Antonino Calabrò1, Federica Ilari2, Lorenzo Rizzo3, Alessia Lezzi4, Simone Zacchino4, Pierluigi Lezzi5, Giovanni Maria Scupola6, Marta Fanton7, Roberto Lupo6, Elsa Vitale8*
- Psychiatry Unit, Nuovo Ospedale Degli Infermi, Biella, Italia
- Department of Translational Medicine, University of Eastern Piedmont, Biella, Italy
- Eating Disorders Cente, Villa Eèa Cooperative Città Azzurra, Bolzano, Italy
- Associazione Nazionale Italiana Tumori, Lecce, Italy
- Neurology Unit, Vito Fazzi Hospital, Local Health Authority (ASL) Lecce, Italy
- Department of Emergency Medicine, San Giuseppe da Copertino Hospital, Local Health Authority Lecce, Italy
- Azienda ospedaliera nazionale SS. Antonio e Biagio e Cesare Arrigo, S.C. Cardiologia, Alessandria, Italy
- Department of Mental Health, Local Health Authority (ASL) Bari, Italy
*Corresponding Author: Elsa Vitale, Department of Mental Health, Local Health Authority (ASL) Bari, Italy. E-mail: vitaleelsa@libero.it; ORCID: 0000-0002-9738-3479.
Cite this article
ABSTRACT
Introduction: Personality disorder sufferers with severe self-harm and experience long psychiatric hospitalizations have complex mental health conditions and are at risk of suicide. When the symptoms of emotional instability are combined with self-harm, the resulting crisis often becomes difficult for patients and caregivers to manage. To improve care during these crises, the Dutch Multidisciplinary Guideline for Personality Disorders designates “brief admission” (BA) hospitalizations as an ameliorative intervention.
Objective: To describe the effectiveness of short hospitalization nursing care for people with borderline personality disorder and who practice self-harm, compared to ordinary hospitalization. Methods: A narrative review was conducted through the Embase and CINAHL databases, the selected articles had to answer the following research questions: “what are the observable benefits of short-term hospitalization on patients with borderline personality disorder?”; and “what are the benefits compared to short hospitalization operators?”.
Results: Seven studies were selected. The results show that BA was perceived as an effective nursing intervention, which promoted the patient’s self-determination and self-care. This helped increase confidence in daily life and allowed people to maintain their daily routines, work, and relationships by decreasing long hospitalizations and increasing patient compliance. There has also been benefit from the staff, who report an improvement in work quality.
Conclusions: This type of hospitalization has developed in Northern European states. BA has never been tested in the Italian healthcare sector. It would be appropriate and desirable, given the results obtained, to experiment with this procedure also in Italy to obtain specific feedback regarding the relationship of short-term hospitalization with our National Health Service. It is hoped that this research can be a stimulus in this sense.
Keywords: Borderline Personality Disorder, Nursing Management, Brief Admission, Patient Experiences, Self-Harm, Short-term hospitalization.
INTRODUCTION
Borderline Personality Disorder (BPD) is the most common personality disorder observed in clinical settings and within societies around the world. This disorder is characterized by various elements: a set of unstable and changing interpersonal relationships; emotional instability which often manifests itself with sudden attacks of anger; poor impulse control associated with self-harm; identity disorders [1]. The prevalence of people with borderline personality disorder in general and clinical psychiatric populations is approximately 4% and 20%, respectively. Approximately 75% of patients with borderline personality disorder attempt suicide and 10% succeed in their attempt [2]. Self-harm is part of the signs and symptoms of BPD and is the act of harming oneself voluntarily but without a conscious or declared suicidal intention (non-suicidal self-harm ANS) [3].
It is a very common phenomenon widespread especially among young people, in fact, it is also a major health care problem among both outpatient psychiatric patients and those in hospital care, with incidence rates of 55% and 65%, respectively. When the subject with BPD practices recurrent acts of self-harm, it is due to his inability to express his own internal suffering, he attacks his own body because he has the impression that by doing so, he will calm down. This becomes difficult to manage both for the patients themselves but above all for the healthcare personnel who deal with them [2]. Patients with borderline personality disorder are followed in both outpatient and hospital settings. Treatment typically begins with community services with day care and individual and/or group psychotherapy, depending on the individual [4].
