Debbie Nomiko1*, Ernawati1, Bettywaty Eliezer1
1Nursing Department, Health Polytechnic Ministry of Health Jambi, Indonesia
Corresponding author: Debbie Nomiko, dr. Tazar Street, BuluranKenali, Kec. Telanaipura, Kota Jambi, Jambi 36361, Indonesia, Orcid :https://orcid.org/0000-0002-3623-7937, Phone: +62 812-7897-981, Email: debbiedebbienomiko@gmail.com
Cita questo articolo
ABSTRACT
Introduction: Sleep quality disorders may cause a decrease in concentration and work performance of individual. It is also believed that nurses with work shifts as health workers may run into sleep quality disorders. Several researches have shown the relationship between sleep quality and the work performance of nurses in shifts duty. This study aimed to determine the relationship of sleep quality and vigilance of nurses in shifts duty in Raden Mattaher hospital Jambi.
Methods: A cross sectional study was performed recruiting 97 nurses working shifts in 3 inpatients wards of the Raden Mattaher Hospital Jambi. Socio-demographic details and data nurses alertness were collected using ad hoc questionnaires, data sleep quality were collected using the Pittsburgh Sleep Quality Index. Relationships among sleep patterns and alertness variables were investigated. Data were analyzed by univariate and chi-square test (CI 95%). Statistical analysis was performed using the SPSS version 16.0.
Results: Results showed an average of 29.4 years of age. Respondents were mostly female, married with working time <5 years. The results of the bivariate analysis show there was not relationship between sleep quality and vigilance of nurses who undergoing shifts in Raden Mattaher hospital Jambi with p-value 0.35.
Conclusion: There was not a relationship between sleep quality and vigilance among nurses undergoing a shift in patients’ rooms
Keywords: Nurses, Sleep Quality, Wakefulness, Shift Work Schedule
INTRODUCTION
The prevalence of sleep quality disorders every year tends to increase, one of the causes is fatigue due to excessive work volume [1–4]. Poor sleep quality may cause adverse effects workers physical and psychological health leading to negative consequence workplace such as mistakes and reduced performances [5–8]. Health professionals have been known to experience fatigue at times. The condition has also long been associated with reduced patient safety [9,10]; decreased satisfaction, health and well-being [11–13]; more conflict among team members [14]; risk of needle stick injuries [14,15] and increased staff turnover [10]. Nurses, the largest group of healthcare providers, are prone to relatively high acute burnout, chronic fatigue, and recovery from fatigue after shift changes [16]. It is closely related to the demands they face throughout the working day, such as physical, mental, emotional demands and pressures associated with shift and non-standard work schedules. These factors place hospital nurses very vulnerable to burnout and its accompanying effects [17].
Nurses are professional workers who use a shift work system, so it can be ascertained that sleep quality disorders can also occur in nurses who undergo shifts [18–20]. Shift work has an impact on disturbances in circadian rhythms [21], and the main one being sleep pattern disturbances that cause sleep deprivation and fatigue [22,23].
Vigilance is degree of readiness of a person in responding to something [24] A person’s level of vigilance is needed at work. Accidents occur as a result of decreased levels of alertness [25]. Variables that affect the level of alertness are monotonous state, level of sleepiness, psychophysiology, distraction, and work fatigue. In the variable of sleepiness level, there are 3 indicator variables, namely, circadian rhythm, sleep quality, and sleep time [26,27]. Research results show that 78% of nurses who work shifts experience changes in sleep quality. Furthermore, poor sleep quality is one of the contributing factors to medical errors that occur in health services [28–30]. The impact of poor sleep quality has been widely studied. Sleep absence is an important predictive factor influencing the occurrence of various chronic diseases such as hypertension [31] and cardiovascular disease [32], and diabetes [33]. Nurses’ inconsistent sleep habits can have a severe impact on their health as well as their ability to do their jobs [34,35].
METHODS
Trial design
A cross-sectional study was made at the Raden Mattaher Hospital Jambi.
Participants
The population in this study was all shift nurses in 3 inpatient installations at Raden Mattaher Hospital Jambi with a total sample of 97 people with the criteria of nurses in the inpatient installation, not leave, having at least a minimum nursing diploma.
Intervention
A study questionnaire was made to collect socio-demographic details and a 24 items questionnaire was implemented to collect nurses’ alertness data. to four point scored Likert scales (always, often, sometimes and never) were used for the self-assessment of nurses’ alertness before, during and after care activities, with particular attention to missed cares, mistakes and documentation management. Nurses’ sleep quality was assessed using the Pittsburgh Sleep Quality Index (PSQI) tool [36]. Authors declare that the PSQI (Indonesian version) permission to use was obtained by the copyright property.
The PSQI is widely considered the gold standard tool for sleep patterns evaluation and quality of sleep assessment. It provides a global score ranged from 0 to 21 where scores higher than 5 means poor sleep quality. Furthermore, it provides 7 sub-scores assessing sleep patterns: subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleeping medications, and daytime dysfunctions. The PSQI questionnaire was translated into Indonesian and
tested for reliability with Cronbachs alpha result of 0.753. Data were collected by three interviewers who were unknown to the participants before the study.
Blinding
In this study, 3 enumerators were used to collect research data. The previous enumerators did not know the participants because they were students who had been trained by the researcher before collecting data.
