Exploring the impact of Nurse Manager Leadership Styles on Nurses' Job Performance at Hamad Medical Corporation: A Cross-Sectional Study
Abdelbasset Ghalgaoui 1, 2, *, Mehdi Halleb 1, Maha Mohamed Marzouk Ahmed 1,
Osama Helmi Mohammad Subih 1, Nabil Ajjel 1
- Department of Nursing, Hamad Medical Corporation (HMC), Doha, Qatar.
- Institut Universitaire de Formation des Cadres (INUFOCAD), Port-au-Prince, Haiti.
* Corresponding author: Abdelbasset Ghalgaoui, Graduate Registered Nurse, Department of Nursing, Hamad Medical Corporation (HMC), Doha, Qatar. PhD Student in Education and Governance, Institut Universitaire de Formation des Cadres (INUFOCAD), Port-au-Prince, Haiti. Email: ghalgaouiabdelbasset@gmail.com
Cite this article
ABSTRACT
Introduction: Nurse performance is vital to patient safety and organizational effectiveness. Leadership style is a recognized determinant of performance, influencing consistency, adaptability, and professional growth. Understanding these dynamics is particularly important in multicultural healthcare environments.
Objective: This study explored the impact of nurse manager leadership styles on nurses’ job performance at Hamad Medical Corporation (HMC).
Methods: A cross-sectional survey was conducted with 980 registered nurses recruited through random sampling. Data were collected using a structured questionnaire including socio-demographic characteristics, the Multifactor Leadership Questionnaire (MLQ-5X), and the Nursing Performance Instrument (NPI). Data analysis was performed using SPSS version 26, applying descriptive statistics, and Spearman’s correlation, Mann–Whitney U, and Kruskal–Wallis H tests.
Results: The workforce was predominantly female (72.1%), married (83.7%), and expatriate, with a mean age of 40.4 years. Transactional leadership (2.57 ±085) was the most common style, followed by transformational (2.20±1.05), while passive-avoidant leadership was minimal (1.49±0.97). Transformational leadership demonstrated strong positive associations with consistency of practice and adaptability. Transactional leadership supported compliance but was less effective in stimulating innovation, while passive-avoidant leadership was negatively correlated with performance outcomes.
Conclusion: Transformational leadership emerged as the most effective style for enhancing nurse performance, while transactional leadership sustained compliance without fostering long-term growth. Strengthening transformational leadership among nurse managers at HMC may improve clinical outcomes, adaptability, and organizational performance.
Keywords: Leadership, Nurses, Job Performance, Practice
INTRODUCTION
In the complex and ever-evolving healthcare environment, the performance of nurses is a cornerstone of quality patient care and organizational success [1–4]. Nurses are at the forefront of healthcare delivery, directly influencing patient outcomes, safety, and satisfaction through their clinical skills, critical thinking, and interpersonal interactions [5–7]. The effectiveness with which nurses execute their duties is not solely dependent on their individual competencies but is significantly shaped by the leadership they receive. Nurse managers, in particular, play a crucial role in fostering an environment that optimizes nursing performance, as their leadership styles directly influence the motivation, development, and productivity of their teams [8].
Job performance in nursing encompasses a broad range of behaviors and outcomes, including adherence to protocols, clinical proficiency, teamwork, communication, and adaptability to challenging situations. High-performing nursing teams contribute to reduced medical errors, improved patient recovery rates, and enhanced overall efficiency within healthcare institutions [9–12]. The leadership styles employed by nurse managers have a profound impact on the performance of their nursing staff. Transformational leadership, characterized by its emphasis on inspiring, empowering, and intellectually stimulating nurses, is often associated with higher levels of performance, as it encourages innovation, professional growth, and a strong sense of ownership [13–16]. This style promotes a positive work environment, which is crucial for fostering high performance. In contrast, transactional leadership, which relies on clear directives, rewards, and corrective actions, can ensure compliance with standards but may not always foster the proactive and adaptive behaviors essential for complex clinical environments [17–19]. Passive-avoidant leadership, marked by a lack of engagement and decision-making, typically has detrimental effects on performance, leading to confusion and disorganization[8]. Recent studies continue to highlight the importance of effective nursing leadership in driving performance outcomes [8,14–19].
While existing literature has explored the relationship between nurse manager leadership styles and job performance, there remains a specific research gap concerning the context of Qatar. Studie in Qatar have investigated aspects such as the generational gap between nurses and nurse managers and its potential impact on job performance [20] . However, a comprehensive understanding of how various nurse manager leadership styles directly influence the diverse aspects of nurses' job performance within the unique healthcare landscape of Qatar, considering its multicultural workforce and specific organizational structures, is still limited. There is a particular need to understand which leadership styles are most effective in promoting optimal job performance among nurses in HMC, given the specific cultural and organizational dynamics of the region.
Objective
This study aims to investigate the specific influence of nurse manager leadership styles on nurses’ job performance at HMC. Specifically, it will examine the relationship between transformational, transactional, and laissez-faire leadership styles and various dimensions of nursing performance. The insights gained will be invaluable for developing targeted leadership training programs and organizational policies designed to optimize nursing performance, ultimately contributing to superior patient care and the sustained success of HMC's healthcare mission.
MATERIALS AND METHODS
Type and Classification of Study
This study employed a quantitative, cross-sectional research design to examine the relationship between nurse manager leadership styles and nurses' job satisfaction, work engagement, and job performance at Hamad Medical Corporation (HMC).
Comparisons and Predictors of Interest
The primary focus was on comparing various nurse manager leadership styles and their respective impacts on staff nurses’ job satisfaction, work engagement, and job performance.
Study Duration
The study was conducted over a period of approximately four months, from November 5, 2024, to March 1, 2025.
Sample Size Justification
To ensure reliability and representativeness of the findings, a sample size calculation was conducted based on a population of approximately 12,000 nurses. Using a 95% confidence level and a ±3% margin of error, a sample size of 980 nurses was determined to be appropriate. The sample size was calculated using Cochran’s formula:
where Z = 1.96, p = 0.5, e = 0.03.
The value p=0.5 was selected to provide the most conservative estimate and ensure an adequate sample size in the absence of prior data, while margin of error e = ±3% was chosen to achieve high precision and reliable representativeness of the study results.
Study Population and Setting
The study targeted registered nurses employed across different departments at Hamad Medical Corporation (HMC), Qatar. A simple random sampling procedure was used to select participants. The sampling frame consisted of the complete roster of licensed nurses at HMC, with each nurse assigned a unique identification number. Randomization was performed using Microsoft Excel’s RAND function to generate a randomly ordered list.
To mitigate potential non-response, the initial calculated sample of 980 nurses (based on a 95% confidence level and ±3% margin of error for a population of approximately 12,000 nurses) was increased by 245 nurses, resulting in 1,225 nurses being contacted. The questionnaire was distributed to these nurses via their official HMC email accounts, and 980 responses were received and included in the final study sample. This approach ensured equal probability of selection and broad representation across hospitals and nursing units within HMC.
The study was conducted exclusively within HMC facilities.
Inclusion Criteria
- Registered nurses currently employed at HMC.
- Nurses who voluntarily consented to participate.
- Nurses with a minimum of six months of experience at HMC to ensure familiarity with the organizational culture and leadership practices.
Exclusion Criteria
- Nurses on leave or absent during data collection.
- Nurses in managerial or supervisory roles.
- Contract or temporary nurses.
Data Collection
Data were collected via structured online questionnaires distributed through Google Forms. The survey instruments covered the following areas:
- Socio-demographic Data
- Collected information included age, gender, nationality, years of nursing experience, tenure at HMC, education level, hospital, and department.
- Multifactor Leadership Questionnaire (MLQ-5X)
This 45-item tool assessed leadership styles (transformational, transactional, and laissez-faire) across dimensions such as inspirational motivation, intellectual stimulation, and contingent reward. Responses were recorded on a 5-point Likert scale (0 = "Not at all" to 4 = "Frequently, if not always") [21].
Items were grouped into their respective leadership dimensions using the MLQ scoring key. For each dimension, a mean score was calculated by summing the responses to the items composing that scale and dividing by the number of valid responses. All leadership style subscales consisted of four items each. Blank or missing responses were excluded from the calculations. Higher mean scores indicated more frequent exhibition of the corresponding leadership behaviors. Leadership dimensions were analyzed as continuous variables rather than categorizing leaders into a single leadership style. The tool demonstrated strong reliability, with Cronbach’s alpha ranging from 0.70 to 0.90.
- Nursing Performance Instrument (NPI)
This 20-item instrument assessed nursing performance across clinical and interpersonal dimensions. Responses were rated on a 6-point Likert scale (1 = "Strongly Disagree" to 6 = "Strongly Agree") [22].
NPI scores were calculated by summing the item responses within each domain and dividing by the number of items to obtain mean domain scores. An overall NPI score was computed by averaging all 9 items. Missing responses were excluded from the calculations. Higher scores indicated better perceived nursing performance.
The instrument yielded a Cronbach’s alpha of 0.80, indicating strong reliability.
Statistical Considerations and Data Analysis
Primary and Secondary Outcomes
- Primary Outcomes: Nurses’ job performance.
- Secondary Outcome: The relationship between nurse manager leadership styles and the three primary outcomes.
Data Analysis Plan
1. Descriptive Statistics
Summarized participant characteristics and key variables using means and standard deviations (mean±SD), or medians and interquartile intervals (IQR), for numerical data, while ranges, and percentages for qualitative and categorical data.
2. Inferential Statistics
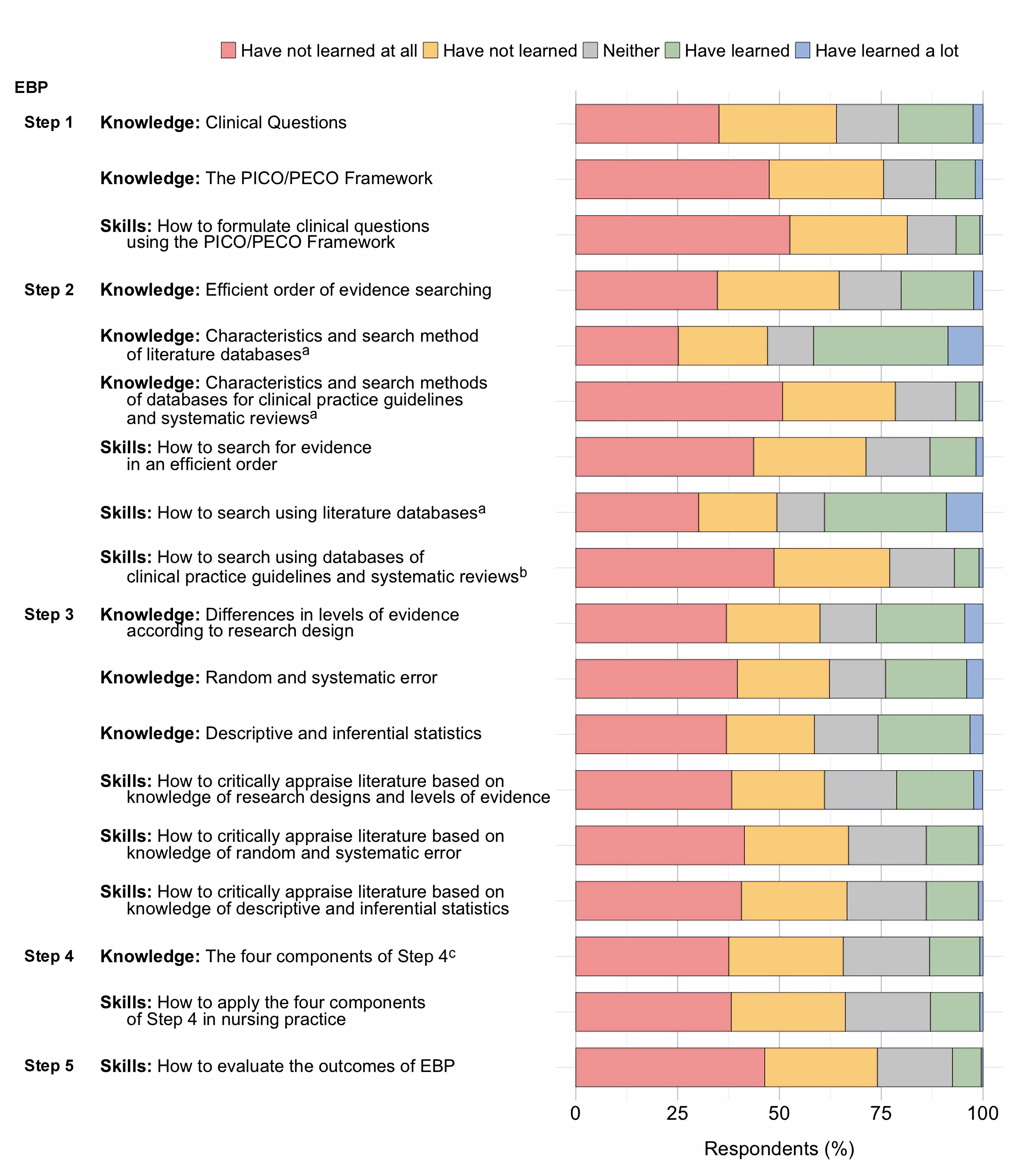
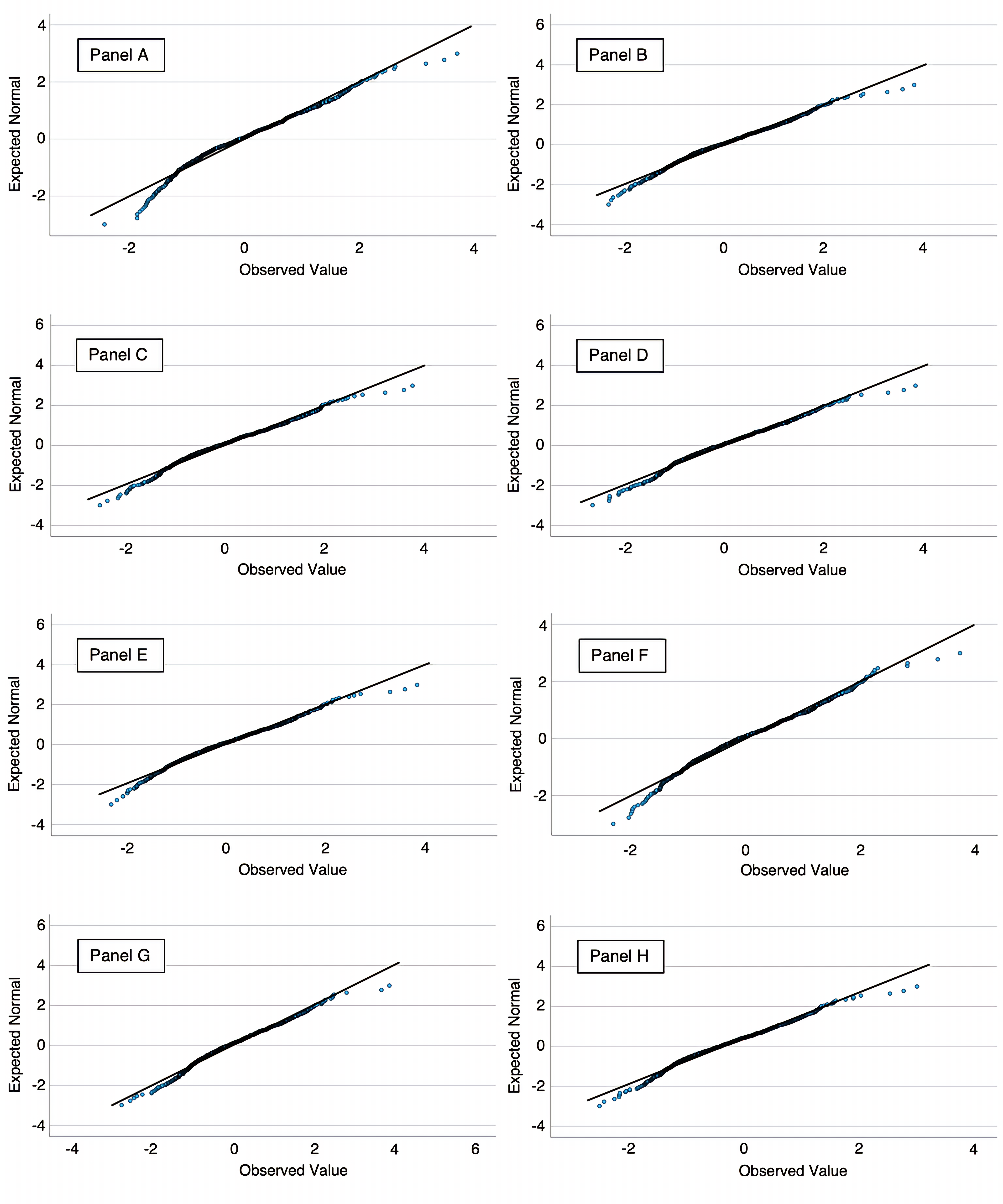
- Normality of continuous variables was assessed using the Shapiro–Wilk test, which indicated non-normal distribution (p < 0.05).
- Spearman’s Correlation Coefficient: Used to assess associations between leadership styles and outcome variables.
- Mann–Whitney U Test: Applied to compare differences in outcome variables between two independent groups
- Kruskal–Wallis H Test: Used to compare differences across three or more independent groups
- A p-value (p) < 0.05 was considered statistically significant.
Statistical Software
All analyses were performed using SPSS-26 (Statistical Package for the Social Sciences-26).
Ethical Approval and Informed Consent Statement
Informed consent was obtained from all study participants. The purpose, procedures, and voluntary nature of the study were explained through official internal communication channels via HMC e-mail. Participants provided electronic consent after having at least two months to review the study information before deciding to participate. Only registered nurses employed at Hamad Medical Corporation (HMC) who met the inclusion criteria were enrolled. No financial incentives were offered for participation.
The study was approved by the Medical Research Center (MRC) – Local Ethics Committee of Hamad Medical Corporation, Qatar (Protocol No. MRC-01-24-356),with approval granted on 15/08/2024, and was conducted in accordance with the principles of the Declaration of Helsinki and Good Clinical Practice (GCP), as well as the regulations of the Ministry of Public Health (MoPH), Qatar. Participant anonymity and data confidentiality were strictly maintained throughout the study.
RESULTS
Demographic and Professional Characteristics
The study sample (N=980) exhibits a predominant representation of females (72.14%), while males account for 27.86%. The sex ratio of 0.39 males per female (Table 1).
| Characteristics | Categories | Frequency (n) | Percent (%) | Mean± SD | Median (IQR) |
| Gender | Male | 273 | 27.86 | ||
| Female | 707 | 72.14 | |||
| Marital Status | Single | 138 | 14.08 | ||
| Married | 820 | 83.67 | |||
| Widowed | 8 | 0.82 | |||
| Separated / Divorced | 14 | 1.43 | |||
| Nationality | Cuban | 36 | 3.67 | ||
| Egyptian | 16 | 1.63 | |||
| Filipino | 332 | 33.88 | |||
| Indian | 413 | 42.14 | |||
| Iranian | 3 | 0.31 | |||
| Jordanian | 64 | 6.53 | |||
| Lebanese | 5 | 0.51 | |||
| Palestinian | 8 | 0.82 | |||
| Somali | 3 | 0.31 | |||
| Sudanese | 51 | 5.20 | |||
| Tunisian | 49 | 5.00 | |||
| Age (years) | ≤30 years | 64 | 6.53 |
40.40 ± 7.89 |
37 (35-46) |
| ]30-45] | 657 | 67.04 | |||
| > 45 | 259 | 26.43 |
Table 1. Demographic Characteristics (N=980)
The majority of participants are married (83.67%), with a smaller proportion being single (14.08%) or widowed (0.82%). In terms of nationality, the most represented groups are Indian (42.14%) and Filipino (33.88%), collectively comprising over 75% of the total sample, while other nationalities, such as Jordanian (6.53%), Sudanese (5.20%), and Tunisian (5.0%), are present in smaller proportions. Certain nationalities, including Iranian (0.31%) and Somali (0.31%), have minimal representation. The mean age of the participants is 40.40 ±7.89 years, with a minimum age of 26 years and a maximum age of 62 years. The majority belonging to the 30-45 age group (67.04%), followed by those over 45 years (26.43%), and only a small percentage ≤30 years (6.53%).
The professional characteristics of the study sample (N=980) reveal a workforce with diverse experience levels and educational backgrounds (Table 2). The mean years of experience as a nurse is 16.85 ± 7.14 years, ranging from 3 to 39 years. The majority have 5-15 years of experience (54.29%), followed by those with more than 15 years (43.57%), and a small proportion with ≤5 years (2.14%). Experience within Hamad Medical Corporation (HMC) follows a similar trend, with a mean of 9.93 ± 7.54 years, ranging from 1 to 36 years. The distribution shows that 36.73% have ≤5 years, 37.65% have 5-15 years, and 25.61% have over 15 years of experience in HMC.
Regarding education, the majority hold a Bachelor’s degree (76.63%), while 14.18% have a diploma, and 9.18% hold a Master’s degree or higher.
The participants are distributed across various hospitals, with the highest representation from Hamad General Hospital (27.55%), followed by Rumailah Hospital (11.63%), Al Wakra Hospital (11.43%), and Women’s Wellness and Research Center (8.16%). Other facilities, including specialty hospitals like the Communicable Disease Center (1.53%) and The Cuban Hospital (1.73%), have lower representation.
In terms of departmental distribution, the Surgical Department (35.51%) and Medical Department (30.20%) have the highest number of participants, followed by Critical Care/Emergency Services (22.45%) and Outpatient and Ambulatory Services (11.84%).
| Characteristics | Categories | Frequency (n) | Percent (%) | Mean± SD | Median (IQR) |
| Years of experience as a nurse | ≤5 years | 21 | 2.14 |
16.85 ± 7.14 |
15(12-22) |
| ]5-15] | 532 | 54.29 | |||
| > 15 | 427 | 43.57 | |||
| Years of experience in HMC | ≤5 years | 360 | 36.73 |
9.93 ± 7.54 |
7(4-17) |
| ]5-15] | 369 | 37.65 | |||
| > 15 | 251 | 25.61 | |||
| Educational background
|
Diploma | 139 | 14.18 | ||
| Bachelor’s degree | 751 | 76.63 | |||
| Master’s degree | 90 | 9.18 | |||
| Hospital
|
Hamad General Hospital | 270 | 27.55 | ||
| Ambulatory Care Center | 58 | 5.92 | |||
| Qatar Rehabilitation Institute | 17 | 1.73 | |||
| NCCCR | 19 | 1.94 | |||
| Mental Health Service | 48 | 4.90 | |||
| Communicable Disease Center | 15 | 1.53 | |||
| Al Khor Hospital | 72 | 7.35 | |||
| Rumailah Hospital | 114 | 11.63 | |||
| Al Wakra Hospital | 112 | 11.43 | |||
| Hazm Mebaireek General Hospital | 64 | 6.53 | |||
| Aisha Bint Hamad Al Attiyah Hospital | 63 | 6.43 | |||
| The Cuban Hospital | 17 | 1.73 | |||
| Women's Wellness and Research Center | 80 | 8.16 | |||
| Heart Hospital | 31 | 3.16 | |||
| Department
|
Critical Care / Emergency Services | 220 | 22.45 | ||
| Medical Department | 296 | 30.20 | |||
| Surgical Department | 348 | 35.51 | |||
| Outpatient (OPD) and Ambulatory Services | 116 | 11.84 |
Table 2. Professional Characteristics (N=980)
Nurse Manager Leadership Styles
The results indicate that transactional leadership (2.57±0.85) is more dominant than transformational leadership (2.20±1.05), suggesting that leaders in this sample primarily rely on structured management approaches, such as performance-based rewards (contingent reward, 2.56±1.05) and active monitoring (management by exception – active: 2.58±0.98), rather than fostering innovation, motivation, or individualized consideration (Table 3).
| Minimum | Maximum | Mean | S D | Median | Q1 | Q3 | |
| Idealized Attributes or Idealized Influence (Attributes) | 0.00 | 4.00 | 2.19 | 1.14 | 2.25 | 1.50 | 3.00 |
| Idealized Behaviors or Idealized Influence (Behaviors) | 0.00 | 4.00 | 2.35 | 1.15 | 2.50 | 1.75 | 3.25 |
| Inspirational Motivation | 0.00 | 4.00 | 2.34 | 1.22 | 2.50 | 1.50 | 3.25 |
| Intellectual Stimulation | 0.00 | 4.00 | 2.21 | 1.11 | 2.25 | 1.50 | 3.00 |
| Individual Consideration | 0.00 | 4.00 | 1.94 | 0.96 | 2.00 | 1.25 | 2.75 |
| Transformational | 0.00 | 4.00 | 2.20 | 1.05 | 2.35 | 1.55 | 3.00 |
| Contingent Reward | 0.00 | 4.00 | 2.56 | 1.05 | 2.75 | 2.00 | 3.25 |
| Mgmt by Exception (Active) | 0.00 | 4.00 | 2.58 | 0.98 | 2.75 | 2.00 | 3.25 |
| Transactional | 0.25 | 4.00 | 2.57 | 0.85 | 2.62 | 2.00 | 3.12 |
| Mgmt by Exception (Passive) | 0.00 | 4.00 | 1.55 | 1.01 | 1.25 | 0.75 | 2.25 |
| Laissez-Faire | 0.00 | 4.00 | 1.43 | 1.05 | 1.25 | 0.50 | 2.25 |
| Passive Avoidant | 0.00 | 4.00 | 1.49 | 0.97 | 1.37 | 0.75 | 2.12 |
| Extra Effort | 0.00 | 4.00 | 2.17 | 1.20 | 2.33 | 1.00 | 3.00 |
| Effectiveness | 0.00 | 4.00 | 2.25 | 1.22 | 2.50 | 1.00 | 3.00 |
| Satisfaction | 0.00 | 4.00 | 2.28 | 1.31 | 2.50 | 1.00 | 3.00 |
| Outcomes of Leadership | 0.00 | 400 | 2.23 | 1.20 | 2.42 | 1.05 | 3.16 |
Table 3. Nurse Manager Leadership Styles
Within transformational leadership, the highest subscale is idealized influence behaviors (2.35±1.15), indicating that some leaders demonstrate strong role-modeling behaviors. However, individual consideration (1.94±0.96) is the lowest, suggesting that leaders may not provide enough mentorship or personalized support to the nurses.
The passive-avoidant leadership style (1.49±0.97) has the lowest overall scores, particularly laissez-faire leadership (1.43±1.05), indicating that leaders in this sample are generally engaged and do not frequently avoid decision-making. However, the management by exception – passive score (1.55±1.01) suggests that some leaders may still wait until problems arise before taking corrective action.
Regarding leadership outcomes, the scores for effectiveness (2.25±1.22) and satisfaction (2.28±1.31) indicate moderate levels of perceived leader effectiveness and staff satisfaction. Overall outcomes of leadership (2.23±1.20) reflect a tendency towards average performance across the sample, with some variability.
Nurses' Job Performance
The results of the Nursing Performance Instrument (NPI) and its three subscales reveal interesting insights into the nursing workforce’s performance (Table 4).
| Minimum | Maximum | Mean | SD | Median | Q1 | Q3 | |
| Physical / mental decrement | 1.00 | 6.00 | 2.91 | 1.11 | 3.00 | 2.00 | 3.66 |
| Consistent practice | 1.00 | 6.00 | 4.73 | 1.29 | 5.00 | 4.25 | 5.75 |
| Behavioral change | 1.00 | 6.00 | 3.61 | 1.33 | 3.50 | 3.00 | 4.50 |
| Nursing Performance Instrument (NPI) | 1.00 | 5.78 | 3.88 | 0.94 | 3.88 | 3.44 | 4.44 |
Table 4. Nurses' Job Performance
The subscale "Physical/Mental Decrement" had a mean score of 2.91±1.11, suggesting that nurses report a moderate level of physical and mental strain, though it is not perceived as a severe issue overall. The "Consistent Practice" subscale scored the highest, with a mean of 4.73±1.29, indicating that nurses generally perceive themselves as maintaining consistent and stable practices in their roles. The "Behavioral Change" subscale, with a mean of 3.61±1.33, suggests that there is moderate evidence of behavioral changes in nursing practice. Lastly, the overall NPI score of 3.88±0.94 indicates a generally positive view of nursing performance, reflecting a moderate level overall.
Comparison of Socio-demographic Characteristics and Their Association with Nurses' Job Performance
Female nurses had significantly higher job performance than male nurses (mean rank: 536.67 vs. 370.92, p < 0.001) (Table 5).
| Characteristics | Categories | Mean Rank | Test | p-value (test) |
| Gender
|
Male | 370,92 | 63861,5 | < 0.001 (MW)*
|
| Female
|
536,67 | |||
| Marital Status | Single | 551.12 |
9.513
|
0.009 (KW)*
|
| Married | 472.37 | |||
| Widowed | 457.50 | |||
| Nationality | Cuban | 268.22 | 150.584
|
< 0.001 (KW)*
|
| Egyptian | 389.00 | |||
| Filipino | 576.75 | |||
| Indian | 498.81 | |||
| Iranian | 715.83 | |||
| Jordanian | 298.00 | |||
| Lebanese | 717.70 | |||
| Palestinian | 754.00 | |||
| Somali | 649.17 | |||
| Sudanese | 486.15 | |||
| Tunisian | 198.83 | |||
| Age (years) | ≤30 years | 568.97 | 29.617
|
< 0.001 (KW)*
|
| ]30-45] | 456.10 | |||
| > 45 | 558.38 | |||
| Years of experience as a nurse
|
≤5 years | 509.26 | 1.273
|
0.529 (KW)*
|
| ]5-15] | 481.21 | |||
| > 15 | 501.15 | |||
| Years of experience in HMC
|
≤5 years | 472.97 | 0.003 | 11.533 (KW)* |
| ]5-15] | 472.07 | |||
| > 15 | 542.74 | |||
| Educational background | Diploma | 425.49 | 9.391
|
0.009 (KW)*
|
| Bachelor’s degree | 498.19 | |||
| Master’s degree | 526.72 | |||
| Hospital | Hamad General Hospital | 527.88 | 61.003 | < 0.001(KW)* |
| Al Khor Hospital | 375.75 | |||
| Rumailah Hospital | 428.29 | |||
| Al Wakra Hospital | 458.57 | |||
| Hazm Mebaireek General Hospital | 500.56 | |||
| Aisha Bint Hamad Al Attiyah Hospital | 462.40 | |||
| The Cuban Hospital | 263.56 | |||
| Women's Wellness and Research Center | 481.40 | |||
| Heart Hospital | 607.08 | |||
| Ambulatory Care Center | 531.40 | |||
| Qatar Rehabilitation Institute | 583.32 | |||
| NCCCR | 683.03 | |||
| Mental Health Service | 493.17 | |||
| Communicable Disease Center | 703.83 | |||
| Department | Critical Care / Emergency Services | 492.86 | 43.713 | < 0.001(KW)* |
| Medical Department | 488.47 | |||
| Surgical Department | 440.61 | |||
| Outpatient (OPD) and Ambulatory Services | 640.84 |
Note: MW = Mann–Whitney U test; KW = Kruskal–Wallis H test; *p < 0.05 indicates statistical significance.
Table 5. Comparison of Socio-demographic Characteristics and Their Association with Nurses' Job Performance.
Single nurses reported the highest performance, followed by married and widowed nurses (551.12 vs. 472.37 vs. 457.50, p = 0.009). Significant differences were observed across nationalities, with Palestinian nurses showing the highest performance and Tunisian nurses the lowest (754.00 vs. 198.83, p < 0.001).
Regarding age, nurses aged ≤30 years had the highest performance, followed by those >45 years and those aged 30–45 years (568.97 vs. 558.38 vs. 456.10, p < 0.001). Years of experience as a nurse were not significantly associated with performance, although nurses with ≤5 years of experience had higher performance than those with >15 years or 5–15 years (509.26 vs. 501.15 vs. 481.21, p = 0.529).
Years of experience at HMC were significantly associated with performance, with nurses having >15 years of experience showing the highest performance and those with 5–15 years the lowest (542.74 vs. 472.07, p = 0.003). Educational background influenced performance, with nurses holding a Master’s degree reporting the highest and those with a diploma the lowest (526.72 vs. 425.49, p = 0.009).
Job performance differed significantly across hospitals, with the Mental Health Service reporting the highest and ABAH the lowest performance (703.83 vs. 263.56, p < 0.001). Finally, departmental differences were significant, with the Surgical Department showing the highest performance and the Medical Department the lowest (640.84 vs. 440.61, p < 0.001).
Correlation between Nurse Manager Leadership Styles and Nurses’ Performance
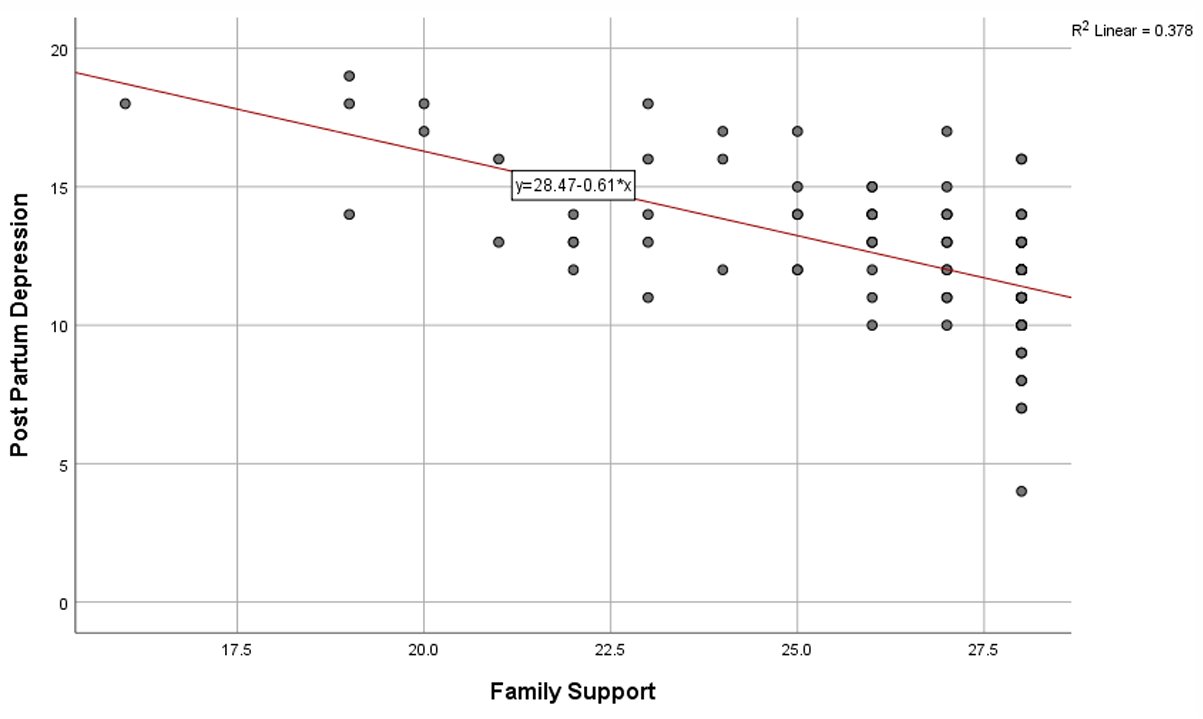
Table 6 explores the relationships between leadership styles and various aspects of nursing performance, including physical/mental decrement, consistent practice, behavioral change, and overall performance measured by the Nursing Performance Instrument (NPI).
Transformational leadership shows a moderate positive correlation with consistent practice (rho = 0.323, p <0.001) and a weak positive correlation with nursing performance (rho = 0.146, p < 0.001). However, there are no significant relationships with physical/mental decrement (rho = 0.017, p = 0.597) or behavioral change (rho = 0.022, p = 0.489). These results suggest that transformational leadership encourages consistent practice and slightly enhances overall performance but does not appear to directly influence nurses' physical or mental well-being or their immediate behavioral adjustments.
|
|
Physical/mental decrement | Consistent practice | Behavioral change | Nursing Performance Instrument (NPI) | |
| Transformational
|
Spearman Coefficient | 0.017 | 0.323 | 0.022 | 0.146 |
| p-value | 0.597 | < 0.001 | 0.489 | <0.001 | |
| Transactional
|
Spearman Coefficient | -0.277 | -0.055 | -0.339 | -0.230 |
| p-value | < 0.001 | 0.083 | < 0.001 | < 0.001 | |
| Passive Avoidant
|
Spearman Coefficient | 0.038 | -0.073 | -0.087 | -0.121 |
| p-value | 0.233 | 0.022 | 0.006 | < 0.001 | |
Table 6. Correlation between Nurse Manager Leadership Styles and Nurses’ Performance.
Transactional leadership presents a negative correlation with physical/mental decrement (rho = -0.277, p < 0.001), behavioral change (rho = -0.339, p < 0.001), and nursing performance (rho = -0.230, p < 0.001). The correlation with consistent practice is not significant (rho = -0.055, p = 0.083). These findings imply that transactional leadership may be associated with declines in behavioral adaptability and overall performance, potentially reflecting a rigid, reward-punishment dynamic that does not foster flexibility or proactive nursing behaviors.
Passive-avoidant leadership demonstrates weak negative correlations with consistent practice (rho = -0.073, p = 0.022), behavioral change (rho = -0.087, p = 0.006), and nursing performance (rho = -0.121, p < 0.001), though no significant relationship is found with physical/mental decrement (rho = 0.038, p = 0.233). This suggests that passive-avoidant leadership slightly undermines effective nursing practices and performance, likely due to a lack of guidance and support.
In summary, transformational leadership has the most positive influence, especially on consistent practice and overall nursing performance. In contrast, transactional leadership seems linked to negative outcomes, particularly regarding behavioral flexibility and performance, while passive-avoidant leadership also has small but significant negative effects.
DISCUSSION
Demographic and Professional Characteristics
The demographic characteristics of the sample provide important context for interpreting job performance outcomes. The high representation of women (72.14%) is consistent with the global nursing workforce [23,24], though the smaller proportion of men (27.86%) may affect team diversity and performance styles [25]. The predominance of married nurses (83.67%) suggests stability, yet also underscores the dual stressors of family and professional responsibilities, which can affect concentration and efficiency [26,27]. The reliance on expatriate staff, especially Indian (42.14%) and Filipino (33.88%) nurses, reflects regional workforce trends but introduces cultural adaptation challenges that may shape performance consistency [28]. The average age (40.40 years) and extensive experience (16.85±7.14 years) demonstrate a mature workforce capable of sustaining performance. However, the limited presence of younger nurses (≤5 years’ experience, 2.14%) may hinder succession planning and innovation. The predominance of bachelor’s degrees (76.63%) indicates solid educational preparation, though the limited advanced degrees (9.18%) highlight opportunities to strengthen specialized competencies.
Nurse Manager Leadership Styles
Leadership findings confirmed transactional leadership (2.57±085) as the dominant style, with contingent rewards (2.56±1.05) and active monitoring (2.58±0.98) driving structured compliance. While these strategies ensure adherence to standards, they may not stimulate the innovation and adaptability increasingly demanded in modern healthcare settings [15,18]. The low emphasis on individual consideration (1.94±0.96) suggests a lack of personalized development, limiting opportunities for performance growth [8]. By contrast, transformational leadership has been consistently linked to enhanced job performance across diverse contexts [14,16]. Although passive-avoidant leadership (1.49±0.97) was rare, its occasional presence risks undermining performance through delayed intervention. These results suggest that adopting transformational leadership at HMC could strengthen consistency, adaptability, and clinical performance.
Nurses' Job Performance
The high consistent practice scores (4.73±1.29) highlight nurses’ reliability in adhering to established protocols, a strength in error-prone healthcare settings. However, moderate behavioral change (3.61±1.33) signals resistance to adapting workflows, possibly due to rigid transactional leadership or fear of reprisal for deviations. The overall performance score (NPI = 3.88) suggests competence but not excellence, aligning with environments prioritizing compliance over innovation. Notably, physical/mental decrement (2.91±1.11) indicates that strain, while not severe, may hinder proactive initiatives. In a similar context in Iran, nurse performance was also reported at a moderate level, with the general performance aspect receiving the highest average score and the mental aspect the lowest [29].
Comparison of Socio-demographic Characteristics and Their Association with Nurses' Job Performance
Job performance varied markedly across demographics. Females outperformed males (p < 0.001), aligning with a study conducted in the same context in Jordan, a Middle Eastern country, which linked female nurses to higher job performance [30]. This gender gap may reflect both enduring social norms around caring roles and targeted soft-skills training that disproportionately benefits female practitioners.
Single nurses showed higher performance (mean rank = 551.12) than married or widowed peers, possibly due to fewer familial responsibilities or greater focus on career progression. This contrasts with studies conducted in Jordan and Turkey, which found no significant relationship between marital status and job performance [30,31]. Nationality-based differences were stark: Palestinian nurses (mean rank = 754.00) excelled, while Tunisians (mean rank = 198.83) underperformed. This may reflect disparities in training quality, language proficiency, or workplace integration. Younger nurses (≤30 years) outperformed older colleagues (p < 0.001), suggesting adaptability to new protocols or technologies. Paradoxically, nurses with >15 years of HMC experience also performed well, indicating that institutional knowledge complements innovation. In the same context, a study conducted in Jordan found that age and experience were related to job performance [30].
Master’s-trained nurses (mean rank = 526.72) outperformed diploma holders, underscoring the value of advanced education in clinical decision-making. Hospitals like the Mental Health Service (mean rank = 703.83). Surgical departments (mean rank = 640.84) reported superior performance, likely due to specialized workflows or interdisciplinary collaboration. These findings advocate for competency-based training and equitable recognition of diverse backgrounds.
Correlation between Nurse Manager Leadership Styles and Nurses’ Job Performance
Transformational leadership moderately enhanced consistent practice (rho = 0.323, p < 0.001) but had no impact on behavioral change, suggesting it fosters reliability over innovation. The findings partially align with those reported by Mohammed Qtait on 2023, who conducted a systematic review of 12 quantitative studies investigating the relationship between leadership styles and nurse performance, reports that transformational leadership had the strongest positive correlation enhancing nursing care quality, job satisfaction, motivation, and patient outcomes [8].
Transactional leadership correlated negatively with performance (rho = -0.230, p < 0.001), particularly behavioral change (rho = -0.339, p < 0.001), implying rigid reward-punishment systems hinder adaptability. However, Qtait’s review found a moderate positive correlation between transactional leadership and nurse performance, indicating some benefits under structured systems [8].
Passive-avoidant leadership also undermined performance (rho = -0.121, p < 0.001), in line with Qtait’s conclusion that laissez-faire leadership had weak or no positive impact [8]. This consistent finding emphasizes that ambiguity, lack of guidance, and disengagement by leaders can significantly reduce nurse motivation and clarity in roles.
Recommendations
The findings of this study highlight the critical need to strengthen transformational leadership competencies among nurse managers at Hamad Medical Corporation (HMC). It is recommended that HMC invest in ongoing leadership development programs that emphasize communication, motivation, and professional empowerment to promote inspiring and participative managerial behaviors. Transformational leadership, by encouraging autonomy and creativity, can significantly enhance both individual and collective nursing performance, fostering consistency in clinical practice and adaptability in complex healthcare settings.
Furthermore, leadership competency assessments should be integrated into managerial performance evaluations to ensure that adopted leadership styles align with organizational goals and contribute to nurse productivity and job satisfaction. Organizational culture should also move toward reducing overreliance on transactional leadership, which focuses primarily on control and rewards, and instead foster more collaborative, innovative, and supportive leadership approaches.
Finally, creating a psychologically and physically supportive work environment is essential to reduce stress and fatigue among nurses, both of which can negatively affect long-term job performance
Strengths and limitations of the study
This study possesses several methodological strengths that enhance its scientific credibility. First, the use of a large and randomly selected sample (N = 980) provides strong representativeness and statistical reliability. The application of validated international instruments, namely the Multifactor Leadership Questionnaire (MLQ-5X) for assessing leadership styles and the Nursing Performance Instrument (NPI) for measuring clinical performance, adds to the study’s methodological rigor. Moreover, the use of robust statistical analyses including Spearman’s correlation, Mann–Whitney U, and Kruskal–Wallis H tests enabled comprehensive exploration of relationships between leadership styles and various aspects of job performance, providing a multidimensional understanding of these dynamics. Despite its strengths, the study also presents certain limitations. The most significant is its cross-sectional design, which limits the ability to infer causality between leadership style and nurse performance. It remains unclear whether transformational leadership directly improves performance, or whether nurses who perform better perceive their leaders as more transformational. Additionally, self-reported data may have introduced response bias, as participants could overestimate their performance due to social desirability or professional pride. Studies would provide a broader and more causal understanding of these leadership–performance relationships.
CONCLUSION
This study clearly demonstrates that nurse manager leadership styles have a significant and differentiated impact on nurses’ job performance within Hamad Medical Corporation. The results reveal that transformational leadership exerts the most substantial positive effect, enhancing consistency in clinical practice, adaptability to change, and overall professional performance. Nurses who perceive their leaders as visionary, supportive, and encouraging are more motivated, committed, and productive. These findings align with international literature showing that transformational leaders foster collaboration, reduce clinical errors, and improve both patient outcomes and staff well-being. In contrast, transactional leadership, while effective in maintaining compliance and operational discipline, tends to have limited influence on creativity and long-term professional growth. Its focus on control and reward systems may sustain performance in routine tasks but fails to nurture the initiative and innovation required in dynamic healthcare environments. On the other hand, passive-avoidant leadership emerges as the least effective style, being associated with disorganization, lack of motivation, and decreased performance due to minimal managerial involvement or guidance.
The implications for nursing leadership are profound. Developing a structured and culturally adaptive transformational leadership model should be a strategic priority for HMC. Such an approach can strengthen clinical performance, enhance innovation, reduce turnover, and promote a collaborative culture focused on quality and patient safety. Ultimately, this study underscores that effective leadership in nursing transcends task management it is fundamentally about mobilizing human potential to achieve excellence, empowerment, and resilience within healthcare organizations.
Local Ethics Committee approval
The study was approved by the Medical Research Center (MRC) – Local Ethics Committee of Hamad Medical Corporation, Qatar (Protocol No. MRC-01-24-356) and was conducted in accordance with the principles of the Declaration of Helsinki and Good Clinical Practice (GCP), as well as the regulations of the Ministry of Public Health (MoPH), Qatar. Participant anonymity and data confidentiality were strictly maintained throughout the study.
Conflicts of interest
This study was conducted in accordance with ethical standards. All participants provided informed consent. The authors declare no conflict of interest.
Sources of funding
This research received funding from the Medical Research Center at HMC.The authors thank the
Author contributions
Conception and design: Abdelbasset Ghalgaoui
Data collection: Abdelbasset Ghalgaoui
Data analysis and interpretation: Abdelbasset Ghalgaoui, Osama Helmi Mohammad Subih, Maha Mohamed Marzouk Ahmed, Mehdi Halleb, Nabil Ajjel.
Drafting of the manuscript: all authors.
Critical revision of the manuscript: Abdelbasset Ghalgaoui, Mehdi Halleb
Final approval: all authors
Acknowledgements
The authors thank the staff of Hamad Medical Corporation for their collaboration.
REFERENCES
- DeLucia PR, Ott TE, Palmieri PA. Performance in Nursing. Reviews of Human Factors and Ergonomics. SAGE Publications; 2009;5:1–40. https://doi.org/10.1518/155723409X448008
- El-Gazar HE, Zoromba MA. Nursing Human Resource Practices and Hospitals’ Performance Excellence: The Mediating Role of Nurses’ Performance. Acta Biomed. 2021;92:e2021022. https://doi.org/10.23750/abm.v92iS2.11247
- Gurses AP, Carayon P, Wall M. Impact of Performance Obstacles on Intensive Care Nurses’ Workload, Perceived Quality and Safety of Care, and Quality of Working Life. Health Services Research. 2009;44:422–43. https://doi.org/10.1111/j.1475-6773.2008.00934.x
- Shahnavazi A, Bouraghi H, Eshkiki MF, Shahnavazi H. The Effect of Perceived Organizational Climate on the Performance of Nurses in Private Hospitals [Internet]. Journal of Clinical Research in Paramedical Sciences. Brieflands; 2021 Dec. https://doi.org/10.5812/jcrps.108532
- Bae JY, Bae SH. The Effect of Clinical Nurses’ Critical Thinking Disposition and Communication Ability on Patient Safety Competency. J Korean Acad Fundam Nurs. Korean Academy of Fundamentals of Nursing; 2022;29:159–69. https://doi.org/10.7739/jkafn.2022.29.2.159
- Saputri CA. The Role of Nursing Interventions in Patient Satisfaction and Outcomes. AHR. 2023;1:75–87. https://doi.org/10.60079/ahr.v1i2.359
- Wieke Noviyanti L, Ahsan A, Sudartya TS. Exploring the Relationship between Nurses’ Communication Satisfaction and Patient Safety Culture. Journal of Public Health Research. SAGE Publications; 2021;10:jphr.2021.2225. https://doi.org/10.4081/jphr.2021.2225
- Qtait M. Systematic Review of Head Nurse Leadership Style and Nurse Performance. International Journal of Africa Nursing Sciences. 2023;18:100564. https://doi.org/10.1016/j.ijans.2023.100564
- Alrabadi N, Shawagfeh S, Haddad R, Mukattash T, Abuhammad S, Al-rabadi D, et al. Medication errors: a focus on nursing practice. J Pharm Health Serv Res. 2021;12:78–86. https://doi.org/10.1093/jphsr/rmaa025
- Asante BL, Zúñiga F, Favez L. Quality of care is what we make of it: a qualitative study of managers’ perspectives on quality of care in high-performing nursing homes. BMC Health Serv Res. 2021;21:1090. https://doi.org/10.1186/s12913-021-07113-9
- Christopher-Dwyer K, Scanlon KG, Crimlisk JT. Critical Care Resource Nurse Team: A Patient Safety and Quality Outcomes Model. Dimensions of Critical Care Nursing. 2022;41:46. https://doi.org/10.1097/DCC.0000000000000501
- Howell EA, Sofaer S, Balbierz A, Kheyfets A, Glazer KB, Zeitlin J. Distinguishing High-Performing From Low-Performing Hospitals for Severe Maternal Morbidity: A Focus on Quality and Equity. Obstet Gynecol. 2022;139:1061–9. https://doi.org/10.1097/AOG.0000000000004806
- Bass BM, Riggio RE. Transformational Leadership. Psychology Press; 2006.
- Hasan AA, Ahmad SZ, Osman A. Transformational leadership and work engagement as mediators on nurses’ job performance in healthcare clinics: work environment as a moderator. Leadersh Health Serv (Bradf Engl). 2023;36:537–61. https://doi.org/10.1108/LHS-10-2022-0097
- Wang H-F, Chen Y-C, Yang F-H, Juan C-W. Relationship between transformational leadership and nurses’ job performance: The mediating effect of psychological safety. Social Behavior and Personality: an international journal. 2021;49:1–12. https://doi.org/10.2224/sbp.9712
- Wijayanti K, Aini Q. The Influence of Transformational Leadership Style to Nurse Job Satisfaction and Performance in Hospital. Journal of World Science. 2022;1:485–99. https://doi.org/10.58344/jws.v1i7.69
- Al-Rjoub S, Alsharawneh A, Alhawajreh MJ, Othman EH. Exploring the Impact of Transformational and Transactional Style of Leadership on Nursing Care Performance and Patient Outcomes. Journal of Healthcare Leadership. Dove Medical Press; 2024;16:557–68. https://doi.org/10.2147/JHL.S496266
- Mekonnen M, Bayissa Z. The Effect of Transformational and Transactional Leadership Styles on Organizational Readiness for Change Among Health Professionals. SAGE Open Nursing. SAGE Publications Inc; 2023;9:23779608231185923. https://doi.org/10.1177/23779608231185923
- Suwarno B. Analysis Head Nurses’ Leadership Styles to Staff Inpatient Nurses’ Job Performance in Hospital. International Journal of Science, Technology & Management. 2023;4:317–26. https://doi.org/10.46729/ijstm.v4i2.770
- Abujaber AA, Nashwan AJ, Santos MD, Al-Lobaney NF, Mathew RG, Alikutty JP, et al. Bridging the generational gap between nurses and nurse managers: a qualitative study from Qatar. BMC Nurs. 2024;23:623. https://doi.org/10.1186/s12912-024-02296-y
- Avolio BJ, Bass BM. Multifactor leadership questionnaire: manual and sample set. Third edition. Place of publication not identified: Mind Garden, Inc.; 2004.
- Sagherian K, Steege LM, Geiger-Brown J, Harrington D. The Nursing Performance Instrument: Exploratory and Confirmatory Factor Analyses in Registered Nurses. J Nurs Res. 2018;26:130–7. https://doi.org/10.1097/jnr.0000000000000215
- Kharazmi E, Bordbar N, Bordbar S. Distribution of nursing workforce in the world using Gini coefficient. BMC Nursing. 2023;22:151. https://doi.org/10.1186/s12912-023-01313-w
- State of the world’s nursing report 2025 [Internet]. 2025 [cited 2025 Sept 22]. https://www.who.int/publications/i/item/9789240110236. Accessed 22 Sept 2025
- Shen J, Guo Y, Chen X, Tong L, Lei G, Zhang X. Male nurses’ work performance: A cross sectional study. 2022;101:e29977. https://doi.org/10.1097/MD.0000000000029977
- Al-Hasnawi AA, Aljebory MKA. Relationship between nurses’ performance and their demographic characteristics. Journal Port Science Research. 2023;6:11–5. https://doi.org/10.36371/port.2023.1.3
- Hwang E, Yu Y. Effect of Sleep Quality and Depression on Married Female Nurses’ Work–Family Conflict. International Journal of Environmental Research and Public Health. Multidisciplinary Digital Publishing Institute; 2021;18:7838. https://doi.org/10.3390/ijerph18157838
- Turjuman F, Alilyyani B. Emotional Intelligence among Nurses and Its Relationship with Their Performance and Work Engagement: A Cross-Sectional Study. Alamri M, editor. Journal of Nursing Management. 2023;2023:1–8. https://doi.org/10.1155/2023/5543299
- Niri M al-SM, Khademian Z, Rivaz M. Nurses’ Performance as a Mediator Between Nurses’ Fatigue and Patient Safety Culture: A Structural Equation Model Analysis. Nursing Open. 2025;12:e70168. https://doi.org/10.1002/nop2.70168
- Al-Harazneh R, Abu shosha GM, Al-Oweidat IA, Nashwan AJ. The influence of job security on job performance among Jordanian nurses. International Journal of Africa Nursing Sciences. 2024;20:100681. https://doi.org/10.1016/j.ijans.2024.100681
- Ari HO. Determining the Relationship Between Work Stress and Job Performance: A Cross-Sectional Study Among Healthcare Workers. Journal of Nursing Management. 2025;2025:5051149. https://doi.org/10.1155/jonm/5051149
![]() This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
SELF-CARE KNOWLEDGE, BEHAVIORAL PRACTICES, AND PREVENTIVE STRATEGIES FOR DIABETIC FOOT ULCERS AMONG INDIVIDUALS WITH DIABETES IN TERTIARY HOSPITALS IN NIGERIA: A CROSS-SECTIONAL STUDY
Oseni Rukayat Ejide ¹, Emmanson Emmanson ²*, Kolawole Ifeoluwapo ¹,
Adejumo Prisca1, Obilor Helen3
- Department of Nursing Sciences, University of Ibadan, Nigeria
- Department of Human Anatomy, University of Cross River State, Nigeria
- School of Nursing, Queen’s University, Kingston, Ontario, Canada
* Corresponding Author: Emmanson Emmanson, Department of Human Anatomy, University of Cross River State, Nigeria. Email: emmansonemmanson35@gmail.com. ORCID: https://orcid.org/0009-0006-7285-7574
Cite this article
ABSTRACT
Introduction: The increasing prevalence of diabetes is a global public health concern, with foot ulcer prevention techniques, low self-care knowledge, and a lack of confidence contributing to complications like foot ulcers.
Methods: This cross-sectional study, conducted between January and December 2022, evaluated foot self-care knowledge, self-efficacy, and self-care behaviors among individuals with diabetes attending public tertiary hospitals in Abeokuta, Nigeria. Data from randomly selected 120 out-patients was collected using a multidimensional questionnaire, and multiple regression analysis was used to assess associations between variables.
Results: It was found that participants’ mean age was 44.8±14.65 years. Majority (58.3%) of them did not attend foot self-care education classes and had received a type-2 diabetes diagnosis within the previous 24 months. Many of the patients had low knowledge of foot self-care (55%), low self-care efficacy (55%) and poor self-care behavior (55%). Poor self-care behavior was predicted by low efficaciousness (p<0.0001) and low knowledge of foot self-care (p<0.0001).
Conclusion: The study concluded that the extent of knowledge significantly influenced self-care behaviors and the efficacy of foot self-care in averting diabetic foot ulcers. Improving these behaviors requires teaching appropriate knowledge through hands-on self-care treatments and gaining support from policymakers for its sustainability.
Keywords: Diabetes Foot Ulcer, Self-Care Knowledge, Efficacy, Behavior, Confidence.
INTRODUCTION
With an increasing prevalence, diabetes mellitus has become a global public health concern [1]. It raises mortality, illness, and medical expenses [1,2]. There are 537 million adults (20–79 years old) worldwide with diabetes as reported by International Diabetes Federation (IDF) [1]. Conversely, by 2060, the incidence of diabetes is expected to increase to 700% for type II and 65% for type I, according to the Centers for Disease Control and Prevention [3]. Additionally, diabetes is thought to be the cause of 6.7 million fatalities annually [1], with 1.5 million of those deaths occurring primarily in low- and middle-income nations [4].
According to IDF data from 2021, 1 in 22 adult Africans has diabetes, and 54% of Africans have diabetes but have not been diagnosed [1]. In Nigeria, the prevalence of diabetes rose from 2.2% in 1997 to over 6% in 2015, a more than 100% increase, according to World Health Organization (WHO) [5]. The IDF stated that the sub-Saharan region had the greatest estimated prevalence of diabetes, at 3,623,500 (3.7%). The prevalence rates of diabetic foot ulcers (DFU) in Nigeria vary from 11% to 32%, according to Ugwu et al. [6]. The rising rate of diabetes in Nigeria has been mostly linked to demographic shifts, including urbanization, the adoption of unsafe habits, poor diets that include sugar-sweetened beverages, inactivity, and dangerous alcohol and tobacco use [5,6]. This has also led to complications such as diabetic foot ulcers. This necessitates investigating the level of knowledge of people with diabetes mellitus (PWDM) on foot ulcer preventive self-care activities in selected hospitals in Abeokuta.
Millions of individuals worldwide are impacted by the dangerous side effect of diabetes called diabetic foot ulcers. It is lethal and can cause gangrene, infection, ischemia problems, neuropathy, macrovascular disease, and microvascular damage. According to Robles et al. [7], DFU is a challenging, expensive, and chronic health problem that increases morbidity and death. According to Oliver and Mutlouglu [8], ulcers are typically persistent and can occur in inpatient as well as outpatient environments. An array of variables, such as male gender, diabetes for over a decade, the advanced age of the patients, obesity, dry skin, insufficient circulation, underpinning nerve damage, callus formation, foot defects, improper foot hygiene, and poorly fitting shoes, are linked to the development of DFU, according to Khan, Khan, & Farooqui [9] and Oliver & Mutlouglu, [8]. Despite being controllable through education, it is the most costly and fatal event related with lower extremity amputation (LEA) and frequently associated with high morbidity and death [6]. Families and societies are consequently forced to bear a greater financial burden [10,11]. Other adverse effects include poor quality-of-life [12, 13]. In light of these burdens, it is important to assess how confident PWDM are in their ability to avoid foot ulcers in the selected hospitals. Therefore, this study assumes there is no significant association between efficacy and behavior of PWDM.
According to Sari et al. [14], poor foot self-care is the main factor contributing to DFU, while appropriate foot self-care can cut the risk of DFU, hospital stays, and amputations by 50%. Client-focused education on self-efficacy in FSC practices should be promoted in a time- and cost-effective manner, as continuous physician supervision is not always possible [15]. For this reason, Adeyemi et al. [16] proposed that appropriate foot care methods and patient education can avoid or lower the risk for DFU in the interim. Previous studies [9,14,17,18] revealed low to moderate foot care practice, inadequate understanding of DFU, and attitudes toward foot care prevention. People with diabetes mellitus in Sub-Saharan Africa also showed fair but insufficient awareness of diabetic foot care [19]; this is comparable to what is available in other parts of the world. Research on effective FSC behavior is still limited, and incidence of DFU, limb loss, and DFU-related premature death have increased in Nigeria. Similar to what was found by Ojewale, Okoye, and Ani [20], their study on FSC behavior and self-efficacy among PWDM in the University College Hospital, Nigeria, revealed a scarcity of investigations. Consequently, research on PWDM self-care knowledge, efficacy, and behavior is crucial. It is therefore important to explore the foot self-care behavior of PWDM in selected hospitals. In line with this, the study tested the hypothesis that there is no significant association between age, gender, educational status and behavior of FSC among PWDM, and that there is no significant association between knowledge of FSC and the behavior of PWDM. Thus, with the goal to prevent foot ulcers, this study assessed PWDM's self-care knowledge, efficacy, and behavior.
MATERIALS AND METHODS
Study design
This is a cross-sectional descriptive study which assessed the FSC knowledge, self-care efficacy and behavior of PWDM toward DFU prevention in Federal Medical Hospital (FMC), and State Hospital, Ijaiye, Abeokuta, Nigeria, between January and December 2022.
Target population
This included PWDM (type 1 and 2) in the selected hospitals.
Study population
PWDM who attended outpatient clinics, who were estimated to be 200 monthly in FMC, and 120 monthly in the State Hospital, Ijaiye, Abeokuta, respectively.
Inclusion criteria
Adult PWDM male and female aged 18 years and above managed for at least three months, that attended OPD clinic of FMC and State Hospital, Ijaiye, Abeokuta and gave consent to participate were included in the study.
Exclusion criteria
PWDM with existing DFU, those critically ill, and those on admission were excluded from the study.
Sample size estimation
The minimum sample size was determined using Cochran’s formula for estimating proportions in large populations:
where:
n0 = initial sample size, Z = standard normal deviation at 95% confidence (1.96), p = estimated proportion of the population with the attribute, q = 1 – p, e = desired margin of error.
Since no prior prevalence estimate of foot-care knowledge among individuals with diabetes in Abeokuta was available, the study used p = 50%. This value is conventionally used when there is insufficient prior data, as it maximizes sample size and increases precision. The margin of error was set at e = 10%. Based on previous values the estimated sample size is:
Additionally, a 20% attrition rate (AR) was included:
![]()
Thus, the final sample size used in this study was 120. Particularly, we adopted a relatively large margin of error (e=10%) and an attrition rate of 20%, as this is an explorative study.
Sampling technique
Two out of the three hospitals in Abeokuta; Federal Medical Center, Abeokuta and State Hospital, Ijaiye were selected using random sampling technique. A total of 120 participants were later recruited from the 2 hospitals.
Instrument for data collection
Data was obtained from respondents using structured and validated questionnaires, the questionnaire was in three sections. Section A addressed demographic data and knowledge of FSC. Section B assessed FSC behavior activities using a validated 26-item self-report tool adapted form of Nottingham Assessment of Functional Foot-care (NAFFS) [21]. While section C addressed the question on foot care efficacy using an adapted 12-item Foot Care Confidence Scale (FCCS) by Sloan Helen L. (2002) [22].
Validity of the instrument
The instrument was subjected to face and construct validity by thorough scrutiny by the researcher’s supervisor and expert clinician caring for PWDM and DFU. The multidimensional validated questionnaire containing sections on FCCS and NAFFS was subjected to forward and backward translation to Yoruba and English to ensure their validity. The items in each section of the instrument were further subjected to content validity testing by submitting the instrument to five experts and using Lawshe's formula to ensure the content validity ratio (CVR) for each item in each section of the instrument, resulting in the content validity index (CVI) for each section. According to Ayre and Sally (2013) [23], the CVR (content validity ratio) proposed by Lawshe (1975) [24] is a linear transformation of a proportional level of agreement on how many “experts” within a panel rate an item “essential” calculated in the following way:
CVR is the content validity ratio, ne is the number of panel members indicating an item “essential,” and N is the number of panel members.Just like r, CVR ranges between -1 through 0 to +1.