When the behavior of these individuals becomes dangerous to their health, treatment may sometimes be necessary. interruption of outpatient treatment, preferring hospitalization in a psychiatric ward to ensure good protection for the patient. However, unplanned or long-term hospitalization for these patients without a clear treatment structure is very often associated with clinical and functional decompensation [5]. Hospitalization has been shown to have limited value, with often a failure to eradicate ideas. aimed at anti-conservative actions, with the development of possible negative side effects such as the beginning of a period of regression and the continuous need for repeated hospitalizations over time [6].
The Dutch Multidisciplinary Guideline for Personality Disorders [7] recommends short-term hospitalization as a treatment and crisis management approach for people with borderline personality disorder. Similarly, the National Institute for Health and Clinical Excellence (NICE) Clinical Guideline [8] for patients with borderline personality disorder mentions the development of autonomy and the promotion of individual choice as key factors for this type of treatment. Patients should be actively involved in finding solutions to their problems even during a crisis, as this allows them to gain experience in managing the crisis and to develop a certain autonomy regarding the decisions to be made at that moment [4].
Early hospitalizations and preventive interventions have made it possible to positively change the subsequent clinical course of individuals with borderline personality disorder. It was soon noticed that preventive psychiatric hospitalizations for such patients led to significantly greater agreement between healthcare professionals and patients on the treatment they would have liked to undertake and thanks to this type of intervention many patients who took part experienced the control over one’s own care. Following this model, to support patients with borderline personality disorder, a specific crisis intervention called “brief admission” (short hospitalization or BA) was developed [2]. With the advent of the new diagnostic and statistical manual in 2014 (DSM V), the new perspectives of this disease have also changed, and therefore also the treatments. Since then a new path has been started, therefore few review studies have been found one of these is by Helleman et,[4] al. who subsequently conducted the experiments that were introduced. With this article we want to raise awareness and bring out new perspectives for the treatment of this pathology
Purpose
To describe the effectiveness of short hospitalization nursing care for people with borderline personality disorder and who practice self-harm, compared to ordinary hospitalization.
MATERIALS AND METHODS
On the day 04/11/2023 with the support of the staff of Biomedical Library Foundation in Biella, Italy, a bibliographic search was conducted within the Embase and CINAHL Complete databases.
Search strategy and keywords used
A narrative review of the literature [9] was conducted following the methodology reported in the ‘Scale for the Assessment of Narrative Review Articles’ (SANRA) [10]. The following research questions were formulated:
- What are the benefits of short hospitalization for patients suffering from BPD?
- What are the benefits compared to short-term hospitalization operators?
To conduct the literature search, a research question was previously outlined using the P.I.O. framework (Table 1), search strings were subsequently created on biomedical databases such as Embase and CINAHL, using the Boolean operators “AND” and “OR” to interconnect the following keywords: Borderline Personality Disorder, Emotionally unstable personality disorder, Injuries, Self-Inflicted, short hospitalization, brief hospital, Nursing Staff, Hospital, Nursing Outcomes, Nursing Management.
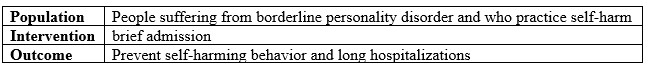
Table 1. The PIO methodology assessment.
Inclusion and Exclusion criteria
All original studies, attributable to primary resources, relevant to the research question illustrated were included. Only references written in English published in the last 15 years were taken into consideration.
However, secondary studies were excluded. Also excluded were all those references such as collections of abstracts, oral dissertations, and those quotes for which it was not possible to find the written “full text” version through the library circuit of the “Virtual Library for Health – Piedmont” (BVS – P).
Literature selection method: From the results of the searches carried out on the databases, a total of 128 bibliographical references were included. The results obtained were analyzed by two evaluators independently, by title and abstract, to identify relevant articles. The selected studies were found in full text format, read critically and the relevant ones were included in the review.
Extrapolated variables; the following data were extrapolated from the included studies: title, authors; study design; study context; mode; results and conclusions and listed in chronological order.
RESULTS
The bibliographic search revealed 128 references, of which 24 in CINAHL Complete and 104 in Embase. After a selection by reading the title and abstract, 96 articles were excluded. The articles initially included were 32; after removing the double 18s, 15 full text articles remained. The results were analyzed by two evaluators independently and read critically; after removing secondary studies, 7 articles were selected, respectively: 5 articles in Embase and 2 articles in CINAHL Complete.
