Knowledge, perceptions and practices associated with timing for breast cancer screening among female students at the University of Zimbabwe: A cross-sectional study
Peter Chikuvadze1, Grace Nkhoma2, Maxwell Mhlanga3*, Augustine Ndaimani4
1,2 Department of Nursing Science, University of Zimbabwe, Harare, Zimbabwe
3 Centre of Gender Equity, University of Global Health, Kigali, Rwanda
4 Centre for Nursing and Midwifery, University of Global Health, Kigali, Rwanda
*Corresponding Author: Maxwell Mhlanga, Centre of Gender Equity, University of Global Health Equity, Kigali, Rwanda. E-mail: mmhlanga@ughe.org
Cite this article
ABSTRACT
Background: Breast cancer remains one of the leading causes of cancer-related mortality among women globally. Early detection through screening is crucial for improving outcomes. However, knowledge gaps, misconceptions, and poor practices around screening timing persist among young women. This study explores the knowledge, perceptions, and practices related to breast cancer screening among female students at the University of Zimbabwe. It aims to inform nursing practice by highlighting the critical role nurses play in addressing these gaps through education, awareness, and guidance on screening timing.
Methods: This analytical cross-sectional study employed random sampling to recruit participants at the University of Zimbabwe from March 4 to April 8. A structured questionnaire with three sections, consisting of closed-ended questions, was used to assess demographic characteristics, as well as knowledge, perceptions, and practices related to breast cancer screening. Data were analyzed using STATA 15, with descriptive statistics presented in tables and figures. Associations between variables were tested using Chi-square, Fisher’s exact tests, and binary logistic regression.
Results: Of the 139 participants, 85% were aged 20-25, single, and undergraduates. Among all age groups, 54% did not perform breast self-examinations. Participants aged 36-40 had significantly higher odds of late screening (OR=17.8, p=0.014) and married participants also had higher odds of later screening (OR=4.42, p=0.009) compared to single participants. Participants who perceived that a healthy diet reduces breast cancer risk had lower odds of late screening (OR=0.32, p=0.021). Participants who knew the recommended age of Breast Self-Examination had higher odds of late screening (OR=2.5, p=0.027). Participants with religious and cultural beliefs influencing their decision-making were significantly more likely to present late (OR = 3.21, p = 0.030).
Conclusion: Socio-demographic factors and health-seeking behaviors significantly influenced breast cancer screening timing. Nurses are pivotal in promoting early screening through tailored health promotion strategies, including raising awareness, addressing misconceptions, and encouraging self-examination practices.
Keywords: Breast cancer, screening, Breast self-examination, Knowledge, Perceptions, Nursing.
INTRODUCTION
Globally, breast cancer remains a significant public health concern as the most prevalent cancer and a leading cause of cancer-related deaths [1]. While incidence rates are higher in developed countries, mortality rates are disproportionately higher in developing countries due to delayed diagnosis and limited access to healthcare services [1, 2]. Early detection through regular screening significantly improves survival rates, making it a critical component of cancer control strategies [3].
Sub-Saharan Africa is experiencing a growing burden of non-communicable diseases, including cancer.
In Zimbabwe, breast cancer ranks among the most common cancers, second only to cervical cancer in mortality rates [4]. Late-stage presentation is prevalent, with over one in four cancers diagnosed among Zimbabwean women being breast cancer [5]. Contributing factors include limited access to diagnostic equipment, low awareness levels, and sociocultural barriers [6]. Additionally, most patients rely on underfunded public health services, which are often inaccessible and expensive, further exacerbating late detection [7].
The onset of breast cancer in Zimbabwe occurs as early as 18 years of age, with incidence increasing significantly among women aged 40 years and older [8]. Despite recommendations for routine screening, including mammography and clinical breast examinations, many women only seek care at advanced stages of the disease [5]. Breast self-examination (BSE) is often the most accessible screening method in low-resource settings, where diagnostic services like mammography are scarce [9]. However, adherence to regular BSE practices is low due to limited knowledge, misconceptions, and cultural influences [10]. Nurses play a unique role in alerting the community to early breast cancer diagnosis, as they typically have the closest contact with female patients [11]. Nurses can use their knowledge of health services to educate women about breast cancer risk factors and available breast cancer screening services and practices [12].
University students represent a unique population within the broader breast cancer risk group, as
they often encounter specific challenges such as lack of awareness, limited healthcare access, and sociocultural factors that may delay early screening [13]. Understanding the knowledge, perceptions, and practices of young women in higher education settings regarding breast cancer screening is crucial for designing targeted interventions.
This study measured the individual knowledge, perceptions, and practices related to breast cancer screening timing among female students at the University of Zimbabwe.
This was an analytical cross-sectional study conducted between March 4 and April 8, 2024, in Harare, Zimbabwe.
Study Setting
The study was conducted at the University of Zimbabwe, located in the capital city, Harare, within Harare Metropolitan Province. Harare is Zimbabwe's economic, political, and cultural hub, with a population exceeding two million people. The University, the oldest and largest institution of higher learning in the country, serves a diverse student population from various socio-economic backgrounds. Female students constitute a significant portion of the student body, offering a valuable demographic for studying breast cancer screening knowledge, perceptions, and practices.
Study Population
All female students enrolled at the University of Zimbabwe aged between 20 and 45 years, with good knowledge of the English language and who agreed to participate in the study were included in the study. All students who had completed their education, were <20 years or >45 years old or did not speak English were excluded. Before the start of the study, the students who agreed to
participate were explained the purpose of the study and were asked to sign the informed consent.
Sample Size Determination
A minimum sample size of 126 participants was calculated using Cochran’s formula for cross-sectional studies:
![]()
where:
- Z is the Z-value for a 95% confidence level (1.96),
- p is the estimated proportion of unawareness of breast self-examination (9%, or 0.09, as reported by Kinteh et al. in 2023 [14]),
- e is the margin of error (5%, or 0.05).
Recruitment Process
Participants were recruited through simple random sampling. Eligible students randomly selected either a “Yes” or “No” card from a container. Those who picked “Yes” cards were enrolled in the study until the required sample size was reached.
Measurement
A single structured questionnaire was used to collect data on factors associated with late presentation for breast cancer screening. The questionnaire comprised three sections. The first section captured participant characteristics, including age, religion, place of residence, and socio-economic background. The section on knowledge and practices assessed participants’ knowledge of breast cancer signs and symptoms, the recommended age for breast self-examination (BSE), and proper BSE techniques. It included eight items scored using a Likert scale. The last section examined factors affecting screening behaviors, such as cultural beliefs, financial constraints, healthcare access, and personal perceptions. The section comprised seven items with responses on a Likert scale.
This tool was closed-ended structured questionnaire that was adapted from three previous studies [15-17]. To ensure clarity, relevance, and validity, the instrument was pre-tested with 16 female students at the University of Zimbabwe who shared characteristics with the target population. Feedback from the pilot study informed minor revisions to improve clarity.
The internal consistency of the tool was evaluated using Cronbach’s alpha, which yielded a reliability coefficient of 0.74, indicating acceptable reliability [18].
Data Collection
Data were collected over 28 weekdays during the study period. Participants completed a self-administered online structured questionnaire. Trained research assistants were available to address any technical difficulties or questions related to the survey.
Ethical Considerations
The study received ethical approval from the Joint Research Ethics Committee of Parirenyatwa Group of Hospitals and the University of Zimbabwe Faculty of Medicine and Health Sciences (JREC Ref 247/2024). Written informed consent was obtained from all participants before enrollment. Confidentiality was maintained by anonymizing participant data, and access was restricted to authorized researchers.
Data Analysis
Data were entered into STATA version 15 for analysis. Descriptive statistics summarized the characteristics of the study population, presented in tables. The chi-square test or Fisher’s exact test, where appropriate, was used to determine associations between categorical variables. Bivariate logistic regression identified predictors of late breast cancer screening, reporting odds ratios (OR), 95% confidence intervals (CI), and p-values. All tests were two-sided, and considered significant if p-value (p) was less than 0.05.
Socio-demographic characteristics of participants and timing for breast cancer screening
Among the 139 participants, the majority (85%) were aged 20–25 years, 4% were aged 26–30 years, 5% were aged 31–35 years, 3% were aged 36–40 years, and 4% were aged 41–45 years. Late presentation for screening was more prevalent among participants aged 36–40 years and age was significantly associated with late presentation timing (p = 0.001) (Table 1).
Most participants were single (84%), followed by married participants (12%), divorced (3%), and widowed (1%). Single participants had the highest proportion of early screenings, whereas 41.2% of married individuals presented late for screening. Marital status was significantly associated with screening timing (p = 0.006) (Table 1).
Pentecostal participants formed the largest religious group (53%), followed by Apostolics and those with no religion (13% each), Protestants (12%), adherents of traditional religion (7%), and finally, Muslims (1%). Late presentation was most pronounced among participants practicing traditional religion and Protestantism, although there was no significant association between religion and late screening (Table 1).
The majority of participants were undergraduates (93%), followed by master's students (7%). Late screening was more prevalent among master's students. However, no significant association was found between the level of study and the timing of screening. The majority of participants resided off-campus (81%), and 17.7% of this group presented late, compared to 19.2% of those residing on campus. However, there was no significant association between place of residence and timing for
screening (Table 1).
| Variable | Category | “Presented late” (No) | “Presented late” (Yes) | Total n (%) | p-value (test) |
| Age | 20-25 | 101 | 17 | 118 (84.9%) | 0.001* (F) |
| 26-30 | 3 | 2 | 5 (3.6%) | ||
| 31-35 | 6 | 1 | 7 (5.0%) | ||
| 36-40 | 1 | 3 | 4 (2.9%) | ||
| 41- 45 | 3 | 2 | 5 (3.6%) | ||
| Marital status | Married | 10 | 7 | 17 (12.2%) | 0.006* (F) |
| Single | 101 | 16 | 117 (84.2%) | ||
| Widowed | 0 | 1 | 1 (0.7%) | ||
| Divorced | 3 | 1 | 4 (2.9%) | ||
| Religion | Pentecostal | 63 | 10 | 73 (52.5%) | 0.48 (F) |
| Protestant | 12 | 5 | 17 (12.2%) | ||
| Islam | 2 | 0 | 2 (1.4%) | ||
| Traditional | 6 | 3 | 9 (6.5%) | ||
| Apostolic | 15 | 4 | 19 (13.4%) | ||
| None | 16 | 3 | 19 (13.4%) | ||
| Level of study | Undergraduate | 108 | 21 | 129 (92.8%) | 0.08 (F) |
| Masters | 6 | 4 | 10 (7.2%) | ||
| Resident on campus | No | 93 | 20 | 113 (81.2%) | 0.78 (F) |
| Yes | 21 | 5 | 26 (18.8%) | ||
| *=Significant,
F= Fisher’s exact test |
|||||
Table 1. Socio-demographic characteristics of the study participants (n=139)
Knowledge of breast cancer and timing late for breast cancer screening
Only knowledge on the recommended age to start BSE (p = 0.027), was associated with timing for breast cancer screening (Table 2).
| Variable | Category | “Presented late” (No) | “Presented late” (Yes) | Total n (%) | p-value (test) |
| Perceived knowledge on breast cancer | Poor | 21 | 3 | 24(17.3%) | 0.76 (F) |
| Fair | 72 | 14 | 86(61.9%) | ||
| Good | 18 | 7 | 25(18.0%) | ||
| Excellent | 3 | 1 | 4(2.9%) | ||
| Total | 114 | 25 | 139(100.0%) | ||
| Educated on breast cancer | No | 42 | 6 | 48(34.5%) | 0.32 (C) |
| Yes | 72 | 19 | 91(65.5%) | ||
| Total | 114 | 25 | 139(100.0% | ||
| Knowledge of signs and symptoms | Low | 27 | 5 | 32(23.0%) | 0.89 (C) |
| High | 87 | 20 | 107(77.0%) | ||
| Total | 114 | 25 | 139(100.0%) | ||
| BSE | Regularly | 13 | 4 | 17(12.2%) | 0.76 (F) |
| Occasionally | 31 | 14 | 45(32.4%) | ||
| No | 70 | 7 | 77(55.4%) | ||
| Total | 114 | 25 | 139(100.0%) | ||
| Knowledge of recommended age to start BSE | No | 87 | 13 | 100(71.9%) | 0.027* (C) |
| Yes | 27 | 12 | 39(28.1%) | ||
| Total | 114 | 25 | 139(100.0%) | ||
| Knowledge on how to perform BSE | No | 89 | 15 | 104(74.8%) | 0.10 (C) |
| Yes | 25 | 10 | 35(25.2%) | ||
| Total | 114 | 25 | 139(100.0%) | ||
| *=Significant,
C= Chi square test F= Fisher’s exact test |
|||||
Table 2. Knowledge of breast cancer and timing for breast cancer screening
Perceptions, other risk factors and late screening breast cancer
Significant associations were found between late screening and the perception that a healthy diet reduces breast cancer risk (p = 0.011), with those who believed this being less likely to present late. Similarly, those who did not perceive Breast Self-Exams (BSE) as uncomfortable were also less likely to present late (p = 0.019). Religious and cultural beliefs were significantly associated with late presentation (p = 0.014). Overall, perceptions and beliefs played a crucial role in the timing of screening (Table 3).
| Variable | Category | “Presented late” (No) | “Presented late” (Yes) | Total n (%) | p-value (test) |
| Perception that health diet reduces risk of Breast cancer | No | 26 | 12 | 38(27.3%) | 0.011* (C) |
| Yes | 88 | 13 | 101(72.7%) | ||
| Total | 114 | 25 | 139(100.0%) | ||
| Perception that BSE is uncomfortable | No | 61 | 5 | 66(88.0%) | 0.019* (F) |
| Yes | 6 | 3 | 9(12.0%) | ||
| Total | 67 | 8 | 75(100.0%) | ||
| Family history of breast cancer | No | 96 | 17 | 113(81.3%) | 0.06 (C) |
| Yes | 18 | 8 | 26(18.7%) | ||
| Total | 114 | 25 | 139(100.0%) | ||
| Religious and cultural beliefs | No | 97 | 16 | 113(81.3%) | 0.014* (C) |
| Yes | 17 | 9 | 26(18.7%) | ||
| Total | 114 | 25 | 139(100.0%) | ||
| Fear of stigma | No | 108 | 21 | 129(92.8%) | 0.06 (C) |
| Yes | 6 | 4 | 10(7.2%) | ||
| Total | 114 | 25 | 139(100.0%) | ||
| *=Significant,
C= Chi square test F= Fisher’s exact test |
|||||
Table 3. Perceptions, other risk factors and timing for breast cancer screening
Factors associated with late presentation of breast with breast cancer
Women aged 36–40 years had significantly higher odds of late breast cancer screening compared to those aged 20–25 years (OR=17.82, 95% CI: [1.75–181.61], p=0.014). Married individuals were significantly more likely to present late for screening (OR = 4.42, 95% CI: [1.46–13.40], p = 0.009*). Participants who knew the recommended age for BSE had significantly higher odds of late screening (Crude OR = 2.15, 95% CI: [1.11–4.14], p = 0.027), suggesting that knowledge alone may not translate into timely screening behavior (Table 4).
Those perceiving a healthy diet as reducing breast cancer risk had significantly lower odds of late screening (OR = 0.32, 95% CI: [0.13–0.79], p = 0.021), highlighting a protective association. Participants who found BSE uncomfortable had higher odds of presenting late for screening (OR = 6.10, 95% CI: [1.16–32.05], p = 0.076), though the association was not statistically significant. Participants with religious and cultural beliefs influencing their decision-making were significantly more likely to present late (OR = 3.21, 95% CI: [1.22–8.43], p = 0.030).
In summary, significant factors for late breast cancer screening include age, marital status, perceptions about health and BSE, and religious or cultural beliefs, highlighting the complex interplay of demographic and psychosocial factors in screening behavior.
| Variable | Presented
Late (Yes) |
Presented
Late (No) |
Crude
Odds Ratio |
95% Confidence Interval | P-value (test) |
| Age | |||||
| 20-25 | 17 | 101 | 1.00 (ref) | - | - |
| 26-30 | 2 | 3 | 3.96 | [0.62 - 25.10] | 0.14 |
| 31-35 | 1 | 6 | 0.99 | [0.11- 8.961] | 0.99 |
| 36-40 | 3 | 1 | 17.82 | [1.75-181.61] | 0.014* |
| 41-45 | 2 | 3 | 3.96 | [0.62 - 25.10] | 0.14 |
| Marital status | |||||
| Single | 16 | 101 | 1.00 (ref) | - | - |
| Married | 7 | 10 | 4.42 | [1.46 - 13.40] | 0.009* |
| Widowed | 1 | 0 | - | - | - |
| Divorced | 1 | 3 | 2.11 | [0.20 - 21.98] | 0.53 |
| Knowledge of recommended age for BSE | |||||
| No | 13 | 87 | 1.00 (ref) | - | - |
| Yes | 12 | 27 | 2.15 | [1.11- 4.14] | 0.027* |
| Perception that healthy diet reduces Breast cancer | |||||
| No | 26 | 12 | 1.00 (ref) | - | - |
| Yes | 18 | 13 | 0.32 | [0.13 - 0.79] | 0.021* |
| Perception that BSE is uncomfortable | |||||
| No | 61 | 5 | 1.00 (ref) | - | - |
| Yes | 6 | 3 | 6.10 | [1.16 - 32.05] | 0.08 |
| Religious and cultural belief | |||||
| No | 16 | 97 | 1.00 (ref) | - | - |
| Yes | 9 | 17 | 3.21 | [1.22 – 8.43] | 0.030* |
Table 4. Factors associated with late screening for breast cancer (n=139)
This study investigated factors associated with late presentation for breast cancer screening among female students at the University of Zimbabwe.
Age was significantly associated with delayed screening, with women aged 36–40 years showing higher odds of late presentation compared to those aged 20–25 years. Similar trends have been observed in Ghana, where younger women were more likely to attend routine screenings due to targeted health promotion campaigns [19]. In contrast, older women in South Africa exhibited misconceptions about breast cancer, perceiving it as a disease primarily affecting younger populations [19]. However, studies by Moodley et al. indicate that younger women may also delay screening due to fear of diagnosis and limited awareness [20, 21]. These variations suggest that access to health information and sociocultural norms play a pivotal role in shaping health-seeking
behavior across age groups.
Married women were more likely to delay screening, consistent with findings in Nigeria, where familial responsibilities and reliance on spouses for financial decisions contributed to delays [22]. Conversely, single women in Kenya demonstrated higher screening uptake, likely due to greater autonomy in decision-making [23]. Cultural expectations and economic dependence within marriage may similarly hinder timely health-seeking behaviors among married women in Zimbabwe.
Surprisingly, knowledge of the recommended age for breast self-examination (BSE) was associated with late screening in this study. This finding diverges from evidence in Tanzania, where knowledge of BSE facilitated earlier screening [24]. In Ethiopia, however, limited awareness led to symptom misinterpretation and delayed care [25]. These discrepancies highlight the complexity of translating knowledge into action, suggesting that barriers such as stigma, fear, or healthcare access may undermine the benefits of awareness.
Perceptions about diet and cancer prevention were linked to lower odds of late screening, aligning with findings from Egypt, where women with dietary knowledge were more proactive in seeking screening [26]. These results underscore the importance of lifestyle education in encouraging early detection behaviors [27].
Cultural and religious beliefs were also significant barriers to timely screening. In Uganda, reliance on spiritual healing delayed early detection [28]. Similarly, some religious practices in Zimbabwe emphasize prayer over medical interventions [29]. Such beliefs strongly influence healthcare decisions, as observed in other studies [30, 31]. Addressing these barriers through community engagement and collaboration with faith leaders could improve screening uptake.
Overall, this study highlights the multifaceted factors influencing late presentation for breast cancer
screening among female students in Zimbabwe. Targeted interventions addressing sociocultural,
informational, and lifestyle barriers are critical for promoting early detection practices.
Implications
The finding that 18% of participants presented late for breast cancer screening, with only 54% performing BSE, is concerning. There is a need to intensify nursing-led social behavior change approaches that use differentiated methods to promote sexual and reproductive health services in tertiary institutions. Early screening initiatives for reproductive cancers should be prioritized.
Targeted screening and awareness campaigns for female students aged 36-40 years should be implemented, alongside promotion of regular BSE as key nursing interventions. Tailored educational materials and support groups for single students can raise awareness about the importance of early detection. This is where community nursing and nursing outreach programs play a vital role in health promotion and social behaviour change communication. Nursing outreach programs targeting tertiary institutions in Zimbabwe should integrate comprehensive education on BSE techniques, the importance of regular screenings, and the benefits of early detection. Collaboration with cultural and religious organizations to disseminate accurate health information and support students influenced by negative beliefs could be helpful.
Limitations of the Study
Reliance on self-reported data regarding student behaviors may lead to overestimation of actual practices due to social desirability bias.
The university-based survey methodology excluded students who were not attending classes or were absent during the survey period; their BSE practices might differ from those who participated. Additionally, the limited sample size and focus on a single university (monocentricity) may affect the generalizability of the findings.
CONCLUSION
This study identified socio-demographic factors, health-seeking behaviors, practices, and perceptions significantly associated with late presentation for breast cancer screening among female students at the University of Zimbabwe. Future nursing health promotion and education programs should adopt differentiated, targeted approaches to increase the success of interventions, improve early detection rates, and encourage simple practices like BSE for effective early breast cancer screening.
Ethics considerations.
Ethics issues have been completely observed by authors.
Funding
The study was not externally funded.
Conflict of Interest
The authors declare that there is no conflict of interest.
Acknowledgements
We extent our gratitude to the University of Zimbabwe for all the support.
Authors’ Contributions
Conceptualization: P.C. and G.N; methodology: P.C. and M.M.; software: P.C. and M.M; validation: P.C, G.N, M.M. and A.N.; statistical analysis: M.M., and A.N.; investigation: P.C.; resources: P.C. and G.N.; data curation: P.C. and M.M.; writing- original draft preparation: P.C.; writing-review and editing: G.N.; M.M and A.N; visualisation: M.M.; supervision: G.N.; projection administration: P.C.; funding acquisition: N/A. All authors have read and agreed to the published version of the manuscript.
REFERENCES
- Sha, R., Kong, Xm., Li, Xy. et al.(2024). Global burden of breast cancer and attributable risk factors in 204 countries and territories, from 1990 to 2021: results from the Global Burden of Disease Study 2021. Biomark Res 12, 87. doi: https://doi.org/10.1186/s40364-024-00631-8
- American Cancer Society. Breast Cancer (2023). Breast self-examination guidelines. Available at: https://www.cancer.org/cancer/types/breast-cancer/screening-tests-and-early-detection/american-cancer-society-recommendations-for-the-early-detection-of-breast-cancer.html. Last access: 16 October 2024.
- World Health Organization. IARC, GLOBACAN (2021). Available at: http://globocan.iarc.fr/factsheets/cancers/breast.asp. Last accessed November 2024.
- Obikunle, A.F., Ade-Oshifogun, B. (2022). Perspectives of African American women about barriers to breast cancer prevention and screening practices: A qualitative study. Afr J Reprod Health. 2022 Jul;26(7):22-28. doi: 10.29063/ajrh2022/v26i7.3.
- Abo Al-Shiekh, S.S., Alajerami, Y.S., Abushab, K.M., Najim, A.A., AlWaheidi, S., Davies, E.A. (2022). Factors affecting delay in the presentation of breast cancer symptoms among women in Gaza, occupied Palestinian territory: a cross-sectional survey. BMJ Open. 12(10):e061847. doi: 10.1136/bmjopen-2022-061847.
- Alsaraireh, A., Darawad, M.W. (2018). Breast cancer awareness, attitude and practices among female university students: A descriptive study from Jordan. Health Care Women Int.;39(5):571-583. doi: 10.1080/07399332.2017.1368516.
- Sung, H., Ferlay, J., Siegel, R.L., Laversanne, M., Soerjomataram, I., Jemal, A., Bray, F. (2021). Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin.1(3):209-249. doi: 10.3322/caac.21660.
- Siegel, R.L., Miller, K.D., Wagle, N.S., Jemal, A. Cancer statistics, 2023. CA Cancer J Clin. 2023. 73(1):17-48. doi: 10.3322/caac.21763.
- Ramathuba, D.U., Ratshirumbi, C.T.., Mashamba, T.M. (2015). Knowledge, attitudes and practices toward breast cancer screening in a rural South African community. Curationis.;38(1):1172. doi: 10.4102/curationis.v38i1.1172.
- Cancer in Zimbabwe. Zimbabwe National Cancer Registry 2022 Annual Report. Available at: https://www.afro.who.int/sites/default/files/202308/WHO%20Zimbabwe%20Annual%20Report%202022%20.pdf. Accessed July 2024.
- Abu Awwad, D., Hossain, S. Z., Mackey, M., Brennan, P., & Adam, S. (2021). Optimising awareness and knowledge of breast cancer screening for nurses through train-the-trainer workshops. Journal of Cancer Education, 1-11.
- McCready, T., Littlewood, D., & Jenkinson, J. (2005). Breast self‐examination and breast awareness: a literature review. Journal of clinical nursing, 14(5), 570-578.
- Magara, M.S., Mungazi, S.G., Gonde, P., Nare, H., Mwembe, D., Madzikova, A., Chagla, L.S., Pereira, J., McKirdy, M.J., Narayanan, S., Grimsey, L., Hicks, J., James, R., Rainsbury, R.M. (2023). Factors leading to the late diagnosis and poor outcomes of breast cancer in Matabeleland South and the Bulawayo Metropolitan Provinces in Zimbabwe. PLoS One. 18(11):e0292169. doi: 10.1371/journal.pone.0292169.
- Kinteh, B., Kinteh, S.L.S, Jammeh, A., Touray, E., Barrow, A. (2023). Breast Cancer Screening: Knowledge, Attitudes, and Practices among Female University Students in The Gambia. Biomed Res Int. 2023 Nov 30;2023:9239431. doi: 10.1155/2023/9239431.
- Ayoub N. M., Al-Taani G. M., Almomani B. A., et al. (2021). Knowledge and practice of breast cancer screening methods among female community pharmacists in Jordan: a cross-sectional study. International Journal of Breast Cancer . 2021:13. doi: 10.1155/2021/9292768.9292768
- Abo Al-Shiekh S. S., Ibrahim M. A., Alajerami Y. S. Breast cancer knowledge and practice of breast self-examination among female university students, Gaza. The Scientific World Journal . 2021;2021:7. doi: 10.1155/2021/6640324.6640324
- Ramya Ahmad S., Asmaa Ahmad A., Nesreen Abdullah A., et al. Awareness Level, Knowledge and Attitude towards Breast Cancer between Medical and Non-Medical University Students in Makkah Region: A Cross Sectional Study. International Journal of Cancer and Clinical Research . 2019;6(1) doi: 10.23937/2378-3419/1410106.
- Seyedkanani, E., Hosseinzadeh, M., Mirghafourvand, M., Sheikhnezhad, (2024). Breast cancer screening patterns and associated factors in Iranian women over 40 years. Sci Rep. 2024 Jul 3;14(1):15274. doi: 10.1038/s41598-024-66342-0.
- Opoku, S.Y., Benwell, M., Yarney, (2012). Knowledge, attitudes, beliefs, behaviour and breast cancer screening practices in Ghana, West Africa. Pan Afr Med J. 2012;11:28. Epub 2012 Feb 17. PMID: 22514762; PMCID: PMC3325066.
- Faryabi, R., Daneshi, S., Davarani, E.R., Yusefi, A.R., Arabpour, M., Ezoji, K., Movahed, E., Daneshi-Maskooni, M., Hussaini, S.M. (2023). The assessment of risk factors and risk perception status of breast cancer in Northern Iran. BMC Womens Health. 2023 May 16;23(1):268. doi: 10.1186/s12905-023-02422-z.
- Hassen, A.M., Hussien, F.M., Asfaw, Z.A., Assen, H.E. (2021). Factors Associated with Delay in Breast Cancer Presentation at the Only Oncology Center in North East Ethiopia: A Cross-Sectional Study. J Multidiscip Healthc. 2021 Mar 19;14:681-694. doi: 10.2147/JMDH.S301337.
- Okobia, M.N., Bunker, C.H., Okonofua, F.E., Osime, (2006). Knowledge, attitude and practice of Nigerian women towards breast cancer: a cross-sectional study. World J Surg Oncol. 2006 Feb 21;4:11. doi: 10.1186/1477-7819-4-11.
- Antabe, R., Kansanga, M., Sano, Y. et al.(2020). Utilization of breast cancer screening in Kenya: what are the determinants?. BMC Health Serv Res 20, 228 (2020). https://doi.org/10.1186/s12913-020-5073-2
- Zewdie, A., Kassie, T.D., Anagaw, T.F. et al. (2024).Advanced-stage breast cancer diagnosis and its determinants in Ethiopia: a systematic review and meta-analysis. BMC Women's Health 24, 284. https://doi.org/10.1186/s12905-024-03133-9
- Gebremariam, A., Dereje, N., Addissie, A., Worku, A., Assefa, M., Abreha, A., Tigeneh, W., Pace, L.E., Kantelhardt, E.J., Jemal, (2021). Factors associated with late-stage diagnosis of breast cancer among women in Addis Ababa, Ethiopia. Breast Cancer Res Treat. 2021 Jan;185(1):117-124. doi: 10.1007/s10549-020-05919-5.
- Akpinar,Y.Y., Baykan, Z., Naçar, M., Gün, I, Çetinkaya, (2011). Knowledge, attitude about breast cancer and practice of breast cancer screening among female health care professionals: a study from Turkey. Asian Pac J Cancer Prev. 2011;12(11):3063-8. PMID: 22393990.
- Kinteh, B., Kinteh, S.L.S., Jammeh, A., Touray, E., Barrow, (2023). Breast Cancer Screening: Knowledge, Attitudes, and Practices among Female University Students in The Gambia. Biomed Res Int. 2023 Nov 30;2023:9239431. doi: 10.1155/2023/9239431
- Galukande, M., Wabinga, H., Mirembe, F., Karamagi, C., Asea, (2016). Breast Cancer Risk Factors among Ugandan Women at a Tertiary Hospital: A Case-Control Study. Oncology. 90(6):356-62. doi: 10.1159/000445379.
- Elmore, S.N.C., Mushonga, M., Iyer, H.S., Kanda, C., Chibonda, S., Chipidza, F., Makunike Mutasa, R., Muchuweti, D., Muguti, E.G., Maunganidze, A., Ndlovu, N., Bellon, J.R., Nyakabau, A.M. (2021). Breast cancer in Zimbabwe: patterns of care and correlates of adherence in a national referral hospital radiotherapy center cohort from 2014 to 2018. Cancer Med. 2021 Jun;10(11):3489-3498. doi: 10.1002/cam4.3764.
- Sambanje, M.N., Mafuvadze, (2012). Breast cancer knowledge and awareness among university students in Angola. Pan Afr Med J.11:70. Epub 2012 Apr 16. PMID: 22655104; PMCID: PMC3361208.
- Al-Biatty, S., Salih, E., Alamin, S., Altoom, N., Babeker, R., Gnawi, O. (2020). Knowledge, attitude and practice of breast self-examination in Khartoum State, Sudan. Clin Med (Lond). 20(Suppl 2):s2-s3. doi: 10.7861/clinmed.20-2-s2.
![]() This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Nurses and pain management in territorial health emergencies: a retrospective study
Federico Pecetta 1, Gian Domenico Giusti 2,3*, Sara Staffaroni 4, Matteo Ricci 5
- Department of Emergency Medicine, Emergency Health Operations Centre Arezzo, San Donato Hospital, Arezzo, Italy
- Department Teaching and Quality, Hospital of Perugia, Perugia, Italy
- Department of Medicine and Surgery of the University of Perugia, Perugia, Italy
- Department of Maternal and Child Health, San Donato Hospital, Arezzo, Italy
- Department of Anaesthesia and Critical Care Careggi University Hospital, University of Florence, Florence, Italy
* Corresponding author: Gian Domenico Giusti, Department of Medicine and Surgery of the University of Perugia, Piazza Lucio Severi, 1 Edificio B - piano +1 - 06132 Perugia, Italy. ORCID: https://orcid.org/0000-0001-9167-9845. Email: giandomenico.giusti@unipg.it.
Cite this article
ABSTRACT
Introduction: Numerous studies show that the prevalence of pain in pre-hospital emergency setting ranges from 20% to 53%. Additionally, the scientific literature reveals a prevalence of moderate-to-severe pain in 20-64% of patients. According to the latest guidelines, it is essential to ensure proper and effective pain management for all patients experiencing pain. Inadequate pain management can result in complications such as delayed recovery and increased patient distress. In pre-hospital setting, emergency nurses are capable of assessing and treating pain using medications such as fentanyl, ketamine, morphine, NSAIDs and paracetamol.
Objective: To evaluate the assessment and treatment of pain by emergency nurses in the pre-hospital setting and assess the potential need for additional training in accordance with the Tuscany region for nurse-staffed ambulances’ analgesia procedure guidelines.
Methods: Retrospective study of 4,738 pre-hospital interventions from September 2022 to September 2023. Data were retrieved from EmMaWeb system and included pain assessment using the Numeric Rating Scale (NRS) and administration of analgesics.
Results: Pain was assessed at least once in 98.3% of the cases. Moderate to severe pain (NRS ≥ 4) was recorded in 14.2% of the patients. Analgesic drugs were administered in 63.6% of patients with NRS ≥ 4, yet the Tuscany region for nurse-staffed ambulances’ analgesia procedure guidelines was not followed in 36.4% of these cases. 79% of the findings with NRS ≥ 7 (severe pain) received analgesic drug treatment. Paracetamol was the most commonly used analgesic, followed by fentanyl, morphine, and ketamine.
Conclusions: Pain assessment practices are well-established in pre-hospital care, but there is still room for improvement in pain management.
Pain management does not comply with the Guidelines set by the World Health Organisation and the European Society of Emergency Medicine, a substantial proportion of patients experiencing moderate to severe pain did not receive adequate analgesia.
This highlights the need for additional education and training for pre-hospital nurses in pain management and the effective use of analgesic medications to ensure greater adherence to the treatment protocols for nurse-staffed ambulance shared within the Tuscany Region.
Keywords: Pain management, Emergency nurses, Pre-hospital care, Analgesic drugs, Pain assessment
INTRODUCTION
Emergency Nurse can take on the role of Team Leader in a healthcare rescue team during severe criticality or clinical instability situations, even without the immediate presence of medical staff [1].
In the Italian healthcare system, where nursing protocols and algorithms for evaluation and treatment are adopted, it is increasingly common for nurses to apply their skills to achieve better results and ensure the success of the rescue operations [2,3].
One of the key interventions is the accurate assessment of pain, followed by rapid and appropriate treatment [4]. When conducted in and out-of-hospital setting, proper pain assessment can improve rescue interventions, representing a standard of quality and a marker of progress in Emergency Medicine [5,6]. Several studies indicate that the prevalence of acute pain in pre-hospital emergency medicine varies between 20% and 53%. [7-11]. Scientific literature also reveals a prevalence of moderate to severe pain in 20–64% of cases [7,8,12]. According to the latest guidelines, it is essential to ensure proper and effective pain management for all patients experiencing pain, starting from the pre-hospital emergency phase. The primary goal is to reduce pain, maintain functionality, and minimise adverse effects [13]. The WHO pain relief scale serves as a comprehensive guide for managing pain. The Numerical Rating Scale (NRS) is the most commonly used pain scale for assessing pain in adult patients within the pre-hospital setting [14].
The NRS can be administered either verbally or in written form. In both formats, patients are asked to rate the intensity of their pain on an 11-point scale, ranging from 0 (no pain) to 10 (worst pain imaginable [15,16]. Pain is considered mild with a score of 1-3, moderate with a score of 4-7, and severe with a score greater than 7 [17].
To improve the management of acute pain, continuous and accurate assessment is recommended. For adults and children capable of verbalising their pain, the NRS and VAS scales are recommended [14].
In Europe, the personnel involved in emergency and urgent healthcare consists of various roles: nurses, paramedics, and doctors. These roles have different levels of education, training, and job specifications, which can influence their ability and authority to administer analgesics to patients in pain [18-20]. The choice of the most effective analgesic depends on various factors, such as the context in which it is administered, the skills of the staff, and the guidelines provided by the WHO ladder [21]. The pharmacological options recommended by the European Society of Emergency Medicine (EUSEM) in accordance with the WHO pain relief ladder include: paracetamol, NSAIDs, opioids, and ketamine [14]. In Italy, scientific societies involved in emergency care have issued recommendations on pain management. According to guidelines, in pre-hospital setting, the ideal analgesic should be simple to use, safe, effective, not to interfere with transport time and have a rapid onset and short half-life to allow for dose titration based on the patient's response [22].
Severe pain in a pre-hospital setting is often poorly and inadequately managed, with the use of analgesic drugs by healthcare professionals reported to be insufficient [23-25].
Nurses can assess and treat pain using drugs such as fentanyl, ketamine, morphine, NSAIDs, and paracetamol [22]. The effectiveness and safety of administering these drugs has been further confirmed by the 2023 recommendations for pain management in pre-hospital settings.
Pharmacological treatment with non-opioid analgesics, such as NSAIDs, Paracetamol, and Ketamine, is a viable alternative to opioid drugs, offering similar efficacy and a more favourable side effect profile [26]. Fentanyl is a rapid and effective analgesic treatment that does not cause significant hypotension, reduction in peripheral oxygen saturation (SpO2) and state of consciousness, therefore, it can be used safely and effectively for pain management in pre-hospital settings [27].
In addition, the safety of Ketamine in low-dose administration was demonstrated with no significant decrease in blood pressure, respiratory rate, heart rate and GCS, and no clinically significant negative events were reported [28]. Numerous studies provide evidence for the safety and efficacy of low-dose (0.1-0.3 mg/kg) Ketamine, whether administered intravenously, intramuscularly, or intranasal. Its use leads to rapid pain relief and causes fewer adverse effects, such as nausea and vomiting, compared to opioids, though it is associated with dizziness, dysphoria, and confusion [29-32].
In the context of prehospital emergency care in the Tuscany Region, various types of basic and advanced rescue vehicles are available: nurse-staffed ambulances, emergency physician cars, basic life support ambulances, and air ambulances. Regarding nurse-staffed ambulances, pain assessment and management are performed by nurses following the Regional Analgesia Procedure.
Pain assessment is performed using the NRS (Numerical Rating Scale), VRS [https://www.fisioscience.it/scale-valutazioni/scala-vrs/]
PAINAD (Pain Assessment in Advanced Dementia), FACES (Faces Pain Scale) and FLACC (Face, Legs, Activity, Cry, Consolability) scales.
The procedure includes the use of analgesic medications based on pain intensity:
- Paracetamol for pain intensity of 4-6
- Ketamine and Morphine for pain intensity ≥ 7
- Fentanyl is used by the operators of the Arezzo Emergency Medical Operations Centre following the implementation of the regional analgesia procedure.
This study was designed to evaluate nursing practices in pain management during pre-hospital care. Specifically, it aims to analyse adherence to international guidelines and the implementation of the Regional Analgesia Protocol by nursing staff affiliated with the Emergency Medical Operations Centre in Arezzo.
Objective:
The main objective of this study is to assess how the territorial emergency nurse evaluates and treats pain. The specific objectives are:
- To verify whether nurses assess pains by completing the relevant section in the rescue report and/or in the patient card filled out by the operational centre operators.
- To determine if a pain assessment with NRS ≥ 4 (moderate to severe pain) leads to appropriate pharmacological treatment.
- To identify the potential need for further training on pain management and analgesic treatment, in accordance with the Tuscany region for nurse-staffed ambulance’s analgesia procedure guidelines.
MATERIALS AND METHODS
A retrospective study was conducted on pain management by nurses on Advanced Life Support vehicles operated by the Local Health Authority of South-East Tuscany, one of the main healthcare providers in Central Italy, at the Emergency Medical Services Dispatch Centre in Arezzo. The regional analgesia procedure guidelines for nurse-staffed ambulances has been used by the healthcare authority.
The advanced life support vehicles involved in the study within the pre-hospital emergency care setting include:
- Ambulances staffed with qualified nurses trained to perform clinical procedures for pain assessment and management.
During pre-hospital care, healthcare professionals complete a standardised emergency care form.
This form includes information about the patient's physical condition, such as pain intensity rated on a 0-10 Numerical Rating Scale (NRS), the type of event, and the pre-hospital triage colour code.
The NRS is a widely recognised pain assessment tool where 0 represents no pain and 10 represents the worst possible pain. For the pharmacological treatment of pain, a Regional Procedure is in place for nurse-staffed ambulances, allowing the administration of analgesic drugs based on the severity of the pain:
- Moderate pain (NRS: 4–6):
- Intravenous Paracetamol up to 15 mg/kg intravenous in children.
- Paracetamol 1 gr in adults.
- In cases of post-traumatic pain, Methoxyflurane is administered via pre-dosed inhalation.
- Severe pain (NRS≥ 7):
- Intravenous Ketamine 0.2-0.5 mg/kg after prior consultation with the dispatch centre physician via telephone.
- Ketamine intramuscular 0.5-1 mg/kg if venous access is not available.
- Intravenous morphine in children: 0.05 mg/kg
- Intravenous morphine for adult patients under 65 years of age: 4 mg (repeatable with 2 mg).
- Intravenous morphine for adult patients over 65 years of age: 2 mg, repeatable with 1 mg if necessary.
The period covered by the study was from 1 September 2022 to 30 September 2023.
Data were extracted from the EmMaWeb (Emergency Management Web) database used by Arezzo Emergency Medical Service Operative Centre, which includes the "rescue report" filled out by the nurse on board and the "patient card" filled by the healthcare personnel at Emergency Medical Service Operative Centre. The data were accessed using an Excel spreadsheet and selected based on the defined inclusion criteria. To achieve the study’s objective, the following outcomes were evaluated:
- At least one recorded pain score using the pain scale.
- Presence and intensity of pain.
- Adherence to the Regional Analgesia Procedure for Advanced Life Support ambulances with a nurse for the pharmacological treatment of pain.
Inclusion Criteria
- All patients assisted, with no age restrictions.
- Emergency medical care administered by nurses on board ambulances.
- Pre-hospital Emergency Care forms dated between 1 September 2022, and 30 September 2023.
- All pre-hospital colour codes for the dispatch of the rescue vehicle and its return to the destination hospital.
Exclusion Criteria
- Pre-hospital emergency care provided by non-healthcare professionals in non-advanced life support vehicles.
- Pre-hospital emergency care delivered by Medical Cars.
Statistical analysis
Data was extracted from the EmMaWeb (Emergency Management Web) database using the MISEMMA program. Data were collected and analysed to describe the distribution of pain based on intensity levels. The categorical variables were presented as simple and cumulative frequencies, as well as percentages. Additionally, a 95% confidence interval (CI 95%) was provided.
A hypothesis test was conducted as an inferential procedure using a z-test for proportions to evaluate whether the frequency of moderate-to-severe pain observed differed significantly from the lower limit of the expected frequency reported in the literature. Furthermore, the p-value was calculated, with a significance level set at <0.05. For the data analysis, Microsoft 365 Excel version 2411 was used.
Ethical consideration
This study constitutes an integral component of the nursing thesis carried out by the first author, supervised by the second author at the second level degree in Nursing Science, University of Perugia. The thesis was submitted for approval on 24 November 2023.
No formal approval by the Local Ethics Committee (LEC) was required for this study; moreover, as by internal guidelines of LEC, the study has obtained necessary approval from the Directorate General of Local Health Authority Tuscany South-East ('Arezzo' Hospital) (18 September 2023).
All clinical data used in this investigation were acquired in a coded and anonymised format, adhering rigorously to the principles and guidelines outlined in the General Data Protection Regulation (2016/679, ‘GDPR’), which encompasses regulations concerning data protection and privacy within the European Union.
Furthermore, the study complies with the tenets of the Privacy Code (Italian legislative decrees 196/2003 and 101/2018) and the study protocol was designed in accordance with Good Clinical Practice, and the study was conducted in accordance with the Declaration of Helsinki.
RESULTS
During the selected period (September 2022 to September 2023), 4,738 rescue interventions were carried out by ambulances with nurses on board (Figure 1).
The number of interventions is related to the extent of the territorial coverage Emergency Medical Service Nurses (in Italian “INDIA”), population density, and whether the territorial emergency medical service provides 24-hour or 12-hour coverage.
In 4,658 out of 4,738 cases (98.3%), pain was recorded at least once by the nurse in the rescue report and/or in the patient card completed by the operations centre staff, while it was not recorded in 80 cases (1.7%). Among the 80 patients whom no pain recording was found, 17 patients (0.37%) still received analgesic treatment.
Pain assessments with NRS (Numerical Rating Scale) ≥ 4 (moderate to severe pain) accounted for 14.2% (n= 660), while those with NRS (Numerical Rating Scale) ≤ 3 (no to mild pain) represented 85.8% (n= 3,998).
Out of the total pain assessments performed (4,658), severe pain (NRS ≥ 7) was observed in 4.30% of cases (n = 200) [95% confidence interval (CI): 3.71–4.87], moderate pain (6 ≥ NRS ≥ 4) in 9.87% of cases (n = 460) [95% CI: 9.01–10.73], while absent or mild pain (NRS ≤ 3) accounted for 85.83% of cases (n = 3998) [95% CI: 84.83–86.83] (Figure 1).
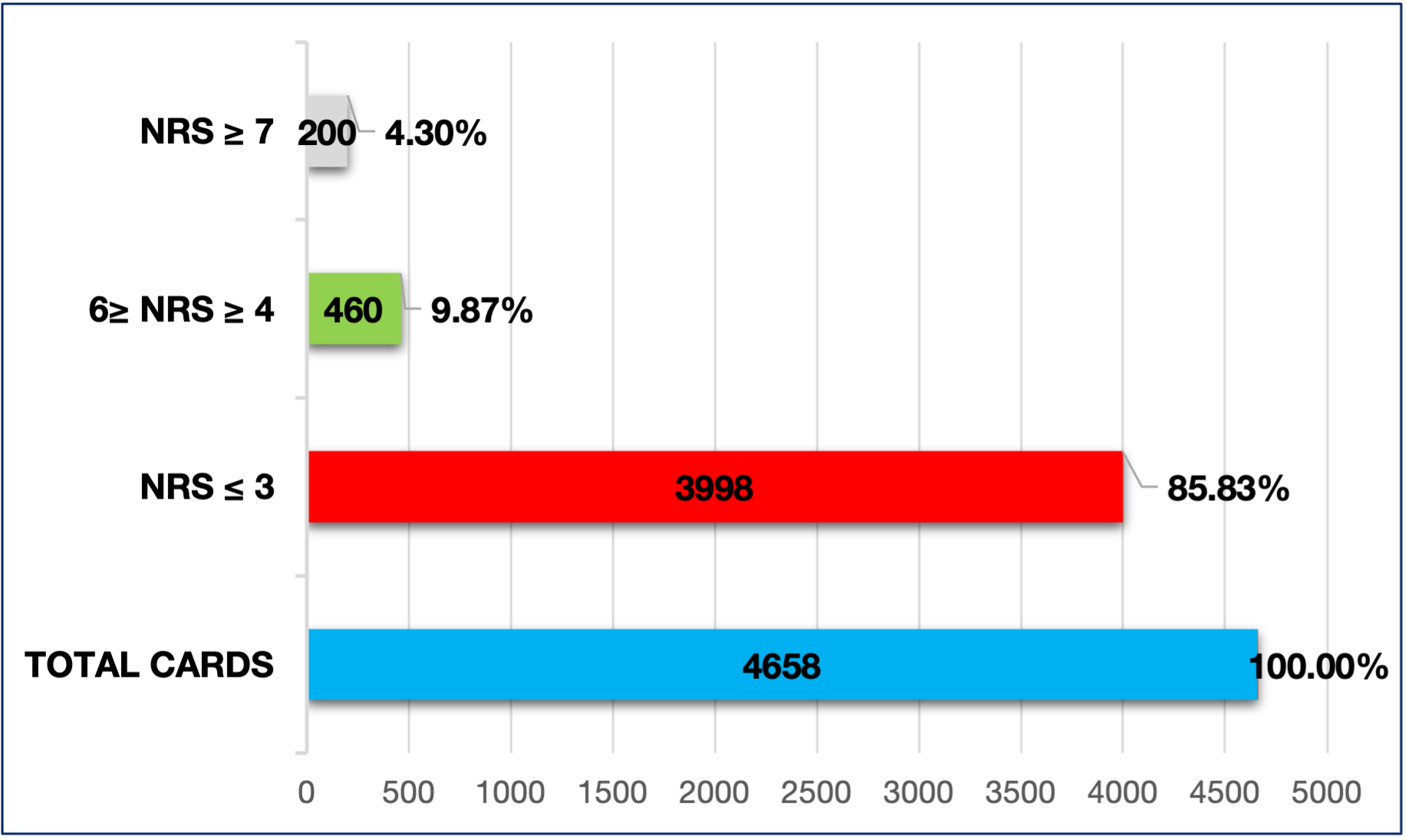 Figure 1. Number of measurements with NRS (Numerical Rating Scale) ≤ 3 (no pain and mild pain); 6 ≥ NRS (Numerical Rating Scale) ≥ 4 (moderate pain), and NRS (Numerical Rating Scale) ≥ 7 (severe pain) on total cards.