The closer to +1 is CVR for an item; the more valid is the item in the scale while CVR values closer to 0 imply lack of content validity. However, CVI is computed by dividing sum of CVR values by the total number of items. CVI is interpreted for the scale the same way CVR values are interpreted for the items. Table 1 displayed the CVIs for the relevant sections of the multidimensional instrument:
|
Instrument |
Number of Items |
Content Validity Index (CVI) |
Comment |
|
Foot Self-care Knowledge scale |
7 |
0.84 |
Valid |
|
FCCS |
12 |
0.76 |
Valid |
|
NAFFS |
26 |
0.86 |
Valid |
Table 1. Validity table
Reliability of the instrument
The reliability of the knowledge part of the questionnaire in section A was established using the Kuder Richardson formula- 20, KR20 conducted on SPSS Version 23 because of the dichotomous nature of the items in the section of the multidimensional instrument. Though the other 2 validated instruments, FCCS and NAFFS reportedly had Cronbach’s alpha reliability indices of 0.92 and 0.91 respectively, but all these instruments were revalidated by administering them on a sample of 30 respondents similar to but entirely different from those recruited for the main study. The reliability index obtained for the instruments was > 0.9 (Table 2).
|
Instrument |
Number of items |
Cronbach Alpha/KR20 |
Comment |
|
Foot Self-care Knowledge scale |
7 |
0.972 |
Sufficiently Reliable |
|
FCCS |
12 |
0.996 |
Sufficiently Reliable |
|
NAFFS |
26 |
0.997 |
Sufficiently Reliable |
Table 2. Reliability indices for the variables in the multidimensional instrument
Method of data collection
After gaining approval from the two institutions' ethical committee, the individual's informed consent, and permission from the head of the OPD at both, the instruments for data collection were given to study participants on clinic days over the course of four months (July to October, 2023), two research assistants attended a two-day training session where they learned about the objectives of the study, the content of foot care and DFU prevention guidelines/standards, FSC behavior and self-efficacy tools, and how to distribute the questionnaires. They were selected from among the registered nurses who care for patients with diabetes and DFU at Sacred Heart Hospital, Lantoro. Targeting their clinic hours on Mondays and Wednesdays, the study settings (FMC and State Hospital, Ijaye, respectively) were visited in the morning. As soon as the surveys were completed, they were gathered. People who were illiterate were helped to complete the surveys by having them translated into their native tongue.
Method of data analysis
Descriptive statistics such as means and standard deviations were used for continuous variables, while frequencies and percentages were used for categorical variables.
Responses to attitudinal or perception-based questions were measured using a 5-point Likert scale (1 = Strongly Disagree, 2 = Disagree, 3 = Neutral, 4 = Agree, 5 = Strongly Agree). Where applicable, composite scores were computed, and the scale reliability was assessed using Cronbach’s alpha.
Inferential statistics, including chi-square tests for categorical variables and independent t-tests or ANOVA for comparing group means, were applied where appropriate.
Statistical significance was set at p < 0.05. Data were entered and analyzed using IBM SPSS Statistics version 23.0 (IBM Corp., Armonk, NY, USA).
RESULTS
One hundred and twenty questionnaires were administered to the respondents, same received and used for analysis.
|
Characteristics |
Categories |
n (%) |
Mean |
SD |
|
Age (years) |
21–30 |
28 (23.3) |
||
|
31–40 |
24 (20.0) |
|||
|
41–50 |
21 (17.5) |
|||
|
51–60 |
26 (21.7) |
44.8 |
14.65 |
|
|
61–70 |
17 (14.2) |
|||
|
>70 |
4 (3.3) |
|||
|
Gender ᵃ |
Female |
85 (70.8) |
1.29 |
0.46 |
|
Male |
35 (29.2) |
|||
|
Marital status ᵇ |
Single |
30 (25.0) |
2.13 |
0.90 |
|
Married |
55 (45.8) |
|||
|
Separated/Divorced |
24 (20.0) |
|||
|
Widowed |
11 (9.2) |
|||
|
Educational status ᶜ |
No formal education |
28 (23.3) |
2.55 |
1.13 |
|
Primary |
31 (25.8) |
|||
|
Secondary |
28 (23.3) |
|||
|
Tertiary |
33 (27.5) |
|||
|
Occupation ᵈ |
Unemployed |
28 (23.3) |
2.53 |
1.08 |
|
Farming |
28 (23.3) |
|||
|
Trading |
37 (30.8) |
|||
|
Civil servant |
27 (22.5) |
|||
|
Type of diabetes ᵉ |
Type 1 |
50 (41.7) |
1.58 |
0.50 |
|
Type 2 |
70 (58.3) |
|||
|
Duration since diagnosis ᶠ |
1–24 months |
87 (72.5) |
1.47 |
0.87 |
|
25–48 months |
17 (14.2) |
|||
|
49–72 months |
9 (7.5) |
|||
|
>72 months |
7 (5.8) |
|||
|
Previous foot–care education ᵍ |
Yes |
50 (41.7) |
1.58 |
0.50 |
|
No |
70 (58.3) |
|||
|
Foot-care frequency ʰ |
Once a week |
16 (13.3) |
2.75 |
1.59 |
|
2–6 times/week |
22 (18.3) |
|||
|
Once a day |
8 (6.7) |
|||
|
>1 time/day |
4 (3.3) |
|||
|
Not applicable |
70 (58.3) |
|||
|
Knowledge of foot care ⁱ |
No idea |
72 (60.0) |
0.48 |
0.65 |
|
Moderate idea |
38 (31.7) |
|||
|
Expert idea |
10 (8.3) |
|||
|
Performs foot care independently ʲ |
Yes |
87 (72.5) |
1.28 |
0.45 |
|
No |
33 (27.5) |
|||
|
**If No, who helps? **ᵏ |
Family |
31 (25.8) |
2.02 |
0.98 |
|
Friends |
2 (1.7) |
|||
|
Not applicable |
87 (72.5) |
Table 3. Sociodemographic characteristics of 120 respondents (Source: Field survey, 2023)
Table 3 showed the demographic distribution of the respondents. The majority 28 (23.1%) of them are in the age group of 21-30 years, while the 4 (3.3%) that were above 70 years were the least in the distribution with the mean age of 44.8±14.65 years. About three-quarters 85 (70.8%) are female, while 35 (29.2%) are male. The majority were married, 55 (45.8%), and 30 (25%) are single. Most of the respondents had higher education 33 (27.5%), while both illiterates and secondary school completers were 28 (23.3%), respectively. Traders were more than other categories at 37 (30.8%) followed by civil servants at 27 (22.5%).
As shown further in Table 3, more than half 70 (58.3%) of the respondents had T2DM with majority 87 (72.5%) diagnosed within the past 24 months. Findings also revealed that 50 (41.7%) of the respondents had prior attendance at FSC education while 70 (58.3%) had no such experience. A few, 16 (13.3%), 22 (18.3%), 8 (6.7%) and 4 (3.3%) of the participants attended once a month, every other month, whenever chanced, and when reminded respectively, while this was not applicable to 70 (58.3%) of them. The majority, 72 (60.0%) of the participants had no idea know what foot care is, 38 (31.7%) had moderate idea while 10 (8.3%) claimed to have expertise idea. Finally, 87 (72.5%) performed foot care by themselves while 33 (27.5%) did not.
Respondents’ knowledge of foot self-care
|
Item |
No |
Yes |
|
|
People with diabetes should check their feet at least once a day |
77(64.2%) |
43(35.8%) |
|
|
People with diabetes should inspect their toes, nails, and cut it straight |
77(64.2%) |
43(35.8%) |
|
|
The feet should be washed, and lotion applied to moisturize them |
77(64.2%) |
43(35.8%) |
|
|
People with diabetes should warm their feet with lantern |
66(55%) |
54(45%) |
|
|
Before putting on shoes, people with diabetes should inspect the interior of them |
76(63.3%) |
44(36.7%) |
|
|
Foot corn/callus should be removed with razor blade |
76(63.3%) |
44(36.7%) |
|
|
People with diabetes should wear shoes that are not too tight |
76(63.3%) |
44(36.7%) |
Table 4. Knowledge of 120 respondents on foot self-care (Source: Field survey, 2023)
From table 4 the majority 77 (64.2%) of the participants declined that, PWDM should check their foot once daily, inspect their toes, nails, and cut it straight and the feet should be washed, and lotion applied to moisturize them. A little above half 66 (55.0%) disagreed with the statement that PWDM should warm their feet with lantern. Additionally, 44 (36.7%) of the respondents indicated that PWDM should wear shoes that are not too tight, remove corns and calluses from their feet with a razor blade, and check the inside of their shoes before wearing them.
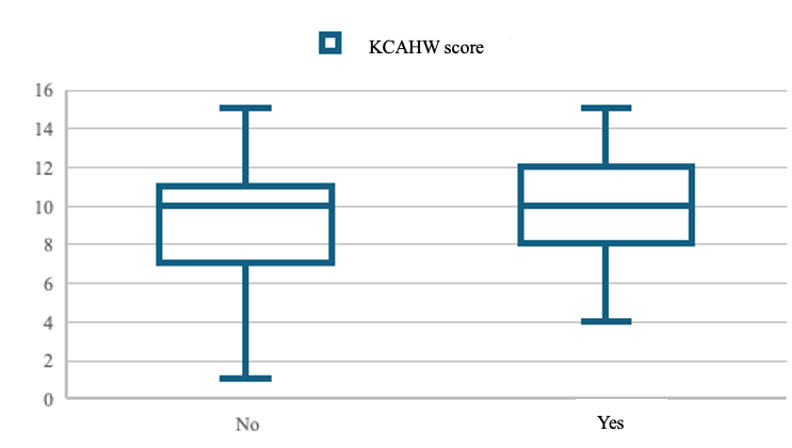
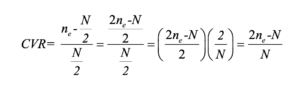
Summary of respondents’ knowledge about foot self-care
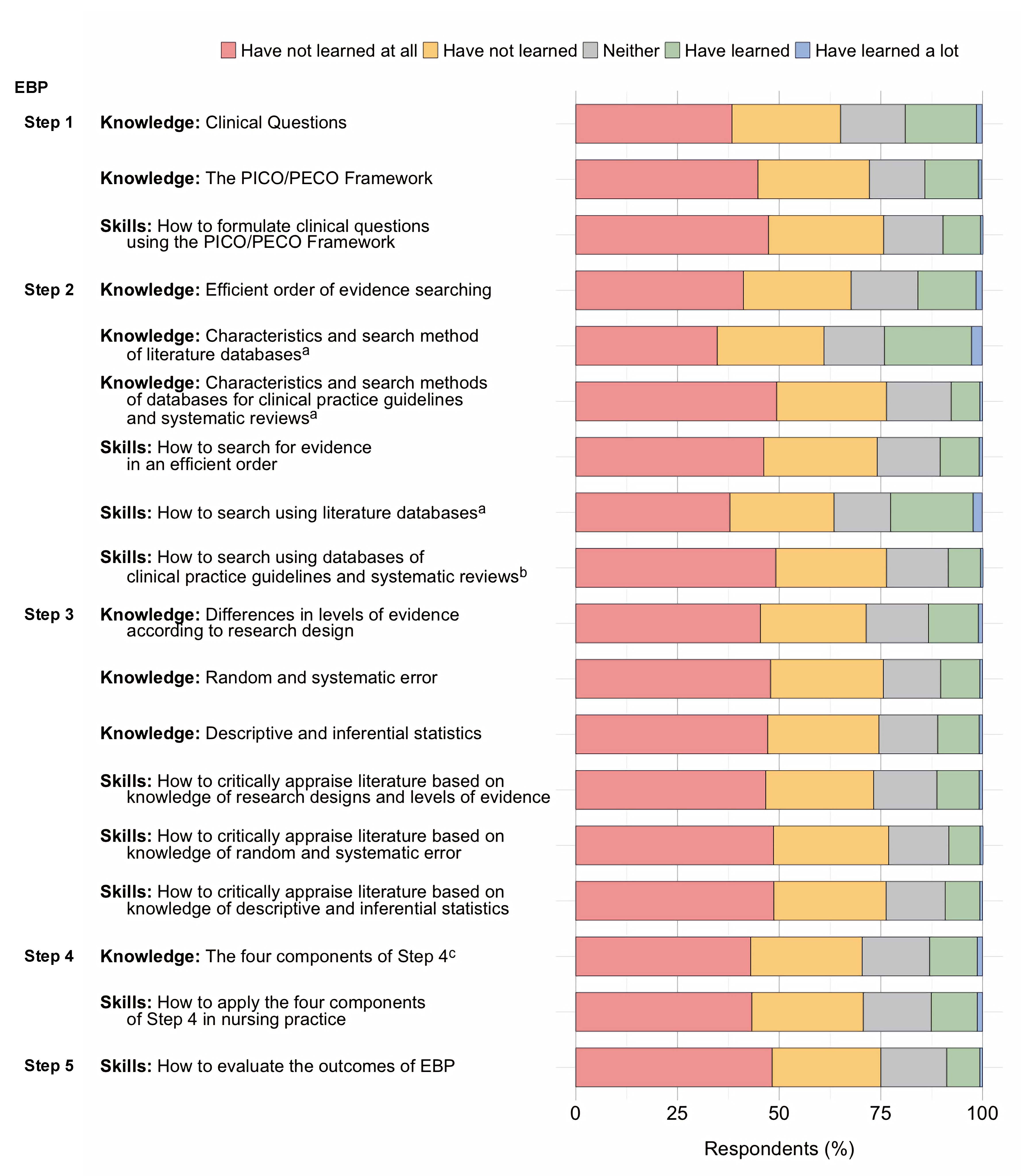
Overall, the mean knowledge score was 9.63+3.08. As shown in Figure 1, 55% of the respondents had low level of knowledge of foot care, 17.5% of them had moderate knowledge while only 27.5% of them had high knowledge of foot self-care.
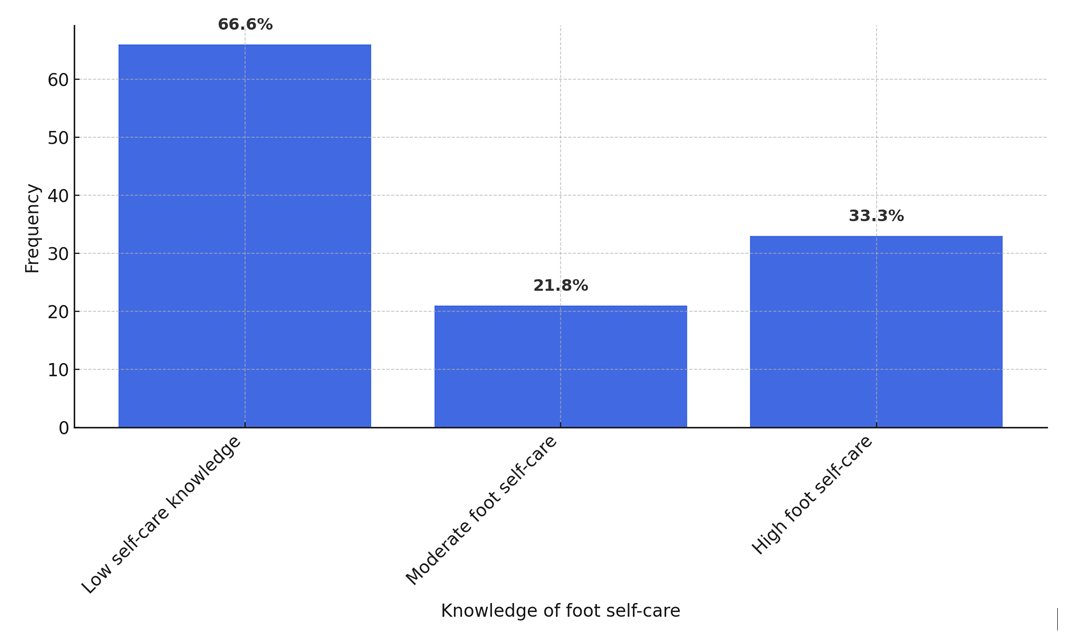
Figure 1. Respondents’ level of knowledge about foot self-care
Self-efficacy to practice foot ulcer preventive activities among patients
|
|
Strongly not confident |
Moderately not confident |
Confident |
Moderately confident |
Strongly confident |
|
f (%) |
f (%) |
f (%) |
f (%) |
f (%) |
|
|
I can protect my feet |
66 (55%) |
0 (0%) |
11 (9.2%) |
32 (26.7%) |
11 (9.2%) |
|
I can examine my feet every day to check for cuts, scratches, blisters, redness, or dryness even if I'm not in pain or uncomfortable. |
66 (55%) |
0 (0%) |
11 (9.2%) |
32 (26.7%) |
11 (9.2%) |
|
I can determine when to use a pumice stone to smooth corns and/or calluses on my feet. I can dry between my toes after washing my feet. I can determine when my toenails need to be clipped by a podiatrist. |
66 (55%) |
0 (0%) |
11 (9.2%) |
32 (26.7%) |
11 (9.2%) |
|
Prior to dipping my feet into the water, I may check the water's temperature. |
66 (55%) |
0 (0%) |
11 (9.2%) |
32 (26.7%) |
11 (9.2%) |
|
Even when I'm not in pain or uncomfortable, I may examine my feet daily to look for cuts, scratches, blisters, redness, or dryness. |
66 (55%) |
0 (0%) |
11 (9.2%) |
32 (26.7%) |
11 (9.2%) |
|
I am able to judge when to use a pumice stone on my foot to remove calluses and/or corns. After washing my feet, I can pat dry between my toes. I am able to tell when a podiatrist is necessary to trim my toenails. |
66 (55%) |
0 (0%) |
0 (0%) |
43 (35.8%) |
11 (9.2%) |
|
I could take a look at the water's temperature before putting my feet in it. |
66 (55%) |
0 (0%) |
0 (0%) |
44 (36.7%) |
10 (8.3%) |
|
If I was told to do so, I can wear shoes and socks every time I walk (includes walking indoors) |
66 (55%) |
0 (0%) |
10 (8.3%) |
44 (36.7%) |
0 (0%) |
|
When I go shopping for new shoes, I can choose shoes that are good for my feet |
66 (55%) |
0 (0%) |
10 (8.3%) |
44 (36.7%) |
0 (0.0%) |
|
I can call my doctor about problems with my feet |
66 (55%) |
0 (0%) |
0 (0%) |
44 (36.7%) |
10 (8.3%) |
|
I can check the insides of my shoes for problems that can harm my feet before putting them on |
55 (45.8%) |
11 (9.2%) |
11 (9.2%) |
33 (27.5%) |
10 (8.3%) |
|
I can routinely apply lotion on my feet if directed to do so |
55 (45.8%) |
11 (9.2%) |
11 (9.2%) |
22 (18.3%) |
21 (17.5%) |
Table 5: Measure of confidence (Self-efficacy), N=120
As shown in Table 5, 66 (55.0%), 0 (0.0%), 11 (9.2%), 32 (26.7%) and 11 (9.2%) of the participants responded that, they were strongly not confident, moderately not confident, confident, moderately confident and strongly confident respectively to each of items ‘I can protect my feet’, ‘even without pain/discomfort, I can look at my feet daily to check for cuts, scratches, blisters, redness or dryness’, ‘After washing my feet, I can dry between my toes’, ‘I can judge when my toenails need to be trimmed by a podiatrist’, ‘I can trim my toenails straight across’, and ‘I can figure out when to use a pumice stone to smooth corns and/or calluses on my feet’. Majority of the participants agreed they were strongly not confident, moderately not confident, confident, moderately confident and strongly confident respectively to item which stated, "I can test the water's temperature before putting my feet into it". Overall, the mean self-efficacy score was 28.47±18.19.
|
Behavior Item |
Response Options |
f (%) |
|
Examination & Hygiene |
||
|
How often do you examine your feet? |
Once a week |
11 (9.2) |
|
2–6 times a week |
55 (45.8) |
|
|
Once a day |
21 (17.5) |
|
|
More than once a day |
33 (27.5) |
|
|
Do you check your shoes before you put them on? |
Once a week |
11 (9.2) |
|
2–6 times a week |
55 (45.8) |
|
|
Once a day |
21 (17.5) |
|
|
More than once a day |
33 (27.5) |
|
|
Do you check your shoes when you take them off? |
Once a week |
33 (27.5) |
|
2–6 times a week |
33 (27.5) |
|
|
Once a day |
21 (17.5) |
|
|
More than once a day |
33 (27.5) |
|
|
Do you wash your feet? |
Once a week |
33 (27.5) |
|
2–6 times a week |
33 (27.5) |
|
|
Once a day |
21 (17.5) |
|
|
More than once a day |
33 (27.5) |
|
|
Do you check feet are dry after washing? |
Once a week |
33 (27.5) |
|
2–6 times a week |
33 (27.5) |
|
|
Once a day |
21 (17.5) |
|
|
More than once a day |
33 (27.5) |
|
|
Do you dry between toes? |
Once a week |
33 (27.5) |
|
2–6 times a week |
33 (27.5) |
|
|
Once a day |
21 (17.5) |
|
|
More than once a day |
33 (27.5) |
|
|
Do you use moisturizing cream on your feet? |
Once a week |
33 (27.5) |
|
2–6 times a week |
33 (27.5) |
|
|
Once a day |
21 (17.5) |
|
|
More than once a day |
33 (27.5) |
|
|
Do you apply cream between toes? |
Once a week |
33 (27.5) |
|
2–6 times a week |
33 (27.5) |
|
|
Once a day |
21 (17.5) |
|
|
More than once a day |
33 (27.5) |
|
|
Are your toenails cut? |
Once a week |
33 (27.5) |
|
2–6 times a week |
33 (27.5) |
|
|
Once a day |
21 (17.5) |
|
|
More than once a day |
33 (27.5) |
|
|
Footwear Habits |
||
|
Do you wear unfastened slippers? |
Most of the time |
33 (27.5) |
|
Sometimes |
33 (27.5) |
|
|
Rarely |
10 (8.3) |
|
|
Never |
44 (36.7) |
|
|
Do you wear sneakers? |
Most of the time |
33 (27.5) |
|
Sometimes |
33 (27.5) |
|
|
Rarely |
10 (8.3) |
|
|
Never |
44 (36.7) |
|
|
Do you wear shoes with straps, Velcro, or lace-up closures? |
Most of the time |
33 (27.5) |
|
Sometimes |
33 (27.5) |
|
|
Rarely |
21 (17.5) |
|
|
Never |
33 (27.5) |
|
|
Do you wear shoes with pointy toes? |
Most of the time |
33 (27.5) |
|
Sometimes |
33 (27.5) |
|
|
Rarely |
21 (17.5) |
|
|
Never |
33 (27.5) |
|
|
Do you dress in mules or flip-flops? |
Most of the time |
33 (27.5) |
|
Sometimes |
33 (27.5) |
|
|
Rarely |
21 (17.5) |
|
|
Never |
33 (27.5) |
|
|
Is it customary to break in new shoes gradually? |
Always |
22 (18.3) |
|
Most of the time |
44 (36.7) |
|
|
Sometimes |
21 (17.5) |
|
|
Rarely/Never |
33 (27.5) |
|
|
Do you wear synthetic socks (e.g., nylon)? |
Most of the time |
22 (18.3) |
|
Sometimes |
44 (36.7) |
|
|
Rarely |
21 (17.5) |
|
|
Never |
33 (27.5) |
|
|
Do you wear shoes without socks/tights? |
Never |
22 (18.3) |
|
Rarely |
44 (36.7) |
|
|
Sometimes |
21 (17.5) |
|
|
Often |
33 (27.5) |
|
|
How often do you replace socks/tights? |
< 4 times/week |
33 (30.3) |
|
4–6 times/week |
21 (19.3) |
|
|
Daily |
33 (30.3) |
|
|
> once/day |
22 (20.2) |
|
|
Barefoot Practices & First Aid |
||
|
Do you go barefoot at home? |
Often |
11 (9.2) |
|
Sometimes |
55 (45.8) |
|
|
Rarely |
21 (17.5) |
|
|
Never |
33 (27.5) |
|
|
Are you barefoot outside? |
Often |
22 (18.3) |
|
Sometimes |
44 (36.7) |
|
|
Rarely |
32 (26.7) |
|
|
Never |
22 (18.3) |
|
|
Do you use a hot water bottle in bed? |
Often |
22 (18.3) |
|
Sometimes |
44 (36.7) |
|
|
Rarely |
32 (26.7) |
|
|
Never |
22 (18.3) |
|
|
For corns, do you use home treatments (e.g., plasters)? |
Never |
22 (18.3) |
|
Rarely |
44 (36.7) |
|
|
Sometimes |
21 (17.5) |
|
|
Often |
33 (27.5) |
|
|
For blisters, do you use a dry dressing? |
Never |
22 (18.3) |
|
Rarely |
44 (36.7) |
|
|
Sometimes |
10 (8.3) |
|
|
Often |
44 (36.7) |
|
|
For cuts/grazes/burns, do you use a dry dressing? |
Never |
22 (18.3) |
|
Rarely |
44 (36.7) |
|
|
Sometimes |
21 (17.5) |
|
|
Often |
33 (27.5) |
Table 6. Respondents’ foot self-care behavior/activities, N=120.
As shown in Table 6, 11 (9.2%), 55 (45.8%), 21 (17.5%) and 33 (27.5%) consented that, they examined their feet and check their shoes before they put them on once a week, 2 – 6 times a week, once a day and more than once a day respectively. Also, 33 (27.5%), 33 (27.5%), 21 (17.5%) and 33 (27.5%) responded once a week, 2 – 6 times a week, once a day and more than once a day respectively to each of items; "Do you wash your feet?" "Do you check that your feet are dry after washing?" "Do you dry between your toes?" "Do you use moisturizing cream on your feet?" "Do you use moisturizing cream between your toes?" and "Are your toenails cut?" - for each item, 33 (27.5%), 33 (27.5%), 10 (8.3%), and 44 (36.7%) of the participants gave their response most of the time, occasionally, seldom, and never, respectively. For questions on "Do you wear trainers?" and "Do you wear slippers without fastenings?" - 33 (27.5%), 21 (17.5%), 33 (27.5%), and 33 (27.5%) of the participants answered each item most of the time, seldom, infrequently, and never, respectively.
For the question, ‘Do you break in new shoes gradually?’, 22 (18.3%), 44 (36.7), 21 (17.5%) and 33 (27.5%) of the subjects responded always, most of the time, sometimes and rarely/never respectively. Similarly, 22 (18.3%), 44 (36.7), 21 (17.5%) and 33 (27.5%) responded most of the time, sometimes, rarely and never respectively to “Do you wear artificial fiber (e.g., nylon) socks. The response pattern was also 22 (18.3%), 44 (36.7), 21 (17.5%) and 33 (27.5%) implying never, rarely, sometimes and often respectively for question ‘Do you wear shoes without socks/stockings/tights?’ ‘Do you change your socks/stockings/tights?’ got the response pattern, 22 (20.2%), 33 (30.3%), 21 (19.3%) and 33 (30.3%) implying more than once a day, daily, 4-6 times a week and less than 4 times a week respectively for a total of 109 responses for the item.
Items ‘Do you walk around the house in bare feet?’ and ‘Do you walk outside in bare feet?’ turned in the response pattern, 11 (9.2%), 55 (45.8), 21 (17.5%) and 33 (27.5%) to denote often, sometime, rarely and never respectively. Also, 22 (18.3%), 44 (36.7%), 32 (26.7%) and 22 (18.3%) gave the responses, often, sometime, rarely and never respectively to item "Do you use a hot water bottle in bed?", item "Do you place your feet close to the flames?" and "Do you place your feet on a radiator?". For item ‘Do you use corn remedies/ corn plasters/paints when you get a corn?’ and item ‘Do you put a dry dressing on a graze, cut or burn when you get one?’, 22 (18.3%), 44 (36.7%), 21 (17.5%) and 33 (27.5%) of the participants responded, never, rarely, sometimes and often respectively to each of the items. On the other hand, the responses to the question, "Do you put a dry dressing on a blister when you get one?" were as follows: 22 (18.3%), 44 (36.7%), 10 (8.3%), and 44 (36.7%). Whereas the mean of 39.34±27.57 was obtained for respondents’ foot self-care behavior.
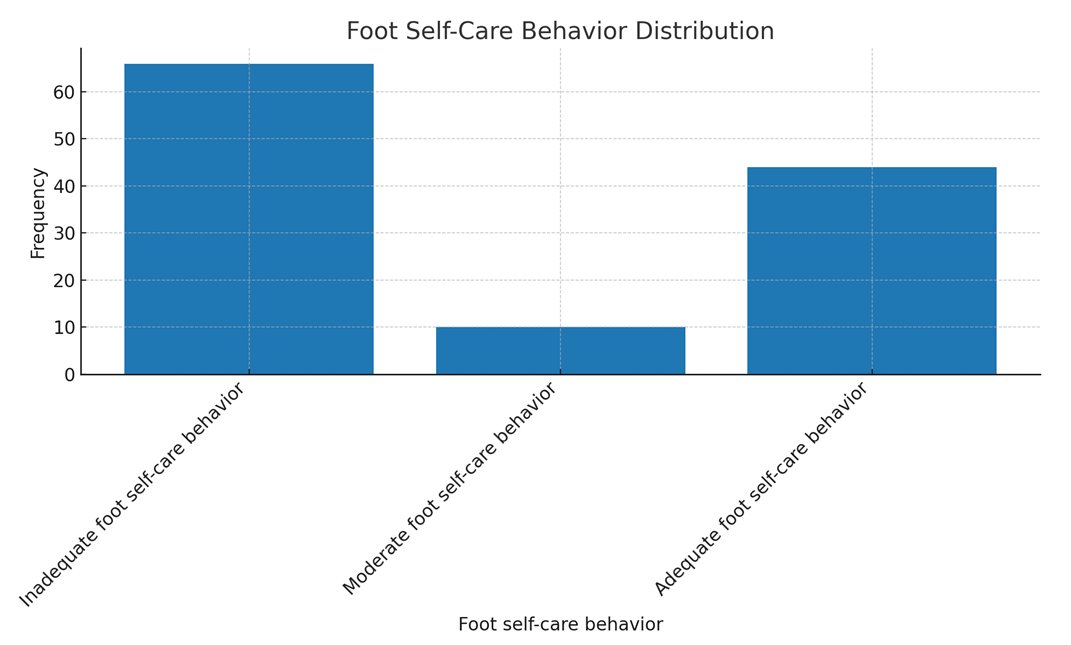
Figure 2. Respondents’ foot self-care behavior
As shown in Figure 2, 66(55%) of them had inadequate foot self-care behavior, only 10 (8.3%) of them had moderate foot self-care behavior, while 44 (36.7%) of the respondents had adequate foot self-care behavior.
Hypotheses testing
Ho: There is no significant individual and composite association between age, gender, educational status and behavior of FSC among PWDM.
|
Model |
Unstandardized Coefficients (B) |
Std. Error |
Standardized Coefficients (Beta) |
t |
Sig. (p-value) |
|
|
(Constant) |
38.543 |
7.692 |
5.011 |
<0.0001 |
||
|
Age |
2.622 |
6.077 |
0.133 |
0.432 |
0.667 |
|
|
Gender |
-1.078 |
9.246 |
-0.018 |
-0.117 |
0.907 |
|
|
Educational Status |
-2.089 |
8.227 |
-0.086 |
-0.254 |
0.800 |
|
|
Note: Dependent Variable = FSC Behavior |
||||||
Table 7. Multivariate analysis between age, gender, educational status and foot self-care behavioramongPWDM
As shown in Table 7, multiple regression analysis was conducted to predict the association between age, gender and educational status and self-care behavior. Particularly, by ANOVA summary for the Regression Model, the resultant model was not significant, F (3, 119) = 0.97, p = 0.962, R2= 0.002. Table 7 revealed that the individual variables also had no significant association of age (t = 0.432, p = 0.667), gender (t = -0.117, p = 0.907) and educational status (t = -0.254, p = 0.800) with FSC behavior.
As shown in Table 8, multiple regression analysis was conducted to test the association between knowledge of FSC, efficacy and self-care behavior of people with diabetes. Particularly, by ANOVA summary for the Regression Model, the resultant model for foot self-care efficacy and FSC knowledge against self-care behavior was significant, F (2, 119) = 589.764, p<0.0001, R2= 0.910.
Table 8 revealed that individual variables had significant association FSC knowledge (t =8.252, p<0.0001) and FSC efficacy (t =3.610, p<0.0001) with FSC behavior.
|
Predictor |
Unstandardized Coefficients (B) |
Std. Error |
Standardized Coefficients (Beta) |
t |
Sig. (p-value) |
|
(Constant) |
-31.312 |
3.983 |
– |
-7.861 |
<0.0001 |
|
Foot Self-Care Knowledge |
6.023 |
0.730 |
0.672 |
8.252 |
<0.0001 |
|
Foot Self-Care Efficacy |
0.446 |
0.123 |
0.294 |
3.610 |
<0.0001 |
|
Note: Dependent Variable = Foot Self-Care Behavior. |
|||||
Table 8. Multivariate analysis between Foot Self-Care Knowledge, Foot Self-Care Efficacy and Foot Self-Care Behavior amongPWDM
DISCUSSION
The current investigation discovered that very few participants were older than 70. This result contradicts the age-based rate reported by Odusan, Amoran, and Salami [25], who observed that the elderly have a higher prevalence of diabetes than youngsters. Nonetheless, the present result is consistent with the CDC's [26] assertion that the number of children, adolescents, and young adults developing DM is rising. The fact that many young people are leading improper lifestyles could help to explain this predicament. Some of these youths, who come from parents who are secure in terms of socioeconomic status yet reside in the city, lead unhealthy lives because they eat junk food and exercise infrequently. This scenario can make a good number of them to be diabetic. The study’s finding in concordance with previous research findings shows more females with diabetes, this agrees with Turan et al. [27] and Wazqar et al. [5] that more females are diagnosed with diabetes more than their male counterparts. Most of the respondents had higher education this is in agreement with Bekele [28] findings that higher educational status is one of the predictors of FSC practices. Majority were T2DM (53.8%) which corresponds with Sen et al. [29] and Wanja et al. [30], of which majority were diagnosed within the last 24 months.
The level of knowledge of PWDM on foot ulcer preventive self-care activities.
One of the main conclusions of this study was that the respondents' level of FSC knowledge was low. Consequently, there is a need for skilled instruction on diabetes FSC and the creation of guidelines for PWDM to carry out FSC. This conclusion runs counter to prior research by Alshammari et al. [31], who discovered that around 282 (76.6%) of the patients in their Riyadh, Saudi Arabia, study had a thorough awareness of foot ulcers and diabetic foot. The literature, however, provides a wealth of evidence to support the reported position of low knowledge of FSC. Goie and Naidoo [12] and Adeyemi et al. [16] for example, agreed with Ogunlana [29] when she stated that individuals with diabetes mellitus in Sub-Saharan Africa have a limited understanding of the complications associated with their disease. As Africans, we rely heavily on the rule of thumb in many situations, particularly in times of emergency when managing diabetes calls for it. Except for the standard, frequently ineffectual recommendations obtained during hospital visits, there are very few proactive steps available for managing the difficulties associated with diabetes in such circumstances. Thus, the creation of an out-of-hospital care regimen becomes necessary.
The self-efficacy of PWDM to practice foot ulcer preventive activities
The discovery that the majority of those who participated had poor FSC Efficacy scores is another indication of the growing mortality and morbidity linked to diabetes and its complications. People lack the abilities, bravery, and self-assurance necessary to combat, control, and overcome DFU, a serious symptom that causes suffering and casualties for diabetics. The findings in this study deviated from the seemingly typical trend, even though Narmawan, Syahrul, and Erika [32] and Sharoni et al. [33] had previously demonstrated that the patients in their studies had high FSC efficacy. Additional published research that supports the inherent deficiencies in FSC efficacy or parallel variables among diabetics include Wazqar et al. [5], Khan et al. [9], Mekonen and Demssie [34], and Turan et al. [27]. These studies were founded on evidentiary viewpoints. It is interesting to know why the present result in this study—which isn't generally praised in the literature—is what it is. However, the majority's low FSC efficacy is not surprising in the slightest because, despite claims to the contrary, a population lacking in knowledge cannot assert that it has high self-efficacy—a concept that is far higher than knowledge and that no conventional education can ensure. In summary, while knowing is crucial for self-care, it might not necessarily translate into self-efficacy. This suggests that educational initiatives that just emphasize knowledge may not result in self-efficacy, and it is unwarranted to assume that a lack of knowledge will lead to a lack of efficacy or self-confidence. This means that, if self-efficacy had been high, the participants in this study would have had low moment foot self-care knowledge.
Foot self-care behavior of people with diabetes
A significant finding of this study indicated that a considerable number of individuals had insufficient foot self-care practices. This leads to the primary rationale of this study. Low levels of self-care behavior are thought to be the underlying cause of DFU. The present finding of low self-care behavior with respect to DFU emphasizes the earlier position of Ammar et al. [35] that foot ulcers and amputations are regrettably prevalent with poverty, improper sanitation and hygiene, and barefoot walking often connecting to worsen the adverse effects of diabetic foot damage. Hirpha, Tatiparthi, and Mulugeta's [13] additional research, which observed that those with diabetes did not sufficiently self-inspect, wash their feet at least once a day, dry after washing, and moisturize the dry skin as they walked barefoot, in sandals or slippers, or in shoes without socks, supports the results under discussion. It is important to stress that the existing practice goes against the advice given by Armstrong et al. [36] and van Netten et al. [37], who provided factual evidence to support their recommendations regarding the importance of routine foot inspections for PWDM. The problem persists when the number of patients in need of health care services is not matched by the number of caregivers and health workers/educators currently in place. This documented anomaly is therefore not unrelated to the culture of unsanitary living, complacency, misinformation, and poor knowledge among some people.
The results demonstrated that foot self-care behavior was not predicted by age, gender, or educational attainment. While earlier research [33,32,20,38] suggested that specific age, gender, and educational level reinforce FSC behavior, the present investigation has documented the opposite for reasons that are closely related to the fact that care behavior is a personal matter, independent of known biases or socioeconomic inclinations.
The findings also highlight the importance of collaboration in attempts to instill the necessary skills and attitude to give the motivation needed for effective self-care behavior. Lastly, the significant individual and joint association of FSC knowledge and foot care self-efficacy with FSC behavior highlights the need for each of these factors to instill self-care behavior. In their research, Wendling and Beadle [39] showed that self-efficacy advancement is a successful nursing intervention for health promotion. Positive outcomes, such as better outcomes for people with diabetes mellitus, fewer admissions, and fewer ER visits, have been linked to this. Additionally, the study offered some limited understanding of the significance of the identified relationships. Support for the necessity of matching knowledge to practical skill training was given in 2016 by Sarkar et al. and Sharoni et al. [33], whose studies, respectively, demonstrated a major beneficial connection between self-efficacy and self-care practices among PWDM and an improvement in FSC behavior, foot care knowledge, foot care outcome expectation, and QoL (physical symptoms) after training.
CONCLUSION
Patients with diabetic foot ulcers (DM) frequently get DFU, and foot self-care (FSC) is a useful strategy to reduce this risk. But self-care is becoming more and more common because paid care services are expensive and there aren't many caregivers accessible. With an emphasis on young individuals aged 21 to 30, the research sought to assess FSC behavior for DM patients. Participants in the study had poor scores on behavior, efficacy, and knowledge assessments. Age, gender, and educational attainment did not significantly correlate with foot self-care behavior.
It is necessary to invest in educational interventions to provide patients with the skills and knowledge necessary for good foot care practices. These initiatives shouldn't, however, necessarily be classified according to factors like age, gender, or educational attainment. The results demonstrated a substantial correlation between efficacy and foot self-care behavior, indicating that increasing efficacy or FSC knowledge on its own might greatly enhance self-care behavior.
According to the study's findings, 91.1% of the variance in foot self-care behavior could be explained by knowledge of FSC and efficacy, which had a substantial composite connection with foot self-care behavior. In order to expedite the practice of foot self-care, educators must impart information of foot self-care (FSC) and its efficacy in addition to the requisite technology, scientific skills, practices, and artistic qualities. For greatest benefit, this will assist DM patients in initiating, managing, and engaging in self-care practices.
Based on the findings and discussions presented in this study, several important recommendations are proposed. Healthcare providers should prioritize expanding and promoting diabetes education programs that not only enhance patients' knowledge of foot self-care (FSC) but also strengthen self-efficacy by teaching practical skills and fostering confidence in patients' ability to carry out these activities. Patients must also be educated on the importance of choosing appropriate footwear, with a strong emphasis on the benefits of well-fitting shoes and the risks of walking barefoot, both indoors and outdoors, as a preventive measure against foot complications. In addition to education, healthcare professionals and educators are encouraged to implement strategies that boost patients' self-efficacy, such as goal-setting, individualized feedback, and supportive reinforcement that affirms their ability to manage self-care effectively.
Developing and distributing clear, concise self-care guidelines or protocols is essential, as is stressing the importance of regular foot examinations. Patients should be empowered to conduct daily foot checks and trained to identify signs such as cuts, blisters, or dryness that may require prompt attention. Furthermore, they should be cautioned against risky practices like using razor blades to remove corns and calluses and instead be encouraged to seek professional care for such concerns. Another important hygiene recommendation is to emphasize the necessity of changing socks regularly to maintain healthy foot conditions and prevent infections. These educational efforts should be institutionalized within healthcare policies at both national and facility levels, and embedded into healthcare training curricula for sustainable impact. Additional studies should be carried out to assess the effectiveness of foot care education, identify barriers to its implementation, and develop strategies to address these challenges.
Limitations and recommendations
The generalizability of the findings may be limited by factors such as sample size and study design, and future research should consider broadening the scope and incorporating multiple methodological approaches to enrich the validity of results. This study contributes to knowledge by showing that while knowledge is important, it alone is insufficient to improve patients’ foot self-care behavior unless it is reinforced by self-efficacy strategies and potentially other factors not examined in this research. It also presents evidence that differentiated learning based on age, gender, or education level may not be necessary for effective foot self-care training among patients. A key outcome of this study is the proposed knowledge-efficacy-behavior framework, which provides a conceptual basis for mastering diabetic foot self-care behavior.
In light of the study’s limitations and findings, further investigations are encouraged. Future researchers may consider integrating more independent variables—such as personal hygiene habits, coexisting health conditions, and access to healthcare services or information—into predictive models for foot self-care behavior. A quasi-experimental study design may also be employed to evaluate the effectiveness of targeted intervention packages on patients’ behavior. Additionally, new tools such as systematic observation instruments can be developed to complement the questionnaire method used in this study, offering a more comprehensive assessment of self-care practices.
Local Ethics Committee approval:
1. The study protocol was approved by the Research and Ethics Committee of Ogun State Hospital Management Board with REF NO: SHA 52/VOL XII/116. Date of approval: August 23, 2023.
2. The study protocol was approved by the Research and Ethics Committee of Federal Medical Center with REF NO: FMCA/470/HREC/01/2023/23NHREC/08/10-2015. Date of approval: June 19, 2023
Competing interests: None to declare.
Funding: This research received no external funding.
Authors’ contribution
Oseni Rukayat: Conceptualized idea and conducted full research.
Emmanson Emmanson: Assisted with the research and manuscript preparation for publication
Kolawole Ifeoluwapo:Assisted with the design of questionnaire and conducting interviews with the selected nurses.
Adejumo Prisca: Was responsible for literature reviews.
Obilor Helen: performed data analysis and edited the manuscript for publication.
REFERENCES
- International Diabetes Federation (2022). Diabetes around the world in 2021. 10th edition. https://diabetesatlas.org/#:~:text=1%20in%208%20adults%20(206,caused%20by%20diabetes%20in%202021. Accessed 24/02/2023.
- Paulsamy, P., Ashraf, R., Alshahrani, S. H. et al. (2021). Social Support, Self-Care Behaviour and Self-Efficacy in Patient with Type 2 Diabetes during the COVID- 19 Pandemic: A Cross-Sectional Study. National Library of Medicine. Healthcare (Basel). 9(11):1607. Doi:10.3390/healthcare9111607. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8622453/. Accessed 02/11/2023.
- Center For Disease Control and Prevention, (2023). Diabetes in Young People Is on the Rise. https://www.cdc.gov/diabetes/resources-publications/research-summaries/diabetes-young-people.html. Accessed 15/11/2023.
- World Health Organization, (2022). Diabetes. https://www.who.int/health-topics/diabetes#tab=tab_1. Accessed 05/06/2022.
- Wazqar AA, Baatya MM, Lodhi FS, Khan AA. Assessment of knowledge and foot self-care practices among diabetes mellitus patients in a tertiary care centre in Makkah, Saudi Arabia: a cross-sectional analytical study. Pan Afr Med J. 2021 Oct 29;40:123. doi: 10.11604/pamj.2021.40.123.30113. PMID: 36118942; PMCID: PMC9463747.
- Ugwu E, Adeleye O, Gezawa I, Okpe I, Enamino M, Ezeani I. Burden of diabetic foot ulcer in Nigeria: Current evidence from the multicenter evaluation of diabetic foot ulcer in Nigeria. World J Diabetes. 2019 Mar 15;10(3):200-211. doi: 10.4239/wjd.v10.i3.200. PMID: 30891155; PMCID: PMC6422858.
- Robles, R. B., Compean Ortiz, L. G., […] and Martinez, S. P. (2017). Knowledge and Practice of Diabetes Foot Care and Risk of Developing Foot Ulcers inMexico May Have Implications for Patients of Mexican Heritage Living in the US. SAGE Journals Vol 43, Issue 3. https://doi.org/10.1177/0145721717706417. Accessed 28/03/2023.
- Oliver, T I. and Mutlouglu, M. (2022). Diabetic Foot Ulcers. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. https://www.ncbi.nlm.nih.gov/books/NBK537328/.Accessed 24/07/2022.
- Khan, Y., M. Khan, M., & Raza Farooqui, M. (2017). Diabetic foot ulcers: a review of current management. International Journal of Research in Medical Sciences, 5(11), 4683–4689. https://doi.org/10.18203/2320-6012.ijrms20174916.
- Rahaman HS, Jyotsna VP, Sreenivas V, Krishnan A, Tandon N. Effectiveness of a Patient Education Module on Diabetic Foot Care in Outpatient Setting: An Open-label Randomized Controlled Study. Indian J Endocrinol Metab. 2018 Jan-Feb;22(1):74-78. doi: 10.4103/ijem.IJEM_148_17. PMID: 29535941; PMCID: PMC5838916.
- Boulton, Andrew. (2021). Diabetic Foot Disease during the COVID-19 Pandemic. Medicina. 57. 97. 10.3390/medicina57020097.
- Goie TT, Naidoo M. (2016). Awareness of diabetic foot disease amongst patients with type 2 diabetes mellitus attending the chronic out-patients department at a regional hospital in Durban, South Africa. Afr J Prm Health Care Fam Med. 8(1), a1170. http://dx.doi.org/10.4102/phcfm.v8i1.1170. Accessed 07/07/2022.
- Hirpha, N., Tatiparthi, R., and Mulugeta, T. (2020). Diabetic Foot Self-Care Practices Among Adult Diabetic Patients: A Descriptive Cross-Sectional Study. https://doi.org/10.2147/DMSO.S285929. Accessed 18/01/2023.
- Rural Health Information Hub (2020). Module 1: Health promotion and disease. Available at: https://www.ruralhealthinfo.org/toolkits/health-promotion/1/introduction. Last access: 02/01/2023.
- Mallorquí-Bagué, N., Lozano-Madrid, M., Toledo, E., Corella, D., Salas-Salvadó, J., Cuenca-Royo, A., ... & Fernández-Aranda, F. (2018). Type 2 diabetes and cognitive impairment in an older population with overweight or obesity and metabolic syndrome: baseline cross-sectional analysis of the PREDIMED-plus study. Scientific reports, 8(1), 16128 doi: 10.1038/s41598-018-33843-8.
- Adeyemi TM, Olatunji TL, Adetunji AE, Rehal S. Knowledge, Practice and Attitude towards Foot Ulcers and Foot Care among Adults Living with Diabetes in Tobago: A Qualitative Study. Int J Environ Res Public Health. 2021 Jul 29;18(15):8021. doi: 10.3390/ijerph18158021. PMID: 34360314; PMCID: PMC8345419.
- Mekonen EG, Gebeyehu Demssie T. Preventive foot self-care practice and associated factors among diabetic patients attending the university of Gondar comprehensive specialized referral hospital, Northwest Ethiopia, 2021. BMC Endocr Disord. 2022 May 11;22(1):124. doi: 10.1186/s12902-022-01044-0. PMID: 35546665; PMCID: PMC9097232.
- Tuha A, Getie Faris A, Andualem A, Ahmed Mohammed S. Knowledge and Practice on Diabetic Foot Self-Care and Associated Factors Among Diabetic Patients at Dessie Referral Hospital, Northeast Ethiopia: Mixed Method. Diabetes Metab Syndr Obes. 2021 Mar 17;14:1203-1214. doi: 10.2147/DMSO.S300275. PMID: 33762837; PMCID: PMC7982550.
- Ogunlana MO, Govender P, Oyewole OO, Odole AC, Falola JL, Adesina OF, Akindipe JA. Qualitative exploration into reasons for delay in seeking medical help with diabetic foot problems. Int J Qual Stud Health Well-being. 2021 Dec;16(1):1945206. doi: 10.1080/17482631.2021.1945206. PMID: 34219610; PMCID: PMC8259813.
- Ojewale, L.Y., Okoye, E. A. and Ani, O. B. (2021). Diabetes Self-Efficacy and Associated Factors among People Living with Diabetes in Ibadan, Southwestern Nigeria. European Journal of Medical and Health Sciences. Vol. 3 No. 6. https://doi.org/10.24018/ejmed.2021.3.6.1129.
- Lincoln, N., Jeffcoate, W., Ince, P., Smith, M. and Radford, K. (2007), Validation of a new measure of protective footcare behaviour: the Nottingham Assessment of Functional Footcare (NAFF). Pract Diab Int, 24: 207-211. https://doi.org/10.1002/pdi.1099
- Sloan HL. Developing and testing of the Foot Care Confidence Scale. J Nurs Meas. 2002 Winter;10(3):207-18. doi: 10.1891/jnum.10.3.207.52564. PMID: 12885146
- Ayre, C., & Scally, A. J. (2014). Critical values for Lawshe’s content validity ratio: Revisiting the original methods of calculation. Measurement and Evaluation in Counseling and Development, 47(1), 79–86. https://doi.org/10.1177/0748175613513808
- Lawshe, C. H. (1975). A quantitative approach to content validity. Personnel psychology, 28(4).
- Odusan, O., Amoran, O. E., & Salami, O.E. (2017). Prevalence and pattern of diabetic foot ulcers among adults with diabetes in a secondary health care facility in Lagos, Nigeria. Anals of health research:3(2). https://www.annalsofhealthresearch.com/index.php/ahr/article/view/70. Accessed 28/03/2023
- Center For Disease Control and Prevention, (2023). Diabetes in Young People Is on the Rise.https://www.cdc.gov/diabetes/resources-publications/research-summaries/diabetes-young-people.html. Accessed 15/11/2023
- Turan, E., Onalan, R., Iscimen, N. C., Ozan, Z. T., Yildirim, T., & Aral, Y. (2020). Foot Self-Care Behavior in Patients with Diabetes. J Soc Health Diab:2020;8:13-17 http://doi.org/10.1055/s-0040-1716812
- Bekele, F., Berhanu, D., Sefera, B., & Babu, Y. (2021). Diabetic foot self-care practices and its predictors among chronic diabetic mellitus patients of Southwestern Ethiopia hospitals: a cross-sectional study. https://doi.org/10.1016/j.ijans.2022.100489. Accessed 25/03/2023.
- Şen HM, Şen H, Aşık M, Özkan A, Binnetoglu E, Erbağ G, Karaman HI. The importance of education in diabetic foot care of patients with diabetic neuropathy. Exp Clin Endocrinol Diabetes. 2015 Mar;123(3):178-81. doi: 10.1055/s-0034-1389981. Epub 2014 Oct 14. PMID: 25314654.
- Wanja L, Mwenda C, Mbugua R, Njau S. (2019). Determinants of foot self-care practices among diabetic patients attending diabetic clinic at a referral hospital, Meru County – Kenya. Int J Sci Res Public. 9(10):p9461. Doi:10.29322/ijsrp.9.10.2019.p9461. Accessed 18/01/2023.
- Alshammari ZJ, Alsaid LA, Parameaswari PJ, Alzahrani AA. Attitude and knowledge about foot care among diabetic patients in Riyadh, Saudi Arabia. J Family Med Prim Care. 2019 Jun;8(6):2089-2094. doi: 10.4103/jfmpc.jfmpc_248_19. PMID: 31334185; PMCID: PMC6618215.
- Narmawan, Narmawan & Syahrul, Syahrul & Erika, Kadek Ayu. (2018). THE BEHAVIOR OF FOOT CARE IN PATIENTS WITH TYPE 2 DIABETES MELLITUS: APPLYING THE THEORY OF PLANNED BEHAVIOUR. Public Health of Indonesia. 4. 129-137. 10.36685/phi.v4i3.209.
- Sharoni SKA, Abdul Rahman H, Minhat HS, Shariff Ghazali S, Azman Ong MH. A self-efficacy education programme on foot self-care behaviour among older patients with diabetes in a public long-term care institution, Malaysia: a Quasi-experimental Pilot Study. BMJ Open. 2017 Jun 8;7(6):e014393. doi: 10.1136/bmjopen-2016-014393. PMID: 28600363; PMCID: PMC5623401.
- Mekonen EG, Gebeyehu Demssie T. Preventive foot self-care practice and associated factors among diabetic patients attending the university of Gondar comprehensive specialized referral hospital, Northwest Ethiopia, 2021. BMC Endocr Disord. 2022 May 11;22(1):124. doi: 10.1186/s12902-022-01044-0. PMID: 35546665; PMCID: PMC9097232.
- Ammar I, Jude E, Katia Langton FR, et al. (2017). International Diabetes Federation (IDF): Clinical Practice Recommendation on the Diabetic Foot: A Guide for Healthcare Professionals. Vol. 127; 2017. Doi:10.1016/j.diabres.2017.04.013. Accessed 18/01/2023.
- Armstrong DG, Boulton AJM, Bus SA. Diabetic Foot Ulcers and Their Recurrence. N Engl J Med. 2017 Jun 15;376(24):2367-2375. doi: 10.1056/NEJMra1615439. PMID: 28614678.
- van Netten JJ, Price PE, Lavery LA, Monteiro-Soares M, Rasmussen A, Jubiz Y, Bus SA; International Working Group on the Diabetic Foot. Prevention of foot ulcers in the at-risk patient with diabetes: a systematic review. Diabetes Metab Res Rev. 2016 Jan;32 Suppl 1:84-98. doi: 10.1002/dmrr.2701. PMID: 26340966.
- Ong JJ, Azmil SS, Kang CS, Lim SF, Ooi GC, Patel A, Mawardi M. Foot care knowledge and self-care practices among diabetic patients in Penang: A primary care study. Med J Malaysia. 2022 Mar;77(2):224-231. PMID: 35338631.
- Wendling S, Beadle V. The relationship between self-efficacy and diabetic foot self-care. J Clin Transl Endocrinol. 2015 Jan 27;2(1):37-41. doi: 10.1016/j.jcte.2015.01.001. PMID: 29159107; PMCID: PMC5685009.
![]() This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
The Impact of Nurse Manager Leadership Styles on Nurse Job Satisfaction: A CrossSectional Study at Hamad Medical Corporation, Qatar
Abdelbasset Ghalgaoui 1, 2 *, Nabil Ajjel 1, Maha Mohamed Marzouk Ahmed 1,
Osama Helmi Mohammad Subih 1, Mehdi Halleb 1
1. Department of Nursing, Hamad Medical Corporation (HMC), Doha, Qatar.
2. Institut Universitaire de Formation des Cadres (INUFOCAD), Port-au-Prince, Haiti.
* Corresponding author: Abdelbasset Ghalgaoui, Graduate Registered Nurse, Department of Nursing, Hamad Medical Corporation (HMC), Doha, Qatar. PhD Student in Education and Governance, Institut Universitaire de Formation des Cadres (INUFOCAD), Port-au-Prince, Haiti. Email: ghalgaouiabdelbasset@gmail.com
Cite this article
ABSTRACT
Introduction: Job satisfaction is a key determinant of nurse retention, morale, and quality of care. Leadership styles directly shape satisfaction by influencing recognition, autonomy, and support within clinical environments. In Qatar’s multicultural nursing workforce, understanding these dynamics is critical.
Objective: This study investigated the relationship between nurse manager leadership styles and nurses’ job satisfaction at Hamad Medical Corporation (HMC).
Method: A cross-sectional survey was conducted with 980 registered nurses recruited through simple random sampling. Data were collected using a structured online questionnaire incorporating socio-demographic data, the Multifactor Leadership Questionnaire (MLQ-5X), and the Minnesota Satisfaction Questionnaire – Short Form (MSQ). Descriptive and inferential statistics, including Spearman’s correlation, Mann–Whitney U, and Kruskal–Wallis H tests, were employed.
Results: The sample was predominantly female (72.1%) and expatriate, with Indian (42.1%) and Filipino (33.9%) nurses forming the largest groups. Transactional leadership (mean = 2.57) was more common than transformational leadership (mean = 2.20). Overall satisfaction levels were moderate. Transformational leadership showed a strong positive correlation with both intrinsic satisfaction (rho = 0.66, p < 0.001) and extrinsic satisfaction (rho = 0.79, p < 0.001), yielding an overall significant relationship with total job satisfaction (rho = 0.73, p < 0.001).Transactional leadership demonstrated a weak to moderate positive correlation (rho = 0.30, p < 0.001), while passive-avoidant leadership showed no meaningful association with satisfaction (rho = 0.06, p = 0.041).
Conclusion: Transformational leadership has the strongest influence on job satisfaction, while transactional and passive-avoidant styles limit long-term fulfillment. Enhancing transformational leadership at HMC may improve satisfaction, retention, and workforce stability.
Keywords: Leadership, Nurses, Job Satisfaction, Retention
INTRODUCTION
In the dynamic and demanding field of healthcare, nurses occupy a vital role. They are not merely caregivers but the backbone of healthcare institutions, providing essential treatment, compassion, and expertise to patients in need. The satisfaction of nurses is a crucial element that directly impacts their well-being, retention, and ultimately the quality of care delivered to patients.
Leadership plays a central role in shaping the experiences of nurses within healthcare organizations. Nurse managers, through their leadership styles, have the ability to empower their teams, foster a supportive work culture, and contribute to overall job satisfaction. Effective leadership can inspire motivation, strengthen commitment, and enhance the professional fulfillment of nurses. Conversely, ineffective or unsupportive leadership can create dissatisfaction, burnout, and even intentions to leave the profession, posing challenges for healthcare quality and staff retention[1,2].
Avolio and Bass have identified three primary leadership styles: transformational, transactional, and passive-avoidant (laissez-faire). Transformational leaders inspire and motivate followers toward shared goals, encouraging innovation and personal growth. Transactional leaders emphasize structure, rewards, and performance management. Passive-avoidant leaders, however, tend to disengage, avoiding intervention and decision-making, often resulting in reduced productivity and workplace dissatisfaction[3,4]. Nurse managers often apply one or a combination of these styles, with varying outcomes on nurse satisfaction.
Studies conducted in Qatar and the surrounding region highlight the prevalence and influence of leadership styles in healthcare. For example, transformational leadership has been shown to be the most commonly practiced style among nursing leaders in Qatar[5]. Additionally, research in Saudi Arabia and Bahrain has demonstrated that transformational and transactional leadership approaches are positively linked to nurses’ satisfaction, commitment, and reduced turnover intentions[6,7]. These findings reinforce the importance of leadership style as a determinant of nurse satisfaction in Middle Eastern healthcare settings, including at HMC.
The relevance of this issue at HMC is further underscored by local research showing that a significant proportion of nurses and healthcare workers have reported dissatisfaction, stress, and turnover intentions, particularly during and after the COVID-19 pandemic[8]. Such challenges highlight the pressing need to evaluate how leadership styles adopted by nurse managers influence nurses’ satisfaction within HMC.
Therefore, this study seeks to explore the perceptions of nurses regarding their managers’ leadership styles and to examine the relationship between these leadership approaches and nurses’ job satisfaction. Understanding this relationship is crucial to developing effective leadership strategies that enhance nurse satisfaction, reduce turnover, and improve the overall quality of patient care. Addressing this gap is essential to achieving Qatar’s National Health Strategy goals for workforce sustainability and excellence in healthcare delivery.
Objectives
This study aimed to describe nurses’ perceptions of their managers’ leadership styles, assess their job satisfaction levels, and examine associations between leadership approaches and satisfaction dimensions.
MATERIALS AND METHODS
Type and Classification of Study
This study employed a quantitative, cross-sectional research design to examine the relationship between nurse manager leadership styles and nurses' job satisfaction at HMC, Qatar.
Comparisons and Predictors of Interest
The primary focus was on comparing various nurse manager leadership styles and their respective impacts on staff nurses’ job satisfaction.
Study Duration
The study was conducted over a period of approximately four months, from November 5, 2024, to March 1, 2025.
Sample Size Justification
To ensure reliability and representativeness of the findings, a sample size calculation was conducted based on a population of approximately 12,000 nurses. Using a 95% confidence level and a ±3% margin of error, an estimate minimal sample size of 1067 nurses was determined to be appropriate. The sample size was calculated using Cochran’s formula:
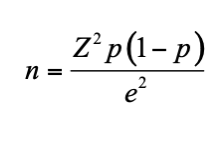
where Z = 1.96, p = 0.5, e = 0.03. Since the estimate minimal sample size is large and >5% compared to the population from which it is obtained (12,000), the sample size can be reduced to 980 nurses.
The value p = 0.5 was chosen to provide the most conservative estimate and ensure adequate sample size in the absence of prior data, while a ±3% margin of error was selected to achieve high precision and reliable representativeness of the study findings.
Study Population and Setting
The study population comprised registered nurses working in various departments across Hamad Medical Corporation (HMC), Qatar. Participants were selected through a simple random sampling method. The sampling frame included the complete list of licensed nurses at HMC, each assigned a unique identification number. Using Microsoft Excel’s RAND function, the list was randomly ordered to facilitate unbiased selection.
To account for an anticipated non-response rate, the initial calculated sample of 980 nurses determined based on a 95% confidence level and a ±3% margin of error for a population of approximately 12,000 nurses was increased by 245, resulting in a total of 1,225 nurses being invited to participate. Questionnaires were distributed via official HMC email accounts, and 980 completed responses were obtained, forming the final study sample. This strategy ensured a representative sample across different hospitals and nursing units within HMC.
The study was carried out exclusively within HMC facilities.
Inclusion Criteria
- Registered nurses currently employed at HMC.
- Nurses who voluntarily consented to participate.
- Nurses with a minimum of six months of experience at HMC to ensure familiarity with the organizational culture and leadership practices.
Exclusion Criteria
- Nurses on leave or absent during data collection.
- Nurses in managerial or supervisory roles.
- Contract or temporary nurses.
Data Collection
Data were collected via structured online questionnaires distributed through Google Forms. The survey instruments covered the following areas:
- Socio-demographic Data
Collected information included age, gender, nationality, years of nursing experience, tenure at HMC, education level, hospital, and department. Age was categorized into three groups (≤30 years, 31–45 years, and >45 years) to reflect early, mid-, and late-career stages. Similarly, years of nursing experience and years of experience within HMC were grouped as ≤5 years, 6–15 years, and >15 years to allow meaningful comparisons between groups and ensure adequate sample sizes for statistical analysis.
- Multifactor Leadership Questionnaire (MLQ-5X)
This 45-item tool assessed leadership styles (transformational, transactional, and laissez-faire) across dimensions such as inspirational motivation, intellectual stimulation, and contingent reward. Responses were recorded on a 5-point Likert scale (0 = "Not at all" to 4 = "Frequently, if not always") [9]. Items were grouped into their respective leadership dimensions using the MLQ scoring key. For each dimension, a mean score was calculated by summing the responses to the items composing that scale and dividing by the number of valid responses. All leadership style subscales consisted of four items each. Blank or missing responses were excluded from the calculations. Higher mean scores indicated more frequent exhibition of the corresponding leadership behaviors. Leadership dimensions were analyzed as continuous variables rather than categorizing leaders into a single leadership style.
The tool demonstrated strong reliability, with Cronbach’s alpha ranging from 0.70 to 0.90.
- Minnesota Satisfaction Questionnaire (Short Form)
This 20-item scale measured job satisfaction across facets such as supervision, pay, promotion, coworkers, and communication. Responses ranged from 1 ("Not Satisfied") to 5 ("Extremely Satisfied")[10]. The instrument showed good internal consistency, with a Cronbach’s alpha range of 0.70 to 0.90.
Primary and Secondary Outcomes
- Primary Outcomes: Nurses’ job satisfaction.
- Secondary Outcome: The relationship between nurse manager leadership styles and the three primary outcomes.
Statistical analysis
Descriptive statistics were used to summarize participant characteristics and key variables such as means, standard deviations, medians, ranges, and percentages. Normality of continuous variables was assessed using the Shapiro–Wilk test, which indicated non-normal distribution (p < 0.05). Therefore, non-parametric statistical tests were applied, including Mann–Whitney U and Kruskal–Wallis H for group comparisons.
Correlation between leadership styles and job satisfaction was analyzed using Spearman’s rank correlation coefficient (ρ) due to non-normal distribution. The statistical tests with p-value < 0.05 were considered significant. All analyses were performed using SPSS-26 software.
Ethical Approval and Informed Consent Statement
Informed consent was obtained from all study participants. The purpose, procedures, and voluntary nature of the study were explained through official internal communication channels via HMC e-mail. Participants provided electronic consent after having at least two months to review the study information before deciding to participate. Only registered nurses employed at HMC who met the inclusion criteria were enrolled. No financial incentives were offered for participation.
The study was approved by the Medical Research Center (MRC) – Local Ethics Committee of Hamad Medical Corporation, Qatar (Protocol No. MRC-01-24-356), with approval granted on 15/08/2024, and was conducted in accordance with the principles of the Declaration of Helsinki and Good Clinical Practice (GCP), as well as the regulations of the Ministry of Public Health (MoPH), Qatar. Participant anonymity and data confidentiality were strictly maintained throughout the study.