Study selected
Below are the synoptic table 2 summarizing the selected articles.
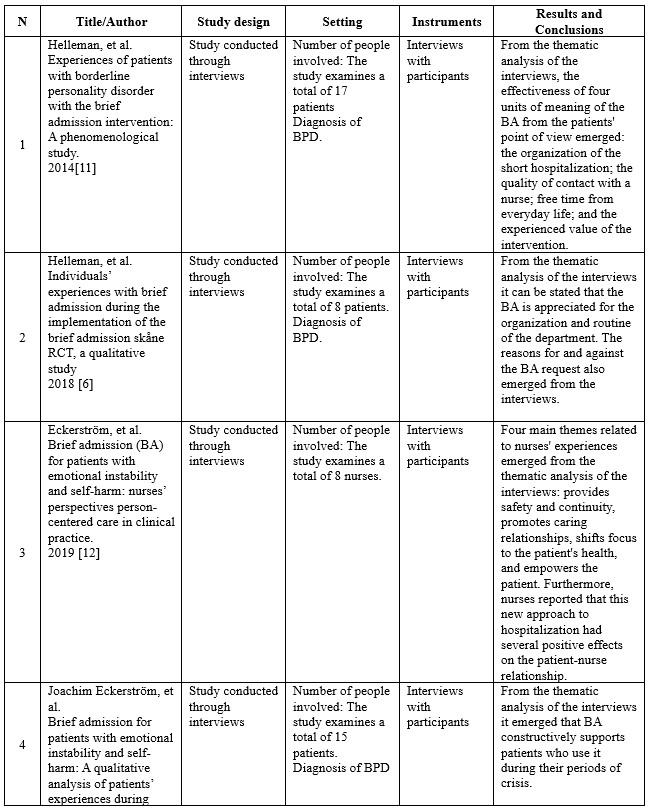
Table 2. Studies selected in the present review.
Study description
The first article is a study conducted through interviews, using Giorgi’s descriptive phenomenological methodology: Experiences of patients with borderline personality disorder with the brief admission intervention: A phenomenological study; published in International Journal of Mental Health Nursing in March 2014 [11]. The researchers’ overall objective was to describe the lived experiences of patients diagnosed with borderline personality disorder during the brief admission. A total of seventeen patients participated in the present study, which was conducted between January 2011 and August 2012. Patients were included according to the following criteria: individuals receiving public mental health services in the Netherlands; sufficient understanding of the Dutch language; diagnosis of borderline personality disorder according to the Diagnostic and Statistical Manual of Mental Disorders-IV (DSM-IV) criteria; ability to sustain an interview; prior experience with brief admission; neither age nor gender were considered. Instead, patients who met the following criteria were excluded: substance abuse; persons who presented fear that the interview would be recorded. Data were collected through interviews lasting between 45 and 75 minutes each, structured following a common pattern and based on clinical experience and a review of relevant Helleman literature. Data saturation was reached when no new meaning units were mentioned after interviews were conducted with 15 participants. Interviews with participants were audio recorded and transcribed verbatim. The meaning units in the transcripts were then identified and analyzed to reveal current problems and patterns following the steps described by Giorgi. Thematic analysis of the interviews revealed the effectiveness of four units of meaning of short hospitalization from the patients’ perspective: the organization of the short hospitalization; the quality of contact with a nurse; the regaining of free time in daily life; and the personal value this type of intervention acquired for patients. These units of meaning formed the essential structure of the experience. Patients also reported that the quality of contact with a nurse is the most important thing. Nurses should therefore be aware of the meaning and value of their relationship with patients with borderline personality disorder considering the strong interpersonal hypersensitivity of such individuals.
The second article is an interview study focusing on qualitative analysis of patients’ experiences: Individuals’ experiences with brief admission during the implementation of the brief admission skåne RCT, a qualitative study; published in Nordic Journal of Psychiatry Nordic [6]. The researchers’ overall objective was to detect possible limitations and strengths of brief admission and what were the reasons for requiring or conversely not requiring this type of admission. A total of 8 patients participated in the present study. Patients were included according to the following criteria: meeting at least three criteria for a diagnosis of borderline personality disorder; having been admitted to a psychiatric hospital for acute care for at least seven days or having presented to a psychiatric emergency room at least three times in the past six months; having recently performed acts of self-harm and/or recurrent suicide attempts; and age ≥18 years to 60 years. In contrast, patients were excluded if they met the following criteria: no regular contact with outpatient psychiatric services; somatic disorder or need for medication management that contributes significantly to the inclusion criteria (e.g., if self-harm occurs only during episodes of hypoglycemia in a diabetic person or in someone with substance-induced psychosis); homeless persons.