Figure 1. Number of measurements with NRS (Numerical Rating Scale) ≤ 3 (no pain and mild pain); 6 ≥ NRS (Numerical Rating Scale) ≥ 4 (moderate pain), and NRS (Numerical Rating Scale) ≥ 7 (severe pain) on total cards.
Cumulative frequency
Total of measurements with NRS (Numerical Rating Scale) between 0 and 10 were 4,658, those with absent or mild pain (NRS ≤ 3) 3,998 (85.83%). The findings with absent-mild-moderate pain (NRS ≤ 6) were 4,458 (95.70%) (Figure 2).
To assess whether the observed frequency of pain with NRS ≥ 4 (moderate-severe) at 14.2% significantly differs from the lower limit of the expected frequency reported in the literature (20%), a z-test for proportions was conducted on a sample of 4,658 subjects.
The null hypothesis (H₀) posits that the observed proportion is equal to the expected proportion, while the alternative hypothesis (H₁) asserts that the observed proportion is lower than the expected proportion.
The z-test for proportions yielded a value of -9.90, indicating that the observed proportion (14.2%) is significantly below the expected proportion (20%). The associated p-value is extremely close to 0, well below the significance threshold (p-value < 0.05).
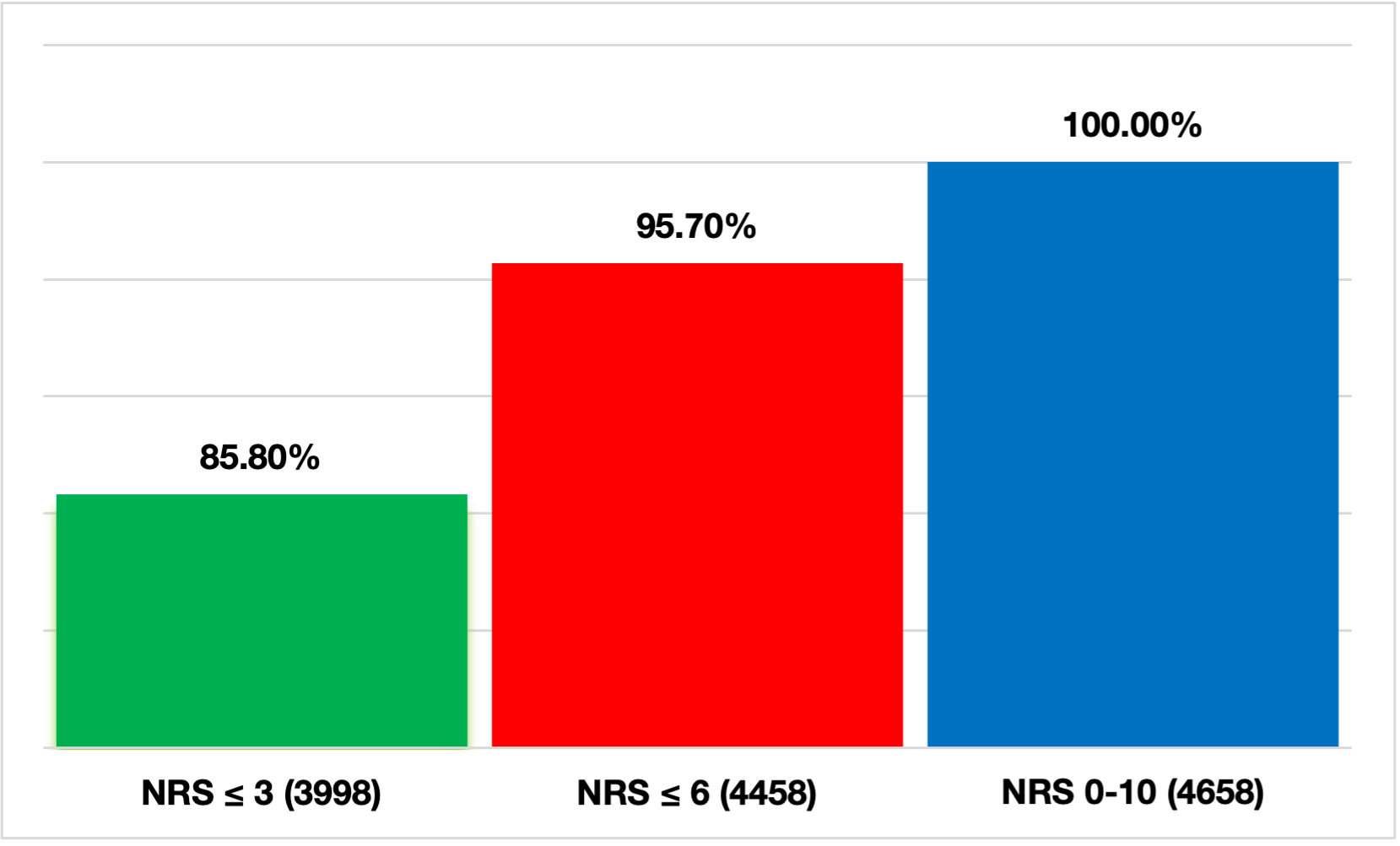 Figure 2. Representation of the cumulative frequency divided by the number and percentages of pain measurements with NRS (Numerical Rating Scale) ≤ 3 (no pain and mild pain), NRS (Numerical Rating Scale) ≤ 6 (no pain, mild pain, moderate pain), and NRS (Numerical Rating Scale) 0-10 (no pain, mild pain, moderate pain, severe pain).
Figure 2. Representation of the cumulative frequency divided by the number and percentages of pain measurements with NRS (Numerical Rating Scale) ≤ 3 (no pain and mild pain), NRS (Numerical Rating Scale) ≤ 6 (no pain, mild pain, moderate pain), and NRS (Numerical Rating Scale) 0-10 (no pain, mild pain, moderate pain, severe pain).
Analgesic drugs were administered following a pain assessment NRS ≥ 4 in 63.6% of cases (420 out of 660 assessments), while the procedure was not applied in 240 cases (36.4%).
Following a pain assessment with NRS ≥ 7 (severe pain), the analgesia procedure was applied in 79% of cases (n = 158), while it was not applied in the remaining 21% of patients (n = 42).
It was highlighted in the study, when pain intensity, as reported by the patient, decreased to a NRS between 4 and 6, there was a significant drop in number of analgesic treatments administered: 262 out of 460 cases (57%) received treatment, while 43% (198 out of 460) did not receive any.
As regard of analgesic drug usage, both NRS ≤ 3 and NRS ≥ 4, paracetamol was the most commonly administered drug (815 cases), followed by fentanyl (181), morphine (102), and ketamine (94) (Table 1).
| FENTANYL | KETAMINE | MORPHINE | PARACETAMOL | |
| INDIA 1 | 5 | 1 | 1 | 1 |
| INDIA 2 | 26 | 10 | 35 | 128 |
| INDIA 3 | 24 | 14 | 4 | 97 |
| INDIA 4 | 13 | 11 | 4 | 61 |
| INDIA 5 | 14 | 9 | 4 | 52 |
| INDIA 6 | 47 | 25 | 27 | 194 |
| INDIA 7 | 23 | 17 | 17 | 125 |
| INDIA 8 | 6 | 3 | 0 | 49 |
| INDIA 9 | 15 | 3 | 10 | 64 |
| INDIA 10 | 8 | 1 | 0 | 44 |
| TOTALE | 181 (15.2%) | 94 (7.9%) | 102 (8.5%) | 815 (68.4%) |
Table 1. Total number of drugs administered for NRS (Numerical Rating Scale) ≤ 3 and NRS ≥ 4 by Advanced Life Support ambulances staffed with nurses (INDIA).
DISCUSSION
The data shows a high level of awareness about pain, as it was assessed at least once in more than 98% of patients.
Only 1.7% of the examined forms lacked of pain assessment, a significantly better result compared to other studies reported in the literature, where the percentage ranges from 32% to 52% [8,12,20].
The recording of pain data during pre-hospital emergency, as recommended by the European Society of Emergency Medicine (EUSEM) guidelines and constitutes the first step towards effective pain management [13]. An accurate assessment of the patient and their pain symptoms is essential for selecting the appropriate analgesic and determining the most suitable route of administration [22].
A proper pain assessment can significantly enhance emergency care interventions, establishing it as one of the key quality standards in emergency medicine [5,6].
There were 17 out of 80 cases where no pain score was recorded, but patients still received pharmacological analgesic treatment.
For cases where no pain score was documented, several factors could explain this: some patients likely did not experience pain, while in other cases, patients may have had pain, but the data was not recorded for various reasons. This underscores the importance of thorough documentation to ensure accurate pain management practices [12].
From the analysed data, it is clear that about 36% of patients with NRS ≥ 4 (moderate-severe pain) and 21% of patients with NRS ≥ 7 (severe pain) did not receive analgesic treatment.
Numerous studies prove that inadequate pain management is common in pre-hospital Emergency-Urgency setting [33,34]. In another study, only 15.6% of all activations documented the receipt of pre-hospital pain medications [35]. One hypothesis related to 40% of moderate to severe pain cases left untreated by nurses could be from a lack of confidence in using the available analgesic drugs.
From the data examined, the occurrence of pain with NRS ≥ 4 (moderate-severe) is greatly reduced (14.2%) if compared to the 20-64% reported in the medical literature [7,8,12].
The z-test value for proportions, which is highly negative, confirms that the observed proportion of moderate-to-severe pain (14.2%) is significantly below the lower limit of the expected range (20%). The value observed in this study is statistically lower than the expected range reported in the literature, supporting the conclusion that the collected data differs significantly from expectations. Given that the p-value is extremely close to zero, we can reject the null hypothesis that the observed distribution of moderate-to-severe pain is equal to the expected distribution.
Regarding the use of analgesic drugs, paracetamol appears to be the most frequently used medication for both NRS ≥ 4 and NRS ≤ 3 pain levels, suggesting nurses are more comfortable with its use and titration, compared to the lower usage of fentanyl, ketamine, and morphine.
The widespread use of intravenous paracetamol is supported by the recommendations of the “Evidence-Based Guidelines for Pre-Hospital Pain Management”. Compared to the exclusive use of intravenous opioids for the initial management of moderate to severe pain, paracetamol is highlighted for its ease of administration and higher tolerability among patients. This makes it a preferred option in pre-hospital settings where effective, yet patient-friendly analgesic interventions are critical. [26]
In other studies, morphine and fentanyl have been the most commonly administered drugs for pain management [35]. A growing need of a better training on how to use painkiller drug is urgent, in particular about the benefits of a valid analgesia. It’s important, especially in certain provincial areas under the responsibility of Advanced Life Support ambulances with a nurse on board (INDIA), which were found to be less consistent in using analgesic drugs relative to the number of rescue interventions performed.
CONCLUSION
Acute pain is widely documented as one of the most common symptoms experienced by patients in the context of emergency and urgent care. This symptom is frequently encountered in pre-hospital settings, highlighting the importance of effective pain management during emergency interventions. [8,36]. According to Mackenzie, pain should be controlled from the very beginning, immediately after the arrival of emergency services: “The pre-hospital care professional has the first and perhaps the only opportunity to interrupt the pain cascade.” This emphasises the crucial role that early intervention plays in managing pain effectively during emergency care [37].
Early and effective pain treatment has a positive impact on both the physiological and psychological condition of patients. It improves comfort and safety, facilitates complex life-support interventions, and, in the long term, reduces the development of post-traumatic stress disorder (PTSD) [23,38-40].
The recently concluded study provides a realistic snapshot of the management of pre-hospital emergencies handled by the Emergency Medical Operations Centre of Arezzo.
The objectives of the study were met, demonstrating that Emergency Medical Service nurses pay considerable attention to assess and treat pain in patients seeking assistance.
63,6% of patients with moderate to severe pain (NRS ≥ 4) received pharmacological treatment through the application of the Tuscany region for nurse-staffed ambulances’ analgesia procedure guidelines. Pain management, however, does not align with the guidelines set by the World Health Organisation (WHO) and the European Society of Emergency Medicine (EUSEM) [14], a significant proportion of patients with moderate-severe pain did not receive adequate analgesia.
Nevertheless, the study also highlights the need for a further training to raise awareness about the benefits of analgesia. However, the study suggests a need for further education and training for pre-hospital nurses on pain management and the use of analgesic drugs to ensure greater adherence to shared treatment protocols within the Tuscany Region. It would be ideal for personnel working in the emergency and urgent care system to undergo a uniform training path, while maintaining their respective competencies, professional scopes, and specific foundational training for each role. The overall goal is to ensure quality care through the functional and operational integration of each sector within the emergency and urgent healthcare system. [41] Nonetheless, the adoption of the assessment and treatment nursing protocols for assessment at the regional level, including the Analgesia Protocol, represents a positive step towards the standardisation of care.
Study limitations:
The main limitation is the data which were collected from a single Emergency Medical Service Operative Centre.
Data regarding the sex, age, and medical conditions of patients treated by Advanced Life Support ambulances with a nurse on board were not collected. Additionally, the lack of pain assessment prevents us from determining whether this omission was due to a genuine absence of pain evaluation or a failure to record the pain, even though it may have been assessed.
Further investigation is needed using the collected data through a direct review of each individual rescue report, in order to establish the reasons of inapplicable regional analgesia procedure guidelines, despite the patient's reported pain being classified as moderate to severe.
Funding statement
This research did not receive any specific grant from funding agencies in the public, commercial, or non-profit sectors.
Conflict of interest
The authors report no conflict of interest.
Authors’ contribution
F.P.: Conceptualisation, Methodology, Investigation, Software Data curation, Writing-Original draft preparation. G.d.G.: Writing - Reviewing and Editing, Supervision. S.S.: Writing- Reviewing and Editing. M.R.: Writing- Reviewing and Editing.
Acknowledgements
We would like to thank the Medical and Nursing Management of the Department of Emergency Medicine of Local Health Authority South-East Tuscany for allowing us to study inside the COES Arezzo.
REFERENCES
- Yamaguchi Y, Matsunaga-Myoji Y, Fujita K. Advanced practice nurse competencies to practice in emergency and critical care settings: A scoping review. Int J Nurs Pract. 2024 Aug;30(4):e13205. https://doi.org/10.1111/ijn.13205
- Mazzolini, E., Garrino, L., & Calabrò, P. (2006). Integration of nursing staff into Medical Emergency Service 118. Emergency Care Journal, 2(4), 29–35. https://doi.org/10.4081/ecj.2006.4.29
- Campo TM, Comer A, Dowling Evans D, Kincaid K, Norton L, Ramirez EG, et al. Practice Standards for the Emergency Nurse Practitioner Specialty. Adv Emerg Nurs J. 2018 Oct/Dec;40(4):240-245. https://doi.org/10.1097/TME.0000000000000209
- Whitley, G. A., Wijegoonewardene, N., Nelson, D., Curtis, F., Ortega, M., & Siriwardena, A. N. (2023). Patient, family member, and ambulance staff experiences of pre-hospital acute pain management in adults: A systematic review and meta-synthesis. Journal of the American College of Emergency Physicians open, 4(2), e12940. https://doi.org/10.1002/emp2.12940
- Studnek JR, Fernandez AR, Vandeventer S, Davis S, Garvey L. The association between patients' perception of their overall quality of care and their perception of pain management in the pre-hospital setting. Prehosp Emerg Care. 2013 Jul-Sep;17(3):386-91. https://doi.org/10.3109/10903127.2013.764948.
- Ariès P, Montelescaut E, Pessey F, Danguy des Déserts M, Giacardi C. Pre-hospital emergency medicine: pain control. Lancet. 2016 Feb 20; 387(10020):747. https://doi.org/10.1016/S0140-6736(16)00325-1.
- Galinski M, Ruscev M, Gonzalez G, Kavas J, Ameur L, Biens D, et al. Prevalence and management of acute pain in pre-hospital emergency medicine. Prehosp Emerg Care. 2010 Jul-Sep;14(3):334-9. https://doi.org/10.3109/10903121003760218.
- McLean SA, Maio RF, Domeier RM. The epidemiology of pain in the pre-hospital setting. Prehosp Emerg Care. 2002 Oct-Dec;6(4):402-5. doi: 10.1080/10903120290938021.
- Ricard-Hibon A, Leroy N, Magne M, Leberre A, Chollet C, Marty J. Evaluation de la douleur aiguë en médecine préhospitalière. Ann Fr Anesth Reanim. 1997;16(8):945-9. French. doi: 10.1016/s0750-7658(97)82142-9.
- Lord B, Cui J, Kelly AM. The impact of patient sex on paramedic pain management in the pre-hospital setting. Am J Emerg Med. 2009 Jun;27(5):525-9. doi: 10.1016/j.ajem.2008.04.003.
- Milojevic K, Cantineau JP, Simon L, Bataille S, Ruiz R, Coudert B, et al. Douleur aiguë intense en médecine d'urgence. Les clefs d'une analgésie efficace. Ann Fr Anesth Reanim. 2001 Nov;20(9):745-51. French. doi: 10.1016/s0750-7658(01)00482-8.
- Friesgaard KD, Riddervold IS, Kirkegaard H, Christensen EF, Nikolajsen L. Acute pain in the pre-hospital setting: a register-based study of 41.241 patients. Scand J Trauma Resusc Emerg Med. 2018;26(1):53. doi:10.1186/s13049-018-0521-2
- Hachimi-Idrissi S, Dobias V, Hautz WE, Leach R, Sauter TC, Sforzi I, et al., Approaching acute pain in emergency settings; European Society for Emergency Medicine (EUSEM) guidelines-part 2: management and recommendations. Intern Emerg Med. 2020 Oct;15(7):1141-1155. Epub 2020 Sep 15. doi: 10.1007/s11739-020-02411-2.
- Guidelines for the management of acute pain in emergency situations, EUSEM (European Society of Emergency Medicine) 2020. Last accessed: November 20, 2024. Available at: https://www.eusem.org/images/EUSEM_EPI_GUIDELINES_MARCH_2020.pdf
- Breivik H, Borchgrevink PC, Allen SM, Rosseland LA, Romundstad L, Hals EK, et al., Assessment of pain. Br J Anaesth. 2008 Jul;101(1):17-24. Epub 2008 May 16. doi: 10.1093/bja/aen103.
- Downie WW, Leatham PA, Rhind VM, Wright V, Branco JA, Anderson JA. Studies with pain rating scales. Ann Rheum Dis. 1978 Aug;37(4):378-81. doi: 10.1136/ard.37.4.378.
- Hartrick CT, Kovan JP, Shapiro S. The numeric rating scale for clinical pain measurement: a ratio measure? Pain Pract. 2003 Dec;3(4):310-6. doi: 10.1111/j.1530-7085.2003.03034.x.
- Albrecht E, Taffe P, Yersin B, Schoettker P, Decosterd I, Hugli O. Undertreatment of acute pain (oligoanalgesia) and medical practice variation in pre-hospital analgesia of adult trauma patients: a 10 yr retrospective study. Br J Anaesth. 2013 Jan;110(1):96-106. Epub 2012 Oct 11. doi: 10.1093/bja/aes355.
- Motov SM, Khan AN. Problems and barriers of pain management in the emergency department: Are we ever going to get better? J Pain Res. 2008 Dec 9;2:5-11. https://doi.org/10.2147/JPR.S4324.
- Siriwardena AN, Asghar Z, Lord B, Pocock H, Phung VH, Foster T, et al., Patient and clinician factors associated with pre-hospital pain treatment and outcomes: cross sectional study. Am J Emerg Med. 2019 Feb;37(2):266-271. doi: 10.1016/j.ajem.2018.05.041. Epub 2018 May 23.
- World Health Organisation (WHO). Cancer pain ladder. Last accessed: November 10, 2024. Available at: Available at http://www.who.int/cancer/palliative/painladder/en/
- Savoia, G., Coluzzi, F., Di Maria, C., Ambrosio, F., Della Corte, F., Oggioni, R., et al. Italian Intersociety Recommendations on pain management in the emergency setting (SIAARTI, SIMEU, SIS 118, AISD, SIARED, SICUT, IRC). Available at: https://www.siaarti.it/news/371885. Last access: 15 January 2025.
- Akbas S, Castellucci C, Nehls F, Müller SM, Spahn DR, Kaserer A. Präklinische Schmerztherapie: Übersicht und Verbesserungsmöglichkeiten. Praxis (Bern 1994). 2022;111(3):157-162. German. https://doi.org/10.1024/1661-8157/a003810
- Friesgaard KD, Kirkegaard H, Rasmussen CH, Giebner M, Christensen EF, Nikolajsen L. Pre-hospital intravenous fentanyl administered by ambulance personnel: a cluster-randomised comparison of two treatment protocols. Scand J Trauma Resusc Emerg Med. 2019 Feb 7;27(1):11. https://doi.org/10.1186/s13049-019-0588-4.
- Ferri P, Gambaretto C, Alberti S, Parogni P, Rovesti S, Di Lorenzo R, et al. Pain Management in a Pre-hospital Emergency Setting: A Retrospective Observational Study. J Pain Res. 2022 Oct 27;15:3433-3445. https://doi.org/10.2147/JPR.S376586.
- Lindbeck G, Shah MI, Braithwaite S, Powell JR, Panchal AR, Browne LR, et al., Evidence-Based Guidelines for Pre-hospital Pain Management: Recommendations. Prehosp Emerg Care. 2023;27(2):144-153. doi: 10.1080/10903127.2021.2018073. Epub 2022 Jan 25.
- Friesgaard KD, Nikolajsen L, Giebner M, Rasmussen CH, Riddervold IS, Kirkegaard H, et al. Efficacy and safety of intravenous fentanyl administered by ambulance personnel. Acta Anaesthesiol Scand. 2016 Apr;60(4):537-43. https://doi.org/10.1111/aas.12662.
- Bronsky ES, Koola C, Orlando A, Redmond D, D'Huyvetter C, Sieracki H, et al. Intravenous Low-Dose Ketamine Provides Greater Pain Control Compared to Fentanyl in a Civilian Pre-hospital Trauma System: A Propensity Matched Analysis. Prehosp Emerg Care. 2019 Jan-Feb;23(1):1-8. https://doi.org/10.1080/10903127.2018.1469704.
- Shimonovich S, Gigi R, Shapira A, Sarig-Meth T, Nadav D, Rozenek M, et al. Intranasal ketamine for acute traumatic pain in the Emergency Department: a prospective, randomized clinical trial of efficacy and safety. BMC Emerg Med. 2016 Nov 9;16(1):43. https://doi.org/10.1186/s12873-016-0107-0.
- Sandberg M, Hyldmo PK, Kongstad P, Dahl Friesgaard K, Raatiniemi L, Larsen R, et al. Ketamine for the treatment of pre-hospital acute pain: a systematic review of benefit and harm. BMJ Open. 2020 Nov 24;10(11):e038134. https://doi.org/10.1136/bmjopen-2020-038134.
- Ghate G, Clark E, Vaillancourt C. Systematic review of the use of low-dose ketamine for analgesia in the emergency department. Can J Emergency Med. 2018;20(1):36–45. Epub 2017/06/28. https://doi.org/1017/cem.2017.48.
- Ahern TL, Herring AA, Anderson ES, Madia VA, Fahimi J, Frazee BW. The first 500: initial experience with widespread use of low-dose ketamine for acute pain management in the ED. Am J Emerg Med. 2015;33(2):197–201. Epub 2014/11/15.https://doi.org/10.1016/j.ajem.2014.11.010
- Oberholzer N, Kaserer A, Albrecht R, Seifert B, Tissi M, Spahn DR, et al. Factors Influencing Quality of Pain Management in a Physician Staffed Helicopter Emergency Medical Service. Anesth Analg. 2017 Jul;125(1):200-209. doi: 10.1213/ANE.0000000000002016
- Helm M, Hossfeld B, Braun B, Werner D, Peter L, Kulla M. Oligoanalgesia in Patients with an Initial Glasgow Coma Scale Score ≥8 in a Physician-Staffed Helicopter Emergency Medical Service: A Multicentric Secondary Data Analysis of >100,000 Out-of-Hospital Emergency Missions. Anesth Analg. 2020 Jan;130(1):176-186. doi: 10.1213/ANE.0000000000004334.
- Hewes, H. A., Dai, M., Mann, N. C., Baca, T., & Taillac, P. (2017). Pre-hospital Pain Management: Disparity By Age and Race. Pre-hospital Emergency Care, 22(2), 189–197. https://doi.org/10.1080/10903127.2017.1367444
- Jennings PA, Cameron P, Bernard S. Epidemiology of pre-hospital pain: an opportunity for improvement. Emerg Med J. 2011 Jun;28(6):530-1. doi: 10.1136/emj.2010.098954. Epub 2010 Aug 2.
- Mackenzie R. Analgesia and sedation. J R Army Med Corps. 2004;150: S45-S55. https://doi.org/10.1136/jramc-146-02-14
- Shehabi Y, Al-Bassam W, Pakavakis A, Murfin B, Howe B. Optimal Sedation and Pain Management: A Patient- and Symptom-Oriented Paradigm. Semin Respir Crit Care Med. 2021 Feb;42(1):98-111. https://doi.org/10.1055/s-0040-1716736.
- Mc Mullan J, Droege C, Strilka R, Hart K, Lindsell C. Intranasal Ketamine as an Adjunct to Fentanyl for the Pre-Hospital Treatment of Acute Traumatic Pain: Design and Rationale of a Randomized Controlled Trial. Prehosp Emerg Care. 2021 Jul-Aug;25(4):519-529. https://doi.org/10.1080/10903127.2020.1808746.
- Holbrook TL, Galarneau MR, Dye JL, Quinn K, Dougherty AL. Morphine use after combat injury in Iraq and post-traumatic stress disorder. N Engl J Med. 2010 Jan 14;362(2):110-7. https://doi.org/10.1056/NEJMoa0903326
- Zamardi E, Sorrentino D, Inglese L, Beghi M, Gandolfi A, Nani S, et al. La soddisfazione del personale tecnico non sanitario del sistema di emergenza-urgenza territoriale dopo intervento formativo dell’infermiere mediante simulazione: uno studio retrospettivo. Scenario;38(2):35-40.
![]()
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
The role of diet during health education programs for the improvement of clinical outcomes in copd patients: Literature review
Rita Citarella 1*, Adriano Brenca 2, Myriam Palomba 3, Maria Guarnaccia 1, Giuseppina Gargiulo 4, Diodato Ferrante 1, Jessica Marano 5, Aniello Lanzuise 6, Serena Pannetta 2
1 Umberto I Hospital, via Alfonso De Nicola, Nocera Inferiore (Salerno), Italy.
2 Maria SS. Addolorata Hospital, Piazza Scuola medica Salernitana, Eboli (Salerno), Italy.
3 Maresca Hospital, via Montedoro 53, Napoli, Italy.
4 Ospedale del Mare, via Enrico Russo 11, Napoli, Italy.
5 San Giovanni Di Dio e Ruggi d’Aragona Hospital, via San Leonardo (Salerno), Italy.
6 Hospital of national importance “Ospedale dei Colli”, Napoli, Italy
* Corresponding author: Citarella Rita, “Umberto I” Hospital in Nocera Inferiore (Salerno), Italy. E-mail: rita.citarella.91@gmail.com
Cite this article
ABSTRACT
Introduction: Chronic obstructive pulmonary disease is a growing health problem. It is a chronic inflammatory lung disorder characterized by progressive, poorly reversible airflow limitation. The identification of modifiable risk factors for prevention and related patient health education have given positive results. We have passed from the observation of risk factors to a careful diet rich in substances capable of improving lung function. The purpose of this integrative review was to identify, describe and summarize previous studies that have investigated the importance of health education about nutrition in patients with COPD.
Materials and methods: For this scope, a review process was conducted following these five steps: 1) identification of the research problem, 2) literature research, 3) data evaluation, 4) data analysis and 5) presentation of the synthesis of the results. After the identification of the research problem, the second phase of the literature research was conducted using the CINAHL and PubMed databases. MeSH search terms included: COPD, health education, malnutrition, and Quality of Life. These terms have been combined each other using boolean operators. The electronic research was limited to the articles published in the English language within the past 10 years. Studies that responded to the hypotheses of bibliographic research were considered. Primary studies, systematic reviews and guidelines were included. Bibliographic research was conducted from 1 June 2024 to 24 October 2024.
Results: Some studies show that by eliminating risk factors, improving nutrition and educating the patient to self-manage the disease through tertiary prevention programs, there has been an improvement in the patients’ quality of life.
Conclusion: Correct health education is important to have “instructions” on the pathology and its self-help management. Outcomes are enhanced by self-efficacy interventions that aim to achieve a healthy lifestyle through behavior modification, especially about diet.
Keywords: COPD, health education, malnutrition and Quality of Life.
INTRODUCTION
Chronic Obstructive Pulmonary Disease (COPD) was ranked as the third leading cause of death worldwide in 2016 [1] and the fourth leading cause of death in the United States in 2017 [2]. The prevalence of COPD was reported to be approximately 300 million in 2017 [3]. Furthermore, the incidence of COPD expected to increase further in the coming years due to an aging population and continued exposure to COPD risk factors, including tobacco smoke, occupational dusts and chemicals, biomass fuel and air pollution [4]. So, COPD can be prevented by reducing exposure to these risk factors, including avoidance or early cessation of smoking [5]. This disease is characterised by persistent respiratory symptoms and airflow limitation [6], providing in this way a significant burden for patients and society. In effect, patients suffering from BPCO complain reduced daily physical activities, impacting on their work and social life. The consequence is often the onset of psychological conditions such as anxiety and depression [7,8]. Together, all these factors decrease health-related quality. COPD is caused by the alveolar wall destruction which results in air trapping and static hyperinflation [9,10], increasing the mortality of these patients compared to the general population [6]. Symptoms of COPD may include chronic and progressive dyspnoea, chronic cough (with or without sputum production), chest tightness or fatigue [11-17]; patients typically do not seek medical help until symptoms have a substantial impact on their daily life [18]. Sarcopenia, which is common in COPD, worsens dyspnoea due to reduced muscle mass leading to decreased exercise capacity and increased breathless ness [19]. In effect, patients with COPD, especially those with advanced emphysema, often have severe nutritional deficiencies. Weight loss in COPD patients has been associated with malnutrition [20] and such patients also have high mortality rates [21]; therefore, they require nutritional support. However, once these patients lose weight, it is difficult for them to regain it. Malnourished COPD patients experience a 1.5-fold increase in resting energy expenditure, compared to the healthy population. Therefore, among the risk factors to pay attention for public health, apart from smoking cessation [22], diet has been recognized as a modifiable risk factor for the development and progression of the disease [23]. A better understanding of the impact of diet on COPD prevention and/or outcomes can raise awareness of the importance of nutritional approaches, providing insights to promote lung health and to prevent disease onset and progression. As we have seen, if the patient follows a good nutritional plan, he can have an improvement in the disease. The nurse plays an important role thanks to good health education that promotes self-care in people with COPD. Currently, patients are provided with disease management training both in hospital and at home to implement patient self-efficacy. Self-efficacy intervention is essential because it aims to achieve a healthy lifestyle through behavior regulation [24], to improve quality of life and avoid the exacerbations [25]. The identification of these modifiable risk factors for prevention is important: Sarcopenia is associated with a poorer quality of life, increased risk of repeated hospital admissions and higher mortality [26]. Good health education can give positive results. The role of the nurse is to support patients in developing self-management skills, providing adequate information and feedback on behaviors in case of exacerbations, also improving their nutritional plans [27]. This type of prevention is called tertiary prevention because it does not indicate the prevention of the disease, but is used to avoid complications, the probability of recurrence and death. The purpose of this integrative review was to identify, describe and summarize previous studies that have investigated the importance of health education about nutrition and its factors in patients with COPD.
MATERIALS AND METHODS
In the study of this topic, we formulated the following questions:
- How can the modification of diet improve the quality of life of COPD patients?
- Is there the impact of health education by health professionals on the adherence to new lifestyles from COPD patients?
We conducted the research using the P.I.O. framework, which stands for population, intervention and outcomes (Table 1).
| POPULATION | COPDS PATIENTS |
| INTERVENTION | HEALTH EDUCATION ABOUT NUTRITIONAL PLAN |
| OUTCOME | REDUCE MORTALITY, HOSPITALISATION, EXACERBATIONS AND WORSENINGS OF SYMPTOMS |
Table 1. The PIO methodology assessment
Study Design
The study design is an integrative review performed following the PRISMA (Preferred Reporting Items for Systematic-review and Meta-Analysis) (PRISMA) guidelines [28]. So, a review process was conducted by C.R. and P.S. following these five steps: 1) identification of the research problem, 2) literature research, 3) data evaluation, 4) data analysis and 5) presentation of the synthesis of the results [29]. Bibliographic research was conducted from 1 June 2024 to 24 October 2024. After the identification of the research problem, the second phase of the literature research was conducted using the CINAHL and PubMed databases. MeSH search terms included: COPD, health education, malnutrition and Quality of Life. These terms have been combined each other using Boolean operators “AND” and “OR”. The search strategies for each database are provided in the search string table (Table 2).
| DATABASE | KEYWORDS COMBINATION |
| PUBMED | modification[All Fields] AND ("diet"[MeSH Terms] OR "diet"[All Fields]) AND improve[All Fields] AND ("quality of life"[MeSH Terms] OR ("quality"[All Fields] AND "life"[All Fields]) OR "quality of life"[All Fields]) AND ("pulmonary disease, chronic obstructive"[MeSH Terms] OR ("pulmonary"[All Fields] AND "disease"[All Fields] AND "chronic"[All Fields] AND "obstructive"[All Fields]) OR "chronic obstructive pulmonary disease"[All Fields] OR "copd"[All Fields]) AND ("patients"[MeSH Terms] OR "patients"[All Fields]) |
| PUBMED | "impact"[All Fields] AND ("health education"[MeSH Terms] OR ("health"[All Fields] AND "education"[All Fields]) OR "health education"[All Fields]) AND ("health personnel"[MeSH Terms] OR ("health"[All Fields] AND "personnel"[All Fields]) OR "health personnel"[All Fields] OR ("health"[All Fields] AND "professionals"[All Fields]) OR "health professionals"[All Fields]) AND adherence[All Fields] AND new[All Fields] AND ("life style"[MeSH Terms] OR ("life"[All Fields] AND "style"[All Fields]) OR "life style"[All Fields] OR "lifestyles"[All Fields]) AND ("pulmonary disease, chronic obstructive"[MeSH Terms] OR ("pulmonary"[All Fields] AND "disease"[All Fields] AND "chronic"[All Fields] AND "obstructive"[All Fields]) OR "chronic obstructive pulmonary disease"[All Fields] OR "copd"[All Fields]) AND ("patients"[MeSH Terms] OR "patients"[All Fields]) |
| CINAHL | Modification AND ("diet"[MeSH Terms] OR "diet") AND improve AND ("quality of life"[MeSH Terms] OR ("quality" AND "life") OR "quality of life") AND ("pulmonary disease, chronic obstructive"[MeSH Terms] OR ("pulmonary" AND "disease" AND "chronic" AND "obstructive") OR "chronic obstructive pulmonary disease" OR "copd" ) AND ("patients"[MeSH Terms] OR "patients"). |
| CINAHL | "impact” AND ("health education"[MeSH Terms]) OR ("health" AND "education") OR ("health education") AND ("health personnel"[MeSH Terms] OR ("health" AND "personnel") OR "health personnel" OR ("health" AND "professionals") OR "health professionals") AND adherence AND new AND ("life style"[MeSH Terms] OR ("life" AND "style”) OR "life style" OR "lifestyles") AND ("pulmonary disease, chronic obstructive"[MeSH Terms] OR ("pulmonary"AND "disease" AND "chronic" AND "obstructive" ) OR "chronic obstructive pulmonary disease" OR "copd") AND ("patients"[MeSH Terms] OR "patients") |
Table 2. Search string in databases.
Inclusion and Exclusion criteria
Studies that responded to the hypotheses of bibliographic research were considered. Primary studies, systematic reviews and guidelines were included. The inclusion criteria used for the selection of articles were human population including both males and females, studies in English language, available abstract, publications of the last 10 years and scientific articles. Articles of national and international scientific literature whose title and content contained at least one of the keywords or a link to them are included. All those quotes for which it was not possible to find the written “full text” version were excluded. The selected studies were found in full text format, read critically and the relevant ones were included in the review.
RESULTS
The selection process resulted in the inclusion of 6 articles, as shown in Figure 1, according to the 2020 Preferred Reporting Items for Systematic-review and Meta-Analysis (PRISMA) guidelines [28].

The following table reports the included studies, describing their features: year of publication, name of authors, title, scope, methodology, study sample and their results (Table 3); 6 articles were identified, published between 2018 and 2024, with different methodology as follows: three randomized controlled trials, two cross-sectional studies and one experimental study. Four studies were conducted in the European countries (Norway [30], Iceland [31], Turkey [32] and Hungary [34]) while only two in Asian continent: exactly, in Japan [33] and China [35].
| YEAR | AUTHORS | TITLE | SCOPE | RESEARCH METHOD | SAMPLE | RESULTS |
| 2018
[30] |
Heidi B Bringsvor, Eva Langeland, [...], and Signe Berit Bentsen | Effects of a COPD self-management support intervention: a randomized controlled trial | Promote self-management, self-efficacy after COPD patient education programs | Randomized controlled trial | 182 patients | In people with COPD, an educational plan gave way to acquire skills and constructive attitudes in self-monitoring of symptoms and disease course. |
| 2019
[31] |
Arora Ros Ingadottir, Anne Marie Beck, Ingibjorg Gunnarsdottir | Oral nutrition supplements and between-meal snacks for nutrition therapy in patients with COPD identified as at nutritional risk: a randomized feasibility trial | To evaluate the impact of nutrients on lung function and COPD progression. Several dietary options may be considered in terms of COPD prevention and/or progression. | Randomized study. | 34 participants at nutritional risk, of which 19 took oral food supplements and 15 snacks, providing 600 kcal and 22 gr of protein per day in addition to the regular daily diet. | In COPD patients who are at nutritional risk, snack foods are more feasible and effective than oral dietary supplements. |
| 2020
[32] |
Ayşe Çevirme, PhD and Gönül Gökçay, PhD student | The impact of an Education-Based Intervention Program (EBIP) on dyspnea and chronic self-care management among chronic obstructive pulmonary disease patients | Evaluate the impact of dyspnea and outcomes on an education-based intervention program (EBIP) versus routine care. | Single-blind randomized controlled study | 51 patients diagnosed with stage 2 chronic obstructive pulmonary disease (COPD) divided into experimental and control groups. Participants are similar in terms of gender, marital status, smoking status, disease duration and age. | In patients with stage II COPD, structured education programs (often including the presence of nurses in the form of home visits and telephone calls) contribute to the management pf COPD symptoms, primarily dyspnea.
|
| 2020
[33] |
Takako mouri, Chieko hatamochi, and Koichi takayama | Education Program for Male Patients with Chronic Obstructive Pulmonary Disease to Change Dietary Behavior | To evaluate the effects of an educational program to change the eating behaviors of male COPD patients. | Experimental study | 22 male participants, of which 11 in the intervention group with an average age of 67 years and 11 in the control group with an average age of 72 years (the patients are only male in order to control the effects of sex on eating behavior). | In order to prevent malnutrition in patients with COPD, it was sufficient to provide them with relevant knowledge in increased energy intake. |
| 2021
[34] |
Fekete, M.; Fazekas-Pongor, V.; Balazs, P.; Tarantini, S.; Szollosi, G.; Pako, J.; Nemeth, A.N.; Varga, J.T. | Effect of malnutrition and body composition on the quality of life of COPD patients.
|
to determine the correlation between nutritional status and quality of life of COPD patients. | cross-sectional study | Fifty patients (mean age was 66 years). Mean body mass index (BMI) was 26.2. | Considering that malnourished COPD patients may have reduced lung function and lower quality of life compared to normal weight patients, nutritional therapy must be included in the treatment of COPD patients combined with nutritional risk screening during the follow-up. |
| 2024
[35] |
Qi Jiang, Zheru Ma, Jing Sun and Yang Li | Association of dietary inflammatory indices with sarcopenia and all-cause mortality in COPD patients | Explore the relationship between sarcopenia in patient with COPD and mortality | cross-sectional study, | 1429 patients | A significant association between concurrent sarcopenia and an increased risk of all-cause mortality in COPD patients within the United States was observed. |
Table 3. Analysis of selected studies
DISCUSSION
The purpose of this integrative review was to identify, describe and summarize previous studies that have investigated the importance of health education about nutrition in patients with COPD, addressing COPD from a non-pharmacological perspective, analysing how a health education about nutritional plan can improve the health of COPD patients. Health education, in terms of self-management interventions, should be part of chronic care for patients with COPD, at all stages of their disease. A good health education also improves self-management of the disease and its awareness [27]. In fact, the patient is able to perceive his own skills and competences in managing the pathology. The identification of modifiable risk factors for the prevention and treatment of COPD is the first step. About this, increased awareness of diet and dietary factors that influence respiratory health may be of interest to public health, due to their effects on the disease course. For this reason, informing and educating the patient should be the main goal with patients suffering from COPD. A randomized controlled trial by Bringsvor et al. [30], involving 182 patients, evaluated the effects of a COPD self-management support intervention. The results showed significant positive changes in patients' attitudes and approaches, with an acquisition of skills thanks to educational activities on disease awareness. This confirms the effectiveness of educational interventions, which should also include nutrition as an integral part of treatment. In line with this evidence, a study conducted by Ingadottir et al. [31], involving COPD patients divided into two groups (one with snacks and the other with food supplements), showed that a weight gain of more than 2 kg was a significant predictor of survival in underweight patients. Both groups gained weight during the 12-month follow-up, but the group receiving snacks showed a greater weight gain than the group receiving food supplements. The results suggest that in COPD patients at nutritional risk, snacks may be more effective and practical than oral supplements. The study by Cevirme et al. [32] also showed that an education-based educational program (EBIP) had positive effects on improving self-management skills, reducing functional disability and improving quality of life. Nurse interventions play an important role in supporting and motivating patients, and COPD patient self-management education reduces the frequency of hospitalizations associated with acute exacerbations and improves patients’ quality of life [36]. In experimental study by Mouri et al [33], the effects of an educational program to change the eating behaviors of COPS patients were also evaluated, including 22 male participants subdivided in two groups (intervention group and control group). The conclusion of this study, as well as in previous studies, was that the prevention of malnutrition and deterioration in patients with COPS could be obtained providing these patients with relevant knowledge and skills in order to increase the energy intake. In fact, in the study “Effect of malnutrition and body composition on the quality of life of COPD patients” [34] an association between low body weight and the severity of COPD was noted, indicating that patients’ nutritional status was linked to their quality of life. This study indicates that malnourished COPD patients may have reduced lung function and lower quality of life compared to normal weight patients. Thus, their findings suggest that nutritional therapy must be included in the treatment of COPD patients during the follow-up [37]. At the end, in the last article “Association of dietary inflammatory indices with sarcopenia and all-cause mortality in COPD patients” [35], the results revealed sarcopenia prevalence in COPD patients, showing a significant association between concurrent sarcopenia and an increased risk of all-cause mortality in COPD patients. Dietary adjustments may be mandatory in order to mitigate muscle wasting and enhance the prognosis of COPD. Targeted nutritional interventions, like high-protein diets, may improve respiratory muscle strength, physical performance, overall health status and quality of life in elderly COPD patients [38]. In the light of the results of different reported studies, in order to obtain a better quality of life and to control the symptoms, the health education programs (also including the intervention of nurse both at the hospital and by home visits) may focus on improving the energy intake and consequently the “status” of muscle mass. An essential concept emerges from all these studies: nutritional status is an important determinant of outcome of COPD and the only way for assessing the nutritional risk of these patients is through longitudinal measurement of body weight and body composition. Probably, two limitations are common to all the studies enrolled in our review; at first, the lack of the evaluation of vitamin D in patients with COPD is to be considered. In effect, as highlighted by Bojesen et al. [39], the prevalence of vitamin D nutrient deficiency is high in COPD and could be incorporated into nutritional risk screening. At second, none of the authors assessed the different metabolic phenotypes of COPD patients, from which a specific nutritional risk is associated to and that it could be useful in patients counselling. Apart from these two limitations, it is clear that nutritional intervention is likely to be effective in undernourished patients and is probably most effective if combined with an exercise programme. Overall, the evidence from our review indicates that a well-balanced diet with sufficient intake of fresh fruits and vegetables is beneficial to COPD patients, not only for its potential benefits on the lung but also for its proven benefits on metabolic and cardiovascular risk. All this can only be achieved through close interaction between the patient and the health professionals in charge, in order to set up a health program that can be reproduced over time, even and especially when the patient provides for his self-management at home without being guided by health personnel. Furthermore, in the future, healthcare professionals should not only pay attention to the early screening of weight loss in COPD patients, but also provide relevant prevention information, in effect, according to the results from Zhou J et al. [40], age, body mass index, smoking and diabetes mellitus are the contributing factors for sarcopenia in patients with chronic obstructive pulmonary disease.
Limitations of the study
This review has some limitations: at first, only two databases were consulted; furthermore, among enrolled reports, one study limited their subjects to patients that were treated for stage II COPD [32] while another report included only Japanese men in the study [34], limiting its interpretation in terms of gender and ethnic groups. Finally, there are not many studies that have dealt with this topic in the last five years; for this reason, the review is limited to a small number of selected articles, which are long-standing dated.
Implications for clinical practice
The review suggests that different strategies should be adopted for patients with COPD. Except of the elimination of smoking as a risk factor in order to improve the lives of these patients, it is needed to pay attention to educational programs, focusing particularly on eating behaviour and dietary factors. Through adequate nutritional support that can ensure the right energy intake and a balanced protein intake, associated with adequate exercise, it will be possible to guarantee a positive maintenance of the efficiency of cognitive and physical functions, essential prerequisites for ensuring the elderly maximum autonomy for an excellent life expectancy. The nurse, being in close and continuous contact with patients, assumes a fundamental role in identifying and preventing the causes of malnutrition with prevention programs. The study emphasises the importance of continued training in communications skills for healthcare professionals supporting people with COPD, particularly acknowledging the patient's concerns in the context of symptom changes/flare-up.