RESULTS
Demographic and Professional Characteristics
The study sample of 980 nurses demonstrated a pronounced gender imbalance, with females constituting nearly three-quarters of the workforce (Table 1). Marriage was the predominant status, and Indian and Filipino nationals together comprised more than three-quarters of the participants, highlighting the concentration of the workforce among specific nationalities. Age distribution indicated that the majority of nurses were mid-career professionals aged 30–45 years (67.04%), whereas younger nurses (≤30 years) formed a small minority (6.53%).
|
Characteristics |
Categories |
Frequency (n) |
Percent (%) |
Mean± SD |
|
Gender |
Male |
273 |
27.86 |
|
|
Female |
707 |
72.14 |
||
|
Marital Status |
Single |
138 |
14.08 |
|
|
Married |
820 |
83.67 |
||
|
Widowed |
8 |
0.82 |
||
|
Separated / Divorced |
14 |
1.43 |
||
|
Nationality |
Cuban |
36 |
3.67 |
|
|
Egyptian |
16 |
1.63 |
||
|
Filipino |
332 |
33.88 |
||
|
Indian |
413 |
42.14 |
||
|
Iranian |
3 |
0.31 |
||
|
Jordanian |
64 |
6.53 |
||
|
Lebanese |
5 |
0.51 |
||
|
Palestinian |
8 |
0.82 |
||
|
Somali |
3 |
0.31 |
||
|
Sudanese |
51 |
5.20 |
||
|
Tunisian |
49 |
5.00 |
||
|
Age (years) |
≤30 years |
64 |
6.53 |
40.40 ± 7.89 |
|
]30-45] |
657 |
67.04 |
||
|
> 45 |
259 |
26.43 |
Table 1. Demographic Characteristics (N=980)
Hospital and departmental distribution demonstrated a concentration of staff in a limited number of facilities and clinical areas. Hamad General Hospital employed the largest share (27.55%), followed by Rumailah (11.63%), Al Wakra (11.43%), and the Women’s Wellness & Research Center (8.16%). The Surgical and Medical departments collectively accounted for more than 65% of participants, whereas Critical Care, Emergency, and Outpatient/ Ambulatory units had smaller staff representation.
These demographic patterns suggest that the HMC nursing workforce is highly experienced and predominantly composed of expatriate professionals, highlighting the importance of culturally adaptive leadership strategies.
|
Characteristics |
Categories |
Frequency (n) |
Percent (%) |
Mean± SD |
|
Years of experience as a nurse |
≤5 years |
21 |
2.14 |
16.85 ± 7.14 |
|
]5-15] |
532 |
54.29 |
||
|
> 15 |
427 |
43.57 |
||
|
Years of experience in HMC |
≤5 years |
360 |
36.73 |
9.93 ± 7.54 |
|
]5-15] |
369 |
37.65 |
||
|
> 15 |
251 |
25.61 |
||
|
Educational background |
Diploma |
139 |
14.18 |
|
|
Bachelor’s degree |
751 |
76.63 |
||
|
Master’s degree |
90 |
9.18 |
||
|
Hospital |
Hamad General Hospital |
270 |
27.55 |
|
|
Ambulatory Care Center |
58 |
5.92 |
||
|
Qatar Rehabilitation Institute |
17 |
1.73 |
||
|
NCCCR |
19 |
1.94 |
||
|
Mental Health Service |
48 |
4.90 |
||
|
Communicable Disease Center |
15 |
1.53 |
||
|
Al Khor Hospital |
72 |
7.35 |
||
|
Rumailah Hospital |
114 |
11.63 |
||
|
Al Wakra Hospital |
112 |
11.43 |
||
|
Hazm Mebaireek General Hospital |
64 |
6.53 |
||
|
Aisha Bint Hamad Al Attiyah Hospital |
63 |
6.43 |
||
|
The Cuban Hospital |
17 |
1.73 |
||
|
Women's Wellness and Research Center |
80 |
8.16 |
||
|
Heart Hospital |
31 |
3.16 |
||
|
Department |
Critical Care / Emergency Services |
220 |
22.45 |
|
|
Medical Department |
296 |
30.20 |
||
|
Surgical Department |
348 |
35.51 |
||
|
Outpatient (OPD) and Ambulatory Services |
116 |
11.84 |
Table 2. Professional Characteristics (N=980)
Nurse Manager Leadership Styles
The analysis of nurse manager leadership styles revealed that transactional leadership was more prominent (mean = 2.57, SD = 0.85; Q1 = 2.00, Q3 = 3.12) compared to transformational leadership (mean = 2.20, SD = 1.05; Q1 = 1.55, Q3 = 3.00). This suggests that managers primarily use structured management approaches, emphasizing performance-based rewards and active monitoring (Table 3).
|
|
Minimum |
Maximum |
Mean |
S D |
Median |
Q1 |
Q3 |
|
Idealized Attributes or Idealized Influence (Attributes) |
0.00 |
4.00 |
2.19 |
1.14 |
2.25 |
1.50 |
3.00 |
|
Idealized Behaviors or Idealized Influence (Behaviors) |
0.00 |
4.00 |
2.35 |
1.15 |
2.50 |
1.75 |
3.25 |
|
Inspirational Motivation |
0.00 |
4.00 |
2.34 |
1.22 |
2.50 |
1.50 |
3.25 |
|
Intellectual Stimulation |
0.00 |
4.00 |
2.21 |
1.11 |
2.25 |
1.50 |
3.00 |
|
Individual Consideration |
0.00 |
4.00 |
1.94 |
0.96 |
2.00 |
1.25 |
2.75 |
|
Transformational |
0.00 |
4.00 |
2.20 |
1.05 |
2.35 |
1.55 |
3.00 |
|
Contingent Reward |
0.00 |
4.00 |
2.56 |
1.05 |
2.75 |
2.00 |
3.25 |
|
Mgmt by Exception (Active) |
0.00 |
4.00 |
2.58 |
0.98 |
2.75 |
2.00 |
3.25 |
|
Transactional |
0.25 |
4.00 |
2.57 |
0.85 |
2.62 |
2.00 |
3.12 |
|
Mgmt by Exception (Passive) |
0.00 |
4.00 |
1.55 |
1.01 |
1.25 |
0.75 |
2.25 |
|
Laissez-Faire |
0.00 |
4.00 |
1.43 |
1.05 |
1.25 |
0.50 |
2.25 |
|
Passive Avoidant |
0.00 |
4.00 |
1.49 |
0.97 |
1.37 |
0.75 |
2.12 |
|
Extra Effort |
0.00 |
4.00 |
2.17 |
1.20 |
2.33 |
1.00 |
3.00 |
|
Effectiveness |
0.00 |
4.00 |
2.25 |
1.22 |
2.50 |
1.00 |
3.00 |
|
Satisfaction |
0.00 |
4.00 |
2.28 |
1.31 |
2.50 |
1.00 |
3.00 |
|
Outcomes of Leadership |
0.00 |
400 |
2.23 |
1.20 |
2.42 |
1.05 |
3.16 |
Table 3. Nurse Manager Leadership Styles.
Within the transactional domain, contingent reward (mean = 2.56, SD = 1.05; Q1 = 2.00, Q3 = 3.25) and management by exception active (mean = 2.58, SD = 0.98; Q1 = 2.00, Q3 = 3.25) were the most utilized strategies.
Among transformational leadership subscales, idealized influence behaviors (mean = 2.35, SD = 1.15; Q1 = 1.75, Q3 = 3.25) scored highest, indicating that some leaders act as strong role models. Conversely, individual consideration (mean = 1.94, SD = 0.96; Q1 = 1.25, Q3 = 2.75) was lowest, suggesting limited mentorship or personalized support for staff.
Passive-avoidant leadership had the lowest overall scores (mean = 1.49, SD = 0.97; Q1 = 0.75, Q3 = 2.12), particularly laissez-faire leadership (mean = 1.43, SD = 1.05; Q1 = 0.50, Q3 = 2.25), showing that managers generally remain engaged and avoid ignoring decision-making responsibilities. Management by exception passive (mean = 1.55, SD = 1.01; Q1 = 0.75, Q3 = 2.25) indicated occasional reactive behaviors. Leadership outcomes were moderate, with effectiveness (mean = 2.25, SD = 1.22; Q1 = 1.00, Q3 = 3.00) and satisfaction (mean = 2.28, SD = 1.31; Q1 = 1.00, Q3 = 3.00) reflecting satisfactory performance from the staff perspective.
The dominance of transactional leadership may reflect the organizational focus on compliance and efficiency rather than on empowerment or innovation.
Nurses' Satisfaction
The results indicate that nurses experience moderate job satisfaction across both intrinsic and extrinsic dimensions as well as in the overall satisfaction measured by the Minnesota Satisfaction Questionnaire (MSQ) - Short Form. For intrinsic satisfaction, 57.55% of participants fall into the average category (Table 4), while 20.41% report low satisfaction, with a mean score of 2.93 ± 0.93 (Q1 = 2.00, Q3 = 2.00). The quartile values indicate that most respondents cluster tightly around the lower end of the moderate range, suggesting limited variability in perceived intrinsic motivators. In contrast, extrinsic satisfaction shows that 57.14% of respondents are moderately satisfied, but a slightly higher percentage (22.86%) report low satisfaction, with a mean score of 2.74 ± 1.01 (Q1 = 2.00, Q3 = 2.00). Similar to intrinsic satisfaction, the Q1 and Q3 values suggest that extrinsic satisfaction is concentrated at the lower boundary of moderate satisfaction, reinforcing the need for improvements in external factors such as pay and recognition.
Regarding overall satisfaction (MSQ), 71.84% of respondents are in the average category, 8.57% report low satisfaction, and 19.59% report high satisfaction, with a mean score of 2.87 ± 0.94 (Q1 = 2.00, Q3 = 2.00). The quartile distribution again shows that the majority of nurses fall at the lower end of the moderate satisfaction range. The moderate satisfaction levels indicate room for improvement, particularly in extrinsic factors such as pay and recognition.
|
|
Range |
Frequency |
Percent |
Min |
Max |
Mean±SD |
Median [Q1, Q3] |
|
Intrinsic Satisfaction |
Low Satisfaction |
200 |
20.41 |
1.00 |
5.00 |
2.93 (0.93) |
3.00 [2.41, 3.58] |
|
Average Satisfaction |
564 |
57.55 |
|||||
|
High Satisfaction |
216 |
22.04 |
|||||
|
Extrinsic Satisfaction |
Low Satisfaction |
224 |
22.86 |
1.00 |
5.00 |
2.74 (1.01) |
2.83 [2.00, 3.50] |
|
Average Satisfaction |
560 |
57.14 |
|||||
|
High Satisfaction |
196 |
20.00 |
|||||
|
General Satisfaction of MSQ |
Low level of satisfaction |
84 |
8.57 |
1.00 |
5.00 |
2.87 (0.94) |
2.95 [2.25, 3.55] |
|
Average level of satisfaction |
704 |
71.84 |
|||||
|
High level of satisfaction |
192 |
19.59 |
Table 4. Nurses' Satisfaction
Comparison of Socio-demographic Characteristics and Their Association with Nurses' Satisfaction
In Table 5, female nurses reported significantly higher job satisfaction than male nurses (mean rank: 506.43 vs 449.23, p = 0.005). Single nurses showed the highest satisfaction, followed by married and widowed nurses (550.57 vs. 473.29 vs 373.50, p = 0.006). Significant differences were observed across nationalities, with Somali nurses reporting the highest satisfaction and Cuban nurses the lowest (665.17 vs 254.44, p < 0.001). No significant differences were found by age, although nurses aged ≤30 years had slightly higher satisfaction than those >45 years and those aged 30–45 years (524.38 vs 513.45 vs 478.15, p = 0.144). Similarly, years of nursing experience showed no significant differences, but nurses with ≤5 years of experience reported higher satisfaction than those with >15 years or 5–15 years (589.64 vs 494.45 vs. 483.42, p = 0.224).
Years of experience within HMC was significantly associated with satisfaction, with nurses having >15 years reporting the highest and those with 5–15 years reporting the lowest satisfaction (537.60 vs 422.53, p < 0.001).
|
Characteristics |
Categories |
Mean Rank |
Statistic |
p-value (Test) |
|
Gender |
Male |
449.23 |
85239.5 |
0.005(MW)* |
|
Female |
506.43 |
|||
|
Marital Status |
Single |
550.57 |
10.32 |
0.006(KW)* |
|
Married |
473.29 |
|||
|
Widowed |
373.50 |
|||
|
Nationality |
Cuban |
254.44 |
35.18 |
< 0.001(KW)* |
|
Egyptian |
375.50 |
|||
|
Filipino |
494.46 |
|||
|
Indian |
502.89 |
|||
|
Iranian |
604.50 |
|||
|
Jordanian |
543.19 |
|||
|
Lebanese |
598.90 |
|||
|
Palestinian |
515.75 |
|||
|
Somali |
665.17 |
|||
|
Sudanese |
442.23 |
|||
|
Tunisian |
518.79 |
|||
|
Age (years) |
≤30 years |
524.38 |
3.87 |
0.144(KW) |
|
]30-45] |
478.15 |
|||
|
> 45 |
513.45 |
|||
|
Years of experience as a nurse |
≤5 years |
589.64 |
2.99 |
0.224(KW) |
|
]5-15] |
483.42 |
|||
|
> 15 |
494.45 |
|||
|
Years of experience in HMC
|
≤5 years |
527.33 |
34.35 |
< 0.001(KW)* |
|
]5-15] |
422.53 |
|||
|
> 15 |
537.60 |
|||
|
Educational background |
Diploma |
529.18 |
11.51 |
0.003(KW)* |
|
Bachelor’s degree |
474.27 |
|||
|
Master’s degree |
566.21 |
|||
|
Hospital |
Hamad General Hospital |
515.00 |
52.14 |
< 0.001(KW)* |
|
Al Khor Hospital |
378.97 |
|||
|
Rumailah Hospital |
503.45 |
|||
|
Al Wakra Hospital |
479.68 |
|||
|
Hazm Mebaireek General Hospital |
505.44 |
|||
|
Aisha Bint Hamad Al Attiyah Hospital |
445.29 |
|||
|
The Cuban Hospital |
280.97 |
|||
|
Women's Wellness and Research Center |
536.80 |
|||
|
Heart Hospital |
594.37 |
|||
|
Ambulatory Care Center |
525.71 |
|||
|
Qatar Rehabilitation Institute |
607.68 |
|||
|
NCCCR |
624.71 |
|||
|
Mental Health Service |
343.33 |
|||
|
Communicable Disease Center |
501.30 |
|||
|
Department |
Critical Care / Emergency Services |
529.34 |
35.339 |
< 0.001(KW)* |
|
Medical Department |
430.85 |
|||
|
Surgical Department |
479.99 |
|||
|
Outpatient (OPD) and Ambulatory Services |
600.57 |
Note: MW = Mann–Whitney U test; KW = Kruskal–Wallis H test; *p < 0.05 indicates statistical significance.
Table 5. Comparison of Socio-demographic Characteristics and Their Association with Nurses' Satisfaction.
Educational background also influenced satisfaction, with nurses holding a Master’s degree reporting the highest satisfaction, followed by diploma and Bachelor’s degree holders (566.21 vs 529.18 vs. 474.27, p = 0.003). Job satisfaction differed significantly across hospitals, with QRI reporting the highest and ABAH the lowest (624.71 vs 280.97, p < 0.001). Finally, departmental differences were significant, with Outpatient (OPD) and Ambulatory Services showing the highest satisfaction and the Medical Department the lowest (600.57 vs 430.85, p < 0.001).
Correlation between Nurse Manager Leadership Styles and Nurses’ Satisfaction
The analysis reveals distinct relationships between leadership styles and job satisfaction dimensions (Table 6).
|
Intrinsic Satisfaction |
Extrinsic Satisfaction |
Minnesota Satisfaction Questionnaire (Short Form) |
||
|
Transformational
|
Spearman Coefficient (rho) |
0.66 |
0.79 |
0.73 |
|
p-value |
< 0.001* |
< 0.001* |
< 0.001* |
|
|
Transactional
|
Spearman Coefficient (rho) |
0.27 |
0.33 |
0.30 |
|
p-value |
< 0.001* |
< 0.001* |
< 0.001* |
|
|
Passive Avoidant
|
Spearman Coefficient (rho) |
0.08 |
0.04 |
0.06 |
|
p-value |
0.007* |
0.142 |
0.041* |
|
Note: *p < 0.05 indicates statistical significance.
Table 6. Correlation between Nurse Manager Leadership Styles and Nurses’ Satisfaction.
Transformational leadership shows the strongest positive correlations with all forms of satisfaction: intrinsic satisfaction (rho = 0.66, p < 0.001), extrinsic satisfaction (rho = 0.79, p < 0.001), and overall job satisfaction measured by the Minnesota Satisfaction Questionnaire (MSQ) (rho = 0.73, p < 0.001). This suggests that employees who perceive their leaders as inspiring, supportive, and visionary tend to experience higher satisfaction both from the work itself and from external rewards.
Transactional leadership also shows positive but more moderate correlations: intrinsic satisfaction (rho = 0.27, p < 0.001), extrinsic satisfaction (rho = 0.33, p < 0.001), and overall satisfaction (rho = 0.30, p < 0.001). This implies that while reward-based leadership influences job satisfaction, its impact is less pronounced than that of transformational leadership, particularly affecting extrinsic satisfaction. In contrast, passive-avoidant leadership has minimal associations with job satisfaction. The correlations are very weak for intrinsic satisfaction (rho = 0.08, p = 0.007) and overall satisfaction (rho = 0.065, p = 0.041), and non-significant for extrinsic satisfaction (rho = 0.04, p = 0.142). This indicates that passive leadership, marked by inaction and avoidance of responsibility, has little to no effect on employee satisfaction.
Overall, these findings highlight the significant role of transformational leadership in fostering job satisfaction, while transactional leadership has a moderate influence, and passive-avoidant leadership remains largely ineffective. These results confirm that transformational leadership is the most powerful predictor of nurse satisfaction, emphasizing the need for leadership development programs at HMC
DISCUSSION
Demographic and Professional Characteristics
The study sample predominantly comprised female nurses (72.14%), reflecting global trends in nursing gender distribution. The underrepresentation of males (27.86%) highlights ongoing gender disparities in the profession, which may influence workplace dynamics and care delivery. The high proportion of married participants (83.67%) suggests a stable workforce, though potential stressors related to work-life balance warrant consideration. The dominance of Indian (42.14%) and Filipino (33.88%) nationalities aligns with Qatar’s reliance on expatriate healthcare workers, raising questions about cultural adaptation and retention strategies. The mean age of 40.40 years and extensive experience (16.85 ± 7.14 years), indicate a mature, seasoned workforce. However, the low representation of nurses with ≤5 years of experience (2.14%) may signal challenges in recruiting younger professionals. The predominance of Bachelor’s degrees (76.63%) reflects standardization in nursing education, yet the limited advanced degrees (9.18%) suggests opportunities for career development. The concentration of nurses in surgical and medical departments (65.71%) underscores the demand for acute care expertise, while lower representation in specialized units (e.g., Communicable Disease Center) may reflect niche-staffing needs.
Nurse Manager Leadership Styles
The predominance of transactional leadership (mean = 2.57) over transformational styles (mean = 2.20), while passive-avoidant leadership was minimal overall (mean = 1.49) suggests a managerial focus on structured, compliance-driven approaches in this healthcare setting. The reliance on contingent rewards (mean = 2.56) and active monitoring (mean = 2.58) aligns with environments prioritizing task completion over innovation, which may reflect high-pressure clinical demands requiring strict adherence to protocols. However, the low emphasis on individual consideration (mean = 1.94) a core transformational trait indicates missed opportunities for personalized mentorship and emotional support, factors critical for nurse retention and job satisfaction. The moderate to low use of management by exception passive (mean = 1.55) suggests some leaders delay addressing issues until problems escalate, potentially eroding trust. These findings mirror studies where transactional leadership ensures baseline efficiency but fails to inspire long-term commitment [3]. The moderate effectiveness (mean = 2.25) and satisfaction (mean = 2.28) scores further underscore the limitations of overly transactional approaches in fostering intrinsic motivation.
Similar patterns have been observed in studies conducted across the Middle East. In this study, transactional leadership dominates, while other studies highlight differences between transformational and transactional leadership styles in healthcare settings. Passive-avoidant leadership remains very rare. A study conducted in Jordan found that respondents perceived transactional leadership as the most prevalent style among their nurse managers, followed by transformational leadership, with passive-avoidant leadership being the least common [11]. Conversely, two studies conducted in Saudi Arabia reported that transformational leadership was the most dominant style [12,13].
Nurses' Satisfaction
Moderate intrinsic (mean = 2.93) and extrinsic (mean = 2.74) satisfaction scores reveal unmet needs in both personal fulfillment and external rewards. The 20.41% reporting low intrinsic satisfaction suggests gaps in professional growth opportunities, such as limited access to training or leadership roles. Extrinsic dissatisfaction (22.86% low satisfaction) may stem from inflexible schedules, inadequate compensation, or insufficient recognition issues exacerbated by transactional leadership’s focus on extrinsic rewards.
In the same regional context, a study conducted in Saudi Arabia also found generally low levels of job satisfaction [14]. In contrast, a study in a public hospital in Poland using the same Minnesota Satisfaction Questionnaire (MSQ) reported higher satisfaction scores, ranging from 3.05 to 3.43, indicating a higher overall level of job satisfaction. In that study, dimensions such as recognition, independence, and working conditions were rated more favorably, and overall satisfaction with work and life was significantly higher [15]. These differences may reflect organizational or leadership factors, such as limited development opportunities or reliance on transactional leadership in our context. Enhancing training access, recognition, and flexibility may help improve satisfaction and address these gaps.
Comparison of Socio-demographic Characteristics and Their Association with Nurses' Satisfaction
Job satisfaction disparities highlight systemic inequities. Females reported higher satisfaction than males (p = 0.005), potentially due to alignment with societal caregiving roles or workplace inclusivity efforts. A study conducted in Poland within a similar context also found a relationship between gender and job satisfaction [15]. Single nurses (mean rank = 550.57) were more satisfied than married or widowed peers, possibly due to fewer work-life conflicts. Somali nurses (mean rank = 665.17) reported the highest satisfaction, while Tunisians (mean rank = 49) expressed profound dissatisfaction, underscoring the impact of cultural integration and institutional support. A cross‐sectional survey in Saudi Arabia found significant associations between nationality and lower job satisfaction, particularly when orientation and language support were lacking[16]. Younger nurses (≤30 years) and those with ≤5 years of experience showed higher satisfaction, suggesting optimism or alignment with early-career expectations. Nurses with >15 years at HMC were more satisfied (p < 0.001), likely due to career stability or leadership roles. Master’s-degree or more holders (mean rank = 566.21) reported greater satisfaction than diploma and bachelor nurses, emphasizing the role of education in professional fulfillment. Hospitals like QRI (mean rank = 624.71) and outpatient departments (mean rank = 600.57) scored highly, possibly due to manageable workloads or patient interaction. Addressing these variations requires culturally sensitive policies and career development pathways. A meta‐analysis study reported that the negative impact of nurse burnout on outcomes was not moderated by age, sex, or experience implying demographic factors alone may not drive overall well-being in broader contexts[17].
Correlation between Nurse Manager Leadership Styles and Nurses’ Satisfaction
Transformational leadership’s exceptionally strong correlation with overall satisfaction (rho = 0.73, p < 0.001), and especially extrinsic satisfaction (rho = 0.79, p < 0.001), is consistent with Specchia et al.’s systematic review of 12 studies, which identified 9 out of 9 studies showing a positive relationship between transformational behaviors and nurses’ job satisfaction[18]. Gebreheat et al.’s integrative review similarly found that 17 out of 17 studies reported a positive impact of transformational leadership on nurses’ job satisfaction[19]. That It is likely due to its emphasis on recognition and shared goals.
Conversely, transactional leadership’s moderate correlation with overall satisfaction (rho = 0.30, p < 0.001), intrinsic satisfaction (rho = 0.27, p < 0.001) and extrinsic satisfaction (rho = 0.33, p < 0.001) mirrors Specchia et al.’s finding that four studies observed positive correlations, three found no significant relationship, and one even reported a negative link between transactional behaviors and satisfaction[18]. While contingent rewards can satisfy baseline needs reflected in our moderate extrinsic coefficient, they lack the deeper emotional resonance necessary to engender long-term commitment or intrinsic fulfillment.
Finally, passive-avoidant leadership exhibited negligible associations with all satisfaction metrics (overall rho = 0.06, p = 0.041; intrinsic rho = 0.08, p = 0.007; extrinsic rho = 0.04, p = 0.142), reinforcing Specchia et al.’s observation that three studies documented a negative correlation between passive-avoidant behaviors and nurse satisfaction[18]. When managers abdicate decision-making and fail to provide feedback or recognition, role ambiguity and diminished trust arise, eroding both extrinsic perceptions (no rewards or performance guidance) and intrinsic drivers (no inspiration or support).
Recommendations
The study underscores the critical importance of nurse manager leadership styles in shaping nurses’ job satisfaction at HMC. Based on the findings, several recommendations are proposed to enhance satisfaction and overall workplace well-being.
Firstly, HMC should invest in comprehensive leadership training programs that prioritize transformational leadership development. Such programs should focus on building leaders’ ability to inspire, empower, and communicate effectively with their teams. Emphasizing qualities such as empathy, recognition, and individualized consideration can strengthen nurses’ intrinsic motivation and sense of belonging, which are key determinants of satisfaction.
Secondly, the organization should foster open communication and participatory decision-making. When nurses are given opportunities to contribute to clinical and administrative decisions, their sense of value and autonomy increases two crucial components of job satisfaction. Leadership practices should therefore promote a culture of inclusion, transparency, and trust across all nursing departments.
In addition, regular satisfaction assessments should be integrated into the organization’s quality improvement framework to monitor workforce morale and identify emerging concerns early. Findings from these assessments can inform policy adjustments, recognition systems, and workload management strategies. Finally, HMC should establish mentorship and peer-support programs where experienced leaders and senior nurses can provide guidance and career support, further enhancing job satisfaction and retention among younger or less experienced staff.
Strengths and limitations of the study
This study is characterized by several notable strengths that enhance its credibility and contribution to nursing leadership research. A major strength lies in its large and diverse sample (N = 980), which ensures representativeness across multiple hospitals and departments within HMC. The use of validated instruments, including the Multifactor Leadership Questionnaire (MLQ-5X) for assessing leadership and the Minnesota Satisfaction Questionnaire (MSQ) – Short Form for measuring job satisfaction, ensures psychometric reliability and international comparability.
Furthermore, the study employs rigorous statistical techniques such as Spearman’s correlation, Mann–Whitney U, and Kruskal–Wallis H tests to analyze associations between leadership styles and satisfaction outcomes. This comprehensive analytical framework provides robust evidence of the differential effects of transformational, transactional, and passive-avoidant leadership on satisfaction levels. Finally, by situating the research within Qatar’s multicultural healthcare context, the study contributes original insights into how leadership behaviors influence satisfaction in a diverse, expatriate workforce a perspective that is often underrepresented in global nursing literature.
Despite its valuable findings, several limitations must be acknowledged. The cross-sectional design restricts causal inference, meaning that while correlations between leadership styles and satisfaction are established, it cannot be conclusively stated that leadership style directly causes changes in satisfaction levels. Longitudinal studies would be needed to track the evolution of satisfaction over time in response to leadership interventions. Additionally, the use of self-administered questionnaires introduces potential response bias, as participants may have provided socially desirable answers rather than fully objective reflections of their experiences. Common-method bias may also have occurred because both leadership styles and job satisfaction were measured through self-report instruments administered in the same session. The homogeneity of the sample, composed largely of expatriate nurses, limits the generalizability of results to settings with different cultural or workforce compositions. Furthermore, the linguistic and cultural diversity of participants may have affected interpretation or understanding of questionnaire items. The study was conducted exclusively at HMC, meaning institutional factors such as policies, resources, or management structures may have influenced outcomes. Finally, there was limited control for potential confounders, as unmeasured factors such as workload, unit-specific culture, or individual personality traits may also have impacted job satisfaction.
CONCLUSION
This study provides evidence that nurse manager leadership styles significantly influence nurses’ job satisfaction at Hamad Medical Corporation (HMC). Transformational leadership emerged as the strongest positive predictor of intrinsic, extrinsic, and overall job satisfaction, suggesting that leaders who inspire, support, and engage their staff foster higher levels of professional fulfillment. Transactional leadership was associated with moderate positive effects, primarily on extrinsic satisfaction, while passive-avoidant leadership showed minimal or negligible impact on all satisfaction dimensions.
The study also identified significant variations in job satisfaction across hospitals, departments, nationalities, and educational levels, highlighting the role of organizational context and workforce diversity in shaping nurses’ experiences. These findings suggest that targeted interventions promoting transformational leadership behaviors such as mentorship, recognition, and participatory decision-making may enhance nurse satisfaction, retention, and overall workforce stability at HMC.
However, this study has limitations that should be considered when interpreting the results. The cross-sectional design prevents causal inferences, and reliance on self-reported data introduces the potential for response bias and common-method bias. Additionally, linguistic and cultural differences among participants may have influenced responses. Therefore, while the results provide valuable insights for HMC, their generalizability to other healthcare settings is limited, and further research using longitudinal or multi-site designs is recommended.
Local Ethics Committee approval
The study was approved by the Medical Research Center (MRC) – Local Ethics Committee of Hamad Medical Corporation, Qatar (Protocol No. MRC-01-24-356), with approval granted on 15/08/2024, and was conducted in accordance with the principles of the Declaration of Helsinki and Good Clinical Practice (GCP), as well as the regulations of the Ministry of Public Health (MoPH), Qatar. Participant anonymity and data confidentiality were strictly maintained throughout the study.
Conflicts of interest
This study was conducted in accordance with ethical standards. All participants provided informed consent. The authors declare no conflict of interest.
Sources of funding
This research received funding from the Medical Research Center at HMC.
Author contributions
Conception and design: Abdelbasset Ghalgaoui
Data collection: Abdelbasset Ghalgaoui
Data analysis and interpretation: Abdelbasset Ghalgaoui
Drafting of the manuscript: all authors
Critical revision of the manuscript: Abdelbasset Ghalgaoui, Nabil Ajjel
Final approval: all authors
Acknowledgements
The authors thank the staff of Hamad Medical Corporation for their collaboration.
REFERENCES
- 1. Çamveren H, Arslan Yürümezoğlu H, Kocaman G. Why do young nurses leave their organization? A qualitative descriptive study. International Nursing Review. 2020;67:519–28. https://doi.org/10.1111/inr.12633
- 2. Labrague LJ, Nwafor CE, Tsaras K. Influence of toxic and transformational leadership practices on nurses’ job satisfaction, job stress, absenteeism and turnover intention: A cross-sectional study. Journal of Nursing Management. 2020;28:1104–13. https://doi.org/10.1111/jonm.13053
- 3. Avolio B. Full Range Leadership Development. 2nd edition. Los Angeles, Calif London: SAGE Publications, Inc; 2010.
- 4. Avolio BJ, Bass BM, editors. Developing Potential Across a Full Range of Leadership TM: Cases on Transactional and Transformational Leadership. New York: Psychology Press; 2001. https://doi.org/10.4324/9781410603975
- 5. Al-Thawabiya A, Singh K, Al-Lenjawi BA, Alomari A. Leadership styles and transformational leadership skills among nurse leaders in Qatar, a cross-sectional study. Nursing Open. 2023;10:3440–6. https://doi.org/10.1002/nop2.1636
- 6. AL-Dossary RN. Leadership Style, Work Engagement and Organizational Commitment Among Nurses in Saudi Arabian Hospitals. Journal of Healthcare Leadership. Dove Medical Press; 2022;14:71–81. https://doi.org/10.2147/JHL.S365526
- 7. Pattali S, Sankar JP, Al Qahtani H, Menon N, Faizal S. Effect of leadership styles on turnover intention among staff nurses in private hospitals: the moderating effect of perceived organizational support. BMC Health Serv Res. 2024;24:199. https://doi.org/10.1186/s12913-024-10674-0
- 8. Nashwan AJ, Abujaber AA, Villar RC, Nazarene A, Al-Jabry MM, Fradelos EC. Comparing the Impact of COVID-19 on Nurses’ Turnover Intentions before and during the Pandemic in Qatar. Journal of Personalized Medicine. Multidisciplinary Digital Publishing Institute; 2021;11:456. https://doi.org/10.3390/jpm11060456
- 9. Avolio BJ, Bass BM. Multifactor leadership questionnaire: manual and sample set. Third edition. Place of publication not identified: Mind Garden, Inc.; 2004.
- 10. Weiss DJ, Dawis RV, England GW, Lofquist LH. Minnesota satisfaction questionnaire–short form. Educational and Psychological Measurement [Internet]. 1977 [cited 2025 July 1]; https://psycnet.apa.org/doiLanding?doi=10.1037%2Ft08880-000. Accessed 1 July 2025
- 11. Suliman M, Aljezawi M, Almansi S, Musa A, Alazam M, Ta’an WF. Effect of nurse managers’ leadership styles on predicted nurse turnover. Nurs Manag (Harrow). 2020;27:20–5. https://doi.org/10.7748/nm.2020.e1956
- 12. Areej Mohammed Asiri, Sabah Mahmoud Mahran, Naglaa Abdelaziz Elseesy. A study of staff nurses’ perceptions of nursing leadership styles and work engagement levels in Saudi general hospitals. International Journal of Advanced and Applied Sciences. IASE; 2023;10:55–61. https://doi.org/10.21833/ijaas.2023.01.008
- 13. Alluhaybi A, Usher K, Durkin J, Wilson A. Clinical nurse managers’ leadership styles and staff nurses’ work engagement in Saudi Arabia: A cross-sectional study. PLOS ONE. Public Library of Science; 2024;19:e0296082. https://doi.org/10.1371/journal.pone.0296082
- 14. Al Bazroun MI, Aljarameez F, Alhamza R, Ahmed GY, Alhybah F, Al Mutair A. Factors influencing job satisfaction and anticipated turnover among intensive care nurses in Saudi Arabia. British Journal of Healthcare Management. Mark Allen Group; 2023;29:1–10. https://doi.org/10.12968/bjhc.2021.0146
- 15. Tomaszewska K, Kowalczuk K, Majchrowicz B, Kłos A, Kalita K. Areas of professional life and job satisfaction of nurses. Front Public Health [Internet]. Frontiers; 2024 [cited 2025 May 13];12. https://doi.org/10.3389/fpubh.2024.1370052
- 16. Almansour H, Gobbi M, Prichard J, Ewings S. The association between nationality and nurse job satisfaction in Saudi Arabian hospitals. Int Nurs Rev. 2020;67:420–6. https://doi.org/10.1111/inr.12613
- 17. Li LZ, Yang P, Singer SJ, Pfeffer J, Mathur MB, Shanafelt T. Nurse Burnout and Patient Safety, Satisfaction, and Quality of Care. JAMA Netw Open. 2024;7:e2443059. https://doi.org/10.1001/jamanetworkopen.2024.43059
- 18. Specchia ML, Cozzolino MR, Carini E, Di Pilla A, Galletti C, Ricciardi W, et al. Leadership Styles and Nurses’ Job Satisfaction. Results of a Systematic Review. International Journal of Environmental Research and Public Health. Multidisciplinary Digital Publishing Institute; 2021;18:1552. https://doi.org/10.3390/ijerph18041552
- 19. Gebreheat G, Teame H, Costa EI. The Impact of Transformational Leadership Style on Nurses’ Job Satisfaction: An Integrative Review. SAGE Open Nursing. SAGE Publications Inc; 2023;9:23779608231197428. https://doi.org/10.1177/23779608231197428
Current state of the experience of receiving evidence-based practice education and its relationship with evidence-based practice knowledge and skills among hospital nurses: A cross-sectional questionnaire survey in Western Japan
Hideaki Furuki 1*, Nao Sonoda 1, Akiko Morimoto 1
- Graduate School of Nursing, Osaka Metropolitan University, Osaka, Japan
* Corresponding author: Hideaki Furuki, MSc, RN, PHN, Osaka Metropolitan University, Graduate School of Nursing, 1–4–3 Asahi-machi, Abeno Ward, Osaka City, Osaka 545–8585, Japan. E-mail address: s21262g@omu.ac.jp
Cite this article
ABSTRACT
Introduction: Although evidence-based practice (EBP) is a core nursing competency, little is known about the extent to which nurses are educated on the five steps of EBP, including the specific educational content within each step, in pre-licensure and in-service education, and how these educational experiences relate to their knowledge and skills.
Objectives: To examine the extent of nurses’ experience of receiving specific educational content related to each step of EBP in pre-licensure and in-service education, and to evaluate the associations between these experiences and EBP knowledge and skills.
Methods: This cross-sectional questionnaire survey was conducted between June and September 2022 among 2,672 employed hospital nurses in Japan. EBP knowledge and skills were measured using the Japanese version of the EBP Questionnaire. Experience of receiving EBP education in pre-licensure and in-service education was assessed using items developed from EBP textbooks and core competency literature. Analysis of covariance and relative importance analysis were conducted to evaluate the association between the experience of receiving EBP education and EBP knowledge and skills.
Results: 718 nurses (26.9%) were included in the final analysis. The findings showed that nurses’ experience of receiving EBP education was generally limited, with fewer than 25% having learned any EBP-education item, except literature databases, in pre-licensure education. Similarly, fewer than 25% have learned each EBP-education item in in-service education. The adjusted mean EBP knowledge and skills score increased progressively with the extent of education received across the five steps of EBP (20.6 for no steps to 35.5 for five steps), showing a consistent dose–response relationship (p for trend < 0.001). Relative importance analysis showed that the Step 4 and Step 5 items were placed toward the upper end of the contribution rankings.
Conclusions: To effectively improve nurses’ EBP knowledge and skills, providing a practical, EBP-specific program that comprehensively covers all five EBP steps would be essential. Additionally, developing programs for training educators would also be essential.
Keywords: Education, Evidence-based practice, Nurse, Knowledge, Skills.
INTRODUCTION
Evidence-based practice (EBP) is defined as a problem-solving approach that can be used to deliver health care that integrates the best evidence from research and patient care data with clinician expertise as well as patient preferences and values [1]. The risks of adverse outcomes such as mortality, falls, and ventilator-associated pneumonia are reported to be reduced when EBP is implemented [2-5]. Both the American Nurses Association and the American Association of Colleges of Nursing have identified EBP as a core competency for nurses, reflecting its critical role in improving patient care [6,7]. Therefore, promoting EBP education for nurses is recognized as a global priority in nursing. Previous studies on the experience of receiving EBP education have reported its prevalence, instructional hours, and delivery formats (e.g., integration into research methodology or statistics courses) in pre-licensure education [8-11]. Since EBP implementation requires knowledge and skills related to its five steps (Step 1: ask, Step 2: acquire, Step 3: appraise, Step 4: apply, and Step 5: assess), it is essential to receive education on each of these steps. However, no study has examined the extent to which nurses have received specific educational content related to each step of EBP, such as how to formulate clinical questions using the PICO (Patient, Intervention, Comparison, Outcome) or PECO (Patient, Exposure, Comparison, Outcome) framework, and search using databases for clinical guidelines and systematic reviews [12]. Clarifying which aspects of EBP education have been adequately covered and which have not is essential for developing an effective EBP educational program. Additionally, although previous studies have examined the relationship between whether nurses received EBP education and EBP knowledge and skills, no research has assessed how the extent of education received across the five EBP steps relates to these competencies [13-15]. Furthermore, there has been no evaluation of which EBP-education items have a greater contribution to EBP knowledge and skills. Such evaluations would clarify how the comprehensiveness of EBP education relates to levels of EBP knowledge and skills, and which EBP-education items have a greater contribution to EBP competency. This, in turn, would inform the design and prioritization of more effective educational programs. Previous studies have identified factors associated with nurses’ EBP knowledge and skills, including age, gender, educational level, years of clinical nursing experience, employment position, advanced practice certification, participation in EBP education, experience conducting research, and resources and organizational support for EBP [12]. These factors are potential confounders when examining associations between educational exposure and EBP competency. This study was conceptually guided by Kirkpatrick’s evaluation model [16], which conceptualizes training outcomes across four cumulative levels: Level 1—Reaction (how favorable, engaging, and relevant the training is), Level 2—Learning (the degree to which participants acquire intended including knowledge, skills, and confidence), Level 3—Behavior (the degree to which participants apply what they learned on the job), and Level 4—Results (the degree to which targeted organizational outcomes occur).
In our study, the primary endpoints—EBP knowledge and skills—map to Level 2 (Learning), and the extent of experience of receiving EBP education was treated as the educational input expected to produce a dose–response in Level-2 outcomes.
Objective
This study aimed to examine the extent of hospital nurses’ experience of receiving specific educational content related to each step of EBP in both pre-licensure and in-service education in Japan. We also evaluated the associations between these educational experiences and EBP knowledge and skills, and which EBP-education items have a greater contribution.
MATERIALS AND METHODS
Study design and participants
This cross-sectional questionnaire survey was conducted between June and September 2022 among hospital nurses from six hospitals in Western Japan (three universities: two private and one public). Sites were selected for convenience based on pre-existing collaborations and confirmed site willingness. All registered nurses working at these hospitals who met the eligibility criteria were invited to participate. The inclusion criteria were as follows: 1) currently employed as a nurse at a hospital and 2) directly involved in patient care. Nurses in managerial positions, such as directors of nursing, assistant directors of nursing, and head nurses, were excluded. A structured, self-administered, paper-based questionnaire was distributed to participants, and completed questionnaires were returned in sealed envelopes via mail. The study protocol was prepared in accordance with the Declaration of Helsinki and approved by the institutional review board of Osaka Metropolitan University (approval date: June 24, 2022; approval number: 2022–215). The present study used data from the same project as our prior publication [17], though it addresses different research aims and conducts independent analyses.
Data collection procedures and instruments for data collection
Participants were provided with a written explanation of the study’s purpose, procedures, and measures to ensure confidentiality, and that participation was voluntary. Informed consent, considered “appropriate consent” under relevant ethical guidelines [18], was obtained by having participants check a box in the consent section of the questionnaire to indicate their agreement. Data collection was coordinated through the nursing departments at the participating hospitals. After obtaining site approvals, the research team mailed a paper-based questionnaire to the Director of Nursing at each collaborating hospital. The directors then distributed the questionnaire to unit head nurses, who in turn handed it to the eligible staff nurses. All questionnaires were self-administered in paper format; no electronic survey was used, and no individual email addresses or staff contact lists were provided to the researchers. Completed questionnaires were placed by respondents into sealed envelopes and returned by postal mail directly to the study office, thereby maintaining respondent anonymity and confidentiality.
EBP knowledge and skills
EBP knowledge and skills were measured using the Japanese version of the Evidence-Based Practice Questionnaire (EBPQ-J) [18], a validated translation of the original EBPQ developed by Upton and Upton (2006). Both versions have demonstrated high reliability and validity [19-21]. Total scores for EBP knowledge and skills range from 9 to 63, with higher scores indicating greater knowledge and skills. The original EBPQ comprises three subscales: EBP implementation, attitudes toward EBP, and EBP knowledge and skills. The EBPQ-J reorganizes these into four subscales by dividing the knowledge and skills domain into two components: EBP knowledge and skills related to research (score range: 7–49) and EBP knowledge and skills related to practice (score range: 2–14). EBP knowledge and skills were assessed using the total scores of the two subdomains in accordance with the components of the EBPQ. Questionnaire items on the EBP knowledge and skills related to research subscale include statements such as, “Ability to apply necessary information to hypotheses in research question studies,” “Knowledge of methods to search for and obtain evidence,” and “Ability to determine whether the contents of a study are valid (level of bias).” Questionnaire items on the EBP knowledge and skills related to practice subscale include statements such as “Ability to share ideas and information with colleagues” and “Ability to convey new information regarding care with colleagues.” Cronbach’s alpha for the EBP knowledge and skills subscale in the present study was 0.95.
Based on previous literature on factors associated with EBP knowledge and skills [12], we collected the following factors as potential confounders in evaluating the relationship between the experience of receiving EBP education and EBP knowledge and skills using a self-administered questionnaire. These included: age, gender, educational level (diploma, associate degree, bachelor's degree, or master's degree), years of clinical nursing experience, employment position (staff nurse, charge nurse, or assistant head nurse), advanced practice certification (none, certified nurse, or certified specialist nurse), number of times conducting research, access to a literature database (yes or no), and organizational attitude toward EBP ("Is your workplace a positive attitude toward EBP?" non-positive, neither, moderately positive, or very positive). Regarding advanced practice certification in Japan, certified nurse specialists are required to complete a graduate program, which aligns with the qualifications for advanced practice roles in other countries, such as nurse practitioners or clinical nurse specialists [22]. In contrast, certified nurses are registered nurses who have completed specialized clinical training, although a master’s degree is not required for this certification.
Experience of receiving EBP education
The experience of receiving EBP education was measured for both pre-licensure and in-service education. EBP-education items were developed based on key textbooks on EBP [23-25] and literature on EBP core competencies for healthcare professionals [26]. Items were categorized into knowledge and skills components and aligned with the five steps of EBP. Step 1 (Ask) included knowledge of clinical questions and the PICO or PECO framework, as well as skills in formulating clinical questions using that framework. Step 2 (Acquire) included knowledge of efficient evidence searching, such as searching in the following order: systems, summaries, clinical practice guidelines, systematic reviews, and original articles. It also encompassed knowledge of the characteristics and search methods of literature databases (e.g., PubMed and Ichushi Web, a bibliographic database indexing primarily Japanese-language literature on medicine, nursing, dentistry, and pharmacy) and of databases for clinical practice guidelines and systematic reviews (e.g., Minds Guideline Library, a database for domestic clinical practice guidelines published in Japan, and the Cochrane Library). Furthermore, Step 2 included skills in conducting searches for evidence using an efficient order and relevant databases. Step 3 (Appraise) included knowledge of differences in levels of evidence according to study design, random and systematic error, and descriptive and inferential statistics, along with skills in critically appraising literature based on these domains. Step 4 (Apply) included knowledge of the four components required to apply evidence in practice—patient’s clinical state and circumstances, research evidence, patient’s preferences and actions, and clinical expertise—as well as skills in applying these components in clinical decision-making. Step 5 (Assess) included the skill of evaluating the outcomes of EBP. For each EBP-education item, participants were asked to rate their experience on a five-point Likert scale: “Have not learned at all,” “Have not learned,” “Neither,” “Have learned,” and “Have learned a lot.”
Statistical analyses
First, descriptive statistics were used to summarize participants’ characteristics. Continuous variables, such as age and EBP knowledge and skills scores, are presented as means and standard deviations, and dichotomous and categorical data as frequencies and percentages. Next, the experience of receiving EBP education in both pre-licensure and in-service education was summarized for each EBP-education item using frequencies and percentages across the five response categories. Third, analysis of covariance (ANCOVA) was conducted to examine the association between the extent of education received across the five steps of EBP and EBP knowledge and skills. In this model, the extent of education received across the five steps of EBP was treated as the independent variable, and the EBP knowledge and skills score as the dependent variable. In this study, due to the small number of participants who responded “Have learned a lot,” this response was combined with “Have learned” into a single category labeled “Have learned” to improve interpretability. Consequently, the level to which EBP education has been experienced was categorized into four levels: “Have not learned at all,” “Have not learned,” “Neither,” and “Have learned.” For each EBP-education item, the level of educational experience was determined based on responses for both pre-licensure and in-service education. Specifically, when participants reported different amounts of education received across the two educational settings, the higher of the two responses was retained, based on the following rank order: “Have not learned at all” < “Have not learned” < “Neither” < “Have learned.” For instance, if a participant responded, “Have not learned at all” in pre-licensure education and “Have learned” in in-service education, their overall experience for that item was categorized as “Have learned.” The extent of education received across the five steps of EBP was derived by considering participants to have received education on a given step only if they responded “Have learned” to all items within that step. Based on the number of steps for which this condition was met, participants were categorized into one of six groups: those who had received education on no, one, two, three, four, or all five steps. The model included potential confounding variables, including gender, educational level, years of clinical nursing experience, position, advanced practice certification, number of times of experience conducting research, access to a literature database, and organizational attitude toward EBP. Adjusted means and 95% confidence intervals were determined for each category, and a p-value for linear trend was calculated from the linear component (F test) of a polynomial contrast within the ANCOVA framework. Fourth, ANCOVA was conducted for each EBP-education item to examine the association between item-specific experience of receiving EBP education and EBP knowledge and skills. All models used the same four ordered categories (“Have not learned at all,” “Have not learned,” “Neither,” “Have learned”) and the same set of covariates as above. Adjusted means and 95% confidence intervals were determined for each category of level to which EBP education has been experienced, and p-values for linear trends were calculated analogously from the linear component (F test) of a polynomial contrast. The effect sizes were calculated using partial η². For all ANCOVA models, we assessed residual normality with Q–Q plots and homogeneity of variance with residual-versus-fitted plots.
Finally, relative importance analysis was conducted using the Lindemann–Merenda–Gold (LMG) method with the R package “relaimpo” to quantify the contribution of each EBP-education item to EBP knowledge and skills [27,28]. The LMG method is particularly useful when explanatory variables are correlated, as it quantifies each variable’s relative importance by averaging its incremental contribution to R² across all possible orderings [29,30]. Each EBP-education item was dummy-coded as a four-level factor (“Have not learned at all,” “Have not learned,” “Neither,” or “Have learned”). The model included the same covariates as in the ANCOVA (gender, educational level, years of clinical nursing experience, employment position, advanced practice certification, number of times of experience conducting research, access to a literature database, and organizational attitude toward EBP). Contributions were expressed as the percentage of the EBP-education items-only R² (i.e., the proportion of variance explained by the EBP-education items after adjustment for covariates), and 95% confidence intervals were obtained via bootstrap resampling (B = 1,000). We used complete-case analysis because overall missingness was low and missingness often occurred in blocks across item batteries, limiting cross-variable information for imputation. All analyses were performed using IBM SPSS Statistics for Windows version 29 software (IBM SPSS Japan, Tokyo, Japan) or R version 4.4.2 (R Foundation for Statistical Computing, Vienna, Austria). All reported p-values were two-tailed, and values of <0.05 were considered statistically significant.
RESULTS
In total, 2,672 nurses were invited to participate. Of these, 766 (28.7%) responded to the mail survey. After excluding those with missing data, 718 nurses (26.9%) were included in the final analysis. The characteristics of the participants are presented in Table 1. The mean age (standard deviation) was 36.0 (10.0) years; more than 90% of the participants were female, 40.1% had a bachelor’s degree, and 4.0% had a master’s degree. More than half the participants had more than 10 years of clinical experience, most were employed at hospitals with access to a literature database, and more than 60% reported that their organization had a positive attitude toward EBP. The mean EBP knowledge and skills score (standard deviation) was 22.4 (10.4) points, indicating a relatively low level of EBP-related competency among the participants.
Variables Personal factors Age (years) 36.0 (10.0) Gender Women 663 (92.3) Men 55 (7.7) Educational level Diploma or associate degree 400 (55.7) Bachelor’s degree 287 (40.0) Master’s degree 31 (4.3) Years of clinical nursing experience ≤3 159 (22.1) 4–9 160 (22.3) ≥10 399 (55.6) Employment position Staff nurse 653 (90.9) Charge nurse or assistant head nurse 65 (9.1) Advanced practice certification No 692 (96.4) Certified nurse or certified specialist nurse 26 (3.6) Number of times conducting research 0 322 (44.9) 1 146 (20.3) ≥2 250 (34.8) Work-environment factors Literature database No 29 (4.0) Yes 689 (96.0) Organizational attitude toward EBP Nonpositive 82 (11.4) Neither 186 (25.9) Moderately positive 281 (39.2) Very positive 169 (23.5) Outcome EBP knowledge and skills score (points) 22.4 (10.4) Note: Age and EBP knowledge and skills score are presented as mean (standard deviation). Dichotomous data and categorical data are presented as n (%). EBP, evidence-based practice.
Table 1. Participants’ characteristics (n=718).
Experience of receiving EBP education in pre-licensure education
Figure 1 illustrates the experience of receiving EBP education in pre-licensure education among Japanese hospital nurses.
Figure 1. Experience of receiving EBP education in pre-licensure education among Japanese hospital nurses
Note on Figure 1
Proportions represent the distribution of responses to each EBP-education item. Items were categorized into knowledge and skills components and aligned with the five steps of EBP.
a Literature databases refer to resources such as PubMed and Ichushi Web, a bibliographic database indexing primarily Japanese-language literature on medicine, nursing, dentistry, and pharmacy.
b Databases for clinical practice guidelines and systematic reviews refer to resources such as the Minds Guideline Library, a database for domestic clinical practice guidelines published in Japan, and the Cochrane Library.
c The four components are as follows: (1) the patient’s clinical state and circumstances, (2) research evidence, (3) the patient’s preferences and actions, and (4) clinical expertise.
EBP: evidence-based practice; PECO: Patient, Exposure, Comparison, Outcome; PICO: Patient, Intervention, Comparison, Outcome.
Overall, participants’ experience of receiving pre-licensure EBP education was limited. The proportion of nurses who reported that they had learned about skills-related items was lower than the proportion who reported that they had learned about knowledge-related items. Approximately 40% of the nurses reported having learned about characteristics and search methods of literature databases, though fewer than 25% reported having learned about any of the other EBP-education items. Fewer than 10% of nurses reported that they had learned how to formulate clinical questions using the PICO/PECO framework regarding characteristics and search methods of databases for clinical practice guidelines and systematic reviews, how to conduct a search using databases for clinical practice guidelines and systematic reviews, and how to evaluate the outcomes of EBP. Table 2 provides detailed results for each EBP-education item.
Have not learned at all Have not learned Neither Have learned Have learned a lot
EBP – Step 1 (Ask) Knowledge Clinical Questions 253 (35.2) 207 (28.8) 109 (15.2) 132 (18.4) 17 (2.4) The PICO/PECO framework 341 (47.5) 202 (28.1) 92 (12.8) 70 (9.7) 13 (1.8) Skills How to formulate clinical questions using the PICO/PECO framework 378 (52.6) 207 (28.8) 86 (12.0) 42 (5.8) 5 (0.7) EBP – Step 2 (Acquire) Knowledge Efficient order of evidence searching 250 (34.8) 215 (29.9) 109 (15.2) 128 (17.8) 16 (2.2) Characteristics and search methods of literature databases a 181 (25.2) 157 (21.9) 81 (11.3) 237 (33.0) 62 (8.6) Characteristics and search methods of databases for clinical practice guidelines and systematic reviews b 365 (50.8) 199 (27.7) 106 (14.8) 42 (5.8) 6 (0.8) Skills How to search for evidence in an efficient order 314 (43.7) 198 (27.6) 113 (15.7) 81 (11.3) 12 (1.7) How to search using literature databasesa 217 (30.2) 138 (19.2) 84 (11.7) 215 (29.9) 64 (8.9) How to search using databases for clinical practice guidelines and systematic reviews b 350 (48.7) 204 (28.4) 114 (15.9) 43 (6.0) 7 (1.0) EBP – Step 3 (Appraise) Knowledge Differences in levels of evidence according to research design 266 (37.0) 165 (23.0) 99 (13.8) 156 (21.7) 32 (4.5) Random and systematic error 285 (39.7) 162 (22.6) 99 (13.8) 143 (19.9) 29 (4.0) Descriptive and inferential statistics 266 (37.0) 155 (21.6) 112 (15.6) 162 (22.6) 23 (3.2) Skills How to critically appraise literature based on knowledge of research designs and levels of evidence 275 (38.3) 164 (22.8) 127 (17.7) 136 (18.9) 16 (2.2) How to critically appraise literature based on knowledge of random and systematic error 297 (41.4) 184 (25.6) 137 (19.1) 92 (12.8) 8 (1.1) How to critically appraise literature based on knowledge of descriptive and inferential statistics 292 (40.7) 186 (25.9) 140 (19.5) 92 (12.8) 8 (1.1) EBP – Step 4 (Apply) Knowledge The four components of Step 4c 270 (37.6) 202 (28.1) 152 (21.2) 88 (12.3) 6 (0.8) Skills How to apply the four components of Step 4 in nursing practice c 274 (38.2) 201 (28.0) 150 (20.9) 87 (12.1) 6 (0.8) EBP – Step 5 (Assess) Skills How to evaluate the outcomes of EBP 333 (46.4) 199 (27.7) 132 (18.4) 51 (7.1) 3 (0.4) Note: Experience of receiving EBP education is presented as the number of participants (%).
a Literature databases refer to resources such as PubMed and Ichushi Web, a bibliographic database indexing primarily Japanese-language literature on medicine, nursing, dentistry, and pharmacy.
b Databases for clinical practice guidelines and systematic reviews refer to resources such as the Minds Guideline Library, a database for domestic clinical practice guidelines published in Japan, and the Cochrane Library.
c The four components are as follows: (1) the patient’s clinical state and circumstances, (2) research evidence, (3) the patient’s preferences and actions, and (4) clinical expertise.
EBP: evidence-based practice: PECO: Patient, Exposure, Comparison, Outcome; PICO: Patient, Intervention, Comparison, Outcome.
Table 2. Experience of receiving EBP education in pre-licensure education among Japanese hospital nurses (n=718)
Experience of receiving EBP education in in-service education
Figure 2 illustrates the experience of receiving EBP education in in-service education among Japanese hospital nurses.
Note on Figure 2
Proportions represent the distribution of responses to each EBP-education item. Items were categorized into knowledge and skills components and aligned with the five steps of EBP.
a Literature databases refer to resources such as PubMed and Ichushi Web, a bibliographic database indexing primarily Japanese-language literature on medicine, nursing, dentistry, and pharmacy.
b Databases for clinical practice guidelines and systematic reviews refer to resources such as the Minds Guideline Library, a database for domestic clinical practice guidelines published in Japan, and the Cochrane Library.
c The four components are as follows: (1) the patient’s clinical state and circumstances, (2) research evidence, (3) the patient’s preferences and actions, and (4) clinical expertise.
EBP, evidence-based practice, PECO, Patient, Exposure, Comparison, Outcome; PICO, Patient, Intervention, Comparison, Outcome.
Figure 2. Experience of receiving EBP education in in-service education among Japanese hospital nurses.
Overall, participants’ experience of receiving EBP education was limited. For all EBP-education items, fewer than 25% of nurses reported that they had learned about the content, with the percentage of respondents who reported learning about skills-related items being even lower than the percentage of those who reported learning about knowledge-related items. Fewer than 10% of nurses reported that they learned how to formulate clinical questions using the PICO/PECO framework, characteristics and search methods of databases for clinical practice guidelines and systematic reviews, how to conduct a search using databases for clinical practice guidelines and systematic reviews, how to critically appraise literature based on knowledge of random and systematic error, how to critically appraise literature based on knowledge of descriptive and inferential statistics, and how to evaluate the outcomes of EBP. Table 3 provides detailed results for each EBP-education item.
Have not learned at all Have not learned Neither Have learned Have learned a lot EBP – Step 1 (Ask) Knowledge Clinical Questions 276 (38.4) 192 (26.7) 114 (15.9) 126 (17.5) 10 (1.4) The PICO/PECO framework 322 (44.8) 197 (27.4) 98 (13.6) 95 (13.2) 6 (0.8) Skills How to formulate clinical questions using the PICO/PECO framework 340 (47.4) 203 (28.3) 105 (14.6) 66 (9.2) 4 (0.6) EBP – Step 2 (Acquire) Knowledge Efficient order of evidence searching 296 (41.2) 190 (26.5) 118 (16.4) 103 (14.3) 11 (1.5) Characteristics and search methods of literature databases a 250 (34.8) 188 (26.2) 107 (14.9) 154 (21.4) 19 (2.6) Characteristics and search methods of databases for clinical practice guidelines and systematic reviews b 355 (49.4) 194 (27.0) 114 (15.9) 50 (7.0) 5 (0.7) Skills How to search for evidence in an efficient order 332 (46.2) 200 (27.9) 111 (15.5) 69 (9.6) 6 (0.8) How to search using literature databasesa 272 (37.9) 184 (25.6) 100 (13.9) 146 (20.3) 16 (2.2) How to search using databases for clinical practice guidelines and systematic reviews b 353 (49.2) 195 (27.2) 109 (15.2) 57 (7.9) 4 (0.6) EBP – Step 3 (Appraise) Knowledge Differences in levels of evidence according to research design 326 (45.4) 187 (26.0) 110 (15.3) 88 (12.3) 7 (1.0) Random and systematic error 344 (47.9) 199 (27.7) 101 (14.1) 69 (9.6) 5 (0.7) Descriptive and inferential statistics 339 (47.2) 196 (27.3) 104 (14.5) 73 (10.2) 6 (0.8) Skills How to critically appraise literature based on knowledge of research designs and levels of evidence 335 (46.7) 190 (26.5) 112 (15.6) 75 (10.4) 6 (0.8) How to critically appraise literature based on knowledge of random and systematic error 349 (48.6) 203 (28.3) 106 (14.8) 55 (7.7) 5 (0.7) How to critically appraise literature based on knowledge of descriptive and inferential statistics 350 (48.7) 198 (27.6) 104 (14.5) 61 (8.5) 5 (0.7) EBP – Step 4 (Apply) Knowledge The four components of Step 4 c 309 (43.0) 197 (27.4) 119 (16.6) 84 (11.7) 9 (1.3) Skills How to apply the four components of Step 4 in nursing practice c 311 (43.3) 197 (27.4) 120 (16.7) 81 (11.3) 9 (1.3) EBP – Step 5 (Assess) Skills How to evaluate the outcomes of EBP 347 (48.3) 192 (26.7) 116 (16.2) 58 (8.1) 5 (0.7) Note: Experience of receiving EBP education is shown as the number of participants (%).
a Literature databases refer to resources such as PubMed and Ichushi Web, a bibliographic database indexing primarily Japanese-language literature on medicine, nursing, dentistry, and pharmacy.
b Databases for clinical practice guidelines and systematic reviews refer to resources such as the Minds Guideline Library, a database for domestic clinical practice guidelines published in Japan, and the Cochrane Library.
c The four components are as follows: (1) the patient’s clinical state and circumstances, (2) research evidence, (3) the patient’s preferences and actions, and (4) clinical expertise.
EBP: evidence-based practice; PECO: Patient, Exposure, Comparison, Outcome; PICO: Patient, Intervention, Comparison, Outcome.
Table 3. Experience of receiving EBP education in in-service education among Japanese hospital nurses (n=718)
Q–Q plots (quantile–quantile plot)
The Q–Q plots (Figure 3, 4 and 5) indicated approximately normal residuals, and the residual-versus-fitted plots showed no funneling, suggesting no material heteroscedasticity.
Figure 3. Normal Q–Q plots of residuals for ANCOVA models (Panels A–H).
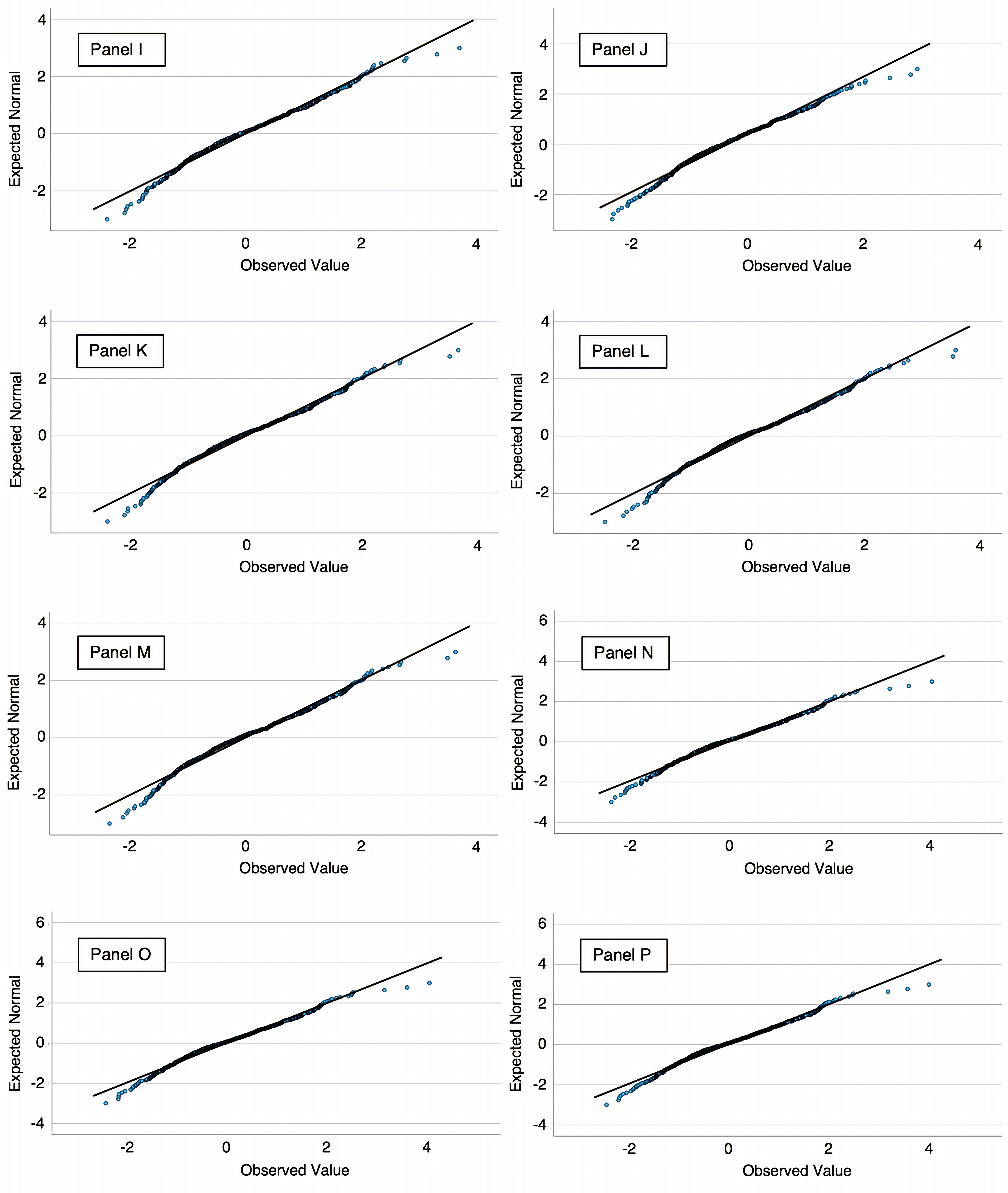
Figure 4. Normal Q–Q plots of residuals for ANCOVA models (Panels I–P).