Data were collected through interviews conducted at the Lund psychiatric clinic, their duration was between 20 and 45 minutes each, and all interviews were conducted following a common pattern. The interviews with the participants were audio-recorded and transcribed verbatim. The units of meaning in the transcripts were then identified and analyzed to reveal current problems and patterns. From the thematic analysis of the interviews, it can be stated that the elements of short hospitalization most valued by the participants were the organization and routine of the ward. This is contrasted with the statements of some patients who reported that they had problems with some negative attitudes of the staff. Regarding the reasons reported for requesting short hospitalization, effective prevention of impulses aimed at self-harm, ending social isolation, creating a daily routine, and having an alternative to excessively long hospitalizations and mandatory hospitalizations emerged. Reasons for not requesting short hospitalization, on the other hand, are fear of rejection and difficulty in deciding the degree of severity of personal problems.
The third article is an interview study focused on qualitative analysis of nurses’ experiences: Brief admission (BA) for patients with emotional instability and self-harm: nurses’ perspectives person-centered care in clinical practice; published in International Journal of Qualitative Studies on Health and Well-being [12]. The researchers’ overall objective was to describe the experiences of nurses working with BA related to patients with emotional instability and self-harm. A total of 8 nurses participated in the present study. Purposive sampling was used to recruit participants. The only criterion that was followed to include the nurses was that they worked, during day shifts, within the selected psychiatric clinic, in the ward where the short hospitalization was taking place. Interviews with participants were audio recorded and transcribed verbatim. Units of meaning in the transcripts were then identified and analyzed to reveal current problems and patterns. Thematic analysis of the interviews revealed four main themes related to nurses’ experiences: providing safety and continuity, promoting relationship as caring time, shifting the focus to inpatient health, and empowering the patient. In addition, nurses reported that this new approach to hospitalization had several positive effects.
The fourth article is an interview study focusing on qualitative analysis of patients’ experiences: Brief admission for patients with emotional instability and self-harm: A qualitative analysis of patients’ experiences during crisis; published in International Journal of Mental Health Nursing [2]. The researchers’ overall goal was to answer the following research questions: what are patients’ experiences during brief admission? What do patients think are the key components of ‘brief admission? What improvements are considered relevant by patients? Purposive sampling was used to recruit participants, starting with contact with those who had most used short admission. A total of fifteen patients participated in the present study. Patients were included according to the following criteria: possessing a documented clinical history of emotional instability (mainly problems with emotion regulation and impulse control, borderline personality disorder); prior experience with brief admission; whether the patient had recently performed acts of self-harm and/or recurrent suicide attempts; neither age nor gender were taken into account. Instead, patients who had a primary diagnosis of psychotic disorder or depressive disorder were excluded.
Data were collected through interviews conducted at participants’ outpatient units, their duration ranged from 13 to 51 minutes each (mean = 31 minutes), and all interviews were conducted following a common pattern and structured based on a review of previous research. Interviews with participants were audio recorded and transcribed verbatim. The units of meaning in the transcripts were then identified and analyzed to reveal current problems and patterns following the steps described by Giorgi. Thematic analysis of the interviews revealed four themes related to patients’ experiences: “it is a break when life gets difficult”; “it is comforting to know that there is help”; “it encourages taking personal responsibility”; and “it is helpful to see problems from a different perspective.” Four themes also described key components: “a clear treatment plan,” “a smooth admission procedure,” “a friendly and welcoming approach from staff,” and “daily conversations.” Finally, three themes described areas for improvement: “feeling guilty for requesting short hospitalization,” “room occupancy problems,” and “differences in staff competence.” Overall, the results indicate that short hospitalization constructively supports patients with emotional instability and self-harm during a period of crisis.