CONCLUSION
This integrative review aimed to identify, describe and summarize previous studies that have investigated how a health education about nutritional plan can improve the health of COPD patients. The results of this systematic review suggest that health education programs, including hospital and home nursing interventions, should focus on improving energy intake and muscle mass, to improve quality of life and control symptoms in COPD patients. The success of these interventions depends on a close collaboration between patients and healthcare professionals, to develop health programs that can be replicated over time, even when the patient is managing his or her condition independently at home. It is therefore essential that healthcare professionals not only monitor weight loss early in COPD patients, but also provide preventive information, considering factors such as age, body mass index, smoking and diabetes, which contribute to sarcopenia and worsen the risk of negative outcomes. Future studies should explore the effectiveness of combined interventions, integrating nutritional education and physical exercise, to improve muscle mass and quality of life and, further, focus on long-term, technology-supported self-management models to monitor and optimize patients' nutritional self-management.
Funding statement
This research did not receive any specific grant from funding agencies in public, commercial or not for profit sectors.
Conflict of interest
The authors report no conflict of interest.
Authors’ contribution
CR was the major contributor in writing the manuscript. BA, PM, GM, GG, FD, MJ, LA and PS performed the data collection and interpreted the patient data regarding pulmonary disease. All authors read and approved the final manuscript.
REFERENCES
- World Health Organization, The top 10 causes of death, https://www.who.int/en/news-room/fact-sheets/detail/the-top-10-causes -of-death, 2018.
- Heron, Deaths: leading causes for 2017, Natl. Vital Stat. Rep. 68 (6) .2019. 1–77.
- GBD Disease Injury Incidence Prevalence Collaborators, Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017, Lancet 392 (10159).2018. 1789–1858, https://doi.org/10.1016/S0140-6736(18)32279-7.
- Global Initiative for Chronic Obstructive Lung Disease, Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease .2019 report 2020.
- World Health Organization, COPD management, 2016.
- Global Initiative for Chronic Obstructive Lung Disease. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. 2021 report. 2021.
- Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. 2012;380(9859):2095–128. doi: 10.1016/S0140-6736(12)61728-0.
- James SL, Abate D, Abate KH, Abay SM, Abbafati C, Abbasi N, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392(10159):1789–858. doi:10.1016/S0140-6736(18)32279-7
- Barnes PJ. Inflammatory mechanisms in patients with chronic obstructive pulmonary disease. J Allergy Clin Immunol. 2016;138(1):16–27. doi: 10.1016/j.jaci.2016.05.011.
- Rossi A, Aisanov Z, Avdeev S, Di Maria G, Donner CF, Izquierdo JL, et al. Mechanisms, assessment and therapeutic implications of lung hyperinflation in COPD. Respir Med. 2015;109(7):785– doi: 10.1016/j.rmed.2015.03.010.
- Van der Molen T, Miravitlles M, Kocks JWH. COPD management: role of symptom assessment in routine clinical practice. Int J Chron Obstruct Pulmon Dis. 2013;8:461–71. doi: 10.2147/COPD.S49392.
- Jones PW. Health status measurement in chronic obstructive pulmonary disease. 2001;56(11):880–7. doi: 10.1136/thorax.56.11.880.
- Weiss ST, DeMeo DL, Postma DS COPD: problems in diagnosis and measurement. Eur Respir J Suppl. 2003;21:4s– doi: 10.1183/09031936.03.00077702.
- Guerra S, Sherrill DL, Venker C, Ceccato CM, Halonen M, Martinez FD. Chronic bronchitis before age 50 years predicts incident airflow limitation and mortality risk. 2009;64(10):894–900. doi: 10.1136/thx.2008.110619.
- Shrikrishna D, Patel M, Tanner RJ, Seymour JM, Connolly BA, Puthucheary ZA, et al. Quadriceps wasting and physical inactivity in patients with COPD. Eur Respir J. 2012;40(5):1115–22. doi: 10.1183/09031936.00170111.
- Watz H, Waschki B, Meyer T, Magnussen H. An official European Respiratory Society statement on physical activity in COPD. Eur Respir J. 2009;33(2):262–72. doi: 10.1183/09031936.00046814
- Kaplan A, Thomas M. Screening for COPD: the gap between logic and evidence. Eur Respir Rev. 2017;26(143): doi: 10.1183/16000617.0113-2016.
- Van den Boom G, Rutten-van Mölken MP, Tirimanna PR, van Schayck CP, Folgering H, van Weel C. Association between health-related quality of life and consultation for respiratory symptoms: results from the DIMCA programme. Eur Respir J. 1998;11(1):67–72. doi: 10.1183/09031936.98.11010067.
- Kim SH, Shin MJ, Shin YB, Kim KU. Sarcopenia Associated with Chronic Obstructive Pulmonary Disease. J Bone Metab. 2019;26(2):65–74. doi: 10.11005/jbm.2019.26.2.65.
- Ingadottir , A.R. Anne Marie Beck, Christine Baldwin , C Elizabeth Weekes , Olof Gudny Geirsdottir, Alfons Ramel, Thorarinn Gislason, Ingibjorg Gunnarsdottir. Two components of the new ESPEN diagnostic criteria for malnutrition are independent predictors of lung function in hospitalized patients with chronic obstructive pulmonary disease (COPD). Clin Nutr.,2018.37,1323–1331. doi: 10.1016/j.clnu.2017.05.031.
- Wilson, D.O.,Rogers, R.M., Wright, E.C., Anthonisen, N.R. Body weight in chronic obstructive pulmonary disease. The National Institutes of Health Intermittent Positive-Pressure Breathing trial. Am Rev Respir Dis.,1989.139,1435–1438. doi: 10.1164/ajrccm/139.6.1435.
- Schulze, M.B., Martinez-Gonzalez, M.A., Fung, T.T., Lichtenstein, A.H., Forouhi, N.G. 2018. Food based dietary patterns and chronic disease prevention. BMJ extension. doi: 10.1136/bmj.k2396.
- Whyand, T., Hurst, J.R., Beckles, M., Caplin, M.E.. Pollution and respiratory disease: Can diet or supplements help? A review. Respir Res.2018. 19, 79. doi: 10.1186/s12931-018-0785-0.
- Cravo A, Attar D, Freeman D, Holmes S, Ip L, Singh SJ. The Importance of Self-Management in the Context of Personalized Care in COPD. Int J Chron Obstruct Pulmon Dis. 2022 Jan 22;17:231-243. doi: 10.2147/COPD.S343108. PMID: 35095272;
- Osborne, R.H., Elsworth, G.R., Whitfield, K.. The Health Education Impact Questionnaire (heiQ): an outcomes and evaluation measure for patient education and self-management interventions for people with chronic conditions. Patient Education Couns,2007.66,192–201. doi: 10.1016/j.pec.2006.12.002. Epub 2007 Feb 22.
- Kaluźniak-Szymanowska A, Krzymińska-Siemaszko R, Deskur-Śmielecka E, Lewandowicz M, Kaczmarek B, Wieczorowska-Tobis K. Malnutrition, Sarcopenia, and Malnutrition-Sarcopenia Syndrome in Older Adults with COPD. 2021 Dec 23;14(1):44. doi: 10.3390/nu14010044.
- Aranburu-Imatz A, López-Carrasco JC, Moreno-Luque A, Jiménez-Pastor JM, Valverde-León MDR, Rodríguez-Cortés FJ, Arévalo-Buitrago P, López-Soto PJ, Morales-Cané I. Nurse-Led Interventions in Chronic Obstructive Pulmonary Disease Patients: A Systematic Review and Meta-Analysis. Int J Environ Res Public Health. 2022 Jul 26;19(15):9101. doi: 10.3390/ijerph19159101.
- Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R, Glanville J, Grimshaw JM, Hróbjartsson A, Lalu MM, Li T, Loder EW, Mayo-Wilson E, McDonald S, McGuinness LA, Stewart LA, Thomas J, Tricco AC, Welch VA, Whiting P, Moher D. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021 Mar 29;372:n71. doi: 10.1136/bmj.n71.
- Whittemore R, Knafl K. The integrative review: updated methodology. J Adv Nurs. 2005; 52(5): 546-553. doi:1111/j.1365-2648.2005.03621.x
- Heidi B Bringsvor, Eva Langeland , Bjørg Frøysland Oftedal , Knut Skaug , Jörg Assmus , Signe Berit Bentsen. Effects of a COPD self-management support intervention: a randomized controlled trial. Int J Chron Obstruct Pulmon Dis. 2018 Nov 8:13:3677-3688. doi: 10.2147/COPD.S181005.
- Arora Ros Ingadottir, Anne Marie Beck, Ingibjorg Gunnarsdottir. Oral nutrition supplements and between-meal snacks for nutrition therapy in patients with COPD identified as at nutritional risk: a randomized feasibility trial. BMJ Open Respir Res 2019 Jan 3;6(1):e000349. doi: 1136/bmjresp-2018-000349
- Ayşe Çevirme, PhD and Gönül Gökçay, PhD student. The impact of an Education-Based Intervention Program (EBIP) on dyspnea and chronic self-care management among chronic obstructive pulmonary disease patients. Saudi Med J. 2020 Dec;41(12):1350-1358. doi: 10.15537/smj.2020.12.25570.
- Takako mouri, Chieko hatamochi, and Koichi takayama. Education Program for Male Patients with Chronic Obstructive Pulmonary Disease to Change Dietary Behavior. Kobe J Med Sci. 2020 Oct 12; PMID: 33431780; PMCID: PMC7837662.
- Fekete, M.; Fazekas-Pongor, V.; Balazs, P.; Tarantini, S.; Szollosi, G.; Pako, J.; Nemeth, A.N.; Varga, J.T. Effect of malnutrition and body composition on the quality of life of COPD patients. Physiol Int. 2021 Jun 29. doi: 10.1556/2060.2021.00170.
- Qi Jiang , Zheru Ma , Jing Sun and Yang Li . Association of dietary inflammatory indices with sarcopenia and all-cause mortality in COPD patients. Front Nutr 2024 May 23:11:1395170. doi: 10.3389/fnut.2024.1395170.
- Özkaptan BB, Kapucu S. Home nursing care with the self-care model improves self-efficacy of patients with chronic obstructive pulmonary disease. Jpn J Nurs Sci. 2016;13:365–377. doi: 10.1111/jjns.12118
- Hallin R, Janson C, Arnardottir RH, Olsson R, Emtner M, Branth S, Gunnar Boman, Frode Slinde. Relation between physical capacity, nutritional status and systemic inflammation in COPD. Clin Respir J 2011; 5(3): 136–42. PMID: 21679348. doi: 10.1111/j.1752-699X.2010.00208.x.
- Bernardes S, da Conceição Eckert I, Burgel CF, Teixeira PJZ, Silva FM. Increased energy and/or protein intake improves anthropometry and muscle strength in chronic obstructive pulmonary disease patients: a systematic review with meta-analysis on randomised controlled clinical trials. Br J Nutr. (2022):1–18. doi: 10.1017/S0007114522000976.
- S Afzal P Lange SE Bojesen et al. Plasma 25-hydroxyvitamin D, lung function and risk of chronic obstructive pulmonary disease. Thorax 2014; 69: 24–31. doi: 10.1136/thoraxjnl-2013-203682.
- Zhou J, Liu Y, Yang F, Jing M, Zhong X, Wang Y, Liu Y, Ming W, Li H, Zhao T, He L. Risk Factors of Sarcopenia in COPD Patients: A Meta-Analysis. Int J Chron Obstruct Pulmon Dis. 2024 Jul 9;19:1613-1622. doi: 10.2147/COPD.S456451. PMID: 39011123; PMCID: PMC11246983.
![]()
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Innovation and Technology in Nursing Education: Challenges and Opportunities
Gianluca Azzellino, Patrizia Vagnarelli
1 Complex Operative Unit (U.O.C.), Adriatic District Area, Territorial operations center. Local Health Authority of Teramo (AUSL 04), Italy
2 Complex Operative Unit (U.O.C.), Adriatic District Area, Territorial operations center. Local Health Authority of Teramo (AUSL 04), Italy
Corresponding author: Gianluca Azzellino, Complex Operative Unit (U.O.C.), District Area Adriatica, Territorial Assistance Department, Local Health Authority of Teramo (AUSL 04), Italy Via Finlandia n. 7/1,65015 Montesilvano, Italy. Email: gianluca.azzellino@aslteramo.it
Cite this article
ABSTRACT
This comment responds to the recently published article on online learning methods during the COVID-19 pandemic. The article describes the challenges, methods, and opportunities of online learning. The authors consider this topic to be very current, interesting, and highly relevant, as the impact that technology will have on the future of nursing education will be significant. However, the challenge posed by the implementation of advanced technologies such as virtual reality (VR) or e-learning requires special attention. These technologies not only enrich students' educational experiences but can be important in adequately and comprehensively preparing students to meet real-world clinical challenges.
Keywords: Nursing training, technological integration, professional development, nursing education innovation, digital tools.
INTRODUCTION
The authors read with interest the article by Husna et al. (2024) addressing the topic of online learning during the COVID-19 pandemic. With the accelerated adoption of digital tools, nursing education is adapting its educational programs to the new technological realities. While it is clear that online learning played an essential role in ensuring the continuity of education during the pandemic, it is necessary to highlight how advanced technologies can further enhance learning. Among these, virtual reality (VR), with its immersive and realistic simulations, could represent an effective future resource to bridge the gap between theory and practice, making nursing education more attractive and engaging.
Through its immersive interactivity, VR effectively eliminates the boredom of conventional teaching and rigid teaching methodologies, triggering greater academic enthusiasm among nursing students and significantly improving their operational skills [1]. The 'digital natives,' as young students are often called, have always been accustomed to technology, so they have no difficulty adapting to change. However, their challenge does not lie in using these technologies but in maintaining focus and management in an online environment, where the negative variable could be represented by reduced attention and direct interaction with peers and faculty. Obviously, things are different for the more experienced generations of nurses, who had no contact with technology during their training. For them, the main challenge is not only managing the new equipment but also adapting work methods consolidated over the years. This generational diversity does not require a one-size-fits-all approach, but rather a differentiated approach to introducing technology into the nursing profession.
DISCUSSION
Research work on online learning methods developed during the Covid-1 pandemic (Husna et al., 2023), highlights the many benefits of technology in nursing education. The authors highlight the numerous advantages of technology in nursing education. During the COVID-19 pandemic, online training proved to be a tool capable of ensuring continuity. However, the exclusive use of online platforms is not suitable for nursing education and is not sufficient to adequately prepare students for the clinical complexity of nursing work. We all know that the nursing profession is going through a period of crisis [2] and that it is essential to deploy all available forces and strategies to renew it, making it attractive and satisfying again. The digitalization of care processes requires ever greater digital skills to ensure high-level care adapted to current knowledge [3].
Virtual reality offers innovative approaches by providing students with phases and moments of clinical experiences in a safe and controlled virtual environment. A significant goal of nursing education is the transfer of theoretical knowledge to clinical practice. In addition to virtual reality, other emerging technologies are significantly contributing to nursing education. For example, e-learning platforms provide a wide range of educational resources such as quizzes, videos, and scenarios. Apps and real-time feedback systems can support learning, making education more inclusive and accessible. A crucial aspect is balancing theoretical and practical training.
Today, innovative tools that simulate realistic cardiac arrest scenarios are used to bridge the gap between theory and practice. The integration of simulations into training ensures the ability to manage multiple cases with unlimited practice, without jeopardizing patient safety. The possibilities offered by virtual reality allow the recreation of immersive, interactive, and realistic scenarios in which the student can practice repeatedly without the need for additional materials or people [5].
In a photorealistic VR scenario, the patient in cardiac arrest is reproduced with high fidelity, providing key clinical signs and patient reactions. During the event, the subject can monitor the patient’s condition and initiate the resuscitation procedure. The learner performs CPR maneuvers from a perspective that projects him into a completely immersive situation [6]. In everyday practice, nurses can use photorealistic VR scenarios to train in the management of complex situations, especially in emergency-urgency operating units. These tools allow them to train in an environment very similar to reality and controlled, without putting the patient's health at risk. Another positive feature of VR training is the improvement of accessibility, as there is no need to organize a physical training session [7]. Initially, the costs of training using these technologies can be high compared to traditional training methods. This can represent a disadvantage and a risk of not being able to guarantee equal access, generating inequalities among students [7]. In conclusion, technology offers several ideas for improvement in training and clinical practice, but it is important to emphasize that this should never completely replace the direct clinical experience of the professional. The main future challenge will be to find a real balance between technologically competent healthcare professionals and professionals willing to guarantee quality care, also based on practical skills and human relationships. It is essential to combine practical experience with new technologies to guarantee complete training.
Conflict of interest
The authors declare no competing interests
Financing
No funding to declare
Author contributions
All authors contributed equally to the work
REFERENCES
- Lange A, Koch J, Beck A, Neugebauer T, Watzema F, Wrona K, Dockweiler C. Learning with Virtual Reality in Nursing Education: Qualitative Interview Study Among Nursing Students Using the Unified Theory of Acceptance and Use of Technology Model JMIR Nursing 2020;3(1):e20249 URL: https://nursing.jmir.org/2020/1/e20249. DOI: https://doi.org/10.2196/20249
- Ginaldi L, Di Mascio R, Sepe I, Colleluori N, De Martinis M. The necessary change of direction for the nursing profession - letter on Petrosino et al. Intensive Crit Care Nurs. Jun 2024; 82:103638. DOI: https://doi.org/10.1016/j.iccn.2024.103638
- De Martinis M, Ginaldi L. (2024) Digital Skills to Improve Levels of Care and Renew Health Care Professions JMIR Med Educ. 10:e58743 URL: https://mededu.jmir.org/2024/1/e58743. DOI: https://doi.org/10.2196/58743
- Ginaldi L, Azzellino G, D'Olimpio A, Grilli V, De Martinis M., Nurse burnout: It is an urgent issue affecting the profession. Int Nurs Rev. 2024 Sep;71(3):411-412. DOI: https://doi.org/10.1111/inr.12987.
- Mundell WC, Kennedy CC, Szostek JH, Cook DA. Simulation technology for resuscitation training: a systematic review and meta-analysis. Resuscitation. 2013 Sep;84(9):1174–83. DOI: https://doi.org/10.1016/j.resuscitation.2013.04.016.
- Federico Semeraro, Giuseppe Ristagno, Gabriele Giulini, Tania Gnudi, Jihan Samira Kayal, Alessandro Monesi, Riccardo Tucci, Andrea Scapigliati, Virtual reality cardiopulmonary resuscitation (CPR): Comparison with a standard CPR training mannequin, Resuscitation, Volume 135, 2019, Pages 234-235, ISSN 0300-9572, DOI: https://doi.org/10.1016/j.resuscitation.2018.12.016
- Sadeghi AH, Peek JJ, Max SA, Smit LL, Martina BG, Rosalia RA, Bakhuis W, Bogers AJ, Mahtab EA. Virtual Reality Simulation Training for Cardiopulmonary Resuscitation After Cardiac Surgery: Face and Content Validity Study. JMIR Serious Games. 2022 Mar 2;10(1):e30456. DOI: https://doi.org/10.2196/30456.
![]()
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Sleep quality and sex-related differences in an older adult population: a web-based cross-sectional study
Emanuele Di Simone1, Noemi Giannetta2, Valerio Ragnoli3, Sara Dionisi4*, Aurora De Leo1,5, Gloria Liquori5, Nicolò Panattoni6, Victoria D’Inzeo3, Laura Tafaro3, Vassilios Papaspyropoulos7, Christian Napoli7, Fabio Fabbian8, Luciano De Biase3, Giovanni Battista Orsi6 & Marco Di Muzio3
- Nursing, Technical, Rehabilitation, Assistance and Research Direction - IRCCS Istituti Fisioterapici Ospitalieri - IFO, Rome, Italy
- UniCamillus-Saint Camillus International University of Health and Medical Sciences; Rome, Italy;
- Department of Clinical and Molecular Medicine, Sapienza University of Rome; Rome, Italy;
- Nursing Technical and Rehabilitation Department - DaTeR Azienda Unità Sanitaria Locale di Bologna; Bologna, Italy;
- Department of Biomedicine and Prevention - University of Rome Tor Vergata, Rome, Italy;
- Department of Public Health and Infectious Diseases, Sapienza University of Rome, Italy.
- Department of Medical Surgical Sciences and Translational Medicine, Sapienza University of Rome, Rome, Italy;
- Department of Medical Sciences, University of Ferrara, Italy.
* Corresponding author: Sara Dionisi, Nursing Technical and Rehabilitation Department - DaTeR Azienda Unità Sanitaria Locale di Bologna
E-mail: sara.dionisi@uniroma1.it
Cite this article
ABSTRACT
Introduction: Aging has significant economic and social implications leading to an increase in chronic diseases and reduced autonomy of the elderly. Sleep disorders are common in the elderly, manifesting reduced sleep quality.
Objective/Purpose: The study aimed to measure the prevalence of sleep disorders in older adults and assess sex differences in sleep quality and sleep problems.
Method: A cross-sectional study based on an online survey was performed according to the STROBE checklist, using pre-validated questionnaires (Pittsburgh Sleep Quality Index) distributed to a sample of older adults. This is the first study evaluating sex differences in sleep quality and problems in the Italian population context using the Pittsburgh Sleep Quality Index assessment tool. The study was conducted in a university hospital in Rome from October 2020 to November 2020, on patients aged >65 years, independent in activities of daily living, with comorbidities and on treatment with up to 2 medications.
Results: 59 patients were included in the study, with an average age of 71.12 years. The results show that among males, the prevalence of poor sleep quality was 51.9%, while among females, the prevalence of poor sleep quality was 62.5%. According to Shapiro-Wilk, the Pittsburgh Sleep Quality Index was not normally distributed. Pittsburgh Sleep Quality Index total scores in males did not differ significantly from females.
Conclusions: Considering scientific literature, recent studies have highlighted the prevalence of sleep disorders in the elderly population and their under-reporting. Providing early intervention not only improves the sleep quality of these people but may also reduce the risk of experiencing adverse health outcomes and susceptibility to frailty.
Keywords: sleep disorders, older adults, sleep quality, Pittsburgh Sleep Quality Index
INTRODUCTION
The increasing growth in life expectancy has produced a natural demographic transition, with a progressively ageing population associated with other variables such as declining fertility and reduced youth mortality [1]. Globally, people aged 65 and older, referred to as "older adults," are the fastest-growing population [2]. Based on the recorded upward trend in population growth, the estimate is that about 16 per cent of the world's population will be 65 years and older by 2050 [3]. According to Italian National Institute of Statistics (ISTAT) data, 33.3 per cent of the Italian population is expected to be in this age group in 2065 [4].
Biological factors, which are very complex to define, will be one of many characteristics differentiating populations and uncorrelated social and economic factors, such as retirement age [5].
Ageing has impactful economic and social implications, as it is a process that encompasses the decline of the body as a whole and the physical and mental capacity that increase with advancing age, leading to an increase in chronic diseases and reduced autonomy in this segment of the population [6]. At the Central Nervous System level, the various implications of its degeneration lead to functional alterations, sometimes even compatible with chronic degenerative cognitive diseases. These alterations include memory deficit, impaired balance maintenance, and sleep disorders [7]. The physiological changes that commonly occur with ageing influencing the sleep cycle bring the appearance of some natural disorders. The concomitance with comorbidities affects the individual's physical and mental health, causing them to feel depressed and helpless, very often also due to chronic pain[8-9]. The study of sleep quality and disorders is widespread among older people and nurses [1,8].
Sleep disorders are common in older adults and are present in up to 40-70% of the specific population, manifesting reduced sleep quality. The main features of sleep disorders in the elderly can be attributed to sleep-maintenance insomnia, repeated nocturnal awakenings, and decreased total sleep with a general decrease in sleep quality [10]. Sleep is a normal physiological process with a crucial therapeutic action and is characterised by a reduction in response to external stimuli and perceptual isolation. A key health element is the sleep-wake cycle, a constituent part of the circadian rhythm, regulated by the anterior hypothalamus and subject to influence by (already known) factors, such as light/darkness alternation, temperature, the action of certain hormones, and a psychological component [9]. The literature shows that the population needs to be aware of the importance of the health of lifestyles that ensure a regular circadian rhythm, sleep and light/darkness alternation [11]. Sleep regulation consists of the S-process, which regulates sleep stages, and the C-process, which controls the circadian pacemaker [12]. Sleep is divided into two phases NREM (Non-Rapid Eye Movement) and REM (Rapid Eye Movement) phase [13].
In older adults, there are some changes in sleep architecture [9]. First, there is an anticipation of the time of lying down in bed and an earlier awakening. There is also an increased sleep latency, that is, an increase in the period of being stationary in bed before falling asleep. At the same time, however, there is a reduction in the total sleep duration, which manifests fragmentation and an increase in nocturnal awakenings due to external stimuli. All this is reflected by an increase in daytime sleep, which is directly proportional to advancing age; it is found that 25 per cent of people aged 75 to 84 years report sleeping during the day [14].
Nicturia and polyuria occur in various conditions, such as diabetes and prostatic hypertrophy. The use of drugs such as diuretics and substances such as coffee and alcohol exacerbate them. These conditions are risk factors for nighttime falls in adult patients [14]. Bilotta states that increasing age leads to increasing frailty, which correlates strongly with falls [15]. The WHO states that 35% of people older than 65 experience a fall yearly, exceeding 42% once they reach 70 years of age [16].
Moreover, some studies have found a strong correlation between low sleep quality and the risk of falling in the elderly [17,18]. The same correlation is found with the use of some medications for the treatment of sleep disorders, including sedative-hypnotic drugs. In addition, the presence of nicturia, precisely in the sleep component related to increased nocturnal awakenings, is among the risk factors for falls during the night [17].
Finally, gender is a determining factor in human health, and women are more predisposed to the onset of sleep disorders, as they have a physiological vulnerability related to hormonal changes, in which alterations in sleep architecture occur, during the premenstrual period, pregnancy, and menopause [19–22].
About the findings in the literature, the ageing process of the population, which physiologically involves a decline in the body, also has important aspects to focus on. At the level of the central nervous system, one of the main problems that may emerge concerns alterations in the sleep cycle. Such alterations can affect a person's well-being by representing an important risk factor for possible related adverse events. Considering these scientific premises, the present study therefore aims to measure the prevalence of sleep disturbances in older adults to be able to identify strategies that may limit the risk of adverse events.
Objective: The present study aims to measure the prevalence of sleep disturbance in older adults by assessing sex differences in sleep quality and sleep disturbance.
MATERIALS AND METHODS
Study design
A cross-sectional study based on an online survey was performed, following the STROBE (Strengthening the Reporting of Observational Studies in Epidemiology) guidelines for cross-sectional study [23] to improve the quality of reporting using a pre-validated questionnaire distributed to a sample of inpatients older adults (Supplementary file 1).
Study Population.
The study population was selected according to a non-probability convenience sampling model. The choice of this sampling model was chosen by the researchers for the ease of recruiting the sample in the Public University Hospital of Rome where the study was conducted. The sample was selected based on specific social and clinical conditions detectable from the medical record, which allowed us to define the inclusion and exclusion criteria set out in the following paragraphs. Specifically, all elderly patients admitted to the hospital were selected, excluding emergency rooms and emergency departments. The choice not to include patients admitted to emergency departments is given by the fact that, in these contexts, the clinical conditions of the person could make both recruitment and completion of the questionnaires difficult.
Each eligible patient was explained the purpose of the study and was presented with the informed consent for participation. Each eligible patient was explained the purpose of the study and given informed consent to participate. Once the consent to participate was obtained through the signature of all participants, the link to access the online questionnaire completion was sent by e-mail. The online compilation of the questionnaire took place through Google Form platform. Anonymity was guaranteed through the assignment of an ID when completing the questionnaire. The study was conducted in a University Hospital in the city of Rome from October 2020 to November 2020.
Ethical consideration
All participants consented to the processing of data as required by EU Regulation 2016/679 [24]. To conduct the study, a formal request was submitted to the Ethics Committee, which was accepted and authorized on 04/26/2017 through the documentation identified with protocol number 343/17.
Inclusion criteria
Patients with the following characteristics were included in the study: absence of progressive neurological diseases (Alzheimer's, Parkinson's) or cognitive deterioration, ability and confidence with the computer and use of the Internet, presence of no more than 2 comorbidities, treated with no more than 2 drugs, age ≥ 65 years. The user's skills in the use of the smartphone were assessed at the time of the application for participation in the study through the filling out of the questionnaire itself.
Exclusion criteria.
Patients with no difficulties in space, time and orientation; and patients younger than 65 years of age with cognitive impairment or progressive neurological disease (Alzheimer's, Parkinson's) and with more than 2 comorbidities were excluded from this study.
Instruments
The Pittsburgh Sleep Quality Index (PSQI) is a retrospective scale used to assess standardised sleep quality [25]. It allows the assessment of possible sleep distribution and discriminates between "good" and "bad" sleepers. It constitutes a self-assessment of patients' sleep quality over the previous month [25].
This questionnaire consists of 19 items, grouped into 7 domains. The seven domains consist of sleep quality, sleep latency, sleep duration, sleep efficiency, sleep disturbance, sleep regulation, medication use, and diurnal dysfunctionality.
The overall score, ranged 0 to 21, is calculated by adding the scores of seven components, from 0 (no difficulty) to 3 scores (severe difficulty). Higher scores indicate worse sleep quality. Usually, a global score higher than five means relevant sleep disturbances in at least two components or moderate challenges in more than three components [25]. Poor sleep quality is defined as when the PSQI score is ≥ 5 points; good sleep quality is when the PSQI score is ≤ 5 points.
The patient fills out the questionnaire and chooses one of the four multiple-choice answers in each item that best describes his sleep over the past month.
The Italian PSQI showed an overall reliability coefficient (Cronbach's α) of 0.835, indicating a high degree of internal consistency [26], which was used in this study.
Statistical analysis
Statistical software IBM SPSS Statistics®, version 26 [27], was used in the statistical procedure. All data is analysed using descriptive analysis through absolute frequencies and percentages. Regarding continuous variables, authors used measures of central tendency like mean and standard deviation (SD) and median with interquartile range [Q1, Q3]. The Shapiro-Wilk test was used to test the normal distribution. According to Shapiro-Wilk, the PSQI were not normally distributed. Based on this consideration, the Mann–Whitney U-test was used. Statistical significance was set at p < 0.05 [28].
RESULTS
Sociodemographic characteristics of the study sample
A total of 59 older adults were included in this study. The median and interquartile ranges for the age of the study participants were 69.00 (65–91). The sample's mean age and standard deviation were 71.12 (± 6.24). Overall, 54.2% (n=32) patients were females, and 45.8% (n=27) were males.
Prevalence of sleep quality
Using the PSQI assessment tool, among the study participants, the prevalence of poor sleep quality was 57.6% (n=34); the prevalence of good sleep quality was 42.2% (n=25).
As shown in Table 1, participants reported a median bedtime of 11.00 pm [22:00, 24:00], a median wake time of 07.00 am [06:00, 08:00]. Most participants 64.4%, (n=38) self-reported a “fairly good” quality of sleep; only 15.3% (n=9) of participants reported a good quality of sleep.
| Variable | Mean ± SD median [Q1, Q3] |
|
| Bedtime | 21:45:00 ± 4:44:07 23:00:00 [22:00, 24:00] |
|
| Wake time | 07:08:58 ± 01:09:05 07:00:00 [06:00, 08:00] |
|
| Total sleep time (h) | 6.593 ± 1.45 7.00 [5.50, 7.00] |
|
| During the past month, how often have you had trouble sleeping because you: | ||
| a) Cannot get to sleep within 30 mins | 0.93 ± 1.065 | |
| b) Wake up in the middle of the night or early in the morning | 1.00 [0.00, 2.00] 1.22 ± 1.121 |
|
| c) Have to get up to use the bathroom | 1.00 [0.00, 2.00] 2.03 ± 1.059 |
|
| d) Cannot breathe comfortably | 2.00 [1.00, 3.00] 0.17 ± 0.461 |
|
| e) Cough or snore loudly | 0.00 [0.00, 0.00] 0.56 ± 0.876 |
|
| f) Feel too cold | 0.00 [0.00, 1.00] 0.41 ± 0.698 |
|
| g) Feel too hot | 0.00 [0.00, 1.00] 0.80 ± 0.979 |
|
| h) Have bad dreams | 0.00 [0.00, 2.00] 0.63 ± 0.849 |
|
| i) Have pain | 0.00 [0.00, 1.00] 0.93 ± 1.096 1.00 [0.00, 2.00] |
|
| PSQI total score | 6.4237 ± 3.00 7.00 [4.00, 9.00] |
|
Table 1. Pittsburgh Sleep Quality Index (PSQI) descriptive statistics on the overall sample
Specific questions on trouble sleeping in the last month showed 49.2% (n=29) were not having difficulties getting sleep within 30 minutes; 35.6 % (n=21) reported that they did not wake up in the middle of the night or early morning. However, during the past month, 47.5% (n=28) used to get up to use the bathroom thrice or more times a week. Most of the sample, self-reported no breathing problems (86.4%, n=51) and coughing or snoring loudly (64.4%, n=38). Most of the sample did not report difficulties in sleeping due to being too cold or too hot (41=69.5% and 31=52.5% respectively) or bad dreams (34=57.6%) or having pain (29=42.9%) during the last month. However, anxiety and concerns due to personal and familiar problems were the troubles sleeping in the previous month reported by 40.7% (n=24) of the sample.
As shown in Table 2, most participants reported good sleep efficacy (40.7% with scores ≥85%; 35.6% with scores between 75-84%), no use of sleep medication in the past month (72.9%), low levels of sleep disturbance (78.0% with a score of 1) and low levels of daytime dysfunction (78.0% with component scores of 0 or 1).
| Variable | Full sample (M ± SD)
n=59 |
Females (M ± SD)
n=32 |
Males (M ± SD)
n=27 |
Females vs Males
p-value |
| Age | 71.12 ± 6.240 | 70.59 ± 6.04 | 71.74 ± 6.52 | 0.45 |
| Bedtime | 21:47:02 ± 4:34:54 | 21:58:35 ± 3:47:08 | 21:28:53 ± 5:43:36 | 0.31 |
| Wake time | 07:08:58 ± 01:09:05 | 06:58:07 ± 00:58:29 | 07:21:51 ± 01:19:04 | 0.27 |
| Total sleep time (h) | 6.59 ± 1.45 | 6.51 ± 1.52 | 6.685 ± 1.39 | 0.91 |
| PSQI total score | 6.42 ± 3.00 | 6.78 ± 3.25 | 6.00 ± 2.67 | 0.38 |
|
PSQI component scores |
||||
| Sleep duration | 1.08 ± 0.82 | 1.13 ± 0.87 | 1.04 ± 0.75 | 0.87 |
| Sleep efficacy | 0.91 ± 1.05 | 1.03 ± 0.99 | 0.77 ± 1.12 | 0.20 |
| Sleep latency | 0.92 ± 0.95 | 1.16 ± 1.08 | 0.63 ± 0.68 | 0.06 |
| Sleep disturbances | 1.21 ± 0.40 | 1.23 ± 0.42 | 1.19 ± 0.39 | 0.70 |
| Sleep quality | 1.08 ± 0.67 | 1.06 ± 0.71 | 1.11 ± 0.64 | 0.78 |
| Sleep medication | 0.54 ± 1.02 | 0.53 ± 1.04 | 0.56 ± 1.01 | 0.76 |
| Daytime dysfunction | 0.67 ± 0.70 | 0.65 ± 0.70 | 0.70 ± 0.72 | 0.78 |
| Note. the range for the PSQI component score variables is 0 to 3. For all PSQI variables,
higher scores indicate worse sleep. |
||||
Table 2. Pittsburgh Sleep Quality Index (PSQI) and components: descriptive statistics and sex differences
Sex differences in sleep
Sex differences in sleep quality and PSQI component levels are shown in Table 2. Females reported going to bed 30 minutes later than males. At the same time, females reported waking up 23 minutes before than males. However, no significant differences were found between the two groups (p=0.31; p=0.27).
Using the PSQI assessment tool, among the males, the prevalence of poor sleep quality was 51.9% (n=14), and good sleep quality was 48.1% (n=13). While among females, the prevalence of poor sleep quality was 62.5% (n=20), and the majority of good sleep quality was 37.5% (n=12).
According to Shapiro-Wilk, the PSQI were distributed elsewhere. PSQI total scores in males (Median= 6.0) did not differ significantly from females (Median = 7.0), U= 489.000, z= 0.873, p=0.38. No differences were found regarding the sleep duration (U=441.500, z=0.156, p=0.87), sleep efficacy (U= 510.000, z= 1.271, p=0.20, sleep latency (U= 544.500, z=1.821, p=0.06), sleep disturbance (U= 435.500, z= 0.378, p=0.70), sleep quality (U= 417.000, z= -0.268, p=0.78), sleep medication (U=416.500, z= -0.302, p=0.76) and daytime dysfunction (U=416.000, z= 0.788, p=0.78) between males and females patients included.
DISCUSSION
This observational study aimed to measure sleep disorder prevalence in older adults. The secondary endpoint of this study was to assess sex differences in sleep quality and disorders. The assessment tool used to achieve this goal was the Pittsburgh Sleep Quality Index (PSQI), a self-assessment of the quality of sleep in patients in the last month [25].
In our findings, among the study participants, the prevalence of poor sleep quality was 57.6%, consistent with a previous study reporting high rates of poor sleep quality, ranging from 40% to 70%, among older adults [9]. As mentioned in the introduction, sleep problems may be caused or exacerbated by institutional settings.
According to our findings, most participants reported good sleep efficacy (40.7% with scores ≥85%; 35.6% with scores between 75-84%), no use of sleep medication in the past month (72.9%), low levels of sleep disturbance (78.0% with a score of 1) and low levels of daytime dysfunction (78.0% with component scores of 0 or 1). These results are consistent with other studies [29,30].
Some epidemiological studies have shown that women experience more stress, anxiety and depression than men [31,32]. Based on this consideration, the secondary outcome of this study was to assess sex differences in sleep quality and problems among - older - men and women.
The prevalence of poor sleep quality was high in both male and female older adults. More than 60% of female and 50% of male older adults were categorised as poor sleepers. These findings are similar to another study's result [33].
However, in our findings, sex differences were not statistically significant. These findings agree with Zhu and colleagues [30], while these results contrast with some of the previous studies, where elderly females had a higher poor sleep quality than older men [33-35]. Specifically, stress, alcohol consumption and physical exercise are the variables related to a good or poor quality of sleep, according to Quan et al. [33].
Beyond sex differences, many studies show that PSQI was significantly correlated with higher depression and anxiety [36,37]. According to that, most of our participants declared that anxiety and concerns due to personal and familiar problems were the troubles sleeping last month.
To our knowledge, this is the first study evaluating sex differences in sleep quality and problems in the Italian population context using the PSQI assessment tool.
Limitations
This study has several limitations - first, the sample size. Our overall study population was fit but small, which may limit the applicability of our findings, so we recommend caution in interpretation above all for the results in sex differences. For this reason, Cronbach's alpha is also inadequate (0.38), suggesting the need to increase the sample through a larger observational study. In this study, the sampling power was not calculated due to the choice of the sampling method.
All these further limits the generalisation of the results. In addition, the sleep quality measurement was based on a web self-reported evaluation without additional data such as sedentary, alcohol consumption or residence of the sample to contextualise sleep quality with conditions like traffic, lighting, or recreation nightlife activities. Finally, due to the way the authors administered the instrument (web-based survey), an accurate response rate could not be assessed.
CONCLUSION
Considering the scientific literature, several studies have highlighted the prevalence of sleep disorders in the elderly population and their underestimation [29,38]. Furthermore, the elderly population is often subjected to the use of multiple drugs that can lead to physiological changes that can in turn affect the quality of sleep [39-42]. A therapeutic plan with diuretics, for example, could influence the quality of sleep. In fact, nocturia seems to be prevalent in the elderly population. It can be associated with an increased risk of falls and negative outcomes for the continuity of sleep, continuously fragmented by awakenings. While frailty does not imply the existence of sleep disorders, on the contrary, these are correlated with a risk of cognitive and physical defects when they precede the onset of dementia [43]. Analysing the quality of sleep of elderly people, in relation to their socio-health condition could be very useful to identify interventions aimed at improving certain situations. Providing early intervention not only improves the quality of sleep for these people but can also reduce the risk of experiencing negative health outcomes and susceptibility to frailty.
Funding statement
This research did not receive any specific grant from funding agencies in the public, commercial, or not for profit sectors.
Conflict of interest
The authors report no conflict of interest.
Authors’ contribution
Study design: V.R., M.D.M., N.G.; C.C.; Data collection: V.D.I., V.R., E.D.S., S.D.; Data analysis: N.G., A.D.L., G.L., N.P..; Study supervision: G.B.O.; C.N., M.D.M.; V.P.; L.T.; F.F.; P.S.L.; Manuscript writing: N.G.; V.R.; N.P.; M.M.; Critical revisions for important intellectual content: M.D.M
Acknowledgements
None.
Supplementary material
STROBE Statement—Checklist of items that should be included in reports of cross-sectional studies.
| Item No | Recommendation | Page No | |
| Title and abstract | 1 | (a) Indicate the study’s design with a commonly used term in the title or the abstract | 1 |
| (b) Provide in the abstract an informative and balanced summary of what was done and what was found | 1 | ||
| Introduction | |||
| Background/rationale | 2 | Explain the scientific background and rationale for the investigation being reported | 1-2 |
| Objectives | 3 | State specific objectives, including any prespecified hypotheses | 1-2 |
| Methods | |||
| Study design | 4 | Present key elements of study design early in the paper | 3-4 |
| Setting | 5 | Describe the setting, locations, and relevant dates, including periods of recruitment, exposure, follow-up, and data collection | 3-4 |
| Participants | 6 | (a) Give the eligibility criteria, and the sources and methods of selection of participants | 3-4 |
| Variables | 7 | Clearly define all outcomes, exposures, predictors, potential confounders, and effect modifiers. Give diagnostic criteria, if applicable | 3-4 |
| Data sources/ measurement | 8* | For each variable of interest, give sources of data and details of methods of assessment (measurement). Describe comparability of assessment methods if there is more than one group | 3-4 |
| Bias | 9 | Describe any efforts to address potential sources of bias | 3-4 |
| Study size | 10 | Explain how the study size was arrived at | 3-4 |
| Quantitative variables | 11 | Explain how quantitative variables were handled in the analyses. If applicable, describe which groupings were chosen and why | 3-4 |
| Statistical methods | 12 | (a) Describe all statistical methods, including those used to control for confounding | 3-4 |
| (b) Describe any methods used to examine subgroups and interactions | 3-4 | ||
| (c) Explain how missing data were addressed | 3-4 | ||
| (d) If applicable, describe analytical methods taking account of sampling strategy | - | ||
| (e) Describe any sensitivity analyses | n.a. | ||
| Results | |||
| Participants | 13* | (a) Report numbers of individuals at each stage of study—eg numbers potentially eligible, examined for eligibility, confirmed eligible, included in the study, completing follow-up, and analysed | 4-6 |
| (b) Give reasons for non-participation at each stage | 4-6 | ||
| (c) Consider use of a flow diagram | 4-6 | ||
| Descriptive data | 14* | (a) Give characteristics of study participants (e.g. demographic, clinical, social) and information on exposures and potential confounders | 4-6 |
| (b) Indicate number of participants with missing data for each variable of interest | 4-6 | ||
| Outcome data | 15* | Report numbers of outcome events or summary measures | 4-6 |
| Main results | 16 | (a) Give unadjusted estimates and, if applicable, confounder-adjusted estimates and their precision (e.g. 95% confidence interval). Make clear which confounders were adjusted for and why they were included | 4-6 |
| (b) Report category boundaries when continuous variables were categorized | n.a. | ||
| (c) If relevant, consider translating estimates of relative risk into absolute risk for a meaningful time period | n.a | ||
| Other analyses | 17 | Report other analyses done—eg analyses of subgroups and interactions, and sensitivity analyses | n.a |
| Discussion | |||
| Key results | 18 | Summarise key results with reference to study objectives | 6-7 |
| Limitations | 19 | Discuss limitations of the study, taking into account sources of potential bias or imprecision. Discuss both direction and magnitude of any potential bias | 6-7 |
| Interpretation | 20 | Give a cautious overall interpretation of results considering objectives, limitations, multiplicity of analyses, results from similar studies, and other relevant evidence | 6-7 |
| Generalisability | 21 | Discuss the generalisability (external validity) of the study results | 6-7 |
| Other information | |||
| Funding | 22 | Give the source of funding and the role of the funders for the present study and, if applicable, for the original study on which the present article is based | 7 |
*Give information separately for exposed and unexposed groups.
Note: An Explanation and Elaboration article discusses each checklist item and gives methodological background and published examples of transparent reporting. The STROBE checklist is best used in conjunction with this article (freely available on the Web sites of PLoS Medicine at http://www.plosmedicine.org/, Annals of Internal Medicine at http://www.annals.org/, and Epidemiology at http://www.epidem.com/). Information on the STROBE Initiative is available at www.strobe-statement.org.
REFERENCES
Ferreira LK, Meireles JFF, Ferreira MEC. Evaluation of lifestyle and quality of life in the elderly: a literature review. Rev Bras Geriatr E Gerontol. ottobre 2018;21(5):616–27.
- Jarzebski MP, Elmqvist T, Gasparatos A, Fukushi K, Eckersten S, Haase D, et al. Ageing and population shrinking: implications for sustainability in the urban century. Npj Urban Sustain. 27 maggio 2021;1(1):17. Doi: 10.1038/s42949-021-00023-z.
- United Nations. World population prospects [Internet]. 2019. Available at: https://population.un.org/wpp/publications/files/wpp2019_highlights.pdf. [last access, 01 september 2024].
- Italian National Institute of Statistics. Il futuro demografico del paese [Internet]. 2018. Available at: https://www.istat.it/it/files/2018/05/previsioni_demografiche.pdf. [last access, 01 september 2024].
- Khorshidi A, Rostamkhani M, Farokhi R, Abbasi-Ghahramanloo A. Association between quality of life, sleep quality and mental disorders in Iranian older adults. Sci Rep. 20 settembre 2022;12(1):15681. Doi: 10.1038/s41598-022-20013-0.
- Alves Faria ADC, Martins MM, Ribeiro OMPL, Ventura-Silva JMA, Teles PJFC, Laredo-Aguilera JA. Adaptation and Validation of the Individual Lifestyle Profile Scale of Portuguese Older Adults Living at Home. Int J Environ Res Public Health. 29 aprile 2022;19(9):5435. Doi: 10.3390/ijerph19095435
- Pera A, Campos C, López N, Hassouneh F, Alonso C, Tarazona R, et al. Immunosenescence: Implications for response to infection and vaccination in older people. Maturitas. settembre 2015;82(1):50–5. Doi: 10.1016/j.maturitas.2015.05.004.
- Di Simone E, Fabbian F, Giannetta N, Dionisi S, Renzi E, Cappadona R, et al. Risk of medication errors and nurses’ quality of sleep: a national cross-sectional web survey study. Eur Rev Med Pharmacol Sci. giugno 2020;24(12):7058–62. Doi: 10.26355/eurrev_202006_21699.
- Gulia KK, Kumar VM. Sleep disorders in the elderly: a growing challenge. Psychogeriatrics. maggio 2018;18(3):155–65. Doi: 10.1111/psyg.12319.
- Praharaj S, Gupta R, Gaur N. Clinical practice guideline on management of sleep disorders in the elderly. Indian J Psychiatry. 2018;60(7):383. Doi: 10.4103/0019-5545.224477.