Figure 5. Normal Q–Q plots of residuals for ANCOVA models (Panels Q–S).
Note on Figures 3-5
Panels: A, six-category model—those who had received education on no, one, two, three, four, or all five steps; B, Step 1—Knowledge: Clinical Questions; C, Step 1—Knowledge: The PICO/PECO Framework; D, Step 1—Skills: How to formulate clinical questions using the PICO/PECO Framework; E, Step 2—Knowledge: Efficient order of evidence searching; F, Step 2—Knowledge: Characteristics and search methods of literature databases; G, Step 2—Knowledge: Characteristics and search methods of databases for clinical practice guidelines and systematic reviews; H, Step 2—Skills: How to search for evidence in an efficient order; I, Step 2—Skills: How to search using literature databases; J, Step 2—Skills: How to search using databases of clinical practice guidelines and systematic review; K, Step 3—Knowledge: Differences in levels of evidence according to research design; L, Step 3—Knowledge: Random and systematic error; M, Step 3—Knowledge: Descriptive and inferential statistics; N, Step 3—Skills: How to critically appraise literature based on knowledge of research designs and levels of evidence; O, Step 3—Skills: How to critically appraise literature based on knowledge of random and systematic error; P, Step 3—Skills: How to critically appraise literature based on knowledge of descriptive and inferential statistics; Q, Step 4—Knowledge: The four components of Step 4; R, Step 4—Skills: How to apply the four components of Step 4 in nursing practice; S, Step 5—Skills: How to evaluate the outcomes of EBP.
Association between the extent of education received across the five steps of EBP and EBP knowledge and skills
Figure 6 illustrates the association between the extent of received education across the five steps of EBP and EBP knowledge and skills scores.
Figure 6. Association between the extent of received education across the five steps of EBP and EBP knowledge and skills
Note on Figure 6
Adjusted mean scores were estimated using analysis of covariance. Scores were adjusted for gender, educational level, years of clinical nursing experience, employment position, advanced practice certification, number of times conducting research, access to a literature database, and organizational attitude toward EBP. Error bars represent 95% confidence intervals.
EBP, evidence-based practice.
The figure shows the mean score for EBP knowledge and skills increased progressively as the number of EBP steps for which education had been received increased. The lowest scores were observed among nurses who had not received education on any of the steps, whereas the highest scores were observed among those who had received education on all five steps. This trend was statistically significant, indicating a dose–response relationship (p for trend<0.001).
Associations between item-specific experience of receiving EBP education and EBP knowledge and skills
Table 4 shows the associations between item-specific experience of receiving EBP education and EBP knowledge and skills scores. For all EBP-education items, participants who reported receiving more EBP education had significantly higher adjusted mean scores for EBP knowledge and skills. The scores showed a consistent increasing trend across the four response categories, and the linear trend was statistically significant for all EBP-education items (p for trend<0.001).
Adjusted meana (95% CI)
p for trend Effect size: partial η² EBP – Step 1 (Ask) Knowledge: Clinical Questions <0.001 0.09 Have not learned at all 18.5 (17.1–20.0) Have not learned 20.5 (19.1–21.8) Neither 25.3 (23.6–26.9) Have learned b 25.7 (24.3–27.0) Knowledge: The PICO/PECO Framework <0.001 0.12 Have not learned at all 19.1 (17.9–20.3) Have not learned 20.8 (19.6–22.1) Neither 25.6 (23.9–27.4) Have learned b 27.8 (26.3–29.3) Skills: How to formulate clinical questions using the PICO/PECO Framework <0.001 0.12 Have not learned at all 19.2 (18.1–20.3) Have not learned 21.7 (20.5–22.9) Neither 25.5 (23.8–27.2) Have learned b 29.4 (27.5–31.3) EBP – Step 2 (Acquire) Knowledge: Efficient order of evidence searching <0.001 0.10 Have not learned at all 18.6 (17.3–20.0) Have not learned 20.5 (19.2–21.8) Neither 24.7 (23.0–26.3) Have learned b 26.4 (25.1–27.7) Knowledge: Characteristics and search methods of literature databases c <0.001 0.07 Have not learned at all 16.5 (14.7–18.4) Have not learned 20.4 (18.7–22.0) Neither 24.5 (22.5–26.4) Have learned b 24.4 (23.3–25.4) Knowledge: Characteristics and search methods of databases for clinical practice guidelines and systematic reviewsd <0.001 0.14 Have not learned at all 19.1 (18.0–20.2) Have not learned 21.9 (20.6–23.2) Neither 24.8 (23.3–26.3) Have learned b 31.1 (29.1–33.1) Skills: How to search for evidence in an efficient order <0.001 0.10 Have not learned at all 19.1 (17.9–20.3) Have not learned 21.3 (20.0–22.6) Neither 24.5 (22.9–26.0) Have learned b 27.9 (26.3–29.5) Skills: How to search using literature databasesc <0.001 0.08 Have not learned at all 17.1 (15.4–18.7) Have not learned 20.3 (18.6–22.1) Neither 23.1 (21.2–25.0) Have learned b 25.0 (24.0–26.0) Skills: How to search using databases for clinical practice guidelines and systematic reviewsd <0.001 0.11 Have not learned at all 19.2 (18.1–20.3) Have not learned 22.1 (20.8–23.4) Neither 25.0 (23.5–26.6) Have learned b 29.1 (27.1–31.0) EBP – Step 3 (Appraise) Knowledge: Differences in levels of evidence according to research design <0.001 0.07 Have not learned at all 18.5 (17.1–19.9) Have not learned 21.1 (19.6–22.6) Neither 24.3 (22.7–26.0) Have learned b 25.5 (24.2–26.8) Knowledge: Random and systematic error <0.001 0.07 Have not learned at all 18.5 (17.2–19.9) Have not learned 22.2 (20.7–23.6) Neither 24.9 (23.2–26.6) Have learned b 25.3 (23.9–26.7) Knowledge: Descriptive and inferential statistics <0.001 0.06 Have not learned at all 18.7 (17.3–20.1) Have not learned 21.5 (20.0–23.0) Neither 24.4 (22.8–26.0) Have learned b 25.3 (24.0–26.7) Skills: How to critically appraise literature based on knowledge of research designs and levels of evidence <0.001 0.09 Have not learned at all 18.3 (17.0–19.7) Have not learned 21.0 (19.5–22.5) Neither 23.9 (22.4–25.4) Have learned b 26.9 (25.4–28.3) Skills: How to critically appraise literature based on knowledge of random and systematic error <0.001 0.10 Have not learned at all 18.6 (17.3–19.8) Have not learned 21.8 (20.5–23.1) Neither 24.2 (22.7–25.7) Have learned b 28.0 (26.3–29.7) Skills: How to critically appraise literature based on knowledge of descriptive and inferential statistics <0.001 0.10 Have not learned at all 18.8 (17.5–20.1) Have not learned 21.2 (19.9–22.6) Neither 24.2 (22.7–25.6) Have learned b 28.1 (26.4–29.7) EBP – Step 4 (Apply) Knowledge: The four components of Step 4e <0.001 0.12 Have not learned at all 18.5 (17.2–19.8) Have not learned 20.7 (19.4–22.0) Neither 24.6 (23.1–26.0) Have learned b 28.2 (26.6–29.7) Skills: How to apply the four components of Step 4 in nursing practicee <0.001 0.12 Have not learned at all 18.4 (17.2–19.7) Have not learned 21.1 (19.8–22.4) Neither 24.6 (23.2–26.1) Have learned b 27.9 (26.3–29.5) EBP – Step 5 (Assess) Skills: How to evaluate the outcomes of EBP <0.001 0.15 Have not learned at all 18.5 (17.3–19.6) Have not learned 21.8 (20.5–23.1) Neither 24.9 (23.5–26.4) Have learned b 30.4 (28.6–32.3) Note: a Adjusted mean scores were estimated using analysis of covariance. Scores were adjusted for gender, educational level, years of clinical nursing experience, employment position, advanced practice certification, number of times conducting research, access to a literature database, and organizational attitude toward EBP.
b The responses “Have learned” and “Have learned a lot” were combined into a single category labeled “Have learned.” For each EBP-education item, the level of educational experience was determined based on responses for both pre-licensure and in-service education. When participants reported different levels of experience across the two educational settings, the higher of the two was retained, following the rank order: “Have not learned at all” < “Have not learned” < “Neither” < “Have learned.”
c Literature databases refer to resources such as PubMed and Ichushi Web, a bibliographic database indexing primarily Japanese-language literature on medicine, nursing, dentistry, and pharmacy.
d Databases for clinical practice guidelines and systematic reviews refer to resources such as the Minds Guideline Library, a database for domestic clinical practice guidelines published in Japan, and the Cochrane Library.
e The four components are as follows: (1) the patient’s clinical state and circumstances, (2) research evidence, (3) the patient’s preferences and actions, and (4) clinical expertise.
CI: confidence interval; EBP: evidence-based practice; PECO: Patient, Exposure, Comparison, Outcome; PICO: Patient, Intervention, Comparison, Outcome.
Table 4. Associations between item-specific experience of receiving EBP education and EBP knowledge and skills (n=718).
Relative importance of EBP-education items for the EBP knowledge and skills
Figure 7 illustrates the relative importance of EBP-education items for the EBP knowledge and skills score.
Figure 7. Relative importance of EBP-education items for the EBP knowledge and skills score.
Note on Figure 7
Bars show the % of EBP education items-only R² contributed by each item, computed using the Lindeman–Merenda–Gold method; error bars are bootstrapped 95% confidence intervals. R²=0.338; adjusted R²=0.270; EBP education items-only R²=0.217. The model included EBP-education items, gender, educational level, years of experience as a clinical nurse, employment position, advanced practice certification, number of experiences conducting research, literature database, and organizational attitude toward EBP.
a Literature databases refer to resources such as PubMed and Ichushi Web, a bibliographic database indexing primarily Japanese-language literature on medicine, nursing, dentistry, and pharmacy.
b Databases for clinical practice guidelines and systematic reviews refer to resources such as the Minds Guideline Library, a database for domestic clinical practice guidelines published in Japan, and the Cochrane Library.
c The four components are as follows: (1) the patient’s clinical state and circumstances, (2) research evidence, (3) the patient’s preferences and actions, and (4) clinical expertise.
EBP, evidence-based practice, PECO, Patient, Exposure, Comparison, Outcome; PICO, Patient, Intervention, Comparison, Outcome.
Ranked by relative importance, the three items accounting for the largest proportion of explained variance were Step 5—Skills (evaluating EBP outcomes), Step 2—Knowledge (characteristics and search methods of databases for clinical practice guidelines and systematic reviews), and Step 4—Knowledge (the four components of Step 4).
Table 5 shows detailed results for the same linear regression model, including unstandardized coefficients, standard errors, p-values, and the change-in-R² (ΔR²) and partial F (ΔF) statistics for all variables.
Factors Reference B (SE) p-value for B ΔR² ΔF p-value for ΔF Experience of receiving EBP education Step 1 (Ask) Knowledge: Clinical Questions 0.002 0.788 0.501 Have not learned vs have not learned at all 0.134 (1.388) 0.923 Neither vs have not learned at all 1.537 (1.698) 0.366 Have learned b vs have not learned at all −0.550 (1.580) 0.728 Knowledge: The PICO/PECO Framework 0.001 0.434 0.729 Have not learned vs have not learned at all −0.868 (2.001) 0.665 Neither vs have not learned at all 1.066 (2.569) 0.678 Have learned b vs have not learned at all 0.981 (2.541) 0.700 Skills: How to formulate clinical questions using the PICO/PECO Framework 0.001 0.316 0.814 Have not learned vs have not learned at all 0.869 (1.991) 0.663 Neither vs have not learned at all −0.061 (2.572) 0.981 Have learned b vs have not learned at all 1.561 (2.668) 0.559 Step 2 (Acquire) Knowledge: Efficient order of evidence searching 0.001 0.457 0.712 Have not learned vs have not learned at all −0.983 (1.418) 0.489 Neither vs have not learned at all 0.700 (1.742) 0.688 Have learned b vs have not learned at all −0.285 (1.630) 0.861 Knowledge: Characteristics and search methods of literature databases c 0.006 1.806 0.145 Have not learned vs have not learned at all 2.983 (1.721) 0.084 Neither vs have not learned at all 3.361 (2.181) 0.124 Have learned b vs have not learned at all 1.291 (1.862) 0.488 Knowledge: Characteristics and search methods of databases for clinical practice guidelines and systematic reviews d 0.007 2.450 0.063 Have not learned vs have not learned at all 0.126 (1.712) 0.941 Neither vs have not learned at all 0.161 (2.044) 0.937 Have learnedb vs have not learned at all 5.267 (2.362) 0.026 Skills: How to search for evidence in an efficient order 0.002 0.622 0.601 Have not learned vs have not learned at all −1.987 (1.546) 0.199 Neither vs have not learned at all −2.202 (1.974) 0.265 Have learned b vs have not learned at all −1.849 (1.936) 0.340 Skills: How to search using literature databases c 0.005 1.553 0.200 Have not learned vs have not learned at all 0.170 (1.801) 0.925 Neither vs have not learned at all 0.507 (2.071) 0.807 Have learned b vs have not learned at all 2.977 (1.820) 0.102 Skills: How to search using databases for clinical practice guidelines and systematic reviews d 0.003 0.920 0.431 Have not learned vs have not learned at all 2.449 (1.877) 0.192 Neither vs have not learned at all 2.042 (2.235) 0.361 Have learned b vs have not learned at all −0.141 (2.382) 0.953 Step 3 (Appraise) Knowledge: Differences in levels of evidence according to research design 0.002 0.687 0.560 Have not learned vs have not learned at all −1.849 (1.875) 0.324 Neither vs have not learned at all −2.001 (2.234) 0.371 Have learned b vs have not learned at all −0.229 (1.980) 0.908 Knowledge: Random and systematic error 0.003 1.088 0.354 Have not learned vs have not learned at all 2.687 (2.142) 0.210 Neither vs have not learned at all 2.707 (2.698) 0.316 Have learned b vs have not learned at all 0.051 (2.387) 0.983 Knowledge: Descriptive and inferential statistics 0.0003 0.110 0.954 Have not learned vs have not learned at all −1.099 (2.165) 0.612 Neither vs have not learned at all −0.453 (2.457) 0.854 Have learned b vs have not learned at all −0.272 (2.189) 0.901 Skills: How to critically appraise literature based on knowledge of research designs and levels of evidence 0.002 0.609 0.609 Have not learned vs have not learned at all 0.132 (2.120) 0.950 Neither vs have not learned at all 1.613 (2.322) 0.487 Have learned b vs have not learned at all 2.325 (2.262) 0.304 Skills: How to critically appraise literature based on knowledge of random and systematic error 0.008 2.664 0.047 Have not learned vs have not learned at all 8.249 (3.581) 0.022 Neither vs have not learned at all −2.465 (4.695) 0.600 Have learned b vs have not learned at all 2.502 (4.050) 0.537 Skills: How to critically appraise literature based on knowledge of descriptive and inferential statistics 0.007 2.342 0.072 Have not learned vs have not learned at all −8.528 (3.629) 0.019 Neither vs have not learned at all 0.019 (4.635) 0.997 Have learned b vs have not learned at all −2.651 (3.863) 0.493 Step 4 (Apply) Knowledge: The four components of Step 4 e 0.002 0.532 0.660 Have not learned vs have not learned at all −0.384 (2.540) 0.880 Neither vs have not learned at all 1.302 (3.083) 0.673 Have learned b vs have not learned at all 2.645 (3.052) 0.387 Skills: How to apply the four components of Step 4 in nursing practicee 0.0005 0.162 0.922 Have not learned vs have not learned at all −0.611 (2.588) 0.814 Neither vs have not learned at all −0.356 (3.182) 0.911 Have learnedb vs have not learned at all −1.695 (3.115) 0.587 Step 5 (Assess) Skills: How to evaluate the outcomes of EBP 0.009 2.948 0.032 Have not learned vs have not learned at all 2.054 (1.560) 0.188 Neither vs have not learned at all 2.006 (1.771) 0.258 Have learned b vs have not learned at all 5.608 (1.960) 0.004 Potential confounding factors Gender 0.001 1.448 0.229 Men vs women 1.584 (1.316) 0.229 Educational level 0.016 8.043 <0.001 Bachelor’s degree vs diploma or associate degree −0.158 (0.932) 0.865 Master's degree vs diploma or associate degree 7.161 (1.869) <0.001 Years of clinical nursing experience 0.001 0.266 0.766 4–9 vs ≤3 −0.16 (1.079) 0.882 ≥10 vs ≤3 −0.757 (1.129) 0.503 Employment position 0.001 0.607 0.436 Charge nurse or assistant head nurse vs staff nurse 1.006 (1.292) 0.436 Advanced practice certification 0.003 2.475 0.116 Certified nurse or certified specialist nurse vs no 3.073 (1.953) 0.116 Number of times conducting research 0.013 6.433 0.002 1 vs 0 1.893 (1.001) 0.059 ≥2 vs 0 3.698 (1.032) <0.001 Literature database 0.001 0.628 0.428 Yes vs no 1.405 (1.773) 0.428 Organizational attitude toward EBP 0.002 0.581 0.628 Neither vs non-positive −0.921 (1.232) 0.455 Moderately positive vs non-positive −0.305 (1.179) 0.796 Very positive vs non-positive 0.388 (1.280) 0.762 Note: These results are from the same model used for the relative-importance analysis in Figure 7.
Dummy variables coded 0 for “have not learned at all”/ 1 for “have not learned”/ 2 for “neither”/ 3 for “have learned” (EBP education items); 0 for women/1 for men (gender); 0 for diploma or associate degree/1 for bachelor's degree/2 for master’s degree (educational level); 0 for “≤3”/1 for “4–9”/2 for “≥10” (years of clinical nursing experience); 0 for staff nurse/1 for charge nurse and assistant head nurse (employment position); 0 for “no”/1 for certified nurse or certified specialist nurse (advanced practice certification); 0 for “0”/1 for “1”/2 for “≥2” (number of times conducting research); 0 for “no”/1 for “yes” (literature database); and 0 for non-positive/1 for neither /2 for moderately positive /3 for very positive (organizational attitude toward EBP).
R²=0.338; adjusted R²=0.270; EBP education items-only R²=0.217.
a EBP knowledge and skills measured by the Evidence-Based Practice Questionnaire Japanese version. EBP knowledge and skills score ranges from 9 to 63, with higher scores indicating more EBP knowledge and skills.
b The responses “Have learned” and “Have learned a lot” were combined into a single category labeled “Have learned.” For each EBP-education item, the level of educational experience was determined based on responses for both pre-licensure and in-service education. When participants reported different levels of experience across the two educational settings, the higher of the two was retained, following the rank order: “Have not learned at all” < “Have not learned” < “Neither” < “Have learned.”
c Literature databases refer to resources such as PubMed and Ichushi Web, a bibliographic database indexing primarily Japanese-language literature on medicine, nursing, dentistry, and pharmacy.
d Databases for clinical practice guidelines and systematic reviews refer to resources such as the Minds Guideline Library, a database for domestic clinical practice guidelines published in Japan, and the Cochrane Library.
e The four components are as follows: (1) the patient’s clinical state and circumstances, (2) research evidence, (3) the patient’s preferences and actions, and (4) clinical expertise.
B: unstandardized coefficients; CI: confidence interval; EBP: evidence-based practice; PECO: Patient, Exposure, Comparison, Outcome; PICO: Patient, Intervention, Comparison, Outcome; SE: standard error; ΔR²: increase in R-squared attributable to adding the variable to a model that already contains all other variables; i.e., the variable’s semi-partial R² (unique contribution); ΔF: partial F statistic for adding the variable to the model.
Table 5. Regression results for the EBP knowledge and skills score a, including all variables.
DISCUSSION
This study investigated the extent of Japanese hospital nurses’ experience of receiving specific educational content related to each step of EBP in both pre-licensure and in-service education and examined its association with EBP knowledge and skills. The findings showed that the experience of receiving EBP education was limited overall, with even lower levels observed for skills-related items. In both pre-licensure and in-service education, fewer than 10% of nurses reported having learned how to formulate clinical questions using the PICO/PECO framework, characteristics and search methods of databases for clinical practice guidelines and systematic reviews, how to search using databases for clinical practice guidelines and systematic reviews, and how to evaluate the outcomes of EBP. Additionally, a statistically significant dose-response relationship was observed between the extent of education received across the five EBP steps and the level of EBP knowledge and skills. Furthermore, in all EBP-education items, higher item-specific experience of receiving EBP education was significantly associated with greater EBP knowledge and skills scores. Furthermore, relative importance analysis showed three leading contributors. These were Step 5—Skills (evaluating EBP outcomes), Step 2—Knowledge (characteristics and search methods of databases for clinical practice guidelines and systematic reviews), and Step 4—Knowledge (the four components of Step 4). These findings suggest that comprehensive exposure to EBP education may play a critical role in developing EBP competencies. Additionally, the observed dose–response between the extent of experience of EBP education and knowledge/skills aligns with Kirkpatrick Level 2 (Learning)—i.e., greater educational coverage is associated with stronger learning outcomes [16]. While our endpoints were confined to Level 2, the model indicates that strengthened learning can support subsequent behavior (Level 3) and results (Level 4). Thus, future studies should extend the evaluation to Levels 3 and 4.
Our findings indicated that nurses’ experience of receiving EBP education was generally limited. Except for items related to literature databases, fewer than 25% of nurses reported having learned about any of the EBP-education items in pre-licensure education. The percentage of nurses who had learned about each EBP-education item in in-service education was consistently below 25%. Although EBP education has been insufficiently embedded in both pre-licensure and in-service curricula in Japan [31,32], such limited exposure is not unique to Japan. Recent reviews have reported that, worldwide, many nurses have never received EBP education [12] and that the overall level of EBP knowledge and skills among nurses remains low [33]. These findings highlight the urgent global need to improve EBP education. However, both pre-licensure and in-service education settings lack sufficient educators capable of providing EBP education [8, 34]. This shortage is likely a major contributor to nurses having limited experience in receiving EBP education. Therefore, developing and implementing training programs to equip educators with the competencies needed to provide EBP education is important. In so doing, the infrastructure for teaching EBP could be strengthened, and EBP implementation in nursing practice can be promoted.
In the present study, a stepwise increase in EBP knowledge and skills scores was observed as the number of EBP steps for which education had been received increased, indicating an association between the comprehensiveness of the EBP education and competency level. Additionally, the item-specific experience of receiving EBP education was positively associated with EBP knowledge and skills scores across all EBP-education items, and a relative importance analysis indicated that the Step 4 and Step 5 items were placed toward the upper end of the contribution rankings. These findings provide quantitative evidence that supports the argument that education encompassing all five steps of EBP is important to improve EBP knowledge and skills [35]. One systematic review has indicated that EBP educational programs tend to focus solely on Steps 1 to 3 of the five steps of EBP [36]. Therefore, future EBP education programs must comprehensively incorporate all five steps rather than only focus on specific ones. At the same time, in the present study, even among nurses who had received education on all five steps, the mean EBP knowledge and skills score was 35.5 on a scale ranging from 9 to 63, indicating that their competency levels remained insufficient. This suggests that to develop EBP competencies, both an adequate extent of educational content and appropriate educational delivery methods are required. In other words, providing practical education programs focused on EBP could be necessary to improve EBP competency levels among nurses effectively. However, EBP education is often integrated into broader courses, such as nursing research or statistics, and is rarely offered as a stand-alone program [8, 9, 10, 11]. Therefore, developing practical, EBP-specific educational programs would be essential to improve nurses' EBP knowledge and skills effectively.
Limitations
This study had several limitations. First, because of the cross-sectional design, a causal association between the experience of receiving EBP education and EBP knowledge and skills cannot be established; however, a statistically significant trend was observed in which EBP knowledge and skills scores increased with the amount of EBP education received, as indicated by the p for trend. This finding serves as additional evidence supporting a dose-response relationship between the two. Second, because the response rate was 28.7%, we must include the possibility of selection bias in which people with relatively more interest in EBP were selected. Third, the study relied on self-reported participant experience with EBP education, which may have introduced recall bias. To obtain a more objective understanding of EBP education's current status, future research should directly investigate institutions such as universities, vocational schools, and healthcare facilities by examining their course offerings, content, and number of instructional hours. Fourth, because our survey data were collected in 2022 (June–September), the findings may not fully reflect the current landscape of EBP education. However, the first explicit mention of EBP in Japan’s pre-licensure education was included in the Model Core Curriculum for Nursing Education (2024 revision) in March 2025 [37]; as this reform will chiefly affect future cohorts, any immediate influence on the educational exposure of the current hospital nursing workforce is likely modest. Finally, this study was conducted in Japan, where EBP education has not been fully promoted. This geographic specificity means that comparisons with findings from countries having more advanced EBP education should be made with caution. Despite this, the results may offer valuable insights, particularly for countries where EBP education is still in its early stages of promotion.
CONCLUSION
We investigated the extent to which hospital nurses in Japan had experienced receiving specific educational content related to each step of EBP in both pre-licensure and in-service education; we also examined its association with EBP knowledge and skills. Fewer than 25% of nurses reported having learned about any of the EBP-education items except for characteristics and search methods of literature databases in pre-licensure education, and fewer than 25% reported having learned about each EBP-education item in in-service education. A dose–response relationship was observed between the number of EBP steps for which education was received and the level of EBP competency. Additionally, the item-specific experience of receiving EBP education was positively associated with EBP knowledge and skills scores across all EBP-education items, and a relative importance analysis indicated that the Step 4 and Step 5 items were placed toward the upper end of the contribution rankings. In the future, to effectively improve the EBP knowledge and skills of nurses, it would be essential to: (1) design educational programs that comprehensively cover all five steps rather than only placing focus on specific steps; (2) develop practical, EBP-specific educational programs; and (3) develop educational programs that enable EBP educators to cultivate professionals capable of delivering such education.
List of abbreviations
EBP: evidence-based practice
PICO: Patient, Intervention, Comparison, Outcome
PECO: Patient, Exposure, Comparison, Outcome
Competing interest
The authors declare that they have no competing financial interests or personal relationships that may have influenced the work reported in this study.
Funding sources
No external funding.
Author contributions
All authors listed meet the authorship criteria according to the guidelines of the International Committee of Medical Journal Editors and agree with the manuscript. Hideaki Furuki: Conceptualization, Methodology, Formal analysis, Investigation, Data curation, Visualization, writing – original draft, writing – review, and editing, and project administration. Nao Sonoda: Conceptualization, Methodology, Formal analysis, Investigation, Data curation, Visualization, writing-review and editing, and project administration. Akiko Morimoto: Conceptualization, Methodology, Formal analysis, Investigation, Data curation, Visualization, writing – review and editing, project administration.
Acknowledgments
We are grateful to all the participants who participated in this study. We thank Miwa Fukumitsu, Haruna Sakamoto, and Risa Koike for their contributions to this study.
REFERENCES
- Melnyk BM, Fineout-Overholt E, Stillwell SB, Williamson KM. Evidence-based practice: Step by step: The seven steps of evidence-based practice. Am J Nurs. 2010;110(1):51–53. doi:10.1097/01.NAJ.0000366056.06605.d2
- Connor L, Dean J, McNett M, Tydings DM, Shrout A, Gorsuch PF, et al. Evidence-based practice improves patient outcomes and healthcare system return on investment: Findings from a scoping review. Worldviews Evid Based Nurs. 2023;20:6–15. doi:10.1111/wvn.12621
- Melnyk BM, Fineout-Overholt E, Giggleman M, Choy K. A test of the ARCC model improves implementation of evidence-based practice, healthcare culture, and patient outcomes. Worldviews Evid Based Nurs. 2017;14(1):5–9. doi:10.1111/wvn.12188
- Wu Y, Brettle A, Zhou C, Ou J, Wang Y, Wang S. Do educational interventions aimed at nurses to support the implementation of evidence-based practice improve patient outcomes? A systematic review. Nurse Educ Today. 2018;70:109–114. doi:10.1016/j.nedt.2018.08.026
- Knežević D, Jović D, Petković M. The impact of introducing a nursing education protocol on the incidence of Clostridium difficile infections in the hospital environment: A quasi-experimental study. NSC Nursing. 2023;2(4):62–84. doi:10.32549/OPI-NSC-89.
- American Association of Colleges of Nursing. The Essentials: Core Competencies for Professional Nursing Education. Washington (DC): AACN; 2021. [Internet]. Available from: https://www.aacnnursing.org/Portals/0/PDFs/Publications/Essentials-2021.pdf (Accessed: September 6, 2025).
- American Nurses Association. Nursing: Scope and Standards of Practice. 4th ed. Silver Spring (MD): American Nurses Association; 2021.
- Hung HY, Huang YF, Tsai JJ, Chang YJ. Current state of evidence-based practice education for undergraduate nursing students in Taiwan: A questionnaire study. Nurse Educ Today. 2015;35:1262–1267. doi:10.1016/j.nedt.2015.05.001
- Malik G, McKenna L, Griffiths D. An analysis of evidence-based practice curriculum integration in Australian undergraduate nursing programs. GSTF J Nurs Health Care. 2015;3(1):158–164. doi:10.7603/s40743-015-0029-z
- Skela-Savič B, Gotlib J, Panczyk M, Patelarou AE, Bole U, Ramos-Morcillo AJ, et al. Teaching evidence-based practice (EBP) in nursing curricula in six European countries – A descriptive study. Nurse Educ Today. 2020;94:104561. doi:10.1016/j.nedt.2020.104561
- Song CE, Kim WG, Lim YJ. An analysis of evidence-based practice courses in Korean nursing education systems. 2019;5(10):e02650. doi:10.1016/j.heliyon.2019.e02650
- Furuki H, Sonoda N, Morimoto A. Factors related to the knowledge and skills of evidence-based practice among nurses worldwide: A scoping review. Worldviews Evid Based Nurs. 2023;20:16–26. doi:10.1111/wvn.12623
- Alqahtani N, Oh KM, Kitsantas P, Rodan M. Nurses’ evidence-based practice knowledge, attitudes and implementation: A cross-sectional study. J Clin Nurs. 2020;29(1–2):274–283. doi:10.1111/jocn.15097
- Filippini A, Sessa A, Di Giuseppe G, Angelillo IF. Evidence-based practice among nurses in Italy. Eval Health Prof. 2011;34(3):371–382. doi:10.1177/0163278710387924
- Tomotaki A, Fukahori H, Sakai I. Exploring sociodemographic factors related to practice, attitude, knowledge, and skills concerning evidence-based practice in clinical nursing. Jpn J Nurs Sci. 2020;17(1):e12260. doi:10.1111/jjns.12260
- Kirkpatrick JD, & Kirkpatrick WK. Kirkpatrick’s four levels of training evaluation. Alexandria: ATD Press; 2016.
- Ministry of Education, Culture, Sports, Science and Technology; Ministry of Health, Labour and Welfare; Ministry of Economy, Trade and Industry. Ethical guidelines for medical and biological research involving human subjects. 2024. Japanese. [Internet]. Available from: https://www.lifescience.mext.go.jp/files/pdf/n2181_01.pdf (Accessed: September 6, 2025).
- Furuki H, Sonoda N, Morimoto A. Relationship between evidence-based practice knowledge and skills and evidence-based practice implementation in subgroups of professional and work environment factors among hospital nurses: A cross-sectional study. Jpn J Nurs Sci. 2025;22(4):e70018. doi:10.1111/jjns.70018
- Tomotaki A, Fukahori H, Sakai I, Kurokohchi K. The development and validation of the Evidence-Based Practice Questionnaire: Japanese version. Int J Nurs Pract. 2018;24(2):e12617. doi:10.1111/ijn.12617
- Leung K, Trevena L, Waters D. Systematic review of instruments for measuring nurses’ knowledge, skills and attitudes for evidence-based practice. J Adv Nurs. 2014;70:2181–2195. doi:10.1111/jan.12454
- Upton D, Upton P. Development of an evidence-based practice questionnaire for nurses. J Adv Nurs. 2006;53(4):454–458. doi:10.1111/j.1365-2648.2006.03739.x
- International Council of Nurses. Guidelines on Advanced Practice Nursing 2020. Geneva: International Council of Nurses; 2020. Available from: https://www.icn.ch/resources/publications-and-reports/guidelines-advanced-practice-nursing-2020 (Accessed: September 6, 2025).
- Guyatt G, Rennie D, Meade MO, Cook DJ, editors. Users’ Guides to the Medical Literature: A Manual for Evidence-Based Clinical Practice. 3rd ed. New York: McGraw-Hill Education; 2015.
- Melnyk BM, Fineout-Overholt E. Evidence-based Practice in Nursing & Healthcare: A Guide to Best Practice. 5th ed. Philadelphia: Wolters Kluwer; 2023.
- Straus SE, Glasziou P, Richardson WS, Haynes RB. Evidence-Based Medicine: How to Practice and Teach EBM. 5th ed. Edinburgh: Elsevier; 2018.
- Albarqouni L, Hoffmann T, Straus S, Olsen NR, Young T, Ilic D, et al. Core competencies in evidence-based practice for health professionals: Consensus statement based on a systematic review and Delphi survey. JAMA Netw Open. 2018;1:e180281. doi:10.1001/jamanetworkopen.2018.0281
- Groemping U. Relative importance for linear regression in R: The package relaimpo. J Stat Softw. 2006;17(1):1–27. doi:10.18637/jss.v017.i01
- Groemping U. relimpo: Relative Importance of Regressors in Linear Models. Version 2.2-7; 2023. [Internet]. Available from: https://cran.r-project.org/web/packages/relaimpo/relaimpo.pdf (Accessed: September 6, 2025).
- Bi J. A review of statistical methods for determination of relative importance of correlated predictors and identification of drivers of consumer liking. J Sens Stud. 2012;27(2):87–101. doi:10.1111/j.1745-459X.2012.00370.x
- Tonidandel S, LeBreton JM. Relative importance analysis: A useful supplement to regression analysis. J Bus Psychol. 2011;26(1):1–9. doi:10.1007/s10869-010-9204-3
- Ministry of Education, Culture, Sports, Science and Technology. Model Core Curriculum for Nursing Education (2024 Revised Edition). 2025. Japanese. [Internet]. Available from: https://www.mext.go.jp/a_menu/koutou/iryou/mext_00021.html (Accessed: October 22, 2025).
- Tomotaki A, Sakai I, Fukahori H, Tsuda Y, Okumura-Hiroshige A. Factors affecting the critical appraisal of research articles in Evidence-Based practices by advanced practice nurses: A descriptive qualitative study. Nurs Open. 2023;10(6):3719-3727. doi:10.1002/nop2.1628
- Li H, Xu R, Gao D, Fu H, Yang Q, Chen X, et al. Evidence-based practice attitudes, knowledge and skills of nursing students and nurses: A systematic review and meta-analysis. Nurse Educ Pract. 2024;78:104024. doi:10.1016/j.nepr.2024.104024
- Abu-Odah H, Said NB, Nair SC, Allsop MJ, Currow DC, Salah MS, et al. Identifying barriers and facilitators of translating research evidence into clinical practice: A systematic review of reviews. Health Soc Care Community. 2022;30:e3265–e3276. doi:10.1111/hsc.13898
- Stevens KR. The impact of evidence-based practice in nursing and the next big ideas. Online J Issues Nurs. 2013;18(2):4.
- Albarqouni L, Hoffmann T, Glasziou P. Evidence-based practice educational intervention studies: A systematic review of what is taught and how it is measured. BMC Med Educ. 2018;18(1):177. doi:10.1186/s12909-018-1284-1
- Ministry of Education, Culture, Sports, Science and Technology. Model Core Curriculum for Nursing Education (2024 Revised Edition). 2025. Japanese. [Internet]. Available from: https://www.mext.go.jp/a_menu/koutou/iryou/mext_00021.html (Accessed: October 12, 2025).
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
AUTISM SPECTRUM DISORDERS KNOWLEDGE: RESULTS FROM AN ITALIAN NURSING STUDENTS MULTICENTER CROSS-SECTIONAL STUDY
Martina Cotugno 1*, Flavio Prezzolini 2, Stefania Catanzaro 3, Emanuele Di Simone 4,
Marco Di Muzio 5, Alessio Mazzotta 3
- Department of Public Health and Infectious Diseases, Sapienza University of Rome, Rome, Italy.
- Department of Emergency Acceptance, Critical Areas and Trauma, University Hospital “Policlinico Umberto I”, Rome, Italy.
- Teaching Center for Healthcare Professions University Hospital “Policlinico Umberto I”, Rome, Italy.
- Department of Medical, Movement and Wellbeing Sciences, Parthenope University of Naples, Naples, Italy.
- Department of Clinical and Molecular Medicine, Sapienza University of Rome, Rome, Italy.
* Corresponding author: Martina Cotugno, master’s degree student in Nursing Sciences, Department of Public Health and Infectious Diseases, Sapienza University of Rome, (Rome), Italy. E-mail: martinacotugno72@gmail.com
Cite this article
ABSTRACT
Introduction: Autism spectrum disorders (ASD) represent a constantly evolving neurodevelopmental condition that requires specific preparation by the entire multidisciplinary team. However, multiple scientific evidences report little training on ASD in nursing degree courses. The study above aims to assess the level of theoretical knowledge of Italian students regarding autism in pediatric age.
Materials and Methods: A multicenter cross-sectional study was conducted on 104 students enrolled in the Nursing degree programme, regularly enrolled in the 2nd and 3rd years of the course at different Italian universities, with or without previous experience in pediatric or mental health services. Knowledge was assessed by administering a validated questionnaire, the Knowledge About Childhood Autism Among Healthcare Workers (KCAHW). Sociodemographic variables and information on training and placement experience with children with ASD were collected. Data were analysed using descriptive and inferential statistics.
Results: The average score obtained on the KCAHW was 9.5 out of 19 (SD = 2.78), indicating an insufficient level of knowledge. Scores were significantly higher among students with direct experience with children with ASD (median: 11.0 vs. 9.3; p=0.015) and among female students than male students (mean: 9.9 vs. 8.7; p=0.016). Theoretical training and age were not significantly different.
Discussion: The results indicate the existence of a vital training gap. Direct clinical experience proves to be decisive in the improvement of theoretical knowledge. Integrating compulsory modules and structured ASD training in nursing education is recommended to ensure competent, small patient-centred care.
Keywords: Autism Spectrum Disorder (ASD); nursing education; undergraduate nursing students; theoretical knowledge; KCAHW questionnaire.
INTRODUCTION
Autism spectrum disorders (ASD) are a neurodevelopmental disorder that is steadily evolving worldwide. According to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) [1], ASD symptoms are defined “persistent deficits in social communication and social interaction across multiple contexts […] restricted, repetitive patterns of behaviour, interests, or activities”, moreover, the DSM-5 frames ASD as a single spectrum condition, replacing previous categorical subtypes and recognizing both the clinical variability and the differing levels of support individuals may need. In 2022, the World Health Organisation (WHO)’s International Classification of Diseases, 11th Revision (ICD-11) provided a similar definition, highlighting the symptoms' pervasive nature and clinical variability [2]. The global prevalence is estimated at around 0,6%. A recent meta-analysis estimated the global prevalence of ASD to be around 1% [3]. Data from the Global Burden of Disease Study estimates that approximately 1 in 127 individuals is affected by an autism spectrum disorder, corresponding to approximately 61.8 million people [4]. In Italy, a national study on children between 7 and 9 years old has identified a prevalence between male and female genders of 4.4:1 [5,6]. These data, gathered from surveys conducted across the entire school-age population in three Italian regions, confirm trends consistent with global trends [5]. The early increase in diagnosis has been attributed to improved screening procedures and greater social awareness. Despite the high prevalence of autism spectrum disorders and the complexity of care they entail, numerous studies show a significant lack of specific training among nurses and, more generally, among healthcare professionals. According to a systematic review, most healthcare professionals report low self-efficacy, a low level of theoretical knowledge and relational difficulties when interacting with patients with ASDs [7]. The results indicate that both undergraduate education on autism is highly heterogeneous and often not mandatory, leading to educational gaps that translate into suboptimal quality of care. An Italian study revealed that more than 60% of pediatric nurses did not receive any specific training on autism spectrum disorders during their academic career [8]. Furthermore, less than 40% consider themselves prepared to manage the nursing care of a child with ASD in both hospital and community settings [8]. Critical issues include lacking communication skills, difficulty using specific behavioural strategies, and limited knowledge of augmentative alternative communication (AAC) tools. This situation is also confirmed internationally. A pilot study on educational programs in the USA has shown that only 10-15% of nursing degree courses include compulsory modules on ASD [9]. A survey of nursing professors pointed out that in most nursing schools, there are no structured courses on autism and, when they are present, they are often limited to short theoretical references [10]. However, more recent studies have confirmed these critical issues internationally. Various studies have shown that, in clinical simulation settings, students show difficulties in emotional and communicative management with patients with ASD [11]. In addition, further studies report that both nurses and students are still partially prepared, underlining the need for specific and standardised training programmes between universities [12-14]. Further studies have confirmed that barriers to caring for patients with ASD are amplified by poorly structured training and poor communication skills among health professionals [7,15]. A systematic review has also highlighted critical issues in health services and communication between professionals, patients and caregivers [16]; in addition, the Italian Ministry of Health provides official information and materials aimed at families and professionals [17]. The guidelines issued by the Italian National Institute of Health (ISS) are now a key reference point for diagnosing and managing autism in Italy. On World Autism Awareness Day, the ISS released data and promoted awareness initiatives. The study highlights the urgent need to include specific content on autism in university programmes, combining a theoretical approach with practical experience in specialist contexts, to ensure safe, competent and truly person-centred care. Despite the obvious clinical and care relevance of autism in Italy, studies assessing nursing students' knowledge of ASD are still lacking. Most research focuses on pediatric nurses already in the working context, while there is little evidence analysing basic training during the university course. This study was conceived to respond to this deficiency to assess Italian nursing students' knowledge of pediatric autism, using a validated instrument, the KCAHW, and involving several university venues throughout Italy. The study intends to offer an up-to-date overview of students' awareness and preparation by highlighting educational inhomogeneities among the various universities and verifying the consistency between internship experiences and the competence acquired on the topic. In summary, this study contributes to the scientific and academic debate on integrating autism training into nursing curricula, with potential implications for the practical training of healthcare professionals and, indirectly, the quality of care provided to pediatric patients with autism.
MATERIALS AND METHODS
Study Designed
A cross-sectional study was conducted to assess the level of knowledge among nursing students about autism spectrum disorders. The aforementioned study design involved the administration of a validated questionnaire, the Knowledge About Childhood Autism Among Healthcare Workers (KCAHW), to a heterogeneous sample of undergraduate students in a single period to replicate the students' theoretical background acquired during their education. Using a validated tool such as the KCAHW aligns with recent methodological approaches that use paediatric simulations or standardised patients with ASD to evaluate training effectiveness [11,20,21]. The KCAHW contains 19 questions divided into four domains:
- Domain 1: 8 questions on inappropriate social interactions in children with ASD;
- Domain 2: 1 question on impaired communication and language development;
- Domain 3: 4 questions on obsessive-compulsive, repetitive and stereotypical behaviours;
- Domain 4: 6 questions on comorbidity and age of onset of the disorder.
Each item has three answer options, only one of which is correct. Correct answers are worth 1 point, while incorrect answers or “don't know” answers are worth 0 points. The total score ranges from 0 to 19, with higher scores indicating greater knowledge. In the literature, a cut-off of 60% correct answers has been proposed to identify a minimum basic level of knowledge. Previous studies have reported satisfactory internal consistency (Cronbach's α =0.97) and adequate content validity for the KCAHW [22].
Study site
The survey was administered online using Google Forms in July 2024. Students who were enrolled in ten nursing degree courses throughout Italy were involved. The universities involved were: Sapienza University of Rome, “Aldo Moro” of Bari, University “del Salento” of Lecce, “Federico II” of Naples, University of Palermo, “Gabriele D'Annunzio” of Chieti-Pescara, "Bicocca" of Milan, and the Universities of Bologna, Firenze and Trieste.
Participants
The sample was composed using a combination of convenience and snowball sampling strategies. Participants were first recruited through convenience sampling, as this approach allowed us access to readily available individuals willing to participate. Then, a snowball sampling strategy was applied to expand the sample and include participants who might otherwise have been difficult to reach, whereby early respondents enrolled additional eligible participants through diffusion of the survey link (direct access to the Google Form platform). The final sample consisted of 104 students enrolled in the nursing degree programme, chosen according to the following inclusion criteria: Enshrined in the second or third year of the degree programme. Previous experience in paediatric or child mental health services was not considered an inclusion criterion but was recorded as a descriptive variable.
For analytical purposes, age was categorized into three groups (18-20, 20-22, ≥23 years). This classification was not intended to represent clinical thresholds but was based on the distribution of the sample and on the typical progression within the nursing degree programme (early years, middle years and delayed or outside prescribed time students).
Ethical considerations
This study adhered to the ethical standards outlined in the Helsinki Declaration and complied with General Data Protection Regulation-EU Regulation 679/2016 (GDPR). According to the Regulation for the functioning of the “Comitato Etico per la Ricerca Transdisciplinare (CERT)” of Sapienza University (Protocol 103110, 31 May 2024), anonymous, non-interventional studies that do not involve the collection of sensitive personal data are exempt from formal ethical approval. As our study fulfilled these criteria, no ethical review was required. Indeed, no sensitive personal data was collected; the questionnaire was designed to gather only general, non-identifiable information. The Google Forms platform, as set by the authors, did not collect any e-mail addresses and automatically anonymised responses with progressive numeric codes, so no personal identification was possible. The participation in the study through questionnaire response implied the acceptance of informed consent to participate, where characteristics and all data collection modalities were reported. Moreover, responders could abandon the survey at any time if the questions were deemed too personal or inappropriate, without any partial responses being collected. The authorisation of the survey administration to students was obtained from the Director of the nursing degree programme, following a previous evaluation of the survey items, structure, and questions.
Statistical analysis
Quantitative variables were described as mean ± standard deviation (SD) if normally distributed, or as median and interquartile range (IQR) if not. Categorical variables were presented as absolute frequencies and percentages. The normality of distributions was verified using the Shapiro-Wilk test, while the homogeneity of variances was verified using Levene's test. Comparisons between two independent groups were performed using the t-test for independent samples when the assumptions of normality and homoscedasticity were met; otherwise, the non-parametric Mann-Whitney U test was applied. Comparisons between more than two groups were performed using one-way ANOVA only in the presence of normal distribution and homoscedasticity; otherwise, the Kruskal-Wallis test was used. Box plots were used for the graphical representation of scores: the horizontal line inside the box represents the median, the box limits correspond to the 25th and 75th percentiles (IQR), and the whiskers indicate the minimum and maximum values. All tests with p-values < 0.05 were considered significant. The internal consistency of the KCAHW was assessed using Cronbach’s α coefficient, calculated on the overall sample. To conclude descriptive statistics were used to summarise the socio-demographic characteristics of the sample. All analyses were performed using IBM SPSS Statistics, version 27.0.
RESULTS
The study included 104 nursing students. The highest response rate was found among the Sapienza University students of Rome, representing approximately 71% of the total participants. The majority were female (71%), with a relatively even age distribution between the groups, 20-22 years (48%) and over 22 (48%). Only 21.1% reported that they had received specific training on ASD during their training, while 14.4% stated that they had cared for children with autism during their internship experience. The average score on the questionnaire was 9.5 out of 19 (SD=2.78), with values ranging from 1 to 15 (Table 1).
Mean Standard deviation (SD) Minimum value Maximum value Median 9.5 2.78 1.0 15.0 10.0 Table 1. KCAHW descriptive statistics
The distribution of the score suggests an insufficient general level of knowledge on the subject of autism in paediatric age. Table 2 shows the distribution of KCAHW scores across the four domains and the total score. Students scored highest in domain 1 (social interaction; mean=4.63, median=5) and domain 3 (repetitive behaviours; mean=2.45, median=3). The lowest performance was observed in domain 2 (communication; mean=0.40, median=0). Domain 4 (comorbidity and age of onset) showed a mean of 2.86 (median=3). The mean total score was 10.35 (SD=3.08, median=10; range 1-17), indicating overall insufficient knowledge.
Domain Items (n)
Standard deviation (SD) Mean Minimum value
Maximum value
Median Domain 1 social interaction
8 1.80 4.63 0 8 5 Domain 2 communication 1 0.49 0.40 0 1 0 Domain 3 Repetitive behaviours 4 1.10 2.45 0 4 3 Domain 4 Comorbidity and onset
6 1.24 2.86 0 5 3 Total score 19 3.08 10.35 1 17 10 Table 2. Distribution of scores across the four domains and total score KCAHW
Statistical tests were then conducted to assess the association between socio-demographic variables and the score obtained (Table 3).
Comparison Statistical test Statistical value p-value ASD training (yes or no) Mann-Whitney U U=1245.0 0.261 Internship experiences with children affected by ASD (yes or no) Mann-Whitney U
U=1080.0
0.015
Sex (female-male) t-test t=2.47 0.016 Age groups (18-20/20-22/≥23) Kruskal-Wallis H=0.49 0.612 Note: Parametric tests (t-test, one-way ANOVA) were applied only when assumptions of normality and homoscedasticity were met; otherwise, non-parametric alternatives (Mann–Whitney U, Kruskal–Wallis) were used. Table 3. Statistical test results
Students who had previously had placement experience with children with ASD scored significantly higher (median: 11.0 vs. 9.3; Mann-Whitney U=1080.0; p=0.015). Similarly, a difference in performance between students with and without clinical experience was also found in a study conducted in 2024, confirming the formative impact of internship activities [13].
Female gender was associated with a significantly higher score (mean: 9.9 vs. 8.7; t=2.47; p=0.016). There was no significant difference between those who had received specific training on autism spectrum disorders and those who had no organised courses on this topic in their curricula (Mann-Whitney U=1245.0; p=0.216). Age did not significantly impact the overall score statistically (Kruskal-Wallis H=0.49; p=0.612).
The scores obtained from the questionnaire were represented graphically as a function of training and clinical-practical internship experience. The box plots show greater variability and a higher median in the groups who have had training placement experience with children with autism spectrum disorders than in those who have not had clinical practice experience in this area. The internal consistency of the KCAHW, assessed through Cronbach’s α, was 0.54 in this sample, in line with other studies on student populations and confirming the multidimensional nature of the tool.
The box plot (Figure 1 and 2) represents the median (horizontal line inside the box), the interquartile range (IQR) (25th-75th percentile; extremes of the box), and the minimum and maximum values (whiskers).
In Figure 1, students who had received specific training on ASD reported higher median scores and less variability than those without training.
In Figure 2, students with internship experience with children with ASD obtained higher scores and a more compact distribution, indicating a generally higher and more homogeneous level of knowledge than the group without direct experience.
Figure 1. Distribution of KCAHW scores based on ASD training
Figure 2. Distribution of KCAHW scores based on internship experience
DISCUSSION
The study analysed the level of theoretical knowledge about autism in developmental age among students in a nursing degree program using a validated instrument, the KCAHW. The results show insufficient knowledge, with an average of less than half of the maximum achievable score. The domain analysis also showed that the lowest scores were obtained in the area of communication (domain 2), while relatively higher scores were found in social interaction (domain 1) and repetitive behaviours (domain 3). These results suggest that the communicative aspects of autism remain particularly underestimated among nursing students, highlighting a specific gap that training curricula should address. This finding is in line with what is reported in the international literature, where a general inadequacy of basic nursing education concerning neurodevelopmental disorders, particularly those of the autistic spectrum, is emphasised [7,10]. One of the most significant pieces of evidence that emerged concerns the positive association between internship experience with children with ASD and a higher score on the questionnaire. This result confirms the effectiveness of clinical-practical learning as a fundamental tool for consolidating theoretical knowledge and developing specific communication and relational skills [9]. In line with these findings, several studies have highlighted how direct field experience is associated with improved professional preparedness and safety [10,12,13]. Realistic simulation is also an effective educational strategy, as some studies have observed improvements in post-simulation communication skills [11,21]. The presence of field experience allows students to consciously confront the complexity of care related to autism spectrum disorders, favouring a less stereotypical approach. This finding aligns with numerous results that show that the perception of nurses' competencies is mainly linked to clinical experience and not only to theoretical training [14,26]. Also of great importance is the significant difference found in gender, with female students reporting higher average results than male students. This datum, already highlighted in other training contexts, could be linked to psycho-social variables such as a greater predisposition to helping relationships or a different motivation in the in-depth study of themes related to the behavioural and relational sphere. Contrary to expectations, the presence or absence of basic theoretical training on ASD did not show statistically significant differences in the scores obtained. This may reflect the poor systematisation and heterogeneity of the content available in the various courses of study and the predominantly theoretical nature of these training modules, which are not supplemented with practical experience. Similarly, the age of the students was not found to be predictive of the level of knowledge, suggesting that the accumulation of academic years does not necessarily guarantee greater competence on the subject. Some researchers propose the integration of new technologies in nursing education. Numerous studies highlight the effectiveness of virtual reality in training students in interactions with patients with autism spectrum disorders [27]. In contrast, others focus on using artificial intelligence to support healthcare professionals in managing ASDs [28]. Several qualitative studies based on clinical simulation have also highlighted areas for improvement in nursing education on autism spectrum disorders [29]. These new perspectives open up different scenarios for the training of healthcare professionals and deserve further investigation. The collected data show a substantial training gap within the Italian nursing curricula. A recent observational study found limited knowledge of nurses regarding autism spectrum disorders [30]. In light of the increasing prevalence of ASD and the growing need for healthcare professionals competent in the management of this population [31], there is an urgent need for the integration of structural, multidisciplinary and experience-based education. Some recent experiments suggest the integration of immersive technologies and intelligent tools to enhance the effectiveness of teaching. Virtual reality, in particular, has proven helpful in improving students' social and relational skills in simulated settings with patients with ASD [27]. Furthermore, the use of artificial intelligence to support early diagnosis and care planning is growing [28], with good results also in training healthcare professionals [32]. Finally, a following step forward is the specific training of pediatric nursing staff on common aggressive behaviours in children with ASD, as reported by several researchers who conducted a pilot RCT showing how simulation increases staff safety and operational skills [33].
Limitations
The study’s main limitations include the small sample size (n=104), the relatively low response rate across the ten university courses involved, and the non-probabilistic nature of the sampling, which limits the generalizability of the results to the entire Italian nursing student population. The low response rate may reflect the voluntary and self-administered nature of the survey, as well as the variability in students' availability and motivation to participate. This aspect could have introduced a further selection bias, as the students who responded may have been more interested or sensitised to the topic compared to those who did not. The choice of the sample was based on the availability and accessibility of students at specific university sites, introducing a possible selection bias. Secondly, a self-administered questionnaire may have exposed the results to social desirability bias or subjective interpretations of the questions, even though the KCAHW is internationally validated. Another limitation is the purely theoretical assessment of knowledge without in-depth exploration of practical or attitudinal expertise or the ability to apply the acquired knowledge in real clinical contexts. Furthermore, the training received was investigated with a single closed question without a qualitative-quantitative assessment of the training content addressed. Finally, as this is a cross-sectional study, it is impossible to establish causal relationships between the analysed variables, but only statistical associations. Forward-looking longitudinal studies could help us understand how knowledge evolves and the real impact of training programmes on acquiring specific competencies. Overall, the findings suggest that nursing students show insufficient knowledge of autism and limited attitudinal preparedness for managing children with ASD. This highlights the need for nursing curricula to include not only theoretical content, but also experiential and practical training aimed at improving students’ attitudes, confidence, and readiness to interact with autistic patients and their families
CONCLUSION
In conclusion, the study highlights the need for a more comprehensive theoretical education in ASD for nursing students, focusing on developing skills in the clinical setting. Educational strategies should therefore address both theoretical knowledge and students’ attitudes toward autism, fostering more adequate preparedness for clinical practice. The absence of statistical significance for the theoretical training received suggests a potential fragmentation and inhomogeneity of the content delivered in degree courses that would merit systemic reflection at an academic and institutional level. In light of the increase in the prevalence of ASD and the growing complexity of care that this condition entails, there emerges an urgent need to integrate specific, up-to-date content applicable in clinical practice into nursing education courses. In particular, it would be better if supervised internship experiences in specialist settings accompany the adoption of mandatory modules on autism within academic programmes. Further multicentre research and larger samples will be necessary to validate these results and further investigate the effectiveness of training interventions in terms of their practical-assistance spin-offs, with a view to continually improving the quality of care for the paediatric population with autism spectrum disorders. Finally, as highlighted in the international literature, an up-to-date and multidisciplinary understanding of autism spectrum disorders is fundamental to improving the quality of care and reducing inequalities in access to care [34]. However, in light of the sustainability of training programmes, it does not seem realistic to envisage the introduction of specific modules for each individual clinical condition. Rather, it would be appropriate to promote cross-cutting strategies aimed at enhancing students' preparation, motivation and attitude before each internship experience, so as to strengthen the link between theory and practice and promote more effective learning in different clinical contexts.
Conflicts of interest and sources of funding
The authors declare that they have no conflicts of interest. This research did not receive any external funding.
Author contributions
MC designed the study, collected the data, and wrote the first draft of the manuscript. FP and SC collected and analysed the data and critically reviewed the paper. MDM and EDS co-supervised the work, contributed to data analysis, and critically reviewed the content. AM supervised the study, and critically reviewed the manuscript. All authors participated in the final revision of the manuscript and approved the submitted version.
REFERENCES
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM-5. 5a ed. Arlington, VA: American Psychiatric Association; 2013. doi: 10.1176/appi.books.978089042559
- World Health Organisation. International classification of diseases for mortality and morbidity statistics (11th revision). Available at: https://icd.who.int. Last access: July 09, 2025
- Salari N, Rasoulpoor S, Rasoulpoor S, Shohaimi S, Jafarpour S, Abdoli N, et al. The global prevalence of autism spectrum disorder: A comprehensive systematic review and meta-analysis. Ital J of Pediatr. 2022;48(1):112. doi: 10.1186/s13052-022-01310-w
- Global Burden of Disease Study 2021 Autism Spectrum Collaborators. The global epidemiology and health burden of the autism spectrum: Findings from the Global Burden of Disease Study 2021. Lancet Psychiatry. 2025;12(2):111–21. doi: 10.1016/S2215-0366(24)00363-8
- Scattoni ML, Fatta LM, Micai M, Sali ME, Bellomo M, Salvitti T, et al. Autism spectrum disorder prevalence in Italy: A nationwide study promoted by the Ministry of Health. Child Adolesc Psychiatry Ment Health. 2023; 17:73. doi: 10.1186/s13034-023-00673-0
- Istituto Superiore di Sanità. Autismo: Prevalenza stimata nella fascia d’età 7–9 anni in Italia – Rapporto Osservatorio Nazionale Autismo. Available from: https://www.iss.it/autismo. Last access: July 09, 2025.
- Corden K, Brewer R, Cage E. A systematic review of healthcare professionals’ knowledge, self-efficacy and attitudes towards working with autistic people. Rev J Autism Dev Disord. 2022; 9:386–99. doi: 10.1007/s40489-021-00263-w
- Corsano P, Cinotti M, Guidotti L. Paediatric nurses’ knowledge and experience of autism spectrum disorders: An Italian survey. J Child Health Care. 2020;24(3):486–95. doi: 10.1177/1367493519875339
- Giarelli E, Ruttenberg J, Segal A. Continuing education for nurses in the clinical management of autism spectrum disorders: Results of a pilot evaluation. J Contin Educ Nurs. 2012;43(4):169–76. doi: 10.3928/00220124-20111101-01
- Gardner MR, Suplee P D, Jerome-D’Emilia B. Survey of nursing faculty preparation for teaching about autism spectrum disorders. Nurse Educ. 2016;41(4):212–6. doi: 10.1097/NNE.0000000000000237
- Jiménez-Ruiz I, Pérez-Cabezas V, Carrillo de la Peña MT, Pozo Rodríguez F. Training nursing students with simulated patients with autism: Communicative and emotional skills development. Clin Simul Nurs. 2022; 66:1–10. doi: 10.1016/j.nepr.2022.103488
- Gercek Ö, Arslan S, Sobcali S. Healthcare students’ perceptions and attitudes towards peers with autism spectrum disorders. J Autism Dev Disord. 2024; doi: 10.1007/s10803-024-06368-5
- Gercek E, Celikkol Sadic Ç, Kocoglu G. The level of knowledge about autism spectrum disorders among healthcare professionals in a Turkish university hospital: A cross-sectional study. Turk J Clin Psychiatry. 2024;27(1):12–20. doi: 10.5505/tjcp.2023.375056
- Cashin A, Watson N, Newman C. Nurses’ knowledge and attitudes towards people with autism spectrum disorder: An international survey. Nurse Educ Today. 2021; 103:104937. doi: 10.1016/j.nedt.2021.104937
- Miri J, Colleague. An assessment of pediatric nurses’ awareness and perceived competence regarding autism spectrum disorder. J Autism Dev Pract. 2023. doi: 10.1155/2023/4815914
- Đorđević M, Glumbić N, Troshanska J. A systematic review of individuals with autism in the healthcare system: Experiences of healthcare workers, individuals with autism and their parents. Hrv Rev Rehabil Istraz. 2025; 61(1):131–43. doi: 10.31299/hrri.61.1.8
- Ministero della Salute. Disturbi dello spettro autistico – Informazioni ufficiali e materiali informativi. Available from: https://www.salute.gov.it/portale/autismo/. Last access: July 09, 2025
- Istituto Superiore di Sanità (ISS). Giornata mondiale della Consapevolezza dell’Autismo: in Italia un bimbo ogni 77. Available from: https://www.iss.it/?p=3421. Last access: July 09, 2025
- Istituto Superiore di Sanità (ISS). Introduction and methods of the evidence-based guidelines for the diagnosis and management of autism spectrum disorder by the Italian National Institute of Health. Health Qual Life Outcomes. 2020; 18:81. doi: 10.1186/s12955-020-01320-4
- Kim E, Song S, Kim S. Development of pediatric simulation-based education: A systematic review. 2023; 22:291. doi: 10.1186/s12912-023-01458-8
- Jiménez‐Ruiz I, Pérez‐Cabezas V, Carrillo‐de‐la‐Peña MT, Pozo‐Rodríguez F. What can be improved in learning to care for people with autism? A qualitative study based on clinical nursing simulation. 66:103488. doi: 10.1016/j.nepr.2022.103488
- Bakare M, Ebigbo P, Agomoh A, Menkiti N. Knowledge about childhood autism among health workers (KCAHW) questionnaire: description, reliability and internal consistency. Clin Pract Epidemiol Ment Health. 2008;4(17). doi: 1186/1745-0179-4-17
- World Medical Association. World Medical Association Declaration of Helsinki: Ethical principles for medical research involving human subjects. JAMA. 2013;310(20):2191–2194. doi: 10.1001/jama.2013.281053
- European Parliament and Council. Regulation (EU) 2016/679 of the European Parliament and of the Council of 27 April 2016 on the protection of natural persons with regard to the processing of personal data and on the free movement of such data, and repealing Directive 95/46/EC (General Data Protection Regulation). Available at: https://eur-lex.europa.eu/eli/reg/2016/679/oj. Last access: August 27, 2025
- Sapienza Università di Roma. Comitato Etico per la Ricerca Transdisciplinare (CERT). Available at: https://www.uniroma1.it/it/pagina/cert-comitato-etico-per-la-ricerca-transdisciplinare. Last access: August 27, 2025
- Cashin A, Watson N, Newman C. A survey of registered nurses’ educational experiences and self perceived capability to care for people with intellectual disability and/or autism spectrum disorder. J Intellect Dev Disabil. 2021; doi: 10.3109/13668250.2021.1967897
- Kourtesis P, Kouklari EC, Roussos P, Mantas V, Papanikolaou K, Skaloumbakas C, et al. Virtual reality training of social skills in autism spectrum disorder: an examination of acceptability, usability, user experience, social skills, and executive functions. arXiv; 2023. doi: 10.48550/arXiv.2304.07498
- Mohammadi Rouzbahani M, Karimipour H. Using artificial intelligence to support diagnosis and care in autism spectrum disorder: A review. arXiv; 2024. doi: 10.48550/arXiv.2407.08902
- Díaz Agea JL, Macías Martínez N, Leal Costa C, Girón Poves G, García Méndez JA, Jiménez Ruiz I. What can be improved in learning to care for people with autism? A qualitative study based on clinical nursing simulation. Nurse Educ Pract. 2022; 66:103488. doi: 10.1016/j.nepr.2022.103488
- Ferrara R, Campagna G, Ricci P, Damato F, Ricci L, Iovino L, et al. Developmental Psychology and Healthcare Professions: Autism Knowledge Among Nurses: An Observational Study. Clin Pract. 2024;14(6):2693–2704. doi: 10.3390/clinpract14060212
- Erdoğan Ç, Turan T. Determination of pediatric nurses’ knowledge of and attitudes towards childhood autism and CT recommendations. Trends Pediatr. 4(2):89–95. doi: 10.59213/TP.2023.84856
- Sandanasamy S, McFarlane P, Okamoto Y, Couper AL. Leveraging machine learning to enhance nurses’ practice for autism spectrum disorder care: A narrative review. J Nurs Res Clin Pract. 2024. doi: 10.32598/JNRCP.2408.1169
- Mitchell ML, Newall FH, Heywood MG, Sokol J, Williamss KJ. Simulation-based education for staff managing aggression and high risk behaviors in children with autism spectrum disorder in the hospital setting: A pilot and feasibility cluster randomized controlled trial. J Nurs Educ Pract. 2021;11(11):48. doi: 10.5430/jnep.v11n11p48
- Lord C, Elsabbagh M, Baird G, Veenstra-Vanderweele J. Autism spectrum disorder. Lancet. 392(10146):508–80. doi: 10.1016/S0140-6736(18)31129-2
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
EXPLORING SELF-EFFICACY, FAMILY SUPPORT, AND POSTPARTUM DEPRESSION IN MOTHERS AFTER CRYPTIC PREGNANCY: A CROSS-SECTIONAL STUDY
Ifa Nofalia 1, Dwi Prasetianingati 1, Dessy Ekawati 1*
- Department of Nursing, Faculty of Health, Institute of Science and Health Technology Insan Cendekia Medika Jombang
* Corresponding author: Dessy Ekawati., Department of Nursing, Faculty of Health, Institute of Science and Health Technology Insan Cendekia Medika Jombang. E-mail: dessyekawati.s1201@gmail.com
Cite this article
ABSTRACT
Introduction: Cryptic pregnancy, or the delayed recognition of pregnancy until late gestation, poses unique psychological challenges for mothers due to the lack of prenatal preparation and sudden transition to motherhood. These circumstances may increase the risk of postpartum depression. Protective factors such as maternal self-efficacy and family support are believed to play an important role in reducing depressive symptoms after childbirth.