The fifth article is a study conducted through inductive and qualitative interviews, uses hermeneutic phenomenological methodology and is inspired by Ricoeur’s theory of interpretation: A Brief Breathing Space: Experiences of Brief Admission by Self-Referral for Self-Harming and Suicidal Individuals with a History of Extensive Psychiatric Inpatient Care; published in Issues Ment Health Nurse [13]. The overall goal of the researchers was to detect the main characteristics as well as pre-expectations and reflections on potential improvements and adaptations of short hospitalization through patients’ personal experiences during their BA. A total of seven patients participated in the present study. Patients were included if they had met the following two criteria: prior experience of short admission; having been admitted to a hospital ward for psychiatric care for at least one hundred and eighty days in the 365 days prior to short admission.
Data collection was carried out through interviews conducted at patients’ homes or within psychiatric clinics in Helsingborg, Lund or Malmo between September and October 2018. All interviews were conducted following a common pattern. Interviews with participants were audio recorded and transcribed verbatim. The units of meaning in the transcripts were then identified and analyzed to reveal current problems and patterns. From the thematic analysis of the interviews, it can be said that the patients experienced the short hospitalization as a worthy antidote to the loss of control in dealing with self-injurious and suicidal instincts; moreover, the relief of not being continually interviewed reduced to some extent the negative feelings of fear in seeking help and care from health care personnel. Contrast this, however, with the statements of some patients who reported how brief hospitalization could offer the help and protection needed in times of mild crisis, but how it was of little help in the face of a more severe crisis.
The sixth article is a study conducted through interviews, using the descriptive qualitative method: Experiences of how brief admission influences daily life functioning among individuals with borderline personality disorder (BPD) and self-harming behavior; published in Journal of Clinical Nursing [14].
The researchers’ overall goal was to explore the experiences of how brief admission affects daily life functioning among individuals with borderline personality disorder and self-injurious behavior. Purposive sampling was used to recruit participants. A total of sixteen patients participated in the present study, which was conducted between November 2020 and January 2021. Patients were included according to the following criteria: diagnosis of borderline personality disorder; experience of brief hospitalization; whether the patient had recently performed acts of self-harm; neither age nor gender were considered. Instead, patients who met the following criteria were excluded: being admitted to a hospital at that time. Data collection was carried out through interviews conducted at the location chosen by each participant, their duration was between 15 and 90 minutes each, and all interviews were structured and conducted following a common pattern.
Data saturation was reached when no new meaning units were mentioned after interviews were conducted with 13 participants. Interviews with participants were audio recorded and transcribed verbatim. The meaning units in the transcripts were then identified and analyzed to reveal current problems and patterns. From the thematic analysis of the interviews, it can be stated that short hospitalization was perceived as a functioning nursing intervention that promoted self-determination and self-care, helping to increase control over one’s everyday life. In addition, short hospitalization made it easier for people to create or maintain a daily routine, employment and social relationships.
The seventh article is a naturalistic study with repeated measures (pre-test and post-test): Patient-Initiated Brief Admission for Individuals with Emotional Instability and Self-Harm: An Evaluation of Psychiatric Symptoms and Health-Related Quality of Life; published in Issues in Mental Health Nursing. Aim was to evaluate how symptoms of anxiety, depression and health-related quality of life (HRQoL) change after patient-initiated brief admission (PIBA), in patients in crisis with increased risk of self-harm. One hundred and thirteen patients were recruited from a Stockholm psychiatric clinic between 2016 and 2020. Upon admission and discharge, patients completed the Hospital Anxiety and Depression Scale (HADS) and the EuroQoL-5 Dimension Questionnaire (EQ-5D). Two outpatient psychiatric clinics and two psychiatric hospital departments in Stockholm specializing in BPD and anxiety disorders were involved initially.
During the 4-year intervention period (2016-2020), a reorganization was performed, and four additional outpatient units were included. By minimizing exclusion criteria and involving only inpatient and outpatient adult psychiatric units specializing in BPD, our patient sample is considered representative of the patient population of these units. One of the units had two patient rooms dedicated to PIBA, while the other unit had one room dedicated to PIBA. Inclusion criteria were as follows: (1) clinical history and current symptomatology of emotional instability (mainly problems with emotion regulation and impulse control) and a history of self-harm and (2) at least one previous period of inpatient care. Of the 145 patients who had PIBA contracts during the intervention period, 113 (78%) gave oral and written informed consent to participate in the study. The results obtained among the 113 patients with PIBA contracts, 57% (n = 64) used PIBA at least once during the study period.