- Di Simone E, Panattoni N, De Giorgi A, Rodríguez-Muñoz P, Bondanelli M, Rodríguez-Cortés F, et al. Googling Insomnia, Light, Metabolism, and Circadian: A Population Interest Simple Report. Brain Sci. 8 dicembre 2022;12(12):1683. Doi: https://doi.org/10.3390/brainsci12121683.
- Suzuki K, Miyamoto M, Hirata K. Sleep disorders in the elderly: Diagnosis and management. J Gen Fam Med. aprile 2017;18(2):61–71. Doi: 10.1002/jgf2.27.
- A ustralian and N ew Z ealand Society for Geriatric Medicine: Position Statement – Sleep in the older person. Australas J Ageing. settembre 2015;34(3):203–12. Doi: 10.1111/ajag.12192.
- Foley DJ, Vitiello MV, Bliwise DL, Ancoli-Israel S, Monjan AA, Walsh JK. Frequent Napping Is Associated With Excessive Daytime Sleepiness, Depression, Pain, and Nocturia in Older Adults: Findings From the National Sleep Foundation ‘2003 Sleep in America’ Poll. Am J Geriatr Psychiatry. aprile 2007;15(4):344–50. Doi: 10.1097/01.JGP.0000249385.50101.67.
- Bilotta C, Nicolini P, Casè A, Pina G, Rossi S, Vergani C. Frailty syndrome diagnosed according to the Study of Osteoporotic Fractures (SOF) criteria and adverse health outcomes among community-dwelling older outpatients in Italy. A one-year prospective cohort study. Arch Gerontol Geriatr. marzo 2012;54(2):e23–8. Doi: 10.1016/j.archger.2011.06.037.
- World Health Organization. WHO global report on falls prevention in older age [Internet]. 2008. Available at: https://www.who.int/publications/i/item/9789241563536. last access, 01 september 2024].
- Berry SD, Lee Y, Cai S, Dore DD. Nonbenzodiazepine Sleep Medication Use and Hip Fractures in Nursing Home Residents. JAMA Intern Med. 13 maggio 2013;173(9):754. Doi: 10.1001/jamainternmed.2013.3795.
- Finkle WD, Der JS, Greenland S, Adams JL, Ridgeway G, Blaschke T, et al. Risk of Fractures Requiring Hospitalization After an Initial Prescription for Zolpidem, Alprazolam, Lorazepam, or Diazepam in Older Adults. J Am Geriatr Soc. ottobre 2011;59(10):1883–90. Doi: 10.1111/j.1532-5415.2011.03591.x
- Baker FC, Driver HS. Circadian rhythms, sleep, and the menstrual cycle. Sleep Med. settembre 2007;8(6):613–22. Doi: 10.1016/j.sleep.2006.09.011.
- Guidozzi F. Sleep and sleep disorders in menopausal women. Climacteric. aprile 2013;16(2):214–9. Doi: 10.3109/13697137.2012.753873.
- Parry BL, Fernando Martínez L, Maurer EL, López AM, Sorenson D, Meliska CJ. Sleep, rhythms and women’s mood. Part II. Menopause. Sleep Med Rev. giugno 2006;10(3):197–208. Doi: 10.1016/j.smrv.2005.09.004.
- Parry BL, Fernando Martínez L, Maurer EL, López AM, Sorenson D, Meliska CJ. Sleep, rhythms and women’s mood. Part I. Menstrual cycle, pregnancy and postpartum. Sleep Med Rev. aprile 2006;10(2):129–44. Doi: 10.1016/j.smrv.2005.09.003.
- Von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for Reporting Observational Studies. Ann Intern Med. 16 ottobre 2007;147(8):573. Doi: 10.1097/EDE.0b013e3181577511.
- Regolamento (UE) 2016/679 del Parlamento e del Consiglio relativo alla protezione delle persone fisicche con riagurado al trattamento dei dati personali, nonchè alla libera circolazione di tali dati che abroga la direttiva 95/46/CE (regolamento generale sulla protezione dei dati). 27 aprile 2016. Available at: https://eur-lex.europa.eu/legal-content/IT/TXT/PDF/?uri=CELEX:32016R0679. [last access, 01 september 2024].
- Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh sleep quality index: A new instrument for psychiatric practice and research. Psychiatry Res. maggio 1989;28(2):193–213. Doi: 10.1016/0165-1781(89)90047-4.
- Curcio G, Tempesta D, Scarlata S, Marzano C, Moroni F, Rossini PM, et al. Validity of the Italian Version of the Pittsburgh Sleep Quality Index (PSQI). Neurol Sci. aprile 2013;34(4):511–9. Doi: 10.1007/s10072-012-1085-y.
- IBM SPSS Statistics 26-Guida per l'utente del sistema principale. Available at: https://www.ibm.com/docs/en/SSLVMB_26.0.0/pdf/it/IBM_SPSS_Statistics_Core_System_User_Guide.pdf. [last access, 01 september 2024].
- Greenland S, Senn SJ, Rothman KJ, Carlin JB, Poole C, Goodman SN, et al. Statistical tests, P values, confidence intervals, and power: a guide to misinterpretations. Eur J Epidemiol. aprile 2016;31(4):337–50. Doi: 10.1007/s10654-016-0149-3.
- Orhan FÖ, Tuncel D, Taş F, Demirci N, Özer A, Karaaslan MF. Relationship between sleep quality and depression among elderly nursing home residents in Turkey. Sleep Breath. dicembre 2012;16(4):1059–67. Doi: 10.1007/s11325-011-0601-2.
- Zhu X, Hu Z, Nie Y, Zhu T, Chiwanda Kaminga A, Yu Y, et al. The prevalence of poor sleep quality and associated risk factors among Chinese elderly adults in nursing homes: A cross-sectional study. Doering S, curatore. PLOS ONE. 15 maggio 2020;15(5):e0232834. Doi: 10.1371/journal.pone.0232834.
- Hodes GE, Epperson CN. Sex Differences in Vulnerability and Resilience to Stress Across the Life Span. Biol Psychiatry. September 2019;86(6):421–32. Doi: 10.1016/j.biopsych.2019.04.028.
- Salari N, Hosseinian-Far A, Jalali R, Vaisi-Raygani A, Rasoulpoor S, Mohammadi M, et al. Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: a systematic review and meta-analysis. Glob Health. dicembre 2020;16(1):57.
- Quan SA, Li YC, Li WJ, Li Y, Jeong JY, Kim DH. Gender Differences in Sleep Disturbance among Elderly Koreans: Hallym Aging Study. J Korean Med Sci. 2016;31(11):1689. Doi: 10.3346/jkms.2016.31.11.1689.
- Liu X, Liu L. Sleep habits and insomnia in a sample of elderly persons in China. Sleep. dicembre 2005;28(12):1579–87. PMID: 16408418.
- Madrid-Valero JJ, Martínez-Selva JM, Ribeiro Do Couto B, Sánchez-Romera JF, Ordoñana JR. Age and gender effects on the prevalence of poor sleep quality in the adult population. Gac Sanit. gennaio 2017;31(1):18–22. Doi: 10.1016/j.gaceta.2016.05.013.
- Bayrak M, Çadirci K. Quality of Sleep in Elderly Patients with Diabetes Mellitus from Turkey: A Cross-Sectional Observational Study. Exp Aging Res. 8 agosto 2022;48(4):373–86. Doi: 10.1080/0361073X.2021.1989929.
- Essien SK, Feng CX, Sun W, Farag M, Li L, Gao Y. Sleep duration and sleep disturbances in association with falls among the middle-aged and older adults in China: a population-based nationwide study. BMC Geriatr. dicembre 2018;18(1):196. Doi: 10.1186/s12877-018-0889-x.
- Tafaro L, Cicconetti P, Baratta A, Brukner N, Ettorre E, Marigliano V, et al. Sleep quality of centenarians: Cognitive and survival implications. Arch Gerontol Geriatr. gennaio 2007;44:385–9. Doi: 10.1016/j.archger.2007.01.054.
- Dionisi S, Muñoz‐Alonso A, Giannetta N, Aranburu‐Imatz A, López‐Soto PJ, Galey‐Chica PA, et al. Knowledge, Attitudes, and Behavior in the administration of medication in the home care setting: Cross‐cultural Spanish adaptation. Public Health Nurs. novembre 2023;40(6):817–25. Doi: 10.1111/phn.13235.
- Dionisi S, Giannetta N, Maselli N, Di Muzio M, Di Simone E. Medication errors in homecare setting: An Italian validation study. Public Health Nurs Boston Mass. novembre 2021;38(6):1116–25. Doi: 10.1111/phn.12946.
- Liquori G, De Leo A, Di Simone E, Dionisi S, Giannetta N, Ganci E, et al. Medication Adherence in Chronic Older Patients: An Italian Observational Study Using Medication Adherence Report Scale (MARS-5I). Int J Environ Res Public Health. 25 aprile 2022;19(9):5190. Doi: 10.3390/ijerph19095190.
- Reading SR, Black MH, Singer DE, et al. Risk factors for medication non-adherence among atrial fibrillation patients. BMC Cardiovasc Disord. 2019;19(1):38. Published 2019 Feb 11. doi:10.1186/s12872-019-1019-1
- Kojima G, Taniguchi Y, Iliffe S, Walters K. Frailty as a Predictor of Alzheimer Disease, Vascular Dementia, and All Dementia Among Community-Dwelling Older People: A Systematic Review and Meta-Analysis. J Am Med Dir Assoc. ottobre 2016;17(10):881–8. Doi: 10.1016/j.jamda.2016.05.013.
![]()
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Effectiveness of palliative home care on clinical, emotional and economic well-being at the end of life: a narrative review
Vincenza Giordano 1, Assunta Guillari 2, Aniello Lanzuise 3, Michele Virgolesi 2*,
Lidia Di Vaio 4 & Teresa Rea 2
- Department of General Surgery and Women's Health, A.O.R.N. (Hospital Company of National Significance) Antonio Cardarelli, Naples (Italy).
- Department of Public Health, University Federico II of Naples, Naples (Italy).
- Corporate Health Management, A.O.R.N. (Hospital Company of National Significance) Sant'Anna e San Sebastiano, Caserta (Italy).
- School of Medicine and Surgery, University Federico II of Naples, Naples (Italy).
* Corresponding author: Michele Virgolesi Ph.D., Department of Public Health, University Federico II of Naples, Sergio Pansini street no. 5, 80131, Naples (Italy). Email: michele.virgolesi@unina.it
Cite this article
ABSTRACT
Introduction: Palliative home care is essential for terminally ill patients. This integrated approach is not limited to physical care, but also embraces the psychological, social and spiritual aspects of the patient. This model of care, focused on the patient and their family, aims to ensure quality health care during the advanced stage of a disease. In addition, by reducing the need for hospital admissions, palliative home care reduces costs, providing a sustainable alternative for the health system.
Objective: To describe the knowledge related to the clinical, emotional and economic impact of palliative home care in cancer patients
Materials and Methods: A narrative review was conducted using databases such as PubMed, Cinahl and Cochrane Library between December 2023 and March 2024, using the Population, Intervention, Outcome (PIO) methodology. The survey generated 551 articles, of which only 6 were relevant to the study. The selection of studies was guided by inclusion and exclusion criteria, with a quality assessment using the Dixon Woods instrument.
Results: The studies included in the review have demonstrated a positive and significant impact of palliative home care on the well-being and quality of life of terminal cancer patients. Some of these studies have examined the clinical efficacy of such treatments in mitigating the patient's symptoms, with conflicting results: while some have shown positive efficacy, others have not found the same result. Regarding the cost-effectiveness, the analysis highlighted a lack of definitive evidence on the possible economic advantage of palliative home care compared to hospital care.
Conclusions: Palliative home care emerges as a crucial element in the nursing care of the terminally ill cancer patient: it offers essential psychological support, enabling patients to feel understood and listened to with regard to their needs and requirements. However, there are some discrepancies, particularly with regard to economic effects and symptom control.
Keywords: palliative home care; terminal care; quality of care; quality of life; cost-effectiveness analysis.
INTRODUCTION
Cancer represents one of the most significant global public health challenges of our time, with a significant and tangible impact on the lives of patients and their families [1,2]. Updated estimates by the International Agency for Research on Cancer (IARC), report almost 20 million new cancer cases worldwide (including non-melanoma skin cancers – NMSC) and 9.7 million cancer deaths (including NMSC). Data indicate that about one in five men or women develop cancer during their lifetime, while about one in nine men and one in 12 women die from it [3].
Over the years, the efforts of the scientific community have focused on improving the quality of life of cancer patients, who find themselves facing complex and challenging obstacles due to the disease. In this perspective, palliative care (PC), understood as the "active and holistic care of individuals of all ages with significant health-related suffering due to serious illness, and especially those nearing the end of life" [4] aims to improve the quality of life of patients, their families and caregivers. [5]
The typical patient undergoing palliative care for advanced cancer is often an older or elderly person with a diagnosis of metastatic or locally advanced malignancy, where curative options are limited or unavailable. This individual has probably been through numerous lines of cancer treatment, including surgery, chemotherapy and radiotherapy, which over time have led to a progressive reduction in quality of life due to cumulative side effects and the disease itself [6]. The clinical condition is characterised by complex and multidimensional symptoms, such as chronic pain, dyspnoea, pronounced asthenia, cachexia, and gastrointestinal symptoms such as nausea and constipation. The patient may also manifest cognitive disorders or psycho-emotional symptoms, such as anxiety, depression and a sense of loss of autonomy, which reflect the heavy psychological impact of the terminal illness [7].
From the socio-familial point of view, the patient is often surrounded by a support network of close family members, but is confronted with the difficulty of having to accept the increasing dependence on others for activities of daily living. Often, this person is in ongoing dialogue with the palliative care team to manage symptoms and make shared decisions about end-of-life care while seeking to maintain some dignity and comfort in the remaining time [8].
According to the World Health Organisation (WHO), PC represents one of the fundamental pillars of health care, involving more than 56.8 million people worldwide annually [9,10]. In Italy, about 1–1.4% of the population needs palliative care, recognised as an integral part of the human right to health [11,12]. In this context, palliative home care plays a crucial role. Palliative home care, in fact, is reflected in a model of care focused on the person, aimed at ensuring high-quality health care [5]. On the physical side, they alleviate debilitating symptoms associated with disease, such as pain, nausea and vomiting, reducing the cancer patient's physical suffering and improving his or her clinical well-being through pharmacological and non-pharmacological therapies [13, 14]. On the emotional level, they offer complete psychological support to the patient and their family members, helping to meet their needs, in order to mitigate emotional distress and achieve spiritual balance [14-16]. This approach not only improves the quality of life of the terminally ill patient, but also alleviates the stress and anxiety of family members, creating a comfortable environment [17]. In the context of home care, nurses play a fundamental role in the delivery of palliative care, often representing the first point of contact for cancer patients. Growing evidence demonstrates the significant positive impact nurses have on the quality of care provided, improving symptom management, emotional support and overall coordination of care [18]. They are committed to creating a safe and efficient home environment, actively collaborating with the patient and family [18]. They instruct the latter on self-care techniques and the use of necessary medical equipment, promoting their autonomy [19]. They plan home care according to individual needs, constantly monitor the patient's clinical conditions and adapt interventions in a timely manner, acting promptly when necessary [19]. Finally, during the terminal stages of the disease, they provide support to the patient and caregivers, aimed at ensuring dignity and peace of mind, facilitating a respectful transition to death [12]. In addition, a study revealed that home care for cancer patients not only optimises their satisfaction, but also results in a more positive experience with a significant reduction in healthcare costs [20]. Patients receiving palliative home care are less likely to be hospitalised or go to the emergency room than those receiving standard care. This helps to reduce the frequency of hospital admissions, days spent in hospitals or care facilities, and medical services used, thus lowering the overall costs of end-of-life care [20-22]. It is estimated that care costs are reduced by about 34% in patients managed through PC compared to those who do not have access to PC.
In light of this, investigating the clinical, emotional and economic effectiveness of palliative home care appears to be of strategic importance in order to improve the approach to end-of-life care for cancer patients.
Objective
To describe the knowledge related to the clinical, emotional and economic impact of palliative home care in cancer patients
MATERIALS AND METHODS
A narrative review was conducted in compliance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses Statement (PRISMA) [23] and the guidelines for writing a narrative review to be published in peer-reviewed journals [24].
Study design
The research aims to answer the following question, formulated according to the Population, Intervention, Outcome (PIO) methodology: To what extent does palliative home care help to ensure clinically, emotionally and economically effective care for patients with terminal cancer over the age of 18?
The PIO defines the population subject to analysis, the intervention to be implemented and the outcomes (Table 1).
| P | Patients > 18 years of age with terminal cancer |
| I | Palliative home care |
| O | Clinical, emotional and economic effectiveness |
Table 1. Question according to the PIO method.
Research strategy
Bibliographic research was conducted in the period between the end of December 2023 and March 2024, consulting the following scientific databases: PubMed, Cinahl, and the Cochrane Library. The keywords used for the research were: "palliative care", "palliative home care", "home care services", "home-based palliative care", "cancer", "cancer patients", "terminally ill", "terminal cancer", "quality of care", "quality of life", "cost-effectiveness analysis", "nurse-patient relations". The keywords were combined through the use of the Boolean operators "AND" and "OR", which made it possible to filter the results and make the search more specific.
Subsequently, to obtain general information on palliative care, websites of national bodies and
scientific associations were consulted. These include the official websites of the Istituto Superiore della Sanità and the Ministry of Health, as well as those of associations such as the Italian Society of Palliative Care (SICP), the Italian Association of Medical Oncology (AIOM), the Italian Association of Cancer Patients (AIMAC) and the European Society for Medical Oncology (ESMO).
Inclusion and exclusion criteria
During the first phase of research and the selection of studies, specific inclusion and exclusion criteria were defined for the various databases, such as PubMed, Cinahl and the Cochrane Library. A restricted time criterion was applied, limiting the survey to articles published between 2019 and 2024. We included: a) primary studies; b) secondary studies; c) articles on patients with cancer over the age of 18; d) articles in English and Italian; e) articles available free of charge for the abstract and full text.
The following were excluded: a) studies concerning patients with oncological diseases under the age of 18 years and those concerning patients with non-oncological diseases; b) articles published before 2019 or which did not meet the stipulated time interval; c) articles written in a language other than English or Italian.
Selection of studies
The survey yielded a total of 551 articles (389 on PubMed, 80 on Cinahl and 82 from the Cochrane Library).
The articles obtained from the three databases were analysed in the preliminary phase. 17 duplicate articles were excluded. The remaining 534 were examined by title and abstract. Of these, 485 were discarded because they were not relevant to the main theme or were inconsistent with the inclusion criteria. Of the 49 remaining articles, the full text was examined. Of these, 43 were excluded from the review because they were not suitable for the search objective and inclusion criteria when reading the full text; 6 articles were included.
The method used in the selection of articles for this review is illustrated below in a flowchart compliant with the PRISMA-ScR (PRISMA Extension for Scoping Reviews) methodology [20]. This diagram highlights the final choice of the included articles (Figure 1).

Figure 1. Flowchart model of PRISMA-ScR (PRISMA Extension for Scoping Reviews).
Quality Assessment
To assess the methodological quality and homogeneity of the studies included in the review, the method proposed by Dixon-Woods was used by means of a specific checklist [25]. This checklist comprises five domains to assess the methodological quality of the studies, and each article was assigned an overall rating based on the assessment of these domains. Studies that received a score of less than 3 "yes" answers were excluded from the analysis. Those with 3 "yes" answers were considered discrete, while studies with 4 "yes" answers were classified as good and those with 5 "yes" answers were considered to be of excellent quality (Table 2).
| Author(s), year | Are the aims and objectives of the research clearly stated? | Is the research design clearly specified and appropriate to the purposes and objectives of the research? | Do the researchers provide a clear account of the process by which their results were reproduced? | Do researchers present enough data to support their interpretations and conclusions? | Is the method of analysis appropriate and adequately explained? | SCORE |
| Patel et al., 2023 | YES | YES | YES | YES | YES | Excellent |
| Riolfi al., 2021 | YES | YES | YES | YES | YES | Excellent |
| Shepperd et al., 2021 | YES | YES | YES | YES | YES | Excellent |
| Biswas al., 2022 | NO | YES | YES | YES | YES | Good |
| Constantinou et al., 2022 | YES | YES | YES | YES | YES | Excellent |
| Kim et al., 2022 | YES | YES | YES | YES | YES | Excellent |
Table 2. Quality appraisal according to Dixon-Woods scale
RESULTS
The results of the review highlighted six studies relevant to the research objective. These include two quantitative cross-sectional studies [26,27], a study using mixed methods [28], a retrospective study [29], a systematic review [30], and finally a cost-effectiveness study [31]. The studies were conducted in several countries, including Bangladesh [26], the Republic of Cyprus [27], India [28], Italy [29], the United Kingdom [30] and Korea [31]. The studies selected by the review involve a total of 1702 patients with cancer. 68 patients participated in the mixed study [28], 375 patients in the retrospective cohort study [29], 1128 patients in the systematic review [30], while 131 patients were involved in the remaining quantitative cross-sectional studies [26,27]. The cost-effectiveness analysis considered a hypothetical cohort of patients with terminal cancer [31]. In two studies [28,29], patients enrolled were predominantly male; in one observational study [26], by contrast, 76.5% of patients were female. Only in one study were there similar proportions between men and women [30]. Of the six included studies, the mixed method study compared palliative home care with hospice care [28], while two studies [30,31] compared palliative home care with the usual palliative care in inpatient units. The main characteristics of the studies are summarised in the following summary table (Table 3);
| Author, year | Study design | Population | Country in which the study was carried out | Goal of the study | Results |
| Biswas al., 2022 [26]
|
Cross-sectional study
|
n=51 terminal cancer patients | Bangladesh | Assessing the quality of life of patients with cancer illnesses receiving palliative home care. Identify the factors that influence physical well-being and symptom control. | Palliative home care proved effective in promoting social and emotional well-being for the majority of patients included in the study. However, it showed limited effectiveness in controlling symptoms. |
| Constantinou et al., 2022 [27]
|
Cross-sectional study
|
n=80 patients with cancer | Republic of Cyprus | Conducting an analysis of the quality and effectiveness of palliative care delivered at home, while assessing the level of patient satisfaction. | Participants rated the overall quality of palliative home care positively, highlighting a satisfactory level of psychological support. |
| Patel et al., 2023 [28] | Mixed method study | n=68 patients with terminal cancer | India | Examining how patients with terminal cancer perceive the quality of palliative care in different contexts and measuring quality of life.Inizio modulo | - Positive impact on the QoL of the terminal patient both at home and in the Hospice.
The need to expand access to palliative care, increasing its coverage. |
| Riolfi al., 2021 [29]
|
Retrospective cohort study |
n=375 cancer patients | Italy | Examining the effectiveness of palliative home care in reducing costs by minimising admissions to acute care facilities. | Palliative home care reduces hospital admissions and hospital days in the last two months of life, while increasing the probability of death at home, ensuring the patient's well-being at the end of life. |
| Shepperd et al., 2021 [30]
|
Systematic review
|
n=1128 patients in the terminal stage | United Kingdom | Examining the effectiveness of palliative home care in reducing the likelihood of death in the hospital setting, in mitigating patient symptoms, in reducing health system costs, as an alternative to hospital and hospice care | Palliative home care increases the likelihood of death at home for the patient. Uncertainty persists regarding symptom control and the impact on health system costs. |
| Kim et al., 2022 [31]
|
Cost-effectiveness analysis study
|
Hypothetical cohort of terminal cancer patients who have benefited from palliative home care. | Korea | To investigate the economic advantage of palliative home care compared to hospital care. | Palliative home care can result in a doubling of expenses compared to hospital care. However, the cost-benefit outcome is uncertain. |
Table 3. Summary of the selected studies
Clinical effectiveness
Two studies included in the review show a positive effectiveness of palliative home care in alleviating patients' symptoms [28,29], while others do not find the same result [26,30]. The study by Riolfi et al. [26] showed that patient care by palliative home care services improves the control of psycho-physical symptoms that occur towards the end of life. Similarly, Patel et al. [28] highlighted effective symptom management by the home care team. In contrast, the research by Biswas et al. [26] found below-average physical well-being in 60.8% of the patients included in the survey, who complained of feeling sick (54.9%), lack of energy (43.1%), and pain (47.1%). The study calls for more research aimed at improving interventions for symptoms. Finally, the study conducted by Shepperd et al. [30] shows uncertain outcomes on symptom control.
Emotional effectiveness
Three studies [26-28] have highlighted the positive impact of palliative home care on the well-being and quality of life of patients with cancer. In the study by Biswas et al. [26], 92.1% of patients who received palliative home care demonstrated above-average emotional and social well-being. However, the greater well-being seems to be related to the duration of the care provided (> months) and to a less ominous prognosis. The investigations by Constantinou et al. [27] and Patel et al. [28] also reveal that palliative home care guarantees greater psychological support.
Cost effectiveness
The impact of palliative home care on health system costs has been the subject of conflicting considerations among the various studies included in the review. The study conducted by Riolfi et al. [29] indicates potential savings thanks to palliative home care that reduces costs related to hospitalisation, access to the emergency room and days in hospital. In contrast, the systematic review conducted by Shepperd et al. [30] highlighted a certain degree of uncertainty regarding the effect of home services on health system costs. The study conducted by Kim et al. [31] also revealed ambiguous and inconclusive results.
DISCUSSION
This review provided an analysis of the clinical, emotional and economic effectiveness of home palliative care for terminal cancer patients. A positive and significant effect of such treatments on patients' psychological well-being was found, in line with studies conducted by Biswas et al. [26], Constantinou et al. [27] and Patel et al. [28]. Home care has been shown to offer essential psychological support, enabling patients to feel understood and listened to about their needs and alleviating the emotional burden of illness. The choice to die at home promotes the emotional well-being of terminal patients, maintaining normality and social integration until the end of life [29-31]. Family support offers spiritual and emotional comfort, reducing anxiety and discomfort. Indeed, none of the research conducted showed that patients prefer to die in a hospital environment rather than in their home environment. However, only a fraction of the estimated total of patients who require it manage to benefit from it. A 2019 study, based on data collected through the palliative home care monitoring portal, showed that in 2013, 38,384 cancer patients were assisted by home care units [32], while many others could not benefit from such services. The Italian reality, therefore, does not guarantee uniform coverage throughout the country; suffice it to say that, at present, only 59% of the local health authorities have an active palliative care network, highlighting the urgent need to expand access [29,33]. The lack of studies conducted specifically in Italy is also a significant limitation in understanding the clinical, emotional and economic effectiveness of home palliative care in the terminal cancer patient. In fact, only one study [29] considered this scenario, whereas the other surveys included in the review refer to different countries. It is well known that differences in health care systems, available resources and modes of care between countries can greatly influence the results of studies and complicate the extension of results in a different context.
One study suggests potential cost savings through home-based services [29], while others, such as the research by Shepperd et al. [30] and Kim et al. [31], point to uncertainties or a lack of significant differences in costs compared to hospital care. It is not yet clear whether home care is more beneficial in terms of results and costs for terminal cancer patients. This highlights the need for further research on the economic impact of palliative home care. Although the cost-effectiveness analysis is not conclusive, the lack of negative impacts on other results could justify the implementation of home services to meet the needs of patients.
Similarly, with regard to symptom control, a diversity in results has emerged that highlights the importance of adopting personalised approaches to manage them effectively.
Palliative home care brings emotional benefits, but uncertainties remain regarding its effectiveness in controlling symptoms and its economic impact compared to hospital care. It is essential to consider patient diversity when designing personalised strategies. Further detailed research is needed to examine these aspects. Despite this, the implementation of home care programmes for end of life seems promising, but it is essential to improve and expand services to respond to the growing demand and ensure adequate support for patients in their home environment.
In this context, the nurse assumes a vital role in offering complete and patient-centred care, designing a personalised care plan. Through specialised training and constant professional updating, the nurse is able to guarantee high-quality palliative care, working in close collaboration with the other professionals in the palliative care team. This multidisciplinary approach ensures that the physical, emotional and spiritual needs of the patient are adequately met [34]. Using their skills, the nurse educates the patient on the management of typical symptoms that can occur during the terminal phase of cancer, such as pain, nausea and dyspnoea, teaching the patient strategies that can be effective.
Nursing not only allows the patient to autonomously manage symptoms, but also helps to provide a feeling of security and tranquillity regarding their situation [35].
At the same time, the nurse is actively engaged in the education of family members, so that they can acquire the skills and competences necessary to offer the appropriate support to the patient [36,37]. In addition, the nurse provides information on the resources available in the community, such as support groups, to expand the usable support network, in order to support the patient and their family during the course of the disease. This significantly contributes to preventing the patient and their loved ones from feeling isolated during this delicate phase [38]. However, nursing care is not only limited to alleviating physical suffering; in fact, the role of the nurse at this critical moment is crucial and goes far beyond the simple monitoring of physical symptoms. They offer constant and comprehensive support to both the patient and their family members, improving quality of life until the last moment. The main objective is to face the evolution of the disease in the most comfortable, reassuring and respectful way possible, and to facilitate a smooth transition towards the end of life that allows the patient to manage their condition with dignity and peace of mind [10,28,33].
Limitations of the study
This review has some limitations, which hinder its applicability in the context of the Italian health system. First, the limited number of databases consulted may have reduced the amount of articles identified, potentially excluding relevant information. The choice of inclusion criteria, although targeted, excluded studies relating to palliative care delivered at the outpatient and hospice level, focusing exclusively on home care. This approach, while guaranteeing a precise focus, on the other hand limits the completeness of the data collected and loses useful knowledge, excluding a broader vision of palliative care.
. Some of the studies included in the review [26-28] had unrepresentative or small samples of participants, which could influence the generalisability of the results.
Implications for clinical practice
The review suggests that palliative home care may be useful for patients with terminal cancer. In particular, the review highlights the benefits that could be derived from the use of palliative home care in promoting the psychological well-being of cancer patients and enabling terminal patients to spend their last days in the comfort of their own home environment, as desired by them. In fact, in order to apply the results of the review, it is essential to implement palliative home care programmes and services that reduce the use of hospital facilities. Adequate human resources must be provided, suitably trained in palliative home care. The health personnel involved in the treatment, in fact, must have advanced skills in pain management, symptom control and coordination of health and social services. This approach not only aims to improve the quality of life of the patient through a more effective control of symptoms, but also to offer fundamental emotional and social support during the advanced stages of a disease. The continuity of home care allows to establish relationships of trust between the patient, family members and the medical team, facilitating a more personalised and human-centred management of care.
Another crucial point concerns the careful monitoring of symptoms. Implementing specific protocols for the assessment and management of symptoms allows treatment to be adapted in a timely manner to the individual needs of the patient, ensuring optimal comfort and improving quality of life even in the most delicate phases. However, it is also essential to consider the economic aspect of palliative home care, therefore, studies dealing with the continuous and accurate cost-benefit assessment are required to balance the clinical effectiveness with the economic sustainability of such interventions.
CONCLUSIONS
The objective of the study was to describe the knowledge related to the clinical, emotional and economic impact of palliative home care in cancer patients. The review conducted suggests that palliative home care is a crucial element in the care of the terminally ill cancer patient, fundamental to ensuring adequate end-of-life management.
Our review shows that home care offers essential psychological support, enabling patients to feel understood and listened to with regard to their needs and requirements. However, some discrepancies have emerged, particularly with regard to the effectiveness of PC in terms of symptom control and reduction of economic costs, therefore, it is hoped that more field studies will be carried out in order to provide a broader and more detailed picture of the effectiveness of palliative care in these areas.
FUNDING STATEMENT
This research received no external funding.
CONFLICT OF INTEREST
The authors report no conflict of interest.
AUTHORS' CONTRIBUTION
All authors contributed equally.
REFERENCES
- World Health Organization (WHO). Cancer 2022. Available at: https://www.who.int/news-room/fact-sheets/detail/cancer. Last access: 29 February, 2024.
- The Italian Ministry of Health. Piano Oncologico Nazionale: documento di pianificazione e indirizzo per la prevenzione e il contrasto del cancro 2023-2027 ("National Cancer Plan: planning and guidance document for cancer prevention and control 2023-2027"), p. 7-8. Available at: https://www.salute.gov.it/imgs/C_17_pubblicazioni_3291_allegato.pdf. Last access: 29 February, 2024.
- Bray F, Laversanne M, Sung H, Ferlay J, Siegel RL, Soerjomataram I, Jemal A. Global cancer statistics 2022: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2024 May–Jun;74(3):229-263. DOI: 10.3322/caac.21834.
- Radbruch L, De Lima L, Knaul F, Wenk R, Ali Z, Bhatnaghar S, Blanchard C, Bruera E, Buitrago R, Burla C, Callaway M, Munyoro EC, Centeno C, Cleary J, Connor S, Davaasuren O, Downing J, Foley K, Goh C, Gomez-Garcia W, Harding R, Khan QT, Larkin P, Leng M, Luyirika E, Marston J, Moine S, Osman H, Pettus K, Puchalski C, Rajagopal MR, Spence D, Spruijt O, Venkateswaran C, Wee B, Woodruff R, Yong J, Pastrana T. Redefining Palliative Care-A New Consensus-Based Definition. J Pain Symptom Manage. 2020 Oct;60(4):754-764. DOI: 10.1016/j.jpainsymman.2020.04.027.
- Heydari H, Hojjat-Assari S, Almasian M, Pirjani P. Exploring health care providers' perceptions about home-based palliative care in terminally ill cancer patients. BMC Palliative Care. 2019;18(1):66. DOI: 0.1186/s12904-019-0452-3
- Temel, J.S., et al. "Early palliative care for patients with metastatic non-small-cell lung cancer." New England Journal of Medicine, vol. 363, no. 8, 2010, pp. 733-742. DOI: 10.1056/NEJMoa1000678.
- Ferrell, B. R., et al. "Palliative care in chronic illness and cancer: A narrative review." Annals of Internal Medicine, vol. 172, no. 5, 2020, pp. 350-356. DOI: 10.7326/M19-3085.
- Kamal, A. H., et al. "Symptom prevalence, treatment patterns, and outcomes among patients with advanced cancer: A National Health and Nutrition Examination Survey analysis." JAMA Oncology, vol. 3, no. 5, 2017, pp. 672-678. DOI: 10.1001/jamaoncol.2016.6746.
- World Health Organization (WHO). Palliative care 2020. Available at: https://www.who.int/news-room/fact-sheets/detail/palliative-care. Last access: 14 February, 2024.
- Worldwide Hospice Palliative Care Alliance (WHPCA) and World Health Organization (WHO). Global Atlas of Palliative Care 2nd Edition. London, 2020. Available at: https://cdn.who.int/media/docs/default-source/integrated-health-services-(ihs)/csy/palliative-care/whpca_global_atlas_p5_digital_final.pdf?sfvrsn=1b54423a_3. Last access: 14 February, 2024.
- The Italian Society of Palliative Care (SICP). Palliative care & IFeC. 2023. Available at: https://www.sicp.it/wp-content/uploads/2023/01/FNOPI-SICP_CP-e-IFEc_V2-Apr23.pdf. Last access: 4 March, 2024.
- The Italian Ministry of Health. Cure palliative in ospedale: un diritto di tutti 2021. ("Palliative care in the hospital: a right for everyone 2021")Available at: https://www.salute.gov.it/imgs/C_17_opuscoliPoster_518_allegato.pdf. Last access: 29 February, 2024.
- Qanungo S, Cartmell KB, Mueller M, Butcher M, Sarkar S, Carlson TG, et al. Comparison of home-based palliative care delivered by community health workers versus usual care: research protocol for a pilot randomized controlled trial. BMC Palliative Care. 2023;22(1). DOI: 10.1186/s12904-023-01235-z
- Maetens A, Beernaert K, De Schreye R, Faes K, Annemans L, Pardon K, et al. Impact of palliative home care support on the quality and costs of care at the end of life: a population-level matched cohort study. BMJ Open. 2019;9(1):e025180. DOI: 1136/bmjopen-2018-025180
- Sepúlveda C, Marlin A, Yoshida T, Ullrich A. Palliative Care: the World Health Organization's global perspective. J Pain Symptom Manage. 2002;24(2):91-6. DOI: 10.1016/s0885-3924(02)00440-2.
- Dhiliwal SR, Ghoshal A, Dighe MP, Damani A, Deodhar J, Chandorkar S, et al. Development of a model of Home-based Cancer Palliative Care Services in Mumbai - Analysis of Real-world Research Data over 5 Years. Indian J Palliative Care. 2022;28(4):360-390. DOI: 25259/IJPC_28_2021
- Gomes B, Calanzani N, Curiale V, McCrone P, Higginson IJ. Effectiveness and cost-effectiveness of palliative home care services for adults with advanced illness and their caregivers. Cochrane Database Syst Rev. 2013;2013(6) DOI: 1590/1516-3180.20161341T2
- Van Klinken M. Palliative and End-of-Life Care: Challenges for Patients and Nurses. Semin Oncol Nurs. 2023;39(6):151527. DOI: 1016/j.soncn.2023.151527
- Danielsen BV, Sand AM, Rosland JH, Førland O. Experiences and challenges of home care nurses and general practitioners in home-based palliative care - a qualitative study. BMC Palliative Care. 2018;17(1):95. DOI: 1186/s12904-018-0350-0
- Brumley R, Enguidanos S, Jamison P, Seitz R, Morgenstern N, Saito S, et al. Increased satisfaction with care and lower costs: results of a randomized trial of in-home palliative care. J Am Geriatr Soc. 2007;55(7):993-1000. DOI: 1111/j.1532-5415.2007.01234.x
- Gonzalez-Jaramillo V, Fuhrer V, Gonzalez-Jaramillo N, Kopp-Heim D, Eychmüller S, Maessen M. Impact of home-based palliative care on health care costs and hospital use: A systematic review. Palliative and Supportive Care. 2021;19(4):474-487. DOI: 1017/S1478951520001315
- Brumley RD, Enguidanos S, Cherin DA. Effectiveness of a home-based palliative care program for end-of-life. J Palliat Med. 2003;6(5):715-24. DOI: 1089/109662103322515220
- Tricco AC, Lillie E, Zarin W, O'Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Checklist and Explanation. Ann Intern Med. 2018;169(7):467-473. DOI: 7326/M18-0850
- Green BN, Johnson CD, Adams A. Writing narrative literature reviews for peer-reviewed journals: secrets of the trade. J Chiropr Med. 2006;5(3):101-17. DOI: 1016/S0899-3467(07)60142-6
- Dixon-Woods M, Cavers D, Agarwal S, Annandale E, Arthur A, Harvey J, et al. Conducting a critical interpretive synthesis of the literature on access to healthcare by vulnerable groups. BMC Med Res Methodol. 2006;6(1). DOI: 1186/1471-2288-6-35
- Biswas J, Faruque M, Banik PC, Ahmad N, Mashreky SR. Quality of life of the cancer patients receiving home-based palliative care in Dhaka city of Bangladesh. PLoS One. 2022;17(7). DOI: 1371/journal.pone.0268578
- Constantinou A, Polychronis G, Argyriadi A, Argyriadis A. Evaluation of the quality of palliative home care for cancer patients in Cyprus: a cross-sectional study. British Journal of Community Nursing. 2022;27(9):454-62. DOI: 12968/bjcn.2022.27.9.454
- Patel D, Patel P, Ramani M, Makadia K. Exploring Perception of Terminally Ill Cancer Patients about the Quality of Life in Hospice based and Home-based Palliative Care: A Mixed Method Study. Indian J Palliative Care. 2023;29(1):57-63. DOI: 25259/IJPC_92_2021
- Riolfi M, Mogliani E, Salvetti I, Poles G, Trivellato E, Manno P. Efficacy and criticality in palliative home care for cancer patients: retrospective cohort study. Recent Prog Med 2021;112(10):647-652. DOI: 10.1701/3679.36655
- Shepperd S, Gonçalves-Bradley DC, Straus SE, Wee B. Hospital at home: home-based end-of-life care. Cochrane Database Syst Rev. 2021;3(3). DOI: 10.1002/14651858.CD009231
- Kim YS, Han E, Lee JW, Kang HT. Cost-Effectiveness Analysis of HomeBased Hospice-Palliative Care for Terminal Cancer Patients. J Hosp Palliative Care. 2022;25(2):76-84. DOI: 14475/jhpc.2022.25.2.76
- Scaccabarozzi G, Lovaglio PG, Limonta F, Peruselli C, Bellentani M, Crippa M. Monitoring the Italian Home Palliative Care Services. Healthcare (Basel). 2019 Jan 2;7(1):4. DOI: 3390/healthcare7010004
- The Italian Society of Palliative Care (SICP). Le cure palliative in Italia: stima del bisogno, rete di offerta, tasso di copertura del bisogno, confronto internazionale. ("Palliative care in Italy: estimation of need, supply network, need coverage rate, international comparison.") 2020. Available at: https://www.sicp.it/wp-content/uploads/2020/12/Cure-palliative-in-talia_Bocconi_211119.pdf. Last access: 31 May, 2024.
- Law no. 38 of 15 March 2010, art. 1 – "Disposizioni per garantire l'accesso alle cure palliative e alla terapia del dolore" ("Provisions to guarantee access to palliative care and pain therapy") (OJ no. 65 of 19/03/2010). Available at: https://www.gazzettaufficiale.it. Last access: 10 February, 2024.
- Marchetti A, Piredda M, Facchinetti G, Virgolesi M, Garrino L, Dimonte V, De Marinis MG. Nurses' Experience of Body Nursing Care: A Qualitative Study. Holist Nurs Pract. 2019 Mar/Apr;33(2):80-89. DOI: 10.1097/HNP.0000000000000314.
- World Health Organization (WHO). Therapeutic patient education: an introductory guide. 2023. Available at: https://iris.who.int/bitstream/handle/10665/372743/9789289060219-eng.pdf?sequence=12. Last access: 6 March, 2024.
- Collins CM, Small SP. The nurse practitioner role is ideally suited for palliative care practice: A qualitative descriptive study. Can Oncol Nurs J. 2019; 29(1):4-9. DOI: 5737/2368807629149
- Hassankhani H, Dehghannezhad J, Rahmani A, Ghafourifard M, Soheili A, Lotfi M. Caring Needs of Cancer Patients from the Perspective of Home Care Nurses: A Qualitative Study. Asian Pac J Cancer Prev. 2022; 23(1):71-77. DOI: 31557/APJCP.2022.23.1.71
![]()
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Transformational Leadership: the key to reducing Intention to Leave In nurses
Gianluca Azzellino 1*, Massimo Bordoni2
1 Department of Territorial Assistance, Local Health Authority (AUSL 04) of Teramo, Italy
2 Department of Social Health. Local Health Authority (AUSL 04) of Teramo, Italy
Corresponding author: Gianluca Azzellino, Department of Social Health. Local Health Authority (AUSL 04) of Teramo, Via Finlandia n. 7/1,65015 Montesilvano, Italy
Email: gianluca.azzellino@aslteramo.it
Cite this article
ABSTRACT
This commentary responds to the recently published article on transformational leadership in the healthcare context. The article explores how transformational leadership can significantly improve efficiency and job satisfaction in nursing teams. Specifically, it highlights the crucial role of this leadership style in fostering a positive work environment and reducing intentions to leave the profession among nurses. At a time of profound crisis for the nursing profession, characterised by staff shortages, increased workload and high rates of abandonment of the profession, transformational leadership could represent an effective model to address these challenges. This leadership approach, based on vision, inspiration, and involvement, can strengthen nurses' motivation and satisfaction by promoting a positive and stimulating working environment. The analysis emphasises the importance of adopting innovative management practices to address current challenges in the healthcare sector, providing a basis for further research and practical implementation.
Keywords: Nursing leadership, Burnout, intention to leave, professional development, nurse education, job satisfaction
INTRODUCTION
The authors read with interest the article by Rizzo et al. (2024) entitled “Transformative leadership and job satisfaction in the nursing profession: A narrative review”. The article offers an in-depth analysis of the effect of transformative leadership on the nursing profession. The authors explore how this leadership style not only positively influences nurses’ job satisfaction, but also their intention to leave the profession. This is particularly relevant in a global context in which the nursing shortage is a critical challenge for healthcare systems. However, the increasing complexity of the healthcare system, coupled with the new challenges posed by the global pandemic, has made the need for an evolution in the nursing leadership model evident. This commentary aims to further explore the findings of Rizzo et al. by contextualizing their study within the current issues facing the nursing profession and discussing the importance of implementing transformative leadership strategies to improve both the quality of healthcare and the intention to stay. Our analysis through a combination of direct experience in the field and critical review of relevant literature, proposes to offer an in-depth perspective on how transformational leadership can be implemented effectively to address current challenges in nursing.
DISCUSSION
It was interesting to read the research work by Rizzo et al. (2024) on the relationship between transformational leadership and job satisfaction. At a time when the healthcare sector is facing unprecedented challenges, stability and satisfaction of nurses have become crucial priorities. Transformational nurse leaders can recognise and anticipate the needs of their nursing staff by establishing a good rapport and making significant efforts to meet their needs to encourage a sense of empowerment and autonomy that can subsequently translate into job satisfaction [1]. Recent studies have shown that nurses working under the guidance of transformational leaders tend to show greater attachment to their role and to the organisation. This results in fewer people leaving the profession, thus reducing turnover and the costs associated with training and induction of new staff. Transformational leadership, defined by Bass as a leadership style that inspires and motivates employees through shared vision, effective communication, individualised attention, and intellectual stimulation, stands out as a leadership model capable of fostering a positive and motivating work environment [2]. A leadership style that promotes autonomy, support and empowerment of nurses can improve job satisfaction, organisational commitment, and nurses' intention to remain in their position by reducing emotional exhaustion [3]. As Rizzo et al. points out, there is therefore a need to identify and fill current gaps in nursing leader competencies and skills through processes of two-way communication and mutual trust between managers and nurses. Cummings et al. conducted a systematic review that showed that transformational leadership behaviour is positively correlated with job satisfaction [4]. Strengthening the sense of belonging and personal fulfilment can reduce burnout and the intention to leave the profession. In an environment where nurses feel valued and supported, they are more likely to remain committed and motivated in their work. Overall, studies support the fact that having positive support factors and working relationships in place, including positive relationships with physicians, leader support, positive leadership style and teamwork, can play a protective role against Burnout [5]. Another positive aspect of this style is its ability to motivate professionals to overcome daily challenges and actively engage in their work. Leaders who display transformational behaviour can inspire staff to see their work as a meaningful mission, rather than just an occupation. Kanste highlighted how transformational leaders are able to foster a sense of purpose among nurses, encouraging them to contribute beyond basic expectations [6]. This increased motivation can result in a reduction in the intention to leave the profession. A cohesive environment can improve the quality of care and increase job satisfaction. Boamah et al. showed how transformational leadership fosters the creation of cohesive and collaborative teams, thus improving outcomes for both patients and nurses. This team cohesion can reduce feelings of isolation and increase the sense of support among staff [7]. Professional development programmes that focus on transformational leadership skills can prepare nurse leaders to lead their teams effectively. It is therefore crucial to invest in the training of leaders capable of adopting this leadership style in order to build motivated and resilient teams. Despite the fact that a transformational leadership style is correlated with better job satisfaction, existing evidence shows that it is rarely used by nursing leaders in healthcare settings [8]. Furthermore, fostering a culture of continuous feedback and professional growth can help leaders develop and maintain transformational behaviours. Secondly, it is crucial to promote policies that foster work-life balance, the creation of open and transparent communication channels, and the recognition and valuing of nurses' contributions. The choice of the best leadership style could be one of the modifiable factors that a healthcare organisation can adopt to create a favourable working environment and promote quality care [9]. Rizzo et al. correctly identified the increasing pressures on nurses and the need for innovative strategies to address the problem. However, we believe that an emphasis on transformational leadership can offer a sustainable solution and practice. The scientific community and policy makers need to seriously consider adopting this leadership model as part of strategies to address the professional crisis. Transformational leadership offers a promising perspective to improve job satisfaction, reduce burnout and intent to leave, and thus contribute to building a more attractive and sustainable healthcare system.