Objective: The purpose of this study is (1) to analyze the relationship between maternal self-efficacy and postpartum depression among mothers with a history of cryptic pregnancy, (2) to analyze the relationship between family support and postpartum depression, and (3) to assess the extent to which maternal self-efficacy and family support predict postpartum depression levels.
Materials and Methods: A cross-sectional study was conducted in Jombang Regency, East Java, Indonesia, from May to August 2025, involving 104 mothers with a history of cryptic pregnancy recruited by non-probability snowball sampling. Maternal self-efficacy was assessed using the 15-item questionnaire developed by Witungga et al. (2024; α = 0.916), family support with the 14-item questionnaire by the same authors (α = 0.836), and postpartum depression with the Edinburgh Postnatal Depression Scale (EPDS; Adli, 2022). Data were analyzed using Spearman’s rank correlation and ordinal logistic regression.
Results: Most respondents had moderate self-efficacy (72.1%), fair family support (65.4%), and no signs of postpartum depression (68.3%). Spearman’s correlation showed significant negative associations between self-efficacy (ρ = –0.426, p = 0.001) and family support (ρ = –0.398, p = 0.002) with postpartum depression. Multivariate ordinal logistic regression indicated that both self-efficacy (B = –0.462, p = 0.014, OR = 0.63, 95% CI = 0.44–0.91) and family support (B = –0.518, p = 0.012, OR = 0.60, 95% CI = 0.40–0.89) were significant protective factors, jointly explaining 28.9% of variance in postpartum depression (Nagelkerke R² = 0.289).
Conclusion: Maternal self-efficacy and family support are significant protective factors against postpartum depression in mothers with cryptic pregnancy. Strengthening maternal confidence and empowering family support systems are essential strategies to mitigate depressive symptoms in this vulnerable group.
Keywords: cryptic pregnancy, family support, maternal self-efficacy, postpartum depression
INTRODUCTION
Postpartum depression (PPD) is a major public health concern, affecting approximately 10–20% of mothers worldwide, with higher prevalence reported in low- and middle-income countries (LMICs) compared to high-income settings [1,2]. In Indonesia, national surveys have shown increasing rates of postpartum depressive symptoms, with prevalence reaching 11.2% in East Java in 2023, indicating a substantial and growing burden [3]. Despite these numbers, many cases remain undetected due to limited screening and strong sociocultural norms that discourage disclosure of psychological distress.
One critical factor influencing maternal adaptation is the level of social and family support. Numerous studies demonstrate that family support functions as a protective buffer against PPD, with inadequate support consistently linked to more severe depressive symptoms [4]. In particular, emotional responsiveness from partners and close relatives helps reduce maternal stress, facilitates the adjustment process to motherhood, and strengthens the bond between mother and infant. On the other hand, rejection, blame, or neglect from family members can worsen emotional instability and increase the risk of depressive outcomes.
Another important determinant of maternal well-being is maternal self-efficacy, defined as a mother’s belief in her ability to successfully care for her infant. Evidence indicates that higher maternal self-efficacy is associated with reduced depressive symptoms, more effective coping strategies, and better overall postpartum adjustment [5,6]. Mothers with low self-efficacy often report feelings of helplessness, decreased motivation to provide infant care, and heightened vulnerability to depression. Strengthening maternal confidence is therefore essential to preventive and therapeutic interventions in postpartum mental health.
Cryptic or denied pregnancy represents a unique context that has received little empirical attention. In this condition, pregnancy remains unrecognized until late gestation or even the onset of labor. Although traditionally considered rare, recent reviews suggest cryptic pregnancies may occur more frequently than previously assumed, and they present distinct psychosocial challenges for both mothers and families [7]. The lack of preparedness, combined with social stigma and disrupted family dynamics, places these mothers at particular risk of postpartum psychological distress. Yet, systematic research on PPD in women with cryptic pregnancies remains extremely limited.
Nurses play a central role in maternal and child health by conducting early screening, providing psychosocial education, and strengthening family-centered care systems. Understanding how maternal self-efficacy and family support influence postpartum depressive symptoms among mothers with cryptic pregnancies is therefore critical for nursing practice and policy.
Objective: This study aims to (1) analyze the relationship between maternal self-efficacy and postpartum depression among mothers with a history of cryptic pregnancy, (2) to analyze the relationship between family support and postpartum depression among mothers with a history of cryptic pregnancy, and (3) to assess the extent to which maternal self-efficacy and family support predict postpartum depression levels among mothers with a history of cryptic pregnancy.
MATERIALS AND METHODS
Study Population
This study was conducted in Jombang Regency, East Java, Indonesia, from April to July 2025. The target population included women who had experienced a cryptic pregnancy within the last one to two years. Due to the rarity and sensitive nature of cryptic pregnancy, a non-probability snowball sampling technique was employed. An initial group of participants (seed respondents) identified through community health centers and local networks served as starting points, and they referred other eligible women who had undergone similar experiences. A total of 104 respondents were successfully recruited.
The study protocol adhered to the ethical principles outlined in the Declaration of Helsinki and was approved by the Scientific and Ethics Committee of the Institute for Learning Development and Quality Assurance, Institute of Science and Health Technology Insan Cendekia Medika Jombang (Ref: LP3M/ICME/ETIK/0425/2025). All participants were fully informed about the study’s objectives and procedures and provided written informed consent prior to participation.
Inclusion Criteria
Participants were eligible for inclusion if they were women aged 18–40 years who had experienced a cryptic pregnancy that resulted in a live birth within the previous 12 months. They were required to be able to read and write in Indonesian, possess adequate cognitive capacity to complete the questionnaire independently, and provide informed consent voluntarily. These criteria were established to ensure that participants could fully understand and respond to the study instruments with accuracy and autonomy.
Exclusion Criteria
Women were excluded from the study if they had a current diagnosis or documented history of major psychiatric disorders such as schizophrenia, bipolar disorder, or major depressive disorder prior to the pregnancy. Additionally, individuals who had experienced fetal loss (miscarriage or stillbirth), or who were undergoing psychiatric treatment unrelated to postpartum depression at the time of data collection, were also excluded. These exclusion criteria aimed to minimize potential confounding effects on the assessment of postpartum depression symptoms.
Instruments
Three validated instruments were used in this study. Maternal self-efficacy was measured using a 15-item Likert-scale questionnaire developed by Witungga et al. (2024), with a Cronbach’s alpha of 0.916; responses ranged from 1 (strongly disagree) to 4 (strongly agree), and scores were categorized as low, moderate, or high. Family support was assessed using a 14-item questionnaire also developed by Witungga et al. (2024), with a Cronbach’s alpha of 0.836; each item was scored dichotomously (yes = 2, no = 1), and total scores were classified into poor, sufficient, or good support [8]. Postpartum depression was evaluated using the Edinburgh Postnatal Depression Scale (EPDS), originally developed by Cox, Holden, and Sagovsky (1987) and adapted into Indonesian by Adli (2022); this 10-item scale assesses maternal mood in the past week, with each item scored from 0 to 3 for a total range of 0–30, where higher scores indicate greater depressive severity. The EPDS has consistently demonstrated robust psychometric properties across international studies, with Cronbach’s alpha values ranging from 0.80 to 0.88 and sensitivity above 85% in detecting postpartum depression [9].
Variables
The independent variables in this study were maternal self-efficacy (categorized into low, moderate, and high) and family support (categorized into poor, fair, and good). The dependent variable was postpartum depression, measured by the Edinburgh Postnatal Depression Scale (EPDS) and categorized into three levels: no signs of depression, depression may be present, and clear signs of depression. Sociodemographic characteristics were included as control variables, consisting of age, last educational attainment, marital status, occupation, family income, place of residence, number of children (including the child from the cryptic pregnancy), gestational age at the time the pregnancy was discovered, previous pregnancy history, access to healthcare, mode of delivery, presence of a birth companion, complications during pregnancy or delivery, and history of mental health problems. Household income was recorded in Indonesian Rupiah (IDR) and converted to United States Dollars (USD) using the 2025 average exchange rate (1 USD ≈ 15,500 IDR) to enhance international readability.
Statistical Analysis
All data were analyzed using SPSS software version 26 for Windows. Descriptive statistics were employed to summarize the sociodemographic characteristics of the participants. The Kolmogorov–Smirnov test was used to assess data normality and indicated that the data were not normally distributed (p < 0.05). Spearman’s rank correlation test was used to evaluate the relationships between maternal self-efficacy, family support, and postpartum depression. To further identify the strength and direction of predictors on postpartum depression levels, ordinal logistic regression analysis was conducted. This method is appropriate given the ordinal nature of the dependent variable and non-normal data distribution. Statistical significance was defined as a p-value less than 0.05.
RESULTS
Sample Characteristics
The mean age of respondents was 28.45 years (SD = 6.14), with the largest proportion aged 25–29 years (32.7%). More than half had completed secondary education (55.8%), were married (89.4%), and worked as housewives (68.3%). More than half of the participants reported a monthly family income between 152 and less than 304 USD (55.8%), with a mean income of 139.78 USD (SD = 88.55) and a median of 187.46 USD (IQR = 44.87–210.26), and the majority resided in urban areas (60.6%). Nearly half had two children, including the child from the cryptic pregnancy (44.2%), and most discovered their pregnancy in the third trimester (≥ 28 weeks) (61.5%); a considerable proportion reported previous pregnancies, including unplanned pregnancy or miscarriage (44.2%). Access to healthcare was most frequently moderate, requiring 30–60 minutes with limited transportation (50%). The most common mode of delivery was spontaneous vaginal delivery at a healthcare facility (48.1%), with most accompanied by a husband or family member during childbirth (67.3%). The majority experienced no pregnancy or delivery complications (72.1%) and none reported a history of mental health disorders (100%). Self-efficacy assessments indicated that self-efficacy was predominantly moderate (72.1%), while family support was most often fair (65.4%). Regarding postpartum depression, most mothers exhibited no signs of depression (68.3%), while nearly one-third showed possible symptoms (31.7%). Table 1 shows the demographic data of respondents.
Characteristic Category n (%) M (SD) Median (IQR) Sociodemographic of Respondent
Age < 20 9 (8.7%) 28.45 (6.137) 28 (24 – 33) 20–24 20 (19.2%) 25–29 34 (32.7%) 30–34 21 (20.2%) ≥ 35 20 (19.2%) Last educational attainment Basic education (Elementary School or equivalent) 46 (44.2%) Secondary education (Junior/Senior High School or equivalent) 58 (55.8%) Higher education (Diploma, Bachelor’s, or Postgraduate) 0 (0%) Marital Status Married 93 (89.4%) Unmarried 3 (2.9%) Divorced/Widowed 8 (7.7%) Occupation Housewife 71 (68.3%) Employed 22 (21.2%) Unemployed 4 (3.8%) Others 7 (6.7%) Family income < USD 60,79 45 (43.3%) USD 139.78 (88.55) USD 187.46 (44.87 – 210.26) USD 152 ≤ 304 58 (55.8%) ≥ USD 303,93 1 (1.0 %) Place of residence Urban 63 (60.6%) Rural 41 (39.4 %) Number of children (including children during cryptic pregnancy) 1 child 42 (40.4 %) 2 children 46 (44.2%) ≥ 3 children 16 (15.4%) Gestational age at the time the pregnancy was discovered < 12 weeks (1st trimester) 19 (18.3%) 12–27 weeks (2nd trimester) 21(20.2%) ≥ 28 weeks (3rd trimester) 64 (61.5%) Previous Pregnancy History No previous pregnancy 27 (26.0%) Yes, all planned pregnancies 31 (29.8%) Yes, including unplanned pregnancy/miscarriage 46 (44.2%) Access to healthcare Easy (≤ 30 minutes, transportation available) 32 (30.8%) Moderate (30–60 minutes, limited transportation) 52 (50%) Difficult (> 60 minutes, poor transportation access) 20 (19.2%) Mode of delivery Spontaneous/vaginal at a healthcare facility 50 (48.1%) Spontaneous/vaginal at home 20 (19.2%) Cesarean section (C-section) at a healthcare facility 24 (23.1%) Others (e.g., without medical assistance) 10 (9.6%) Presence of a birth companion Husband/Family 70 (67.3%) Healthcare provider 32 (30.8%) Alone/No attendant 2 (1.9%) Complications during Pregnancy or delivery None 75 (72.1%) Present 29 (27.9%) Mental health history None 104 (100%) Self - Efficacy Low 0 (0%) 32.45 (5.812) 32 (28 – 37) Moderate 75 (72.1%) High 29 (27.9%) Family Support Poor 0 (0%) 28.63 (4.925) 29 (25–32) Fair 68 (65.4%) Good 36 (34.6%) Postpartum Depression No signs of depression 71 (68.3%) 10.82 (3.214) 11 (9 – 13) Depression may be present 33 (31.7%) Clear signs of depression 0 (0%) Abbreviations: n = number; % = percentage; M = mean; SD = standard deviation; IQR = interquartile range; USD = United States Dollar. All variables had complete data (n = 104).
Table 1. Sociodemographic, Self – Efficacy, Family Support and Postpartum Depression.
Relationship Between Self-Efficacy and Postpartum Depression
The Spearman correlation test results indicate a negative and significant relationship between self-efficacy and postpartum depression, with a correlation coefficient of ρ = –0.426 and a significance value of p value = 0.001 (Table 2). This finding suggests that higher levels of self-efficacy are associated with lower levels of postpartum depression. The strength of the relationship is moderate and remains statistically significant.
Variable M (SD) Median (IQR) Sig. (2-tailed) Spearman Correlation Self-efficacy 32.45 (5.812) 32 (28 – 37) Correlation coefficient ρ = –0.426, p value = 0.001**
Postpartum depression 10.82 (3.214) 11 (9 – 13) *p < 0.05, **p < 0.01, SD = standard deviation, IRQ = interquartile range [Q1, Q3]; M = mean.
Table 2. Relationship Between Self-Efficacy and Postpartum Depression (N = 104).
Figure 1 presents a scatter plot showing a moderate negative correlation (ρ = –0.426, p value = 0.001) between self-efficacy and postpartum depression. This correlation suggests that higher levels of maternal self-efficacy are associated with lower levels of postpartum depression. The results also indicate that the relationship between these two variables is moderate and statistically significant.
Figure 1. Scatter Plot of Postpartum Depression Levels by Self-Efficacy Levels. The trend line is in red.
The crosstabulation analysis further shows the distribution of respondents based on self-efficacy levels and postpartum depression symptoms (Table 3).
Self-Efficacy Postpartum Depression Total No signs of depression Depression may be present Moderate 55 20 75 High 16 13 29 Total 71 33 104 Table 3. Crosstabulation of Self-Efficacy and Postpartum Depression.
Among those with moderate self-efficacy, 55 mothers reported no signs of depression, while 20 mothers showed possible signs of depression, totaling 75 individuals. In contrast, among those with high self-efficacy, 16 mothers reported no signs of depression and 13 mothers experienced possible depression, totaling 29 individuals.\
Relationship Between Family Support and Postpartum Depression
Correlation analysis using Spearman's correlation coefficient indicates a negative and significant relationship between family support and postpartum depression, with a correlation coefficient of ρ = –0.398 and a significance value of p value = 0.002 (Table 4). This suggests that higher levels of family support are associated with lower levels of postpartum depression, and the strength of this relationship is moderate and statistically significant.
Variable M (SD) Median (IQR) Sig. (2-tailed) Spearman Correlation Family support 28.63 (4.925) 29 (25–32) Correlation coefficient ρ = –0.398, p value = 0.002**
Postpartum depression 10.82 (3.214) 11 (9–13) *p < 0.05, **p < 0.01, SD = standard deviation, IRQ = interquartile range [Q1, Q3]; M = mean.
Table 4. Relationship Between Family Support and Postpartum Depression (N = 104)
Figure 2 presents a scatter plot to visualize the joint values for the family support and postpartum depression variables, and to observe possible relationships, trends, between the variables. We observed from Figure 2 a moderate negative correlation (ρ = –0.398, p value = 0.002) between family support and postpartum depression. This correlation suggests that higher levels of family support are associated with lower levels of postpartum depression. The results also indicate that the relationship between these two variables is moderate and remains statistically significant.
Figure 2. Scatter Plot of Postpartum Depression Levels by Family Support Levels. The trend line is in red.
The crosstabulation analysis further shows the distribution of respondents based on family support and postpartum depression symptoms (Table 5).
Family Support Postpartum Depression Total No signs of depression Depression may be present Fair 44 24 68 Good 27 9 36 Total 71 33 104 Table 5. Crosstabulation of Family Support and Postpartum Depression
Among mothers with fair family support, 44 reported no signs of depression while 24 experienced possible signs of depression, totaling 68 individuals. Conversely, among those with good family support, 27 mothers reported no depression and 9 mothers experienced possible depression, totaling 36 individuals.
The Combined Effect of Maternal Self-Efficacy and Family Support on Postpartum Depression
The results of the multivariate ordinal logistic regression analysis showed that both maternal self-efficacy and family support have significant effects on postpartum depression. The overall model shows a Nagelkerke R² value of 0.289, indicating that the combination of maternal self-efficacy and family support explains 28.9% of the variability in postpartum depression levels.
In Table 6, we reported the results of the multivariate ordinal logistic regression analysis of maternal self-efficacy and family support on postpartum depression.
Predictor B SE Wald OR (Exp(B)) 95% CI for OR p value Maternal self-efficacy -0.462 0.188 6.030 0.63 0.44 – 0.91 0.014 * Family support -0.518 0.205 6.367 0.60 0.40 – 0.89 0.012 * -2 Log Likelihood 178.21 Nagelkerke R² 0.289 *Significant at p < 0.05
Table 6. Multivariate Ordinal Logistic Regression of Maternal Self-Efficacy and Family Support on Postpartum Depression (n = 104).
The parameter estimates indicate that maternal self-efficacy has a significant negative association with postpartum depression (B = –0.462, Wald = 6.018, p value = 0.014, OR = 0.63, 95% CI = 0.44–0.91). This means that mothers with higher self-efficacy are less likely to experience postpartum depression. Similarly, family support also shows a significant negative association with postpartum depression (B = –0.518, Wald = 6.367, p value = 0.012, OR = 0.60, 95% CI = 0.40–0.89), indicating that greater family support reduces the risk of postpartum depression. These findings suggest that maternal self-efficacy and family support are both protective factors against postpartum depression, and their combined contribution highlights the importance of strengthening personal and social resources for mothers during the postpartum period.
DISCUSSION
This study demonstrates that maternal self-efficacy has a significant negative relationship with postpartum depression among mothers with a history of cryptic pregnancy. This aligns with the first objective of the study, which was to examine the association between self-efficacy and depressive symptoms. The finding supports Bandura’s theory of self-efficacy, which emphasizes the individual’s belief in their ability to organize and carry out tasks as a key factor in managing stress and emotional well-being [9]. Mothers with higher self-efficacy are able to adapt more effectively to the demands of motherhood, thereby lowering their vulnerability to depression. In the context of cryptic pregnancy, where mothers experience limited prenatal preparation, reduced medical supervision, and a sudden transition to motherhood, self-efficacy becomes an essential psychological resource [10]. Similar results have been reported in other countries. For instance, Chase et al. (2021) found that low maternal self-efficacy was strongly associated with higher levels of postpartum depression, suggesting that interventions aimed at improving confidence can be applied across different cultural settings [11].
The second objective of the study was to examine the role of family support in maternal mental health. Family support also showed a significant negative association with postpartum depression, reinforcing the importance of social and cultural contexts. Support from close relatives, especially spouses, provides emotional reassurance, practical help, and a sense of security, all of which buffer against the stress of childbirth and early parenting [12]. This result echoes findings from Delong et al. (2022), who demonstrated that social support plays a protective role in maternal well-being and strengthens maternal–infant interactions [13]. In Indonesia, where collectivist culture and family involvement in childcare are deeply rooted, family support becomes even more crucial. Mothers who experience cryptic pregnancy may feel shocked, unprepared, or even stigmatized due to the late discovery of their condition. In such situations, family members, particularly nurses within the community or family health settings, play a vital role in reducing stigma and supporting maternal adjustment [14].
The third objective of the study was to explore the combined effects of maternal self-efficacy and family support. The multivariate regression analysis confirmed that these two factors jointly predict postpartum depression, explaining nearly one-third of the variance. This suggests that personal psychological resources and external social support interact to shape maternal mental health outcomes. Comparable results have been found in other regions, where interventions that simultaneously enhance coping skills and involve family members proved more effective in reducing postpartum depression than those focusing on a single factor [15]. From a nursing perspective, this highlights the need for nurses to not only build mothers’ confidence through education and counseling but also to engage families in the care process [16]. The clinical implication is that nursing practice in both community and hospital settings should adopt a family-centered approach to maternal mental health. Furthermore, for future research, cross-cultural studies could provide valuable insights into how these factors operate in different healthcare systems and societies, and how nurses can tailor interventions to local needs.
Limitations
This study has several limitations. First, the use of a snowball sampling technique limits the representativeness of the sample and increases the risk of selection bias, as respondents were recruited through networks and may not reflect the broader population of mothers with cryptic pregnancy. Second, the reliance on self-reported questionnaires raises the possibility of recall bias and social desirability bias, where participants may underreport depressive symptoms or overstate family support. Third, this study did not control for other important psychosocial or environmental variables, such as marital conflict, domestic violence, or financial instability, which may independently contribute to postpartum depression. Fourth, the research was conducted in a single geographic area (Jombang Regency, East Java), and thus the findings may be influenced by local cultural norms and may not be generalizable to other populations with different sociocultural backgrounds. Finally, the cross-sectional design of this study prevents causal inferences, as it only identifies associations rather than longitudinal patterns. Future studies should adopt prospective or longitudinal designs with random sampling to establish causal pathways and improve external validity.
CONCLUSION
According to this study, maternal self-efficacy and family support are significant protective factors against postpartum depression among mothers with a history of cryptic pregnancy. Mothers with higher self-efficacy and stronger family support are less likely to experience depressive symptoms after childbirth. These findings reinforce previous evidence that both personal psychological resources and social environments are central in determining maternal mental health outcomes. The study highlights the urgent need for interventions that not only enhance maternal self-efficacy through counseling, psychoeducation, and peer support but also strengthen family involvement in postpartum care. Given that cryptic pregnancy presents unique psychological challenges due to the sudden recognition of pregnancy, integrated strategies focusing on both individual empowerment and family support systems may serve as effective preventive measures for postpartum depression.
Author Contributions
Study conceptualization and design (I.N., D.P., D.E.), data collection and analysis (I.N., D.E.), interpretation and manuscript drafting (I.N., D.P., D.E.), critical manuscript revision (D.E., D.P.). All authors have read and approval the final version of the manuscript.
Local Ethics Committee approval
This study was approved by the Research Ethics Committee of the Institute of Science and Health Technology Insan Cendekia Medika Jombang (reference number LP3M/ICME/ETIK/0425/2025 on February 10, 2025.
Conflict of Interest
The authors declare no conflicts of interest.
Funding Sources
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Acknowledgements
We extend our deepest gratitude to the mothers who shared their experiences of cryptic pregnancy and postpartum adjustment, as well as their families who supported this study by participating in interviews and completing the questionnaires. Without their openness, trust, and participation, this research would not have been possible.
REFERENCES
- Roddy Mitchell A, Gordon H, Lindquist A, Walker SP, Homer CSE, Middleton A, et al. Prevalence of Perinatal Depression in Low- and Middle-Income Countries: A Systematic Review and Meta-analysis. JAMA Psychiatry 2023;80:425–31. https://doi.org/10.1001/jamapsychiatry.2023.0069.
- Shorey S, Chee CYI, Ng ED, Chan YH, Tam WWS, Chong YS. Prevalence and incidence of postpartum depression among healthy mothers: A systematic review and meta-analysis. J Psychiatr Res 2018;104:235–48. https://doi.org/10.1016/j.jpsychires.2018.08.001.
- Bestari, A. D., Westriningrum, L., Didah, D., Gumilang, L., & Mandiri,
(2025). Faktor-Faktor yang Berhubungan dengan Resiko Depresi
Postpartum pada Ibu Nifas di Kota Bandung. Malahayati Nursing Journal,
7(2), 658-674. https://doi.org/10.33024/mnj.v7i2.17747- Cho H, Lee K, Choi E, Cho HN, Park B, Suh M, et al. Association between social support and postpartum depression. Sci Rep 2022;12. https://doi.org/10.1038/S41598-022-07248-7,.
- Han L, Zhang J, Yang J, Yang X, Bai H. Between Personality Traits and Postpartum Depression: The Mediated Role of Maternal Self-Efficacy. Neuropsychiatr Dis Treat 2022;18:597. https://doi.org/10.2147/NDT.S346327.
- Zarroug M, Altaf MF, Shaikh S, Tidjani A, Bashir O, Ayash MI, et al. The Prevalence and Risk Factors of Postpartum Depression Among Saudi Arabian Women—A Systematic Review and Meta-Analysis. Healthc 2025;13:2040. https://doi.org/10.3390/HEALTHCARE13162040/S1.
- Duckitt K. Cryptic pregnancy. Case Reports Women’s Heal 2023;38:e00503. https://doi.org/10.1016/J.CRWH.2023.E00503.
- Witungga RAA, Purwatiningrum DA, Gumanti KA, Sariati Y. The Relationship Of Maternal Self-Efficacy And Family Social Support To The Achivement Of Maternal Identity In Postpartum Women With A History Of Early Marriage. JKM (Jurnal Kebidanan Malahayati) 2024;10:1349–58. https://doi.org/10.33024/jkm.v10i12.17682.
- Adli FK. Edinburgh Post-natal Depression Scale (EPDS): Deteksi Dini dan Skrining Depresi Post-partum. J Kesehat 2022;13:430–6. https://doi.org/10.26630/JK.V13I2.2741.
- Shuriah NN, McFarland E, Spenn B, Butz McManus K, McManus B. Denial of Pregnancy or Cryptic Pregnancy. BIO4960 Pract Biol I 2024.
- Chase T, Shah A, Maines J, Fusick A. Psychotic pregnancy denial: a review of the literature and its clinical considerations. J Psychosom Obstet Gynecol 2021;42:253–7. https://doi.org/10.1080/0167482X.2020.1789584,.
- Chechko N, Losse E, Stickel S. A case report involving the experience of pervasive pregnancy denial: detailed observation of the first 12 postpartum weeks. BMC Psychiatry 2022;22. https://doi.org/10.1186/s12888-022-04377-1.
- Delong H, Eutrope J, Thierry A, Sutter-Dallay AL, Vulliez L, Gubler V, et al. Pregnancy denial: a complex symptom with life context as a trigger? A prospective case–control study*. BJOG An Int J Obstet Gynaecol 2022;129:485–92. https://doi.org/10.1111/1471-0528.16853,.
- Dlamini LP, Hsu YY, Shongwe MC, Wang ST, Gau ML. Maternal Self-Efficacy as a Mediator in the Relationship Between Postpartum Depression and Maternal Role Competence: A Cross-Sectional Survey. J Midwifery Women’s Heal 2023;68:499–506. https://doi.org/10.1111/JMWH.13478;JOURNAL:JOURNAL:18791565B;WGROUP:STRING:PUBLICATION.
- Mercan Y, Selcuk KT. Association between postpartum depression level, social support level and breastfeeding attitude and breastfeeding self-efficacy in early postpartum women. PLoS One 2021;16:e0249538. https://doi.org/10.1371/JOURNAL.PONE.0249538.
- César-Santos B, Bastos F, Dias A, Campos MJ. Family Nursing Care during the Transition to Parenthood: A Scoping Review. Healthcare 2024;12:515. https://doi.org/10.3390/HEALTHCARE12050515.
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
EFFECTIVENESS OF TAPPING AND MASSAGE TECHNIQUE IN PROMOTING VENOUS DILATION FOR PERIPHERAL INTRAVENOUS CATHETER INSERTION: A SYSTEMATIC REVIEW
Rita Citarella 1*, Aniello Lanzuise 2, Vittoria Masullo 3 Marco Abagnale 4
- Department of Surgery and Anesthesia, “Umberto I” Hospital of Nocera Inferiore”, 84014, Salerno, Italy.
- Corporate Health Management, "Ospedale dei Colli",80131, Napoli, Italy.
- University surgical clinic, “San Giovanni di Dio e Ruggi d’Aragona”,84131, Salerno, Italy.
- Department of Critical Care, M. Scarlato Hospital, 84018, Scafati, Salerno, Italy.
* Corresponding author: Rita Citarella, Department of Surgery and Anesthesia at Umberto I Hospital of Nocera Inferiore, 84014 Salerno, Italy. E-mail: rita.citarella.91@gmail.com
Cite this article
ABSTRACT
Introduction: Peripheral intravenous catheter (PIVC) insertion is a common clinical procedure, yet achieving successful venous access, particularly at the first attempt, remains a significant challenge. Techniques such as tapping and massage have been proposed to enhance venous dilation and facilitate cannulation.
Objective: This study aims to evaluate and compare the effectiveness of tapping and massage each compared to tourniquet-only application, in promoting peripheral venous dilation.
Materials and Methods: This study is a systematic review conducted following the PRISMA 2020 guidelines. A systematic search was conducted in PubMed, Scopus, MEDLINE, and CINAHL. All databases were accessed in April 2025 to retrieve studies published between January 2015 and April 2025. Studies were eligible if they involved adult participants, compared tapping and/or massage with standard tourniquet application or control, and reported outcomes related to vein diameter, cross-sectional area, or palpability. Quality assessment was performed using the NIH Quality Assessment Tool and for the risk of bias was used the ROBINS-I.
Results: Tapping was associated with modest improvements in vein diameter and palpability in some studies, but not in others. Massage showed improvements in palpability, yet no clear advantage over tapping was consistently demonstrated. No clear clinical advantage of one technique over the other was consistently demonstrated, and no study assessed outcomes such as first-attempt success rate. Methodological limitations included small sample sizes, and lack of randomization.
Conclusions: Both tapping and massage may promote venous dilation in young, healthy adults, but the evidence is limited. The generalizability of these findings to broader clinical populations, including elderly patients and those with difficult venous access, is uncertain. High-quality studies involving diverse populations and standardized outcome measures are needed to establish the effectiveness of these techniques in routine clinical practice.
Keywords: tapping technique, massage technique, venous dilation, peripheral intravenous catheter, phlebotomy, venipuncture.
INTRODUCTION
Peripheral intravenous catheter (PIVC) placement is a common procedure performed in approximately 80% of hospitalized patients to administer infusion solutions and antibiotics [1]. It is one of the most commonly recommended vascular access methods for short-term infusion therapy (≤7 days) and administration of low-osmolarity or low-irritation drugs [2,3]. It is also approved for emergency situations, regardless of the drugs administered [4]. The demand for PIVC in older adults is increase due to the rapid growth of the aging population [5]. However, several studies have reported higher initial failure rates of PIVC insertion in older adults up to 39% compared to younger adults, where rates range from 12% to 30% [6]. PIVC failure not only leads to complications and delayed treatments but also affects patient’s quality of life and increases healthcare costs [7].
For safe and successful PIVC insertion, it is crucial to select an appropriate vein. Traditionally, vein selection is based on visual inspection, palpation, or imaging techniques such as infrared or ultrasound devices. Larger veins are generally recommended for easier cannulation [8], and achieving adequate venous dilation is essential for the procedure’s success. Current guidelines recommend inserting the PIVC into the forearm cutaneous veins rather than the median cubital vein, due to considerations of daily activities and lower complication risks [9,10]. However, the forearm veins are thinner, branch more peripherally, and are often more difficult to access compared to the median cubital vein [11]. As a result, between 12% and 26% of patients require multiple attempts for successful PIVC insertion following an initial failure [12]. Repeated PIVC punctures increase the risk of complications such as pain, nerve damage, and accidental arterial puncture [13]. Furthermore, these multiple attempts result in additional time and staffing costs associated with the procedure [14]. Difficulty in establishing peripheral intravenous access is a common clinical challenge, particularly in patients with fragile veins, obesity, dehydration, or chronic illnesses [15]. Failed first-attempt cannulation can delay treatment, increase patient discomfort, and raise healthcare costs. Nurses are primarily responsible for PIVC placement in most clinical settings [16]. Therefore, identifying and applying effective, evidence-based techniques to facilitate venous dilation is a key component of nursing practice, with direct implications for patient safety and quality of care [17]. Understanding which technique whether tapping, massaging, or other methods is the most effective in promoting venous dilation is essential for optimizing clinical practice. Evidence-based recommendations are needed to guide nurses in selecting the best approach, ensuring both procedural success and patient comfort [18]. PIVC insertion relies on palpation to identify a vein's Therefore, it is essential to ensure adequate venous dilation and to carefully select an appropriate vein for PIVC insertion through palpation. The most commonly used technique for promoting venous dilation involves applying a tourniquet to induce venous stasis [19]. However, relying solely on a tourniquet may not always provide sufficient dilation. To enhance the effect of the tourniquet, nurses often instruct patients to open and close their fist or maintain a clenched fist. Additionally, they may massage the forearm, tap over the vein [20], or apply warmth to the forearm [21].
Among these methods, tapping and massaging are proactive techniques in which the nurse provides direct stimulation to the vein. These techniques do not require the patient's active participation or the use of additional equipment, and they can be implemented quickly and easily in various clinical situations [22]. Tapping is recommended when the target vein is not prominent and/or needs to be made more prominent for venipuncture [23] and is an effective method of vasodilation [24]. The following factors are reported to be involved in vasodilation mechanisms by tapping: the production of nitric oxide (NO) and other vasoactive substances from the endothelium by mechanical stress, such as shear stress, and the axon reflex associated with pain stimulation [25]. Despite the widespread use of techniques such as tapping and massaging in clinical practice, current international guidelines lack specific recommendations regarding their effectiveness in promoting venous dilation [26]. Limited studies have investigated the physiological mechanisms and clinical efficacy of these manual stimulation techniques, highlighting the need for further research to establish evidence-based best practices.
Purpose
This systematic review aims to evaluate and compare the effectiveness of tapping and massage each compared to tourniquet-only application, in promoting peripheral venous dilation.
MATERIALS AND METHODS
We conducted a systematic review following the preferred reporting items for systematic reviews and meta-analyses, the PRISMA statement version 2020 [26]. We used the PICO (Table 1) framework.
|
POPOLATION |
Patients undergoing peripheral intravenous catheter (PIVC) insertion |
|
INTERVENTION |
Tapping or massage as techniques for venous dilation |
|
COMPARISON |
Tourniquet |
|
OUTCOME |
Efficacy of techniques in promoting venous dilation, measured by changes in vein diameter, cross-sectional area and vein palpability. |
Table 1. PICO framework
Eligibility Criteria
We included both observational and experimental studies that: involved patients undergoing peripheral intravenous catheter (PIVC) insertion; compared tapping and/or massage with tourniquet-only or control techniques; reported outcomes related to venous dilation, such as vein diameter, cross-sectional area, or palpability; were published in English in peer-reviewed journals from January 2015 to April 2025. We excluded: studies on pediatric or animal populations; systematic reviews, commentaries, letters, and abstracts; studies involving non-manual techniques (ultrasound-guided cannulation or pharmacologic interventions). We excluded pediatric patients, elderly individuals, and those with chronic conditions because the available literature on this topic primarily involved healthy adult participants. This choice reflects the current scope of published evidence rather than a methodological preference.
Search Strategy
We performed a comprehensive literature search in PubMed, Scopus, MEDLINE (via EBSCOhost), and CINAHL. The literature search covered the period from January to April 2025. All databases were accessed in April 2025. We used relevant MeSH terms and Boolean operators. A full list of search strings is reported in Table 2.
|
DATABASE |
SEARCH STRING |
|
PubMed |
("phlebotomy"[MeSH Terms] OR "phlebotomy"[All Fields] OR "venipuncture"[All Fields] OR "venipunctures"[All Fields] OR ("phlebotomy"[MeSH Terms] OR "phlebotomy"[All Fields] OR "phlebotomies"[All Fields]) OR (("cutaneous"[All Fields] OR "cutaneously"[All Fields] OR "cutanous"[All Fields]) AND ("vein s"[All Fields] OR "veins"[MeSH Terms] OR "veins"[All Fields]))) AND ("mechanical"[All Fields] OR "mechanically"[All Fields] OR "mechanicals"[All Fields] OR "mechanics"[MeSH Terms] OR "mechanics"[All Fields] OR "mechanic"[All Fields] OR ("tapped"[All Fields] OR "tapping"[All Fields] OR "tappings"[All Fields]) OR ("massage"[MeSH Terms] OR "massage"[All Fields] OR "massages"[All Fields] OR "massaged"[All Fields] OR "massager"[All Fields] OR "massagers"[All Fields] OR "massaging"[All Fields]) OR ("palpate"[All Fields] OR "palpated"[All Fields] 24/04/2025 120 9 OR "palpates"[All Fields] OR "palpating"[All Fields] OR "palpation"[MeSH Terms] OR "palpation"[All Fields] OR "palpations"[All Fields] OR "palpator"[All Fields] OR "palpators"[All Fields])) AND ((("veins"[MeSH Terms] OR "veins"[All Fields] OR "vein"[All Fields]) AND ("visibilities"[All Fields] OR "visibility"[All Fields] OR "visible"[All Fields] OR "visibles"[All Fields])) OR ("veins"[MeSH Terms] OR "veins"[All Fields] OR "venous"[All Fields]) OR ("venodilating"[All Fields] OR "venodilation"[All Fields] OR "venodilator"[All Fields] OR "venodilators"[All Fields]) OR ("vasodilate"[All Fields] OR "vasodilated"[All Fields] OR "vasodilates"[All Fields] OR "vasodilating"[All Fields] OR "vasodilation"[MeSH Terms] OR "vasodilation"[All Fields] OR "vasodilations"[All Fields] OR "vasodilative"[All Fields] OR "vasodilator agents"[Pharmacological Action] OR "vasodilator agents"[Supplementary Concept] OR "vasodilator agents"[All Fields] OR "vasodilator"[All Fields] OR "vasodilator agents"[MeSH Terms] OR ("vasodilator"[All Fields] AND "agents"[All Fields]) OR "vasodilators"[All Fields])) |
|
SCOPUS |
( INDEXTERMS ( phlebotomy ) OR ALL ( phlebotomy ) OR ALL ( venipuncture ) OR ALL ( venipunctures ) OR ( INDEXTERMS ( phlebotomy ) OR ALL ( phlebotomy ) OR ALL ( phlebotomies ) ) OR ( ( ALL ( cutaneous ) OR ALL ( cutaneously ) OR ALL ( cutanous ) ) AND ( ALL ( "vein s" ) OR INDEXTERMS ( veins ) OR ALL ( veins ) ) ) ) AND ( ALL ( mechanical ) OR ALL ( mechanically ) OR ALL ( mechanicals ) OR INDEXTERMS ( mechanics ) OR ALL ( mechanics ) OR ALL ( mechanic ) OR ( ALL ( tapped ) OR ALL ( tapping ) OR ALL ( tappings ) ) OR ( INDEXTERMS ( massage ) OR ALL ( massage ) OR ALL ( massages ) OR ALL ( massaged ) OR ALL ( massager ) OR ALL ( massagers ) OR ALL ( massaging ) ) OR ( ALL ( palpate ) OR ALL ( palpated ) OR ALL ( palpates ) OR ALL ( palpating ) OR INDEXTERMS ( palpation ) OR ALL ( palpation ) OR ALL ( palpations ) OR ALL ( palpator ) OR ALL ( palpators ) ) ) AND ( ( ( INDEXTERMS ( veins ) OR ALL ( veins ) OR ALL ( vein ) ) AND ( ALL ( visibilities ) 24/04/2025 282 52 OR ALL ( visibility ) OR ALL ( visible ) OR ALL ( visibles ) ) ) OR ( INDEXTERMS ( veins ) OR ALL ( veins ) OR ALL ( venous ) ) OR ( ALL ( venodilating ) OR ALL ( venodilation ) OR ALL ( venodilator ) OR ALL ( venodilators ) ) OR ( ALL ( vasodilate ) OR ALL ( vasodilated ) OR ALL ( vasodilates ) OR ALL ( vasodilating ) OR INDEXTERMS ( vasodilation ) OR ALL ( vasodilation ) OR ALL ( vasodilations ) OR ALL ( vasodilative ) OR ALL ( "vasodilator agents" ) OR CHEM ( term ) OR ALL ( "vasodilator agents" ) OR ALL ( vasodilator ) OR INDEXTERMS ( "vasodilator agents" ) OR ( ALL ( vasodilator ) AND ALL ( agents ) ) OR ALL ( vasodilators ) ) ) AND ( LIMIT-TO ( SUBJAREA , "NURS" ) ) |
|
MEDLINE |
((MH phlebotomy+) OR phlebotomy OR venipuncture OR venipunctures OR ((MH phlebotomy+) OR phlebotomy OR phlebotomies) OR ((cutaneous OR cutaneously OR cutanous) AND ("vein s" OR (MH veins+) OR veins))) AND (mechanical OR mechanically OR mechanicals OR (MH mechanics+) OR mechanics OR mechanic OR (tapped 24/04/2025 143 OR tapping OR tappings) OR ((MH massage+) OR massage OR massages OR massaged OR massager OR massagers OR massaging) OR (palpate OR palpated OR palpates OR palpating OR (MH palpation+) OR palpation OR palpations OR palpator OR palpators)) AND ((((MH veins+) OR veins OR vein) AND (visibilities OR visibility OR visible OR visibles)) OR ((MH veins+) OR veins OR venous) OR (venodilating OR venodilation OR venodilator OR venodilators) OR (vasodilate OR vasodilated OR vasodilates OR vasodilating OR (MH vasodilation+) OR vasodilation OR vasodilations OR vasodilative OR "vasodilator agents" OR (MW "vasodilator agents") OR "vasodilator agents" OR vasodilator OR (MH "vasodilator agents+") OR (vasodilator AND agents) OR vasodilators)) |
|
CINAHL |
((MH phlebotomy+) OR phlebotomy OR venipuncture OR venipunctures OR ((MH phlebotomy+) OR phlebotomy OR phlebotomies) OR ((cutaneous OR cutaneously OR cutanous) AND ("vein s" OR (MH veins+) OR 24/04/2025 40 veins))) AND (mechanical OR mechanically OR mechanicals OR (MH mechanics+) OR mechanics OR mechanic OR (tapped OR tapping OR tappings) OR ((MH massage+) OR massage OR massages OR massaged OR massager OR massagers OR massaging) OR (palpate OR palpated OR palpates OR palpating OR (MH palpation+) OR palpation OR palpations OR palpator OR palpators)) AND ((((MH veins+) OR veins OR vein) AND (visibilities OR visibility OR visible OR visibles)) OR ((MH veins+) OR veins OR venous) OR (venodilating OR venodilation OR venodilator OR venodilators) OR (vasodilate OR vasodilated OR vasodilates OR vasodilating OR (MH vasodilation+) OR vasodilation OR vasodilations OR vasodilative OR "vasodilator agents" OR (MW "vasodilator agents") OR "vasodilator agents" OR vasodilator OR (MH "vasodilator agents+") OR (vasodilator AND agents) OR vasodilators)) |
Table 2. Search String
Study Selection
After removing duplicates, two authors (RC and MA) independently screened titles and abstracts. Full texts were retrieved when eligibility was unclear. Discrepancies were resolved through discussion. The selection process followed PRISMA 2020 recommendations and was supported by Rayyan software [27], while to organize and manage the references we used Zootero.
Data Extraction
Two authors independently extracted data using a predefined form. Extracted information included author, year, country, study design, sample size, participant characteristics, intervention, and main outcomes. Final verification was conducted by RC and MA.
Quality Assessment and Risk of Bias
Methodologically, two authors (RC, MA) independently assessed the quality of the included articles using tools from the National Institutes of Health (NIH) [28] for observational and controlled intervention studies. The first author (RC) was the final decider of the overall quality assessment. The quality assessment criteria included the following items:
Q1. Clear statement of objectives
Q2. Adequacy of sample size
Q3. Clear description of participant characteristics
Q4. Description of intervention techniques (tapping, massage, or control)
Q5. Description of outcome measures (venous diameter, cross-sectional area, palpability)
Q6. Appropriateness of data analysis methods
Q7. Use of validated outcome measures
Q8. Blinding of outcome assessors
Q9. Randomization process described
Q10. Allocation concealment
Q11. Reporting of dropout, or missing data
Q12. Reporting of study limitations
Q13. Ethical approval and consent
The summary of the study quality assessment is shown in Table 3.
|
Authors |
Q1 |
Q2 |
Q3 |
Q4 |
Q5 |
Q6 |
Q7 |
Q8 |
Q9 |
Q10 |
Q11 |
Q12 |
Q13 |
|
Ichimura et al., 2015 [30] |
Y |
N |
Y |
Y |
Y |
Y |
Y |
N |
N |
N |
Y |
Y |
Y |
|
Yasuda et al., 2019 [31] |
Y |
N |
Y |
Y |
Y |
Y |
Y |
N |
N |
N |
Y |
Y |
Y |
|
Yasuda et al., 2020 [32] |
Y |
N |
Y |
Y |
Y |
Y |
Y |
N |
N |
N |
Y |
Y |
Y |
|
Yasuda et al., 2023 [33] |
Y |
N |
Y |
Y |
Y |
Y |
Y |
N |
N |
N |
Y |
Y |
Y |
Legend: Y: YES (the study met the criterion); N: NO (the study did not meet the criterion).
Table 3. Quality assessment table Summary of studies quality assessment based on NIH
From the table, we can deduce that all studies responded positively (Y) to most of the criteria related to the description of interventions, outcomes, statistical analyses, participants, and ethical approval (Q1, Q3–Q7, Q11–Q13). However, common limitations were identified in the criteria related to randomization procedures (Q2, Q9), blinding of outcome assessors (Q8), and allocation concealment (Q10), where all studies showed an “N”. This indicates that, while the studies provided a clear description of interventions and outcomes, they lacked critical information about how participants were allocated to groups (randomization), how blinding was implemented, and how selection bias was avoided (allocation concealment). Furthermore, all included studies were conducted exclusively on young and healthy adult populations (ages 20–29 years), limiting the generalizability of findings to broader clinical contexts.
The risk of bias in the included studies was assessed using the ROBINS-I (Risk Of Bias In Non-randomized Studies - of Interventions) tool [29]. This tool evaluates the risk of bias across seven domains using three judgements (serious, moderate and low): confounding (D1), selection of participants (D2), classification of interventions (D3), deviations from intended interventions(D4), missing data (D5), measurement of outcomes (D6), and selection of reported results. This system allowed a clear visualization of potential sources of bias across the studies.
The final judgment was based on a consensus between two independent authors, with the first two authors (RC, MA) acting as the final decision-maker in case of disagreements. Given the quasi-experimental nature of the included studies, ROBINS-I [29] was considered the most appropriate method for evaluating bias in this systematic review. (Figure 1)

Figure 1. Risk of bias assessment in the selected articles according to ROBINS-I tool.
In summary, all four studies showed moderate to serious concerns across several domains, particularly due to lack of randomization details, blinding, potential confounding factors, and small sample sizes. These methodological limitations, combined with the exclusive inclusion of young healthy adult participants, should be taken into account when interpreting the findings.
RESULTS
A total of 585 records were identified through database searches (PubMed: 120; Scopus: 282; MEDLINE: 143; CINAHL: 40). After removing 120 duplicates, 465 records remained for title and abstract screening. Of these, 442 were excluded based on inclusion criteria. Twenty-three full-text articles were assessed, and 4 studies met all eligibility criteria and were included in the final synthesis (see PRISMA flow diagram, Figure 2).
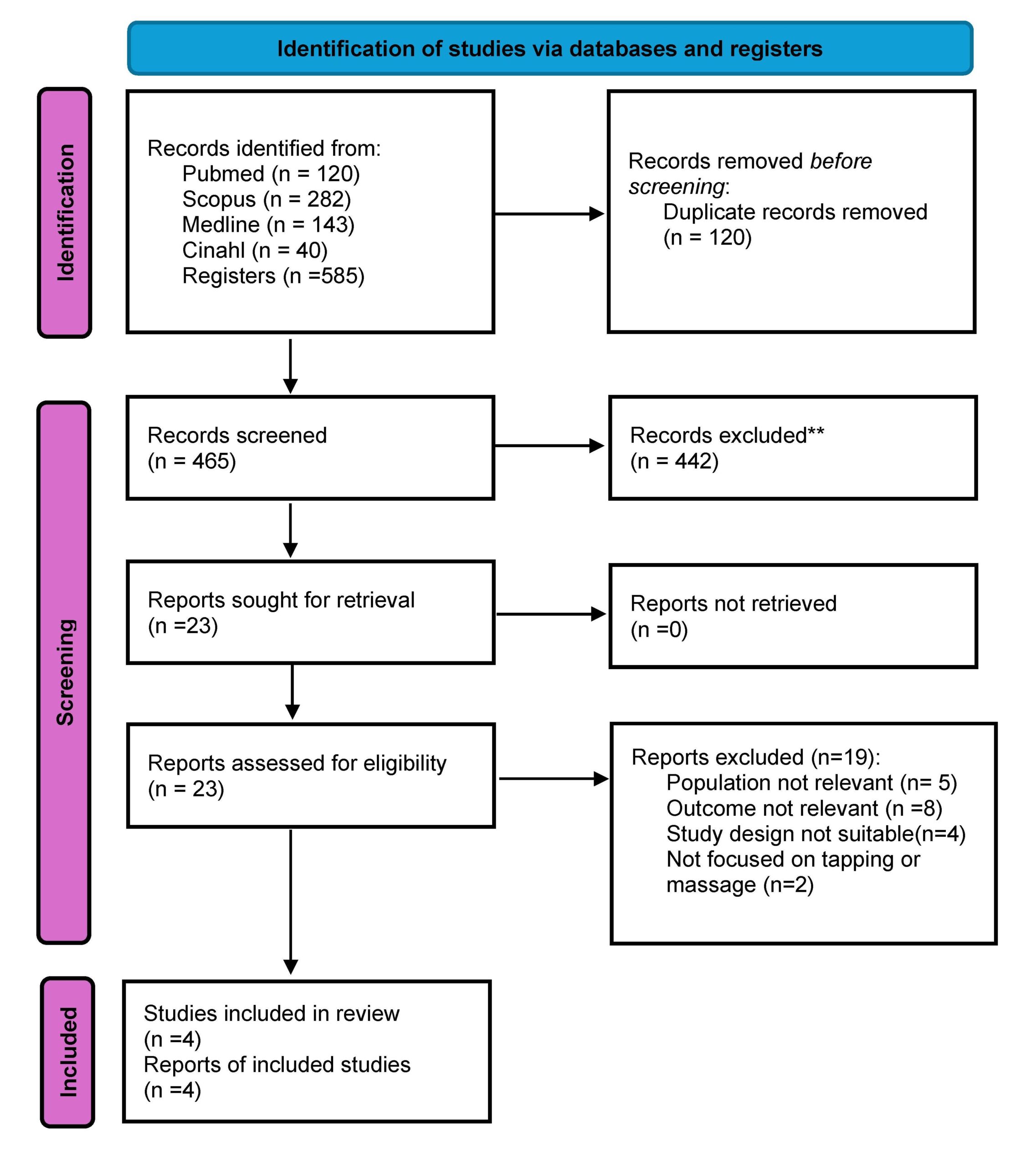
Figure 2. Prisma flowchart for literature search
All included studies were conducted in Japan between 2015 and 2023 and involved a total of 120 healthy adult participants, mostly nursing students with a mean age between 20 and 29 years. The designs were either quasi-experimental or observational. The interventions evaluated included tapping, massage, and tourniquet-only techniques, aimed at enhancing venous dilation prior to PIVC insertion. A total of four studies met the inclusion criteria. This limited number reflects the current scarcity of primary research focused on the use of tapping and massage techniques for peripheral venous access.
The primary outcomes of interest were vein diameter (mm), vein cross-sectional area (mm²), and vein palpability (score). The vein diameter and cross-sectional area were measured using ultrasound in experimental designs, while the vein palpability were assessed through palpation scores in quasi-experimental or observational studies. For quantitative studies that reported statistical comparisons, we collected available data such as means, standard deviations, and, where applicable, p-values, odds ratios (OR), and 95% confidence intervals (CI) (Table 4). No studies reported clinical endpoints such as first-attempt success rate.
|
Study |
Intervention |
Outcome measure |
Tapping (mean ± SD) |
Massage (mean ± SD) |
Control (mean ±SD) |
p-value |
OR |
95% CI |
|
Ichimura et al., 2015 [30] |
Tapping, Control |
Vein diameter (mm) |
2.98± 0.45 |
- |
2.51±0.38 |
<0.01 |
1.75 |
1.15-2.35 |
|
Yasuda et al., 2019 [31] |
Tapping, Massage |
Vein palpability (score) |
4.5±0.6 |
3.8±0.7 |
3.2±0.5 |
<0.01 |
2.1 |
1.40-2.80 |
|
Ichimuda et al., 2020 [32] |
Tapping, Massage |
Cross-sectional area (mm²) |
6.45±1.32 |
5.87±1.20 |
5.32±1.15 |
<0.05 |
1.65 |
1.05-2.25 |
|
Yasuda et al., 2023 [33] |
Tapping, Massage |
Vein diameter (mm) |
3.12 ± 0.54 |
2.85±0.49 |
2.72±0.44 |
<0.01 |
1.85 |
1.20-2.50 |
SD: standard deviation
Table 4. Interventions, outcomes and available data of the selected studies
General Characteristics
The studies were conducted in laboratory settings, maintaining a controlled environment similar to clinical conditions (temperature 22-24 ̊C, humidity 45-65%) consistent with summer hospital standards. Participants were seated with their arms on a shape [30-32] or supine keeping their forearms on the bed during the intervention [33]. The populations studied were exclusively composed of healthy young adults aged approximately 20-29 years, without clinical comorbidities or indications of difficult venous access (DVA). It is important to note that the inclusion of young, healthy volunteers was a limitation dictated by the available literature, as no studies involving older adults, hospitalized patients, or individuals with comorbidities were found in the literature search. Therefore, the generalizability of the findings to broader patient populations remains limited. All studies compared tapping (a light, repetitive mechanical stimulation applied to the skin) and/or massage (manual pressure and friction techniques) with a control group where only a tourniquet was used. The primary outcomes measured were:
- Venous diameter (mm): assessed using ultrasound, representing the width of the vein (n=4; 100%)
- Cross-sectional area (mm²): a two-dimensional measure of the vein’s size, assessed using ultrasound (n=3; 75%)
- Vein palpability (score): a qualitative measure of how easily the vein could be felt during palpation (n=3; 75%)
No studies assessed the first-attempt success rate of peripheral intravenous catheter (PIVC) insertion or reported clinical outcomes related to successful cannulation. (Table 5).
|
Author(s) (year) |
Aim |
Study design |
Participants |
Evaluation methods |
Effect of tapping |
Effect of massage |
|
Ichimira et al., 2015 [30] |
To compare tapping and control groups for vein diameter |
Experimental study |
40 ha (20 yrs) |
Ultrasound |
Increased diameter |
Not assessed |
|
Yasuda et al.,2019 [31] |
To assess vein palpability under different stimulation techniques |
Quasi Experimental study |
30 ha (20-29 yrs) |
Palpation score |
Higher palpability |
Moderate palpability) |
|
Ichimura et al., 2020 [32] |
To evaluate cross-sectional area increase through tap |
Experimental study |
20 ha (19-22 yrs) |
Ultrasound |
Higher increase |
Moderate increase |
|
Yasuda et al., 2023 [33] |
To evaluate the effect of tap and mas on -vein diameter |
Quasi Experimental study |
40 ha (20-29 yrs) |
Ultrasound |
Greater increase in vein diameter |
Moderate increase in vein diameter |
Tap= tapping; Mas= massage; healthy adult= ha; yrs= years. Tapping showed higher numerical values compared to massage, but differences were not consistently statistically significant across all studies.
Table 5. Characteristics of studies included.
DISCUSSION
This systematic review aimed to evaluate the effects of tapping and massage techniques on venous dilation during peripheral intravenous catheter (PIVC) placement, compared to the standard use of a tourniquet alone. The findings suggest that both interventions may help improve vein visibility and diameter, offering a potential advantage in clinical practice, especially in settings where vascular access is challenging. Physiologically, gentle cutaneous stimulation is believed to enhance local blood flow through neurovascular mechanisms, including sympathetic reflexes and activation of mechanoreceptors [24,25]. While the included studies employed different approaches to measurement such as ultrasound imaging [30,32,33] and palpation [31,33], they all reported improvements in vein dilation following tapping or massage, supporting the hypothesis that these techniques promote local vasodilation. Although all included studies reported positive effects of tapping or massage on vein dilation, the magnitude and consistency of these effects varied. Two studies [30,32] measured outcomes using ultrasound, reporting significant increases in vein diameter and cross-sectional area following intervention. One study [31] assessed palpability scores through subjective evaluation, while another [33] used a combination of both methods. These methodological differences likely contributed to the variation in outcomes observed.
Importantly, the effectiveness of tapping and massage techniques may vary based on patient characteristics. All included studies were conducted on healthy young adults aged between 20 to 29 years. This homogeneous population limits the generalizability of findings to broader clinical contexts, such as elderly patients or those with chronic conditions (e.g., diabetes, obesity), who may present different venous characteristics or an increased risk of difficult venous access (DVA). None of the studies stratified results by specific comorbidities or clinical variables, making it difficult to assess the potential differential effects of the interventions in diverse patient populations. The modifiable factors analyzed in the included studies were related to the application of tapping or massage techniques before peripheral intravenous catheter (PIVC) insertion. [Table 4] Tapping showed a greater impact on vein diameter (OR range 1.75 – 2.10), vein cross-sectional area (OR range 1.65 – 1.85), and vein palpability (OR range 1.85 – 2.10) compared to control conditions. However, the differences between tapping and massage were not statistically significant, suggesting that both techniques may have comparable effects. The studies consistently demonstrated that both tapping and massage significantly increase venous dilation compared to control, likely due to the mechanical stimulation triggering the release of nitric oxide and other vasodilators. Massage was also associated with improved vein diameter and palpability, although the effects were generally less pronounced than tapping. No studies reported adverse events associated with either tapping or massage. Regarding non-modifiable factors, none of the studies explicitly analyzed demographic variables such as age or gender in relation to venous dilation outcomes. These findings suggest that both tapping and massage are simple, effective, and low-cost interventions for improving venous dilation prior to PIVC insertion, particularly in patients with difficult venous access. Most existing guidelines continue to focus primarily on tourniquet use and warming techniques, while both tapping and massage remain underutilized in clinical practice. This review highlights the need to consider incorporating tapping and massage into standard protocols, as these techniques have shown comparable efficacy in promoting venous dilation. Although none of the included studies specifically investigated patients with difficult venous access (DIVA), it is reasonable to hypothesize that such techniques could offer clinical benefits in this population, where failed attempts can lead to delays, discomfort, and increased resource utilization. However, further research is required to confirm their effectiveness in more complex clinical scenarios. Comparison with existing literature, also, highlights an underutilization of these techniques in clinical guidelines. Most vascular access protocols continue to emphasize traditional methods such as tourniquet application, fist clenching, or local warming [2,21,26], while manual techniques like tapping and massage are seldom formally recommended despite their frequent use in practice [20,22]. This disconnect may stem from the lack of high-quality studies evaluating these methods. However, tapping has shown a clear physiological rationale through its stimulation of nitric oxide release and vasodilatory reflexes [24,25,32], reinforcing its potential value in pre-cannulation practice. Importantly, none of the reviewed studies reported adverse effects associated with these interventions [30-33]. Despite their promise, the current evidence base is limited by several methodological shortcomings. This review has several limitations. First, all included studies were conducted on small, homogeneous samples of young, healthy adults, and were conducted in Japan which limits the external validity of the findings. None of the studies used randomization or blinding, increasing the risk of selection and performance bias. Sample sizes were generally small, and no power analyses were reported. Additionally, outcome assessment methods varied widely (e.g., ultrasound vs. subjective palpation), which hindered direct comparison across studies. The studies included standardized outcome measures (vein diameter, cross-sectional area, palpability), ensuring comparability of results. However, limitations include the small number of studies (n = 4), limited geographical representation, and the absence of data on pediatric, oncology, or chronic disease populations. These factors limit the ability to draw broad clinical recommendations. Finally, the overall methodological quality of the included studies was moderate, and the risk of bias was found to be moderate to serious, particularly in relation to confounding variables and outcome measurement. Despite these limitations, the results are promising. The consistency of findings suggests a potential benefit that warrants further investigation in patients with greater vascular access difficulty. Tapping and massage are simple, non-invasive, and cost-effective techniques that could be integrated into standard practice to facilitate vascular access, particularly in emergency departments, outpatient clinics, or in cases where veins are difficult to locate. These findings provide a preliminary but meaningful foundation for future clinical trials with more rigorous design, broader populations, and standardized outcome measures. Rather than representing a limitation of our review process, the small number of eligible studies highlights a significant gap in literature.
This review contributes to mapping and critically analyzing the available evidence on this underexplored topic.
Strengths
A key strength of this review is the focused synthesis of experimental [28, 30] o quasi experimental [29,31] evidence on a specific intervention (tapping and massage) for a well-defined outcome (venous dilation prior to PIVC). By focusing on a specific, yet clinically relevant topic, this review addresses a clear gap in the literature and offers practical insights for improving pre-cannulation practices. The methodology followed PRISMA 2020 guidelines, with a robust search strategy across multiple databases and a transparent risk of bias assessment using the ROBINS-I tool [29], ensuring a rigorous and reproducible approach. The inclusion of objective outcome measures such as vein diameter, cross-sectional area, and palpability adds further strength to the review. The review aims to spark interest in future research and contribute to the development of evidence-based guidelines for vascular access optimization. Furthermore, this review highlights the need for a paradigm shift in vascular access practices. While guidelines traditionally emphasize tourniquet application and warming techniques, simple, hands-on interventions like tapping and massage remain largely overlooked in clinical protocols. By shedding light on these low-cost, non-invasive strategies, this review advocates for their potential role in standard vascular access preparation, especially in resource-limited settings where advanced technologies may not be readily available.
CONCLUSIONS
This review suggests that tapping and massage techniques, when used in conjunction with a tourniquet, may improve peripheral vein dilation and palpability in healthy adults. Although the evidence is preliminary and limited by the methodological quality of the studies, the results point to simple, low-cost strategies that could support more effective intravenous access—particularly in clinical situations where veins are difficult to locate. From a practical perspective, these interventions may offer nurses a non-invasive tool to enhance vascular access success, potentially reducing patient discomfort and the need for repeated attempts. Future research should aim to confirm these effects through randomized controlled trials involving larger and more diverse populations. Standardized outcome measures and long-term follow-up will be essential to validate the efficacy and safety of these techniques in real-world clinical settings. Further high-quality primary research is urgently needed to strengthen the evidence base and support future systematic reviews with greater methodological robustness.
Registration
This work has been archived in Prospero with ID CRD420251066139.
Funding statement
This research did not receive any specific grant from funding agencies in public, commercial or not for profit sectors.
Conflict of interest
The authors report no conflict of interest.
Authors’ contributions
RC and MA were the major contributors in writing the manuscript. VM, and AL performed the data collection and interpreted the patient data. All authors read and approved the final manuscript.
REFERENCES
- Alexandrou E, Ray-Barruel G, Carr PJ, Frost SA, Inwood S, Higgins N, Lin F, Alberto L, Mermel ùL, Rickard CM; OMG Study Group. Use of Short Peripheral Intravenous Catheters: Characteristics, Management, and Outcomes Worldwide. J Hosp Med. 2018 May 30;13(5). doi: 10.12788/jhm.3039. PMID: 29813140.