There was a significant decrease in symptoms of anxiety and depression, as reflected in the HADS score, after the first hospitalization, with a medium effect size. Significant reductions in both anxiety and depression symptoms were also observed after subsequent hospitalizations. Combining the two subscales of the HADS, the results showed a large effect (d = 0.75) on the total burden of psychiatric symptoms. This result was confirmed in the analysis of the EQ-5D dimension “anxiety/depression,” with a large reduction (d = 0.72) in symptoms. The HRQoL of the participants increased significantly, with a large effect as measured by the EQ-5D VAS and a mean effect as measured by the EQ-5D index. and analysis of each dimension of the EQ-5D index showed that only the “Anxiety/depression” dimension was significantly decreased (except for “Habitual Activities” in the third admission to PIBA). This specific EQ-5D result was consistent with the changes in anxiety and depression symptoms in the HADS.
The potential reasons for the absent effect on the “Mobility” and “Self-care” dimensions could be due to low levels of symptomatic load in these areas. Moreover, they were not the primary indication for PIBA. The decrease in the “Habitual Activities” dimension was not significant for the first, second, and fourth admissions to PIBA. This could be an area for improvement and show the need to further educate health care providers on helping patients with behavior activation and helping self-help regarding initiating their daily activities. Almost all participants (95.2%) described PIBA as a constructive intervention. The importance of getting quick help when psychiatric symptoms worsen. The results of this study also reported high ratings (M = 9.02 out of 10) regarding the approach from staff, which aligns with previous studies of PIBA [11,12] in which a friendly and welcoming attitude from health care providers was described.
Based on this, our hypothesis is that PIBA is cost-effective and efficient in terms of utilization. The overall purpose of PIBA is to provide a patient-initiated time-out in a safe environment when a crisis is imminent, the patients in this study, in which most had been diagnosed with a disorder that was previously considered “difficult to treat”, stated that PIBA fulfills its stated purpose.
DISCUSSION
The objective of this review was to describe published studies on the effectiveness of short hospitalization nursing care for people with borderline personality disorder and who practice self-harm, six studies were identified of which 6 are qualitative [2,6,11–14] and one quantitative [15].
The thematic strengths found by the patients are summarized in these 4 macro areas identified by Helleman [6] and common to other authors: were: 1 Structure and routine, 2 Positive staff attitudes, 3 The experience of self and 4 Negative staff attitudes.
- Structure and routine: Patients reported value in knowing that a BA was available to them and experienced it as helpful in regaining basic sleep and eating routines, getting respite from the demands at home, and creating meaning safety. The fact that they could be sure that there would be daily conversations reportedly created a feeling of safety. Even just knowing that BA was a possibility was mentioned as something important, even if it wasn’t used. The reported perception was that the BA had prevented them from self-harming and attempting suicide. However, self-harm treatment was not perceived as the focus of BA. Rather, BA’s role was to meet basic needs by providing “rest from real life” by letting go of daily duties or overthinking to do something.
- Positive attitudes from staff: Patients also reported positive attitudes from staff. A warm welcome at the start of the BA is “more important than people think”. The experience of being listened to, taken seriously and feeling responsible for their health was perceived as building their confidence. The operators ensured daily conversations, which led to feelings of greater safety.
- The experience of the self: main objective of the BA, during admission the responsibility for managing current crises is in the hands of the participants themselves. This was mostly described as a positive experience: patients were able to take control of their situation, self-determine (taking medications not from nurses but self-managed), keep personal items, sense of independence and integrity, all in one protected environment where discussion is always possible.
- Weaknesses noted by patients were linked to: From the staff as lack of knowledge about BA, negative attitudes about BA expressed in front of patients, which created an unwelcome and unsafe feeling and lack of time. Lack of time was another factor. This made them feel rejected, which in turn increased distress and negative thoughts.
Organizationally: Mixing BA with acute hospitalizations was a challenge for patients in BA when they found themselves relatively stable compared to other hospitalized patients. This led to worries about irritating others, feelings of guilt for trying to use BA preventively. It has been noted that having only one room, within an acute ward, undermines the entire purpose of the BA as the risk of being left alone during the crisis and without support from providers is very high.