Conflict of interest
The authors declare no competing interests
Financing
No funding to declare
Author contributions
All authors contributed equally to the work
REFERENCES
- Asif M, Jameel A, Hussain A, Hwang J, Sahito N. Linking Transformational Leadership with Nurse-Assessed Adverse Patient Outcomes, and the Quality of Care: Assessing the Role of Job Satisfaction and Structural Empowerment. Int J Environ Res Public Health. 2019 Jul 4;16(13):2381. doi: 10.3390/ijerph16132381. PMID: 31277478; PMCID: PMC6651060.
- Jr, Morgan. (2006). Leadership and performance beyond expectations, by Bernard M. Bass. New York: The Free Press, 1985, 191 pp. $26.50. Human Resource Management. 25. 481 - 484. 10.1002/hrm.3930250310.
- Laschinger HK, Wong CA, Cummings GG, Grau AL. Resonant leadership and workplace empowerment: the value of positive organizational cultures in reducing workplace incivility. Nurs Econ. 2014 Jan-Feb;32(1):5- 15, 44; quiz 16. PMID: 24689153.
- Cummings GG, Tate K, Lee S, Wong CA, Paananen T, Micaroni SPM, Chatterjee GE. Leadership styles and outcome patterns for the nursing workforce and work environment: A systematic review. Int J Nurs Stud. 2018 Sep;85:19-60. doi: 10.1016/j.ijnurstu.2018.04.016. Epub 2018 May 3. PMID: 29807190.
- Dall’Ora C, Ball J, Reinius M, Griffiths P. Burnout in nursing: a theoretical review. Hum Resour Health. 2020 Jun 5;18(1):41. doi: 10.1186/s12960-020-00469-9. PMID: 32503559; PMCID: PMC7273381.
- Kanste, Outi. (2008). The Association between Leadership Behaviour and Burnout among Nursing Personnel in Health Care. Nordic Journal of Nursing Research. 28. 4-8. 10.1177/010740830802800302.
- Boamah SA, Spence Laschinger HK, Wong C, Clarke S. Effect of transformational leadership on job satisfaction and patient safety outcomes. Nurs Outlook. 2018 Mar-Apr;66(2):180-189. doi: 10.1016/j.outlook.2017.10.004. Epub 2017 Nov 23. PMID: 29174629.
- Morsiani G, Bagnasco A, Sasso L. How staff nurses perceive the impact of nurse managers' leadership style in terms of job satisfaction: a mixed method study. J Nurs Manag. 2017 Mar;25(2):119-128. doi: 10.1111/jonm.12448. Epub 2016 Dec 5. PMID: 27917561.
- Phillips LA, de Los Santos N, Jackson J. Licensed practical nurses' perceptions of their work environments and their intentions to stay: A cross-sectional study of four practice settings. Nurs Open. 2021 Nov;8(6):3299-3305. doi: 10.1002/nop2.1046. Epub 2021 Aug 25. PMID: 34432374; PMCID: PMC8510757.
![]() This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Monitoring of toxicities induced by Chimeric Antigen Receptor T-cell therapy: Protocol for a phenomenological study on the experiences of nurses
Valentina Simonetti 1†, Letizia Governatori 2†, Francesco Galli 3, Cesare Tozzi 4, Romano Natalini 4, Andrea Toccaceli 5, Francesco Pastore 6, Giancarlo Cicolini 1 & Dania Comparcini 7*
- Department of Innovative Technologies in Medicine and Dentistry, “G. d 'Annunzio” University of Chieti-Pescara, Chieti, Italy; v.simonetti@unich.it; https://orcid.org/0000-0002-7185-4850 (VS); g.cicolini@unich.it; https://orcid.org/0000-0002-2736-1792 (GC).
- Department of General and Specialist Surgery, Adult and Pediatric Orthopaedics Clinic, University Hospital "Azienda Ospedaliero Universitaria Delle Marche", Ancona, Italy; letizia.governatori@ospedaliriuniti.marche.it (LG).
- Faculty of Medicine and Surgery, Polytechnic University of Marche, Ancona, Italy; galli.francesco77@gmail.com; https://orcid.org/0009-0000-3550-1268 (FG).
- Department of Internal Medicine, Haematology Clinic, PICC Unit, University Hospital "Azienda Ospedaliero Universitaria Delle Marche", Ancona, Italy; tozzicesare1973@gmail.com (CT); romano.natalini@ospedaliriuniti.marche.it. (RN).
- Nursing Department, University Hospital "Azienda Ospedaliero Universitaria Delle Marche", Ancona, Italy; andrea.toccaceli@ospedaliriuniti.marche.it (AT).
- Department of Biomedicine and Prevention, University of Rome “Tor Vergata”, Rome, Italy; francesco.pastore@uniba.it (FP).
- Interdisciplinary Department of Medicine, “Aldo Moro” University of Bari, Bari, Italy; dania.comparcini@uniba.it; https://orcid.org/0000-0003-3622-6370 (DC).
† The authors LG and VS contributed to the study in equal measure.
* Corresponding author: Dania COMPARCINI (DC), PhD, MSc, RN, research fellow. Interdisciplinary Department of Medicine, “Aldo Moro” University of Bari, Italy; email: dania.comparcini@uniba.it; https://orcid.org/0000-0003-3622-6370.
Cite this article
ABSTRACT
Introduction: Chimeric Antigen Receptor T-cell therapy (CAR-T) represents the most recent immunotherapy’s innovation to cure some refractory and/or relapsing haematological tumours.
However, because of the life-threatening toxicities it might cause such as Cytokine Release Syndrome and Immune Cell Associated Neurotoxicity Syndrome, patients are closely monitored by nurses for the early identification of toxicities during the post-infusion phase of CAR-T cell therapy. Exploring the nurses’ experience with respect to any difficulties related to the monitoring is important since these issues can be perceived by patients and affect the nurse-patient’s caring relationship, considered as a shared lived experience between the patient and the nurse.
Aim: This study aims to investigate haematology nurses’ lived experience with monitoring CAR-T’s induced toxicities.
Materials and methods: A qualitative study following Cohen's phenomenological methodology will be conducted through semi-structured interviews in a sample of Italian nurses working in haematology units, who have had previous experience in the management of patients undergoing CAR-T therapy for at least two months and who have performed the monitoring for the same months of experience; the interviews will be audio-recorded and then transcribed verbatim. Two researchers will carry out the manual analysis and interpretation of the collected data independently, identifying themes and sub-themes.
Conclusion: To explore the nurses’ experiences in this field could facilitate the identification of the educational needs, at individual and group level. Despite it is important to consider contextual variables, the findings of this study could contribute to develop evidence supporting advanced and specialized nursing care in the haematological setting.
Keywords: hematology, nursing, CAR-T therapy, phenomenological, qualitative.
INTRODUCTION
Chimeric Antigen Receptor T-cell (CAR-T) therapy is the latest immunotherapy approach for the treatment of certain resistant or relapsing haematological cancers [1], including: Acute Lymphoblastic Leukaemia, diffuse large B-cell lymphoma, primary mediastinal large B-cell lymphoma and mantle cell lymphoma. However, despite being designed to act selectively in eliciting a targeted immune response against neoplastic cells, anti-CD19 CAR-T cell therapy is not free of risks and even serious side effects. The most frequent toxicities are Cytokine Release Syndrome (CRS), reported in 57% to 93% of patients who underwent CAR-T [2], and Immune Effector Cells Associated Neurotoxicity Syndrome (ICANS), which occurs in 20% to 70 % of patients [3]. Nevertheless, while they are often manageable and reversible, they can prove fatal, requiring close patient monitoring, early recognition of toxicities, and prompt intervention to reduce morbidity and mortality [3].
To achieve this, patients are closely monitored by nurses after infusions following specific protocols and procedures adopted in the operating units. More specifically, monitoring by nurses includes the assessment of vital parameters as well as typical signs and symptoms of Cytokine Release Syndrome (CRS) and neurological toxicity (ICANS) [4]. Specifically, to facilitate the identification of early manifestations of neurotoxicity, close monitoring using validated nursing instruments [5] is necessary, including the handwriting test and the quantification of the “ICE - Immune Effector Cell-associated Encephalopathy score”. The latter enables the mental status of patients to be assessed by identifying four ICANS grades (numbered 1 to 4) according to the presence or absence of consciousness impairment, seizures, motor alterations and symptoms of high intracranial pressure [6].
Thus, monitoring enables the nurse to conduct a targeted assessment of the patient's condition in the post-infusion phase, which is decisive for a timely approach to CAR-T toxicities by activating the entire multidisciplinary team. Said approach effectively relies on the meticulous execution of the objective examination, where a high patient assessment frequency [7] enables the practitioner to perceive even the most subtle changes in the patient's psycho-physical condition.
A recent study showed that for patients undergoing CAR-T cell therapy and experiencing significant side effects, continuous monitoring by nurses provides them with a sense of security, and they particularly appreciate the time nurses devote (in addition to monitoring activity) to engaging in dialogue and expressing an interest in their state of health [8]. Therefore, it is essential to acquire deeper insights into the challenges nurses face during the complication monitoring phase, considering that patients may sense such difficulties, which may, consequently, affect the caring relationship established during this crucial assistance.
As a fundamental aspect of nursing practice, the nurse-patient relationship is part of a broader context in which nurses use their senses, knowledge, and experience to exercise professional judgment and discernment when providing care in specific situations [9]. As such, a thorough examination of patients' care experience and the related outcomes must also be conducted with due consideration for the experiences narrated by the haematology nursing staff, since the practice of nursing care necessarily implies a shared experience of the relevant dynamics [10,11].
However, the topic of nursing care in the management of patients undergoing CAR-T cell therapy is a relatively new area of investigation, so few studies have been conducted in the field of nursing. The limited literature has only investigated the experience of patients undergoing CAR-T therapy and/or their caregivers without delving into the experience itself and the meaning attributed to this experience by those who care for patients and/or interact with and support caregivers [12-14]. Moreover, only one study, conducted in China, investigated the experience of a group of oncology nurses in managing this specific subpopulation of patients but was focused on nursing competence [15]. This study did not examine the nurse's key role during the toxicity monitoring phase in-depth, and the main focus was on aspects related to nursing skills rather than the significance of the experience.
To date, to the best of our knowledge, no study has explored nurses' experiences in the monitoring and care of this specific category of haematological patients, even though the aforementioned scientific literature frequently emphasises the importance of nursing care at all stages of the clinical care process and particularly during the post-infusion phase.
Study aim
The purpose of this study is to explore the experience of nurses caring for haematology patients during the monitoring of the main toxicities associated with CAR-T therapy.
MATERIALS AND METHODS
Study design
A hermeneutical phenomenological study will be conducted according to Cohen’s method [16]. A summary of the planned operating times for the study is shown in Table 1.
| Study phases | Activities | Estimated duration (time) | Follow-up |
| Definition and planning | Review and analysis of the literature, research question | 1 month (September) | Focus: researchers; stakeholders. |
| Development of the research design, context analysis, selection of potential data acquisition centres | 2 months (October–November) | ||
| Drawing up of draft protocol | 2 months (December–January) | ||
| Review and finalisation of the protocol. | 2 months (February–March) | ||
| Authorisations by the participating centres.
Request for an opinion form the Ethics Committee (EC) |
2 months and 15 days (April–June) | ||
| “Bracketing” process and exchanges between researchers | 15 days (June) | ||
| 2. Recruitment of participants | Recruitment of data acquisition centre and participants | 15 days (July) | Focus: participants |
| Finalisation of the sampling plan | |||
| Informed consent | |||
| Data collection | Pre-test data collection tool (pilot interviews) and finalisation of interview questions | 15 days (July) | |
| Conduct of interviews and return of transcripts | 1 month (August–September) | ||
| Data analysis | Data preparation: transcription, reading of interviews (units of meaning)# | 1 month (September–October) | Focus: texts (transcribed interviews) |
| Data codification and reduction process | |||
| Thematic analysis | |||
| Writing and editing | |||
| Discussion and sharing of emerging themes (provisional) | 15 days (October) | Focus: researchers, participants | |
| Final report | Drafting of the final report, manuscript. | 1 month (November) | Focus: scientific community, stakeholders |
Table 1. Envisaged timeline for the study (2023–2024).
The phenomenological approach is based on the understanding of questions of meaning and the actual experiences of informants [16] by combining the methodological properties of descriptive (Husserlian) and interpretative (Gadmerian) phenomenology. The former descriptive scope aims to describe the experiences of individual members of the cohort under study after a preliminary phase in which the researchers set aside prejudices and preconceptions about the phenomenon under investigation (“bracketing”). This is crucial to reduce the influence of such prejudices and preconceptions on the subsequent phase, in which the themes and data emerging from the interviews are respectively extrapolated and analysed. The interpretative intent, on the other hand, examines and interprets the reported experiences in depth [17]. Therefore, since this methodological approach focuses on understanding questions of meaning and the real-life experiences of the respondents [16], it is particularly suited to nursing-related research and topics seldom explored in the literature. It is also instrumental in the broader context of a working organisation for identifying perceived needs and the solutions that can best address them [16].
Participants and study context
The participating cohort will be recruited from haematology operating units in Italy, identified at the national level among the accredited haematology and onco-haematology centres of advanced specialisation for the treatment of leukaemias and lymphomas, compliant with specific requirements and authorisations for cell therapies as prescribed by AIFA, the Italian Medicines Agency.
Intentional (“propositional”) sampling will be carried out within each data collection centre according to a homogeneity criterion [18,19] to investigate differences and variations within a relatively homogeneous sample [18, 20] in relation to experience in handling the monitoring cards of patients subject to complications associated with CAR-T therapy. This sampling will enable the researchers to deliberately select a cohort of nurses who possess specific expertise and experience in the management of complication monitoring based on a set of pre-established criteria (inclusion and exclusion criteria); this is of fundamental importance in order to obtain a sample capable of providing meaningful, subject-specific information as well as credible and reliable explanations of the phenomenon under study, irrespective of the cohort size [21].
Sampling will continue until data saturation is reached, understood as a process of conducting interviews sequentially until the concepts expressed by the respondents are repeated several times without introducing new concepts or themes [22]. The unitary element of analysis will coincide with the experience under study; therefore, considering that a single respondent can generate many concepts, large samples in numerical terms are not necessarily useful for generating a comprehensive dataset with respect to the purpose of the study and the phenomenon of interest [23]. Indeed, in a qualitative dataset, most new information is generated early in the process and generally follows an asymptotic curve whereby new information declines after a small number of interviews or data analyses [24]. In particular, with regard to studies marked by a high level of population homogeneity, the literature indicates that a sample of six interviews is sufficient to foster the development of meaningful themes and useful interpretations related to the phenomenon under study [25]. Therefore, in accordance with the above and considering that the scope of phenomenology is to explore the common features of real-life experiences gleaned from data provided by only a few individuals who have experienced a particular phenomenon as subjects capable of providing detailed and in-depth information [23], in accordance with claims stated in the literature regarding sample sizes for phenomenological studies, which generally vary from 5 to 25 respondents [26], a sample cohort of 6 to 12 nurses is deemed acceptable for this study.
Inclusion and exclusion criteria
Subject to voluntarily agreeing to participate in the study by signing the informed consent, the study will include all nurses who provide direct patient care at the data collection centres and who have passed the probationary period within the organisation for the inclusion of newly recruited or newly assigned nurses in the operating unit. The selected nurses will have had appreciable experience (for a minimum of two months) in managing patients undergoing CAR-T therapy and must be practised in the use of assessment tools (at least on one occasion) during the same months of experience.
Nurses who provide day hospital care at the operating unit and those in exclusively organisational roles will be excluded from the study.
Data collection tools and study procedures
Interview
For data collection, we developed a draft semi-structured interview outline with open-ended questions that will allow participants to express themselves freely [16]. The interview outline was drawn up considering previous similar studies carried out in the haematology field [12-15] and following discussion within the research group and discussion with expert haematology clinicians working in an accredited Italian haematology and oncohaematology centre with high specialisation in the treatment of leukaemias and lymphomas, meeting specific requirements and authorisations for cell therapies.
The envisaged main questions are as follows: “Please could you tell us about your experience with monitoring CAR-T therapy-induced toxicities for patients in the Haematology Unit?; “How would you describe your experience using CRS and neurological toxicity monitoring tools such as the ICE score and the handwriting test?”; “Regarding your experience, what were the positive and negative aspects? Can you please provide some examples?”. If further investigation of the emerging themes is required, the researcher will add specific questions to the interview to clarify the contents expressed. Finally, the interview will conclude by asking participants if they need to add anything else or report anything specific to what has already been said. This will be solicited by the following question: “Do you have any further comments or suggestions?”; in the event of a negative response, the interview will be considered completed.
In addition, demographic data will be collected from participants relating to age, gender, level of education, marital status, years of work as a nurse, years of work as a nurse in the current haematology unit, previous clinical experience (work areas/clinical specialities in which you have served as a nurse).
Once the necessary ethical authorisations for study commencement have been obtained, a limited number of pilot interviews (at least two) will be conducted to test the draft interview outline and possibly fine-tune it before proceeding with the study.
Data collection
In keeping with the method proposed by Cohen and co-authors [16], before conducting the interviews, all researchers will undertake a process aimed at suspending, i.e. bracketing their personal expectation bias, assumptions, and preconceptions, if any, regarding the phenomenon being studied. According to the proposed method, this approach is crucial as it reduces the likelihood of the researcher's judgements influencing the extrapolation of themes from the interviews [16].
Each interview will be conducted face-to-face, individually, by a researcher with professional experience in the field of haematology, but who is not part of the team working in the data collection centre. In addition, interviews will be conducted by prior agreement with the individual participant in a location that ensures participants feel comfortable, facilitating spontaneous and natural responses [16].
Subject to written informed consent, each interview will be recorded using protected digital tools that are not accessible except to researchers so that they can subsequently be transcribed verbatim for data analysis purposes. Subsequently, the transcripts will be returned to the interviewees for comments or clarification. Considering the impossibility of establishing a predetermined interview duration, given the purpose of the study and the complexity of the phenomenon to be examined, a time of between 40 and 70 minutes is envisaged for each interview.
Data analysis
Two researchers will independently analyse the data extracted from the interviews using a manual approach [27,28]. In accordance with the method of Cohen and co-authors [16], the data analysis will comprise the following principal phases: (I) The Data Preparation Phase, in which the interviews, previously recorded, will be transcribed verbatim and transferred to digital media; in this phase, the units of analysis (words, phrases or themes) will be selected, and a repeated and in-depth reading of the transcripts will be carried out, through the process of immersion in the data [29] to become familiar with the transcripts and highlight the essential features within each interview [30,31] while simultaneously carrying out an initial interpretation of the contents that will guide the codification of the data in the subsequent analysis phases [16]. (II) the Data Codification and Reduction Process: in this phase, the researchers will reorganise the contents of the interviews, grouping content pertaining to the same subject, eliminating any digressions that stray from the phenomenon under study and simplifying the respondents' spoken language without actually modifying the content expressed; a “line by line” analysis of what the participants reported will be carried out to provide “a label of meaning” to each part of the text [16], starting the reduction process while maintaining the overall essence of the contents expressed [16]. (III) Thematic Analysis: the purpose of the thematic analysis is to systematically describe and interpret the meaning of the qualitative data generated by the interviews, generating themes that will be finally analysed and presented [32]. At this stage, once an overall interpretation of the contents has been obtained, sentences in the text will be underlined by writing “headings” in the margin of the text that will represent the provisional names and/or themes assigned to the most salient content aspects [16,33-36]. To this end, colours may be used, or specific text segments may be highlighted to indicate potential interpretative patterns instrumental to identifying data segments; similarly labelled interview passages will then be grouped and appropriately reorganised [16]. In this way, as the main headings are identified, the extracted data will be collected and grouped manually within each codification, generating an initially unrestricted list of categories [36]. (IV) The Writing and Editing Process [35]: a reflexive writing and rewriting process will initially identify themes that will be followed by an in-depth examination and comparative analysis of the same within a broader framework to validate the overall meaning derived from the contents of the interviews [16]. The lists of categories will then be grouped into higher-order headings of broader scope capable of describing and augmenting the understanding of the phenomenon, thereby generating new knowledge [36]. The category reduction process will involve pooling similar or related observations and comparing data from within the same category with data from other categories [36]. Finally, the abstraction process will make it possible to formulate a general description of the phenomenon under study by formulating specific categories (general and subcategories) that will be named using words that reference their content [29]. A deep probing of the meaning of the interview content will lead to an overall understanding of the respondents’ real-life experiences as expressed within the emergent themes. This understanding will be supported by recourse to margin notes as part of the hermeneutic process underlying the transformation of the text fields into a coherent narrative [16,37]. (V) Following thematic analysis, the researchers will discuss the provisional emergent themes with the other members of the research team, including qualitative research and haematology nursing experts. Subsequently, the provisional themes will be returned to the participants to verify that the researchers had correctly interpreted their submissions, and only then will they be confirmed.
Methodological rigour
To minimise social desirability bias, the interviews will be conducted by a researcher who has no previous involvement with the study centre in a professional capacity. The researchers tasked with analysing the data will also have previous oncological work experience, albeit in different settings other than the data collection centre; this will underpin the credibility of the research process. The practice of “bracketing” will promote critical thinking among researchers to ensure methodological rigour and avoid the contamination of individual judgement during data analysis [16]. The practice of “bracketing” will promote critical thinking among researchers, ensuring methodological rigour and avoiding the contamination of individual judgement during data analysis [16]. Furthermore, to reinforce the collaborative relationship between participants and researchers and confirm the accuracy of outcomes, respondents will be asked to provide feedback on the (provisional) themes identified (member-checking of participants); they will also be offered the opportunity to add details or clarifications regarding their experience, if necessary [38].
Ethical considerations and protection of data confidentiality
The study was submitted to an independent Ethics Committee, which expressed a favourable opinion on the conduct of the study (Project identification code 1697/CEL – CARTINF Study; approval number 389|13/06/2024).
Nurses' involvement in the survey will be voluntarily, and the semi-structured interviews will be preceded by asking study participants for written consent to their participation, recording of the interviews, and processing of related data. They will also receive all information about the study's purpose, how data is collected and managed, and its confidentiality.
Anonymity will be guaranteed as prescribed by prevailing legislation on the processing of personal data and respect for privacy (Italian Laws nos. 675 & 676 of 31 December 1996, Official Journal of 08/01/1997, Article 7 of Italian Legislative Decree no. 196 of 30 June 2003 and European Privacy Regulation EU 2016/679, General Data Protection Regulation – GDPR). Relevant data will be strictly used for the purposes of the study.
Presentation of results
The results of the study will be presented in narrative form, reporting excerpts from interviews in support of the identified themes and sub-themes. Furthermore, graphic aids in the form of charts and tables will be included to enhance visualisation of the interview outcomes and related analyses (e.g. with respect to the originally codified themes) in terms of response frequencies and percentages [32]. In particular, tables may be used to express thematic outcomes quantitatively (e.g. organisation of the various themes according to the number of codes they contain), the intent being to facilitate and not replace the presentation of the interview extracts in narrative form.
DISCUSSION
To date, the real-life experiences of nurses responsible for monitoring CAR-T therapy toxicity have not been significantly studied or reported in the literature. No such research has been undertaken in Italy, while, at an international level, only a recent study conducted in China investigated the views of nurses caring for this patient category to assess the skills and knowledge required for the specific care context [15]. Yet, given the broader scope of contextual acquired knowledge, close investigation into the aspects of the nursing experience with respect to one of the salient aspects of caring for this patient segment is of paramount importance. Such aspects manifestly impact clinical practice and enrich caring skills, not only in terms of scientific knowledge, but also in relation to intrinsic, humanistic, relational and affective aptitudes [39-42]. Indeed, nurses also expand and refine their knowledge over time by elaborating their clinical practice experiences [43]; in this sense, the findings of this study could be beneficial in understanding how experience, not only educational but also clinical, can provide benchmarks for adapting and refining onco-haematology nursing care concerning the delicate and complex phase of complication monitoring in patients undergoing CAR-T cell therapy. As highlighted in the literature, in fact, the cumulative process of structuring and drawing on real-life experience engenders a body of knowledge that represents a resource for interpreting past and present experiences and, at the same time, anticipating and supporting the shaping of future experiences [43]. Ultimately, with regard to the nursing skills specific to these care contexts, the study findings may provide useful information for the development of advanced skills aimed at implementing clinical practice improvement projects. The latter would strive to optimise care time using appropriate and effective documentation, enriching the effort dedicated to a caring relationship with patients that ensures optimal quality of care and clinical safety. Moreover, appreciation of the meanings attributed to individual experiences may enhance the crucial role of haematology nurses in the management and monitoring of treatment-related toxicity, which is acknowledged as an influential factor in the overall patient experience and related care outcomes [44]. Reflecting on the advanced expertise of affirmed professionals working in multidisciplinary teams as well as on individual and group needs may increase professionals' awareness of the importance of sharing their real-life experiences. Accordingly, the methodology devised for this study and its findings may serve to develop organisational strategies aimed at effective professional training in contexts involving the introduction of specific nursing activities instrumental to the introduction of new clinical procedures and protocols. Indeed, there is a need to invest in nursing leadership and governance in order to promote further empowerment of the role of the function and to respond to the need for strong nursing standards [45] in oncohaematology practice. Lastly, the findings of this study may also stimulate thinking within the universities since, in order to invest in university education that produces advanced nursing expertise within multidisciplinary teams, it is essential that curricula are appropriately aligned with health priorities and emerging issues, both from a global and national perspective [46].
CONCLUSIONS
The introduction of innovative and complex procedures necessitates the development of healthcare and educational strategies that support the advancement and recognition of nursing expertise in specific care settings. Thus, building on the individual insights of each participant, the findings of this study may reveal hitherto unknown aspects of haematology nursing and contribute to the recent debate on advanced nursing skills by providing a detailed understanding of the experiences of nurses in haematology care.
Limitations of the study
The study may entail some limitations; the results may be affected by contextual organisational variables, which are difficult to generalise to all clinical scenarios, although they are easily transferable to a variety of contexts, also considering that the centres approved for the administration of CAR-T cell therapy meet the same national standards defined by AIFA. Nonetheless, to further ensure the credibility and transferability of the results to other organisational contexts, nurses should be selected from several approved centres throughout Italy. In addition, given the subject matter, some interviewees might place undue emphasis on the positive aspects of direct patient care while more readily identifying critical organisational factors, which do not directly impact their role identity as individuals and professional team members to the same extent.
Funding
This research did not receive any specific funding from funding bodies in the public, commercial or non-profit sectors.
Conflicts of interest
None.
Authors’ contributions
Concept and methodology: VS, LG, DC, GC; preparation and drawing up of the original manuscript draft: VS, LG, DC; supervision: GC, DC; methodology; writing, revision, and editing: LG, FG, CT, RN, AT, FP. All authors contributed to the finalisation of the study protocol and approved the final manuscript.
REFERENCES
- Alexander, M. E., Culos, K. A., Roddy, J., Shaw, J. R., Bachmeier, C. A., Shigle, T. L., & Mahmoudjafari, Z. (2021). Chimeric Antigen Receptor T cell therapy: a comprehensive review of clinical efficacy, toxicity, and best practices for outpatient administration. Transplantation and Cellular Therapy, Transplantation and Cellular Therapy, 27(7), 558–570. https://doi.org/10.1016/j.jtct.2021.01.014
- Yáñez, L., Sanchez-Escamilla, M., & Perales, M. (2019). CAR T cell toxicity: current management and future directions. HemaSphere, 3(2), e186. https://doi.org/10.1097/hs9.0000000000000186
- Santomasso, B., Nastoupil, L. J., Adkins, S., Lacchetti, C., Schneider, B. J., Anadkat, M. J., Atkins, M. B., Brassil, K., Caterino, J. M., Chau, I., Davies, M., Ernstoff, M. S., Fecher, L. A., Funchain, P., Jaiyesimi, I., Mammen, J. S., Naidoo, J., Naing, A., Phillips, T., & Ghosh, M. (2021). Management of immune-related adverse events in patients treated with chimeric antigen receptor T-cell therapy: ASCO Guideline. Journal of Clinical Oncology, 39(35), 3978–3992. https://doi.org/10.1200/jco.21.01992
- Reiser, V. L. (2020). Beyond CAR T-Cell therapy: continued monitoring and management of complications. Journal of the Advanced Practitioner in Oncology, 11(2), 159-167. https://doi.org/10.6004/jadpro.2020.11.2.4
- Yakoub-Agha, I., Chabannon, C., Bader, P., Basak, G. W., Bonig, H., Ciceri, F., Corbacioglu, S., Duarte, R. F., Einsele, H., Hudecek, M., Kersten, M. J., Köhl, U., Kuball, J., Mielke, S., Mohty, M., Murray, J., Nagler, A., Robinson, S., Saccardi, R., & Kröger, N. (2019). Management of adults and children undergoing chimeric antigen receptor T-cell therapy: best practice recommendations of the European Society for Blood and Marrow Transplantation (EBMT) and the Joint Accreditation Committee of ISCT and EBMT (JACIE). Haematologica, 105(2), 297–316. https://doi.org/10.3324/haematol.2019.229781
- Ellard, R., Kenyon, M., Hutt, D., Aerts, E., De Ruijter, M., Chabannon, C., Mohty, M., Montoto, S., Wallhult, E., & Murray, J. (2022). The EBMT immune effector cell nursing guidelines on CAR-T therapy: a framework for patient care and managing common toxicities. Clinical Hematology International, 4(3), 75–88. https://doi.org/10.1007/s44228-022-00004-8
- Baer, B. (2021). CAR T-Cell Therapy: updates in nursing management. Clinical Journal of Oncology Nursing, 25(3), 255–258. https://doi.org/10.1188/21.cjon.255-258.
- Leinemann, V., & Krutter, S. (2024, February). 'The last bridge' - How patients experience the CAR T-cell therapy: A qualitative study. European Journal of Oncology Nursing, 68, 102494. https://doi.org/10.1016/j.ejon.2023.102494
- Martinsen, K. (2006). Care and Vulnerability. Translated by Linn Elise Kjerland. Akribe. ISBN 8279501150, 9788279501152.
- Boykin, A., & Schoenhofer, S. (1993). Nursing as caring: A model for transforming practice (Vol. 15–2549). National League for Nursing.
- Hynnekleiv II, Jensen JK, Giske T, Lausund H, Maeland E, Heggdal K. (2024, April). Patients' and Nurses' experiences of caring in nursing: An integrative literature review across clinical practices. Journal of Clinical Nursing, 33(4), 1233-1255. https://doi.org/10.1111/jocn.16964
- Mao, Y., Huang, L., Ruan, H., Guo, Y., Ni, S., & Ling, Y. (2023). Patients' experience with chimeric antigen receptor T-cell therapy for DLBCL in China: a qualitative study. Supportive Care in Cancer, 31(5), 303. https://doi.org/10.1007/s00520-023-07763-x
- Stenson, C.L., Vidrine, J., Dewhurst, F., Osborne, W., Menne, T., & Stocker, R. (2022). A qualitative service evaluation of patient and caregiver experiences of CAR-T therapy: recommendations for service development and implications for palliative care teams. Palliative Medicine, 37(2), 215-220. https://doi.org/10.1177/02692163221138880
- Whisenant, M., Srour, S. A., Williams, L. A., Subbiah, I. M., Griffin, D., Ponce, D., Kebriaei, P., Neelapu, S. S., Shpall, E. J., Ahmed, S., & Wang, X. S. (2021). The unique symptom burden of patients receiving CAR T-Cell therapy. Seminars in Oncology Nursing, 37(6), 151216. https://doi.org/10.1016/j.soncn.2021.151216
- He, J., Li, J., Feng, L. N., Feng, L. X., Qiang, W., Wang, W., & Dong, L. (2024). Oncology nurse competency in chimeric antigen receptor T-cell therapy: A qualitative study. Nurse Education Today, 132, 106040. https://doi.org/10.1016/j.nedt.2023.106040
- Cohen, M. Z., Kahn, D. L., & Steeves, R. H. (2000). Hermeneutic Phenomenological Research: A Practical Guide for Nurse Researchers. SAGE Publications.
- Bartoli, D., Trotta, F., Pucciarelli, G., Simeone, S., Miccolis, R., Cappitella, C., Rotoli, , & Rocco, M. (2022). The lived experiences of family members who visit their relatives in Covid-19 intensive care unit for the first time: a phenomenological study. Heart & Lung, 54, 49–55. https://doi.org/10.1016/j.hrtlng.2022.03.012
- Patton, M. Q. (2002). Qualitative research and evaluation methods (3rd ed.). Thousand Oaks: Sage.
- Creswell, J. W., & Poth, C. N. (2018). Qualitative inquiry and research design: Choosing among five approaches (4th ed.). Thousand Oaks, CA: Sage Publications.
- Denieffe, S. (2020). Commentary: Purposive sampling: complex or simple? Research case examples. Journal of Research in Nursing, 25(8), 662-663. https://doi.org/10.1177/1744987120928156
- Douglas, H. (2022). Sampling Techniques for Qualitative Research. In M.R. Islam, N.A. Khan, & R. Baikady (Eds.), Principles of Social Research Methodology. Springer, Singapore. https://doi.org/10.1007/978-981-19-5441-2_29
- Trotter R.T., II (2012) Qualitative research sample design and sample size: resolving and unresolved issues and inferential imperatives. Preventive Medicine55(5), 398–400.
- Starks, H., & Trinidad, S. B. (2007). Choose your method: A comparison of phenomenology, discourse analysis, and grounded theory. Qualitative Health Research, 17(10), 1372-1380. https://doi.org/10.1177/1049732307307031
- Guest, G., Namey, E., & Chen, M. (2020). A simple method to assess and report thematic saturation in qualitative research. PLoS ONE, 15(5), e0232076. https://doi.org/10.1371/journal.pone.0232076
- Guest, G., Bunce, A., & Johnson, L. (2006). How many interviews are enough? An experiment with data saturation and variability. Field Methods, 18(1), 59-82.
- Creswell, J. (1998). Qualitative inquiry and research design: Choosing among five traditions. Thousand Oaks, CA: Sage.
- Braun, V., & Clarke, V. (2006). Using thematic analysis in psychology. Qualitative Research in Psychology, 3(2), 77-101. https://doi.org/10.1191/1478088706qp063oa
- Mattimoe, R., Hayden, M. T., Murphy, B., & Ballantine, J. (2021). Approaches to analysis of qualitative research data: A reflection on the manual and technological approaches. Accounting, Finance & Governance Review, 27.
- Polit, D. F., & Beck, C. T. (2004). Nursing Research: Principles and Methods. Lippincott Williams & Wilkins, Philadelphia, PA.
- Kockelmans, J. J. (1975). Towards an interpretive or hermeneutic social science. Graduate Faculty Philosophy Journal: New School of Social Research, 5, 73-96.
- Steeves, R. H. (1992). Technical notes: A typology of qualitative data. Western Journal of Nursing Research, 14(4), 532-536.
- Wæraas, A. (2022). Thematic Analysis: Making Values Emerge from Texts. In G. Espedal, B. Jelstad Løvaas, S. Sirris, & A. Wæraas (Eds.), Researching Values. Palgrave Macmillan, Cham. https://doi.org/10.1007/978-3-030-90769-3_9
- Barritt, L., Beekman, X., Bleeker, H., & Mulderij, K. (1983). A handbook for phenomenological research in education. Ann Arbor: University of Michigan, School of Education.
- Barritt, L., Beekman, T., Bleeker, H., & Mulderij, K. (1984). Analyzing phenomenological descriptions. Phenomenology and Pedagogy, 2(1), 1-17.
- van Manen, M. (1984). "Doing" phenomenological research and writing: An introduction. Alberta, Canada: Department of Secondary Education
- Burnard, P. (1991). A method of analysing interview transcripts in qualitative research. Nurse Education Today, 11, 461–466.
- Kahn, D. L., & Steeves, R. H. (1994). Witnesses to suffering nursing knowledge, voice, and vision. Nursing outlook, 42(6), 260–264. https://doi.org/10.1016/0029-6554(94)90046-9
- Lincoln, Y. S., & Guba, E. G. (1986). But is it rigorous? Trustworthiness and authenticity in naturalistic evaluation. New Directions for Program Evaluation, (30), 73–84.
- Zannini, L. (2008). Medical humanities e medicina narrativa. Nuove prospettive nella formazione dei professionisti della cura. Raffaello Cortina, Milano.
- Mortari, L. (2006). La pratica dell’aver cura. Mondadori, Milano.
- Manara, D., Villa, G., & Moranda, D. (2015). Alla ricerca della salienza: Analisi fenomenologica del disagio etico. L’infermiere, n.1, 2015. Retrieved from https://www.infermiereonline.org/2015/03/31/alla-ricerca-della-salienza-analisi-fenomenologica-del-disagio-etico/
- Benner, P. (2000). The roles of embodiment, emotion and lifeworld for rationality and agency in nursing practice. Nursing Philosophy, 1, 5-19.
- Bilodeau, K., Henriksen, C., Aloisio Alves, C., Piché, L., Pepin, J., Lee, V., Vachon, M. F., Folch, N., Pomey, M. P., & Fernandez, N. (2024). Learning to provide humanistic care and support in the context of chronic illness: Insights from the narratives of healthcare professionals in hemato-oncology. European Journal of Oncology Nursing, 69, 102522. https://doi.org/10.1016/j.ejon.2024.102522
- Lobban, L., & Perkins, S. (2013). Role of the specialist nurse in caring for patients with myeloma. Nursing Standard, 28(5), 37-41. doi: 10.7748/ns2013.10.28.5.37.e8046.
- International Council of Nurses (ICN). Guidelines on advanced practice nursing 2020. Ginevra. Disponible a: https://www.icn.ch/system/files/documents/2020-04/ICN_APN%20Report_EN_WEB.pdf. Ultimo accesso: 16 gennaio 2024.
- World Health Organization (WHO). State of the Worlds’s Nursing 2020: Investing in Education. Jobs and Leadership. Geneva, Switzerland. Disponibile a: https://www.who.int/publications/i/item/9789240003279. Ultimo accesso: 16 gennaio 2024.
![]() This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Mentorship effect on healthcare providers' adherence to postpartum haemorrhage guidelines and maternal outcomes in Rwanda. A quasi-experimental study
Benjamin David Habikigeni 1, Arlette Bizimana 2, Maxwell Mhlanga 3*, Tsion Yohannes 4
1;2;3;4 Centre of Gender Equity, University of Global Health Equity, Kigali, Rwanda
* Corresponding Author: Maxwell Mhlanga Centre of Gender Equity, University of Global Health Equity, Kigali, Rwanda
Cite this article
ABSTRACT
Background: Postpartum hemorrhage (PPH) is a leading cause of maternal morbidity and mortality worldwide. Effective management of PPH heavily relies on adherence to clinical guidelines. Mentorship programs aim to enhance healthcare providers' (HCPs) knowledge, skills, and guideline adherence, but their impact on guideline adherence needs evaluation.
Objective: To evaluate the effect of a clinical mentorship program on HCPs' adherence to PPH clinical guidelines and patient outcomes at Muhima District Hospital (DH) and its associated health centers (HCs).
Methods: A quasi-experimental design was used to compare HCPs' adherence to clinical guidelines before and after mentorship. Maternal outcomes were also analyzed in relation to guideline adherence. Standardized medical records provided data, and consecutive sampling included cases sequentially from medical registers. The Wilcoxon test was used to assess the effect of mentorship on adherence to guidelines. Multivariate regression analysis was performed to explore the relationship between mentorship, guideline adherence, and maternal outcomes.
Results: The study included 384 women with PPH. Adherence to clinical guidelines before (96.4%) and after (95.8%) the mentorship program showed no significant change (P-value = 0.25). However, adherence to guidelines was significantly associated with better maternal outcomes (P-value < 0.001). Multivariate logistic regression indicated significantly lower odds of no complications in cases where guidelines were not followed. Adherence to guidelines (AOR = 0.061, 95% CI: 0.001- 0.026), prolonged labor (AOR = 187.25, 95% CI: 13.07- 2683.14), blood loss (AOR = 0.004 95% CI: 0.000 - 0.0008), and specific causes of PPH (AOR = 0.013, 95% CI: 0.000- 0.068) had significant associations with maternal outcomes.
Conclusion: Adherence to clinical guidelines is critical for high-quality care and improved maternal outcomes in PPH cases. The study confirms the positive impact of guideline adherence on maternal outcomes, emphasizing the importance of promoting and strengthening adherence. While the mentorship program supported high adherence rates among HCPs, it alone may not be sufficient to ensure adherence, suggesting the influence of additional factors, such as training from other institutions.
Keywords: Mentorship, Healthcare Providers, Postpartum Hemorrhage, Maternal Outcomes, Clinical Guidelines, Quasi-experimental Study
INTRODUCTION
A woman dies unnecessarily every two minutes due to preventable pregnancy and childbirth-related issues [1]. Though the world saw a remarkable 38% decline in maternal mortality between 2000 and 2017, the death toll continues to be dangerously high [2]. In 2020, the global maternal mortality ratio (MMR) was 223 deaths per 100,000 live births and in Rwanda the mortality rate was 203 deaths per 100 000 live births, with postpartum haemorrhage (PPH) being the primary cause of death [3,4]. PPH is the major contributor to maternal deaths, responsible for 27.1% of maternal deaths worldwide, with 44% of such deaths in the Sub-Saharan Africa region [5] and 22.7% in Rwanda [6]. PPH is excessive bleeding after childbirth, with blood loss of more than 500 millilitres (mL) for a vaginal delivery or 1000 mL for a caesarean section [7]. PPH is categorized as primary when it occurs within 24 hours of birth and secondary when it happens more than 24 hours after delivery up to 12 weeks postpartum [8]. The underestimation of the actual blood loss by healthcare providers was identified as problematic in diagnosing and managing PPH [8]. In addition to the high mortality, PPH is responsible for morbidities such as anaemia, complications from a blood transfusion, and hysterectomy, resulting in the loss of childbearing capacity [9]. Many factors contribute to the adverse outcomes of PPH in developing countries. Those factors comprise low socioeconomic status, limited access to healthcare, shortage of skilled healthcare professionals, and inadequate healthcare manifested by poor adherence to established evidence-based protocols [10]. Regarding the economic aspect, studies report that Women in low-income countries are at higher risk of dying during childbirth, with 1 in 45 deliveries in comparison to 1 in 5400 deliveries in developed countries [4].
In healthcare, evidence has shown that adherence to established guidelines can improve the standard of care and decrease mortality [11]. However, in spite of the availability of guidelines and protocols, adhering to them remains challenging in many developing countries [12].
Regular training and education for healthcare professionals on PPH guidelines and protocols can
help ensure they have the knowledge and skills to provide high-quality care [12]. Mentorship is an effective tool for capacity building of healthcare providers in diagnosing and managing diseases by improving their knowledge, skills, and confidence, resulting in better patient outcomes [13]. Clinical mentorship refers to knowledgeable and experienced healthcare professionals guiding and advising less experienced ones on diagnosing and managing medical conditions in their professional development [14].
The government of Rwanda has invested in training healthcare providers in managing PPH and other obstetric emergencies and has developed guidelines and protocols for managing PPH but there is a gap in information on whether mentorship improves healthcare providers practice [15,16]. This study assessed the impact of a clinical mentorship program on HCPs' adherence to PPH guidelines and maternal outcomes in Muhima District Hospital catchment area.
MATERIALS AND METHODS
Design and setting: A quasi-experimental non-equivalent before-and-after study was conducted in the maternity department of two health centers, Cornum and Rwampara in the Nyarugenge district of Kigali city. Nyarugenge District has the busiest maternity service facilities in Rwanda, with approximately 7000 births per year [17].
Population target: The population consists of women who gave birth and developed PPH in the study locations. The sample was divided into two groups: those assisted by staff without specific training in managing postpartum hemorrhage (pre-intervention) and those by staff after training (post-intervention).
Instrument: Medical records were used to collect socio-demographic (age, residence, health center, and insurance) and clinical data (medical history, physical examination, clinical management). A checklist was used for evaluation at the postopography. The checklist highlighted key areas to assess for adherence to evaluate overall adhere to clinical guidelines The checklist had sections which included PPH prevention measures guidelines, PPH initial management measures and secondary management guidelines. Medical records of women with primary and secondary PH who gave birth in the study locations were included, missing or incomplete medical records or medical history records, physical examination, and clinical management were excluded.
Jhpiego-Rwanda tutoring program:
Jhpiego Rwanda is implementing a clinical mentorship program using a model called ‘Low Dose High Frequency’. Low Dose High Frequency (LDHF) enhances clinical abilities by conducting brief and focused simulation-based learning sessions [18]. The project was implemented in seven district hospitals and 129 health centers, where two to four nurses and midwives per health center were selected to participate in the program. The training was conducted from January 2021 to April 2021. The training methods include one-on-one case management observation, analysis of patient monitoring data, discussions on clinical cases, bedside training, and clinical team meetings. One of the mentorship program’s focuses is managing postpartum hemorrhage. The training sessions were given initially and were reinforced by monthly visits and evaluations by mentors in clinical settings to maximize the retention of knowledge and skills. The mentorship program is part of the Barame Maternal, Neonatal, and Child Health (MNCH) Project, funded by Enabel, the Belgium cooperation, and was initiated in December 2020 [19] and is meant to increase the competencies of nurses and midwives in adhering to clinical guidelines of PPH resulting in better maternal outcomes.
Measure(s)
The healthcare providers’ adherence to clinical guidelines was determined using a checklist, by evaluating the partographs. Each required action performed was given one point. A necessary action not performed was given zero. A total score was calculated and the corresponding percentage. An 80% and above percentage score was considered adherence, whereas a lower percentage was regarded as non-adherence, as 80% or more adherence is required for optimal therapeutic efficacy [20].
Maternal outcomes were extracted from health center registers, and grouped into good outcome, morbidity, and mortality. Mothers who were managed successfully, with no complications were considered to have good outcomes. Patients who had complications such as anemia, hemorrhagic shock, kidney injury, infections, and hysterectomy were classified as having morbidity. Mothers who died due to PPH had mortality as an outcome.
Data collection
Data collection started after approval from the Institutional Review Board (IRB) at the University of Global Health Equity (UGHE) and authorization from the Muhima DH and HCs administrations. We explored the health center registers to find patients who had PPH. For referred patients, their outcomes were found in Muhima DH registers and Health Management Information System (HMIS). Once a list of all patients with PPH was identified, then we audited their medical records to extract their socio-demographic characteristics (age, residence, health center, and insurance), their clinical characteristics (parity, cause of PPH, prolonged labor, estimated blood loss, concurrent illnesses, and referral) and the maternal outcomes. We assessed adherence to the partographs using a checklist. There was no direct contact with patients whose records were selected. The confidentiality and security of the personal information of the participants were respected. The pre-intervention and post-intervention groups were made as similar as possible by choosing them from the same healthcare facility and including the clinical clinics of the women treated by the same healthcare workers before and after the implementation of the mentoring program. The group of women enrolled from 1 December 2018 to 1 December 2020 correspond to the pre-mentoring program sample, those from 1 May 2021 to 1 May 2023 correspond to the women assisted by personnel who have carried out the training (post-mentoring).
