takahashi M, Yamazaki S. & Iwai T. Fournier’s gangrene: report of six cases. Surgery Today. 2001; 31: 553-556.
- Safioleas M, Stamatakos M, Mouzopoulos G, Diab A, Kontzoglou K & Papachristodoulou A. Fournier’s gangrene: exists and it is still lethal. Surgical Clinics of North America. 2006; 38: 653-657.
- Jeong HJ, Park SC, Seo IY & Rim JS. Prognostic factors in Fournier gangrene. International Urology and Nephrology; 2005 12: 1041-1044.
- McKay TC & Waters WB Fournier’s gangrene as the presenting sign of an undiagnosed human immunodeficiency virus infection. Journal of Urology. 1994; 152: 1552-1554.
- Sarani B, Strong M, Pascual J & Schwab CW. Necrotizing fasciitis: current concepts and review of the literature. Journal of the American College of Surgeon. 2009; 208: 279-88.
- Cardoso JB & Féres O. Grangena de Fournier. Medicina. 2007; 40: 493-9.
- Torremadé Barreda J, Millán Scheiding M, Suárez Fernández C, Cuadrado Campaña JM, Rodríguez Aguilera J, Franco Miranda E, et al. Fournier gangrene. A retrospective study of 41 cases. Cirugía Española. (English Ed). 2010; 87: 218-23.
- Uppot RN & Levy HM. Patel PH. Case 54: Fournier gangrene. Radiology. 2003; 226: 115-117.
- Smith GL, Bunker CB & Dinneen MD. Fournier’s gangrene. British Journal of Surgery, 1998; 81: 347-355.
- Rotondo N. Fournier’s gangrene: an unusual presentation of sepsis. The Journal of Emergency Medicine. 2002; 23: 413-414.
- Saffle JR, Morris SE & Edelman L.Fournier’s gangrene: management at a regional burn center. J Burn Care Res.2008; 29: 196-203
- Villanueva-Sáenz E, Martínez Hernández-Magro P, Valdés Ovalle M, Montes Vega J, Alvarez-Tostado FJF. Experience in management of Fournier’s gangrene. Tech Coloproctol. 2002; 6: 5-13
- Chao L, Xu Z, Long-Fei L, Fan Q, Jin-Bo C & Xiong-Bing Z. Hyperbaric Oxygen Therapy as an Adjuvant Therapy for Comprehensive Treatment of Fournier’s Gangrene. Urology Internationalis 2015; 94 (4): 453-8.
- Dellinger RP, Levy MM, Carlet JM, Bion J, Parker MM, Jaeschke R et al. Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shocks. Intensive Care Medicine. 2008; 34 (1): 17–60.
- Jallali N, Withey S & Butler PE. Hyperbaric oxygen as adjuvant therapy in the management of necrotizing fasciitis. American Journal of Surgery. 2005; 189 (4): 462-466
- de Nadai TR, Daniel RF, de Nadai MN, da Rocha JJ, Féres O. Hyperbaric oxygen therapy for primary sternal osteomyelitis: a case report. Journal of Medical Case Report.2013; 7:67.
- Parra RS, Lopes AH, Carreira EU, Feitosa MR, Cunha, FQ, Garcia SB et al. Hyperbaric oxygen therapy ameliorates TNBS-induced acute distal colitis in rats, Medical Gas Reserch. 2015; 5.6.
- Plafki C, Peters P, Almeling M, Welslau W & Busch R. Complications and side effects of hyperbaric oxygen therapy. Aviation, Space, and Environmental Medicine. 2000; 71: 119–124.
- Lo T, Song C, Alismail A, et al. Hyperbaric oxygen therapy: how safe is it for critically ill patients? Critical Care Medicine. 2014; 42: A1520.
- Smerz RW. Incidence of oxygen toxicity during the treatment of dysbarism. Undersea & Hyperbaric Medical Society.2004; 31: 199–202
- D’Agostino Dias M, Fontes B, Poggetti RS, Birolini D. Hyperbaric oxygen therapy: types of injury and number of sessions–a review of 1506 cases. Undersea & Hyperbaric Medical Society.2008; 35: 53-60.
- Mindrup SR, Kealey GP, Fallon B. Hyperbaric oxygen for the treatment of fournier’s gangrene. Journal of Urology. 2004; 173: 1975-1977.
- Creta M, Longo N, Arcaniolo D, Giannella R., Cai T, Cicalese A et al. Hyperbaric oxygen therapy reduces mortality in patients with Fournier’s Gangrene. Results from a multi-institutional observational study. Minerva Urology and Nefrology.2020; 72: 223-228.
- Hollabaugh RS, Dmochowski RR, Hickerson WL, Cox CE. Fournier’s gangrene: therapeutic impact of hyperbaric oxygen. Plast Reconstructive Surgery.1998; 101: 94-100.
- Korhonen K, Hirn M, Niinikoski J. Hyperbaric oxygen in the treatment of Fournier’s gangrene. European Journal of Surgery. 1998; 164: 251-255.
- Feres O, Feitosa MR, Ribeiro da Rocha JJ, Miranda JM, Dos Santos LE, Féres AC et al. Hyperbaric oxygen therapy decreases mortality due to Fournier’s gangrene: a retrospective comparative study. Medical Gas Research 2021; 11 (1): 18-23.
- Mehl AA, Filho DC, Mantovani LM, Grippa MM, Berger R, Krauss D, Ribas D. Management of Fournier’s gangrene: experience of a university hospital of Curitiba. Rev Col Bras Cir. 2010; 37 (6): 435-41.
- Anheusera P, Mühlstädtb S, Kranzc J, Schneidewindd L, Steffensc J, Fornarab P. Significance of Hyperbaric Oxygenation in the Treatment of Fournier’s Gangrene: A Comparative Study. Urology Internationalis 2018; 101: 467–471.
- Shaw JJ, Psoinos C, Emhoff TA, Shah SA, Santry HP. Not Just Full of Hot Air: Hyperbaric Oxygen Therapy Increases Survival in Cases of Necrotizing Soft Tissue Infections. Surgical Infections. 2014; 15 (3): 328-335.
- Hung MC, Chou CL, Cheng LC, Ho H, Niu KC, Chen HL et al. The role of hyperbaric oxygen therapy in treating extensive Fournier’s gangrene Urological Science 2016; 27 (3): 148-153.
- Rosa I & Guerriero F. Hyperbaric Oxygen Therapy for the Treatment of Fournier’s Gangrene: A Review of 34 Cases. Scientific Review by Ordem dos Médicos 2015; 28 (5): 619-623.
- Devaney B, Frawley G, Frawley L, Pilcher D.V. Necrotising soft tissue infections: the effect of hyperbaric oxygen on mortality. Anaesthesia Intensive Care. 2015; 83 (6): 685-92.