The quantitative study by Eckerström [15] analyzes the aspects of anxiety/depression and quality of life through two scales, the first Hospital Anxiety and Depression Scale (HADS) and the second EuroQoL-5 Dimension Questionnaire (EQ-5D). The data collected validates those of previous studies for anxiety and depression, a significant decrease in symptoms of anxiety and depression, as reflected in the HADS score, after the first hospitalization. Significant reductions in anxiety and depression symptoms were also observed after subsequent hospitalizations. Combining the two subscales of the HADS, the results showed a large effect (d = 0.75) on total psychiatric symptom burden. This result was confirmed in the analysis of the EQ-5D dimension “anxiety/depression”, with a large reduction (d = 0.72) in symptoms. These findings match the results of a previous study, which included 15 patient respondents who reported that BA helped them overcome suicidal thoughts, depressive symptoms, and emotional distress [12]. The quality-of-life results highlight that nearly all participants (95.2%) described BA as a constructive intervention, the importance of receiving rapid help when psychiatric symptoms worsen. The results of this study also reported high ratings regarding the staff approach. Patients who have experienced both BA and regular hospital care describe the latter as old-fashioned, as patients have to wait until they get worse to receive treatment and demonstrate their need for help with self-harm as already demonstrated by Lindkvist’s study [13].
In reference to the second research question “What are the benefits compared to short-term hospitalization operators?” Eckerström’s study [12] aims to describe the experiences of nurses working with BA in relation to patients with emotional instability and self-harm, through interviews. The data that emerged also confirms from the nurses some data already collected by the patients from a care perspective such as: provides safety and continuity; direct access to the patient, without going through official channels Emergency, urgency and acceptance department (DEA), Mental Health Center (CSM) has improved communication between operators and patients, reducing misunderstandings that sometimes arise when communications are filtered through different nurses and doctors. Know what you both expect from the contract.
Furthermore, nurses described their new responsibility as challenging because they had to support patients with nursing interventions rather than medications or monitoring alone. In this sense the improvement of the patient-nurse relationship leads to a greater understanding of the person behind the patient, which was mostly described in a positive way.
Promoting person-centered care led to a demonstration of nurses’ confidence in their patients’ abilities fostered a positive relationship in which patients began to act more constructively, leading to mutual respect and a more balanced relationship. However, such in-depth reporting was painful because it became too close to the patients. BA gave nurses the mandate and the possibility to focus on nursing care, making the best use of those concepts of empathy that belong to us.
CONCLUSIONS
The objective of this review was to describe published studies on the effectiveness of short hospitalization nursing care for people with borderline personality disorder and who practice self-harm. Considering what was assessed in the discussions, we can affirm that short hospitalization is the best nursing intervention in terms of effectiveness and results obtained in the treatment of the population taken into consideration. The aspects of greatest interest that have the best outcomes are: quality of the patient-nurse relationship, the regaining of free time in daily life, the awareness of support for quality and duration of care, the management of self-harming and suicidal instincts, the promotion of self-determination and self-care, the maintenance of valid social relationships in the family and in the working world, the increase in the perception of security.
Undoubtedly within our review we took into consideration the critical issues that emerged such as: organizational factors, patients in BA admitted to emergency facilities, lack of staff training.
Nurses should therefore be aware of the meaning and value of their relationship with patients suffering from borderline personality disorder considering the strong interpersonal hypersensitivity of such subjects.
Short-term hospitalization was born and developed within the psychiatric wards and healthcare facilities of Northern European states, where nowadays it very often represents the most used treatment for the care of people with borderline personality disorder, as well as all the complications that this diagnosis brings. As regards the situation in our country, however, there are no studies that deal with this topic. In Italy, in fact, short hospitalization has never been experimented with, despite the effectiveness demonstrated by the results obtained from this treatment. Given the modest number of studies that we have analyzed for this type of hospitalization, it would be appropriate and desirable to experiment with this procedure also in Italy to have specific feedback regarding the relationship of short hospitalization with our National Health Service.
It is considered appropriate to continue and stimulate research into this topic, given the few studies on this subject present in the literature, as the topic we have discussed is one with a strong social impact.
Strengths and limitations
The strengths of the study are: original argument on a developing topic which has demonstrated excellent results, from the research carried out the presence of only one revision carried out by Helleman 2014 at the beginning of the process, 2014 subsequently no other revisions were found. It is believed to be an important contribution for the scientific community to be able to make known a patient-centered care model and consequently to be able to implement it in other contexts as well.
The limits are specific to narrative reviews: poor reproducibility of the research, little specificity.
Furthermore, the study was self-financed which led to a search of a few databases and the possibility of downloading full texts.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest.