Data analysis
Descriptive statistics were used to summarize data in SPSS 26. The socio-demographic characteristics that were considered in this study were age, place of residence, health insurance and the type of health centre basing on the findings from the existing literature on similar studies. Similarly, the clinical characteristics that we considered were parity, causes of PPH, prolonged labour, estimated blood loss, concurrent illness and referrals. The chi-square test or Fisher’s exact test were performed to evaluate significant differences in proportions or percentages between the two groups. Fisher’s exact test was used where the chi-square test was not appropriate. Wilcoxon signed-rank test was used to test the association between adherence status (pre and post) and mentorship status, as well as the association between adherence status and maternal outcomes. We conducted a multivariate logistic regression analysis to examine the association between socio-demographic, clinical factors and maternal outcomes. Adjusted Odds ratio, Confidence Intervals, and p-values were reported. Finally, all tests with p-value (P) < 0.05 were considered significant.
Ethical considerations
The study was approved by the University of Global Health Equity Institutional Review Board (UGHE-IRB/2023/013) and Rwanda Ministry of Health (NHRC/2023/PROT/16).
RESULTS
Socio-demographic characteristics
A total of 384 women of which 192 were in the pre- group and 192 were in the post group were
reviewed in this study. Two hundred and four women (53.1%) were from Cornum Health Center and 180 (46.9%) from Rwampara Health Center (Table 1).
| Socio-demographic characteristics | Before mentorship
Frequency (%) |
After mentorship
Frequency (%) |
|
| Health center | Cornum
Rwampara |
102 (53.1%)
90 ( 46.9%) |
102 (53.1%)
90 (46.9%) |
| Age | 40-49 years
30-39 years 20-29 years 10-19 years |
3 (1.6%)
40 (20.8%) 125 (65.1%) 24 (12.5%) |
1 (0.5%)
47 (24.5%) 132 (68.8%) 12 (6.3%) |
| Residence | Urban
Peri-urban |
145 (75.5%)
47 (24.5%) |
157 (81.8%)
35 (18.2%) |
| Insurance | Had insurance
No insurance |
188 (97.9%)
4 (2.1%) |
186 (96.9%)
6 (3.1%) |
Table 1. Socio-demographic characteristics of samples
Clinical characteristics
Regarding clinical characteristics of women with PPH as recorded in medical records, the majority of the women were multiparous. Most patients, (93%) had perineal tears and (97.1%) had blood loss between 500-1000 ml (Table 2).
| Clinical characteristics | Before mentorship
Frequency (%) |
After mentorship
Frequency (%) |
|
| Parity | Primiparity
Multiparity Grand multiparity |
77 (40.1%)
108 (56.3%) 7 (3.6%) |
72 (37.5%)
115 (59.9%) 5 (2.6%) |
| Cause of PPH | Perineal tear
Cervical tear Uterine atony Retained placenta Perineal tear and retained placenta |
174 (90.6%)
5 (2.6%) 4 (2.1%) 7 (3.6%) 2 (1%) |
183 (95.3%)
0 (0.0%) 5 (2.6%) 4 (2.1%) 0 (0.0%) |
| Prolonged labor | No
Yes |
184 (95.8%)
8 (4.2%) |
192 (97.9%)
0 (0.0%) |
| Estimated
blood loss |
>1000 ml
500-1000 ml |
6 (3.1%)
186 (96.9%) |
5 (2.6%)
187 (97.4%) |
| Concurrent illness | None
Preeclampsia |
191 (99.5%)
1 (0.5%) |
192 (100%)
0 (0.0%) |
| Referred to a
higher level |
No
Yes |
186 (96.9%)
6 (3.1%) |
185 (96.4%)
7 (3.6%) |
Table 2. Clinical Characteristics
Healthcare providers’ adherence to clinical guidelines
The Wilcoxon signed-rank test was conducted to determine whether the intervention was had an overall significant effect on adherence to clinical guidelines. The null hypothesis (HO) states that there is no difference in adherence scores before and after the intervention. With a p-value of 0.25, we fail to reject the null hypothesis at the 0.05 significance level (Table 3). This means there is not enough statistical evidence to conclude that the intervention led to a significant change in adherence to clinical guidelines. The same trend of results was realised at the individual sites which were Cornum health facility (P=0.25) and Rwampara (P=0.71) (Table 3).
|
Variable |
N |
Median
Pre-Intervention |
Median
Post-Intervention |
p-value |
Positive
Ranks Sum |
Negative
Ranks Sum |
| Adherence
Score (overall) |
192 | 83.7
(73.3-85.2) |
82.9
(71.1-83.2) |
0.25 | 3402 | 2246 |
| Adherence score (Cornum) | 102 | 83.9
(73.2-84.2) |
82.9
(70.4-83.2) |
0.25 | 1218 | 722 |
| Adherence
Score (Rwampara) |
90 | 83.4
(82.14-83.24) |
82.8
(80.33-83.24) |
0.71 | 520 | 415 |
Table 3. Adherence to clinical guidelines.
Factors associated with maternal outcomes
There was a statistically significant association between adherence level and maternal complications (P<0.0001), Blood loss and maternal complications (P<0.0001), prolonged labor and maternal complications (P<0.00195) and causes of PPH with maternal complications (P< 0.0001) (Table 4). Conversely, there was no association between age category (P=0.19), place of residence (P=0.51), Health center (P=0.16), parity (P=0.53), concurrent illnesses (P=1.0) and maternal complications (Table 4).
|
Variables Modalities |
Complications n (%) |
No complications n (%) |
P-value (test) |
|
| Adherence level | Did not adhere
Adhered |
9 (64.3%)
5 (35.7%)
|
6 (1.6%)
364 (98.4%)
|
<0.0001* (F) |
| Age group | 10-19 years
20-29 years 30-39 years 40-49 years |
1 (7.1%)
8 (57.1%) 4 (28.6%) 1 (7.1%) |
35 (9.5%)
249 (67.3%) 83 (22.4%) 3 (0.8%) |
0.19 (F)
|
| Residence | Urban
Peri-urban |
10 (71.4%)
4 (28.6%) |
292 (78.9%)
78 (21.1%) |
0.51 (F) |
| Health center | Cornum
Rwampara |
10 (71.4%)
4 (28.6%) |
194 (52.4%)
176 (47.6%) |
0.16 (F) |
| Insurance | No insurance
Had insurance |
1 (7.1%)
13 (92.6%) |
9 (2.4%)
361 (97.6%) |
0.31 (F) |
| Blood loss | 500- 1000 ml
>1000 ml |
5 (35.7%)
9 (64.3%) |
368 (99.5%)
2 (0.5%) |
<0.0001* (F) |
| Parity | Primiparity
Multiparity Grande multiparity |
5 (35.7%)
8 (57.1%) 1 (7.1%) |
144 (38.9%)
215 (58.1%) 11 (3.0%) |
0.53 (F) |
| Prolonged labor | No
Yes |
11 (78.6%)
3 (21.4%) |
365 (98.6%)
5 (1.4%) |
0.00195* (F) |
| Concurrent illnesses | None
Preeclampsia |
14 (100%)
0 (0%) |
369 (99.7%)
1 (0.3%) |
1.0 (F) |
| Causes of PPH | Perineal tear
Cervical tear Uterine atony Retained placenta Perineal tear and retained placenta |
2 (14.3%)
2 (14.3%) 8 (57.1%) 2 (14.3%) 0 (0%) |
355 (95.9%)
3 (0.8%) 1 (0.3%) 9 (2.4%) 2 (0.5%) |
<0.0001* (F) |
| *=significant test, C=chi-square test; F= Fisher’s exact test | ||||
Table 4. Factors associated with maternal outcomes.
Logistic regression analysis on adherence to clinical guidelines and maternal outcomes
We conducted a multivariate logistic regression analysis to examine the association between clinical factors and maternal outcomes. Variables in bivariate analysis with a p-value <0.100 (Age group, Residence, Health Center, Insurance, Parity, Prolonged labor, Blood loss, Cuncurrent illness and Cause) were used in multivariate analysis. Multivariate regression analysis was done using the “enter” method. Adjusted Odds ratio, (AOR) Confidence Intervals, and p-values were reported. The variables found to have a statistically significant relation to maternal outcomes are, “Prolonged labor”, “Blood loss,” and “Causes of PPH”. Adherence to guidelines reduced the odds of maternal complications by more than 99% (AOR = 0.0061, 95% CI: 0.001- 0.0264) (Table 5).
| Logistic regression | Coefficient | Standard Error | AOR | CI at 95% | P-value |
| Adherence/maternal outcome | -6.80 | 0.005 | 0.0061 | 0.001- 0.0264 | <0.0001* |
| Age/maternal outcome | 0.08
|
1.77 | 1.13 | 0.05 – 24.31 | 0.94 |
| Residence/maternal outcome | -0.50 | 0.73 | 0.42 | 0.01 – 13.00 | 0.62
|
| HC/maternal outcome | -0.85 | 0.40 | 0.24 | 0.01 – 6.21 | 0.39
|
| Insurance/ maternal outcome | -0.17 | 1.82 | 0.61 | 0.002 – 205.14 | 0.87 |
| Parity/maternal outcome | -0.83 | 0.44 | 0.35 | 0.03 – 4.10 | 0.41
|
| Prolonged labor/maternal outcome | 3.85 | 254.35 | 187.25 | 13.07 – 2683.14 | <0.0001* |
| Blood loss/ maternal outcome | -5.15 | 0.00 | 0.0004 | 0.000 – 0.008 | <0.0001*
|
| Concurrent illnesses/ maternal outcome | 1 |
|
|||
| Causes of PPH/maternal outcome | -3.32 | 0.017 | 0.013 | 0.000 – 0.168 | 0.001*
|
| Constant | 0.74 | 8722 | 942.30 | 0.00 – 7.14e+10 | 0.46
|
| *=significant test; AOR=Adjusted odd ratio; CI= AOR confidence interval at 95% | |||||
Table 5. Logistic regression of independent variables and maternal outcomes.
DISCUSSION
This present study aimed to investigate the effect of a mentorship program on healthcare providers’ adherence to PPH clinical guidelines and the maternal outcomes of women who developed PPH Nyarugenge district.
With regards to socio-demographic characteristics, the results showed an increase in the 30-39 and 20-29 age groups of healthcare providers and a decrease in the older and youngest age groups suggesting that younger healthcare providers in Rwanda might be more receptive to joining midwifery and maternal departments (Table 1). Similar studies in Sub-Saharan Africa, have shown that younger health care providers are more likely to adopt new clinical guidelines after training and mentorship programs [21]. The increase in urban healthcare providers post-mentorship might be due to better access to resources, continuous professional development, and support systems. In Rwanda, urban areas often have better healthcare infrastructure, which can facilitate better adherence to guidelines. Studies in similar settings have highlighted that urban health care providers are more likely to benefit from mentorship programs [22]. Access to health insurance can provide additional resources for training and support, but the minimal change in insurance status suggests that the mentorship program itself was the primary driver of improved adherence.
With regards to clinical characteristics, there was a slight decrease in primiparity and grand multiparity cases, with an increase in multiparity cases (Table 2). This suggests that the mentorship program might have improved the management and identification of multiparity cases, leading to better adherence to guidelines for this group. Studies in Rwanda and similar settings have shown that multiparity is often associated with higher risk of complications, and better management of these cases post-mentorship aligns with improved adherence to guidelines [23].
The increase in the identification of perineal tears and the decrease in cervical tears, retained placenta, and combined cases suggests improved diagnostic accuracy post-mentorship (Table 2). Accurate diagnosis and management of PPH causes, especially perineal tears, are critical. Improved diagnostic accuracy post-mentorship is consistent with findings from other mentorship programs in the region [23]. Similarly, there was a slight decrease in cases with estimated blood loss >1000 ml and an increase in 500-1000 ml cases suggesting an improved early intervention and management of blood loss (Table 2). Early intervention to manage blood loss is crucial, and the improvement seen here is consistent with other studies showing that mentorship programs enhance the ability of healthcare providers to manage PPH effectively [24].
Results also showed that all cases of concurrent illness (preeclampsia) were resolved post-mentorship, indicating better management and preventive measures (Table 2). Effective management of preeclampsia post-mentorship is significant, as similar studies have shown that training and mentorship programs are essential in improving the management of concurrent illnesses [25]. The complete elimination of prolonged labour cases post-mentorship indicates better intrapartum care, aligning with studies highlighting the importance of mentorship in improving
labor management [26].
Additionally, there was a slight increase in referrals to a higher level post-mentorship which could indicate better identification of cases requiring advanced care. Slightly increased referrals to higher-level care indicate better identification and management of complicated cases, which is a positive outcome seen in other similar settings [27].
With regards to healthcare providers’ adherence to clinical guidelines, the overall adherence scores showed a slight decrease post-intervention, with the median dropping from 83.7 to 82.9 (Table 3). Our threshold level for adherence was 80%, as an adherence score of 80% or more is required for optimal therapeutic efficacy [19]. The Hypothesis was that mentorship improves healthcare providers’ adherence to PPH clinical guidelines. The p-value of 0.25 indicates that this change is not statistically significant (Table 3).
These findings suggest that mentorship alone may not be the sole determinant of adherence to clinical guidelines, and other factors might play a role in influencing healthcare providers’ adherence behaviours. Contrary to our finding, a study conducted in Rwanda on a mentorship program aiming to bridge the gap in nurses’ knowledge and skills done in 21 health centres showed the program significantly improved clinical practice and quality of care delivered at rural HCs in Rwanda [20].
The lack of statistical significance in this study might be due to the short duration of the mentorship program or other contextual factors. Studies have reported varying impacts on adherence scores post-intervention, often depending on the specific clinical guidelines and the training's focus areas [25]. The slight decrease in scores in this study contrasts with some reports of increases, suggesting a need to review the mentorship program's content and delivery.
Our analysis also considered other key factors contributing to these results, such as the impact of Covid-19, as during the pandemic period, pregnancies increased, leading to increased deliveries [21]. Furthermore, other programs aimed at enhancing healthcare providers' skills could impede the
effectiveness of the current mentorship approach and adherence to established guidelines.
Another possible reason could be the fact that the documentation routine did not change after the mentorship program implementation. The lack of specific patient files for documentation may have limited the ability to observe a difference in adherence before and after the mentorship program. Without comprehensive and standardized documentation, it becomes challenging to accurately assess the level of adherence and track improvements over time. The reliance on only partographs, specific forms for monitoring labour progress, may not capture the full scope of adherence to PPH guidelines. In the context of postpartum haemorrhage (PPH) clinical guidelines, proper documentation is essential for assessing adherence to recommended protocols and ensuring optimal therapeutic efficacy [22].
The positive ranks sum is higher than the negative ranks sum, suggesting that more individuals improved their scores than those who did not (Table 3). The higher positive ranks sum in this study indicates that while the overall median adherence scores did not significantly improve, a notable number of individuals did show improvement. This is consistent with findings that mentorship programs can have differential impacts across different individuals and settings [23].
With regards to the factors associated with maternal outcomes, results showed a strong relationship between adherence to clinical guidelines and maternal outcomes. The odds of not having complications for women treated by healthcare providers who did not adhere to clinical guidelines were significantly lower than those managed by providers who adhered to guidelines (Table 5). Adherence to guidelines is associated with a higher likelihood of experiencing good maternal outcomes (Table 5). The results resonate with a post-hoc analysis study done in India on adherence to evidence-based practices during childbirth to prevent childbirth-related mortality and morbidity, where they found that adherence to WHO Safe Childbirth Checklist (SCC) during delivery was significantly associated with reduced odds of childbirth-related mortality and morbidity, and
neonatal mortality [26].
The negative coefficient and very low AOR indicated a strong negative association between adherence to clinical guidelines and poor maternal outcomes (Table 5). The significant p-value (P<0.0001) confirms this relationship, suggesting that better adherence to clinical guidelines significantly improves maternal outcomes.(Table 5). Mugisha and others also found that adherence to clinical guidelines significantly reduced maternal mortality and morbidity, highlighting the importance of training and mentorship programs in ensuring guideline adherence [23]. Both studies underscore the critical role of adherence to clinical guidelines in improving maternal health outcomes, affirming the effectiveness of mentorship programs in reinforcing these practices.
Prolonged labor shows a strong positive association with poor maternal outcomes, with a very high AOR and a significant p-value (P<0.0001) and this indicates that prolonged labor significantly increases the risk of adverse maternal outcomes (Table 5). Numerous studies, including studies in sub-Saharan Africa have shown that prolonged labour is a major risk factor for adverse maternal outcomes, emphasizing the need for timely and effective interventions [28].The significant impact of prolonged labour across studies highlights the necessity for interventions targeting labour management within mentorship programs to improve maternal health
Severe blood loss is strongly negatively associated with maternal outcomes, with an extremely low AOR and a significant p-value (P<0.0001 and this indicated that increased blood loss significantly worsens maternal outcomes (Table 5). Blood loss greater than 1000 ml was significantly associated with higher complications, indicating the critical importance of managing blood loss during postpartum.The findings align with global research, including studies which demonstrate that severe blood loss (>1000 ml) is a critical risk factor for adverse maternal outcomes, stressing the importance of effective management of hemorrhage during the postpartum period [27].
Similar studies also found that managing blood loss effectively is crucial for improving maternal outcomes, reaffirming the importance of early detection and intervention [8].
Different causes of PPH are strongly negatively associated with maternal outcomes, with a very low
AOR and a significant p-value (P<0.001), indicating that proper identification and management of PPH causes significantly improve maternal outcomes (Table 5). Ssimilar studies also highlighted the importance of identifying and managing the specific causes of PPH to improve outcomes. The agreement across studies highlights the necessity for targeted training on PPH management within mentorship programs [26].
The results showed that most women had no complications (96.4%) (Table 4). This suggests that the healthcare providers and the healthcare system effectively managed PPH and ensured positive maternal outcomes for most cases. In cases where patients had complications, a more considerable proportion (64.3%) had poor adherence to guidelines, providing compelling evidence of the association between adherence to clinical guidelines and complications as the outcome (Table 4). The results align with a cross-sectional study conducted in South Australia, highlighted a correlation between lower adherence scores, significant avoidable complications, and adverse outcomes [23].
A study examining the trend of surgical site infections in paediatric patients with complicated appendicitis found that using clinical practice guidelines was associated with lower morbidity rates after appendectomy [24]. Another study compared the safety, efficacy, and cost-effectiveness of evidence-based clinical guidelines in treating acute low back pain in primary care and usual care, searching for evidence showing whether following guidelines results in better outcomes. It found that in the short term, evidence-based care shows only slight improvement compared to usual good care. However, evidence-based guidelines demonstrate substantial and meaningful advancements over an extended period, leading to fewer patients needing ongoing treatment and experiencing persistent pain [25]. Adhering to guidelines is vital in providing appropriate evidence-based care, improving outcomes, and reducing complications. Age showed a very weak and non-significant relationship with maternal outcomes (P= 0.94) (Table 5). This suggests that age, in isolation, may not be a strong predictor of maternal outcomes, emphasizing the need to focus on other clinical and demographic factors.
Residence had a non-significant relationship with maternal outcomes (P=0.62 (Table 5). Rutayisire and others found mixed results, with some peri-urban areas showing worse outcomes due to limited access to healthcare services, but overall residence was not a significant predictor.Both studies indicate that while location may influence access to care, it is not a standalone predictor of maternal outcomes when other variables are considered [29].
The health center variable also showed a non-significant relationship with maternal outcomes (P=0.39)(Table 5). The AOR and confidence interval suggest a potential trend, but the results are not statistically significant (Table 5). This study's findings align with the idea that adequate training and mentorship can standardize care quality across different health centers, reducing outcome disparities
Insurance status shows no significant impact on maternal outcomes (P=0.87) (Table 5). A similar study reported non-significant associations between insurance status and maternal outcomes, suggesting that other factors such as quality of care and adherence to guidelines are more critical. Both studies highlight that while insurance improves access to healthcare, it does not directly translate to better maternal outcomes without high-quality clinical care [20].
Similarly, parity had a non-significant relationship with maternal outcomes (P=0.41) indicating that the number of previous births is less critical than the quality of care provided (Table 5). Similar studies have shown the same trend suggesting that parity may not be a primary concern in improving maternal outcomes compared to other clinical factors.
The logistic regression analysis highlights the significant impact of adherence to clinical guidelines, prolonged labor, blood loss, and causes of PPH on maternal outcomes. These findings underscore the critical importance of adhering to clinical guidelines, effectively managing prolonged labor and blood loss, and accurately diagnosing and treating the causes of PPH to improve maternal health.
CONCLUSION
The study results showed that though the clinical mentorship program had no significant effect in improving adherence levels to clinical guidelines for PPH, the high adherences rates observed among healthcare providers in this study contributed to positive maternal outcomes and to a reduction in the incidence of morbidity. Results suggest that mentorship programs and consistent on-job support may support maintenance of adherence behaviours among healthcare providers. However, mentorship alone may not be the sole determinant of adherence. Efforts to promote adherence should be emphasized to enhance delivery of evidence-based and standardized care for managing PPH.
Study Strengths
One advantage of this study is that it allowed us to make a temporal comparison of changes in adherence to clinical guidelines and maternal outcomes in the same facilities over time, pre- and post-mentorship. Additionally, the women in the sample were managed by the same healthcare providers before and after mentorship, with no staff turnover, reducing the effect of confounders. Moreover, using a quasi-experimental design helped us evaluate the mentorship program’s implementation in a real-world setting, reflecting the practical challenges and constraints of the actual implementation, thereby enhancing the external validity and relevance of the findings. Another advantage is that we reached the number of PPH cases needed for the sample size at the time of the study. Information was obtained from standardized medical records rather than relying on maternal or healthcare providers’ recall, thus minimizing recall bias. Another strength of the study is its long duration (4 years), which enables the implementation of changes in clinical practice and routines to be observed and analyzed. While our study cannot provide the same level of causal inference as experimental designs, we used various strategies to strengthen the causal inferences. These include careful selection and matching of comparison groups. We ensured that the medical records of women who had PPH were from the same health centers and treated by the same healthcare providers before and after the mentorship. Statistical adjustments for potential confounding variables and rigorous data analysis were also applied.
Study Limitations
It is essential to acknowledge the limitations of this study. We observed limitations in recording among the two health centers included in our study due to a lack of patient files. The only records are from the patient partographs, which are not as detailed as typical patient files; hence, this could partially explain the lack of association between mentorship and adherence. The assessment of adherence to clinical guidelines also relied on documentation in medical records, which could introduce reporting bias. Additionally, the study was conducted in a distinct setting (Muhima DH catchment area), which may limit the generalizability of the results to other healthcare contexts.
Ethics considerations.
Ethics issues have been completely observed by authors.
Funding
We want to acknowledge the University of Global Health Equity of providing technical and financial support for the successful completion of this study.
Conflict of Interest
The authors declare that there is no conflict of interest.
Acknowledgements
We want to thank JHPIEGO Rwanda for the support in the success of the research as preceptors.
We also extent our gratitude to the University of Global Health Equity for all the support.
Authors’ Contributions
Benjamin David Habikigeni: Development of the original manuscript
Arlette Bizimana: Development of the original manuscript
Maxwell Mhlanga: Review of manuscript, editing and discussion
Tsion Yohannes: Review of manuscript, editing and references
REFERENCES
- World Health Organization. (2019). Maternal mortality. WHO-FACTS. https://www.who.int/news-room/fact-sheets/detail/maternal-mortality
- World Bank. (2017). The number of maternal deaths | Data. World Bank-DATA. https://data.worldbank.org/indicator/SH.MMR.DTHS
- Demographic and Health Survey. (2021). Demographic and Health Survey Report. https://dhsprogram.com/pubs/pdf/FR370/FR370.pdf Accessed: 2022-12-20
- (2022). WHO postpartum hemorrhage (PPH) summit. WHO-PPH Summit. https://www.who.int/publications/m/item/who-postpartum-haemorrhage-(PPH)-summit
- Federation International de Gynecology et Obstetric. (2018). PPH is leading to unnecessary deaths | Figo. FIGO. https://www.figo.org/news/pph-leading-unnecessary-deaths
- Bazirete, O., Nzayirambaho, M., Umubyeyi, A., Uwimana, M. C., & Evans, M. (2020). Influencing factors for preventing postpartum hemorrhage and early detection of childbearing women at risk in Northern Province of Rwanda: beneficiary and health worker perspectives. BMC Pregnancy and Childbirth, 20(1), 1–14. https://doi.org/10.1186/S12884-020-03389-7/TABLES/1
- Wormer, K. C., Jamil, R. T., & Bryant, S. B. (2022). Acute Postpartum Hemorrhage. StatPearls. https://www.ncbi.nlm.nih.gov/books/NBK499988/
- Nzeribe, E. A., Onyegbule, O. A., Idih, E. E., Anyaeze, C. M., Chukwumam, D., Nzeribe, E. A., Onyegbule, O. A., Idih, E. E., Anyaeze, C. M., & Chukwumam, D. (2019). Assessment of the Accuracy of Estimation of Blood Loss by Health Care Professionals in Federal Medical Centre Assessment Owerri, Nigeria. Open Journal of Obstetrics and Gynecology, 9(1), 83–91. https://doi.org/10.4236/OJOG.2019.91009
- Takang, W. A., Florent, F. Y., Obichemti, E. T., Fukara, O. V., Takang, W. A., Florent, F. Y., Obichemti, E. T., & Fukara, O. V. (2022). Factors Associated with Postpartum Hemorrhage amongst Primigravidae Women; the Case of Two Hospitals within the Bamenda Health District. Open Journal of Obstetrics and Gynecology, 12(8), 793–813. https://doi.org/10.4236/OJOG.2022.128068
- Henry, J., Clarke-Deelder, E., Han, D., Miller, N., Opondo, K., Oguttu, M., Burke, T., Cohen, J. L., & McConnell, M. (2022). A cross-sectional study of health care providers’ knowledge of clinical protocols for postpartum hemorrhage care in Kenya. BMC Pregnancy and Childbirth, 22(1), 1–12. https://doi.org/10.1186/S12884-022-05128-6/TABLES/4
- Taj, M., Brenner, M., Sulaiman, Z., & Pandian, V. (2022). Sepsis protocols to reduce mortality in resource-restricted settings: A systematic review. Intensive and Critical Care Nursing, 72, 103255. https://doi.org/10.1016/J.ICCN.2022.103255
- Puchalski Ritchie, L. M., Khan, S., Moore, J. E., Timmings, C., van Lettow, M., Vogel, J. P., Khan, D. N., Mbaruku, G., Mrisho, M., Mugerwa, K., Uka, S., Gülmezoglu, A. M., & Straus, S. E. (2016). Low- and middle-income countries face many common barriers to the implementation of maternal health evidence products. Journal of Clinical Epidemiology, 76, 229–237. https://doi.org/10.1016/J.JCLINEPI.2016.02.017
- Alves, S. L. (2021). Improvements in Clinician, Organization and Patient Outcomes Make a Compelling Case for Evidence-Based Practice Mentor Development Programs: An Integrative Review. Worldviews on Evidence-Based Nursing, 18(5), 283–289. https://doi.org/10.1111/WVN.12533
- Wilson, G., Larkin, V., Redfern, N., Stewart, J., & Steven, A. (2017). Exploring the relationship between mentoring and doctors’ health and well-being: a narrative review. Journal of the Royal Society of Medicine, 110(5), 188. https://doi.org/10.1177/0141076817700848
- Bazirete, O., Nzayirambaho, M., Umubyeyi, A., Karangwa, I., & Evans, M. (2022). Risk factors for postpartum hemorrhage in the Northern Province of Rwanda: A case-control study. PLoS ONE, 17(2). https://doi.org/10.1371/JOURNAL.PONE.0263731
- Ministry of Health Rwanda. (2018). Maternal Newborn and Child Health Strategic Plan. MOH REPORTS.
- Mukankusi, J. (2020). RAM-ENABEL-BARAME MENTORSHIP PROJECT BASELINE ASSESSMENT NARRATIVE REPORT.
- Atukunda MPH, I. T., & Conecker MPH, G. A. (2017). Effect of a low-dose, high-frequency training approach on stillbirths and early neonatal deaths: a before-and-after study in 12 districts of Uganda. The Lancet Global Health, 5, S12. https://doi.org/10.1016/S2214-109X(17)30119-5.
- (2022). Open. Enabel Belgian Development Agency / Rwanda: New effort in mentorship harmonization to improve healthcare service delivery. Open. Enabel. https://open.enabel.be/en/RWA/2382/1657/u/rwanda-new-effort-in-mentorship-harmonization-to-improve-healthcare-service-delivery.html
- Kim, J., Combs, K., Downs, J., & Tillman, F. I. (2018). Medication adherence: The elephant in the room. ResearchGate; unknown. https://www.researchgate.net/publication/322921419_Medication_adherence_The_elephant_in_the_room
- Manzi, A., Hirschhorn, L. R., Sherr, K., Chirwa, C., Baynes, C., Awoonor-Williams, J. K., Hingora, A., Mboya, D., Exavery, A., Tani, K., Manzi, F., Pemba, S., Phillips, J., Kante, A. M., Ramsey, K., Bawah, A., Nimako, B. A., Kanlisi, N., Jackson, E. F., … Pio, A. (2017). Mentorship and coaching to support strengthening healthcare systems: Lessons learned across the five Population Health Implementation and Training partnership projects in sub-Saharan Africa. BMC Health Services Research, 17(3), 5–16. https://doi.org/10.1186/S12913-017-2656-7/TABLES/5
- Isangula K, Mbekenga C, Mwansisya T, Mwasha L, Kisaka L, Selestine E, Siso D, Rutachunzibwa T, Mrema S, Pallangyo E. Healthcare Providers' Experiences With a Clinical Mentorship Intervention to Improve Reproductive, Maternal and Newborn Care in Mwanza, Tanzania. Front Health Serv. 2022 May 6;2:792909. doi: 10.3389/frhs.2022.792909.
- Yamuragiye, A., Ndayisenga,J., Nkurunziza, A., Bazirete, O.,Uwimana, M. (2023). Benefits of a Mentorship Program on Interprofessional Collaboration in Obstetric and Neonatal Care in Rwanda: A Qualitative Descriptive Case Study. Rwanda Journal of Medicine and Health Sciences Vol. 6 No. 1, March 2023 https://dx.doi.org/10.4314/rjmhs.v6i1.9
- Abdul-Kadir R, McLintock C, Ducloy AS, El-Refaey H, England A, Federici AB, Grotegut CA, Halimeh S, Herman JH, Hofer S, James AH, Kouides PA, Paidas MJ, Peyvandi F, Winikoff R. Evaluation and management of postpartum hemorrhage: consensus from an international expert panel. Transfusion. 2014 Jul;54(7):1756-68. doi: 10.1111/trf.12550.
- Tinna Baldvinsdóttir, Blomberg, M., & Lilliecreutz, C. (2018). Improved clinical management but the not patient outcome in women with postpartum hemorrhage—An observational study of practical obstetric team training. 13(9), e0203806–e0203806. https://doi.org/10.1371/journal.pone.0203806
- Millington, S., Edwards, S., Clark, R. A., Dekker, G. A., & Arstall, M. (2021). The association between guidelines adherence and clinical outcomes during pregnancy in a cohort of women with cardiac co-morbidities. PLoSONE, 16(7). https://doi.org/10.1371/JOURNAL.PONE.0255070
- Sharma DD, Chandresh NR, Javed A, Girgis P, Zeeshan M, Fatima SS, Arab TT, Gopidasan S, Daddala VC, Vaghasiya KV, Soofia A, Mylavarapu M. The Management of Preeclampsia: A Comprehensive Review of Current Practices and Future Directions. Cureus. 2024 Jan 2;16(1):e51512. doi: 10.7759/cureus.
- Wakeman, D., Livingston, M. H., Levatino, E., Juviler, P., Gleason, C., Tesini, B., Wilson, N. A., Pegoli, W., Jr, & Arca, M. J. (2022). Reduction of surgical site infections in pediatric patients with complicated appendicitis: Utilization of antibiotic stewardship principles and quality improvement methodology. Journal of pediatric surgery, 57(1), 63–73. https://doi.org/10.1016/j.jpedsurg.2021.09.031
- McGuirk, B., King, W., Govind, J., Lowry, J., & Bogduk, N. (2015). Safety, efficacy, and cost-effectiveness of evidence-based guidelines for the management of acute low back pain in primary care. Spine, 26(23), 2615–2622. https://doi.org/10.1097/00007632-201512010-00017
- Say, L., Chou, D., Gemmill, A., Tunçalp, Ö., Moller, A. B., Daniels, J., ... & Alkema, L. (2014). Global causes of maternal death: a WHO systematic analysis. The Lancet Global Health, 2(6), e323-e333. DOI: 10.1016/S2214-109X(14)70227-X
- Zhang, J., Troendle, J., Reddy, U. M., Laughon, S. K., Branch, D. W., Burkman, R., ... & Hibbard, J. U. (2010). Contemporary cesarean delivery practice in the United States. American Journal of Obstetrics and Gynecology, 203(4), 326.e1-326.e10. doi: 10.1016/j.ajog.2010.06.058.
- Semrau, K. E. A., Miller, K. A., Lipsitz, S., Fisher-Bowman, J., Karlage, A., Neville, B. A., Krasne, M., Gass, J., Jurczak, A., Singh, V. P., Singh, S., Delaney, M. M., Hirschhorn, L. R., Kodkany, B., Kumar, V., & Gawande, A. A. (2020). Does adherence to evidence-based practices during childbirth prevent perinatal mortality? A post-hoc analysis of 3,274 births in Uttar Pradesh, India. BMJ Global Health, 5(9), e002268. https://doi.org/10.1136/BMJGH-2019-002268
- Shahbazi Sighaldeh, S., Nazari, A., Maasoumi, R., Kazemnejad, A., & Mazari, Z. (2020). Prevalence, related factors and maternal outcomes of primary postpartum hemorrhage in governmental hospitals in Kabul-Afghanistan. BMC Pregnancy and Childbirth, 20(1), 1–9. https://doi.org/10.1186/S12884-020-03123-3/TABLES/6
![]() This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
An assessment of factors associated with full vaccination coverage rate among children aged 12-23 months in Masvingo district; Zimbabwe. A cross-sectional study
Nomore Nyengerai 1, Maxwell Mhlanga 2*
- Department of Public Health, University of Zambia
- Centre of Gender Equity, University of Global Health Equity, Zimbabwe
* Corresponding author: Maxwell Mhlanga., Centre of Gender Equity, University of Global Health Equity. Rwanda. E-mail: mmhlanga@ughe.org
Cite this article
ABSTRACT
Introduction: Immunization is one of the most cost-effective nursing interventions aimed at reducing ill health and premature death among children. Despite tremendous efforts by governments, vaccination coverage remains low, especially in developing countries. Masvingo district is one of the districts with low vaccination coverage in the country.
Objectives: This study sought to assess immunization coverage, identify determinants of vaccination coverage and assess factors associated with low full immunization coverage in Masvingo district, Zimbabwe.
Methods: An analytical cross-sectional study design was conducted between January 2019 and February 2019. Masvingo province was purposively selected due to its low vaccination coverage (60.3%) according to the Zimbabwe Demographic and Health Survey 2015. WHO cluster sampling was used to select households. A total of 354 children and their mothers residing in Masvingo district were recruited for the study. Pre-tested interviewer-administered questionnaires were used to collect data. Bivariate analysis was employed to assess factors associated with low vaccination coverage.
Results: An estimated 89.5% of children aged 12-23 months were fully vaccinated by card or mothers’ recall. Factors significantly associated with full vaccination coverage rates (P<0.001) included birth order, distance to the nearest health facility, waiting time, place of birth, number of Antenatal care visits, possession of a vaccination card, place of residence, mother/caregiver’s highest level of education, household expenditure per month, and overall knowledge of the vaccination schedule. After controlling for all these factors, only household expenditure per month (P=0.001), having a vaccination card (P=0.047), and overall knowledge of the vaccination schedule (P=0.002) were statistically significant predictors of full vaccination coverage rates.
Conclusion: Although full vaccination coverage is improving, it is still below the Global Vaccine Action Plan target. Factors associated with low full vaccination coverage include marital age, marital status, level of education, religion, household expenditure, distance to the health center, waiting time, and Antenatal Care and Post-natal Care care utilization. There is no single factor solely responsible for low vaccination coverage; rather, it is influenced by a combination of multiple factors. Nursing interventions at community level should focus on increasing community mobilization strategies that foster saturation coverage to achieve herd immunity for all vaccine preventable child diseases.
Keywords: Vaccination coverage, utilization, children, cross-sectional study, community mobilization, vaccination hesitancy
INTRODUCTION
In 1974, the World Health Organization (WHO) launched the Expanded Programme on Immunization (EPI) and nurses have played a pivotal role in the success of this programme and in promoting universal health coverage through the primary health care approach. The aim of the EPI was to administer life-saving vaccines to all eligible children across the globe. At that time, only six diseases—pertussis, poliomyelitis, tuberculosis, tetanus, measles, and diphtheria—were targeted [1]. Vaccination is regarded as the most economical child survival intervention, improving children’s quality of life while preventing sickness, disability, and death from vaccine-preventable illnesses [1]. According to UNICEF, each dollar spent on vaccination brings about USD 44 in economic benefits through therapeutic cost savings and productive time loss [2]. Nurses are at the centre of successful child vaccination programmes through as they are the ones who implement the Expanded programme of immunisation at both health facility and community level.
According to WHO, the proportion of children vaccinated against the six vaccine-preventable diseases was around 5% initially. This figure has increased to over 80% during the past four decades [3]. This improvement follows the integration of immunization services into broader public health services by many governments. The Global Vaccine Action Plan (GVAP) was launched in 2012 by WHO and partners, with the primary goal of ensuring equitable access to vaccines, thereby preventing avoidable child illnesses, disability, and death. The coverage level set by GVAP for countries is 90% and above for DTP3 and a minimum of 80% in each district by the year 2020 [3]. WHO highlighted that only 123 countries managed to achieve this target by 2017 [1].
Despite the remarkable increase in global vaccination coverage, it still falls below the target set by GVAP [1]. Due to inequitable distribution of nursing and general health services, including immunization, many children, particularly in developing countries, remain unvaccinated. WHO and UNICEF predict that two in every 20 children are left unvaccinated, while 20% of children do not receive all required vaccine doses. In 2017 alone, around 19.9 million children did not receive all three doses of DTP3 during their first year of life. Additionally, about 33.3% of children under 5 years old die from diseases that could be prevented by vaccines [1].
The government of Zimbabwe, through the Ministry of Health and Childcare, introduced the Zimbabwe Expanded Programme on Immunization (ZEPI) in 1982 [4]. Initially, the government adopted the WHO recommendation of vaccination against only six diseases. As research continued and new vaccines were developed, the government made great strides in incorporating them into routine immunization [4]. In 1999, the Hepatitis B vaccine was introduced, followed by the Pentavalent vaccine (DTP-HB-Hib) in 2008. Haemophilus influenzae was included as part of the Pentavalent vaccine. To combat pneumonia, the Pneumococcal Conjugate Vaccine (PCV) was introduced in 2012, followed by the Rotavirus vaccine in 2014 to fight diarrheal diseases [4]. The second dose of the measles vaccine, including the rubella component, was introduced in 2015. In 2018, the government rolled out the Human Papillomavirus (HPV) vaccine nationwide for girls aged 10 to 14 years following a successful pilot project started in 2014.
In Zimbabwe, children are considered fully vaccinated if they receive the following: BCG at birth or first contact, three doses of oral polio vaccine, three doses of Pentavalent, three doses of PCV, two doses of Rotavirus vaccine, and a single dose of measles [4]. These doses should be administered during the first year of life. The Multiple Indicator Cluster Survey (MICS) of 2014 revealed that only 69.2% of children aged 12 to 23 months were fully vaccinated at the time of the survey, and 5% were unvaccinated [5]. Similarly, the Zimbabwe Demographic and Health Survey (ZDHS) of 2015 found that only 73% of children in the same age group were fully vaccinated, while 9.8% were unvaccinated [6]. Despite differences in survey methodologies, both highlighted inadequacies in meeting the GVAP targets for DTP3 (90%) and measles-rubella (95%). This leaves the country vulnerable to outbreaks of vaccine-preventable diseases. Except for BCG, the Multiple Cluster Survey of 2014, all other vaccine coverages were far below the GVAP target [6].
According to both the Multiple Indicator Cluster Survey and the Demographic Health Survey, Masvingo province had the lowest vaccination coverage in the country, with 78.1% and 60.3% respectively [6]. The 2015 Demographic Health Survey revealed that Masvingo province recorded the highest proportion (20.7%) of unvaccinated children.
In Zimbabwe, children are vaccinated through static and outreach services conducted by community nurses and primary health care nurses. According to the Ministry of Health and Childcare, all primary course vaccines should be administered during the first year of life. BCG is given at birth or the first contact, while the other three sets of vaccines are administered from 6 weeks to 14 weeks at four-week intervals. Thereafter, the measles-rubella vaccine is given at 9 months. Given the vulnerability of children under 2 years to various illnesses, polio and measles vaccines are administered at 18 months to boost their immune systems. Extra doses are typically given during campaigns.
The Global Alliance for Vaccines (Gavi) and partners initiated the EPI programme in 1974 to expand immunization services and prevent avoidable illnesses and deaths in children. From 1974 to 2014, global coverage of EPI services increased from 5% to 80% [3]. Although global coverage shows an increasing trend, it remains below the GVAP targets [1]. Consequently, many children, especially in developing countries, are either unvaccinated or partially vaccinated. WHO and UNICEF of 2018 report that two out of every 20 children are left unvaccinated, while one does not complete all recommended vaccine doses [1]. WHO estimates that approximately 19.9 million children did not receive the DTP3 vaccine, and around 33.3% of children under the age of 5 die from vaccine-preventable illnesses [1].
The government of Zimbabwe identified three diseases (pneumonia, diarrhoea, and measles) as among the top five causes of avoidable and premature death in children under 5 years. This implies that the vaccination programme is a critical child survival activity that can improve children's quality of life [7]. The government and EPI partners provide technical, financial, and coordination support to expand, improve, and intensify the EPI programme. Various initiatives have been implemented to improve immunization coverage, including health worker training, providing vehicles for EPI activities, supplying cold chain equipment, and implementing strategies like Reach Every Child (RED), My Village My Home, and Child Health Days [8]. However, despite these initiatives, vaccination coverage decreased from 90% in 2014 to 87% in 2017 [9]. Masvingo district's coverage has remained persistently low, consistent with findings from MICS of 2014 and DHS of 2015 [5-6]. Although several studies have explored factors linked to low vaccination coverage, none have been conducted specifically in Masvingo district. Given the persistent low immunization coverage in Masvingo district, determining the factors associated with this low performance is critical. The findings will inform health promotion messaging and ultimately generate demand and utilization of immunization services.
Objective: This study sought to assess immunization coverage, identify determinants of vaccination coverage and assess factors associated with low full immunization coverage in Masvingo district, Zimbabwe.
MATERIALS AND METHODS
Study setting and design
This study was carried out in Masvingo district, Zimbabwe. The district is 292 km to the south of Zimbabwe’s capital, Harare and is bordered by Gutu district on the north, Chiredzi district south, Zaka and Chivi districts on the east and west respectively. The latest data based on 2012 census projections showed that its’ population is approximately 224,209 and 7,041 are under-5-year-old children [4].
An analytical cross-sectional study was conducted between January 2019 and February 2019. Masvingo province was purposively selected because she had the lowest (60.3%) vaccination coverage according to ZDHS (2015) [6]. WHO cluster sampling was used for selecting the households.
Study population and sampling
The source population of this study were all children within 12 to 23 months age group with their parents residing in Masvingo district. The study population consisted of 354 children within this age group whose mothers/caregivers were sampled.
Case definition: A Case was any child aged 12 to 23 months residing in Masvingo district full immunised between January 2019 and February 2019 confirmed by a child health card/ mother recall.
Sample Size and Sampling Methodology
Masvingo province has the lowest (60, 3%) vaccination coverage according to ZDHS thus was purposively samples [6]. Also, the province had the highest percentage (20.7%) of unvaccinated children with 12 months to 23 months. Furthermore, the administrative data from 2005-2017 revealed that Masvingo district was one of the persistent low performers in the province.
The sample size required was determined using single proportion population formula with 5% margin of error assumption (D), 95% confidence level (), and the immunization coverage assumed between 60% in Masvingo to 87% in Matabeleland North as per ZDHS 2015. Therefore, we we hypothesized a prevalence p = 73%, so that the hypothesized prevalence is within the range [68%, 78%]. The required sample size for this study was computed as follows:
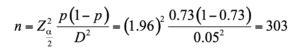
where n = minimum estimate sample size Zα/2 at 95% CI is 1.96; D =margin of error- 5%; hypothesized a prevalence of fully immunized coverage p = 73%. Finally, the sample size was enlarged to 354 mothers to reduce possible statistical biases due data loss.
Sampling was done in accordance to WHO’s multistage cluster sampling [9]. The district was divided into three clusters namely Masvingo South, North and central. Then, fifteen villages were selected from each cluster making a total of 45 villages from all clusters using lottery method. The total sample size was allocated proportionally to villages depending on the number of 12-23 months old children. The first child from each village was selected randomly and the rest of the children were selected from subsequent households until the sample size is fulfilled. In case of two and above eligible children in a household, the investigator will randomly select one child.
Inclusion and Exclusion Criteria
Inclusion Criteria
- All mothers/caregivers aged 16 years and above.
- Mothers/caregivers of children aged 12-23 months residing in Masvingo district for at least 12 months prior to data collection date.
- Adults willing and able to give informed consent to take part.
Exclusion Criteria
- All mothers aged 15 years and below
- All mothers/ caregivers of children below the age of 12 months and those above 23 months.
- Mothers/ caregivers of children residing outside Masvingo district or has been in Masvingo district for a period less than 12 months.
- Mothers/caregivers who were unwilling to participate or incapacitated to give consent.
Data Collection
The survey was conducted in Masvingo district from January to February 2019. The investigator collected information on demography, vaccination status, health services utilisation and other relevant information using interviewer-administered structured questionnaires. The questionnaires were developed from review of immunisation literature, adapted from Zimbabwe Demographic Health Survey and WHO questionnaires for immunisation coverage.
The questionnaire was evaluated for test-retest reliability with 10 people randomly selected at Zaka rural health centre who were from non-participating villages. The test-retest assessments were 5 days apart. Participants were not told that they would be re-tested to minimise bias. Item completion of the questions and percentage agreement between test–retest assessments was calculated for each question and it was in the range of 90-100% for all questions. Based on these results the questionnaire was adopted for use in the study.
Face and construct validity was enhanced through subjecting the questionnaire to review by Experts public health and aligning the research instrument to the conceptual framework that informed behaviour and immunisation services uptake.
The questionnaires were pretested at Gutu Mission Hospital to check for acceptability of the data collection tool, to estimate response rate, questions that are difficult to answer and estimating the length of time to complete the questionnaire so that adjustments were made to the data collection tools. The pretested study area was not included into his study.
Dependent variable
In this study, the vaccination status of the child was the dependent variable. According to Ministry of Health and Child Care ZEPI policy, children are said to be fully vaccinated when given BCG (one dose), Polio, PCV and Pentavalent (three doses each), Rotavirus (two doses) and Measles Rubella (one dose) during the first year of life [6]. In this analysis, fully vaccination status was a dummy variable derived from summing up all the above stated vaccines as per Zimbabwe Expanded Programme on Immunisation schedule. The information on antigens given and dates of administration was extracted from children’s vaccination records or mothers’ recall if records were not available. In cases where vaccination records were absent, the caregiver was asked to report the period and number of doses for each antigen given in order to ascertain the vaccination status of the child. In a bid to minimise recall bias, recalling techniques like period of administration, route and site of administration were included in the instruments.