- Zingg W, Barton A, Bitmead J, Eggimann P, Pujol M, Simon A, Tatzel J. Best practice in the use of peripheral venous catheters: A scoping review and expert consensus. Infect Prev Pract. 2023 Feb 3;5(2):100271. doi: 10.1016/j.infpip.2023.100271. PMID: 36910422; PMCID: PMC9995289.
- Moureau NL, Alexandrou E. Vessel Health and Preservation: The Right Approach for Vascular Access. Springer International Publishing. doi:10.1007/978-3-030-03149-7_3
- Pittiruti M, Van Boxtel T, Scoppettuolo G, Carr P, Konstantinou E, Ortiz Miluy G, Lamperti M, Goossens GA, Simcock L, Dupont C, Inwood S, Bertoglio S, Nicholson J, Pinelli F, Pepe G. European recommendations on the proper indication and use of peripheral venous access devices (the ERPIUP consensus): A WoCoVA project. J Vasc Access. 2023 Jan;24(1):165-182. doi: 10.1177/11297298211023274. Epub 2021 Jun 4. PMID: 34088239.
- Carr PJ, Rippey JCR, Cooke ML, Trevenen ML, Higgins NS, Foale AS, Rickard CM. Factors associated with peripheral intravenous cannulation first-time insertion success in the emergency department. A multicentre prospective cohort analysis of patient, clinician and product characteristics. BMJ Open. 2019 Apr 2;9(4):e022278. doi: 10.1136/bmjopen-2018-022278. PMID: 30944127; PMCID: PMC6500093.
- Keogh S, Shelverton C, Flynn J, Mihala G, Mathew S, Davies KM, Marsh N, Rickard CM. Implementation and evaluation of short peripheral intravenous catheter flushing guidelines: a stepped wedge cluster randomised trial. BMC Med. 2020 Sep 30;18(1):252. doi: 10.1186/s12916-020-01728-1. PMID: 32993628; PMCID: PMC7526260.
- Gala S, Alsbrooks K, Bahl A, Wimmer M. The economic burden of difficult intravenous access in the emergency department from a United States' provider perspective. J Res Nurs. 2024 Feb;29(1):6-18. doi: 10.1177/17449871231213025. Epub 2024 Jan 16. PMID: 38495321; PMCID: PMC10939017.
- Blanco P. Ultrasound-guided peripheral venous cannulation in critically ill patients: a practical guideline. Ultrasound J. 2019 Oct 17;11(1):27. doi: 10.1186/s13089-019-0144-5. PMID: 31624927; PMCID: PMC6797689.
- Hadaway L.C., Millam D.A. On the road to successful I.V. starts. Nursing. 2005;35:1–14. doi: 10.1097/00152193-200505001-00001. PMID: 15855836.
- Ingram P, Lavery I. Peripheral intravenous cannulation: safe insertion and removal technique. Nurs Stand. 2007; 22(1):44-47. PMID: 17941430. doi: 10.7748/ns2007.09.22.1.44.c4613
- Gagne P, Sharma K. Relationship of Common Vascular Anatomy to Cannulated Catheters. Int J Vasc Med. 2017;2017:5157914. doi: 10.1155/2017/5157914. PMID: 29410917; PMCID: PMC5749287.
- Lapostolle F, Catineau J, Garrigue B, Monmarteau V, Houssaye T, Vecci I, Tréoux V, Hospital B, Crocheton N, Adnet F. Prospective evaluation of peripheral venous access difficulty in emergency care. Intensive Care Med. 2007 Aug;33(8):1452-7. doi: 10.1007/s00134-007-0634-y. PMID: 17554524.
- Nickel B, Gorski L, Kleidon T, Kyes A, DeVries M, Keogh S, Meyer B, Sarver MJ, Crickman R, Ong J, Clare S, Hagle ME. Infusion Therapy Standards of Practice, 9th Edition. J Infus Nurs. 2024 Jan-Feb 01;47(1S Suppl 1):S1-S285. doi: 10.1097/NAN.0000000000000532. PMID: 38211609.
- Dougherty L. Peripheral cannulation. Nurs Stand. 2008 Sep 3-9;22(52):49-56; quiz 58. doi: 10.7748/ns2009.04.23.33.59.c7187. PMID: 18792744.
- Sabri A, Szalas J, Holmes KS, Labib L, Mussivand T. Failed attempts and improvement strategies in peripheral intravenous catheterization. Biomed Mater Eng. 2013;23(1-2):93-108. doi: 10.3233/BME-120735. PMID: 23442240.
- Carr PJ, Rippey JCR, Cooke ML, Trevenen ML, Higgins NS, Foale AS, Rickard CM. Factors associated with peripheral intravenous cannulation first-time insertion success in the emergency department. A multicentre prospective cohort analysis of patient, clinician and product characteristics. BMJ Open. 2019 Apr 2;9(4):e022278. doi: 10.1136/bmjopen-2018-022278. PMID: 30944127; PMCID: PMC6500093.
- Masamoto T, Yano R. Characteristics of expert nurses' assessment of insertion sites for peripheral venous catheters in elderly adults with hard-to-find veins. Jpn J Nurs Sci. 2021 Jan;18(1):e12379. doi: 10.1111/jjns.12379. PMID: 33025696.
- Marsh N, Larsen EN, Takashima M, Kleidon T, Keogh S, Ullman AJ, Mihala G, Chopra V, Rickard CM. Peripheral intravenous catheter failure: A secondary analysis of risks from 11,830 catheters. Int J Nurs Stud. 2021 Dec;124:104095. doi: 10.1016/j.ijnurstu.2021.104095. PMID: 34689013.
- Potter, P.; Perry, A.; Stockert, P.; Hall, A. Fundamentals of Nursing: Concepts, Process, and Practice, 9th ed.; Elsevier Mosby: St. Louis, MI, USA, 2017.
- Santos-Costa P, Paiva-Santos F, Sousa LB, Bernardes RA, Ventura F, Salgueiro-Oliveira A, Parreira P, Vieira M, Graveto J. Evidence-Informed Development of a Bundle for Peripheral Intravenous Catheterization in Portugal: A Delphi Consensus Study. Nurs Rep. 2022 Jul 7;12(3):498-509. doi: 10.3390/nursrep12030047. PMID: 35894037; PMCID: PMC9326523.
- Lenhardt R, Seybold T, Kimberger O, Stoiser B, Sessler DI. Local warming and insertion of peripheral venous cannulas: single blinded prospective randomised controlled trial and single blinded randomised crossover trial. BMJ. 2002 Aug 24;325(7361):409-10. doi: 10.1136/bmj.325.7361.409. PMID: 12193353; PMCID: PMC119431.
- Biyik Bayram S, Caliskan N. Effects of local heat application before intravenous catheter insertion in chemotherapy patients. J Clin Nurs. 2016 Jun;25(11-12):1740-7. doi: 10.1111/jocn.13193. PMID: 27028834.
- Sasaki S, Murakami N, Matsumura Y, Ichimura M, Mori M. Relationship between tourniquet pressure and a cross-section area of superficial vein of forearm. Acta Med Okayama. 2012;66(1):67-71. doi: 10.18926/AMO/48083. PMID: 22358141.
- Simón-López LC, Luquero-Bueno S, Ovejero-Benito MC, Cuesta-Lozano D, Goodman-Casanova JM, Vargas-Castrillón E, Mazarro DO, De Miguel-Cáceres A, Posada-Moreno P, Zaragoza-García I, Ortuño-Soriano I. Benefits of the application of heat and pressure on peripheral venous cannulation in adults: A randomized controlled trial. J Adv Nurs. 2021 Mar;77(3):1533-1545. doi: 10.1111/jan.14655. PMID: 33219590.
- van Loon FHJ, van Hooff LWE, de Boer HD, Koopman SSHA, Buise MP, Korsten HHM, Dierick-van Daele ATM, Bouwman ARA. The Modified A-DIVA Scale as a Predictive Tool for Prospective Identification of Adult Patients at Risk of a Difficult Intravenous Access: A Multicenter Validation Study. J Clin Med. 2019 Jan 26;8(2):144. doi: 10.3390/jcm8020144. PMID: 30691137; PMCID: PMC6406455.
- Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R, Glanville J, Grimshaw JM, Hróbjartsson A, Lalu MM, Li T, Loder EW, Mayo-Wilson E, McDonald S, McGuinness LA, Stewart LA, Thomas J, Tricco AC, Welch VA, Whiting P, Moher D. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Syst Rev. 2021 Mar 29;10(1):89. doi: 10.1186/s13643-021-01626-4. PMID: 33781348; PMCID: PMC8008539.
- Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan-a web and mobile app for systematic reviews. Syst Rev. 2016 Dec 5;5(1):210. doi: 10.1186/s13643-016-0384-4.
- National Institutes of Health (2014). Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies. Available online at: https://www.nhlbi.nih.gov/health-pro/guidelines/in-develop/cardiovascular-risk-reduction/tools/cohort (last access 24/05/2025)
- J.A. Sterne, M.A. Hernán, B.C. Reeves, et al. ROBINS-I: A tool for assessing risk of bias in non-randomised studies of interventions BMJ 2016;355:i4919. doi: 10.1136/bmj.i4919.
- Ichimura M, Sasaki S, Mori M, Ogino T. Tapping but not massage enhances vasodilation and improves venous palpation of cutaneous veins. Acta Med Okayama. 2015;69(2):79-85. doi: 10.18926/AMO/53336. PMID: 25899629.
- Yasuda K, Sato S, Okada K, Yano R. The venodilation effects of tapping versus massaging for venipuncture. Jpn J Nurs Sci. 2019 Oct;16(4):491-499. doi: 10.1111/jjns.12261. PMID: 31222981.
- Ichimura M, Sasaki S, Ogino T. Tapping enhances vasodilation for venipuncture even in individuals with veins that are relatively difficult to palpate. Clin Anat. 2020 Apr;33(3):440-445. doi: 10.1002/ca.23559. PMID: 31908028.
- Yasuda K, Okada K, Sugimura N, Yano R. Do Tapping and Massaging during Tourniquet Application Promote Dilation of Forearm Cutaneous Veins? A Pilot Quasi-Experimental Study. Healthcare (Basel). 2023 Feb 10;11(4):522. doi: 10.3390/healthcare11040522. PMID: 36833056; PMCID: PMC9956355.
![]() This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Presenting Cues to Promote Clinical Reasoning in Physical Assessment for Undergraduate Nursing Students: A Randomized Controlled Study
Akifumi Maeda 1*, Akemi Hirao 1, Akiko Sugimoto 1, Motoko Hori 2
- Department of Critical Care and Emergency Nursing, Faculty of Nursing, Senri Kinran University, Osaka, Japan
- Department of Chronic Care Nursing, Faculty of Nursing, Senri Kinran University, Suita, Osaka, Japan
* Corresponding author: Akifumi Maeda, Department of Critical Care and Emergency Nursing, Faculty of Nursing, Senri Kinran University, 5-25-1 Fujishirodai, Suita, Osaka, Japan. ORCID: http://orcid.org/0000-0002-2628-2224. E-mail: ak-maeda@cs.kinran.ac.jp
Cite this article
ABSTRACT
Introduction: Physical assessment is a fundamental clinical skill in nursing practice and crucial to developing effective nursing care plans. Thus, acquiring knowledge and skills in physical assessment is an essential competence for undergraduate nursing students.
Objective: This study aimed to investigate the effect of utilizing pre-assignment work and presenting specific cues about a case on the clinical reasoning skills of undergraduate nursing students by comparing an intervention group that received specific cues with a control group that did not.
Materials: This randomized controlled trial involved second-year undergraduate nursing students. Participants were randomly assigned to an intervention or control group. Both groups completed a pre-assignment related to heart failure and participated in a 60-minute group case study session. The intervention group received specific cues related to the case during the session, guiding their assessment and care planning. Clinical reasoning skills were evaluated subjectively using the Clinical Reasoning Skills Self-Assessment Scale (CRSS) and objectively by analyzing the students’ responses to the group task.
Results: A total of 94 participants were randomly assigned to either the intervention group (n= 47) or the control group (n= 47). While the pre-session CRSS scores were similar between groups, the post-session scores on several items related to information gathering, interpretation, problem identification, and goal setting were significantly higher in the intervention group. Qualitative analysis of narrative responses revealed that the intervention group provided more specific and patient-centered nursing care plans based on the patient's symptoms, whereas the control group offered more generalized interventions.
Conclusion: The use of pre-assignment and specific cues enhanced students’ ability to interpret patient information and formulate individualized nursing care plans. This approach effectively improved clinical reasoning skills in physical assessment and may serve as a practical alternative in educational settings lacking simulation-based resources.
Keywords: Clinical Reasoning, Physical Assessment, Undergraduate Nursing Student, Cues.
INTRODUCTION
Physical assessment refers to the process of collecting and evaluating information about a patient's physical condition through interviews and physical examination techniques, including inspection, palpation, percussion, and auscultation [1]. It is a core clinical competency in nursing practice [2] and is essential for developing effective nursing care plans [3]. Because accurately collecting both subjective and objective patient data enables nurses to appropriately assess a patient's condition [4], acquiring physical assessment skills is critically important for undergraduate nursing students [5].
In recent years, simulation-based education has attracted attention as an effective method for undergraduate nursing students to acquire physical assessment skills and become clinically competent upon graduation [6,7]. However, implementing simulation-based education requires considerable time and effort, as well as dedicated facilities, expensive manikins, and trained instructors, thereby imposing significant material and human resource burdens [8]. Moreover, the number of students who can participate in a simulation session simultaneously is limited [6], and institutions with large class sizes face challenges in widely implementing this approach. Therefore, there is a need to explore alternative and efficient methods for teaching physical assessment.
The information obtained through physical examination provides specific cues that serve as the starting point for clinical reasoning [9]. Rather than separating physical assessment from clinical reasoning, integrating these two areas in the learning process is expected to enhance students’ practical judgment skills. Clinical reasoning in nursing is defined as the process through which nurses collect and interpret information based on cues, understand patients’ conditions and problems, plan and implement nursing interventions, and evaluate and reflect on outcomes [9]. Physical assessment and clinical reasoning share many commonalities: both involve collecting and interpreting information about a patient’s condition and making decisions regarding nursing care, which require observation, interpretation, and judgment skills [1,9]. By learning these processes in an integrated manner, students can move beyond mere observation of physical findings to logical analysis of the information, identification of patient problems, and development of appropriate nursing care plans.
A "cue" refers to an identifiable physiological or psychosocial change experienced by a patient and includes patient information and recalled knowledge obtained through history-taking and assessment [10]. Tanner positioned these cues, referred to as “noticing,” as the foundation of clinical reasoning [11]. New graduate nurses often collect excessive amounts of information due to underdeveloped skills in distinguishing relevant from irrelevant data when attempting to accurately assess patient conditions and situations [12]. This tendency is also seen in undergraduate nursing students, who frequently struggle to identify key information among a large volume of data, leading to unfocused assessments and disruption of the clinical reasoning process. Although simulation-based education has been explored to improve students’ clinical reasoning, there is limited evidence regarding alternative, low-cost instructional methods that integrate cue recognition with physical assessment in case-based learning [13]. In particular, few studies have rigorously examined whether providing targeted cues during group discussions can enhance the clinical reasoning process in undergraduate nursing education [14].
As one approach to addressing this issue, the present study aimed to examine the effect of using pre-assignment work to help undergraduate nursing students obtain cues during a case-based physical assessment on their clinical reasoning ability.
Objective
This study aimed to examine the effects of using pre-assignment work and presenting specific cues in a case on the clinical reasoning skills of second-year undergraduate nursing students during physical assessment by comparing an intervention group that received specific cues with a control group that did not.
MATERIALS AND METHODS
Study Design
This study employed a parallel-group, two-arm, randomized controlled trial (RCT) design conducted to evaluate the effectiveness of a cue-based educational intervention on clinical reasoning skills in physical assessment. The study was implemented as part of an existing physical assessment course at a private women's university in western Japan.
The design and reporting followed the CONSORT 2025 guidelines for randomized trials [15] in educational research. Intervention and control groups received structured group learning sessions, with only the intervention group being exposed to specific case-related cues. Outcome assessments included both subjective (self-assessment scale) and objective (task-based) measures.
Conceptual Framework
Figure1 presents a conceptual diagram illustrating the process of clinical reasoning and the intervention applied during physical assessment. In this study, the process of clinical reasoning was defined as "the sequence from information collection regarding a case to the planning of interventions (nursing care)."
Participants in the intervention group progressed through the assignments by selecting and recording the information they deemed necessary, based on the "cues" presented by the researcher and the content of their pre-assignment work. This study aimed to examine how the provision of "cues" influenced the subsequent quality of information interpretation, patient understanding, and intervention planning.
The evaluation was structured to verify the effect of the intervention through both subjective and objective assessments, including scores from the Clinical Reasoning Skills Self-Assessment Scale (CRSS), and the content of students' interviews, physical examinations, and nursing care descriptions related to the case.
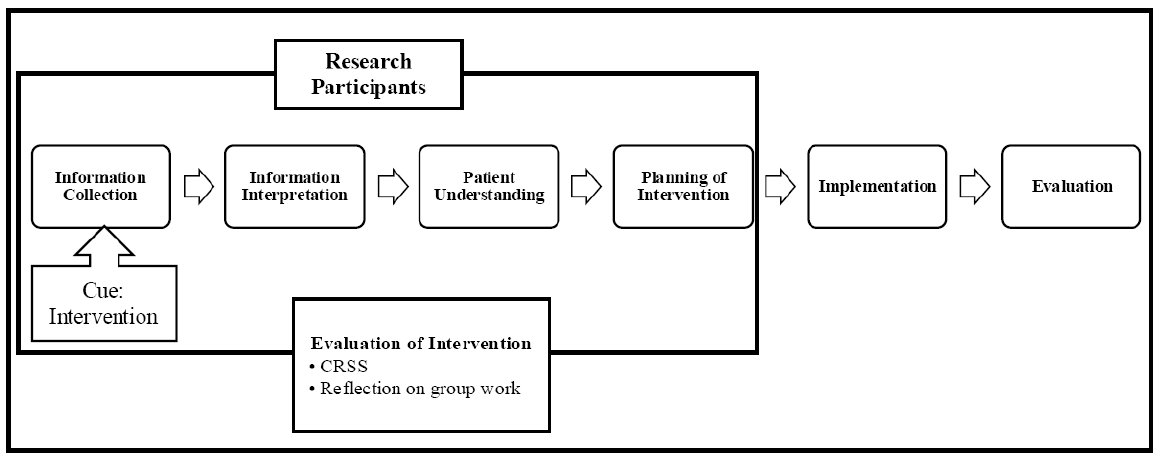
This diagram outlines the clinical reasoning process from information collection to evaluation.
The intervention group received cues to support reasoning during physical assessment, and outcomes were evaluated using CRSS and reflection.
CRSS = Clinical Reasoning Skills Self-Assessment Scale.
Figure 1. Conceptual Framework
Operational Definition
Cue: A cue refers to an identifiable physiological or psychosocial change experienced by a patient and includes patient information, and the recall of related knowledge obtained through history-taking and assessment [10]. In this study, a cue is operationally defined as the judgment material obtained by students through the use of pre-work and thinking based on mechanisms and rationales, enabling them to appropriately assess the condition of the case.
Sample Size
The sample size was calculated to compare the CRSS scores between the intervention and control groups at the end of the study. Based on an alpha level (α) of 0.05, a power (1-β) of 0.80, and a medium effect size of 0.7 (Cohen’s d), a minimum of 35 participants per group was required. Therefore, the minimum total sample size needed was 70 participants. The effect size was estimated based on results from previous similar educational intervention studies in nursing. Particularly, the total sample was expanded to 94 patients to reduce the possible bias due to missing information or data loss. In this way, 47 patients were assigned to each group. The sample size calculation was conducted using G*Power [16].
Study Population
The study was conducted at a private women’s university located in western Japan. The participants were second-year undergraduate students enrolled in the university’s Department of Nursing. All students were female by institutional policy.
Recruitment and Consent Procedure
Seven days prior to the study session, the researchers distributed an informed consent form and provided both verbal and written explanations of the study's objectives and procedures. Students were instructed to submit the completed consent form into a designated collection box at the university by the day before the session. Submission of the form was considered as consent to participate in the study.
Exclusion Criteria
Students were excluded if they (1) were absent, arrived late, or left early on the day of the session; (2) failed to complete the required pre-assignment; or (3) submitted incomplete responses on the CRSS.
Group Allocation
The randomization sequence was generated by the researcher using a computer-generated random number table with a 1:1 allocation ratio. To ensure allocation concealment, group assignments were placed in opaque, sealed envelopes and numbered sequentially. After each participant submitted their informed consent form, a separate coordinator-who was not involved in enrollment, intervention delivery, or outcome assessment-opened the envelope corresponding to the participant. This procedure ensured that neither the personnel responsible for enrollment nor the participants had prior knowledge of group assignments. Participants were blinded to their assigned group throughout the study period. However, due to the nature of the intervention, researchers were not blinded.
This study was not registered in a clinical trial registry, as it involved an educational intervention implemented within an existing university course and did not fall under ICMJE [17] or CONSORT [15] requirements for mandatory trial registration. No changes were made to the original study protocol during the course of the study.
Pre-assignment
To prepare students for the group case study session, a pre-assignment related to heart failure was distributed 14 days in advance. The assignment consisted of six questions focusing on the pathophysiology, assessment, and nursing care of a patient suspected of heart failure (see Appendix Table A1). Students were instructed to complete the assignment individually at home and bring it with them on the day of the session. This pre-assignment was designed to encourage students to review fundamental knowledge about heart failure and to consider appropriate examination methods and nursing interventions. Given the increasing global prevalence of heart failure, particularly in aging populations [18-20], emphasis was placed on recognizing symptoms and planning care based on clinical reasoning.
Study Procedures
The study was conducted on July 11, 2024, during scheduled lectures on physical assessment. Prior to participation, all students had completed 540 minutes of practical training in interview techniques and physical assessments of the respiratory, cardiovascular, gastrointestinal, musculoskeletal, and neurological systems.
Intervention
The intervention and control groups conducted the group case study sessions at separate times and in different classrooms to avoid contamination. Each session was facilitated by four researchers, all of whom were experienced nursing educators with training in physical assessment and case-based learning. To ensure consistency across sessions, all researchers referred to a common set of verbal cues prepared in advance (see Appendix Table A2), which guided the timing and content of each task. Additionally, a pre-session briefing was conducted among all researchers to align their understanding of the procedures, clarify roles, and ensure a uniform approach to facilitation. Both groups received a pre-assignment related to heart failure and completed it individually before the session. Based on previous findings suggesting that collaborative learning enhances clinical reasoning skills among nursing students [21], students worked in teams of 5-6 during the 60-minute sessions and completed six tasks sequentially using written case materials (see Appendix Table A3). Each group’s responses were recorded on standardized answer sheets. In the intervention group, specific cues were presented by the researcher prior to each task to support students’ clinical reasoning. These cues guided students to apply their pre-assignment knowledge and consider pathophysiological mechanisms. For example, prior to the Inspection task, students were asked: “Think about the visible changes or symptoms caused by heart failure.” A complete list of the cues provided is shown in Appendix Table A2.
Outcome Measures
The outcomes were evaluated using both subjective and objective measures.
CRSS Scores
Subjective evaluation of clinical reasoning skills was conducted using the Japanese version of the CRSS [22]. The original CRSS is a 26-item, five-point Likert scale developed to assess clinical reasoning processes in nursing [23]. The Japanese version has demonstrated high reliability (Cronbach’s alpha = 0.95) and acceptable content validity (CVI = 0.78) among nurses and undergraduate nursing students [22]. In the present study, 12 items specifically related to behaviors in direct clinical practice-such as implementing patient care, selecting appropriate interventions, and evaluating care outcomes-were excluded based on the consensus of the research team, as the intervention did not involve actual patient care or clinical settings. Consequently, 14 items that assessed cognitive and judgmental aspects of reasoning, including data gathering, interpretation, and planning, were retained for analysis. Although the original CRSS is multidimensional in design, the retained items in this study primarily reflect the cognitive components of clinical reasoning. The original Japanese version demonstrated acceptable content validity (CVI= 0.78); however, the modified 14-item version used in this study has not undergone a separate content validity evaluation. A total score was calculated by summing the responses to the 14 selected items (score range: 14-70), with higher scores indicating greater perceived clinical reasoning ability. The internal consistency of the modified scale was confirmed in this study, yielding a Cronbach’s alpha of 0.94. The use of the Japanese version of the CRSS was approved by the original developers.
Task Responses
Objective evaluation was conducted based on the written responses of each group to the six case-based tasks. Two evaluators-members of the research team with expertise in nursing education-assessed the specificity and appropriateness of the proposed nursing care using a predefined rubric developed for this study. The rubric included criteria such as: Alignment with the patient’s symptoms and condition, Clarity and feasibility of the proposed care, and Use of patient-specific data rather than generalized interventions. Prior to analysis, the evaluators reviewed several sample responses and calibrated their judgments through discussion to ensure consistency. Although the evaluators were members of the research team, the group allocation of each response was blinded during the assessment process to minimize potential bias.
Statistical Analysis
The CRSS scores for the intervention and control groups were confirmed to be non-normally distributed using the Shapiro-Wilk test. Therefore, the 15-item scores were summarized using the median and interquartile range. The Mann-Whitney U test was used to compare the CRSS scores between the intervention and control groups, and the Wilcoxon signed-rank test was used to compare pre-and post-session scores within each group. For the Mann-Whitney U test, mean rank values were reported in addition to p-values, particularly for items where the medians were equal between groups. For the Wilcoxon signed-rank test, we reported both the test statistic (W) and standardized Z values alongside p-values to enhance the clarity and rigor of the within-group comparisons. A two-tailed p-value less than the 5% significance level was considered statistically significant. All statistical analyses were performed using SPSS, Version 26.0 (IBM Corp, Armonk, NY, USA). Although students worked in small groups of 5-6 during the sessions, the statistical analysis did not account for potential cluster effects. This was because the CRSS was completed independently by each participant, and all instructional materials and procedures were standardized across groups to minimize variability related to group dynamics. Missing data were handled by complete case analysis; participants with incomplete CRSS responses were excluded from the final analysis.
Narrative Responses
Statistical analysis was not performed on the narrative responses. Instead, the responses were analyzed qualitatively using a basic content comparison approach. Two researchers independently reviewed the written narratives from each group and compared the content in terms of specificity and appropriateness of the proposed nursing care interventions. Discrepancies in interpretation were discussed and resolved through consensus to enhance the credibility of the analysis. While a formal thematic analysis was not conducted, this comparative review provided insights into differences in the depth and relevance of reasoning between groups. The lack of a formal qualitative methodology is acknowledged as a limitation of this study and is addressed in the limitations section.
Ethical Considerations
This study was approved by the Senri Kinran University Institutional Review Board (IRB; Approval Number: K24-007 dated May 27, 2024). Participants were informed that their participation and cooperation in the study were entirely voluntary and that non-participation would not result in any disadvantage. They were also informed, both in writing and verbally, that the study would be conducted during the lecture of the Physical Assessment course, and that their participation or non-participation would have no impact on their course grades. In addition, participants were advised that if they felt that their participation influenced their grades or if they perceived any misconduct or harassment related to the study, they could consult with the Harassment Advisory Committee established within the university.
For students who chose not to participate in the study, it was explained that while they would attend the lecture together with other students, they were not required to complete the CRSS and their data would not be included in the study analysis. Due to group assignment logistics, some students who declined to participate were included in the same groups as control group participants. These students were also given the supplementary exercise conducted for the intervention group after the completion of the study to ensure that no disadvantage would arise from their non-participation. Similarly, to prevent any disadvantage, participants assigned to the control group were provided with the same instructional content used for the intervention group after the study was completed.
RESULTS
Participant Flow
A total of 107 second-year undergraduate nursing students were eligible to participate. Of these, 94 students (87.8%) consented to take part in the study. Among those who consented, 93 were 20 years old and one was 22 years old. Participants were randomly assigned to either the intervention group (n = 47) or the control group (n = 47). However, one student in the control group was excluded due to late arrival, resulting in 93 students (86.9%) who completed the intervention as planned-47 in the intervention group and 46 in the control group. Each group was further subdivided into teams of five to six students, resulting in nine subgroups per condition. Due to missing responses on the post-session CRSS, three participants in the intervention group and four in the control group were excluded from the final analysis. Therefore, CRSS data from 44 participants in the intervention group and 42 in the control group were included in the analysis. The flow of participant enrollment, exclusion, allocation, and final inclusion for analysis is illustrated in Figure 2.
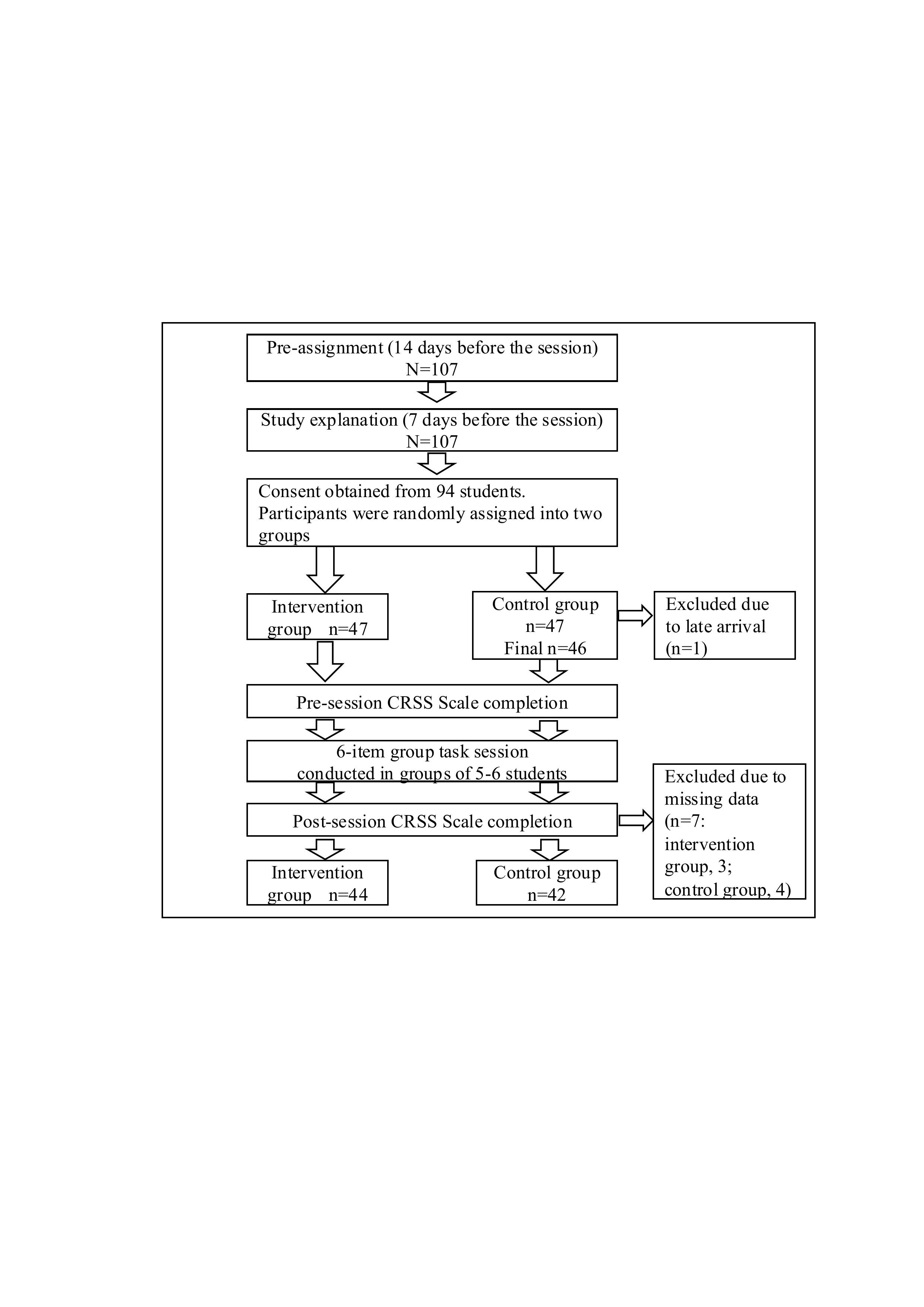
107 students were recruited; 94 consented and were assigned to two groups. After exclusions, CRSS data from 86 participants were analyzed (intervention: 44, control: 42).
CRSS = Clinical Reasoning Skills Self-Assessment Scale.
Figure 2. Study Flow and the Number of Study Participants.
Comparison of the CRSS Scores
The pre-session scores of the CRSS Scale showed no significant differences between the intervention and control groups on all 15 items. However, the post-session scores of the intervention group were significantly higher than those of the control group on ten items (Table 1, 2)
|
No. |
Question items |
Intervention group (n = 44) |
Control group (n = 42) |
Mean Rank (Intervention) |
Mean Rank (Control) |
P value |
|
1 |
I can apply the interview and physical examination to assess the patient’s condition. |
3.00 (2.25-4.00) |
3.00 (3.00-4.00) |
43.60 |
43.39 |
0.96 |
|
2 |
I can interpret the information collected. |
4.00 (3.00-4.00) |
3.50 (3.00-4.00) |
44.51 |
42.44 |
0.67 |
|
3 |
I can recognize the need for more information. |
3.00 (3.00-4.00) |
3.00 (2.75-4.00) |
46.86 |
39.98 |
0.16 |
|
4 |
I can distinguish between necessary and unnecessary information. |
3.00 (3.00-4.00) |
3.00 (2.00-4.00) |
44.50 |
42.45 |
0.68 |
|
5 |
I can anticipate how my decisions will affect the patient's condition. |
4.00 (3.00-4.00) |
3.00 (2.00-4.00) |
47.65 |
39.15 |
0.09 |
|
6 |
I can assess the cause and effect relationships in the patient’s condition. |
3.00 (2.25-4.00) |
3.00 (3.00-3.00) |
45.64 |
41.26 |
0.38 |
|
7 |
I can recognize the need for patient care. |
4.00 (4.00-4.00) |
4.00 (3.75-4.00) |
43.98 |
43.00 |
0.82 |
|
8 |
I can identify nursing problems. |
3.00 (3.00-4.00) |
3.00 (3.00-4.00) |
42.78 |
44.25 |
0.76 |
|
9 |
I can notice changes in the patient's condition. |
4.00 (4.00-4.00) |
4.00 (3.00-4.00) |
46.74 |
40.11 |
0.14 |
|
10 |
I can prioritize the patient’s needs. |
3.00 (3.00-4.00) |
3.00 (3.00-4.00) |
40.93 |
46.19 |
0.28 |
|
11 |
I can establish nursing plans. |
3.00 (2.00-4.00) |
3.00 (3.00-3.00) |
42.95 |
44.05 |
0.83 |
|
12 |
I can plan the necessary care. |
3.50 (3.00-4.00) |
3.00 (3.00-4.00) |
44.55 |
42.40 |
0.67 |
|
13 |
I can determine patient care. |
3.00 (2.25-4.00) |
3.00 (3.00-4.00) |
44.17 |
42.80 |
0.78 |
|
14 |
I can determine patient care quickly. |
3.00 (2.00-4.00) |
3.00 (2.00-3.00) |
45.16 |
41.76 |
0.50 |
|
15 |
Total |
49.00 (40.00-51.00) |
46.00 (41.0-50.25) |
45.50 |
41.40 |
0.44 |
Note 1: The scores for the question items and the total score are presented as medians (interquartile range).
Note 2: The data were analyzed using the Mann-Whitney U test.
Table 1. Comparison of the Pre-session Scores of the CRSS Between the Intervention and Control Groups.
|
No. |
Question items |
Intervention group (n = 44) |
Control group (n = 42) |
Mean Rank (Intervention) |
Mean Rank (Control) |
P value |
|
1 |
I can apply the interview and physical examination to assess the patient’s condition. |
4.00 (4.00-5.00) |
4.00 (4.00-4.00) |
48.17 |
38.61 |
0.039* |
|
2 |
I can interpret the information collected. |
4.00 (4.00-5.00) |
4.00 (4.00-4.00) |
49.07 |
37.67 |
0.014* |
|
3 |
I can recognize the need for more information. |
4.00 (4.00-5.00) |
4.00 (3.00-4.00) |
50.90 |
35.75 |
0.002* |
|
4 |
I can distinguish between necessary and unnecessary information. |
4.00 (4.00-4.00) |
4.00 (3.00-4.00) |
49.20 |
37.52 |
0.015* |
|
5 |
I can anticipate how my decisions will affect the patient's condition. |
4.00 (4.00-5.00) |
4.00 (3.00-4.00) |
49.09 |
37.64 |
0.019* |
|
6 |
I can assess the cause and effect relationships in the patient’s condition. |
4.00 (4.00-5.00) |
4.00 (3.00-4.00) |
49.32 |
37.40 |
0.016* |
|
7 |
I can recognize the need for patient care. |
4.00 (4.00-5.00) |
4.00 (4.00-5.00) |
47.72 |
39.08 |
0.076 |
|
8 |
I can identify nursing problems. |
4.00 (3.00-5.00) |
4.00 (3.00-4.00) |
47.51 |
39.30 |
0.103 |
|
9 |
I can notice changes in the patient's condition. |
4.00 (4.00-5.00) |
4.00 (3.00-4.00) |
50.27 |
36.40 |
0.005* |
|
10 |
I can prioritize the patient’s needs. |
4.00 (4.00-5.00) |
3.00 (3.00-4.00) |
47.36 |
39.45 |
0.111 |
|
11 |
I can establish nursing plans. |
4.00 (4.00-4.75) |
4.00 (3.00-4.00) |
48.42 |
38.35 |
0.040* |
|
12 |
I can plan the necessary care. |
4.00 (4.00-5.00) |
4.00 (3.00-4.00) |
48.07 |
38.71 |
0.062 |
|
13 |
I can determine patient care. |
4.00 (3.00-4.00) |
4.00 (3.00-4.00) |
47.75 |
39.05 |
0.076 |
|
14 |
I can determine patient care quickly. |
4.00 (4.00-4.00) |
3.00 (3.00-4.00) |
48.72 |
38.04 |
0.03* |
|
15 |
Total |
60.00 (53.50.-63.00) |
52.00 (48.00-59.00) |
51.84 |
34.76 |
0.002* |
Note 1: The scores for the question items and the total score are presented as medians (interquartile range).
Note 2: The data were analyzed using the Mann-Whitney U test. Significant differences are indicated by P < 0.05*.
Table 2. Comparison of the Post-session Scores of the CRSS Between the Intervention and Control Groups.
In the between-group comparisons, no significant differences were found between the intervention and control groups in any of the 15 items before the session (Table 3).
However, after the session, the intervention group scored significantly higher than the control group on 10 out of the 15 items (Table 4).
|
No. |
Question items |
Pre-session |
Post-session |
Test Statistic (W) |
Z value |
P value |
|
1 |
I can apply the interview and physical examination to assess the patient’s condition. |
3.00 (2.25-4.00) |
4.00 (4.00-5.00) |
498.00 |
-4.50 |
< 0.001* |
|
2 |
I can interpret the information collected. |
4.00 (3.00-4.00) |
4.00 (4.00-5.00) |
221.00 |
-3.15 |
0.002* |
|
3 |
I can recognize the need for more information. |
3.00 (3.00-4.00) |
4.00 (4.00-5.00) |
549.00 |
-5.01 |
< 0.001* |
|
4 |
I can distinguish between necessary and unnecessary information. |
3.00 (3.00-4.00) |
4.00 (4.00-4.00) |
423.00 |
-4.73 |
< 0.001* |
|
5 |
I can anticipate how my decisions will affect the patient's condition. |
4.00 (3.00-4.00) |
4.00 (4.00-5.00) |
232.50 |
-2.96 |
0.003* |
|
6 |
I can assess the cause and effect relationships in the patient’s condition. |
3.00 (2.25-4.00) |
4.00 (4.00-5.00) |
506.00 |
-4.70 |
< 0.001* |
|
7 |
I can recognize the need for patient care. |
4.00 (4.00-4.00) |
4.00 (4.00-5.00) |
293.50 |
-3.76 |
< 0.001* |
|
8 |
I can identify nursing problems. |
3.00 (3.00-4.00) |
4.00 (3.00-5.00) |
425.00 |
-4.22 |
< 0.001* |
|
9 |
I can notice changes in the patient's condition. |
4.00 (4.00-4.00) |
4.00 (4.00-5.00) |
277.00 |
-4.00 |
< 0.001* |
|
10 |
I can prioritize the patient’s needs. |
3.00 (3.00-4.00) |
4.00 (4.00-5.00) |
441.00 |
-4.54 |
< 0.001* |
|
11 |
I can establish nursing plans. |
3.00 (2.00-4.00) |
4.00 (4.00-4.75) |
528.00 |
-5.13 |
< 0.001* |
|
12 |
I can plan the necessary care. |
3.50 (3.00-4.00) |
4.00 (4.00-5.00) |
456.00 |
-4.21 |
< 0.001* |
|
13 |
I can determine patient care. |
3.00 (2.25-4.00) |
4.00 (3.00-4.00) |
419.00 |
-3.99 |
< 0.001* |
|
14 |
I can determine patient care quickly. |
3.00 (2.00-4.00) |
4.00 (4.00-4.00) |
496.00 |
-5.15 |
< 0.001* |
|
15 |
Total |
49.00 (40.00-51.00) |
60.00 (53.50.-63.00) |
939.00 |
-5.63 |
< 0.001* |
Note 1: The scores for the question items and the total score are presented as medians (interquartile range).
Note 2: The data were analyzed using the Wilcoxon signed-rank sum test. Significant differences are indicated by P < 0.05*.
Table 3. Comparison of the Pre-and Post-session Scores of the CRSS of the Intervention Group.
|
No. |
Question items |
Pre-session |
Post-session |
Test Statistic (W) |
Z value |
P value |
|
1 |
I can apply the interview and physical examination to assess the patient’s condition. |
3.00 (3.00-4.00) |
4.00 (4.00-4.00) |
345.00 |
-3.97 |
< 0.001* |
|
2 |
I can interpret the information collected. |
3.50 (3.00-4.00) |
4.00 (4.00-4.00) |
207.00 |
-2.24 |
0.02* |
|
3 |
I can recognize the need for more information. |
3.00 (2.75-4.00) |
4.00 (3.00-4.00) |
381.00 |
-4.28 |
< 0.001* |
|
4 |
I can distinguish between necessary and unnecessary information. |
3.00 (2.00-4.00) |
4.00 (3.00-4.00) |
234.00 |
-3.17 |
0.001* |
|
5 |
I can anticipate how my decisions will affect the patient's condition. |
3.00 (2.00-4.00) |
4.00 (3.00-4.00) |
264.00 |
-2.84 |
0.004* |
|
6 |
I can assess the cause and effect relationships in the patient’s condition. |
3.00 (3.00-3.00) |
4.00 (3.00-4.00) |
391.50 |
-3.40 |
0.001* |
|
7 |
I can recognize the need for patient care. |
4.00 (3.75-4.00) |
4.00 (4.00-5.00) |
117.00 |
-2.02 |
0.04* |
|
8 |
I can identify nursing problems. |
3.00 (3.00-4.00) |
4.00 (3.00-4.00) |
253.00 |
-2.69 |
0.007* |
|
9 |
I can notice changes in the patient's condition. |
4.00 (3.00-4.00) |
4.00 (3.00-4.00) |
109.00 |
-2.23 |
0.02* |
|
10 |
I can prioritize the patient’s needs. |
3.00 (3.00-4.00) |
3.00 (3.00-4.00) |
149.00 |
-2.30 |
0.02* |
|
11 |
I can establish nursing plans. |
3.00 (3.00-3.00) |
4.00 (3.00-4.00) |
318.50 |
-3.81 |
< 0.001* |
|
12 |
I can plan the necessary care. |
3.00 (3.00-4.00) |
4.00 (3.00-4.00) |
348.50 |
-3.49 |
< 0.001* |
|
13 |
I can determine patient care. |
3.00 (3.00-4.00) |
4.00 (3.00-4.00) |
288.00 |
-2.98 |
0.003* |
|
14 |
I can determine patient care quickly. |
3.00 (2.00-3.00) |
3.00 (3.00-4.00) |
295.00 |
-3.71 |
< 0.001* |
|
15 |
Total |
46.00 (41.0-050.25) |
52.00 (48.00-59.00) |
826.5 |
-4.69 |
< 0.001* |
Note 1: The scores for the question items and the total score are presented as medians (interquartile range).
Note 2: The data were analyzed using the Wilcoxon signed-rank sum test. Significant differences are indicated by P < 0.05*.
Table 4. Comparison of the Pre-and Post-session Scores of the CRSS of the Control Group.
Narrative Responses
During the session, participants in both the intervention and control groups provided narrative responses to a six-task group assignment.
For five of the tasks-Interview, Inspection, Palpation, Percussion, and Auscultation-no notable differences were observed between the two groups. Therefore, the common themes identified from both groups are summarized in Appendix Tables A4-A8. Appendix Tables A4-A8 present representative excerpts of the written narrative responses from both the intervention and control groups for the five physical assessment tasks. These tables illustrate how students applied clinical reasoning to assess physical signs and symptoms through written responses.
However, clear differences emerged between the intervention and control groups in the sixth task, which required students to propose nursing care plans for the simulated patient. Table 5 summarizes these responses, categorized into common responses and those unique to each group.
The intervention group provided more specific nursing care plans based on the patient's symptoms. Example responses included: "Have a lap blanket available for the patient during wheelchair transfer to address cold extremities." "Accompany the patient to the tests/examinations, considering palpitations and shortness of breath."
In contrast, the control group tended to offer general nursing care responses commonly associated with heart failure rather than case-specific interventions. Example responses included: "Provide guidance and management regarding restrictions on salt and water intake."
|
Responses |
|
Common responses from the intervention and control groups |
|
Measure vital signs (respiration, percutaneous oxygen saturation, pulse, blood pressure, respiratory rate and body temperature). |
|
Ensure comfortable positions (Fowler's position or the orthopneic position). |
|
Transfer the patient in a wheelchair due to shortness of breath and edema. |
|
Prepare and administer oxygen therapy. |
|
Explain what to expect before and after the tests/examinations and provide psychological care to reduce the patient's anxiety. |
|
Provide care for edema. |
|
Responses unique to the intervention group |
|
Accompany the patient to the tests/examinations, considering palpitations and shortness of breath. |
|
As emotional support, ask the patient if they are cold or how they are feeling. |
|
Prepare a vomit disposal bag. |
|
Check for changes in the patient's physical condition, facial color, and overall appearance during the examination. |
|
Used closed questions to make it easier for the patient to respond. |
|
Have a lap blanket available for the patient during transfer in a wheelchair to help with cold extremities. |
|
Responses unique to the control group |
|
Provide guidance and management regarding restrictions on salt and fluid intake. |
|
Provide nutritional guidance, including limiting indulgences and alcohol consumption. |
|
Provide bathing assistance. |
|
Perform measures to prevent pressure ulcers. |
|
Explain appropriate actions when symptoms worsen. |
|
Provide care for delirium. |
|
Provide rehabilitation exercise for range of motion. |
|
Provide guidance on lifestyle after discharge and outpatient follow-ups. |
|
Mange fluid balance by monitoring the body weight and urine output. |
|
Perform medication management and administration, including monitoring the effects and side effects. |
Table 5. Narrative Responses Provided by the Intervention and Control Groups: Nursing Care
DISCUSSION
This study aimed to examine the effectiveness of using pre-assignment work and specific cues in a case-based group learning session to enhance the clinical reasoning skills of undergraduate nursing students in physical assessment. The findings revealed two key outcomes that support the value of this educational approach.
First, although the pre-session scores of the CRSS Scale between the intervention and control groups showed no significant difference, the post-session scores of the intervention group were significantly higher on 10 items compared to the control group. The lack of significant differences in pre-session CRSS scores between groups supports the internal validity of the findings by indicating comparable baseline levels of clinical reasoning skills. The intervention group scored significantly higher on items related to information collection (No. 1) and interpretation (Nos. 2 and 6), problem identification (No. 9), and goal setting (Nos. 11 and 14).
Effective clinical reasoning requires nurses to accurately collect relevant cues and take appropriate action for the right patient, at the right time, and for the right reason [24]. Our findings suggest that the participants in the intervention group self-assessed improvements in their ability to collect and interpret information by utilizing the pre-assignment and interpreting the specific cues provided by the researcher as prompts for clinical reasoning. Furthermore, the significantly higher post-session scores in the intervention group indicate that the participants were able to recognize improvements not only in information collection and interpretation but also in planning appropriate nursing care interventions tailored to the patient's needs. These results imply that the intervention strengthened their ability to link patient information to problem identification and appropriate decision-making.
These findings are consistent with previous research indicating that collaborative and cue-based learning strategies can enhance clinical reasoning skills among nursing students. For example, Levett-Jones et al. [10] found that structured case-based learning promoted deeper analysis and more accurate clinical judgments. However, whereas many previous studies focused primarily on simulation-based or full-scale clinical scenarios, the present study demonstrates that similar improvements in clinical reasoning can be achieved through brief, structured interventions embedded in routine coursework. This suggests that even short, well-designed activities can meaningfully contribute to students’ development of clinical reasoning competencies.
Second, regarding the task responses, there were no notable differences between the intervention and control groups in the Interview, Inspection, Palpation, Percussion, and Auscultation tasks. This result is likely because physical assessment skills are generally acquired through repeated practice [3], and both groups had already completed basic training in these skills before participating in the study. However, significant differences emerged in the Nursing Care task.
Participants in the intervention group provided more specific and patient-centered nursing care plans based on the symptoms presented in the case. For example, their responses included: "Have a lap blanket available for the patient during wheelchair transfer to address cold extremities." "Accompany the patient to the tests/ examinations, considering palpitations and shortness of breath."
In contrast, the control group tended to offer generalized nursing interventions typical for heart failure patients, without tailoring their care to the specific symptoms of the case. Example responses included: "Provide guidance and management regarding restrictions on salt and water intake."
This difference suggests that participants in the control group lacked the ability to accurately identify and prioritize patient-specific cues, which was also reflected in their CRSS scores after the session. Supporting nursing students to focus on relevant cues, understand patient conditions and problems, and appreciate how these cues influence clinical judgments and patient outcomes is essential for the development of clinical reasoning skills [25]. In this study, specific cues provided by the researcher helped guide the intervention group participants to focus on the most relevant signs and symptoms, interpret them logically, and develop more targeted and appropriate nursing care interventions. The success of this intervention highlights the importance of structured support strategies in nursing education to bridge the gap between physical assessment findings and effective clinical decision-making. While this study demonstrated immediate improvements in clinical reasoning skills and nursing care specificity following the intervention, it did not assess long-term retention or the transfer of these skills to clinical practice. The sustainability of the observed learning gains and their impact on real-world nursing settings remain unknown. Future studies should incorporate follow-up assessments to evaluate whether these improvements are maintained over time and translated into clinical competence.
Implications for Practice and Future Research
The intervention used in this study, which encouraged undergraduate nursing students to utilize pre-assignment work and obtain specific cues during physical assessment, demonstrated potential for effectively fostering clinical reasoning skills even in settings with limited facilities and time.
This approach could be feasibly integrated into existing lecture-based curricula without the need for high-cost simulation equipment, making it particularly suitable for institutions with limited resources. For example, instructors can implement similar cue-enhanced case discussions in small group settings using printed case materials and structured prompts to guide clinical reasoning.
Future research should examine the long-term impact of this approach on knowledge retention and clinical performance. Additionally, comparative studies across multiple institutions and varying educational contexts are needed to assess the generalizability and scalability of the intervention. Investigating the effectiveness of this method in combination with simulation-based or OSCE-style assessments may also provide insights into optimizing nursing education strategies.
CONCLUSION
This study investigated the effectiveness of combining pre-assignment work with the provision of specific cues during a case-based group learning session to enhance clinical reasoning skills in undergraduate nursing students.
The findings indicate that the intervention group demonstrated significantly greater improvements in clinical reasoning ability compared to the control group, as evidenced by higher post-session scores on 10 items of the CRSS Scale. While no notable differences were observed in task responses related to Interview, Inspection, Palpation, Percussion, and Auscultation, the Nursing Care task revealed important distinctions. Students in the intervention group were more likely to identify relevant information and formulate specific, patient-centered care plans, suggesting a deeper understanding of the case context.
Overall, the results suggest that integrating structured pre-assignment learning with cue-based support can effectively foster clinical reasoning skills. This approach may be particularly beneficial in educational environments where access to simulation-based instruction is limited, offering a practical and scalable strategy to strengthen students’ reasoning capabilities in physical assessment.
Limitations
This study has several limitations. First, it was conducted at a single private women's university, potentially limiting generalizability due to contextual factors such as instructional style. Additionally, gender-related differences in clinical reasoning ability and learning preferences were not examined. These differences may influence how students engage with cue-based learning strategies, and therefore, the applicability of the results to mixed-gender or male student populations remains uncertain.
Second, the study assessed only immediate post-session outcomes; thus, the long-term retention and transfer to clinical practice remain unknown.
Third, while narrative responses were qualitatively reviewed, the absence of a formal thematic or content analysis may have limited the depth of qualitative insights.
Fourth, the sample size calculation followed a parametric approach based on an independent samples t-test using Cohen’s d index, which is commonly employed in educational intervention research.
We acknowledge that Cohen’s d is not the standard effect size for non-parametric tests like the Mann-Whitney U test used in this study. However, due to the lack of established tools supporting a priori power analysis for non-parametric effect sizes such as η² or rank-biserial correlation, we used Cohen’s d as a practical approximation.
Finally, the analysis did not account for potential clustering effects or use an intention-to-treat approach, which may introduce bias and affect the robustness of the findings.
Conflict of interest
The authors declare that they have no conflicts of interest.
Funding
This study was funded by a 2024 Cardiovascular Disease Nursing Research Grant (No. 12) from the Japan Cardiovascular Research Foundation.
Authors contribution
Author 1: Akifumi Maeda, MNS, RN, Lecturer, Faculty of Nursing, Senri Kinran University, Osaka, Japan, Contribution: Conception, design, supervision, funding, materials, data collection and processing, analysis and interpretation, literature review, writing, and critical review. E-mail: ak-maeda@cs.kinran.ac.jp; ORCID; http://orcid.org/0000-0002-2628-2224
Author 2: Akemi Hirao, PhD, RN, Professor, Faculty of Nursing, Senri Kinran University, Osaka, Japan, Contribution: Analysis and interpretation, literature review, writing, and critical review. E-mail: a-hirao@cs.kinran.ac.jp; ORCID: http://orcid.org/0009-0004-2902-5372
Author 3: Akiko Sugimoto, MNS, RN, Assistant Professor, Faculty of Nursing, Senri Kinran University, Osaka, Japan, Contribution: Conception, design, supervision, literature review, and writing. E-mail: a-sugimoto@cs.kinran.ac.jp; ORCID: http://orcid.org/0009-0003-0506-8370
Author 4: Motoko Hori, MNS, RN, Assistant Professor, Faculty of Nursing, Senri Kinran University, Osaka, Japan, Contribution: Conception, design, supervision, literature review, and writing. E-mail: m-hori@cs.kinran.ac.jp; ORCID; http://orcid.org/0000-0003-0864-2473
Acknowledgment
The authors wish to thank Nakaba Cosley for reviewing and providing English language editing on an earlier draft of the manuscript. We also express our sincere gratitude to the developers of the Japanese version of the CRSS for granting us permission to adapt and use the instrument in this study.
AI tools Usage
During the preparation of this manuscript, ChatGPT (OpenAI, https://openai.com/chatgpt) was utilized to assist with the initial English translation of the Japanese manuscript into English. The authors critically reviewed, edited, and validated all AI-generated outputs to ensure their accuracy, clarity, and appropriateness for scholarly publication. Additionally, professional English language editing was performed by Nakaba Cosley to finalize the manuscript. Importantly, no parts of the research data, study results, analysis, or scientific content were generated or altered using AI tools.
Appendix
|
No. |
Pre-assignment |
|
1 2 3 4 5 6 |
What diseases can cause heart failure? What symptoms are associated with failure of the right and left heart? What mechanisms cause those symptoms? What types of physical examinations are performed to address these symptoms? What nursing care can be provided to patients with heart failure? What tests are needed to diagnose and determine the treatment of heart failure? |
Table A1. Pre-assignment
|
The instructor asked participants to refer to their pre-assignment responses and provided the following verbal cues before they began working on each item as a group. |
|
|
Interview |
Think about the mechanism of heart failure that causes the patient's symptoms (dyspnea and edema) and interview the patient, including any associated symptoms. |
|
Inspection |
Think about the visible changes or symptoms caused by heart failure. |
|
Palpation |
Think about the palpable changes or symptoms caused by heart failure. |
|
Percussion |
Think about the symptoms or changes caused by heart failure that can be identified by percussing the body. |
|
Auscultation |
Think about auscultatory changes, such as heart or lung sounds, or symptoms caused by heart failure. |
|
Nursing care |
Think about the nursing care needed based on the patient's current condition and situation. |
Table A2. Verbal Cues Presented to the Intervention Group
|
Case scenario |
|
78-year-old female. The patient has been followed up on an outpatient basis after valve replacement surgery for mitral regurgitation. During her outpatient visit, she says, “I get short of breath when I walk a little, and the legs are swollen.” You’re an outpatient clinic nurse and suspect the patient may be suffering from heart failure. |
|
Group task |
|
Think about the interview and physical examination, using the answers in the pre-assignment to gather information that will provide evidence of heart failure. Also think about the specific nursing care based on the patient's current condition. Describe the contents of the interview, physical examination, and nursing care on the answer sheet. |
Table A3. Case scenario and Group task
|
Responses |
|
Symptom location |
|
Interview the patient about edema of the legs (left-right differences, one leg or both legs). |
|
Symptom history |
|
Interview the patient about when edema of the legs and shortness of breath started and any subsequent changes. |
|
Symptom severity |
|
Interview the patient about the severity of shortness of breath (on a scale of 1 to 10) and the severity of edema (whether socks leave marks or shoes can be worn). |
|
Associated symptoms |
|
Interview the patient if any associated symptoms are present, including loss of appetite, nausea, weight changes, fatigue, and sensation of coldness. |
|
Contributing factors |
|
Interview the patient about situations in which shortness of breath occurs (when walking or at rest). |
|
Interview the patient about lifestyle (physical activity and salt and fluid intake). |
|
Medication |
|
Interview the patient about whether or not the patient is taking any medication, the type of medication, and the medication status. |
Table A4. Narrative Responses Provided by the Intervention and Control Groups: Interview
|
Responses |
|
Respiration |
|
Observe respiratory rate, rhythm, depth, and the presence of orthopnea. |
|
Cyanosis |
|
Observe changes in the color of the skin, nails, and lips. |
|
Distension of the jugular veins |
|
Observe for distension and pulsation of the jugular veins. |
|
Facial color and complexion |
|
Observe for pallor, jaundice, and fatigue in facial complexion. |
|
Edema |
|
Observe for edema, left-right differences, the degree of swelling, and its location (legs and face). |
|
Sweating |
|
Observe for cold sweats and sweating. |
|
Somatotype and abdominal distention |
|
Observe for obesity and abdominal distention. |
Table A5. Narrative Responses Provided by the Intervention and Control Groups: Inspection
|
Responses |
|
Vocal fremitus |
|
Check for decreased or absent vibration of the thorax. |
|
Pulse |
|
Check the pulse rate, rhythm, presence of arrhythmia, left-right differences, and strength. |
|
Coldness of limbs |
|
Check the temperature and presence of coldness in the limbs. |
|
Edema |
|
Press the shin or ankle with a finger to check for indentation, depth, and the time to return. |
|
Liver |
|
Check the size, shape, and tenderness of the liver. |
Table A6. Narrative Responses Provided by the Intervention and Control Groups: Palpation
|
Responses |
|
Pleural effusion |
|
Check for pleural effusion. |
|
Ascites |
|
Check for ascites. |
|
Liver |
|
Check the size of the liver. |
Table A7. Narrative Responses Provided by the Intervention and Control Groups: Percussion
|
Responses |
|
Breath sounds |
|
Check for left-right differences, moist rales, dry rales, and adventitious sounds. |
|
Heart sounds |
|
Check for an accentuated or diminished first heart sound, a loud second heart sound, a third heart sound, and a fourth heart sound. |
|
Vascular murmurs |
|
Check for murmurs in the carotid artery, abdominal aorta, renal artery, and arteries of the lower extremities. |
|
Abdomen |
|
Check for bowel sounds. |
Table A8. Narrative Responses Provided by the Intervention and Control Groups: Auscultation
REFERENCES
- Alfaro-LeFevre R. Nursing process and clinical reasoning. Nurs Educ Perspect. 2012; 33(1): 7, doi: 10.5480/1536-5026-33.1.7.
- Chua WL, Legido-Quigley H, Ng PY, Ali S, Arora S, Liaw SY, et al. Seeing the whole picture in enrolled and registered nurses’ experiences in recognizing clinical deterioration in general ward patients: a qualitative study. Int J Nurs Stud. 2019; 95: 56-64. doi: 10.1016/j.ijnurstu.2019.04.012.
- Goto H, Yamauchi T. Nurse perceptions of physical assessment skills for detecting acute progression of heart failure. Jpn J Nurs Sci. 2020; 18(1): e12368. doi:10.1111/jjns.12368.
- Zambas S, Smythe E A, Koziol-Mclaine J. The consequences of using advanced physical assessment skills in medical and surgical nursing: A hermeneutic pragmatic study. Int J Qual Stud Health Well-being. 2016; 11: 32090. doi: 10.3402/qhw.v11.32090.
- Morrell S, Giannotti N, Pittman G, Roche M, McKinlay L, et al. Physical assessment skills taught in nursing curricula: a scoping review. JBI Evid Synth. 2021; 19(11): 2929-2957. doi: 10.11124/JBIES-20-00086.
- Cant R. P, Cooper, S J. Simulation-based learning in nurse education: systematic review. J Adv Nurs. 2010; 66(1): 3-15. doi:10.1111/j.1365-2648.2009.05240.x.
- Tawalbeh L. Effect of simulation on the confidence of university nursing students in applying cardiopulmonary assessment skills: A randomized controlled trial. J Nurs Res. 2017; 25(4): 289-295. doi: 10.1097/JNR.0000000000000170.
- Ferrari A, Maglio S, Tamirat S, Tesfaye M, Wolde M, Manenti F, et al. Nursing and midwifery simulation training with a newly developed low-cost high-fidelity placenta simulator: a collaboration between Italy and Ethiopia. BMC Med Educ. 2024; 24(1): 42. doi: 10.1186/s12909-024-06152-0.
- Hoffman K. A Comparison of decision-making by expert and novice nurses in the clinical setting, monitoring patient haemodynamic status post abdominal aortic aneurysm surgery. PhD Thesis. University of Technology, Sydney; 2007 [cited 2025 May 2]. Available from: http://hdl.handle.net/10453/21800.
- 10.Levett-Jones T, Hoffman K, Dempsey J, Jeong SY, Noble D, Norton C, et al. The 'five rights' of clinical reasoning: an educational model to enhance nursing students' ability to identify and manage clinically 'at risk' patients. Nurse Educ Today. 2010; 30(6): 515-520. doi: 10.1016/j.nedt.2009.10.020.
- Tanner CA. Thinking like a nurse: a research based model of clinical judgment. J Nurs Educ. 2006; 45(6): 204-211. doi: 10.3928/01484834-20060601-04.
- Hoffman A K, Aitken L M, Duffield C. A comparison of novice and expert nurses’ cue collection during clinical decision-making: Verbal protocol analysis. Nurse Educ Today. 2016; 46:1335-1344. doi: 10.1016/j.nedt.2016.04.001.
- Shin S, Park J H, Kim J H. Effectiveness of patient simulation in nursing education: Meta-analysis. Nurse Educ Today. 2015;35(1):176–182. doi:10.1016/j.nedt.2014.09.009.
- Bahramnezha F, Shakour M, Ravanipour M, Moattari M. Clinical reasoning education: Evaluating the effect of script strategy and reflective practice on nursing students’ reasoning development. BMC Res Notes. 2024;17:240. doi:10.1186/s13104-025-07338-5.
- Hopewell S, Chan AW, Collins GS, Hróbjartsson A, Moher D, Schulz KF, et al. CONSORT 2025 Statement: updated guideline for reporting randomised trials. BMJ. 2025; 388: e081123. doi: 10.1136/bmj-2024-081123.
- Faul F, Erdfelder E, Lang AG, Buchner A. GPower 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behavior Research Methods. 2007; 39(2):175–191. doi:10.3758/BF03193146.
- International Committee of Medical Journal Editors. Clinical Trials Registration. ICMJE. 2022 [cited 2025 Jun 2]. Available from: http://www.icmje.org/recommendations/browse/publishing-and-editorial-issues/clinical-trial-registration.html
- Ponikowski P, Anker SD, AlHabib KF, Cowie MR, Force TL, Hu S, et al. Heart failure: preventing disease and death worldwide. ESC Heart Failure. 2014; 1(1): 4–25. doi: 10.1002/ehf2.12005.
- Okura Y, Ramadan MM, Ohno Y, Suzuki K, Tanaka F, Matsumoto Y, et al. Impending epidemic: future projection of heart failure in Japan to the year 2055. Circ J. 2008; 72(3): 489-491.