Author Contributions
All Authors equally contributed.
Acknowledgments
Authors thank all the staff of Biomedical Library Foundation in Biella, Italy.
REFERENCES
[1] American Psychiatric Association. DSM-5 Manuale diagnostico e statistico dei disturbi mentali. Quinta. Milano: Raffaello Cortina Editore; 2014.
[2] Eckerström J, Flyckt L, Carlborg A, Jayaram‐Lindström N, Perseius K. Brief admission for patients with emotional instability and self‐harm: A qualitative analysis of patients’ experiences during crisis. Int J Ment Health Nurs 2020;29:962–71. https://doi.org/10.1111/inm.12736.
[3] Hawton K, Saunders KEA, O’Connor RC. Self-harm and suicide in adolescents. Lancet Lond Engl 2012;379:2373–82. https://doi.org/10.1016/S0140-6736(12)60322-5.
[4] Helleman M, Goossens PJJ, Kaasenbrood A, Van Achterberg T. Evidence Base and Components of Brief Admission as an Intervention for Patients With Borderline Personality Disorder: A Review of the Literature: Evidence Base and Components of Brief Admission as an Intervention for Patients With Borderline Personality Disorder. Perspect Psychiatr Care 2014;50:65–75. https://doi.org/10.1111/ppc.12023.
[5] Liljedahl SI, Helleman M, Daukantaité D, Westrin Å, Westling S. A standardized crisis management model for self-harming and suicidal individuals with three or more diagnostic criteria of borderline personality disorder: The Brief Admission Skåne randomized controlled trial protocol (BASRCT). BMC Psychiatry 2017;17:220. https://doi.org/10.1186/s12888-017-1371-6.
[6] Helleman M, Lundh L-G, Liljedahl SI, Daukantaité D, Westling S. Individuals’ experiences with brief admission during the implementation of the brief admission skåne RCT, a qualitative study. Nord J Psychiatry 2018;72:380–6. https://doi.org/10.1080/08039488.2018.1467966.
[7] Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M. Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ 2008:a1655. https://doi.org/10.1136/bmj.a1655.
[8] NICE. Borderline Personality Disorder: Treatment and Management. Leicester (UK): British Psychological Society (UK); 2009.
[9] Grant MJ, Booth A. A typology of reviews: an analysis of 14 review types and associated methodologies. Health Inf Libr J 2009;26:91–108. https://doi.org/10.1111/j.1471-1842.2009.00848.x.
[10] Baethge C, Goldbeck-Wood S, Mertens S. SANRA-a scale for the quality assessment of narrative review articles. Res Integr Peer Rev 2019;4:5. https://doi.org/10.1186/s41073-019-0064-8.
[11] Helleman M, Goossens PJJ, Kaasenbrood A, van Achterberg T. Experiences of patients with borderline personality disorder with the brief admission intervention: a phenomenological study. Int J Ment Health Nurs 2014;23:442–50. https://doi.org/10.1111/inm.12074.
[12] Eckerström J, Allenius E, Helleman M, Flyckt L, Perseius K-I, Omerov P. Brief admission (BA) for patients with emotional instability and self-harm: nurses’ perspectives – person-centred care in clinical practice. Int J Qual Stud Health Well-Being 2019;14:1667133. https://doi.org/10.1080/17482631.2019.1667133.
[13] Lindkvist R-M, Westling S, Liljedahl SI, Landgren K. A Brief Breathing Space: Experiences of Brief Admission by Self-Referral for Self-Harming and Suicidal Individuals with a History of Extensive Psychiatric Inpatient Care. Issues Ment Health Nurs 2021;42:172–82. https://doi.org/10.1080/01612840.2020.1789787.
[14] Enoksson M, Hultsjö S, Wärdig RE, Strömberg S. Experiences of how brief admission influences daily life functioning among individuals with borderline personality disorder (BPD) and self‐harming behaviour. J Clin Nurs 2022;31:2910–20. https://doi.org/10.1111/jocn.16118.
[15] Eckerström J, Carlborg A, Flyckt L, Jayaram-Lindström N. Patient-Initiated Brief Admission for Individuals with Emotional Instability and Self-Harm: An Evaluation of Psychiatric Symptoms and Health-Related Quality of Life. Issues Ment Health Nurs 2022;43:593–602. https://doi.org/10.1080/01612840.2021.2018530.
![]() This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.