The vaccination dates were recorded against each antigen from the vaccination card or caregiver’s recall. Vaccination dates were checked against the recommended ZEPI schedule. In cases where the vaccination date was wrongly or not recorded, the antigens were considered as not administered. Children with 12 months to 23 months’ vaccination status were categorised as fully immunised and partially or unvaccinated. The child was considered partially/ incompletely vaccinated when one or more doses were missed. Children who did not receive any antigen were classified as unvaccinated.
Independent variables
The demographic and socio-economic characteristics of the child, mother, health systems, and utilization were the independent variables. These included the sex, age, and birth order of the child; the age, education level, occupation, and marital status of the mother; religion; distance from the health facility; travel time; health facility utilization; place of residence (rural-urban); and communication and knowledge of the immunization schedule.
Data Analysis
In this analysis, SPSS version 20 and STATA 15 were used for capturing, cleaning and tabularisation of all the data collected using questionnaires. The descriptive data was presented in tables as figures as frequencies and percentages. The chi-square test or Fisher’s exact test were performed to evaluate significant differences in proportions or percentages between the two groups. Fisher’s exact test was used where the chi-square test was not appropriate.
Univariate analysis was employed to describe distribution of children’s full vaccination status by characteristics of child, mother and health system and utilisation. Predictors for the vaccinations of the children were assessed by dichotomizing outcome variable (child vaccination status) into fully vaccinated and not fully vaccinated. Predictor variables having a p-value < 0.05 were taken into a multivariable logistic regression analysis to see associations between dependent and independent variables. All independent variables identified to significantly associate with the vaccination statuses of the children at bivariate analysis (p-value < 0.05) were taken into a multivariable analysis. We used the “ENTER” approach for multi-variable regression analysis to assess the association between children’s full vaccination status and factors associated with their vaccination status. Finally, all p-values were always two-sided and all tests with p-value (P) < 0.05 were considered significant.
Ethical Considerations
The investigators obtained ethical approval from the Ethics Committee of the University of Lusaka and the Medical Research Council of Zimbabwe approval number MRCZA/2099, approved on 11 January 2019.
The permission to collect data was sought from Masvingo Provincial Medical Director and Masvingo District Medical Officer respectively.
A written consent was obtained from all participants prior to each interview session.
All the participants were assured that they can withdraw from the process whenever they wanted with no disadvantage to their care.
Privacy and confidentiality were maintained throughout the study process. Measures to ensure confidentiality where clients were told that no information shall be shared to other people and privacy were carried out.
RESULTS
Full vaccination coverage rate in Masvingo district
A total of 354 caregivers and their children participated in this study. The full vaccination rate among children aged 12 to 23 months in Masvingo District was found to be 89.3% (316). The full vaccination coverage rate by vaccination card was 88.1% (312) (Table 1).
| Variable (n=354) | Full immunisation status | No vs Yes
p-value (test) |
|
| No (%) | Yes (%) | ||
| Possession of a vaccination card
No Yes- card not seen Yes- card seen |
10 (26.3) 7 (18.4) 21 (55.3) |
4 (1.3) 5 (1.6) 307 (97.2) |
<0.001* (F) |
| Ever had a vaccination card
Yes No |
26 (68.4) 12 (31.6) |
316 (100.0) 0 (0.0) |
<0.001* (F) |
| *=significant test, F= Fisher’s exact test | |||
Table 1. Presumed factors associated with vaccination coverage rates
Out of 37 caregivers whose children missed one or more vaccines, the majority 15 (28%) cited
religious reasons, long walking distance to the vaccination site 11 (20%), and unavailability of the vaccine 10 (19%) as the major causes of missing the vaccines.
Fear of side effects and inconvenience of vaccination time contributed 11 and 7 percent respectively. Other reasons cited were mobility to neighboring countries in search of greener pastures (15%).
Summary of reasons for missing any vaccines are presented graphical on figure—below.
Figure 1. Reasons for missing any vaccine among 12-23 months age group in Masvingo district
Socio-demographic characteristics of the study participants
Of the 354 children aged 12 to 23 months included in the study, 152 (42.9%) were males and 202 (57.1%) were females. The mean age was 16.6 months (SD = 0.17). Most (66.9%) of the children were of the 1st-2nd birth order, 27.2% (96) were of the 3rd-4th birth order, and 5.9% (21) were of the 5th birth order or higher. The majority, 73.4%, lived in rural areas, while 26.6% resided in urban areas.
The majority of children, both fully immunized and not, were in the 16–20-month age group. Among those not fully immunized, 55.2% were males. About 84% of the children not fully immunized lived in rural areas and were mainly of the 3rd-4th birth order.
The majority of caregivers in both groups were aged 18-24 years and were married: 92.1% in the
not fully immunized group and 94.0% in the fully immunized group. There was a statistically significant association between caregivers' highest level of education and the child's immunization status (p<0.001). Most caregivers in both groups were not employed outside the home.
Regarding household expenditure, the majority of those with not fully immunized children spent
less than 50 USD per month (84.2%), whereas the majority of those with fully immunized children spent 50-500 USD per month. Most children not fully immunized (78.9%) belonged to apostolic religious groups, while the majority of fully immunized children (88.6%) were non-apostolic. There was a statistically significant association between immunization status and religion (P<0.001). Additionally, the majority of caregivers with not fully immunized children were non-professional health workers, compared to 56.6% of caregivers with fully immunized children who were professionals.
Tables 2 and Table 3 below present the socio-demographic characteristics of the study participants by immunization status.
| Variable (n=354) | Full immunisation status | No vs Yes
p-value (test) |
|
| No | Yes | ||
| Child’s age group in months
12 - 15 16 - 20 21 – 23 |
14 (36.8) 15 (39.5) 9 (23.7) |
129 (40.8) 146 (46.2) 41 (12.9) |
0.20 (C) |
| Sex
Male Female |
21(55.2) 17 (44.8) |
131(41.5) 185 (58.5) |
0.10 (C) |
| Residence
Rural Urban |
32 (84.2) 6 (15.8) |
228 (72.2) 88 (27.8) |
0.11 (C) |
| Child’s birth order
1st-2nd 3rd-4th 5th and above |
13 (34.2) 19 (50.0) 6 (15.8) |
224 (70.9) 77 (24.4) 15 (4.7) |
<0.001* (C) |
| Maternal/caregiver age group in years
Less than 18 18 – 24 25 – 40 40+ |
2 (5.3) 21 (55.2) 14 (36.8) 1 (2.6) |
8 (2.5) 179 (56.6) 124 (39.2) 5 (1.6) |
0.79 (F) |
| Marital status
Married Never married |
35 (92.1) 3 (7.9) |
297 (94.0) 19 (6.0) |
0.65 (F) |
| Mothers’ Highest level of education
Primary Secondary Tertiary |
22 (57.9) 16 (42.1) 0 (0.0) |
47 (14.9) 238 (75.3) 31(9.8) |
<0.001* (F) |
| *=significant test; C=chi-square test; F= Fisher’s exact test | |||
Table 2. Socio-demographic characteristics of participants by immunisation status.
| Variable (n=354) | Full immunisation status | No vs Yes
p-value (test) |
|
| No | Yes | ||
| Work outside home
Yes No |
1 (2.6) 37 (97.4) |
53 (16.8) 261(82.6) |
0.021* (C) |
| Household expenditure in USD
Less than $50 $50-500 Above $500 |
32 (84.2) 6 (15.8) 0 (0.0) |
65 (20.6) 243 (76.9) 8 (2.5) |
<0.0001* (F) |
| Religion
Apostolic Non-Apostolic |
30 (78.9) 8 (2.1) |
36 (11.4) 280 (88.6) |
<0.0001* (C) |
| Occupation
Professional Non-professional |
1 (14.3) 6 (85.7) |
30 (56.6) 23 (43.3) |
0.049* (F) |
| *=significant test; C=chi-square test; F= Fisher’s exact test | |||
Table 3. Socio-demographic characteristics of participants by immunisation status
Health services accessibility and utilization
Regarding the distance from the health facility, a greater proportion (55.3%) of children who were
not fully immunized lived more than 10 km from the nearest facility, whereas the majority (58.2%) of those fully immunized lived within 5 km of the nearest clinic. The association between distance from the health facility and immunization status was very significant (P<0.001). The majority of caregivers in both groups perceived that the waiting time at the health facility was too long, and there was a significant association between immunization status and perceived waiting time at the health facility (P<0.001). All children who were fully immunized had caregivers who had attended ANC, and the association between ANC attendance and immunization status was very significant (P<0.001). Mothers who had attended more than four ANC visits were least likely to have their children not fully immunized (P<0.001). The majority (98.1%) of caregivers whose children were fully immunized had delivered at a health institution, and the association between place of birth and immunization status was very significant (P<0.001). Women who had four PNC visits and had a discussion with nurses about vaccination were more likely to have their children vaccinated (P<0.001), (Table 4).
| Variable (n=354) | Full immunisation status | No vs Yes
p-value (test) |
|
| No | Yes | ||
| Distance from health facility
Less than 5km 5- 10km Above 10km |
7 (18.4) 10 (26.3) 21 (55.3) |
184 (58.2) 105 (33.2) 27 (8.5) |
<0.001* (C) |
| Waiting time at facility
Too long Reasonable |
20 (52.6) 18 (47.4) |
296 (93.7) 20 (6.3) |
<0.001*(C) |
| ANC attendance
Yes No |
31(81.6) 7 (18.4) |
316 (100.0) 0 (0.0) |
<0.001* (F) |
| Number of ANC visits
No visit 1-3 visits 4+ visits |
7 (18.4) 24 (63.2) 7 (18.4) |
0 (0.0) 86 (27.2) 230 (72.8) |
<0.001*(F) |
| Place of birth
Health institution Non-Health institution |
25 (65.8) 13 (34.2) |
310 (98.1) 6 (1.9) |
<0.001*(F) |
| Number of PNC visits attended
None Less than 4 4 visits |
7 (18.4) 26 (68.4) 5 (13.2) |
0 (0.0) 51 (16.1) 265 (83.9) |
<0.001*(F) |
| Discussion with nurse about vaccination
Yes N0 |
22 (57.9) 16 (42.1) |
305 (96.5) 11(3.5) |
<0.001*(C) |
| *=significant test; C=chi-square test; F= Fisher’s exact test | |||
Table 4. Summary of health services access and utilisation
Information, communication and knowledge
In relation to information and communication, results showed a statistical significant association between source of health information and immunisation status (P<0.001). The most frequent sources of information mentioned were health workers (79.9%), community leaders (92.9%), radios (42.1%) and Village Health Workers (30.8%). The results of the study revealed that the television and the newspapers were the least frequently used sources of information with 16.4% and 4% respectively. Regarding mothers’/ caregivers’ knowledge of schedule for immunization, the majority, 318 (89.8%) gave the correct timelines for all antigens while 36 (10.2%) had limited or no knowledge. Most of the respondents were well versed with vaccination schedule for BCG (95.4%) and Measles (94.4%). Despite these high knowledge levels, 14 (4%) indicated that they know nothing about the immunization schedule. Children born to mothers with partial knowledge on the vaccination schedule (71.1%) were less likely to be fully immunised whereas those born to fully knowledgeable mothers were more likely to be fully vaccinated (P<0.001) (Table 5).
| Variable (n=354) | Full immunisation status | No vs Yes
p-value (test) |
|
| No | Yes | ||
| Knowledge of vaccination schedule | |||
| OPV
No dose 1-2 doses 3 doses |
10 (26.3) 7 (18.4) 21 (55.3) |
4 (1.3) 5 (1.6) 307 (97.2) |
<0.001 (F) |
| PENTAVALENT
No dose 1-2 doses 3 doses |
10 (26.3) 8 (2.1) 20 (52.6) |
4 (1.3) 5 (1.6) 307 (97.2) |
<0.001* (F) |
| PCV
No dose 1-2 doses 3 doses |
10 (26.3) 11 (28.9) 17 (44.7) |
4 (1.3) 5 (1.6) 307 (97.2) |
<0.001*(F) |
| MEASLES
No dose 2 doses |
10 (26.3) 28 (73.7) |
7 (2.2) 310 (97.8) |
<0.001* (C) |
| Overall Knowledge level
Partial knowledge Full knowledge |
27 (71.1) 11 (28.9) |
9 (2.8) 307 (97.2) |
<0.001* (C) |
| *=significant test; C=chi-square test; F= Fisher’s exact test | |||
Table 5. Knowledge of vaccination schedule
Predictors of full vaccination coverage rate in Masvingo district
The study did a multivariate binary regression analysis to determine the predictors of full vaccination coverage rate in Masvingo district. All factors that had a statistical significant association with immunisation status were controlled for and these included birth order, mothers’ level of education, spouse’s level of education, work outside home, household expenditure per month, religion, having a vaccination card, distance to the clinic, time to reach health facility, waiting time at outreach and overall knowledge level on immunisation schedule. Only household expenditure per month (AOR=18.77, 95% CI = 3.13-11.21), having a vaccination card (AOR=11.78, 95% CI = 1.03-13.41) and overall knowledge on vaccination schedule (AOR=10.01,
95% CI = 2.32-43.25) were statistically significant predictors of full vaccination coverage rates
(Table 6).
| Immunisation status and: | Coefficient | Adjusted Odds ratio (AOR) | AOR CI at 95% | p-value |
| Birth order | 1.15 | 2.14 | 0.58 – 7.84 | 0.25 |
| Mother’s level of education | -0.05 | 0.96 | 0.17 – 5.33 | 0.96 |
| Spouse’s level of education | 1.08 | 2.64 | 0.46 – 15.30 | 0.28 |
| Work outside home | 1.92 | 11.91 | 0.95 – 14.90 | 0.051 |
| HH expenditure per month | 3.21 | 18.77 | 3.13 – 11.21 | 0.001* |
| Religion | 1.66 | 4.92 | 0.75 – 32.47 | 0.098 |
| Having a vaccination card | 1.99 | 11.78 | 1.03 – 13.41 | 0.047* |
| Distance to the clinic | -0.71 | 0.09 | 0.01 – 68.56 | 0.48 |
| Time to reach clinic | 0.82 | 16.06 | 0.02 – 12.56 | 0.41 |
| Waiting time at outreach | 0.86 | 2.46 | 0.32 – 19.04 | 0.39 |
| Overall knowledge on vaccination | 3.09 | 10.01 | 2.32 – 43.25 | 0.002* |
| * =significant test | ||||
Table 6. Predictors of full vaccination coverage rate in Masvingo district.
DISCUSSION
Full vaccination coverage rates
Based on the results of this study, full vaccination coverage by both card and mother’s recall was found to be 89.5%. This coverage is much higher compared to the provincial coverage of 78.1% [5], 65.4% [7], 60.3% [6], and 85% [10]. The finding was also higher than the 64% rate that had been reported in the previous 2011 ZDHS report [11]. These variances may be attributed to different methods used, areas covered, data quality issues, and denominator differences. Children with vaccination cards were more likely to be fully vaccinated (P<0.001).
In line with Meleko’s finding in 2015, this study established that more children (82.6%) with vaccination records/cards were fully vaccinated compared to those without [12]. Similar studies conducted in Ghana, Bangladesh, and India after the peak of the COVID-19 pandemic reported full vaccination coverage rates for children 12-23 months that ranged from 67% to 88% [13-15]. This suggests that vaccination cards, which contain vital information such as milestones and vaccination schedules, act as reminders to parents. Low vaccination among those without cards may be attributed to mothers’/caregivers’ recall bias. Similar to previous studies [7, 12], this study revealed variations in antigens given at the same period, such as OPV 3 and DTP 3. These variations suggest missed opportunities due to stock-outs, poor screening, and data quality issues. Policymakers should ensure and monitor that vaccination cards are distributed freely, reaching even the remotest mother-child pairs to promote high full vaccination coverage rates in Masvingo.
Socio-Demographic Characteristics of the Study Participants
This study assessed the association of full vaccination with the index child's sex, age, birth order, and place of residence. No evidence suggested that the child's sex influenced vaccination status, consistent with findings from ZDHS of 2015, Mukungwa in 2015, and studies in Ethiopia and Indonesia [6-7]. However, birth order was a significant predictor; higher birth orders were associated with lower vaccination rates, as seen in previous studies. This trend may reflect decreased enthusiasm and increased resource competition with higher birth orders.
Place of residence also showed a significant association with full vaccination. Contrary to Mukungwa’s findings, this study found that children in rural areas were more likely to be fully vaccinated than those in urban areas (OR=0.48, 95% CI = 0.01-0.93). This may be due to the increased number of urban poor who cannot afford health services.
Factors significantly associated with full vaccination status included maternal age, marital status, mother's education, spouse's education, household expenditure, and religion. Marital status was a key determinant, with married mothers more likely to fully vaccinate their children (OR=1.33, 95% CI = 1.12-5.56), possibly due to additional resources and support from spouses. Similar studies in low to medium income countries showed the same trends even after the Covid-19 pandemic [13-15].
Education level also positively influenced vaccination rates. Educated mothers are more likely to seek health services, though other factors still play a role. Fathers' education similarly impacted vaccination status, likely due to their ability to make informed health decisions. This aligns with findings by Meleko and others, which reported that children of literate fathers were 2.42 times more likely to be fully vaccinated [12].
Employment type significantly affected vaccination rates. Children of non-professional workers were less likely to be fully vaccinated compared to those of professional health workers. Monthly household expenditure also correlated with vaccination status; children in households spending less than $50 per month were less likely to be fully vaccinated. This underscores the need for community health insurance models to enhance equity in health service access.
Economic status, measured by household expenditure, was another predictor of full vaccination. Wealthier families exhibited better health-seeking behaviors, despite free vaccination services in Zimbabwe, suggesting that indirect costs like transportation influence vaccination decisions.
Religious affiliation also impacted vaccination coverage. The study found that 54.5% of children from apostolic sect families were partially or unvaccinated, compared to 97% from other Christian denominations. Despite efforts to raise health awareness among apostolic sect members, some still prefer faith healing over modern medical interventions, confirming Mukungwa's findings [12].
Health Service Accessibility and Utilization
Distance to the nearest health facility, waiting time, place of delivery, antenatal care (ANC) and postnatal care (PNC) clinic services utilization, and having a vaccination card were found to influence the likelihood of full vaccination. Children born to mothers who walk more than 10 km to a health facility are 13 times less likely to be fully vaccinated than those who walk less than 10 km (OR=13.22, 95% CI = 5.77-17.01). This finding aligns with studies by UNICEF, Mukungwa, and Legesse and Dechasa, which identified long walking distances as a barrier to immunization [7, 16-17].
Contrary to Ayano (2015), this study found no significant association between travel time and full vaccination status [18]. However, mothers who deemed waiting times reasonable were 13 times more likely to fully immunize their children (OR=13.32). This result highlights the importance of reducing wait times, particularly during busy seasons.
Antenatal care utilization strongly correlates with full vaccination status. Mothers who attended at least four ANC visits were more likely to fully vaccinate their children, consistent with studies by Mukungwa, Sunguti et al., and Herliana and Douiri [7,12,19]. The World Health Organization recommends at least four ANC visits, during which mothers receive education on child care and immunization. This study found that 97% of women who attended four or more ANC visits fully vaccinated their children, compared to 73.7% who attended fewer visits.
Place of delivery also significantly influenced full vaccination status. Mothers who gave birth at health facilities were 27 times more likely to vaccinate their children (OR=26.67; 95% CI: 16.74-36.55). This finding aligns with previous studies and highlights the importance of health facility deliveries, where vaccination is initiated before discharge and mothers receive guidance on future vaccinations.
Postnatal care follow-up visits were another strong predictor of full vaccination. This study revealed that 98% of mothers who attended the recommended four PNC visits fully vaccinated their children, compared to 60.7% among those who attended fewer visits. PNC clinics provide opportunities for health professionals to administer due and overdue vaccines and discuss child health issues.
Discussions about vaccination with health professionals during pregnancy significantly influenced full vaccination status. Children of mothers who had such discussions were more likely to be fully vaccinated, consistent with findings by from similar studies [13-15,17]. These discussions positively impact mothers' health-seeking behaviors, leading to increased demand and utilization of
immunization services and higher full vaccination coverage for children aged 12-23 months.
Communication, Information, and Knowledge
Though there was a significant association between the source of information and full vaccination,
the majority (79.9%) of mothers and caregivers received information about immunization from health workers and community leaders. This is likely due to the fact that most (73.4%) study participants were from rural areas where access to electronic and print media was limited. The study revealed a significant association between mothers' and caregivers' knowledge about the vaccination schedule and the full vaccination status of the index child. This result is consistent with previous studies which found that knowledge about vaccination was a significant determinant of the full vaccination status of index children [12,18]. It also aligns with findings by Xeuatvongsa et al., which showed that low full vaccination coverage was mainly due to limited knowledge about immunization [20].
Predictors of full immunisation coverage
After controlling for birth order, mothers’ level of education, spouse’s level of education, work outside the home, household expenditure per month, religion, having a vaccination card, distance to the clinic, time to reach the health facility, waiting time at outreach, and overall knowledge level on the immunisation schedule, only household expenditure per month (AOR=18.77, 95% CI = 3.13–11.21), having a vaccination card (AOR=11.78, 95% CI = 1.03–13.41), and overall knowledge of the vaccination schedule (AOR=10.01, 95% CI = 2.32–43.25) were statistically significant predictors of full vaccination coverage rates. These factors should be fully addressed in the community health strategy to improve full immunisation coverage rates in Masvingo district.
These results are crucial for nursing. Understanding these factors enables nurses to identify barriers
to immunization, which is essential for preventing childhood diseases. Enhanced vaccination
coverage ensures community health, reduces morbidity and mortality rates, and lowers healthcare costs by preventing outbreaks. Moreover, insights from this study can guide nurses in developing targeted interventions, educational campaigns, and policy recommendations to improve vaccination rates, ultimately leading to better health outcomes for children and the broader community. This aligns with nursing's core mission of promoting public health and disease prevention.
Limitations
In the absence of vaccination records, information about the index child’s vaccination status was obtained from the mothers’ or caregivers’ recall. Thus, the accuracy of the information relied on the mothers’ or caregivers’ ability to precisely remember the vaccination period and antigens given to the child. Additionally, the accuracy depended on the mothers’ or caregivers’ honesty. This information is subject to recall bias. This study was a cross-sectional survey and could only assess the association between various risk factors and full vaccination coverage but not causal inferences. Similarly, there are chances that the coverage rates could have changed significantly between the time the study was conducted and now since in between the Covid-19 pandemic struck and pandemics have always been associated with reduction in vaccination coverage rates.
Strength
One person collected the data for this study, eliminating the chances of inter-observer biases. Most of the mothers and caregivers had vaccination cards available, enhancing the accuracy of the data.
CONCLUSION
This study assessed factors linked to low full vaccination coverage among children aged 12-23 months in Masvingo district, finding a coverage rate of 89.5%, higher than previous estimates but still below GVAP targets for some vaccines like measles. Socio-demographic factors such as birth order, place of residence, family and maternal factors, and household expenditure significantly influenced vaccination. Accessibility to health facilities, waiting times, antenatal and postnatal care utilization, and possession of a vaccination card were also crucial. Effective outreach and integrated approaches, including educational programs and promoting maternal and child health activities, are essential to improving vaccination coverage and should be prioritized in nursing strategic planning for effective community mobilization. Health system strengthening measures should also consider strengthening the supply chain for vaccines and effective distribution strategies to improve access to vaccination services. It is crucial that community nursing interventions employ innovative approaches to ensure saturation coverage and easy accessibility of maternal and child services to address barriers to full coverage.
Funding statement
This research did not receive any specific grant from funding agencies in the public, commercial, or not for profit sectors.
Conflict of interest
The authors report no conflict of interest.
Authors’ contribution
Nomore Nyengerai: Development of the original draft; Maxwell Mhlanga: Review of the manuscript, data analysis and discussion.
Acknowledgements
We would want to acknowledge Masvingo Provincial Medical Directorate for allowing us to carry out our research at their institution.
REFERENCES
- WHO and UNICEF. (2018) Progress and Challenges of Achieving Universal Immunisation Coverage, 2017 WHO/UNICEF Estimates of National Immunisation Coverage, Data. Available online: https://www.who.int/teams/immunization-vaccines-and-biologicals/immunization-analysis-and-insights/global-monitoring/immunization-coverage/who-unicef-estimates-of-national-immunization-coverage. Accessed on 19 February 2019- WHO, Geneva.
- (2018) Immunisation Coverage. Available online: http://www.who.int/news-room/fact-sheets/detail/immunization-coverage ( Accessed on 14 October 2019)
- Ministry of Health and Child Care. (2018): Zimbabwe Expanded Programme on Immunisation- revised Policy Document, Ministry of Health and Child Care: Harare. Available on: https://extranet.who.int/countryplanningcycles/sites/default/files/planning_cycle_repository/zimbabwe/zimbabwe_epi_cmyp_2015 - 2019_0.pdf (Accessed on 10 January 2021.
- Ministry of Health and Child Care, (2015). Report on Evaluation of Coverage Achieved during Zimbabwe Measles/Rubella and Vitamin A Catch Up Campaign combined with Assessment of Routine Immunization: Part II Coverage Survey: Routine Immunization, December 2015, MoHCC National Expanded Programme on Immunization: Harare. Available online: https://www.unicef.org/zimbabwe/media/356/file/Factors%20Influencing%20Vaccine%20Hesitancy%20and%20Immunization%20Coverage%20in%20Zimbabwe.pdf. Accessed on 13 October 2018).
- Zimbabwe National Statistical Agency, (2015). Multiple Indicator Cluster Survey 2014, Harare: ZIMSTAT. Available online: https://microdata.worldbank.org/index.php/catalog/2527. Accessed on 13 October 2018).
- ZIMSTAT & ICF International. (2016). Zimbabwe Demographic and Health Survey: Key Indicators, Rockville, Maryland, USA: ZIMSTAT and ICF International. Available online: https://www.dhsprogram.com/pubs/pdf/FR322/FR322.pdf. Accessed on 18 October 2018.
- Mukungwa, T. (2015). Factors Associated with Full Immunization Coverage amongst Children aged 12-23 Months in Zimbabwe, African Population Studies 29(2): 1761-1774. DOI:https://doi.org/10.11564/29-2-745
- Ministry of Health and Child Care. (2014) Zimbabwe Expanded Program on Immunization Comprehensive Multi-Year Plan 2015-2019, Government of Zimbabwe: Harare, p4. Available online: https://www.sida.se/en/publications/expanded-programme-on-immunization-in-zimbabwe. Accessed on 21 October 2018.
- (2015) Vaccination Surveys Cluster Surveys: Reference Manual, Version 3 Working Draft, updated July 2015. Available online: https://www.technet-21.org/en/topics/data/vaccination-coverage-surveys-technical-resources. Access on 15 October 2018.
- Zimbabwe National Statistics Agency. (2012) Zimbabwe Population Census 2012: National Report, ZIMSTAT, Harare. Available online: https://www.dhsprogram.com/pubs/pdf/FR322/FR322.pdf. Accessed on 18 October 2018.
- Kriss JL, Goodson J, Machekanyanga Z, Shibeshi ME, Daniel F, Masresha B, Kaiser R. Vaccine receipt and vaccine card availability among children of the apostolic faith: analysis from the 2010-2011 Zimbabwe demographic and health survey. Pan Afr Med J. 2016 May 11;24:47. DOI: 10.11604/pamj.2016.24.47.8663.
- Meleko, A., Geremew, M. & Birhanu, F. (2017) Assessment of Child Immunization Coverage and Associated Factors with Full Vaccination among Children Aged 12–23 Months at Mizan. DOI: 10.1155/2017/7976587
- Akanpaabadai EA, Adiak AA, Nukpezah RN, Adokiya MN, Adjei SE, Boah M. Population-based cross-sectional study of factors influencing full vaccination status of children aged 12- 23 months in a rural district of the Upper East Region, Ghana. BMC Pediatr. 2024 Mar 8;24(1):168. DOI: 10.1186/s12887-024-04662-w.
- Khanam M, Jahan NA. Determinants of Full Vaccination Coverage among Children Aged 12-23 Months in Bangladesh: A Comparison between High- and Low-Performing Divisions. Int J Pediatr. 2024 May 15;2024:7787593. DOI: 10.1155/2024/7787593.
- Islam T, Mandal S, Chouhan P. Influence of socio-demographic factors on coverage of full vaccination among children aged 12-23 months: a study in Indian context (2015-2016). Hum Vaccin Immunother. 2021 Dec 2;17(12):5226-5234. DOI: 10.1080/21645515.2021.1977056.
- Sunguti, J., Neave, P. & Taylor, S. (2016). Family factors associated with immunization uptake in children aged between twelve and fifty-nine months: a household survey in Kakamega Central district, Western Kenya Healthcare in Low-resource Settings 2016. DOI :10.4081/hls.2016.5447
- Phukan, R., Barman, M. and Mahanta, J. (2008). Factors Associated with Immunization Coverage of Children in Assam, India: Journal of Tropical Pediatrics Vol. 55, No. 4. DOI: 10.1093/tropej/fmn025
- Legesse, E. & Dechasa, W. (2015). An assessment of child immunization coverage and its determinants in Sinana District, Southeast Ethiopia BMC Pediatrics (2015) 15:31. DOI: https://doi.org/10.1186/s12887-015-0345-4
- Ayano, B. (2015) Factors Affecting Fully Immunization Status of Children Aged 12- 23 Months in Hosanna Town, South Ethiopia. J Preg Child Health 2: DOI :10.4172/2376-127X.1000185
- Herliana, P., & Douiri, A. (2017). Determinants of immunisation coverage of children aged 12–59 months in Indonesia: a cross-sectional study. BMJ open, 7(12), https://bmjopen.bmj.com/content/7/12/e015790
- Xeuatvongsa, A., Hachiya, M., Miyano, S., Mizoue, T. and Kitamura, T. (2017) Determination of factors affecting the vaccination status of children aged 12–35 months in Lao People’s Democratic Republic.(Online). DOI: 10.1016/j.heliyon.2017.e00265
- Aman Town, Bench Maji Zone, Southwest Ethiopia Hindawi International Journal of Pediatrics Volume 2017. DOI: https://doi.org/10.1155/2017/7976587
- Gelaye SS, Yenit MK, Baraki AG. Rural Vaccination Coverage Among Children Aged 12-23 Months Was Higher Than the Urban Counterparts: A Comparative Cross-Sectional Study in Pawi District, Ethiopia. Pediatric Health Med Ther. 2021 Mar 19;12:119-127. DOI: 10.2147/PHMT.S299064.
![]() This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Assessment of the Impact of Smart Refrigerators on the Preanalytical Phase to Enhance the Transport and Storage of Blood Samples in Primary Care
Vidal Navarro Ana 1. Férriz Tena Náyades 1. Carreres Giménez María Encarnación 1. Verdu Quirant Trinidad 1. Menchón Simón María de las Nieves 2. Campello García María José 2. Serrano López Juan Francisco 2 and Soler Climent Esther 3*.
- Primary Care. Health Department Elche General Hospital, Elche, Alicante, Spain; FISABIO, Valencia, Spain.
- Clinical analysis laboratory. Health Department Elche General Hospital, Elche, Alicante, Spain; FISABIO, Valencia, Spain.
- Research and Innovation Area. Health Department Elche General Hospital, Elche, Alicante, Spain; FISABIO, Valencia, Spain.
* Corresponding author: Soler Climent, Esther. E-mail: soler_estcli@gva.es
Cite this article
ABSTRACT
Introduction: This study investigates the impact of smart refrigerators on the logistics and management of biological samples, emphasizing the critical phases of transport and storage to enhance the pre-analytical quality of blood samples. Efficient sample management is crucial for ensuring diagnostic accuracy.
Objective: The primary objective is to evaluate the efficiency of smart refrigerators equipped with cloud technology in optimizing the transport and storage of biological samples. The secondary objective is to assess healthcare personnel's perceptions and satisfaction with these technologies.
Method: A longitudinal prospective analysis was conducted to assess both the quantitative incidence of pre-analytical errors and the qualitative perceptions of healthcare personnel regarding these technologies. Samples were collected from six primary care centers within the Elche General Health Department, with one center using smart refrigerators and five using conventional methods. The refrigerators featured GPS, real-time temperature sensors, alert systems for cold chain interruptions, and RFID technology. Training on refrigerator use, systematic data collection on pre-analytical errors, and surveys and semi-structured interviews with healthcare personnel were conducted. Descriptive methods and hypothesis testing, including Z-statistics and logistic regression models, were used for statistical analysis.
Results: The analysis revealed a significant decrease in the incidence of coagulated and hemolyzed samples at the center using smart refrigerators. Specifically, the rate of coagulated samples was reduced by 69.39%, while hemolyzed samples decreased by 78.12%. This improvement contrasts with trends observed in centers using conventional practices. A significant 94.62% of the staff reported a positive experience with the smart refrigerators, highlighting high satisfaction and the importance of stricter control in handling and transporting samples to prevent errors.
Conclusions: The use of smart refrigerators in the transport and storage of biological samples effectively improves the pre-analytical quality of blood samples, reduces pre-analytical errors, and enhances staff satisfaction. These findings underscore the importance of incorporating advanced technologies in the management of biological samples in primary care settings.
Keywords: Pre-Analytical Phase, Smart Refrigerators, Pre-analytical Error, Medical Laboratory, Blood Preservation.
INTRODUCTION
In recent decades, the imperative to reduce costs has driven the healthcare sector towards the consolidation and centralization of diagnostic services in high-capacity laboratories [1]. This transformation underscores the critical importance of efficiently transporting various biological samples from peripheral collection points to centralized analysis centers, highlighting the need for optimized logistics and meticulous sample management to ensure diagnostic accuracy [2]. As emphasized by Giavarina and Lippi, precision is crucial at every stage of the diagnostic process [3]. The ability of clinical laboratories to deliver reliable results depends on the rigorous implementation of standardized procedures throughout the pre-analytical, analytical, and post-analytical phases of the diagnostic process. Studies by Rak-Pasikowska et al. and Carraro et al. highlight frequent errors and the nature of these in the pre-analytical phases, illustrating common challenges and underscoring the importance of addressing them to enhance overall diagnostic quality [4,5]. The pre-analytical phase is particularly complex, involving numerous variables that can significantly impact the quality of analytical results. These variables range from the patient’s physiological conditions to the methodologies used in sample collection, underscoring the necessity for meticulous and standardized management at this crucial stage [6,7]. It is important to recognize that the pre-analytical phase comprises two sub-stages: extralaboratory and intralaboratory, each with its own set of challenges and potential sources of error, which can be difficult to quantify due to the variability in their occurrence [8,9]. Efforts to manage the pre-analytical phase more effectively have been documented extensively. Akande discusses the quality management of the pre-analytical phase, emphasizing monitoring and control to mitigate errors before they affect the test outcomes [10]. Similarly, Lee's work on reducing pre-analytical errors through quality improvement activities in a university hospital setting showcases practical applications of these principles [11]. Cornes reviews the evolution of the pre-analytical phase and projects future advancements that could further reduce errors [12]. Rodríguez-Ravelo and Marcel highlight the broad impact of pre-analytical variables on clinical laboratory results [13]. Lastly, innovations such as the specialized Vacutainer systems play a crucial role in improving sample integrity during collection and transport [14]. Moreover, Lippi et al. highlight that the quality of blood samples, particularly the prevalence of hemolyzed samples, is a frequent cause of specimen nonconformity in clinical laboratories, indicating the urgent need for strategies to improve the quality of blood samples [15]. Tóth et al. demonstrated that hemolysis is a common pre-analytical problem in both newborns and adults, significantly affecting analysis results [9,16]. Bostic et al. reported that their laboratory managed to reduce the number of insufficient samples for coagulation tests by tracking and eliminating expired blood collection tubes, suggesting an effective strategy to minimize this type of pre-analytical error [17]. In another study, Lippi et al. showed how brief venous stasis during extraction can significantly alter the results of coagulation tests, emphasizing the importance of standardizing the venipuncture process [18]. Van Geest-Daalderop et al. evaluated the effect of pre-analytical variables, including the time between blood collection and PT/INR determinations, and found significant effects based on storage conditions and handling, recommending a maximum of 6 hours between blood collection and PT/INR determination [19].
These findings underline the interrelationship between pre-analytical management, diagnostic accuracy, and operational efficiency, stressing the continuous need for quality improvement throughout all phases of the diagnostic process, especially in standardizing pre-analytical procedures. The prevalence of pre-analytical errors varies significantly between different countries, reflecting global variability in sample handling practices and standards [8,13]. Hemolysis, in particular, frequently undermines the accuracy of critical tests such as INR and aPTT [20,21]. Economically, pre-analytical errors, especially those resulting from hemolyzed samples, impose a substantial financial burden on health institutions, significantly affecting hospital budgets [10,22]. Detailed analysis of hemolysis causes reveals a range of factors, from collection techniques to sample transport, highlighting the need for careful and standardized practices to minimize its incidence [23,24].
Proper management of blood sample transport is essential for precise and reliable clinical analyses. Recent studies emphasize how mechanical agitation during the transport of non-centrifuged samples can significantly affect test results, underscoring the importance of selecting transportation methods that preserve sample integrity [25]. The implementation of advanced technologies, such as smart refrigerators, offers a promising solution. These devices integrate cutting-edge temperature and vibration controls essential for maintaining optimal conditions during transport [26]. Their ability to ensure a stable environment and monitor temperature in real-time is a crucial advancement in preventing sample coagulation or degradation. The significance of these findings necessitates specific research to explore the impact of smart refrigerators on the pre-analytical process. Despite the lack of direct evidence evaluating these technologies in specific contexts, it is imperative to investigate their potential to enhance the traceability and control of blood samples, particularly in primary care. This approach could not only mitigate pre-analytical errors but also enhance the quality and reliability of clinical analyses.
OBJECTIVE
Main objective
To evaluate the efficiency and applicability of smart refrigerators integrated with cloud-based systems for the transport of biological samples.
This study primarily investigates the potential of these advanced refrigeration and monitoring systems to improve control over the cold chain and reduce the potential for vibration and impacts from collection to final destination. However, it is acknowledged that due to the lack of comprehensive data and investigation, conclusions regarding their effect on pre-analytical errors are preliminary and largely based on the surrogate endpoint of hemolysis reduction.
Secondary objectives
- To determine health personnel's perception and evaluation of the impact that repeated sample collection has on their routine clinical work.
- To examine satisfaction with the use of smart refrigerators at the end of the study period through interviews with all health professionals involved in the sample handling, transfer, and processing stages.
MATERIAL AND METHODS
Study Design
This study employs a prospective longitudinal design to evaluate the efficiency of smart refrigerators in transporting biological samples from primary care centers to a central laboratory. It utilizes both quantitative and qualitative methods to assess not only the incidence of pre-analytical errors but also the healthcare staff's perception of the need for action and their satisfaction with these technologies.
Population and Sample
The study analyses blood samples collected from six primary care centers within the Elche General Health Department, serving 168,975 people. It compares pre-analytical problems at one center using smart refrigerators to send samples to the central laboratory with five centers that did not use them. Questionnaires were administered to 97 health professionals to assess the impact of repeated sample collection. Additionally, interviews were conducted with all personnel involved in sample handling, transport, and processing to assess satisfaction with the refrigerators.
Materials
Smart refrigerators equipped with GPS tracking, real-time temperature sensors (maintaining 2°C to 8°C), alerts for cold chain interruptions, RFID (Radio Frequency Identification) access control, and anti-vibration systems were used. The use of RFID access control ensures a secure and efficient system for tracking and managing access to the refrigerators, preventing unauthorized entry and maintaining the integrity of the samples by ensuring that only authorized personnel can handle them. This technology enhances traceability and accountability, as every access event is recorded, providing a detailed audit trail that helps in monitoring the handling process and improving overall security and reliability.
Control of Confounding Variables
To ensure internal validity, differences in staff training, transport conditions, and sample collection procedures were meticulously controlled through standardized protocols across all centers. Staff experience, the professional-to-population ratio, and professional rotation were consistent among the centers.
Procedures
The study involved training personnel in the use of smart refrigerators, systematic data collection on pre-analytical incidents, and conducting surveys and semi-structured interviews with health personnel.
Instrument Validation
Questionnaires and interviews underwent a validation process, including expert review and a pilot test, followed by adjustments based on factor analysis and item reliability (Cronbach's Alpha).
Statistical Analysis
Data are presented as number and percentage for categorical variables, and continuous data are expressed as mean ± standard deviation (SD).
Advanced statistical techniques were applied, starting with descriptive analyses to understand the basic characteristics of the data. Hypothesis-testing methods, including the Z statistic for comparing proportions, Odds Ratios (OR) with 95% CI, and logistic regression models, were used to explore the relationship between the use of smart refrigerators and the reduction of pre-analytical errors.
To assess the reliability of the questionnaires administered to healthcare professionals, Cronbach's alpha value was calculated to determine the internal consistency of measurement instruments.
Finally, all tests with p-value< 0.05 were considered significant. Data were analyzed using R software.
Ethics and Research Integrity
All procedures were reviewed and approved by the institutional ethics committee. Informed consent was obtained from all participants, ensuring confidentiality and ethical data handling.
Ethics committee protocol number: PI 89_2022_NIPAP-22. The project received approval on September 6, 2022.
RESULTS
The initial questionnaire, which evaluated perceptions of pre-analytical issues and their frequency, achieved a Cronbach's alpha value of 0.87, indicating high reliability. Similarly, the final questionnaire aimed at assessing satisfaction with the use of smart refrigerators showed a Cronbach's alpha value of 0.91, reflecting excellent internal consistency. These results suggest that both questionnaires were reliable and consistent instruments, validating the methodological robustness of the study and reinforcing confidence in the findings obtained.
The data in Table 1 provide a comprehensive view of healthcare personnel's perceptions regarding the challenges and critical areas in the pre-analytical phase of blood sample analysis.
| Question | Responses |
| How often is repeating the blood analyses of the patients necessary? | Hardly ever: 30.93% (n=30), Sometimes: 54.64% (n=53), Often: 8.25% (n=8), Very often: 3.09% (n=3), Do not know/do not answer: 3.09% (n=3) |
| In your opinion, where do you think lies the biggest source of errors in blood analyses? | Specimen transport: 24.74% (n=24), Specimen preparation and analysis: 14.43% (n=14), Specimen storage conditions: 19.59% (n=19), Specimen collection: 23.71% (n=23), Protocol non-compliance by the patient: 11.34% (n=11), Do not know/do not answer: 6.19% (n=6) |
| Which measures do you think should be taken in order to avoid errors in blood analyses? | Considering the patients: 16.49% (n=16), Considering the staff: 20.62% (n=20), Considering the training: 23.71% (n=23), Considering monetary resources: 3.09% (n=3), Considering the available material resources: 29.90% (n=29), Do not know/do not answer: 6.19% (n=6) |
| How would you rate the current storage and transport of specimens system of the primary care centre? | Bad: 3.09% (n=3), Fair: 16.49% (n=16), Good: 55.67% (n=54), Excellent: 8.25% (n=8), Do not know/do not answer: 16.49% (n=16) |
| Do you think a higher control of the influential variables in transport and storage of the specimens would have a positive influence for avoiding errors? | Yes: 84.54% (n=82), No: 8.25% (n=8), Do not know/do not answer: 7.22% (n=7) |
Table 1. Percentage of answers in relation to experiences and perception of the healthcare staff.
According to Table 1, a significant majority of respondents (54.64%) reported that it is "sometimes" necessary to repeat blood tests due to errors, highlighting the frequency of pre-analytical issues encountered in their daily routine.
When asked about the primary source of errors in blood tests, respondents identified several key areas: sample transportation (24.74%, n=24), sample collection (23.71%, n=23), and storage conditions (19.59%, n=19). These areas were highlighted as the most critical points where errors occur, emphasizing the need for specific interventions. Regarding measures to prevent errors in blood tests, the responses varied. The most frequently suggested measures included considering the available material resources (29.90%, n=29) and focusing on staff training (23.71%, n=23). Other important areas included addressing patient-related factors (16.49%, n=16) and considering healthcare personnel (20.62%, n=20).
When rating the current storage and transportation systems in their primary care centers, most respondents rated them as "Good" (55.67%, n=54) while 16.49% (n=16) rated them as "Fair" and 8.25% (n=8) as "Excellent." However, a notable 16.49% (n=16) were unsure or did not respond. Finally, when asked if increased control over variables affecting the transportation and storage of samples would positively impact error reduction, a large majority (84.54%, n=82) believed it would. This consensus underscores the importance of strict controls in these areas to improve the accuracy and reliability of blood tests.
| Question | Domain
Likert scale |
Mean ± SD |
| How would you rate the impact that, in your view, the repetition of specimens collection has on the patients' lives? | Impact
1 to 10 (1 = no impact; 10 = highest impact) |
7.05 ± 0.65 |
| How would you rate the impact that, in your view, the repetition of specimens collection has on the primary care centre? | 7.52 ± 0.41 | |
| How would you rate the efficiency of work performed in the pre-analytical phase of the specimens in this primary care centre? | Efficiency
1 to 10 (1 = poor; 10 = excellent) |
7.69 ± 0.61 |
| Do you think that the Collection Phase needs more urgent attention in order to improve the efficiency in the pre-analytical phase of the specimens in this primary care centre? | Priority
1 to 5 (1 = lowest; 5 = highest) |
3.82 ± 0.41 |
| Do you think that the Storage Phase needs more urgent attention in order to improve the efficiency in the pre-analytical phase of the specimens in this primary care centre? | 4.20 ± 0.41 | |
| Do you think that the Transport Phase needs more urgent attention in order to improve the efficiency in the pre-analytical phase of the specimens in this primary care centre? | 4.25 ± 0.55 | |
| Do you think that the Handling Phase needs more urgent attention in order to improve the efficiency in the pre-analytical phase of the specimens in this primary care centre? | 4.48 ± 0.5 |
Table 2. Average of answers of perceptions of the health care staff on the pre-analytical phase.
The perceived need for repetition significantly impacts both patients' lives and the functioning of the health center, with mean scores of 7.05 ± 0.65 and 7.52 ± 0.41 respectively. The assessments also highlight handling and transportation as critical pre-analytical sub-stages requiring immediate attention, with urgency scores of 4.48 ± 0.5 and 4.25 ± 0.55 respectively. Given the multicentric nature of the study, a multilevel analysis was essential to adjust for variability between centers, providing more accurate estimates of the impact of smart fridges. Sensitivity analyses were also conducted to assess the robustness of the findings against different methodological assumptions, such as various inclusion/exclusion criteria and data handling methods for missing data.
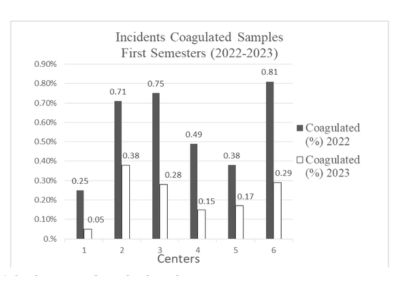
Figure 1. Incidence rates of coagulated samples.
This figure represents the incidences of coagulated samples relative to the total number of samples received. Centers using conventional refrigerators experienced reductions in the incidence of coagulated samples by 80.0%, 46.48%, and 34.67% in Centers 1, 2, and 3 respectively. In contrast, Center 4, which was equipped with smart technology, achieved a significant reduction from 0.49% to 0.15%, translating to a 69.39% decrease. To quantify these effects more precisely, logistic regression models were applied, adjusting for multiple covariates such as technology usage, center size, and staff training hours. The analysis revealed that the use of smart refrigerators is significantly associated with a reduction in the need to repeat tests (p < 0.001), as shown in Table 3.