- Conrad N, Judge A, Tran J, Mohseni H, Hedgecott D, Crespillo AP, et al. Temporal trends and patterns in heart failure incidence: a population-based study of 4 million individuals. The Lancet. 2018; 391(10120): 572-580. doi: 10.1016/S0140-6736(17)32520-5.
- Harmon MM, Thompson C. Clinical reasoning in pre-licensure nursing students. Teach Learn Nurs. 2015; 10(2): 63-70. doi: 10.1016/j.teln.2014.12.001.
- Naya K, Sakuramoto H, Nojima K, Ohkawa M, Tanaka Y, et al. Translation, reliability, and validity of the Japanese clinical reasoning skills self-evaluation scale: An instrument design study. Cureus. 2024; 16(1): e53177. doi: 10.7759/cureus.53177.
- Havola S, Haavisto E, Mäkinen H, Jalonen P, Koivisto J. The effects of computer-based simulation game and virtual reality simulation in nursing students' self-evaluated clinical reasoning skills. Comput Inform Nurs. 2021; 39(11): 725-735. doi: 10.1097/CIN.0000000000000748.
- Andersen B. Mapping the terrain of the discipline. In: Gray G, Pratt R, editors. Towards a Discipline of Nursing. Melbourne: Churchill Livingstone; 1991. p. 95-124.
- Benner P. From novice to expert: Excellence and power in clinical nursing practice. 2nd ed. Upper Saddle River (NJ): Prentice Hall; 2001.
![]() This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
EFFICACY OF NEGATIVE PRESSURE WOUND THERAPY IN LAPAROTOMY WOUNDS: PROTOCOL FOR A SYSTEMATIC REVIEW AND META-ANALYSIS
Melania De Filippo 1, Marco Abagnale 2*, Anella Di Costanzo 3, Valeria Visconti 4,
Fabio Gennaro Abagnale 2, Rita Citarella 5
1 Department of Abdominal Oncology, Colorectal Surgical Oncology, Istituto Nazionale Tumori – IRCCS "Fondazione G.Pascale”, Napoli, 80131, Napoli, Italy.
2 Department of Critical Care, Unit of Anesthesiology and Intensive Care, M. Scarlato Hospital, Scafati (SA), 84018, Local Healt of Salerno, Salerno, Italy.
3 Department of Cardiac Thoracic Vascular Surgery, Cardiac Thoracic Vascular Surgery, Pineta Grande Hospital, Castel Volturno, Caserta, 81030, Italy.
4 Department of Medicine, Rheumatology Unit, M. Scarlato Hospital, Scafati (SA), 84018, Local Healt of Salerno, Salerno, Italy.
5 Department of Surgery and Anaesthesia, "Umberto I" Hospital of Nocera Inferiore", 84014, Salerno, Italy.
* Corresponding author: Marco Abagnale, e-mail: abagnale.marco@gmail.com
Cite this article
ABSTRACT
Introduction: A laparotomy is a surgical procedure involving an abdominal incision to access the peritoneal cavity, commonly performed for diagnostic and therapeutic purposes, including trauma management and the treatment of gynecological, pelvic, and abdominal conditions. In this context, negative pressure wound therapy (NPWT) serves as an effective adjunct to wound management by applying subatmospheric pressure to the wound bed, thereby promoting granulation tissue formation and reducing local inflammation.
Objective: This systematic review will aim to evaluate the efficacy of NPWT compared to standard wound care in adult patients undergoing laparotomy, with specific attention to key clinical outcomes such as wound healing time, surgical site infection rates, wound dehiscence, and overall complication rates.
Materials and methods: The systematic review follows the PRISMA guidelines and uses the PICO framework for search terms. The studies will be identified through important databases (PubMed, Scopus, CINAHL and Web of Science). Methodological quality and risk of bias will be assessed with JBI critical assessment tools. This protocol for a systematic review has been registered on PROSPERO (N. CRD420251058825).
Results: The results of the systematic search and selection process will be reported using a PRISMA flowchart. The extracted data will include wound healing time, granulation tissue development, infection rates, and adverse events. The quantitative synthesis will be conducted if the homogeneity of the data allows it.
Conclusions: This systematic review will synthesize the available evidence on the efficacy of NPWT in the management of laparotomy wounds. The findings will have implications for clinical practice in surgical wound care and may contribute to the development of standardized wound management protocols.
Keywords: Laparotomy, negative pressure wound therapy, bandages, wound healing, granulation tissue, systematic review.
INTRODUCTION
A laparotomy involves a surgical incision through the abdominal wall to access the peritoneal cavity during a laparotomy procedure [1-5]. This incision is typically a large vertical cut that allows surgeons to examine and treat conditions within the abdominal organs. The term "laparotomy" itself denotes this surgical approach, which is often employed in both emergency and planned surgical settings [6]. Laparotomy remains a common surgical procedure worldwide, particularly in the treatment of abdominal trauma, intestinal obstruction, perforated bowel, and malignancies [3]. Despite its widespread use, laparotomy is associated with a high incidence of postoperative wound complications. Recent data indicate that surgical site infections (SSIs) occur in approximately 20–30% of laparotomy cases, especially in high-risk settings such as emergency surgeries or in patients with comorbidities. According to a multicenter cohort study published in 2022, SSI rates after emergency abdominal surgery reached up to 33%, with wound dehiscence observed in 4–6% of cases [7,8]. Wound dehiscence, defined as the partial or complete separation of a surgically closed wound, is strongly associated with increased morbidity, delayed recovery, and higher mortality. In a recent analysis conducted in the United States, SSIs following laparotomy were found to contribute to an average extended hospital stay of 9.7 days and increased treatment costs by over $20,000 per patient [9]. Surgical wound dehiscence (SWD) occurs in approximately 1% of patients within 30 days following laparotomy, with a prevalence of up to 3% in hepatobiliary surgery [8]. Among older patients, the incidence may reach 10%, with an associated mortality rate of up to 45% [9]. A study involving 674 patients undergoing emergency laparotomy documented a 31.9% rate of surgical complications, including 16.3% SSIs and 5% wound dehiscence. Furthermore, 19.1% of patients required surgical reintervention, while 53.6% experienced additional medical complications such as respiratory failure or sepsis [10].
These complications place a significant burden on healthcare systems. For example, a 2023 analysis estimated that surgical site infections alone contribute to over USD 3.3 billion in annual costs in the United States, primarily due to extended hospital stays, additional interventions, and increased resource utilization [6,7]. In addition, wound complications often require additional interventions, such as reoperations, prolonged antibiotic therapy, or advanced wound care support, thus placing a considerable burden on both healthcare systems and patients. Effective postoperative wound management is therefore essential to reduce these risks and promote optimal recovery. Conventional dressing techniques may be insufficient in high-risk patients or in complex surgical settings. In recent years, NPWT has emerged as an innovative approach to improving surgical wound healing. By applying controlled subatmospheric pressure through a sealed dressing system, NPWT improves tissue perfusion, reduces local edema, and facilitates the removal of exudates and contaminants [11,12]. It also promotes the formation of granulation tissue and can promote faster and longer-lasting wound closure.
Although NPWT is increasingly utilized across various surgical disciplines, no systematic review focused exclusively on its effectiveness in laparotomy wounds exists to date, there is still limited consensus regarding its efficacy specifically in laparotomy wounds. Available studies show heterogeneous results, often influenced by variability in patient populations, the type of procedure (elective vs. emergency laparotomy), surgical techniques, and NPWT protocols (e.g., pressure settings, duration, frequency of dressing changes). Furthermore, many investigations suffer from methodological limitations, small sample sizes, or a lack of attention to patient-reported outcomes such as pain, quality of life, and satisfaction with care. While some reviews in other surgical contexts have reported potential benefits of NPWT, there is currently no systematic synthesis specifically focused on laparotomy wounds. In light of these gaps, the present protocol for a systematic review aims to guide a rigorous systematic review designed to comprehensively assess the clinical efficacy of NPWT in this specific surgical population.
The use of negative pressure wound therapy (NPWT) in laparotomy wounds may offer substantial clinical advantages over conventional wound care approaches. By promoting faster wound healing, reducing the incidence of surgical site infections, and decreasing the risk of wound dehiscence, NPWT has the potential to improve surgical outcomes, particularly in high-risk patients. Its application may also reduce the need for reoperations and prolonged antibiotic therapy, thereby shortening hospital stays and facilitating earlier discharge. From a patient-centered perspective, NPWT may lead to improved pain control, better quality of life, and enhanced satisfaction with care. Integrating NPWT into postoperative care pathways could thus contribute to more efficient resource use and support the development of evidence-based protocols aimed at optimizing recovery following major abdominal surgery.
This systematic review aims to evaluate the efficacy of NPWT in laparotomy wounds by analyzing key clinical outcomes, including wound healing time, incidence of surgical site infection, wound dehiscence, and complication rates. The systematic review will also plan to consider patient-centered outcomes such as pain, quality of life, and satisfaction with care, supporting evidence-based decision-making in postoperative wound treatment.
OUTCOMES
Primary Outcomes
- Incidence of surgical site infection (SSI)
- Wound healing time (days from surgery to complete epithelialization or closure)
- Rate of wound dehiscence (partial or complete separation of the wound)
Secondary Outcomes
- Postoperative pain scores (as measured by validated pain scales, e.g., VAS or NRS)
- Quality of life (measured by validated tools such as EQ-5D, SF-36)
- Patient satisfaction with wound care
- Length of hospital stay
- Rate of reoperation related to wound complications
- Incidence of wound-related hospital readmissions
This systematic review will focus exclusively on adult patients (≥18 years) undergoing laparotomy procedures in either elective or emergency surgical settings.
Where sufficient data homogeneity is identified across studies in terms of populations, interventions, and outcome measures, a meta-analysis will be conducted. Statistical heterogeneity will be assessed using the I² statistic, with a threshold of I² > 50% indicating substantial heterogeneity. In such cases, a random-effects model will be applied. If heterogeneity is too high or data are insufficiently comparable, results will be synthesized using a narrative approach, supported by structured tables and descriptive analysis. Subgroup analyses (e.g., by type of laparotomy or patient risk profile) will be considered where appropriate and data permit.
MATERIALS AND METHODS
Study Protocol
This preliminary protocol for a systematic review is designed to ensure methodological consistency and alignment of the selected studies with the overall objectives of the systematic review. The final synthesis will aim to provide a clear and evidence-based contribution to the scientific discourse on the topic.
The protocol for a systematic review will be conducted in accordance with PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analysis) guidelines. In particular, the PRISMA-P (Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols) checklist [13,14] was used to structure this protocol for a systematic review [refer to supplemental files for the complete checklist], while the full PRISMA 2020 guidelines will be used in the reporting of the final manuscript of the systematic review.
Eligibility criteria
The systematic research was developed following the PICO framework described in Table 1.
| Popolation | Patients undergoing laparotomy and with laparotomy surgical wound |
| Intervention | Negative pressure wound therapy |
| Confront | Standard Care |
| Outcome | Granulation Tissue / Wound Healing |
Table 1. PICO Framework
Eligibility criteria will include peer-reviewed primary research studies investigating the efficacy of negative pressure wound therapy in the management of laparotomy wounds. Eligible study designs will include observational studies (cohort, cross-sectional), quasi-experimental studies, randomized controlled trials (RCTs), non-randomized controlled trials, and interventional studies. The exclusion criteria will outline parameters to maintain the focus and integrity of the systematic review. Studies investigating non-laparotomies wounds, the use of other devices such as Prevena or PICO or conventional dressings, secondary studies, outcomes not related to healing will also be excluded. Similarly, editorials and opinion articles lacking primary data, animal studies, and experimental or laboratory models will be excluded from the scope of this systematic review. In addition, studies focused exclusively on pediatric populations (<18 years) will not be considered. Unpublished studies and academic theses typically lack the rigorous peer review process necessary to ensure methodological soundness, thus raising questions about their reliability and scientific validity. Similarly, while conference abstracts can offer preliminary insights into ongoing research, they are often concise and not sufficiently detailed, lacking the comprehensive data and analytical depth needed to support solid conclusions. The experimental protocols, although valuable for the understanding of the proposed methodologies, do not present empirical results and therefore offer limited utility in evidence-based evaluations. No language restrictions will be applied during the literature search to ensure comprehensive coverage of the available evidence. To mitigate the risk of excluding relevant non-English studies, the systematic review team will use professional translation tools and, when necessary, involve collaborators or native speakers for accurate interpretation of full texts. Articles in languages unfamiliar to the systematic review team will be assessed for eligibility through translated abstracts or consulted with multilingual experts when available.
Sources of information
This systematic review will include primary research studies that directly address the research question, including randomized controlled trials (RCTs), cohort studies, cross-sectional studies, case-control studies, and qualitative investigations.
The protocol for a systematic review was developed using the PICO (Population–Intervention–Comparison–Outcome) framework to ensure a methodologically sound and targeted approach to the synthesis of evidence. To ensure the completeness of the review, a structured and systematic research strategy will be employed. Carefully selected search terms will be applied to multiple electronic databases, including MEDLINE (via PubMed), CINAHL (via EBSCO), Web of Science (WOS), and SCOPUS. All eligible studies published up to the date of data extraction will be considered. Given the specific objective of the research question, the PICO framework will facilitate the precise delineation of the scope of the systematic review (Table 1).
Two independent reviewers will conduct the first screening of the titles and abstracts. In the event of disagreement, a fourth reviewer will be consulted to reach consensus. Full-text articles will be evaluated to determine final eligibility for inclusion in the systematic review.
Research strategy
We used keywords and search terms as shown in the Table 2 Duplicate records will be identified and removed using Rayyan software (Rayyan Enterprise, Cambridge, MA, USA, , accessed on 29.4.2025 [15].
| #1 Laparotomy"[MeSH Terms] |
| #2 Negative Pressure Wound Therapy"[MeSH Terms] |
| #3 negative pressure wound therapy"[MeSH Terms] OR ("negative pressure"[All fields] AND "wound"[All fields] AND "therapy"[All fields]) OR "negative pressure wound therapy"[All fields] OR ("empty"[All fields] AND "assisted"[All fields] AND "closure"[All fields]) OR "void-assisted closure"[All fields] |
| #4 Bandages"[MeSH Terms] Or "Bandages, Hydrocolloids"[MeSH Terms] Or "Occlusive Dressings"[MeSH Terms] |
| #5 Wound healing"[MeSH terms] OR "Granulation tissue"[MeSH terms] |
Table 2. Key terms and search strategy.
The defined keywords adhere to the Mesh term for health research. The keywords being used are varied because they are tailored to the search engine. The keywords are combined with Boolean operators such as “OR” and “AND” (Table 3)
| Database | Research | Results | Date |
| PubMed | ("Laparotomy"[MeSH Terms] AND "Negative Pressure Wound Therapy"[MeSH Terms]) OR ("Negative Pressure Wound Therapy"[MeSH Terms] OR ("Negative Pressure"[All Fields] AND "Wound"[All Fields] AND "Therapy"[All Fields]) OR "Negative Pressure Wound Therapy"[All Fields] OR ("Blank"[All Fields] AND "Assisted"[All Fields] AND "Closure"[All Fields]) OR "Vacuum Assisted Closure"[All Fields])) AND ("Bandages"[MeSH Terms] OR "Bandages, hydrocolloids"[MeSH terms] or "occlusive dressings"[MeSH terms]) and ("Wound healing"[MeSH terms] or "granulation tissue"[MeSH terms]) | 703 | 29/04/2025 |
| Scopus | (INDEXTERMS(Laparotomy) AND INDEXTERMS("Negative Pressure Wound Therapy")) OR (INDEXTERMS("Negative Pressure Wound Therapy") OR (ALL("negative pressure") AND ALL(wound) AND ALL(therapy)) OR ALL("Negative Pressure Wound Therapy") OR (ALL(vacuum) AND ALL(assisted) AND ALL(closure)) OR ALL("vacuum-assisted closure"))AND (INDEXTERMS(BANDAGES) OR INDEXTERMS("Bandages, Hydrocolloid") OR INDEXTERMS("Occlusive Dressings")) AND (INDEXTERMS("Wound Healing") OR INDEXTERMS("Granulation Tissue")) | 1176 | 29/04/2025 |
| CINAHL | ((HD Laparotomy+) AND (HD "Negative Pressure Wound Therapy+")) OR ((MH "Negative Pressure Wound Therapy+") OR ("Negative Pressure" AND Wound And Therapy) OR "Negative Pressure Wound Therapy" OR (Vacuum AND Assisted Closure AND) OR "Vacuum Assisted Closure")AND ((MH Bandages+) OR (MH "Bandages, Hydrocolloid+") OR (MH "Occlusive Dressings+")) AND ((MH "Wound Healing+") OR (MH "Granulation Tissue+")) | 921 | 29/04/2025 |
| WOS | (ALL=Laparotomy AND ALL="Negative Pressure Wound Therapy") OR (ALL="Negative Pressure Wound Therapy" OR (ALL="negative pressure" AND ALL=wound AND ALL=therapy) OR ALL="Negative Pressure Wound Therapy" OR (ALL=vacuum AND ALL=assisted AND ALL=closure) OR ALL="Vacuum-Assisted Closure")AND (ALL=Bandages OR ALL="Bandages, Hydrocolloid" OR ALL="Occlusive Dressings") AND (ALL="Wound Healing" OR ALL="Granulation Tissue") | 230 | 01/05/2025 |
Table 3. The search string
Selection process
The methodological quality of the included studies will be assessed using the Joanna Briggs Institute (JBI) critical evaluation tools, selecting the appropriate checklist based on the study design (e.g., case-control studies, case reports, cohort studies, case series, quasi-experimental studies, and randomized controlled trials) [16]. Each tool includes multiple elements, with response options limited to: Yes, No, ambiguous not applicable. This systematic review protocol will follow the Preferred Reporting Items for Systematic Reviews and Meta-Analyses Protocols (PRISMA-P) guidelines [14,17]. The process of selecting and extracting data will take place in two distinct phases. Initially, two reviewers will independently review the titles and abstracts of all records retrieved using Rayyan software [15] to identify potentially suitable studies. Any disagreements will be resolved by consensus; If necessary, a third reviewer will be consulted to reach the resolution. In the second phase, three reviewers will independently evaluate the full texts of the selected studies and proceed with data extraction. To ensure methodological rigor and consistency throughout the review process, each included study will be critically evaluated for both internal validity and relevance.
The following data will be extracted independently by two reviewers:
- Author(s)
- Year and country of publication
- Study design
- Study population
- Clinical or care context
- Speech(s)
- Primary and secondary outcomes
- Main Findings/Achievements
Data collection process
A PRISMA flowchart will be included to provide a visual representation of the study selection process, detailing the number of records identified, reviewed, evaluated for eligibility, and excluded, along with justifications for exclusion. This revision will follow a systematic and standardized data collection procedure, using a predefined data extraction module to ensure consistency and reproducibility. Key data elements to be extracted from each included study will include: study design, participant characteristics, intervention details, outcome measures, and key outcomes. Quantitative data will be synthesized through narrative synthesis, allowing for a descriptive comparison between studies. Instead, qualitative results will be analyzed using thematic synthesis, aimed at identifying themes, insights, and patterns through the evidence base. Each study will be ranked according to its level of evidence, thus allowing for a comparative assessment of the robustness and reliability of the results. This integrative synthesis of mixed methods will combine qualitative and quantitative evidence to develop a comprehensive understanding of the efficacy of NPWT in laparotomy wound management.
Scan risk assessment study
The risk of bias in included studies will be systematically assessed by two or more independent reviewers using the ROBINS-E (Risk Of Bias In Non-Randomized Studies of Exposures) tool, which is specifically designed to assess bias in observational studies [14].
In the event of disagreement, discrepancies will first be discussed between two reviewers. If consensus cannot be reached, a third reviewer will be consulted to resolve the issue. To evaluate inter-rater reliability during the selection process, the level of agreement between reviewers will be quantitatively assessed using Cohen’s Kappa coefficient.
The ROBINS-E tool assesses the risk of bias in seven areas:
- Confusion bias
- Bias in the selection of participants
- Bias in exposure classification
- Bias due to deviations from planned interventions (post-exposure)
- Bias due to missing data
- Bias on the measurement of results
- Bias on the selection of the reported results.
Each domain will be assessed individually, and domain-level judgments will inform the overall assessment of bias risk for each study. Overall judgment will be classified as low risk, some concerns, high risk or critical risk of bias, in accordance with the ROBINS-E guidelines.
To assess the methodological quality of non-randomised studies, the ROBINS-E tool will be used. This tool was selected because it is specifically designed to evaluate bias in studies assessing the effects of exposures, which is appropriate given the observational nature of many studies expected in this systematic review (e.g., cohort studies comparing NPWT with conventional wound care). ROBINS-E includes domains such as confounding, selection of participants, measurement of exposure and outcomes, and selection of reported results—providing a comprehensive framework for appraising the internal validity of non-randomised designs. Compared to ROBINS-I, which is tailored more closely to interventions and clinical trials, ROBINS-E better aligns with the anticipated heterogeneity in clinical exposure settings observed in surgical wound management research.
Synthesis methods
In accordance with the Joanna Briggs Institute (JBI) data extraction framework, two or more independent reviewers will perform data extraction from full-text articles included in the systematic review to ensure completeness and accuracy. The information collected will include the key characteristics of the study, such as the author and year of publication, country of origin, study objectives, sample demographics, methodology and design, type of intervention, reported outcomes, and key findings. All data will be entered into a Microsoft Excel® spreadsheet to facilitate the construction of structured summary tables and comparative analysis. The synthesis of the results will be mainly narrative in nature, with the aim of identifying and describing recurring patterns and thematic elements in studies. This approach will allow reviewers to highlight conceptual consistencies, methodological trends, and gaps in the literature that could inform future research. Quantitative data, when available, will be presented descriptively, while qualitative data will be analyzed thematically to derive common insights and meaningful interpretations. The synthesis will be guided by a structured framework that explores relationships both within individual studies and across the broader evidence base, in order to map key themes and areas of convergence. In case the included studies demonstrate sufficient methodological and statistical homogeneity, a meta-analysis will be conducted using RevMan 5.3 software. A randomized effects model will be applied to account for variability expected in study design, intervention types, and population characteristics.
Where appropriate, data from included studies will be pooled in a meta-analysis. Heterogeneity will be assessed using the I² statistic and Chi-square test. If substantial heterogeneity is detected (I² > 50%), a random-effects model will be used; otherwise, a fixed-effect model will be applied. To explore sources of heterogeneity, subgroup analyses will be conducted based on predefined variables such as type of laparotomy (elective vs. emergency), NPWT protocol (duration, pressure setting), and patient risk profile (e.g., age, comorbidities). Sensitivity analyses will also be performed by excluding studies at high risk of bias or with small sample sizes to test the robustness of the findings.
Meta-Analysis Criteria
Where appropriate, data from included studies will be pooled in a meta-analysis. Heterogeneity will be assessed using the I² statistic and Chi-square test. If substantial heterogeneity is detected (I² > 50%), a random-effects model will be used; otherwise, a fixed-effect model will be applied. To explore sources of heterogeneity, subgroup analyses will be conducted based on predefined variables such as type of laparotomy (elective vs. emergency), NPWT protocol (duration, pressure setting), and patient risk profile (e.g., age, comorbidities). Sensitivity analyses will also be performed by excluding studies at high risk of bias or with small sample sizes to test the robustness of the findings.
Measurements and results
To ensure a comprehensive evaluation of the efficacy of NPWT in the management of laparotomy wounds, this systematic review will focus on both clinical and patient-centered outcomes. Primary outcomes of interest will include wound healing indicators such as time to complete wound closure, wound infection rates, incidence of wound dehiscence, and length of hospital stay. These measures are considered essential for evaluating the clinical efficacy and safety of NPWT compared to conventional wound care methods. Secondary outcomes will encompass broader dimensions of efficacy, including patient-reported outcomes such as pain reduction, quality of life, and satisfaction with care, when available. Additional findings may include the need for resurgery or revision, antibiotic use, and healthcare resource utilization, providing a more holistic understanding of the impact of NPWT in both acute and post-operative phases. Data related to these outcomes will be extracted and analyzed in relation to study design, population characteristics, intervention protocols, and duration of follow-up. The heterogeneity of result definitions and measurement tools will be taken into account in the summary to ensure the validity and applicability of the results. Through this multidimensional outcome framework, the systematic review aims to generate robust evidence on the clinical efficacy, patient benefit, and potential health system implications of NPWT in the context of laparotomy wound management.
Impact of the review
This systematic review will synthesize original research studies evaluating the efficacy of NPWT in adult patients (≥18 years old) undergoing laparotomy. By systematically analyzing outcomes such as wound healing time, infection rates, and surgical site complications, the systematic review aims to clarify the clinical value of NPWT in laparotomy wound management compared to standard wound care approaches. The systematic review will adopt a structured and transparent methodology to ensure the robustness and reproducibility of the results. Emphasis will be placed on identifying which patient populations and clinical conditions benefit most from NPWT, as well as examining intervention protocols, duration, and care settings. This evidence-based approach will facilitate the integration of best practices into perioperative wound management and postoperative care pathways. If NPWT has been shown to significantly improve clinical outcomes, it can offer a cost-effective and scalable intervention to improve surgical recovery, reduce complications, and optimize hospital resource utilization. In addition, the findings of this systematic review can help healthcare professionals develop targeted postoperative protocols and inform clinical decision-making, ultimately helping to improve patient safety and the quality of surgical care.
DISCUSSION
This systematic review protocol aims to evaluate the efficacy of negative pressure wound therapy (NPWT) in the management of laparotomy wounds, with a primary focus on clinical outcomes such as wound healing time, surgical site infection (SSI) rates, wound dehiscence, and postoperative complications. These outcomes are critical indicators of recovery quality and patient safety following major abdominal surgery [18,19]. NPWT has been shown to promote wound healing through mechanisms such as edema reduction, enhanced local perfusion, and stimulation of granulation tissue formation [11]. Furthermore, it may contribute to a lower incidence of SSIs, particularly in high-risk patients or contaminated surgical fields [12]. Evaluating its clinical efficacy relative to conventional wound care is therefore essential to inform evidence-based surgical practice.
Secondary outcomes will include patient-reported pain scores, quality of life measures, length of hospital stay, readmission rates, and healthcare resource utilization. These broader metrics are fundamental for understanding not only the clinical effectiveness of NPWT, but also its impact on patient experience and economic sustainability [20]. Improved wound outcomes may facilitate earlier discharge, reduce the need for reoperation or prolonged antibiotic therapy, and ultimately lower the overall burden on healthcare systems. Given the significant clinical and financial consequences associated with postoperative complications, the systematic use of NPWT may yield substantial cost savings by decreasing resource consumption and improving care efficiency, particularly in high-risk surgical populations.
This systematic review aims to assess whether the clinical benefits of NPWT are accompanied by tangible economic advantages, thereby providing a robust evidence base to support more informed clinical decision-making and health policy development. By synthesizing current evidence, the systematic review will offer guidance for surgeons, wound care specialists, and nursing professionals, particularly in identifying patient populations and surgical contexts in which NPWT provides the greatest benefit—such as obese individuals, contaminated wounds, or high-tension closures [21]. Ultimately, the findings may contribute to the development of standardized, cost-effective postoperative wound management protocols and promote the integration of advanced wound care technologies into routine surgical practice [22].
Implications for clinical practice
The findings generated by this systematic review may provide a foundation for informing future clinical guidelines on postoperative wound care in laparotomy patients. Should NPWT demonstrate significant clinical benefits, such evidence could support its broader adoption in both public and private healthcare settings. In public systems, this may contribute to more efficient resource allocation by reducing complication rates and hospital stay durations. In private care contexts, it could offer cost-effective strategies that enhance patient satisfaction and surgical outcomes. By synthesising available data across various healthcare environments, the systematic review aims to produce insights that are broadly applicable and relevant to multidisciplinary clinical decision-making. Overall, this systematic review aims to generate evidence that is generalisable across diverse healthcare systems, promoting evidence-based, patient-centered surgical care.. Integrating NPWT as a standard wound care strategy could significantly contribute to improving surgical outcomes by accelerating wound healing, reducing the incidence of surgical site infections, and minimizing wound-related complications. These benefits are particularly relevant in high-risk surgical populations, such as those with obesity, diabetes, or immunosuppression, where wound healing is often impaired. Educating healthcare professionals, especially nurses and surgical staff, on the appropriate indications, application techniques, and monitoring of NPWT is essential to ensure its effective implementation. A structured training approach can help improve adherence to evidence-based wound care protocols and promote consistency in clinical practice. In addition, standardized NPWT protocols can support early mobilization, reduce the need for reoperation, and help reduce hospital stays, ultimately decreasing the burden on healthcare systems. From a patient-centered perspective, the use of NPWT can also improve postoperative experience by reducing pain, improving comfort, and promoting a faster return to daily activities. Effective laparotomy wound management through advanced wound care technologies such as NPWT not only promotes physical recovery but can also positively impact psychological well-being and patient satisfaction. Integrating NPWT into routine postoperative care pathways has the potential to optimize resource utilization, improve clinical efficiency, and align surgical wound management with modern quality and safety standards in healthcare delivery. Therefore, this systematic review aims to support evidence-based decision-making and inform the development of targeted guidelines for the management of laparotomy wounds using NPWT. From an economic point of view, NPWT implementation can offer significant cost savings potential despite the initial expense of the device and consumables. Studies have shown that the use of NPWT can lead to a reduction in overall treatment costs by decreasing the incidence of postoperative wound complications, shortening the length of hospital stay, and minimizing the need for additional surgery or prolonged antibiotic therapy. These factors collectively contribute to lower resource utilization, particularly in high-risk surgical populations where complications are more frequent and costly to manage. In addition, by accelerating wound healing and facilitating early discharge, NPWT can help increase bed turnover and improve hospital efficiency, which is especially relevant in resource-constrained healthcare facilities. While the upfront costs of NPWT systems may seem prohibitive, health economics has shown that these are often offset by downstream savings associated with avoided complications and reduced readmission rates. Therefore, integrating NPWT into standard postoperative care protocols can not only improve patient outcomes, but also represent a cost-effective strategy for surgical services that aims to optimize quality while maintaining financial sustainability.
Limitations
This systematic review may encounter several methodological limitations. While no language restrictions are applied during the selection process, allowing for the inclusion of studies published in any language, a potential risk of bias in selection remains if relevant non-English studies are lost due to translation constraints or limited access to full texts. To mitigate this, translation tools and, when necessary, native speakers will be used to ensure accurate interpretation and data extraction. Another limitation concerns the heterogeneity of the studies included. Differences in surgical indications, patient populations, wound classifications, NPWT protocols (e.g., pressure levels, frequency of dressing changes), and control interventions may call into question the feasibility of conducting a meta-analysis and may limit the comparability of results between studies. In addition, variations in reporting and outcome measurement, such as wound healing time, infection rates, or quality of life indicators, could affect the consistency of outcomes. These discrepancies can introduce a degree of variability that complicates the interpretation of the aggregated results. The risk of bias in primary studies is also a potential limitation. While validated critical evaluation tools will be used to assess methodological quality, the inclusion of observational studies, in particular, may lead to evidence that is more susceptible to confusion and bias due to lack of randomization and blinding. Finally, while the systematic review focuses on adult patients undergoing laparotomy, the diversity of surgical and clinical settings may limit the generalizability of findings to other surgical populations or wound types. However, this systematic review aims to provide a rigorous and comprehensive summary of the available evidence on the efficacy of NPWT in the management of laparotomy wounds.
Meta-bias
Potential meta-biases, including publication bias and selective reporting, will be assessed using funnel charts and the Egger test when at least 10 studies are available for a given outcome. To detect selective reporting of results, study protocols or study registries will be compared with published reports, where accessible.
All studies will be evaluated using the ROBINS-E tool, which includes domains that assess deviations from intended interventions and selective reporting, allowing for a structured assessment of reporting bias and its potential impact on systematic review conclusions.
In addition to assessing publication bias through funnel plots and Egger’s test (where applicable), this protocol for a systematic review acknowledges the inherent limitations associated with relying on published literature. Studies with statistically significant or positive findings are more likely to be published, potentially leading to overestimation of effect sizes. To mitigate this, the search strategy includes grey literature sources and trial registries when available. Furthermore, the systematic review team will consider the impact of language and database indexing bias and transparently report any imbalances in study availability across outcomes or settings. These considerations will help contextualize the findings and strengthen the interpretation of the synthesized evidence.
Funding statement
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Conflict of interest
The authors report no conflict of interest.
Authors’ contribution
AM, DFM and CR were the major contributors in writing the manuscript. DCA, VV and AFG performed the data collection and interpreted the patient data. All authors read and approved the final manuscript.
REFERENCES
1. Rajaretnam N, Okoye E, Burns B. Laparotomy. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 [cited 2025 May 22]. Available from: http://www.ncbi.nlm.nih.gov/books/NBK525961/
2. Cleveland Clinic [Internet]. [cited 2025 May 22]. Laparotomy. Available from: https://my.clevelandclinic.org/health/treatments/24767-laparotomy
3. Badia JM, Casey AL, Petrosillo N, Hudson PM, Mitchell SA, Crosby C. Impact of surgical site infection on healthcare costs and patient outcomes: a systematic review in six European countries. J Hosp Infect. 2017 May;96(1):1–15.
4. Anderson DJ, Podgorny K, Berríos-Torres SI, Bratzler DW, Dellinger EP, Greene L, et al. Strategies to prevent surgical site infections in acute care hospitals: 2014 update. Infect Control Hosp Epidemiol. 2014 Jun;35(6):605–27.
5. van Ramshorst GH, Nieuwenhuizen J, Hop WCJ, Arends P, Boom J, Jeekel J, et al. Abdominal wound dehiscence in adults: development and validation of a risk model. World J Surg. 2010 Jan;34(1):20–7.
6. de Lissovoy G, Fraeman K, Hutchins V, Murphy D, Song D, Vaughn BB. Surgical site infection: incidence and impact on hospital utilization and treatment costs. Am J Infect Control. 2009 Jun;37(5):387–97.
7. Argenta LC, Morykwas MJ. Vacuum-assisted closure: a new method for wound control and treatment: clinical experience. Ann Plast Surg. 1997 Jun;38(6):563–76; discussion 577.
8. Wilkes RP, Kilpad DV, Zhao Y, Kazala R, McNulty A. Closed incision management with negative pressure wound therapy (CIM): biomechanics. Surg Innov. 2012 Mar;19(1):67–75.
9. Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015 Jan 1;4(1):1.
10. Shamseer L, Moher D, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. 2015 Jan 2 [cited 2025 Feb 8]; Available from: https://www.bmj.com/content/349/bmj.g7647
11. Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan-a web and mobile app for systematic reviews. Syst Rev. 2016 Dec 5;5(1):210.
12. Mengesha MB, Chekole TT, Abraha HE, Tsegay EW, Atsbaha AH, Gebreslassie M, et al. Feasibility, acceptability, and effectiveness of group antenatal care on the continuum of care and perinatal outcomes in Sub-Saharan Africa: A systematic review and meta-analysis protocol. PLoS One. 2025 Apr 22;20(4):e0311473.
13. Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015 Jan 1;4(1):1.
14. Higgins JPT, Morgan RL, Rooney AA, Taylor KW, Thayer KA, Silva RA, et al. A tool to assess risk of bias in non-randomized follow-up studies of exposure effects (ROBINS-E). Environ Int. 2024 Apr;186:108602.
15. Norman G, Shi C, Goh EL, Murphy EM, Reid A, Chiverton L, et al. Negative pressure wound therapy for surgical wounds healing by primary closure. Cochrane Database Syst Rev. 2022 Apr 26;4(4):CD009261.
16. Banwell PE, Téot L. Topical negative pressure (TNP): the evolution of a novel wound therapy. J Wound Care. 2003 Jan;12(1):22–8.
17. Hyldig N, Vinter CA, Kruse M, Mogensen O, Bille C, Sorensen JA, et al. Prophylactic incisional negative pressure wound therapy reduces the risk of surgical site infection after caesarean section in obese women: a pragmatic randomised clinical trial. BJOG. 2019 Apr;126(5):628–35.
18. Sahebally SM, McKevitt K, Stephens I, Fitzpatrick F, Deasy J, Burke JP, et al. Negative Pressure Wound Therapy for Closed Laparotomy Incisions in General and Colorectal Surgery: A Systematic Review and Meta-analysis. JAMA Surg. 2018 Nov 1;153(11):e183467.
19. Mouës CM, Heule F, Hovius SER. A review of topical negative pressure therapy in wound healing: sufficient evidence? Am J Surg. 2011 Apr;201(4):544–56.
![]() This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
PERCEIVED CAUSES OF CONFLICT AND METHODS OF CONFLICT RESOLUTION AMONG NURSES IN NIGERIAN HOSPITALS
Oseni Rukayat1, Ekpoanwan Esienumoh2, Fakeye Grace 3, Emmanson Emmanson 3*
- Sacred Heart College of Nursing Sciences - Lantoro Abeokuta, Ogun State, Nigeria
- Department of Nursing Sciences, University of Uyo, Akwa Ibom State, Nigeria
- Department of Human Anatomy, University of Cross River State, Nigeria
* Corresponding Author: Emmanson Emmanson, Department of Human Anatomy, University of Cross River University State, Nigeria. E-mail: emmansonemmanson35@gmail.com
Cite this article
ABSTRACT
Introduction: Inherent in every relationship irrespective of number of people involved is the tendency for conflict to occur, either at the intrapersonal, interpersonal, intra-professional or inter-professional level with positive or negative outcome depending on effective resolution of the conflict and the time of resolving it. Conflict has been known to bring about improved relationship, increased cohesiveness, improved communication and productivity when handled and resolved timely. The aims of the study are to identify perceived causes of workplace conflict among nurses and the resolution methods they employ.
Materials and Methods: A cross-sectional research design was used for the study. The sample was 90 nurses on permanent appointment with the hospital drawn using convenient sampling technique. Instruments were validated Rahim Organizational Conflict Inventory (ROCI II) and structured questionnaire on causes of conflicts adapted from Mukeshimana and Asingzwe (2016). Data were analyzed using descriptive statistics of frequencies and percentages and chi-square inferential statistics for causes and resolution methods for conflict at 0.05 level of significance.
Results: The outcome of the study revealed that majority of the respondents are registered nurses and registered midwives only 64 (71.1%), 66 (73.3%) were NO I or NO II; only 8 (8.9%) had Masters or higher education. Injustice (95.6%), unreasonable patient and relative expectation (93.3%), and lack of respect from other health professionals and unequal workload and work schedule (91.1% each) were identified as major causes of workplace conflict. Most prominent method of conflict resolution identified was collaboration (x = 69).
Conclusion: In conclusion, institution should organize training and retraining of nurses regularly, employ more nurses to prevent burnout and job dissatisfaction that can lead to conflict.
Keywords: Collaboration, Workplace conflict, Conflict resolution, Injustice, Nurses
INTRODUCTION
Conflict according to Ronquillo et al. (2023) [11], is the disagreement or difference of opinions between or among individuals which could involve conflicting group or team goals versus individual member’s agendas, insights, or goals which could be potentially harmful to the organization, however, conflict could be positive, promote team-building skills, critical thinking, and bring up new ideas when effectively managed by a competent leader.
Organizational conflict has been known to be an actual or perceived divergent opinion by opposing members of the organization which could involve values, interests, and needs. Opposing members could be individuals on horizontal line of management, or vertical line of management; irrespective of the cause the consequence is usually the same – reduced productivity if the conflict is not resolved early and appropriately (Awan & Saeed, 2015) [3].
Conflict is a part of interpersonal relations and is unfortunately unavoidable and a part of our daily life. For most people, conflict is often threatening and stressful, however conflict can result in the individual or organization discussion of differences that lead to creative solutions, accelerates change in an organization, especially in small businesses, where it is easy to formulate and implement new policies (Ronquillo et al. 2025) [12]. Ronquillo et al. 2025, continued that conflict prompts modification of policies and operation procedures in the organization. In cases of extreme conflict, the organization may conduct a complete overhaul of its leadership, bringing in managers with fresh ideas. According to Awan & Saeed (2015) [3], any threat to the harmony of the organization resulting in conflict sometimes may ultimately impacts negatively on the organization efficiency. Furthermore, where individual and organizational interest conflicts; when people working in an organization cannot maintain a work environment of harmony especially between the manager and subordinate then organizational efficiency, organizational progress cannot be achieved.
According to Oresanjo (2015) [8], conflict is widespread in human societies, meaning that it cannot be ruled out in any human organization, be it schools and colleges, business firms or even social clubs etc. He stated further that conflict is bound to occur because every individual is dependent on other individuals in the organization and once there is interaction, therefore, conflict cannot be ruled out. He maintained that conflict is seen as both disruptive force within an organization and primary source of individual stress. However, it is not entirely destructive. The goal of an organization should be how to control conflict in order not to degenerate into crisis rather than eliminating it.
Every organization is faced with one conflict or the other at a point in the organizational cycle especially when members of the organization perceived or believed that their interest or goal may be jeopardized and not achieved as the organization is progressing. According to Smiley (2010) [13]; Adeyemi and Aigbavboa (2022) [1], managing conflict or conflict resolution is one of the paramount skills that managers must be trained on and must be maintained to ensure organizational efficiency.
Most of the time organizational conflict occur as a result of unhealthy working environment, poor management with some staff being overloaded with work and some other staff are viewed as being redundant this may be consequent to poor organization structure or restructuring; unfair treatment which may be perceived or actual; there may be no clear-cut definition of job roles or job specification. The major causes being poor communication among members of the organization; favouritism with some being promoted while others are not promoted, jealousy and struggle for power have also been identified by different researchers as causes of conflict.
Workplace violence experienced by healthcare teams especially nurse seems to be due to lack of satisfying conflict resolution or when patient and their relations feel their needs are not being met. This problem has been reported repeatedly in most hospitals in Nigeria (Ogbonnaya et al., 2023) [6] same was experienced recently in Sacred Heart Hospital, Lantoro. The need for effective conflict resolution by nurses to prevent escalation of conflict prompted the interest for this study. From literature reviewed by the researcher it was discovered that there is paucity of research work conducted on causes of conflict and the methods of conflict resolution among nurses, between the nurse and other health care professionals; nurses and patient and/or patient’s relations.
This research assessed the causes of workplace conflict among nurses in Sacred Heart Hospital, Lantoro, Abeokuta, Ogun state and methods of conflict resolutions utilized by them.
MATERIALS AND METHODS
Study Population
This was a descriptive cross-sectional study conducted among clinical nurses at Sacred Heart Hospital, Lantoro, Nigeria, between September 2021 and August 2022, with final data analysis completed by December 2022.
The study targeted registered nurses currently working in the hospital across different clinical departments and nursing cadres. Nurses were selected from inpatient and outpatient units based on their availability and consent to participate.
The study protocol matched the Declaration of Helsinki ethical guidelines for clinical studies, and it was approved by the Technical Scientific Committee of Sacred Heart Hospital, Lantoro, with approval letter dated September 15, 2021, ref: SHH/EC/EA/05/09/21. All participants were informed and signed their informed consent.
Inclusion criteria
- Registered nurses licensed by the Nursing and Midwifery Council of Nigeria
- Minimum of 2 years of clinical experience
- Willingness to give informed consent and participate voluntarily
Exclusion criteria
- Nurses on annual leave, sick leave, or study leave during the study period
- Nurses who declined to provide informed consent.
Instrument
This study utilized a common instrument—the Rahim Organizational Conflict Inventory–II (ROCI–II) created by Rahim (1983)—to assess conflict management styles among nurses. Specifically, Forms A, B, and C of the ROCI-II with 28 items each were used to assess conflict resolution styles when dealing with supervisors (Form A), subordinates (Form B), and peers (Form C). The instrument assesses five conflict management styles: Integrating (Collaborating), Obliging (Accommodating), Dominating (Competing), Avoiding, and Compromising.
All of the items on the ROCI-II are measured on a 5-point Likert scale, from 1 = Strongly Disagree to 5 = Strongly Agree. The 28 items on each of the two forms are arrayed into five subscales that correspond to the five conflict resolution styles. The item classification into each style is as follows:
1) Integrating (Collaborating) – 7 items, 2) Obliging (Accommodating) – 6 items, 3) Dominating (Competing) – 5 items, 4) Avoiding – 6 items, 5) Compromising – 4 items.
In addition, an adapted version of the Causes of Conflict Questionnaire by Mukeshimana and Asingzwe (2016) [5] was employed to assess potential causes of conflict in the workplace. The adapted instrument included structured items designed to bring out nurses' views of interpersonal, organizational, and communication-related causes of conflict. The items also received scores on a 5-point Likert scale ranging from 1 = Strongly Disagree to 5 = Strongly Agree. To ensure content validity, the instruments were reviewed by nursing science and educational measurement and evaluation specialists. They checked the items for consistency, relevance, and clarity with the initial instruments. Minor modifications were effected to improve the appropriateness and readability of the questionnaire items to the study environment from their inputs. The final instrument retained the fundamental constructs and design of the initial instruments.
Statistical Analysis
Data obtained were analyzed based on objectives and hypotheses. Socio-demographic data was analyzed using descriptive statistics and presented on a percentage and frequency table.
The non-parametric Friedman test was used for testing the differences between three or more dependent variables. If the Friedman test was positive (P<0.05), the post hoc Wilcoxon signed-rank test was used for pairwise comparison. The chi-square test or Fisher's exact test were performed to assess significant differences in proportions or percentages between two independent variables. Fisher's exact test was used when the chi-square test was found to be inappropriate. Causes and Methods of conflict were analyzed using SPSS version 20 and presented with tables. All the hypotheses were tested with a significance level of 0.05.
RESULTS
Ninety-six copies of the questionnaire were distributed to sample selected for the study but only 90 copies (93.8%) of returned questionnaire were completely filled and met the criteria for analysis. Therefore, 90 copies of the questionnaire were analyzed.
| Characteristics | % (n) |
| Gender | |
| Female | 95.6% (86) |
| Male | 4.4% (4) |
| Religion | |
| Christian | 93.3% (84) |
| Islam | 6.7% (6) |
| Marital status | |
| Single | 51.1% (46) |
| Married | 42.2% (38) |
| Divorced | 4.4% (4) |
| Widow | 2.2% (2) |
| Level of education | |
| RN/RM | 71.1% (64) |
| BNSc | 20.0% (18) |
| ≥MSc | 8.9% (8) |
| Cadre | |
| NO I – NO II | 73.3% (66) |
| SNO - PNO | 11.1% (10) |
| ACNO - ADN | 15.6% (14) |
| Grade level | |
| Below 13 | 73.3% (66) |
| 13 - 15 | 22.2% (20) |
| 16 and above | 4.4% (4) |
Table 1. General characteristics of the sample.
Table 1 shows that more female nurses 86 (95.6%) than male nurses 4 (4.4%) participated in the study. A majority of the respondents are Christians 84 (93.3%). About half of the respondents are single 46 (51.1%), while widows are 2 (2.2%). A majority of the respondents are RN/RM only 64 (71.1%); only 8 (8.9%) had Master’s or higher education. For the cadre, more than half 66 (73.3%) are NO I or NO II. Similarly, 66 (73.3%) are below grade level 13, followed by those on grade level 13 – 15 with 20 (22.2%).
| Causes | Agree % (n) | Disagree % (n) |
| Distrust | 88.9% (80) | 11.1% (10) |
| Refusal to take orders from doctor | 64.4% (58) | 35.6% (32) |
| Doctors consider themselves as superior | 80.0% (72) | 20.0% (18) |
| Lack of respect from other health professionals | 91.1% (82) | 8.9% (8) |
| Different level of education | 77.8% (70) | 22.2% (20) |
| Conflict of interest and absence of procedure and strategies | 80.0% (72) | 20.0% (18) |
| Lack of respect and lack of attention to patient | 71.1% (64) | 28.9% (26) |
| Being insulted by the doctor before patient | 82.2% (74) | 17.8% (16) |
| Order from a doctor which is out of the scope of my practice | 75.6% (68) | 24.4% (22) |
| Delay of the doctor to answer my call in emergency case | 88.9% (80) | 11.1% (10) |
| Injustice from some nurse managers | 95.6% (86) | 4.4% (4) |
| Favouritism | 86.7% (78) | 13.3% (12) |
| Unequal workload and work schedule | 91.1% (82) | 8.9% (8) |
| Unreasonable patient and relative expectation | 93.3% (84) | 6.7% (6) |
| Imbalance nurse-patient ratio | 88.9% (80) | 11.1% (10) |
Table 2. Distribution of Respondent on Causes of Conflict (N = 90)
Table 2 shows that all the items identified constitute strong causes of conflict ranging between 58 (64.0%) and 86 (95.6%) out of 90, with refusal to take orders from doctors being the least count 58 (64.0%) while 86 (95.6%) of the respondents supported injustice from some nurse managers as the major cause of conflict in the hospital, followed by unreasonable patient and relative expectation (93.3%), unequal workload and lack of respect from other health professionals (91.1% each). Delay of the doctor to calls in emergency cases, imbalance nurse-patient ratio, and distrust were also significant causes of conflict with 88.9% respectively.
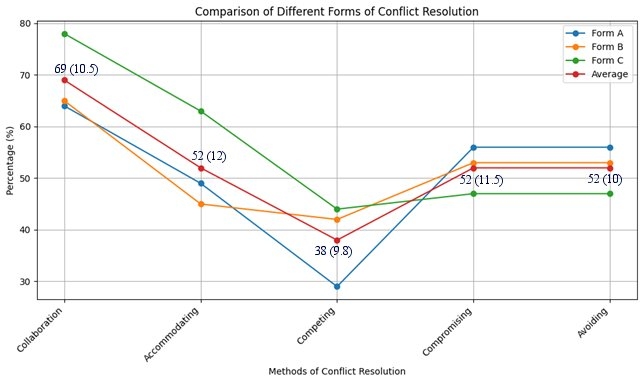
Figure 1: Percentage distribution of responses to method of conflict resolution utilized by nurses (N = 90). The figure shows the mean percentage values and the standard deviations in brackets.
The figure above shows positive response to various methods of conflict resolution in the hospital. Form A depicts conflict resolution with subordinates, Form B depicts conflict resolution among colleagues, Form C depicts method of conflict resolution among superior. Average of the responses shows the overall average performance across board or of the three forms. It can be observed that most of the respondents discouraged the use of competing resolution with an average score of 38% while they supported the use of collaboration with an average score 69%. Accommodating, compromising and avoiding have equal percentages (average 52.0% each). Therefore, it can be deduced that majority of nurses utilize collaboration in conflict resolution (69.0%) while few nurses use competing (38.0%) in resolving conflict in Sacred Heart Hospital, Lantoro, Abeokuta.
Statistical analysis using the Friedman test (χ² = 92.15, df = 4, p < 0.001) confirmed a significant difference in method preference. Post hoc Wilcoxon signed-rank tests (Holm-corrected) showed that collaboration (median: 69.0) was significantly more used than competing (median: 38.0, p < 0.001), accommodating (median: 52.0, p = 0.003), and avoiding (median: 52.0, p = 0.005). Competing was also significantly less used than accommodating (median: 52.0, p = 0.007).
Table 3 presents a cross-tabulation of the respondents’ preferred methods for conflict resolution in relation to their demographic and professional characteristics, including gender, cadre, and level of education. This descriptive overview highlights distribution patterns across the five conflict resolution styles.
| Characteristics | Accommodating | Avoiding | Collaborating | Competing | Compromising | Total |
| Gender | ||||||
| Male (n=4) | – | – | 4 (100.0%) | – | – | 100.0% |
| Female (n=86) | 6 (7.1%) | 20 (23.8%) | 37 (42.9%) | 4 (4.8%) | 18 (21.4%) | 100.0% |
| Cadre | ||||||
| NO II (n=24) | 1 (4.2%) | 4 (16.7%) | 13 (54.2%) | 1 (4.2%) | 5 (20.8%) | 100.0% |
| NO I (n=9) | 1 (11.1%) | 2 (22.2%) | 3 (33.3%) | – | 3 (33.3%) | 100.0% |
| SNO (n=2) | – | 1 (50.0%) | 1 (50.0%) | – | – | 100.0% |
| PNO (n=1) | – | – | 1 (100.0%) | – | – | 100.0% |
| ACNO (n=1) | – | – | – | 1 (100.0%) | – | 100.0% |
| CNO (n=1) | – | – | 1 (100.0%) | – | – | 100.0% |
| ADN (n=5) | – | 3 (60.0%) | 1 (20.0%) | – | 1 (20.0%) | 100.0% |
| Level of Education | ||||||
| Diploma (n=54) | 2 (3.7%) | 8 (14.8%) | 32 (59.3%) | 2 (3.7%) | 10 (18.5%) | 100.0% |
| B.Sc. (n=12) | 2 (16.7%) | 3 (25.0%) | 3 (25.0%) | 1 (8.3%) | 3 (25.0%) | 100.0% |
| M.Sc. (n=8) | – | 8 (100.0%) | – | – | – | 100.0% |
| Others (n=4) | – | 1 (25.0%) | 2 (50.0%) | – | 1 (25.0%) | 100.0% |
Table 3. Cross tabulation of association of respondent’s characteristics and their method of conflict resolution (N = 90).
Table 4 summarizes the results of statistical analyses used to examine the association between respondents’ characteristics and their chosen method for conflict resolution. Chi-square tests, likelihood ratios, and Fisher-Freeman-Halton exact tests were applied to assess significance.
The analysis showed that there is no significant association between gender and method of conflict resolution used by nurses. The Fisher’s exact test was also carried out because 60% of the expected cell frequencies were below 5, with a minimum expected count of 0.18 which violates the chi square assumption. The p-value (0.453) was greater than the significant level (0.05). Hence, there is no evidence to reject the null hypothesis.
| Gender | Value | df | Asymptotic Sig. (2-sided) | Exact Sig. (2-sided) |
| Pearson Chi-Square | 5.029a | 4 | 0.284 | 0.310 |
| Likelihood Ratio | 6.537 | 4 | 0.162 | 0.176 |
| Fisher-Freeman-Halton Exact Test | 3.402 | 0.453 | ||
| N of Valid Cases | 88 | |||
| Cadre | ||||
| Pearson Chi-Square | 62.306a | 24 | 0.0 | |
| Likelihood Ratio | 35.889 | 24 | 0.056 | 0.02* |
| Fisher-Freeman-Halton Exact Test | 31.533 | 0.049* | ||
| N of Valid Cases | 86 | |||
| Education | ||||
| Pearson Chi-Square | 19.407a | 12 | 0.079 | 0.090 |
| Likelihood Ratio | 18.398 | 12 | 0.104 | 0.097 |
| Fisher-Freeman-Halton Exact Test | 17.089 | 0.073 | ||
| N of Valid Cases | 88 | |||
| * = significant test | * = significant test | * = significant test | * = significant test | * = significant test |
Table 4. Analysis of the association between several variables and method of conflict resolution.
The analysis also showed that there is a significant association between cadre and method of conflict resolution used by nurses. The Fisher’s exact test was carried out because 88.6% of the expected cell frequencies were below 5, with a minimum expected count of 0.09 which violates the chi square assumption. The p-value (0.049) was lower than the significant level (0.05). Hence, the null hypothesis is rejected, and the conclusion is that there is an association between cadre and the conflict resolution.
The level of education was also tested with the style of conflict resolution used by nurses. The Fisher’s exact test was used instead of the chi-square test because 80% of the expected cell frequencies were below 5, with a minimum expected frequency of 0.09 which violates the chi-square assumption. The p-value (0.073) was greater than the significant level (0.05). Hence, there is no evidence to reject the null hypothesis.
DISCUSSION
The perceived factors causing conflict experienced by nurses include injustice from some nurse managers (95.6%) being the major cause of conflict, unreasonable patient and relative expectation (93.3%), unequal workload and lack of respect from other health professionals (91.1% each). Delay of the doctor to calls in emergency cases, imbalance nurse-patient ratio, and distrust (88.9% each), this was supported by Pitsillidou, et al. (2018) [9] findings among health professionals in hospitals of Cyprus to record the types of conflict management that health professionals in Cyprus hospitals encounter in their daily work and to explore the conflicts, their parameters and causes, and the role ambiguity faced by hospital employees. It was discovered that health professionals identified heavy workload, low pay, and varying instructions from different leaders as causes of conflict. In addition, the findings of a study by Olajide et al. (2015) [7] on conflict among nurses and doctors in 2 tertiary hospitals in Ekiti State indicated that odds of conflicts were significantly higher with limited opportunities for staff interaction (OR=1.8, CI=1.1-2.9); desire for power (autonomy) by doctors (OR=3.2, CI=1.9-5.2) and desire for more influence by nurses (OR=12.5, CI=4.8-41.3). Chances of expressing conflicts were significantly higher as strikes (OR=2.1; 1.3-3.5) but less with physical assaults (OR=0.1, CI=0.03-0.41). This is also, supported by Akpabio et al. (2015) [2] research finding which showed that un-resolved conflicts may be linked to poor communication resulting from refusal to cooperate, poor team collaboration and problem-solving, decreased clients’ satisfaction, distrust, split camps, gossips and disruption of work-flow, overwork and poor rewarding system each with frequency of 222 (92.0%); patients-related conflict and leadership conflicts each with frequency of 218 (90.0%); misunderstanding involving nursing colleagues with a frequency of 194 (81.0%); poor work environment 192 (80.0%); conflicts with other health professionals with 189 (78.0%) frequency and discrimination issues with 180 (61.0%) frequency.
Methods of conflict resolution include collaboration, accommodation, and compromising. The study revealed that more than half of the nurses utilized collaboration (69.0%), accommodating, compromising and avoiding (52.0% respectively) and only a few used competitions as a method of conflict resolution. A Friedman test revealed a significant difference in utilizing these conflict resolution methods (χ² = 92.15, df = 4, p < 0.001). Post hoc Wilcoxon signed-rank tests with Holm-Bonferroni correction showed that collaboration was significantly more utilized than competing (p < 0.001), meaning that nurses certainly utilize collaborative styles more than confrontational styles. This is in contrast with the results of Pitsillidou, et al. (2018) [9], that respondents utilized avoidance (73.2%) over negotiation for mutual benefit (54.2%), and compromise (40.5%) as conflict management mechanisms, as compared with the results of Adeyemi and Aigbavboa (2022) [1], that collaboration, accommodating, negotiating, compromising, and mediating were the most common conflict resolution styles utilized by Southwest Nigerian construction professionals. In addition, collaboration was employed significantly more than accommodating (p = 0.003) and avoiding (p = 0.005). These findings validate the perspective that nurses regard collaborative approaches as not only professionally appropriate but also more effective in resolving intricate interpersonal and hierarchical disputes within the clinical setting. Collaboration enhances mutual respect and problem-solving, which are essential values in nursing practice. The findings mirror Adeyemi and Aigbavboa's (2022) [1] results, which also indicated extremely high reliance on cooperation as a conflict resolution style.
Competing was utilized significantly less than accommodating (p = 0.007), demonstrating that aggressive or assertive styles are actively avoided or rejected by nurses. This aligns with the philosophy of caregiving in nursing, which promotes empathy and de-escalation. While some degree of assertiveness may be required in critical care practice, the overall avoidance of competitive conflict resolution suggests a strong professional culture that prioritizes harmony over hierarchy.
Surprisingly, no difference was detected in the use of accommodating, compromising, and avoiding styles (p > 0.05). This can reflect the pragmatic interchangeability of these styles on a day-to-day basis, especially if nurses attempt to minimize friction but not necessarily the source. This passivity or neutrality can be a coping strategy in environments where power imbalances are prevalent, or where organizational constraints reduce formal conflict resolution mechanisms.
There is no relationship between gender and level of education, and conflict resolution style used by nurses, except cadre which influenced conflict resolution approach. This suggests that positional status in an organization plays a role in managing conflict, perhaps due to variations in authority, confidence, and experience. This finding is against Birkhoff's (2015) [4] that gender significantly influences conflict dynamics at the individual and societal levels. In order to understand the role of gender in conflict comprehensively, it is important to examine it through individual, interpersonal, and societal levels. Gender may manifest itself in conflicts through how parties interpret and make sense of the conflict. Birkhoff also presented the findings of Gwartney-Gibbs to support his findings that gender also had an effect on dispute handling mechanisms. Conflict resolution processes for women were not as effective as those of men. For example, women would avoid more than resolving the conflict. However, the current findings show that within professional clinical environments such as Sacred Heart Hospital, formalized positions and codes of conduct can counteract the influences of gender and educational level and bring about similar conflict resolution styles across demographic groups. This highlights the importance of looking more closely at contextual and institutional determinants of conflict behaviour in healthcare organizations, particularly the influence of leadership structure and support systems on employee behaviour.
Implications for practice and future research
The findings have practical implications for policymakers and healthcare administrators. Since the most common approach to resolving conflict was collaboration, institutions should promote team-based training and workshops on collaborative communication improvement, leadership, and emotional intelligence among nurses. Resolving the main causes of conflict e.g., injustice by nurse managers, expectations of patients, and workload disparities can increase job satisfaction, collaboration, and overall patient care quality.
Future studies should seek to conduct multi-centre studies with larger populations of studies in different geopolitical settings of Nigeria for maximum generalizability. Longitudinal studies may also be helpful in identifying changes in conflict resolution patterns over time. Qualitative studies exploring nurses' lived experiences of workplace conflict can also help in understanding factors involved and aid in devising context-specific interventions.
CONCLUSION
The study concludes that the major factors causing conflict among nurses are injustice from some nurse managers, unreasonable patient and relative expectation, unequal workload and lack of respect from other health professionals, delay of the doctor to calls in emergency cases, imbalance nurse-patient ratio, and distrust. Collaboration was discovered to be the main method of conflict resolution utilized by nurses in Sacred Heart Hospital, Lantoro, irrespective of their socio-demographic status of gender and level of education. However, cadre of the nurses influenced method of conflict resolution used.
Limitations
This study was limited to a single hospital, which may affect the generalizability of the findings. The sample size was relatively small, and data collection relied on self-reported responses, which may introduce bias. Future studies should include larger, multi-centre samples for broader applicability.
Funding statement
This research did not receive any specific grant from funding agencies in the public, commercial, or not for profit sectors.
Conflict of interest
The authors report no conflict of interest.
Authors’ contribution
- Oseni Rukayat: Conceptualized idea and conducted full research.
- Ekpoanwan Esienumoh: assisted with the design of questionnaire and conducting interviews with the selected nurses.
- Fakeye Grace: Was responsible for literature reviews
- Emmanson Emmanson: performed data analysis and edited the manuscript for publication.
Acknowledgements
We sincerely appreciate the management and nursing staff of Sacred Heart Hospital, Lantoro, for their support. Special thanks to our academic institutions, mentors, and colleagues for their guidance. We also acknowledge our families and friends for their unwavering encouragement throughout this research. Thank youall.
REFERENCES
- Adeyemi, B. S. and Aigbavboa, C. O. (2022). An Exploratory Factor Analysis for Conflict Resolution Methods among Construction Professionals. MDPI. Vol. 12(6). .
- Akpabio I. I., John M. E., Akpan M. I., Akpabio F. A. and Uyanah D. A. (2015). Work-related Conflict and Nurses’ role performance in a tertiary hospital in South-south Nigeria. Journal of Nursing Education and Practice, 6(2). . Accessed 27/10/2022.
- Awan, A. R. and Saeed S. (2015). Conflict Management and Organizational Performance: A case Study of Askari Bank Ltd. Research Journal of Finance and Accounting, 6(11), . Accessed 24/04/2022.
- Birkhoff J. (2015). Gender, Conflict and Conflict Resolution. . Accessed 17/10/2022
- Mukeshimana M. and Asingzwe D. (2016). Nurse-Doctor Relationship in Rwanda: A Questionnaire Survey. IOSR Journal of Nursing and Health Science.. Accessed 12/09/2022.
- Ogbonnaya, G. U., Ukaegbu, A. U., Aguwa, E., and Emma-Ukaegbu, U. A study on workplace violence against health workers in a Nigerian tertiary hospital. . Accessed 22/01/2023.
- Olajide, A. T., Asuzu M.C, and Obembe T.A. (2015). Doctor-Nurse Conflict in Njgerian Hospitals: Causes and Modes of expression. Journal of Advances in Medicine and Medical Research. VOL. 9(10). . Accessed 04/06/2021.
- Oresanjo, N. O. (2015). Conflict Management in School Organization in Nigeria. International Journal of Development and Management Review. V10(1). https://www.ajol.info>ijdmr>article>view.pdf. Accessed 17/10/2021.
- Pitsillidou, M. , Farmakas, A., Noula, M., and Roupa, Z. (2018). Conflict Management among health Professionals in hospitals in Cyprus. Journal of Nursing Management, 26(3-4). . Accessed on 24/04/2022.
- Rahim, M. A. (1983). Measurement of Organizational Conflict. The Journal of General Psychology, 109(2), 189-199.
- Ronquillo, Y. , Ellis, V. L, &Toney-Butler, T. J. (2023). Conflict Management. National Library of Medicine. ncbi.nlm.nih.gov/books/NBK4704321/
- Ronquillo, Y. , Ellis, V. L., &Toney-Butler, T. J. (2025). Conflict Management. In StatPearls. StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK470432/
- Smiley, F. (2010). Leadership Guide to Conflict and Conflict Management. . Accessed 24/04/2022.
![]() This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Articolo formattato
Federico D’Urso 1*, Salvatore Trifiletti 2, Edoardo Falcone 1, Mara Gracy Basile 1, Ulrico Angeloni 1
1. Public Health Unit, Italian Red Cross – National Headquarters, 00151, Rome, Italy
2. Department of Medical, Surgical Sciences and Advanced Technologies “G. F. Ingrassia”, University of Catania, 95125, Catania, Italy.