The logistic regression analysis based on the adjusted dummy data shows that both the use of smart refrigerators and staff training hours have a significant impact on reducing the need to repeat blood tests. Larger centers tend to have a higher likelihood of pre-analytical errors, suggesting the need for specific strategies to address logistical and operational challenges in these settings. Implementing advanced technologies and investing in staff training are presented as effective measures to improve accuracy and efficiency in the pre-analytical phase of blood tests.
| Variable | Coefficient | OR (95% CI) | p-value |
| Intercept | 0.5 (0.1, 0.9) | 1.65 (1.10, 2.46) | 0,02* |
| Center Size | 0.01 (0.005, 0.015) | 1.01 (1.005, 1.015) | 0,04* |
| Training Hours | -0.02 (-0.03, -0.01) | 0.98 (0.97, 0.99) | 0,01* |
| Use of Smart Fridges | -0.5 (-0.75, -0.25) | 0.61 (0.47, 0.78) | <0.0001* |
| * = significant test | |||
Table 3. Logistic regression analysis on the need to repeat tests
The model’s constant has a coefficient of 0.50, indicating the baseline probability of repeating tests when all other variables are zero. The 95% confidence interval for this coefficient ranges from 0.10 to 0.90, with a p-value of 0.02. These results suggest that the constant is significantly different from zero, implying that there is an inherent probability of test repetition even in the absence of other factors. Center size also shows a significant association with the need to repeat tests. The coefficient for this variable is 0.01, with a 95% confidence interval ranging from 0.005 to 0.015 and a p-value of 0.04. A positive coefficient indicates that a larger center size is associated with a higher probability of needing to repeat tests. This may be due to the additional logistical challenges and greater operational complexity faced by larger centers. On the other hand, staff training hours are inversely related to the need to repeat tests. The coefficient for this variable is -0.02, with a 95% confidence interval ranging from -0.03 to -0.01 and a p-value of 0.01. This result indicates that more training hours are associated with a lower probability of needing to repeat tests, underscoring the importance of continuous staff training to improve accuracy and efficiency in the pre-analytical phase. The use of smart refrigerators is significantly associated with a reduction in the need to repeat tests, with a coefficient of -0.50. The 95% confidence interval for this variable ranges from -0.75 to -0.25, and the p-value is 0.0001. This negative coefficient suggests that the implementation of advanced technologies such as smart refrigerators improves pre-analytical efficiency and reduces errors, validating the effectiveness of this technology.
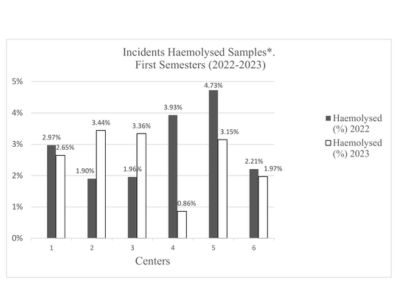
Figure 2. Incidence rates of hemolyzed samples.
Figure 2 represents the incidences of hemolyzed samples in relation to the total number of samples received. Centers 1, 5, and 6 experienced reductions of 10.77%, 33.40%, and 10.86%, respectively. Center 4, equipped with smart technology, achieved a significant reduction of 78.12%, (10.77% vs 78.12%, Z=14.20, p<0.001).
Figure 3 shows the incidences of hemolyzed samples in relation to the total number of samples received.
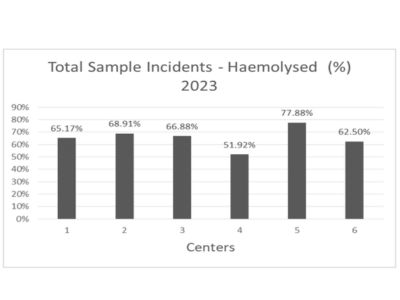
Figure 3. Incidence rates of hemolyzed samples over the total incidences.
Further analysis of the incidence relative to all samples from the first half of 2023, as shown in Figures 2 and 3, continues to demonstrate Center 4’s superior performance with lower rates of both coagulated (2.21%) and hemolyzed (51.92%) samples compared to other centers. These results underscore the effectiveness of smart refrigerators in reducing pre-analytical errors and improving the overall operational efficiency of diagnostic processes in health centers.
Healthcare Staff Satisfaction - Regarding the secondary objective focused on healthcare staff satisfaction with smart refrigerators, the data reveal a notably favorable perception. Although only 79.41% of the surveyed healthcare workers had direct experience with the smart refrigerators, the majority of these professionals reported very positive experiences (63.85%), with an additional 30.77% rating it positively. Significantly, no participants reported a negative perception, with the remaining percentage abstaining from making an assessment.
Refrigerator Quality Assessment - The overall quality of the refrigerators was highly rated, with an average score of 8.67 out of 10. These results highlight the acceptance and satisfaction with the technological innovations applied to the transportation of biological samples, promising not only to reduce pre-analytical errors but also to improve the overall operational efficiency of diagnostic
processes in health centers.
DISCUSSION
This study explores the incidence of pre-analytical errors during the transportation phase of biological samples, focusing on the use of smart refrigerators. Compared to centers without this technology, Center 4 demonstrated significant reductions in the rates of coagulated (69.39%) and hemolyzed samples (51.92%). These findings align with previous research emphasizing the need to optimize the pre-analytical phase to ensure diagnostic quality and patient safety [27]. The efficacy of smart refrigerators in mitigating pre-analytical errors is also supported by other studies highlighting the importance of proper sample management in mass spectrometry-based metabolomics studies [28]. The significant reduction in hemolyzed samples underscores the value of environmental control technologies in maintaining sample integrity during transportation. This is consistent with the findings of Lippi et al. [5], who indicate that proper management in the pre-analytical phase is crucial to minimize errors that affect laboratory results. Additionally, Alcantara et al. [30] discuss how pre-analytical errors, such as hemolysis, significantly contribute to variability in laboratory results, impacting diagnostic accuracy and reliability, thus reinforcing the need for technological interventions. In contrast, studies by Cornes [12] and Lee [11] address the improvement of pre-analytical errors in laboratories without advanced technologies.
However, it is important to acknowledge the primary investigational weakness of this study: the reliance on a single surrogate endpoint, the reduction in hemolyzed samples, to assess the effectiveness of the new system for sample transportation. While this endpoint showed significant improvement, the other chosen surrogate endpoint, the reduction in coagulated samples, did not demonstrate similar statistical significance, limiting the comprehensiveness of the study's findings. Further, despite efforts to gather more comprehensive data, conclusions regarding the impact on other pre-analytical errors remain preliminary. The value of the Z statistic used in this study confirms the significance of reductions in hemolyzed samples and, as suggested by West et al. [31], indicates the need for more refined methodologies to capture and analyze pre-analytical data, which could enhance assessments of the impact of smart refrigerators. The internal consistency of the questionnaires administered to healthcare professionals, measured by Cronbach's alpha, demonstrated high reliability, with values of 0.87 and 0.91 for the initial and final questionnaires, respectively. These results suggest that both questionnaires were reliable and consistent instruments, validating the study's methodological robustness and reinforcing confidence in the findings obtained.
Regarding healthcare professionals’ perceptions of the challenges and critical areas in the pre-analytical phase of blood sample analysis, the majority of respondents (54.64%) indicated that it is “sometimes” necessary to repeat blood tests due to errors, highlighting the frequency of pre-analytical problems in their daily routine. The main sources of errors identified were sample transportation (24.74%), sample collection (23.71%), and storage conditions (19.59%). These areas were highlighted as the most critical points where errors occur, emphasizing the need for specific interventions [32]. Measures suggested to prevent errors in blood analysis included consideration of available material resources (29.90%) and staff training (23.71%), highlighting the importance of these factors in improving the accuracy and reliability of analyses [10]. When evaluating the current system of sample storage and transportation, the majority of respondents rated it as “Good” (55.67%), while 16.49% rated it as “Fair” and 8.25% as “Excellent”. Additionally, a notable proportion (16.49%) was unsure or did not respond. Most respondents (84.54%) believed that greater control of variables influencing sample transportation and storage would positively impact error reduction, underscoring the importance of strict controls in these areas to improve the accuracy and reliability of blood analyses [12]. The perceived need for test repetition significantly impacts both patients' lives and the health center's operations, with average scores of 7.049 and 7.516, respectively. Evaluations also highlight handling and transportation as critical pre-analytical sub-phases requiring immediate attention, with urgency scores of 4.48 and 4.25, respectively.
Given the multicenter nature of the study, a multilevel analysis was conducted to adjust for variability between centers, providing more accurate estimates of the impact of smart refrigerators. Sensitivity analyses were also performed to assess the robustness of findings against different methodological assumptions, such as various inclusion/exclusion criteria and methods of handling missing data [31].
The incidence rates of coagulated samples significantly decreased in centers using conventional refrigerators, with reductions of 80.00%, 46.48%, and 34.67% in Centers 1, 2, and 3, respectively. In contrast, Center 4, equipped with smart technology, achieved a significant reduction from 0.49% to 0.15%, representing a 69.39% decrease. To quantify these effects more precisely, logistic regression models were applied, adjusting for multiple covariates such as technology use, center size, and staff training hours. The analysis revealed that the use of smart refrigerators is significantly associated with a reduction in the need for repeat tests (p < 0.001). The logistic regression model based on adjusted data shows that both the use of smart refrigerators and staff training hours significantly impact the reduction of repeat blood test needs. Larger centers tend to have a higher likelihood of pre-analytical errors, suggesting the need for specific strategies to address logistical and operational challenges in these environments. Implementing advanced technologies and investing in staff training emerge as effective measures to improve accuracy and efficiency in the pre-analytical phase of blood analysis [10].
Regarding healthcare staff satisfaction with smart refrigerators, the data reveals a notably favorable perception. Although only 79.41% of surveyed healthcare workers had direct experience with smart refrigerators, most of these professionals reported very positive experiences (63.85%), with an additional 30.77% rating them positively. Significantly, no participant reported a negative perception, with the remaining percentage abstaining from evaluation. The overall quality of the refrigerators was highly valued, with an average score of 8.67 out of 10. These results highlight the acceptance and satisfaction with technological innovations applied to the transportation of biological samples, promising not only to reduce pre-analytical errors but also to improve the overall operational efficiency of diagnostic processes in health centers [27].
CONCLUSION
This study confirms that the implementation of smart refrigerators significantly reduces the incidence of pre-analytical errors, particularly hemolyzed samples, during the transportation phase of biological samples. The results align with prior research emphasizing the importance of optimizing the pre-analytical phase to ensure diagnostic quality and patient safety [27]. Smart refrigerators proved effective in mitigating errors by maintaining environmental control, as evidenced by significant reductions in hemolyzed samples [28].
The internal consistency of the administered questionnaires, with high Cronbach's alpha values, validates the reliability of the instruments used to gather data on pre-analytical issues and healthcare staff satisfaction. The consistent responses highlight the robustness of the study's methodology and reinforce confidence in the findings obtained.
Healthcare professionals identified transportation, collection, and storage conditions as the primary sources of pre-analytical errors. These insights underscore the need for targeted interventions in these areas. Suggested measures to prevent errors included improving material resources and enhancing staff training, emphasizing the critical role these factors play in ensuring the accuracy and reliability of blood analyses [10].
The logistic regression analysis demonstrated that both the use of smart refrigerators and increased staff training significantly reduce the need for repeat tests, particularly in larger centers where logistical challenges are more pronounced [10]. The study also revealed a notably favorable perception among healthcare staff regarding the effectiveness of smart refrigerators, with high satisfaction scores further validating their utility [27].
LIMITATIONS
This study on the efficacy of smart refrigerators in mitigating preanalytical errors during the transport and storage of biological samples identifies several key limitations that must be considered: Monitoring Period: The study was conducted from January to July 2023, excluding the hotter months of August and September. The absence of these months may overlook how extreme temperatures could affect the performance of smart refrigerators in maintaining sample integrity. This limits the ability to generalize the results to more adverse climatic conditions, which could have a significant impact on preanalytical errors. Generalizability of Results: The research was limited to a small number of primary care centers within the Elche Health Department. While the results are encouraging, their applicability to other settings with different logistical infrastructures and climates may vary, suggesting caution in broader extrapolation of these findings.
Variability in Implementation and Use: There is inherent variability in how technology is adopted and used across different centers. Assumptions of uniform training and homogeneous management of technology might not hold universally, potentially affecting the replicability of the results. Variability in staff training and operational procedures may introduce differences in the effectiveness of smart refrigerators.
Subjective Data: Much of the qualitative data derives from self-reported questionnaires and interviews, which are susceptible to biases such as the social desirability effect. This could influence the accuracy of reported perceptions regarding preanalytical issues and satisfaction with smart refrigerators. These data should be interpreted cautiously and considered complementary to the quantitative findings.
Confounding Variables: Despite rigorous protocols to control confounding factors, there are uncontrolled variables, such as equipment maintenance or workflow variations, that could influence the outcomes. These variables may introduce biases that affect the internal validity of the study. It is crucial to acknowledge these limitations and consider their potential impact on the findings.
These limitations, while noteworthy, do not diminish the value of the findings but highlight areas for future research to refine and validate the benefits of the technology in diverse settings. Future studies should include longer and more varied monitoring periods, a broader diversity of study centers, and a more thorough evaluation of the implementation and use of technology practices to ensure the generalizability and robustness of the results.
Funding statement
This research did not receive any specific grant from funding agencies in the public, commercial, or not for profit sectors.
Authors’ contribution
Collective authorship responds to a joint contribution in all section.
Conflict of interest
The authors report no conflict of interest.
REFERENCES
- Cakirca G. The evaluation of error types and turnaround time of preanalytical phase in biochemistry and hematology laboratories. Iran J Pathol. 2018;13(2):173–8. doi: 10.30699/IJP.13.2.173.
- Fraga OR, Segarra XN, Ortega AG, Cantalejo FR, Rioja RG, Queral LA, et al. Preanalytical recommendations for the measurement of acid-base balance and blood gases. Rev Lab Clin. 2019;12(4):e66-e74. doi: 10.1016/J.LABCLI.2018.12.001.
- Giavarina D, Lippi G. Blood venous sample collection: Recommendations overview and a checklist to improve quality. Clin Biochem. 2017;50(10-11):568-573. doi: 10.1016/j.clinbiochem.2017.02.021.
- Rak-Pasikowska A, Goniwiecha D, Bil-Lula I. Analysis of preanalytical phase errors in a medical diagnostic laboratory. Diagnostyka Laboratoryjna. 2019. doi: 10.5604/01.3001.0013.7440.
- Carraro P, Zago T, Plebani M. Exploring the initial steps of the testing process: frequency and nature of pre-preanalytic errors. Clin Chem. 2012;58(3):638-42. doi: 10.1373/clinchem.2011.175711.
- Lippi G, Betsou F, Cadamuro J, Cornes M, Fleischhacker M, Fruekilde P, et al. Preanalytical challenges - time for solutions. Clin Chem Lab Med. 2019;57(7):974–81. doi: 10.1515/cclm-2018-1334.
- Gosselin RC, Marlar RA. Preanalytical variables in coagulation testing: setting the stage for accurate results. Semin Thromb Hemost. 2019;45(5):433-448. doi: 10.1055/s-0039-1692700.
- Stankovic AK, DiLauri E. Quality improvements in the preanalytical phase: focus on urine specimen workflow. Clin Lab Med. 2008;28(2):339–50, viii. doi: 10.1016/j.cll.2007.12.011.
- Tóth J, Oláh AV, Petercsák T, Kovács T, Kappelmayer J. Detection of haemolysis, a frequent preanalytical problem in the serum of newborns and adults. EJIFCC. 2020;31(1):6–14. PMID: 32256284 PMCID: PMC7109500.
- Akande T. Quality Management of the Pre-Analytical Phase of Total Laboratory Testing Process: Monitoring and Control. Curr J Appl Sci Technol. 2018. doi: 10.9734/CJAST/2018/43874.
- Lee NY. Reduction of pre-analytical errors in the clinical laboratory at the University Hospital of Korea through quality improvement activities. Clin Biochem. 2019;70:24–29. doi: 10.1016/j.clinbiochem.2019.05.016.
- Cornes M. The preanalytical phase–Past, present and future. Ann Clin Biochem. 2020;57(1):4-6. doi: 10.1177/0004563219867989.
- Rodríguez-Ravelo MA, Marcel EA. Preanalytical variables and their influence on clinical laboratory results. Rev Mex Patol Clin. 2007;54(4):159-167. Available from: [https://www.medigraphic.com/pdfs/patol/pt2007/pt074c.pdf](https://www.medigraphic.com/pdfs/patol/pt-2007/pt074c.pdf).
- Vacutainer. CPT™ Cell Preparation Tube with Sodium Heparin For the Separation of Mononuclear Cells from Whole Blood Sterile Interior 8 mL Draw Capacity [16 x 125mm tube Size] For In Vitro Diagnostic Use. 2011. Available from: [https://www.bdbiosciences.com/content/dam/bdb/marketingdocuments/PI_CPT_heparin_March_2016_VDP4010507_web_500010323.pdf](https://www.bdbiosciences.com/content/dam/bdb/marketingdocuments/PI_CPT_heparin_March_2016_VDP4010507_web_500010323.pdf).
- Lippi G, von Meyer A, Cadamuro J, Simundic AM. Blood sample quality. Diagnosis. 2019;6(1):25–31. doi: 10.1515/dx-2018-0018.
- Tian G, Wu Y, Jin X, Zeng Z, Gu X, Li T, et al. The incidence rate and influence factors of hemolysis, lipemia, icterus in fasting serum biochemistry specimens. PLoS One. 2022;17(1):e0262748. doi: 10.1371/journal.pone.0262748.
- Bostic G, Thompson R, Atanasoski S, Canlas C, Hong Y, Kolins M, et al. Quality Improvement in the Coagulation Laboratory: Reducing the Number of Insufficient Blood Draw Specimens for Coagulation Testing. Lab Med. 2015;46(4):347–35. doi: 10.1309
- Lippi G, Salvagno GL, Montagnana M, Guidi GC. Short-term venous stasis influences routine coagulation testing. Blood Coagul Fibrinolysis. 2005;16(6):453-458. doi: 10.1097/01.mbc.0000178828.59866.03.
- Geest-Daalderop J, Mulder A, Winter L, Hoekstra M, Besselaar A. Preanalytical variables and off-site blood collection: influences on the results of the prothrombin time/international normalized ratio test and implications for monitoring of oral anticoagulant therapy. Clin Chem. 2005;51(3):561-8. doi: 10.1373/clinchem.2004.043174.
- Gosselin RC. Review of coagulation preanalytical variables with update on the effect of direct oral anticoagulants. Int J Lab Hematol. 2021;43:109-116. doi: 10.1111/ijlh.13585.
- Plebani M. Quality in laboratory medicine: 50 years on. Clin Biochem. 2016;50(3):101-104. doi: 10.1016/j.clinbiochem.2016.10.007.
- Plebani M. Errors in clinical laboratories or errors in laboratory medicine? Clin Chem Lab Med. 2006;44(6):750–759. doi: 10.1515/CCLM.2006.123.
- Senes M, Bercik Inal B, Benli Aksungar F, Cinaroglu I, Eker P, Sonmez C, Yucel D. TBS preanalytical phase working group survey study–preanalytical phase in coagulation laboratories. Turk J Biochem. 2021;46(1):13-21. doi: 10.1515/tjb-2019-0512.
- Patel S, Nanda R, Sahoo S, Mohapatra E. Congruity in Quality Indicators and Laboratory Performance. Indian J Clin Biochem. 2018;33(3):341-347. doi: 10.1007/s12291-017-0687-9.
- Wallin O, Söderberg J, Grankvist K, Jonsson P, Hultdin J. Preanalytical effects of pneumatic tube transport on routine haematology, coagulation parameters, platelet function and global coagulation. Clin Chem Lab Med. 2008;46(10):1443-9. doi: 10.1515/CCLM.2008.288.
- Kim SJ, Yoo S, Kim HO, Bae H, Park J, Seo KJ, Chang B. Smart Blood Bag Management System in a Hospital Environment. 2006. doi: 10.1007/11872153_44.
- Lippi G, Banfi G, Church S, Cornes M, De Carli G, Grankvist K, Kristensen GB, Ibarz M, Panteghini M, Plebani M, Nybo M, Smellie S, Zaninotto M, Simundic AM. Preanalytical quality improvement: In pursuit of harmony, on behalf of European Federation for Clinical Chemistry and Laboratory Medicine (EFLM) Working group for Preanalytical Phase (WG-PRE). Clin Chem Lab Med. 2015;53(3):357–370. doi: 10.1515/cclm-2014-1051.
- Chaudhry AS, Inata Y, Nakagami-Yamaguchi E. Quality analysis of the clinical laboratory literature and its effectiveness on clinical quality improvement: a systematic review. J Clin Biochem Nutr. 2023;73(2):108–115. doi: 10.3164/jcbn.23-22.
- Ren J, Zhang A, Kong L, Wang X. Advances in mass spectrometry-based metabolomics for investigation of metabolites. RSC Adv. 2018;8:22335-22350. doi: 10.1039/c8ra01574k.
- Alcantara J, et al. Analysis of preanalytical errors in a clinical chemistry laboratory: a 2-year study. Medicine. 2022;101(1):e29853. doi: 10.1097/MD.0000000000029853.
- West J, et al. Preanalytical errors in medical laboratories: a review of the available methodologies of data collection and analysis. Ann Clin Biochem. 2017;54(1):14-19. doi: 10.1177/0004563216669384.
- Peck Palmer OM, Dasgupta A. Review of the Preanalytical Errors That Impact Therapeutic Drug Monitoring. Ther Drug Monit. 2021;43(6):595-608. doi: 10.1097/FTD.0000000000000901.
![]() This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Assessment of the Impact of the Job Satisfaction on Anxiety Level among Hospital Nurses in Lebanon: A Cross-Sectional Study
Mohammad Kobeissi 1, Fatima Bahja 1, Hayat Al Akoum 1,2
1 Lebanese University, Faculty of Public Health, hospital and risk management master program, Lebanon.
2 Jinan University, Faculty of Public Health, Lebanon.
*Corresponding author: Mohammad Kobeissi: Lebanese University, Faculty of Public Health, hospital and risk management master program, Lebanon.
Email: Koubeissimohammad1@gmail.com
Cite this article
ABSTRACT
Introduction: During the past 4 years Lebanon suffered from a major economic crisis and a health care system crisis after COVID pandemic. Nurses as a part of the healthcare system, had to deal with the impact of both crisis and the consequences.
"In this study, job satisfaction and anxiety levels of nurses from 4 Lebanese public and private hospitals were assessed. Correlations of the job satisfaction and anxiety levels among them and with sociodemographic, professional and socio-economic ones, were evaluated.
Objectives: This study helps to determine the prevalence of the psychological distress and its association with the job satisfaction among hospital nurses during economic crisis in South and Beirut hospitals.
Materials and Methods: It is a cross-sectional study that aims to identify a cause-effect relation between hospital nurses Job satisfaction, level of anxiety and different sociodemographic and professional characteristics. The study was done through an online questionnaire including: an introduction to the study, an agreement of participation, the sociodemographic and professional information of the participants, the Generalized Anxiety Disorder Assessment (GAD-7) rating scale and the Nursing Workplace Satisfaction Questionnaire “NWSQ”.
Results: Findings confirmed a significant relationship among salary decreasing due to economic crisis and job dissatisfaction (Spearman’s rho = 0.157; p-value =0.009); and significant relationship between lower levels of job satisfaction and higher anxiety levels of Lebanese hospital nurses (Spearman’s rho = 0.367; p-value <0.0001). Additionally, further correlations among sociodemographic and professional variables had explored.
Conclusion: The study shows the correlation between the decreased nurses job satisfaction with the increased level of anxiety among nurses in Beirut and South of Lebanon hospitals, a negative correlation between salaries during the economic crisis in parallel with the average spending per month and the total job satisfaction, and a positive correlation between the job satisfaction and the anxiety levels. Also, both anxiety level and job satisfaction among nurses were subjective to the hospital locations and categories, the sociodemographic and professional characteristics and the economic crisis which has a significant impact on the nursing physiological status.
Keywords: job satisfaction, anxiety, public hospitals, private hospitals, nurses, economic crisis.
INTRODUCTION
Job satisfaction refers to one's general emotional response towards his/her job resulting from their own appraisal or job experience and includes various dimensions and factors. Job satisfaction is also defined as one's tendency or positive feelings toward one's job. The Job satisfaction and work environment are of great importance, job satisfaction forms the fundamentals of most management policies to increase the productivity and efficiency of the organization [1]. Job satisfaction therefore is related to the positive sensation resulted from a job or profession and will affects individuals' attitudes towards their jobs [2].
In general, nurses represent a professional group with great physical and psychological pressure due to multiple work-related demands, shift working hours, and complex interpersonal relationships, for this reason health care worker have a high risk of psychological distress. They are forced to act and make quick decisions and it is a never-ending process of learning through experience [3].
The economic crisis has a big effect on anxiety levels, and it can have some serious results leading to negative effects on person’s life. Anxiety is the feeling of fear that occurs when faced with threatening or stressful situations. It is a normal response when confronted with danger, but, if it is overwhelming or the feeling persists, it could be regarded as an anxiety disorder.
Many studies were performed by measuring the job stress among nurses and its adverse effects. A quantitative cross-sectional survey aimed to establish correlation of self-reported skill levels and behaviors in relation to evidence-based practice, was conducted in early 2012 among senior nurses and midwives of a regional New South Wales Local Health District. The study used the Nurses Workplace Satisfaction Questionnaire “NWSQ” to assess the nurses’ satisfaction. The study concluded that nursing workplace policy which promotes and supports the pursuit of post-graduate education and which promotes job satisfaction gain, is likely to result in evidenced based practice capacity-related gains among senior nurses and midwives [4].
Another study aimed to assess the prevalence and risk factors of these mental states in a representative sample of Australian nurses. The Depression Anxiety Stress Scale was administered to 102 nurses. Information about sociodemographic and professional and work characteristics were obtained using lifestyle and in-house designed questionnaires. Prevalence rates of depression, anxiety, and stress were found to be 32.4%, 41.2%, and 41.2% respectively. Binominal logistic regressions for depression and stress were significant (p = 0.007, p = 0.009). Job dissatisfaction significantly predicted a higher risk of nurses developing symptoms of depression and stress respectively (p = 0.009, p = 0.011) [5].
For nearly 4 years, Lebanon has been assailed by the most devastating, multi-pronged crisis in its modern history. The unfolding economic and financial crisis that started in October 2019 has been further exacerbated by the economic impact of the COVID-19 outbreak, the massive Port of Beirut explosion in August 2020, Russia and Ukraine war, and the currency crisis.
Lebanon hospitals are facing the worst resource shortage experienced in the last decades as consequence of the above-mentioned facts, and nurses working in Lebanese healthcare system are doing their utmost to overcome this challenging situation.
A study conducted in Lebanon aimed to examine the direct effect of nurses’ emotional intelligence on their job satisfaction, as well as the indirect effect through the mediating role of job stress. The sample consisted of 365 nurses working in Lebanese hospitals during the COVID-19 period. The results revealed that emotional intelligence elements (Self-awareness, self-management, social-awareness and relationship-management) had a significant positive effect on nurses’ job satisfaction [6].
Nurses may experience Job dissatisfaction from a failure to cope with competitive work environments, long work hours coupled with overtime and an encroachment on personal life by the psychological burden associated with ethical dilemmas and decision making for patients. This leaves them with negative perception and lack of motivation and commitment to their work and the organization. This, in turn, affects the performance of the organization and ultimately, its bottom line.
Job satisfaction among hospital nurses has been studied in many developing and developed countries, but not in areas recently affected by wars and refugee crises or economic crises in the Middle East including Lebanon.
Objectives
The purpose of the study is to describe and compare the level of satisfaction and anxiety and its effect on the performance of nurses among Beirut and South of Lebanon hospitals and to proof that there is a correlation between the hospital Nurse's job satisfaction and the increased level of anxiety. This study helps to determine the prevalence of the psychological distress and its association with the job satisfaction among hospital nurses during economic crisis in South and Beirut hospitals. This will help to measure the level of nurse's job satisfaction among nurses in Beirut and in South of Lebanon hospitals, to identify the factors that influence the job satisfaction among nurses, and to assess whether nurses job satisfaction cause a decrease in the level of anxiety among nurses. It also help to describe job satisfaction and anxiety among nurses in some public and private university hospitals in Beirut and South Lebanon, to measure the effect of the hospital’s category on job satisfaction and anxiety levels, controlling for significant determinants, and to determine significant determinants of job satisfaction and anxiety and to create a “best-fit” model highlighting modifiable factors leading to potential improvements.
MATERIALS AND METHODS
Population
Nurses of all categories (nursing directors, nursing supervisors, head nurses, registered nurses and practical nurses) from four university hospitals, two publics and two privates, in Beirut and South of Lebanon were assessed in this study.
Inclusion/ Exclusion criteria
Every respondent with a work experience less than 4 years was excluded to ensure the assessment of the economic crisis on the salaries and its impact on the job satisfaction and anxiety level.
Instruments
The study is based on a closed-ended questionnaire that was as an electronic survey with many sections: The first section was an introduction to the study, describing the purpose of the study and its procedure, followed by an explicit question on the agreement to participate in this study and serving as an informed consent.
The second section addressed sociodemographic and professional information such as the gender of the participants, age, number of experience years, number of working days per week, number of working hours per day, if they work another job, their marital status, if they have kids and how many, their salary ranges before economic crisis and during economic crisis as well as their current average spending per month.
The third section contained the Generalized Anxiety Disorder Assessment (GAD-7) rating scale which addresses as a 4 points with 0 as “Not at all”, 1 “several days”, 2 “more than half the days” and 3 “nearly every day”, rating the following symptoms of anxiety: Feeling nervous, anxious or on edge, not being able to stop or control worrying, worrying too much about different things, trouble relaxing, being so restless that it is hard to sit still, becoming easily annoyed or irritable, feeling afraid as if something awful might happen. The total score for the seven items ranges from 0 to 21 is calculated as per the following scale: 0-4= minimal anxiety, 5-9= mild anxiety, 10-14: moderate anxiety and 15–21: severe anxiety. The GAD-7 has a sensitivity of 89% and a specificity of 82%. It is moderately good at screening three other common anxiety disorders - panic disorder (sensitivity 74%, specificity 81%), social anxiety disorder (sensitivity 72%, specificity 80%) and post-traumatic stress disorder (sensitivity 66%, specificity 81%) [7].
The fourth section enclosed The Nursing Workplace Satisfaction Questionnaire “NWSQ” using 5 points Likert scale from 1 as fully agree to 5 as definitely disagree, and it is a questionnaire used to evaluate dimensions of job satisfaction related to overall satisfaction with high validity, reliability and specificity demonstrated. It includes 17 points under 3 sections intrinsic, extrinsic and relational job satisfaction: how much does the nurse enjoy his/her job, criteria of doing their job and the people they work with. Exploratory factor analysis confirmed the validity of this 'three-way' conceptualization of nursing job satisfaction. Internal consistency analysis on a larger sample of responses yielded high Cronbach's Alpha values for all three domains and for the total overall, suggesting a stable and reliable measure [8].
Statistical analysis
Data were presented as number and percentage for categorical variables, and continuous data were expressed as the mean ± standard deviation (SD) and median and interquartile range (IQR= [Q1, Q3]). The data is gathered using a Google form, then transferred to SPSS program version 26. Chi-square test or Fisher’s exact test were performed to evaluate significant differences in proportions or percentages between the two groups. Fisher’s exact test was used where the chi-square test was not appropriate. The relationship between two numerical variables was calculated using Spearman correlation coefficient rho where the variable distributions were not Normal. The test for normal distribution was performed using the Shapiro-Wilk test. Finally, all tests with p-value (p) < 0.05 were considered significant.
RESULTS
298 responses from nurses of all categories, from 4 hospitals were gathered, 21 responses excluded according to the exclusion criteria and 277 responses were included in the study, the responses are distributed according to the following table:
| Parameters | Frequency (%) /
mean ±SD, median (IQR) |
| Age | 35.89 ±6.79
36 (10) |
| Years of experience | 13.09 ±5,71
13 (10) |
| Working days / week | 4.21 ±0.67
4 (0) |
| Working hours / day | 11.49 ±2.14
12 (0) |
| Salary Per Month Before the economic crisis (in USD) | 869.5 ±241.65
870 (160) |
| Salary Per Month during the economic crisis (in USD) | 328.5 ±129.21
350 (230) |
| Average spending / month in (USD) | 484.5 ±285.42
360 (430) |
| Hospital location
South of Lebanon Beirut |
157 (56.7%) |
| 120 (43.3%) | |
| Hospital category
Private university hospital Public university hospital |
178 (64.3%) |
| 99 (35.7%) | |
| Job position
Registered nurse Head nurse Practical nurse |
222 (80.1%) |
| 28 (10.1%) | |
| 27 (9.7%) | |
| Gender
Female Male |
180 (65.0%) |
| 97 (35.0%) | |
| Working in closed units
No Yes |
151 (54.5%) |
| 126 (45.5%) | |
| Working schedule
Alternate shifts Day duty Night duty |
128 (46.2%) |
| 86 (31.0%) | |
| 63 (22.7%) | |
| Working in another job
No Yes |
195 (70.4%) |
| 82 (29.6%) | |
| Marital status
Married Single Widowed Divorced |
219 (79.1%) |
| 35 (12.6%) | |
| 18 (6.5%) | |
| 5 (1.8%) |
Table 1. Statistical distribution of the categorical sociodemographic and professional characteristics.
The chi-square test and Fisher’s exact test showed a correlation between the hospital location, the hospital category, the job position, the working schedule, the nurse’s job satisfaction, working in a single job or more, the marital status and the nurse’s job satisfaction. In addition, the results showed no correlation between the gender and whether working in closed unit or not with the nursing job satisfaction.
| variables | Job Satisfaction Levels n (%) | p-value (test) | ||
| satisfied | neutral | dissatisfied | ||
| Hospital location
Beirut South of Lebanon |
20 (16.0) |
73 (60.8) |
27 (22.5) |
0.002* (C) |
| 27 (17.2) | 65 (41.4) | 65 (41.4) | ||
| Hospital category
Private university hospital Public university hospital |
48 (27.3) |
40 (22.2) |
90 (50.5) |
<0.0001* (C) |
| 11 (11.2) | 65 (65.2) | 23 (23.6) | ||
| Job position
Head nurse Practical nurse Registered nurse |
7 (25.0) |
14 (50.0) |
7 (25.0) |
0.0011* (F) |
| 12 (44.4) | 7 (25.9) | 8 (29.6) | ||
| 28 (12.6) | 117 (52.7) | 77 (34.7) | ||
| Gender
Male Female |
16 (16.5) |
45 (46.4) |
36 (37.1) |
0.59 (C) |
| 31 (17.2) | 93 (51.7) | 56 (31.1) | ||
| Working in closed units
No Yes |
26 (17.2) |
77 (51.0) |
48 (31.8) |
0.86 (C) |
| 21 (16.7) | 61 (48.4) | 44 (34.9) | ||
| Working schedule
Alternate shifts Day duty Night duty |
16 (12.5) |
73 (57.0) |
39 (30.5) |
0.0001* (C) |
| 22 (25.6) | 45 (52.3) | 19 (22.1) | ||
| 9 (14.3) | 20 (31.7) | 34 (54.0) | ||
| Working in another job
No Yes |
34 (17.4) |
117 (60) |
44 (22.6) |
<0.0001* (C) |
| 13 (15.9) | 21 (25.6) | 48 (58.5) | ||
| Marital status
Divorced Married Single Widowed |
1 (20.0) |
2 (40.0) |
2 (40.0) |
<0.0001* (F) |
| 27 (12.3) | 117 (53.4) | 75 (34.2) | ||
| 19 (54.3) | 12 (34.3) | 4 (11.4) | ||
| 0 (0.0) | 7 (38.9) | 11 (61.1) | ||
| *=significant test, C=chi-square test; F= Fisher’s exact test | ||||
Table 2. Relationships between categorical sociodemographic and professional characteristics, and the NWSQ.
The Spearman correlation test showed a positive correlation between: the age, working hours/ day, the average spending/ month, the years of experience and the nurses’ job satisfaction levels. However, no correlation was found between the working days/ week, with the nurses’ job satisfaction levels, the salary average before the economic crisis and the nurses’ job satisfaction levels, and the salary average during the economic crisis and the nurses’ job satisfaction levels.
| Correlation analysis | Spearman's rho (p-value) |
| Age / Job Satisfaction Levels | 0.157** (p-value =0.009) |
| Years of experience / Job Satisfaction Levels | 0.140* (p-value=0.019) |
| Working days-week / Job Satisfaction Levels | 0.012 (p-value=0.85) |
| Working hours-day / Job Satisfaction Levels | 0.164** (p-value=0.006) |
| Salary per month before the economic crisis (in USD) / Job Satisfaction Levels | 0.004 (p-value =0.95) |
| Salary per month during the economic crisis (in USD) / Job Satisfaction Levels | -0.112 (p-value =0.063) |
| Average spending /month (in USD) / Job Satisfaction Levels | 0.447** (p-value<0.0001) |
| *= Correlation is significant at the 0.05 level (2-tailed);
**= Correlation is significant at the 0.01 level (2-tailed). |
|
Table 3. Spearman correlation table between numerical sociodemographic and professional characteristics and the NWSQ.
The chi-square test and Fisher’s exact test showed a correlation between the hospital location, the hospital category, the working schedule, whether working in another job or not and the nurse’s anxiety levels, and no correlation between the job position, the gender, whether working or not in a closed unit, the marital status and the nurses’ anxiety level.
| variables | Anxiety Levels n (%) | p-value
(test) |
||
| Mild anxiety | Moderate anxiety | Severe anxiety | ||
| Hospital location
Beirut South of Lebanon |
7 (5.8) |
54 (45.0) |
59 (49.2) |
0.016* (C) |
| 7 (4.5) | 46 (29.3) | 104 (66.2) | ||
| Hospital category
Public university hospital Private university hospital |
3 (3.0) |
14 (14.1) |
82 (82.8) |
<0.0001* (C) |
| 11 (6.2) | 86 (48.3) | 81 (45.5) | ||
| Job position
Head nurse Practical nurse Registered nurse |
1 (3.6) |
10 (35.7) |
17 (60.7) |
0.54 (F) |
| 2 (7.4) | 6 (22.2) | 19 (70.4) | ||
| 11 (5.0) | 84 (37.8) | 127 (57.2) | ||
| Gender
Male Female |
3 (3.1) |
36 (37.1) |
58 (59.8) |
0.62 (F) |
| 11 (6.1) | 64 (35.6) | 105 (58.3) | ||
| Working in closed units
No Yes |
9 (6.0) |
58 (38.4) |
84 (55.6) |
0.45 (C) |
| 5 (4.0) | 42 (33.3) | 79 (62.7) | ||
| Working schedule
Alternate shifts Day duty Night duty |
3 (2.3) |
57 (44.5) |
68 (53.1) |
0.012* (F) |
| 9 (10.5) | 25 (29.1) | 52 (60.5) | ||
| 2 (3.2) | 18 (28.6) | 43 (68.3) | ||
| Working in another job
No Yes |
11 (5.6) |
83 (42.6) |
101 (51.8) |
0.0005* (F) |
| 3 (3.7) | 17 (20.7) | 62 (75.6) | ||
| Marital status
Divorced Married Single Widowed |
0 (0.0) |
1 (20.0) |
4 (80.0) |
0.89 (F) |
| 11 (5.0) | 83 (37.9) | 125 (57.1) | ||
| 2 (5.7) | 11 (31.4) | 22 (62.9) | ||
| 1 (5.6) | 5 (27.8) | 12 (66.7) | ||
| *=significant test, C=chi-square test; F= Fisher’s exact test | ||||
Table 4. Relationships between categorical sociodemographic and professional characteristics and the GAD-7.
The Spearman Correlation Coefficient showed no correlation between the years on experience, the working days/week, the working hours/day and the average salary per month before the economic crisis with the anxiety levels. It also showed a negative correlation between the average salary per month during the economic crisis and the nurses’ anxiety level, and a significant positive correlation between the average spending per month and the nurses’ anxiety levels.
| Correlation analysis | Spearman's rho (p-value) |
| Age/ Nurses’ Anxiety Levels | 0.001 (p-value= 0.99) |
| Years of experience/ Nurses’ Anxiety Levels | 0.022 (p-value= 0.71) |
| Working days-week/ Nurses’ Anxiety Levels | -0.040 (p-value= 0.51) |
| Working hours - day/ Nurses’ Anxiety Levels | 0.006 (p-value= 0.92) |
| Salary per month before the economic crisis (in USD)/ Nurses’ Anxiety Levels | 0.004 (p-value= 0.94) |
| Salary per month during the economic crisis (in USD)/ Nurses’ Anxiety Levels | -0.352** (p-value <0.0001) |
| Average spending /month (in USD)/ Nurses’ Anxiety Levels | 0.493** (p-value <0.0001) |
| **. Correlation is significant at the 0.01 level (2-tailed). | |
| *. Correlation is significant at the 0.05 level (2-tailed). | |
Table 5. Spearman correlation table between numerical sociodemographic and professional characteristics and the GAD-7.
In addition to the above results, the Spearman correlation test shows a high statistical significance between the hospital nurses’ salaries during the economic crisis and job satisfaction, and a high statistical significance between the job satisfaction and the anxiety level. These correlations are identified by a negative relation between salary per month during the economic crisis and total job satisfaction score: decreased salary per month during the economic crisis leads to a higher job satisfaction score (high score means low job satisfaction), and a positive relation between total job satisfaction score and the total anxiety score: increased total job satisfaction score leads to a higher anxiety score (high score means high anxiety level).
| Spearman’s correlations | Total job satisfaction score | Total anxiety score | |
| Salary per month during the economic crisis (in USD) | Spearman’s correlation | -0.157** | |
| p-value | 0.009 | ||
| Total job satisfaction score | Spearman’s correlation | 0.367** | |
| p-value | <0.0001 | ||
| **. Correlation is significant at the 0.01 level (2-tailed). | |||
Table 6. Correlation between the nurses’ salaries during the economic crisis and the nurses’ job satisfaction, and between the nurses' job satisfaction and the nurses' anxiety levels.
DISCUSSION
Our results show that there is a correlation between the hospital nurse’s job satisfaction and the increased level of anxiety during economic crisis in Lebanon, this result matches what already found in similar study performed in 2016 and showed that a significant proportion of nurses suffered from stress, as well as their satisfaction with job is very low with severe anxiety [9].
Our results also show that there is a cause-effect relation between the salary range and the job dissatisfaction and the level of anxiety
, similar result confirmed by a study in Saudi Arabia, that assessed how dissatisfaction with salary, workload and teamwork, individually and in combination, was associated with those conditions, concluded that the dissatisfaction with workload were significantly associated with both anxiety and stress [10]. Furthermore, our results confirmed that scores for job satisfaction are higher, with lower scores for anxiety, among nurses practicing in private university hospitals compared to those practicing in public university hospitals. This comparison was not found in the literature in our available knowledge. These results are comparable to a cross-sectional study in China in 2019 that focused on the associations between the sub dimensions of occupational stress and psychosomatic wellbeing among nurses, and identified that workload and time pressure were correlated with anxiety. The study also identified that professional and career issues were associated with depression, and that interpersonal relationships and management problems were associated with anxiety, depression, and somatic symptoms [11]. Finally, the results confirm that scores for job dissatisfaction and anxiety are higher among nurses with low salaries compared to their colleagues with high ones, which goes along with what already have been showed in a study conducted in Lebanon and investigated the reasons for the migration of Lebanese nurses and incentives that would attract them back to their home country and showed that the top reasons for nurses to leave Lebanon included unsatisfactory salary or benefits [12].
<
CONCLUSION
In conclusion the results show the correlation between the decreased nurses job satisfaction with the increased level of anxiety among the hospital nurses in Beirut and South of Lebanon hospitals.
The results of our study also show the high negative correlation between salaries after economic crisis in parallel with the average spending per month and the total job satisfaction in addition to a high positive correlation between the total job satisfaction and the anxiety levels. In addition to the mentioned above, the results showed that both anxiety level and job satisfaction among hospital nurses are subjective to the hospital locations and categories, and to the variables in the sociodemographic and professional characteristics. It also shows how the economic crisis has a significant impact on the nursing physiological status in both job satisfaction and anxiety levels.
Limitations
The study limitation was to have the approval of the of the hospitals in Beirut and South of Lebanon do fill the questionnaire by their staff. We had to shift to other hospitals of the same categories and restart the approval process which compromised our study time.
Local Ethics Committee approval: Approval from three Institutional Review Boards with letters references: “2023-1105” on December 12, 2023, “3/2024” on February 5, 2024, and “IRB23RP26” on December 12, 2023 were obtained for the study.
- Conflict of interest and source of funding statement
The authors report no conflict of interest, and the research did not receive any specific grant from funding agencies in the public, commercial, or not for profit sectors.
Authors’ contribution
All authors contributed to the final manuscript.
REFERENCES
- Jelena Culibrk, M. D., Job Satisfaction, Organizational Commitment and Job Involvement: The Mediating Role of Job Involvement, Frontiers, (2018). DOI:3389/fpsyg.2018.00132.
- Siti Nurjanah, V. P., The influence of transformational leadership, job satisfaction, and organizational commitments on Organizational Citizenship Behavior (OCB) in the inspectorate general of the Ministry of Education and Culture, Researh Gate, (2020). DOI:1080/23311975.2020.1793521.
- Sajed Faisal Ghawadra, K. L., Psychological distress and its association with job satisfaction among nurses in a teaching hospital, Journal of Clinical Nursing, (2019). DOI: 1111/jocn.14993
- Greg Fairbrother, A. C., Evidence Based Clinical Nursing Practice in a Regional Australian Healthcare Setting: Predictors of Skills and Behaviours. Collegian, (2015). DOI:1016/j.colegn.2015.03.005.
- . Shamona Maharaj, T. L., Prevalence and Risk Factors of Depression, Anxiety, and Stress in a Cohort of Australian Nurses. International Journal of Environmental Research and Public Health, (2018). DOI: 3390/ijerph16010061.
- Suzan Al Kadi, A. R., Nurses’ Emotional Intelligence, Satisfaction in Lebanon: The Mediating Role of Job Stress. International Review of Management and Marketing. (2023). DOI: https://doi.org/10.54729/2789-8296.1131.
- Nerys Williams, GAD-7 questionnaire, Occupational Medicine, (2014). DOI:1093/occmed/kqt161.
- Greg Fairbrother, A. J., Development and validation of the Nursing Workplace Satisfaction Questionnaire (NWSQ), Contemporary Nurse, (2014). DOI:5172/conu.2009.34.1.010.
- Mohsen Poursadeghiyan, M. A., Relationship Between Job Stress and Anxiety, Depression andJob Satisfaction in Nurses in Iran. Medwell Journals, (2016).. https://www.researchgate.net/publication/311351564_Relationship_Between_Job_Stress_and_Anxiety_Depression_and_Job_Satisfaction_in_Nurses_in_Iran.
- Nazmus Saquib, M. S.-M.-M., Association of Cumulative Job Dissatisfaction with Depression, Anxiety and Stress among Expatriate Nurses in Saudi Arabia. Journal of Nursing Management, (2019). DOI: 1111/jonm.12762.
- Bo Gu, Q. T., The association between occupational stress and psychosomatic wellbeing among Chinese nurses: A cross-sectional survey. Medicine, (2019). DOI: 1097/MD.0000000000015836.
- Mohamad Alameddine, S. A.-E.-H., What Made Lebanese Emigrant Nurses Leave and What Would Bring Them Back? A Cross-Sectional Survey. International Journal of Nursing Studies, (2020). DOI: 1016/j.ijnurstu.2019.103497.
![]() This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