* Corresponding author: Federico D’Urso, Public Health Unit, Italian Red Cross – National Headquarters, 00151, Rome, Italy. E-mail: federico.durso@gmail.com
Cite this article
ABSTRACT
Introduction: Biocontainment transfer represents a complex and delicate phase of care, especially in light of the increased demand for safe handling of patients affected by highly transmissible diseases. The COVID-19 pandemic has highlighted the critical need for structured approaches to ensure quality care and safety during these transfers.
Objective: To propose a structured nursing model for managing the care of conscious and communicative patients undergoing biocontainment transport, based on nursing diagnoses and standardized interventions.
Methods: A theoretical-conceptual model was developed based on the NANDA-I 2024–2026 taxonomy to identify nursing diagnoses related to perception, cognition, and stress tolerance. These were systematically combined with appropriate interventions from the Nursing Interventions Classification (NIC) and expected outcomes from the Nursing Outcomes Classification (NOC). The model addresses the clinical and psychological needs of patient across the three phases of transport: pre-transport, transport, and post-transport, with particular focus on anxiety management, communication, and adaptation to isolation.
Results: In the pre-transport phase, the diagnosis of Excessive Anxiety was addressed with interventions to reduce emotional distress and improve patient cooperation through clear, empathetic communication. During transport, the impairment of verbal communication caused by protective equipment and isolation barriers was mitigated through simplified language, visual aids, and strategies to ensure mutual understanding. In the post-transport phase, the model focused on enhancing the patient's coping capacity and resilience, offering emotional support and structured interventions to manage stress and process the experience.
Conclusions: The proposed model provides a comprehensive and systematic framework for nursing care during biocontainment transfers, integrating both clinical and emotional aspects to reduce patient vulnerability and improve the quality of care. As a theoretical model built upon standardized nursing taxonomies, it lays the groundwork for future clinical applications. Prospective and pilot studies will be essential to validate its effectiveness and feasibility in real-world healthcare settings.
Keywords: Biocontainment, Biocontainment patient transport, Nursing process, Clinical complexity, Advanced nursing practice.
INTRODUCTION
The current healthcare landscape has changed radically compared to a few years ago; the COVID-19 pandemic has highlighted structural and staffing shortages on a global scale [1,2]. The increase in the number of patients affected by highly transmissible diseases requiring high-intensity care has led to the widespread introduction of isolation devices that were once reserved for extremely rare situations. Biocontainment isolators have proven to be essential in the transport of these patients and typically include a protective plastic enclosure, a High Efficiency Particulate Air (HEPA) filter that removes harmful airborne particles, and a ventilation system that maintains a clean airflow at controlled pressure, preventing the escape of pathogens [2].
In the presence of diseases characterized by a high risk of mortality or a lack of appropriate preventive measures and effective treatments, the use of isolators becomes essential to ensure maximum safety for both the patient and healthcare personnel [1,3,4].
Preparing and managing the patient for a biocontainment transfer represents one of the most complex challenges for healthcare personnel, requiring protocols and technologies to guarantee both staff protection and the quality of patient care [2].
The use of biocontainment isolators can be compared to a form of physical restraint, as they impose an isolation measure that limits the patient's interaction with the external environment [5].
Although biocontainment isolators are essential for the safe transport of patients, their implementation presents significant logistical and organizational challenges that must be addressed [1,2].
Several studies have addressed the logistical and clinical challenges associated with the transport of patients in high-level containment. Gibbs et al. (2019) provide a comprehensive review of air medical evacuation protocols for biocontainment transport, focusing on technical and operational safety measures [1]. Similarly, Corradi et al. (2021) assess the public health implications of biocontainment systems used in ambulances, while D’Urso et al. (2024) describe possible care protocols for patients transferred using a biocontainment stretcher [2,6]. However, these contributions primarily emphasize technical configurations and infection control, without proposing a structured model of nursing care.
Studies investigating patient management within dedicated biocontainment units (e.g., Flinn et al., 2021) and during pandemic conditions Rehn et al., 2023 have highlighted the complexity of delivering safe care in isolation, yet they stop short of defining a standardized nursing process [3,7]. Other investigations have explored the communicative and emotional needs of patients in constrained settings. For example, the impact of personal protective equipment (PPE) on communication is well documented (Aengst et al., 2022; Saunders et al., 2021), and the relevance of augmentative and alternative communication (AAC) strategies in ICUs has been addressed by Costello (2000) and Zaylskie et al. (2024) [5,8-10]. Ten Hoorn et al. (2016) offer a systematic review on communication with mechanically ventilated patients, further supporting the need for dedicated relational strategies in high-complexity care [11].
While these studies help define the relational and contextual challenges of care in isolation, they do not translate into a structured, taxonomy-based model. Beam et al. (2010) and Swickard et al. (2014), for example, offer insights into the organization of biocontainment units and interfacility critical care transport, but without applying NANDA-I, NIC, or NOC frameworks [12,13].
This overview of the current literature confirms the absence of validated nursing care models specifically designed for conscious and communicative patients undergoing biocontainment transfers, thereby justifying the development of a structured approach grounded in standardized nursing taxonomies.
To fill this gap and address these challenges, the development of a structured nursing care model, based on targeted nursing diagnoses, is essential to guide clinical practice. Such a model can improve patient safety, enhance the quality of communication, and ensure continuity of care throughout the different phases biocontainment transfer process [6,7].
Objective and purpose
The aim of this study is to develop and propose an innovative structured nursing model designed to address both the clinical and psychological needs of conscious and communicative patients undergoing biocontainment transport. The model integrates standardized nursing diagnoses, interventions, and outcomes to enhance communication, reduce anxiety, and improve overall patient care across all phases of transport, laying the foundation for future clinical validation.
DEVELOPMENT OF THE CARE MODEL
Sampling and Eligibility
This study consists of a theoretical and methodological proposal for a structured care model for conscious and communicative patients without the actual collection of clinical data.
The model is designed for future applications in clinical practice and is intended to be validated in prospective studies involving real patients and healthcare teams.
Instruments
The care model is based on the integration of nursing diagnoses (NDs) from the NANDA-I 2024–2026 taxonomy and integrates elements from the NIC (Nursing Interventions Classification) and NOC (Nursing Outcomes Classification) systems. The selection of nursing diagnoses, interventions, and outcomes was informed by a narrative review of literature related to care in isolation, high-risk transport, and psychological support in confined environments. Due to the absence of specific scientific studies on biocontainment transfers, references from similar contexts were used. The process was further refined through structured consensus among the authors, all of whom have experience in emergency nursing and biocontainment patient management. To correctly select the appropriate NDs, an in-depth analysis was conducted of all thirteen domains included in the NANDA-I 2024–2026 classification. Some domains were excluded from consideration for the biocontainment transfer of conscious and communicative patients, as they were not relevant to the specific context. Domain 1 (Health Promotion) was excluded due to its focus on long-term behavioral patterns, domains 2 (Nutrition) and 3 (Elimination and Exchange) were not considered since they are not typically involved in short-term transfers and are managed in longer-duration ones. Domain 4 (Activity/Rest) was excluded because of its limited relevance during transport. Domains 6 (Self-Perception), 7 (Role Relationships), 8 (Sexuality) and 10 (Life Principles) were deemed not pertinent to biocontainment transfer. Furthermore, the domains 12 (Comfort) and 13 (Growth/Development) were excluded because they are not central in urgent care situations.
Domain 11 (Safety/Protection), although potentially relevant from a clinical standpoint, was excluded because it primarily focuses on physical risks such as infections or trauma. The typical patient considered is already in a similar condition; however, the main goal of the proposed model is instead to enhance the communicative, relational, and emotional dimensions of care through structured nursing interventions. Given these factors, the analysis focused on two specific domains the domain 5, (Perception/Cognition) with particular attention to cognitive understanding and communication and domain 9 (Coping/Stress Tolerance), which addresses psychological and emotional reactions. Within domain 5, only class 5 (Communication) was retained, as it includes diagnoses that are directly applicable to the needs of conscious patients experiencing communication difficulties due to the constraints of the biocontainment context, including the use of PPE. The other classes within this domain class 1 (Attention), 2 (Orientation) and 3 (Sensation/Perception), were excluded as they currently contain no NDs. Class 4 (Cognition) was also excluded, as it refers to cognitive deficits that require specific clinical and pharmacological management. In the case of a disoriented patient placed in a biocontainment isolator, such a condition would likely be exacerbated by the restrictive environment, making sedation the most appropriate and safe option for transport. Regarding domain 9, only class 2 (Emotional Responses) was included, as it encompasses diagnoses such as anxiety, ineffective coping, and stress responses, which are frequently observed in patients subjected to restrictive isolation. The remaining classes, 1 (Post-Trauma Responses) and 3 (Impulse Control), were excluded. In particular, class 1 was deliberately not considered, as the aim of the proposed model is to prevent the onset of post-traumatic stress symptoms related to the biocontainment transfer, by supporting the patient through structured interventions that reduce emotional overload and promote coping during the procedure. Based on this taxonomic analysis, the nursing care model was structured into three distinct phases, pre-transport, transport, and post-transport, each associated with specific nursing diagnoses, related interventions, and expected outcomes.
Pre-transport phase
The lack of knowledge about the biocontainment stretcher and the procedures to be carried out during the transfer generates, at this stage, significant emotional distress and anticipatory anxiety. The nursing diagnosis excessive anxiety (00400), classified under domain 9, class 2, was selected based on observations conducted in clinical practice, where behavioral and physiological signs such as agitation, increased heart rate, and verbal expressions of concern are commonly noted.
Other diagnoses within the same class, such as fear (00390) or impaired resilience (00210), were excluded because they involve long-term patterns or cannot be adequately documented within the limited timeframe of the transfer.
To address this diagnosis, the NIC interventions anxiety reduction (5820) and emotional support (5270) were selected, with the expected NOC outcome being anxiety Self-Control (1402). [14]
Since the goal of this care model is to promote coping, we preferred to use the NOC Anxiety Self-Control (1402), as it reflects the objective of enhancing the patient’s conscious management of anxiety.
The NOC Anxiety Level (1211) may be useful for an initial clinical assessment or for pre-post comparisons, but its purpose would remain limited to quantifying the symptom.
In this phase, it may be useful to conduct an initial assessment of the patient's anxiety level, followed by a second evaluation to measure the effectiveness of interventions, using a rapid-assessment tool such as the Generalized Anxiety Disorder-7 (GAD-7) scale [15,16].
Transport phase
The use of the biocontainment stretcher and PPE generates significant communication barriers between patients and healthcare professionals. Within domain 5, class 5 of the NANDA-I taxonomy, the diagnosis Readiness for Enhanced Communication (00185) was excluded, as it is focused on strengthening a communicative process that is already functioning. In this context, however, it is necessary to implement an alternative communication system to replace the traditional one, which is compromised by operational conditions.
Similarly, the diagnosis Risk for Impaired Verbal Communication (00434) was excluded because it refers to a susceptibility to communication impairment, whereas in the current scenario the impairment is already present.
The most consistent was found to be DN Impaired Verbal Communication (00051), which characterizes a limited or nonexistent capacity for verbal communication. [9,10]
The selected nursing interventions are Communication Enhancement: Speech Deficit (4976) chosen to facilitate effective information exchange through alternative communicative methods during the transport phase.
Communication (0902), the related NOC, enables the assessment of the efficacy of the patient-provider relationship in situations where communication is constrained.
Post-transport phase
In this phase, the patient faces the need for emotional recovery and coping support following the biocontainment transfer, the DNs Readiness for Enhanced Coping (00158), classified under domain 9, class 2, was selected, as it reflects the patient’s willingness and potential to strengthen adaptive strategies in response to an acute stress situation [14,16].
This choice is based on the authors’ clinical observations in most cases; conscious and cooperative patients exhibit transient emotional discomfort that can be interpreted as a normal physiological response to stress rather than a failure of their coping abilities. Consequently, diagnoses such as Ineffective Coping (00069) were excluded, as they would imply a dysfunction in stress management and risk labeling a temporary and reactive experience as a psychological disorder.
The care objective is not the treatment of a psychological condition, but rather the enhancement of the patient’s existing personal resources by fostering resilience and facilitating the emotional processing of the experience through structured interventions.
In line with this approach, several standardized nursing interventions (NIC) were selected to support the patient’s adaptation and increase their stress management capacity. Among them, Coping Enhancement (5230) represents the core intervention aimed at promoting an adaptive response to the experience.
These are supported by Emotional Support (5270) which is essential for normalizing emotional reactions, containing residual anxiety, and facilitating emotional rebalancing.
Relational interventions such as Active Listening (NIC 4920) and Counseling (NIC 5240) complete the care plan by allowing for deeper processing of the experience and fostering continuity in the nurse–patient relationship beyond the acute phase.
The expected outcomes identified are Coping (NOC 1302), Personal Resiliency (NOC 1309) and Anxiety control (NOC 1402) as they allow for the systematic evaluation of the patient’s adaptive process and the effectiveness of the nursing support provided during the recovery phase.
To assess coping strategies, the Brief COPE Inventory scale may be used, [17] while the Connor-Davidson Resilience Scale (CD-RISC), including the short form (CD-RISC-10), could be adopted to measure the ability to recover from adverse events, potentially establishing a proper follow-up for the patient [18].
The effectiveness of the proposed nursing interventions can be evaluated through a combination of NOC indicators (e.g., Anxiety Self-Control, Communication, Coping), behavioral observations, and, when applicable, validated psychological scales such as the State-Trait Anxiety Inventory (STAI-Y) or Hospital Anxiety and Depression Scale (HADS) [19,20].
The model was developed through a review of literature from related care contexts (e.g., intensive care units, isolation wards) and the consensus among the authors, formed during recent the COVID-19 pandemic. These choices provide a foundation for guiding future empirical validation and pilot implementation.
Statistical Analysis
As this work presents a theoretical nursing care model and does not involve the collection of quantitative data, no statistical analysis was performed. Future prospective studies, involving structured data collection and patient outcomes measurement, will be necessary to validate the proposed model using appropriate statistical methods.
DESCRIPTION OF THE PROPOSED MODEL
In biocontainment transfers, three distinct phases of nursing care can be identified: the preparatory phase before transport (pre-transport), the transfer phase using the isolator (transport), and the final phase after transport (post-transport). Each phase presents specific care and assistance needs.
Before transport, the patient may experience excessive anxiety related to the procedures and the outcome of the transfer, also due to the visual impact of the isolator. Its limited space may cause a sense of claustrophobia, further intensifying the level of distress.
The observation of specific defining characteristics, such as behavioral/emotional signs like anguish, psychomotor agitation, and verbalized fears, as well as physiological signs like increased heart rate and blood pressure, facial flushing, and a trembling voice, suggests a state of disproportionate and persistent concern in response to perceived threats. Based on these elements, the most appropriate nursing diagnosis is Excessive Anxiety (00400), as it accurately reflects the patient’s distress, expressed through both emotional and behavioral signs and physical hyperactivation.
The primary goal becomes Anxiety Self-Control (NOC 1402), assessed through a reduction in agitation and increased patient cooperation. To achieve this, targeted interventions are necessary. Anxiety Reduction (NIC 5820) and Emotional Support (NIC 5270) are essential to create a reassuring environment and foster empathetic communication.
During biocontainment transport, the use of PPE and the isolator may create concrete communication barriers, [3,5,8] resulting in frustration or misunderstanding. This scenario corresponds to the diagnosis Impaired Verbal Communication (00051), characterized by limited or absent ability to receive, process, transmit, and/or use a symbol system. The outcome to be achieved is Communication (NOC 0902).
The intervention plan includes a key nursing intervention, the Communication Enhancement: Speech Deficit (NIC 4976), which encourages the use of alternative communication channels (e.g., visual aids) and promotes the use of shared language, ensuring mutual understanding.
Concrete examples include:
Use of visual aids such as augmentative and alternative communication (AAC) boards, [9] shared with the patient during the pre-transport phase, or tablets/whiteboards to facilitate needs expression.
Active listening techniques: maintaining eye contact, nodding, asking clarifying questions, allowing time for patient responses [11].
Frequent comprehension checks: asking the patient to repeat or rephrase the information received to confirm understanding.
By implementing these strategies, nurses support patients in overcoming communication barriers related to PPE, isolators, and other devices, maintaining an effective and safe level of interaction.
In the post-transport phase, the need to strengthen coping strategies becomes particularly evident when the patient shows difficulty processing the experience or managing stress from isolation. In this context, the diagnosis Readiness for Enhanced Coping (00158) describes the possibility of reinforcing cognitive and/or behavioral efforts to deal with distressing situations.
The expected outcomes (NOC) include Coping (1302), Personal Resiliency (1309), and Anxiety Self-Control (1402). The aim is to increase the patient’s ability to manage stressful events, [21] show flexibility in new circumstances, and limit agitation or irritability.
Several key interventions (NIC) support this goal:
Coping Enhancement (5230), which encourages identification of existing strategies and discovery of additional resources (e.g., family support via video call, mindfulness techniques) [14].
Emotional Support (5270), offering empathetic listening and normalization of stress reactions [22].
Active Listening (4920) and Counseling (5240), which aid in processing the experience, reduce frustration, and foster patient cooperation [22-24].
Counseling (5240) supports the patient in processing emotional distress by fostering a trusting, empathetic relationship. It helps the patient identify sources of discomfort, express concerns, and explore adaptive coping strategies, thereby enhancing self-awareness and emotional stability after the transfer process [18,22].
PhaseDiagnosis (Code)DomainClass
| Phase | Diagnosis (Code) | Domain | Class | NIC | NOC |
| Pre-transport | Excessive Anxiety (00400) | 9 | 2 | Anxiety Reduction (NIC 5820) | Anxiety Self-Control (NOC 1402) |
| Emotional Support (NIC 5270) | |||||
| Transport | Impaired Verbal Communication (00051) | 5 | 5 | Communication Enhancement: Speech Deficit (NIC 4976) | Communication (NOC 0902) |
| Post-transport | Readiness for Enhanced Coping (00158) | 9 | 2 | Coping Enhancement (NIC 5230) | Coping (NOC 1302) Personal Resiliency (NOC 1309) Anxiety Self-Control (NOC 1402) |
| Emotional Support (NIC 5270) | |||||
| Active Listening (NIC 4920) | |||||
| Counseling (NIC 5240) |
Table 1. Association between the phases of biocontainment transport and the related elements of the nursing process.
Table 2 illustrates the functionality and operational implementation of the proposed model across the three phases of biocontainment transfer. That table presents a structured fictitious clinical case; for each phase, it describes a generic patient scenario along with the corresponding nursing interventions. This approach aims to exemplify how the theoretical model can be translated into clinical practice, promoting its reproducibility and applicability in high-complexity care settings.
| Phase | Fictitious Case Description | Practical Nursing Interventions |
| Pre-transport | A conscious and oriented adult patient is informed of an imminent transfer toward the radiology department using a biocontainment stretcher. Upon seeing the isolator, the patient becomes visibly agitated, expresses fear, and shows signs of anxiety (e.g., flushed face, tachycardia). | • Apply Anxiety Reduction (NIC 5820) • Use Emotional Support (NIC 5270) • Perform a rapid anxiety screening (GAD-7) • Introduce the AAC board |
| Transport | During transfer, communication is significantly impaired due to PPE and physical barriers. |
|
| Post-transport | After reaching the destination, the patient expresses emotional exhaustion and stress. |
|
Table 2. Fictitious clinical case illustrating nursing interventions across the phases of biocontainment transport.

Figure 1. Conceptual flowchart illustrating nursing diagnoses, interventions (NIC), outcomes (NOC), assessment tools and practical applications across the phases of biocontainment transport.
DISCUSSION
The aim of this study is to develop and propose an innovative structured nursing model designed to address both the clinical and psychological needs of conscious and communicative patients undergoing biocontainment transport. As mentioned in the introduction, most of the literature currently published focuses on the organizational, logistical and technological aspects of the transfer to biocontainment rather than offering organized and systematic nursing care models. Since it incorporates nursing diagnoses, interventions, and expected outcomes based on the NANDA-I, NIC, and NOC taxonomies, the model offered here represents an original contribution in this context. It provides a theoretical and practical approach focused on the psychological, communicative, and relational needs of conscious and communicative patients throughout the entire transfer process. This model is a novel idea that can be validated and applied in high-complexity care settings because of its attention to care detail, taxonomic clarity, and clinical application. The structured model developed highlights how each phase of biocontainment transfer presents specific and distinct care needs. The systematic approach to managing pre-transfer anxiety, maintaining effective communication during transport, and providing psychological support after transfer underscores the need for personalized and coordinated interventions.
The integration of nursing diagnoses, NOC outcomes, and NIC interventions enables the construction of a comprehensive care response that addresses not only clinical aspects but also emotional and relational dimensions.
The impact of biocontainment on patient-provider communication is particularly significant [3,5].
The use of PPE and isolating devices presents real obstacles and requires well-planned alternative strategies to prevent further emotional deterioration.
Finally, the post-transport phase is often underestimated but can be a critical moment for the patient to process the experience. Strengthening coping skills and promoting resilience not only improve clinical outcomes but also enhance the patient’s overall care experience [21].
Limitation
This theoretical nursing care model was developed through the integration of taxonomy and expert consensus, without direct patient involvement.
The implementation and effectiveness in real clinical settings have not yet been evaluated; future studies should be structured to assess the outcomes related to its application through quantitative measurements and subsequent evaluations in biocontainment transfer settings.
Such investigations will be essential to refine the model and confirm its clinical relevance and utility.
The proposed nursing care model can be practically applied in various high-complexity clinical settings, such as infectious disease units, intensive care units, and specialized medical transport services for highly infectious patients.
To validate the model’s effectiveness, the systematic collection of clinical data before and after the biocontainment transfer is recommended. Among the possible assessment tools, the GAD-7 scale may be used for anxiety, the Brief COPE Inventory for coping strategies, and the CD-RISC-10 for resilience levels. In cases of limited verbal communication, the use of structured observational checklists and AAC (Augmentative and Alternative Communication) tools can provide reliable alternative measurements.
The analysis of collected data may include descriptive statistics and inferential tests to compare pre- and post-intervention conditions. These strategies will allow for measuring the model’s impact on key care outcomes and refining its applicability for potential structured implementation in the future.
CONCLUSIONS
The management of patients in biocontainment requires a strategic combination of clinical and communication skills to address the nursing diagnoses that emerge throughout the three phases of transfer. By applying structured care models, it is possible to improve clinical outcomes, reduce biological risks, and ensure effective communication even in extreme isolation conditions. The integration of protocols and nursing interventions provides an effective solution to the demands of complex and highly specialized care. Although the efficiency of the suggested model has not yet been confirmed in practical situations, it constitutes a substantial theoretical advance to the nursing management of biocontainment transfers. In order to confirm its practical application and quantify its observable advantages on important care outcomes, pilot projects and prospective studies should be started and carried out in real care situations. The model's robustness can only be verified and its organized adoption encouraged by means of rigorous testing
Ethical Approval
For this study, no formal approval from the Local Ethics Committee was required.
Conflicts of Interest and Funding Sources
The authors declare that they have no conflicts of interest related to this work. The study received no financial support from public or private entities, including pharmaceutical or industrial companies.
Authors’ Contributions
Federico D’Urso: conceived the study, developed the care model, and coordinated the writing of the manuscript. Salvatore Trifiletti: contributed to the organization of the NANDA-I, NIC, and NOC framework. Edoardo Falcone: participated in literature review and content refinement. Mara Gracy Basile: contributed to methodological structure and theoretical validation. Ulrico Angeloni: revised and validated the entire study and ensured its clinical and theoretical consistency. All authors read and approved the final version of the manuscript.
Acknowledgments
The authors would like to thank the staff of the Italian Red Cross – Public Health Department for their continuous support and collaboration in developing the proposed model. Special thanks also to the academic community for the critical reflection that inspired the elaboration of this work.
REFERENCES
Gibbs, S. G., Herstein, J. J., Le, A. B., Beam, E. L., Cieslak, T. J., Lawler, J. V., Santarpia, J. L., Stentz, T. L., Kopocis-Herstein, K. R., Achutan, C., Carter, G. W., & Lowe, J. J. (2019). Review of Literature for Air Medical Evacuation High-Level Containment Transport. Air medical journal, 38(5), 359–365. HYPERLINK "https://doi.org/10.1016/j.amj.2019.06.006"https://doi.org/10.1016/j.amj.2019.06.006
D’Urso, F., Meroni, L., Rech, R., Musumeci, A., Bonini, A., Piotti, C., Ciriaci, A. and Menghini, S. (2024) “Possible care protocols for patients undergoing road transfer on a biocontainment stretcher model N 36 (36 m3 air ˃60 ACH)”, Emergency Care Journal, 20(3). doi: 10.4081/ecj.2024.12334.
Rehn, M., Heyerdahl, F., Osbakk, S. A., Andresen, Å. E., & Hagemo, J. (2023). Challenges and Risks in Out-of-Hospital Transport of Patients During the Coronavirus Disease 2019 Pandemic. Air medical journal, 42(3), 191–195. HYPERLINK "https://doi.org/10.1016/j.amj.2023.02.002"https://doi.org/10.1016/j.amj.2023.02.002
Garibaldi, B. T., Conger, N. G., Withers, M. R., Hatfill, S. J., Gutierrez-Nunez, J. J., & Christopher, G. W. (2019). Aeromedical Evacuation of Patients with Contagious Infections. Aeromedical Evacuation: Management of Acute and Stabilized Patients, 317–335. HYPERLINK "https://doi.org/10.1007/978-3-030-15903-0_20"https://doi.org/10.1007/978-3-030-15903-0_20
Aengst, J., Walker-Stevenson, G., Harrod, T., Ivankovic, J., Neilson, J., & Guise, J. M. (2022). Uncomfortable yet necessary: The impact of PPE on communication in emergency medicine. International journal for quality in health care: journal of the International Society for Quality in Health Care, 34(4), mzac095. HYPERLINK "https://doi.org/10.1093/intqhc/mzac095"https://doi.org/10.1093/intqhc/mzac095
Corradi, M., Cattaneo, A., Plicco, C., & Bossi, E. (2021). HTA of novel biocontainment systems for ambulance transport: public health implications. The European Journal of Public Health, 31(Suppl 3), ckab165.132. HYPERLINK "https://doi.org/10.1093/eurpub/ckab165.132"https://doi.org/10.1093/eurpub/ckab165.132
Flinn, J. B., Hynes, N. A., Sauer, L. M., Maragakis, L. L., & Garibaldi, B. T. (2021). The role of dedicated biocontainment patient care units in preparing for COVID-19 and other infectious disease outbreaks. Infection control and hospital epidemiology, 42(2), 208–211. HYPERLINK "https://doi.org/10.1017/ice.2020.451"https://doi.org/10.1017/ice.2020.451
Saunders, G. H., Jackson, I. R., & Visram, A. S. (2021). Impacts of face coverings on communication: an indirect impact of COVID-19. International journal of audiology, 60(7), 495–506. HYPERLINK "https://doi.org/10.1080/14992027.2020.1851401"https://doi.org/10.1080/14992027.2020.1851401
Costello, J.M. (2000). AAC intervention in the intensive care unit: The children's hospital Boston model. Augmentative and Alternative Communication, 16, 137 - 153.
Zaylskie, L. E., Biggs, E. E., Minchin, K. J., & Abel, Z. K. (2024). Nurse perspectives on supporting children and youth who use augmentative and alternative communication (AAC) in the pediatric intensive care unit. Augmentative and alternative communication (Baltimore, Md.: 1985), 40(4), 255–266. HYPERLINK "https://doi.org/10.1080/07434618.2023.2284269"https://doi.org/10.1080/07434618.2023.2284269
Ten Hoorn, S., Elbers, P. W., Girbes, A. R., & Tuinman, P. R. (2016). Communicating with conscious and mechanically ventilated critically ill patients: a systematic review. Critical care (London, England), 20(1), 333. HYPERLINK "https://doi.org/10.1186/s13054-016-1483-2"https://doi.org/10.1186/s13054-016-1483-2
Beam, E.L., Boulter, K.C., Freihaut, F., Schwedhelm, S. and Smith, P.W. (2010), The Nebraska Experience in Biocontainment Patient Care. Public Health Nursing, 27: 140-147. HYPERLINK "https://doi.org/10.1111/j.1525-1446.2010.00837.x"https://doi.org/10.1111/j.1525-1446.2010.00837.x
Swickard, S., Swickard, W., Reimer, A., Lindell, D., & Winkelman, C. (2014) Adaptation of the AACN Synergy Model for Patient Care to Critical Care Transport. Crit Care Nurse, 34(1),16–28. doi: 10.4037/ccn2014573.
Sánchez-Almagro, C. P., Romero-Sánchez, J. M., White-Ríos, M., González Del Pino, C. A., & Paloma-Castro, O. (2022). NANDA International nursing diagnoses in the coping/stress tolerance domain and their linkages to Nursing Outcomes Classification outcomes and Nursing Interventions Classification interventions in the pre-hospital emergency care. Journal of advanced nursing, 78(10), 3273–3289. HYPERLINK "https://doi.org/10.1111/jan.15280"https://doi.org/10.1111/jan.15280
Villarreal-Zegarra, D., Paredes-Angeles, R., Mayo-Puchoc, N. et al. Psychometric properties of the GAD-7 (General Anxiety Disorder-7): a cross-sectional study of the Peruvian general population. BMC Psychol 12, 183 (2024). https://doi.org/10.1186/s40359-024-01688-8
Ganesan S, Balasubramanian B, Krishnamurthy P, Govindan R, Mani N. Effects of Tele-Counseling on Reducing Anxiety Levels of COVID-19 Patients in Isolation Wards: An Observational Study. Indian Journal of Psychological Medicine. 2022;45(1):43-46. doi:10.1177/02537176221139598
Solberg, M. A., Gridley, M. K., & Peters, R. M. (2022). The Factor Structure of the Brief Cope: A Systematic Review. Western journal of nursing research, 44(6), 612–627. HYPERLINK "https://doi.org/10.1177/01939459211012044"https://doi.org/10.1177/01939459211012044
Kuiper, H., van Leeuwen, C. C. M., Stolwijk-Swüste, J. M., & Post, M. W. M. (2019). Measuring resilience with the Connor-Davidson Resilience Scale (CD-RISC): which version to choose?. Spinal cord, 57(5), 360–366. HYPERLINK "https://doi.org/10.1038/s41393-019-0240-1"https://doi.org/10.1038/s41393-019-0240-1
Dias, P., Clerc, D., da Rocha Rodrigues, M. G., Demartines, N., Grass, F., & Hübner, M. (2022). Impact of an Operating Room Nurse Preoperative Dialogue on Anxiety, Satisfaction and Early Postoperative Outcomes in Patients Undergoing Major Visceral Surgery-A Single Center, Open-Label, Randomized Controlled Trial. Journal of clinical medicine, 11(7), 1895. HYPERLINK "https://doi.org/10.3390/jcm11071895"https://doi.org/10.3390/jcm11071895
Haugan, G., & Drageset, J. (2014). The hospital anxiety and depression scale--dimensionality, reliability and construct validity among cognitively intact nursing home patients. Journal of affective disorders, 165, 8–15. https://doi.org/10.1016/j.jad.2014.04.042
Ocloo, J., Garfield, S., Franklin, B. D., & Dawson, S. (2021). Exploring the theory, barriers and enablers for patient and public involvement across health, social care and patient safety: a systematic review of reviews. Health research policy and systems, 19(1), 8. HYPERLINK "https://doi.org/10.1186/s12961-020-00644-3"https://doi.org/10.1186/s12961-020-00644-3
Madl, J. E. M., Sturmbauer, S. C., Janka, R., Bay, S., & Rohleder, N. (2022). Preparing patients according to their individual coping style improves patient experience of magnetic resonance imaging. Journal of behavioral medicine, 45(6), 841–854. HYPERLINK "https://doi.org/10.1007/s10865-022-00361-y"https://doi.org/10.1007/s10865-022-00361-y
Wallace L. M. (1986). Communication variables in the design of pre-surgical preparatory information. The British journal of clinical psychology, 25 (Pt 2), 111–118. HYPERLINK "https://doi.org/10.1111/j.2044-8260.1986.tb00679.x"https://doi.org/10.1111/j.2044-8260.1986.tb00679.x
Caddick, J., Jawad, S., Southern, S., & Majumder, S. (2012). The power of words: sources of anxiety in patients undergoing local anaesthetic plastic surgery. Annals of the Royal College of Surgeons of England, 94(2), 94–98. HYPERLINK "https://doi.org/10.1308/003588412X13171221501267"https://doi.org/10.1308/003588412X13171221501267
![]() This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Biocontainment Transfer: A structured nursing model for enhancing patient care
Federico D’Urso 1*, Salvatore Trifiletti 2, Edoardo Falcone 1, Mara Gracy Basile 1, Ulrico Angeloni 1
1. Public Health Unit, Italian Red Cross – National Headquarters, 00151, Rome, Italy
2. Department of Medical, Surgical Sciences and Advanced Technologies “G. F. Ingrassia”, University of Catania, 95125, Catania, Italy.
* Corresponding author: Federico D’Urso, Public Health Unit, Italian Red Cross – National Headquarters, 00151, Rome, Italy. E-mail: federico.durso@gmail.com
Cite this article
ABSTRACT
Introduction: Biocontainment transfer represents a complex and delicate phase of care, especially in light of the increased demand for safe handling of patients affected by highly transmissible diseases. The COVID-19 pandemic has highlighted the critical need for structured approaches to ensure quality care and safety during these transfers.
Objective: To propose a structured nursing model for managing the care of conscious and communicative patients undergoing biocontainment transport, based on nursing diagnoses and standardized interventions.
Methods: A theoretical-conceptual model was developed based on the NANDA-I 2024–2026 taxonomy to identify nursing diagnoses related to perception, cognition, and stress tolerance. These were systematically combined with appropriate interventions from the Nursing Interventions Classification (NIC) and expected outcomes from the Nursing Outcomes Classification (NOC). The model addresses the clinical and psychological needs of patient across the three phases of transport: pre-transport, transport, and post-transport, with particular focus on anxiety management, communication, and adaptation to isolation.
Results: In the pre-transport phase, the diagnosis of Excessive Anxiety was addressed with interventions to reduce emotional distress and improve patient cooperation through clear, empathetic communication. During transport, the impairment of verbal communication caused by protective equipment and isolation barriers was mitigated through simplified language, visual aids, and strategies to ensure mutual understanding. In the post-transport phase, the model focused on enhancing the patient's coping capacity and resilience, offering emotional support and structured interventions to manage stress and process the experience.
Conclusions: The proposed model provides a comprehensive and systematic framework for nursing care during biocontainment transfers, integrating both clinical and emotional aspects to reduce patient vulnerability and improve the quality of care. As a theoretical model built upon standardized nursing taxonomies, it lays the groundwork for future clinical applications. Prospective and pilot studies will be essential to validate its effectiveness and feasibility in real-world healthcare settings.
Keywords: Biocontainment, Biocontainment patient transport, Nursing process, Clinical complexity, Advanced nursing practice.
INTRODUCTION
The current healthcare landscape has changed radically compared to a few years ago; the COVID-19 pandemic has highlighted structural and staffing shortages on a global scale [1,2]. The increase in the number of patients affected by highly transmissible diseases requiring high-intensity care has led to the widespread introduction of isolation devices that were once reserved for extremely rare situations. Biocontainment isolators have proven to be essential in the transport of these patients and typically include a protective plastic enclosure, a High Efficiency Particulate Air (HEPA) filter that removes harmful airborne particles, and a ventilation system that maintains a clean airflow at controlled pressure, preventing the escape of pathogens [2].
In the presence of diseases characterized by a high risk of mortality or a lack of appropriate preventive measures and effective treatments, the use of isolators becomes essential to ensure maximum safety for both the patient and healthcare personnel [1,3,4].
Preparing and managing the patient for a biocontainment transfer represents one of the most complex challenges for healthcare personnel, requiring protocols and technologies to guarantee both staff protection and the quality of patient care [2].
The use of biocontainment isolators can be compared to a form of physical restraint, as they impose an isolation measure that limits the patient's interaction with the external environment [5].
Although biocontainment isolators are essential for the safe transport of patients, their implementation presents significant logistical and organizational challenges that must be addressed [1,2].
Several studies have addressed the logistical and clinical challenges associated with the transport of patients in high-level containment. Gibbs et al. (2019) provide a comprehensive review of air medical evacuation protocols for biocontainment transport, focusing on technical and operational safety measures [1]. Similarly, Corradi et al. (2021) assess the public health implications of biocontainment systems used in ambulances, while D’Urso et al. (2024) describe possible care protocols for patients transferred using a biocontainment stretcher [2,6]. However, these contributions primarily emphasize technical configurations and infection control, without proposing a structured model of nursing care.
Studies investigating patient management within dedicated biocontainment units (e.g., Flinn et al., 2021) and during pandemic conditions Rehn et al., 2023 have highlighted the complexity of delivering safe care in isolation, yet they stop short of defining a standardized nursing process [3,7]. Other investigations have explored the communicative and emotional needs of patients in constrained settings. For example, the impact of personal protective equipment (PPE) on communication is well documented (Aengst et al., 2022; Saunders et al., 2021), and the relevance of augmentative and alternative communication (AAC) strategies in ICUs has been addressed by Costello (2000) and Zaylskie et al. (2024) [5,8-10]. Ten Hoorn et al. (2016) offer a systematic review on communication with mechanically ventilated patients, further supporting the need for dedicated relational strategies in high-complexity care [11].
While these studies help define the relational and contextual challenges of care in isolation, they do not translate into a structured, taxonomy-based model. Beam et al. (2010) and Swickard et al. (2014), for example, offer insights into the organization of biocontainment units and interfacility critical care transport, but without applying NANDA-I, NIC, or NOC frameworks [12,13].
This overview of the current literature confirms the absence of validated nursing care models specifically designed for conscious and communicative patients undergoing biocontainment transfers, thereby justifying the development of a structured approach grounded in standardized nursing taxonomies.
To fill this gap and address these challenges, the development of a structured nursing care model, based on targeted nursing diagnoses, is essential to guide clinical practice. Such a model can improve patient safety, enhance the quality of communication, and ensure continuity of care throughout the different phases biocontainment transfer process [6,7].
Objective and purpose
The aim of this study is to develop and propose an innovative structured nursing model designed to address both the clinical and psychological needs of conscious and communicative patients undergoing biocontainment transport. The model integrates standardized nursing diagnoses, interventions, and outcomes to enhance communication, reduce anxiety, and improve overall patient care across all phases of transport, laying the foundation for future clinical validation.
DEVELOPMENT OF THE CARE MODEL
Sampling and Eligibility
This study consists of a theoretical and methodological proposal for a structured care model for conscious and communicative patients without the actual collection of clinical data.
The model is designed for future applications in clinical practice and is intended to be validated in prospective studies involving real patients and healthcare teams.
Instruments
The care model is based on the integration of nursing diagnoses (NDs) from the NANDA-I 2024–2026 taxonomy and integrates elements from the NIC (Nursing Interventions Classification) and NOC (Nursing Outcomes Classification) systems. The selection of nursing diagnoses, interventions, and outcomes was informed by a narrative review of literature related to care in isolation, high-risk transport, and psychological support in confined environments. Due to the absence of specific scientific studies on biocontainment transfers, references from similar contexts were used. The process was further refined through structured consensus among the authors, all of whom have experience in emergency nursing and biocontainment patient management. To correctly select the appropriate NDs, an in-depth analysis was conducted of all thirteen domains included in the NANDA-I 2024–2026 classification. Some domains were excluded from consideration for the biocontainment transfer of conscious and communicative patients, as they were not relevant to the specific context. Domain 1 (Health Promotion) was excluded due to its focus on long-term behavioral patterns, domains 2 (Nutrition) and 3 (Elimination and Exchange) were not considered since they are not typically involved in short-term transfers and are managed in longer-duration ones. Domain 4 (Activity/Rest) was excluded because of its limited relevance during transport. Domains 6 (Self-Perception), 7 (Role Relationships), 8 (Sexuality) and 10 (Life Principles) were deemed not pertinent to biocontainment transfer. Furthermore, the domains 12 (Comfort) and 13 (Growth/Development) were excluded because they are not central in urgent care situations.
Domain 11 (Safety/Protection), although potentially relevant from a clinical standpoint, was excluded because it primarily focuses on physical risks such as infections or trauma. The typical patient considered is already in a similar condition; however, the main goal of the proposed model is instead to enhance the communicative, relational, and emotional dimensions of care through structured nursing interventions. Given these factors, the analysis focused on two specific domains the domain 5, (Perception/Cognition) with particular attention to cognitive understanding and communication and domain 9 (Coping/Stress Tolerance), which addresses psychological and emotional reactions. Within domain 5, only class 5 (Communication) was retained, as it includes diagnoses that are directly applicable to the needs of conscious patients experiencing communication difficulties due to the constraints of the biocontainment context, including the use of PPE. The other classes within this domain class 1 (Attention), 2 (Orientation) and 3 (Sensation/Perception), were excluded as they currently contain no NDs. Class 4 (Cognition) was also excluded, as it refers to cognitive deficits that require specific clinical and pharmacological management. In the case of a disoriented patient placed in a biocontainment isolator, such a condition would likely be exacerbated by the restrictive environment, making sedation the most appropriate and safe option for transport. Regarding domain 9, only class 2 (Emotional Responses) was included, as it encompasses diagnoses such as anxiety, ineffective coping, and stress responses, which are frequently observed in patients subjected to restrictive isolation. The remaining classes, 1 (Post-Trauma Responses) and 3 (Impulse Control), were excluded. In particular, class 1 was deliberately not considered, as the aim of the proposed model is to prevent the onset of post-traumatic stress symptoms related to the biocontainment transfer, by supporting the patient through structured interventions that reduce emotional overload and promote coping during the procedure. Based on this taxonomic analysis, the nursing care model was structured into three distinct phases, pre-transport, transport, and post-transport, each associated with specific nursing diagnoses, related interventions, and expected outcomes.
Pre-transport phase
The lack of knowledge about the biocontainment stretcher and the procedures to be carried out during the transfer generates, at this stage, significant emotional distress and anticipatory anxiety. The nursing diagnosis excessive anxiety (00400), classified under domain 9, class 2, was selected based on observations conducted in clinical practice, where behavioral and physiological signs such as agitation, increased heart rate, and verbal expressions of concern are commonly noted.
Other diagnoses within the same class, such as fear (00390) or impaired resilience (00210), were excluded because they involve long-term patterns or cannot be adequately documented within the limited timeframe of the transfer.
To address this diagnosis, the NIC interventions anxiety reduction (5820) and emotional support (5270) were selected, with the expected NOC outcome being anxiety Self-Control (1402). [14]
Since the goal of this care model is to promote coping, we preferred to use the NOC Anxiety Self-Control (1402), as it reflects the objective of enhancing the patient’s conscious management of anxiety.
The NOC Anxiety Level (1211) may be useful for an initial clinical assessment or for pre-post comparisons, but its purpose would remain limited to quantifying the symptom.
In this phase, it may be useful to conduct an initial assessment of the patient's anxiety level, followed by a second evaluation to measure the effectiveness of interventions, using a rapid-assessment tool such as the Generalized Anxiety Disorder-7 (GAD-7) scale [15,16].
Transport phase
The use of the biocontainment stretcher and PPE generates significant communication barriers between patients and healthcare professionals. Within domain 5, class 5 of the NANDA-I taxonomy, the diagnosis Readiness for Enhanced Communication (00185) was excluded, as it is focused on strengthening a communicative process that is already functioning. In this context, however, it is necessary to implement an alternative communication system to replace the traditional one, which is compromised by operational conditions.
Similarly, the diagnosis Risk for Impaired Verbal Communication (00434) was excluded because it refers to a susceptibility to communication impairment, whereas in the current scenario the impairment is already present.
The most consistent was found to be DN Impaired Verbal Communication (00051), which characterizes a limited or nonexistent capacity for verbal communication. [9,10]
The selected nursing interventions are Communication Enhancement: Speech Deficit (4976) chosen to facilitate effective information exchange through alternative communicative methods during the transport phase.
Communication (0902), the related NOC, enables the assessment of the efficacy of the patient-provider relationship in situations where communication is constrained.
Post-transport phase
In this phase, the patient faces the need for emotional recovery and coping support following the biocontainment transfer, the DNs Readiness for Enhanced Coping (00158), classified under domain 9, class 2, was selected, as it reflects the patient’s willingness and potential to strengthen adaptive strategies in response to an acute stress situation [14,16].
This choice is based on the authors’ clinical observations in most cases; conscious and cooperative patients exhibit transient emotional discomfort that can be interpreted as a normal physiological response to stress rather than a failure of their coping abilities. Consequently, diagnoses such as Ineffective Coping (00069) were excluded, as they would imply a dysfunction in stress management and risk labeling a temporary and reactive experience as a psychological disorder.
The care objective is not the treatment of a psychological condition, but rather the enhancement of the patient’s existing personal resources by fostering resilience and facilitating the emotional processing of the experience through structured interventions.
In line with this approach, several standardized nursing interventions (NIC) were selected to support the patient’s adaptation and increase their stress management capacity. Among them, Coping Enhancement (5230) represents the core intervention aimed at promoting an adaptive response to the experience.
These are supported by Emotional Support (5270) which is essential for normalizing emotional reactions, containing residual anxiety, and facilitating emotional rebalancing.
Relational interventions such as Active Listening (NIC 4920) and Counseling (NIC 5240) complete the care plan by allowing for deeper processing of the experience and fostering continuity in the nurse–patient relationship beyond the acute phase.
The expected outcomes identified are Coping (NOC 1302), Personal Resiliency (NOC 1309) and Anxiety control (NOC 1402) as they allow for the systematic evaluation of the patient’s adaptive process and the effectiveness of the nursing support provided during the recovery phase.
To assess coping strategies, the Brief COPE Inventory scale may be used, [17] while the Connor-Davidson Resilience Scale (CD-RISC), including the short form (CD-RISC-10), could be adopted to measure the ability to recover from adverse events, potentially establishing a proper follow-up for the patient [18].
The effectiveness of the proposed nursing interventions can be evaluated through a combination of NOC indicators (e.g., Anxiety Self-Control, Communication, Coping), behavioral observations, and, when applicable, validated psychological scales such as the State-Trait Anxiety Inventory (STAI-Y) or Hospital Anxiety and Depression Scale (HADS) [19,20].
The model was developed through a review of literature from related care contexts (e.g., intensive care units, isolation wards) and the consensus among the authors, formed during recent the COVID-19 pandemic. These choices provide a foundation for guiding future empirical validation and pilot implementation.
Statistical Analysis
As this work presents a theoretical nursing care model and does not involve the collection of quantitative data, no statistical analysis was performed. Future prospective studies, involving structured data collection and patient outcomes measurement, will be necessary to validate the proposed model using appropriate statistical methods.
DESCRIPTION OF THE PROPOSED MODEL
In biocontainment transfers, three distinct phases of nursing care can be identified: the preparatory phase before transport (pre-transport), the transfer phase using the isolator (transport), and the final phase after transport (post-transport). Each phase presents specific care and assistance needs.
Before transport, the patient may experience excessive anxiety related to the procedures and the outcome of the transfer, also due to the visual impact of the isolator. Its limited space may cause a sense of claustrophobia, further intensifying the level of distress.
The observation of specific defining characteristics, such as behavioral/emotional signs like anguish, psychomotor agitation, and verbalized fears, as well as physiological signs like increased heart rate and blood pressure, facial flushing, and a trembling voice, suggests a state of disproportionate and persistent concern in response to perceived threats. Based on these elements, the most appropriate nursing diagnosis is Excessive Anxiety (00400), as it accurately reflects the patient’s distress, expressed through both emotional and behavioral signs and physical hyperactivation.
The primary goal becomes Anxiety Self-Control (NOC 1402), assessed through a reduction in agitation and increased patient cooperation. To achieve this, targeted interventions are necessary. Anxiety Reduction (NIC 5820) and Emotional Support (NIC 5270) are essential to create a reassuring environment and foster empathetic communication.
During biocontainment transport, the use of PPE and the isolator may create concrete communication barriers, [3,5,8] resulting in frustration or misunderstanding. This scenario corresponds to the diagnosis Impaired Verbal Communication (00051), characterized by limited or absent ability to receive, process, transmit, and/or use a symbol system. The outcome to be achieved is Communication (NOC 0902).
The intervention plan includes a key nursing intervention, the Communication Enhancement: Speech Deficit (NIC 4976), which encourages the use of alternative communication channels (e.g., visual aids) and promotes the use of shared language, ensuring mutual understanding.
Concrete examples include:
Use of visual aids such as augmentative and alternative communication (AAC) boards, [9] shared with the patient during the pre-transport phase, or tablets/whiteboards to facilitate needs expression.
Active listening techniques: maintaining eye contact, nodding, asking clarifying questions, allowing time for patient responses [11].
Frequent comprehension checks: asking the patient to repeat or rephrase the information received to confirm understanding.
By implementing these strategies, nurses support patients in overcoming communication barriers related to PPE, isolators, and other devices, maintaining an effective and safe level of interaction.
In the post-transport phase, the need to strengthen coping strategies becomes particularly evident when the patient shows difficulty processing the experience or managing stress from isolation. In this context, the diagnosis Readiness for Enhanced Coping (00158) describes the possibility of reinforcing cognitive and/or behavioral efforts to deal with distressing situations.
The expected outcomes (NOC) include Coping (1302), Personal Resiliency (1309), and Anxiety Self-Control (1402). The aim is to increase the patient’s ability to manage stressful events, [21] show flexibility in new circumstances, and limit agitation or irritability.
Several key interventions (NIC) support this goal:
Coping Enhancement (5230), which encourages identification of existing strategies and discovery of additional resources (e.g., family support via video call, mindfulness techniques) [14].
Emotional Support (5270), offering empathetic listening and normalization of stress reactions [22].
Active Listening (4920) and Counseling (5240), which aid in processing the experience, reduce frustration, and foster patient cooperation [22-24].
Counseling (5240) supports the patient in processing emotional distress by fostering a trusting, empathetic relationship. It helps the patient identify sources of discomfort, express concerns, and explore adaptive coping strategies, thereby enhancing self-awareness and emotional stability after the transfer process [18,22].
PhaseDiagnosis (Code)DomainClass
| Phase | Diagnosis (Code) | Domain | Class | NIC | NOC |
| Pre-transport | Excessive Anxiety (00400) | 9 | 2 | Anxiety Reduction (NIC 5820) | Anxiety Self-Control (NOC 1402) |
| Emotional Support (NIC 5270) | |||||
| Transport | Impaired Verbal Communication (00051) | 5 | 5 | Communication Enhancement: Speech Deficit (NIC 4976) | Communication (NOC 0902) |
| Post-transport | Readiness for Enhanced Coping (00158) | 9 | 2 | Coping Enhancement (NIC 5230) | Coping (NOC 1302) Personal Resiliency (NOC 1309) Anxiety Self-Control (NOC 1402) |
| Emotional Support (NIC 5270) | |||||
| Active Listening (NIC 4920) | |||||
| Counseling (NIC 5240) |
Table 1. Association between the phases of biocontainment transport and the related elements of the nursing process.
Table 2 illustrates the functionality and operational implementation of the proposed model across the three phases of biocontainment transfer. That table presents a structured fictitious clinical case; for each phase, it describes a generic patient scenario along with the corresponding nursing interventions. This approach aims to exemplify how the theoretical model can be translated into clinical practice, promoting its reproducibility and applicability in high-complexity care settings.
| Phase | Fictitious Case Description | Practical Nursing Interventions |
| Pre-transport | A conscious and oriented adult patient is informed of an imminent transfer toward the radiology department using a biocontainment stretcher. Upon seeing the isolator, the patient becomes visibly agitated, expresses fear, and shows signs of anxiety (e.g., flushed face, tachycardia). | • Apply Anxiety Reduction (NIC 5820) • Use Emotional Support (NIC 5270) • Perform a rapid anxiety screening (GAD-7) • Introduce the AAC board |
| Transport | During transfer, communication is significantly impaired due to PPE and physical barriers. |
|
| Post-transport | After reaching the destination, the patient expresses emotional exhaustion and stress. |
|
Table 2. Fictitious clinical case illustrating nursing interventions across the phases of biocontainment transport.

Figure 1. Conceptual flowchart illustrating nursing diagnoses, interventions (NIC), outcomes (NOC), assessment tools and practical applications across the phases of biocontainment transport.
DISCUSSION
The aim of this study is to develop and propose an innovative structured nursing model designed to address both the clinical and psychological needs of conscious and communicative patients undergoing biocontainment transport. As mentioned in the introduction, most of the literature currently published focuses on the organizational, logistical and technological aspects of the transfer to biocontainment rather than offering organized and systematic nursing care models. Since it incorporates nursing diagnoses, interventions, and expected outcomes based on the NANDA-I, NIC, and NOC taxonomies, the model offered here represents an original contribution in this context. It provides a theoretical and practical approach focused on the psychological, communicative, and relational needs of conscious and communicative patients throughout the entire transfer process. This model is a novel idea that can be validated and applied in high-complexity care settings because of its attention to care detail, taxonomic clarity, and clinical application. The structured model developed highlights how each phase of biocontainment transfer presents specific and distinct care needs. The systematic approach to managing pre-transfer anxiety, maintaining effective communication during transport, and providing psychological support after transfer underscores the need for personalized and coordinated interventions.
The integration of nursing diagnoses, NOC outcomes, and NIC interventions enables the construction of a comprehensive care response that addresses not only clinical aspects but also emotional and relational dimensions.
The impact of biocontainment on patient-provider communication is particularly significant [3,5].
The use of PPE and isolating devices presents real obstacles and requires well-planned alternative strategies to prevent further emotional deterioration.
Finally, the post-transport phase is often underestimated but can be a critical moment for the patient to process the experience. Strengthening coping skills and promoting resilience not only improve clinical outcomes but also enhance the patient’s overall care experience [21].
Limitation
This theoretical nursing care model was developed through the integration of taxonomy and expert consensus, without direct patient involvement.
The implementation and effectiveness in real clinical settings have not yet been evaluated; future studies should be structured to assess the outcomes related to its application through quantitative measurements and subsequent evaluations in biocontainment transfer settings.
Such investigations will be essential to refine the model and confirm its clinical relevance and utility.
The proposed nursing care model can be practically applied in various high-complexity clinical settings, such as infectious disease units, intensive care units, and specialized medical transport services for highly infectious patients.
To validate the model’s effectiveness, the systematic collection of clinical data before and after the biocontainment transfer is recommended. Among the possible assessment tools, the GAD-7 scale may be used for anxiety, the Brief COPE Inventory for coping strategies, and the CD-RISC-10 for resilience levels. In cases of limited verbal communication, the use of structured observational checklists and AAC (Augmentative and Alternative Communication) tools can provide reliable alternative measurements.
The analysis of collected data may include descriptive statistics and inferential tests to compare pre- and post-intervention conditions. These strategies will allow for measuring the model’s impact on key care outcomes and refining its applicability for potential structured implementation in the future.
CONCLUSIONS
The management of patients in biocontainment requires a strategic combination of clinical and communication skills to address the nursing diagnoses that emerge throughout the three phases of transfer. By applying structured care models, it is possible to improve clinical outcomes, reduce biological risks, and ensure effective communication even in extreme isolation conditions. The integration of protocols and nursing interventions provides an effective solution to the demands of complex and highly specialized care. Although the efficiency of the suggested model has not yet been confirmed in practical situations, it constitutes a substantial theoretical advance to the nursing management of biocontainment transfers. In order to confirm its practical application and quantify its observable advantages on important care outcomes, pilot projects and prospective studies should be started and carried out in real care situations. The model's robustness can only be verified and its organized adoption encouraged by means of rigorous testing
Ethical Approval
For this study, no formal approval from the Local Ethics Committee was required.
Conflicts of Interest and Funding Sources
The authors declare that they have no conflicts of interest related to this work. The study received no financial support from public or private entities, including pharmaceutical or industrial companies.
Authors’ Contributions
Federico D’Urso: conceived the study, developed the care model, and coordinated the writing of the manuscript. Salvatore Trifiletti: contributed to the organization of the NANDA-I, NIC, and NOC framework. Edoardo Falcone: participated in literature review and content refinement. Mara Gracy Basile: contributed to methodological structure and theoretical validation. Ulrico Angeloni: revised and validated the entire study and ensured its clinical and theoretical consistency. All authors read and approved the final version of the manuscript.
Acknowledgments
The authors would like to thank the staff of the Italian Red Cross – Public Health Department for their continuous support and collaboration in developing the proposed model. Special thanks also to the academic community for the critical reflection that inspired the elaboration of this work.
REFERENCES
Gibbs, S. G., Herstein, J. J., Le, A. B., Beam, E. L., Cieslak, T. J., Lawler, J. V., Santarpia, J. L., Stentz, T. L., Kopocis-Herstein, K. R., Achutan, C., Carter, G. W., & Lowe, J. J. (2019). Review of Literature for Air Medical Evacuation High-Level Containment Transport. Air medical journal, 38(5), 359–365. HYPERLINK "https://doi.org/10.1016/j.amj.2019.06.006"https://doi.org/10.1016/j.amj.2019.06.006
D’Urso, F., Meroni, L., Rech, R., Musumeci, A., Bonini, A., Piotti, C., Ciriaci, A. and Menghini, S. (2024) “Possible care protocols for patients undergoing road transfer on a biocontainment stretcher model N 36 (36 m3 air ˃60 ACH)”, Emergency Care Journal, 20(3). doi: 10.4081/ecj.2024.12334.
Rehn, M., Heyerdahl, F., Osbakk, S. A., Andresen, Å. E., & Hagemo, J. (2023). Challenges and Risks in Out-of-Hospital Transport of Patients During the Coronavirus Disease 2019 Pandemic. Air medical journal, 42(3), 191–195. HYPERLINK "https://doi.org/10.1016/j.amj.2023.02.002"https://doi.org/10.1016/j.amj.2023.02.002
Garibaldi, B. T., Conger, N. G., Withers, M. R., Hatfill, S. J., Gutierrez-Nunez, J. J., & Christopher, G. W. (2019). Aeromedical Evacuation of Patients with Contagious Infections. Aeromedical Evacuation: Management of Acute and Stabilized Patients, 317–335. HYPERLINK "https://doi.org/10.1007/978-3-030-15903-0_20"https://doi.org/10.1007/978-3-030-15903-0_20
Aengst, J., Walker-Stevenson, G., Harrod, T., Ivankovic, J., Neilson, J., & Guise, J. M. (2022). Uncomfortable yet necessary: The impact of PPE on communication in emergency medicine. International journal for quality in health care: journal of the International Society for Quality in Health Care, 34(4), mzac095. HYPERLINK "https://doi.org/10.1093/intqhc/mzac095"https://doi.org/10.1093/intqhc/mzac095
Corradi, M., Cattaneo, A., Plicco, C., & Bossi, E. (2021). HTA of novel biocontainment systems for ambulance transport: public health implications. The European Journal of Public Health, 31(Suppl 3), ckab165.132. HYPERLINK "https://doi.org/10.1093/eurpub/ckab165.132"https://doi.org/10.1093/eurpub/ckab165.132
Flinn, J. B., Hynes, N. A., Sauer, L. M., Maragakis, L. L., & Garibaldi, B. T. (2021). The role of dedicated biocontainment patient care units in preparing for COVID-19 and other infectious disease outbreaks. Infection control and hospital epidemiology, 42(2), 208–211. HYPERLINK "https://doi.org/10.1017/ice.2020.451"https://doi.org/10.1017/ice.2020.451
Saunders, G. H., Jackson, I. R., & Visram, A. S. (2021). Impacts of face coverings on communication: an indirect impact of COVID-19. International journal of audiology, 60(7), 495–506. HYPERLINK "https://doi.org/10.1080/14992027.2020.1851401"https://doi.org/10.1080/14992027.2020.1851401
Costello, J.M. (2000). AAC intervention in the intensive care unit: The children's hospital Boston model. Augmentative and Alternative Communication, 16, 137 - 153.
Zaylskie, L. E., Biggs, E. E., Minchin, K. J., & Abel, Z. K. (2024). Nurse perspectives on supporting children and youth who use augmentative and alternative communication (AAC) in the pediatric intensive care unit. Augmentative and alternative communication (Baltimore, Md.: 1985), 40(4), 255–266. HYPERLINK "https://doi.org/10.1080/07434618.2023.2284269"https://doi.org/10.1080/07434618.2023.2284269
Ten Hoorn, S., Elbers, P. W., Girbes, A. R., & Tuinman, P. R. (2016). Communicating with conscious and mechanically ventilated critically ill patients: a systematic review. Critical care (London, England), 20(1), 333. HYPERLINK "https://doi.org/10.1186/s13054-016-1483-2"https://doi.org/10.1186/s13054-016-1483-2
Beam, E.L., Boulter, K.C., Freihaut, F., Schwedhelm, S. and Smith, P.W. (2010), The Nebraska Experience in Biocontainment Patient Care. Public Health Nursing, 27: 140-147. HYPERLINK "https://doi.org/10.1111/j.1525-1446.2010.00837.x"https://doi.org/10.1111/j.1525-1446.2010.00837.x
Swickard, S., Swickard, W., Reimer, A., Lindell, D., & Winkelman, C. (2014) Adaptation of the AACN Synergy Model for Patient Care to Critical Care Transport. Crit Care Nurse, 34(1),16–28. doi: 10.4037/ccn2014573.
Sánchez-Almagro, C. P., Romero-Sánchez, J. M., White-Ríos, M., González Del Pino, C. A., & Paloma-Castro, O. (2022). NANDA International nursing diagnoses in the coping/stress tolerance domain and their linkages to Nursing Outcomes Classification outcomes and Nursing Interventions Classification interventions in the pre-hospital emergency care. Journal of advanced nursing, 78(10), 3273–3289. HYPERLINK "https://doi.org/10.1111/jan.15280"https://doi.org/10.1111/jan.15280
Villarreal-Zegarra, D., Paredes-Angeles, R., Mayo-Puchoc, N. et al. Psychometric properties of the GAD-7 (General Anxiety Disorder-7): a cross-sectional study of the Peruvian general population. BMC Psychol 12, 183 (2024). https://doi.org/10.1186/s40359-024-01688-8
Ganesan S, Balasubramanian B, Krishnamurthy P, Govindan R, Mani N. Effects of Tele-Counseling on Reducing Anxiety Levels of COVID-19 Patients in Isolation Wards: An Observational Study. Indian Journal of Psychological Medicine. 2022;45(1):43-46. doi:10.1177/02537176221139598
Solberg, M. A., Gridley, M. K., & Peters, R. M. (2022). The Factor Structure of the Brief Cope: A Systematic Review. Western journal of nursing research, 44(6), 612–627. HYPERLINK "https://doi.org/10.1177/01939459211012044"https://doi.org/10.1177/01939459211012044
Kuiper, H., van Leeuwen, C. C. M., Stolwijk-Swüste, J. M., & Post, M. W. M. (2019). Measuring resilience with the Connor-Davidson Resilience Scale (CD-RISC): which version to choose?. Spinal cord, 57(5), 360–366. HYPERLINK "https://doi.org/10.1038/s41393-019-0240-1"https://doi.org/10.1038/s41393-019-0240-1
Dias, P., Clerc, D., da Rocha Rodrigues, M. G., Demartines, N., Grass, F., & Hübner, M. (2022). Impact of an Operating Room Nurse Preoperative Dialogue on Anxiety, Satisfaction and Early Postoperative Outcomes in Patients Undergoing Major Visceral Surgery-A Single Center, Open-Label, Randomized Controlled Trial. Journal of clinical medicine, 11(7), 1895. HYPERLINK "https://doi.org/10.3390/jcm11071895"https://doi.org/10.3390/jcm11071895
Haugan, G., & Drageset, J. (2014). The hospital anxiety and depression scale--dimensionality, reliability and construct validity among cognitively intact nursing home patients. Journal of affective disorders, 165, 8–15. https://doi.org/10.1016/j.jad.2014.04.042
Ocloo, J., Garfield, S., Franklin, B. D., & Dawson, S. (2021). Exploring the theory, barriers and enablers for patient and public involvement across health, social care and patient safety: a systematic review of reviews. Health research policy and systems, 19(1), 8. HYPERLINK "https://doi.org/10.1186/s12961-020-00644-3"https://doi.org/10.1186/s12961-020-00644-3
Madl, J. E. M., Sturmbauer, S. C., Janka, R., Bay, S., & Rohleder, N. (2022). Preparing patients according to their individual coping style improves patient experience of magnetic resonance imaging. Journal of behavioral medicine, 45(6), 841–854. HYPERLINK "https://doi.org/10.1007/s10865-022-00361-y"https://doi.org/10.1007/s10865-022-00361-y
Wallace L. M. (1986). Communication variables in the design of pre-surgical preparatory information. The British journal of clinical psychology, 25 (Pt 2), 111–118. HYPERLINK "https://doi.org/10.1111/j.2044-8260.1986.tb00679.x"https://doi.org/10.1111/j.2044-8260.1986.tb00679.x
Caddick, J., Jawad, S., Southern, S., & Majumder, S. (2012). The power of words: sources of anxiety in patients undergoing local anaesthetic plastic surgery. Annals of the Royal College of Surgeons of England, 94(2), 94–98. HYPERLINK "https://doi.org/10.1308/003588412X13171221501267"https://doi.org/10.1308/003588412X13171221501267
![]() This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.