Ethical Consideration
Before carrying out data collection, the researcher first took care of ethical permission. The authors state that this study followed all ethical clearance processes and was approved by the health research ethics committee of Jambi Universitys Faculty of Medicine and Health Sciences.
Statistical methods
Data were presented as numbers or percentages for categorical variables. Continuous data are expressed as the mean ± standard deviation (SD), or median with Interquartile Range (IQR). The chi square test and Fisher’s exact test were performed to evaluate significant differences of proportions or percentages between two groups. Particularly Fisher’s exact test was used where the chi square test was not appropriate. All tests with p-value (p)<0.05 were considered significant. Statistical analysis was performed using the SPSS version 16.0 application.
RESULTS
Ninety-seven out of one hundred twenty-two nurses working shifts in 3 wards) qualified nurses
completed their studies. The results of this study presented in the table 1.
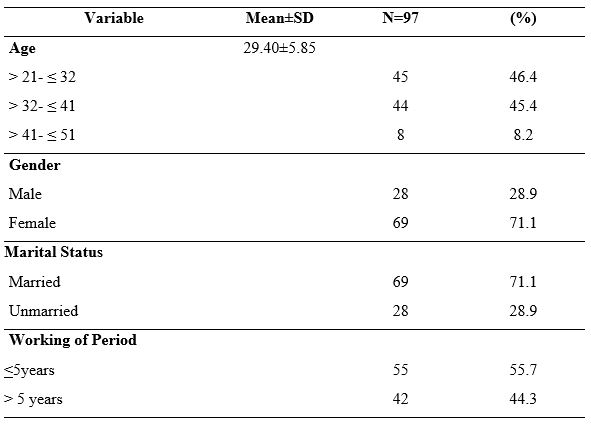
Table 1. Demographic Data of Nurses Undergoing Shift
Most of respondents were female (71.1%), married (71.1%) and have working of period < 5 years (55.7%). These results showed the average age of the respondents was 29.40 years, and the age range was between 21-51 years (SD 5.85).
Table 2 shows the results of the assessment of the seven components of the respondent’s sleep quality, it was found that the component of the use of sleeping pills (using pills) had the highest score in terms of not using, namely 97.93%, the second highest score was the component of the subject’s sleep quality, namely the subjective average of respondents stated 86.6% had good sleep quality. The results also showed that most of the respondents had sleep disturbances as much as 65%, and as many as 40% had sleep efficiency in the range of 75-84%.
That most nurses (86.6%) have good sleep quality based on subjective sleep quality. In the second component (sleep latency), most of the respondents (51.5%) had a sleep latency of 1-2 hours, and merely a small portion (7.2%) had a sleep latency of 5-6 hours.

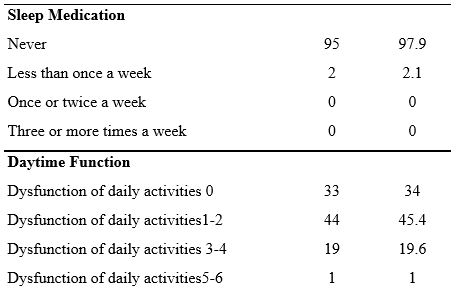
Table 2. Sleep Quality Components: Subjective and Objective Sleep Quality measures
In the third component (sleep duration), most of the respondents, as many as 32% of respondents, had sleep duration < 5 hours and only five respondents (5.2%) had sleep duration > 7 hours. Furthermore, 26.8% of the fourth component had a daily sleep efficiency > 85%, and only 14 respondents (14.4%) had a daily sleep efficiency of 14.4%. This result is slightly different from the previous study [49], which showed that 73.5% of nurses have sleep efficiency >85%.
Sleep quality in terms of sleep disturbance components shows that most of the respondents (67%) have sleep disorders with a score of 1-9, then for the use of sleeping pills, most of the respondents (97.93%) have never used sleeping pills at all.
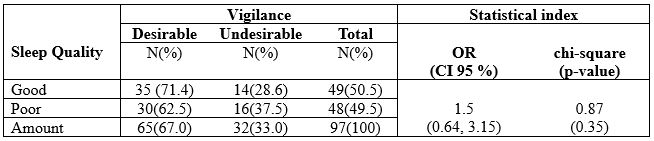
Table 3. The Correlation Between Sleep Quality and Vigilance Among Nurses undergoing Shift
The results of statistical tests obtained a p-value = 0.35, so it can be concluded that there was not a
significant relationship between sleep quality and vigilance among nurses who undergoing a shift in
the hospital.
DISCUSSION
Statistically it was found that in this study, there was no relationship between sleep quality and nurses’ work alertness, although descriptively it can be reported that Nurses with good sleep quality tend to have good vigilance, and contrarily, nurses who have poor sleep quality tend to have less vigilance (see table 3). It significantly affects the productivity of nurses at work, where nurses in carrying out their work with good vigilance will work with good performance compared to nurses who are less alert.
Nurses who work night and rotating hours have been proven to have more trouble staying awake on duty and make twice as many mistakes as those who work day and evening shifts. More than 20% of workers in industrialized countries work shifts, and about 10% of them are diagnosed with sleep disorders [37]. Many factors affect sleep quality, one of which is shift work. Individuals who work shifts or shifts have difficulty adjusting to changing sleep schedules [6].
Poor sleep quality mainly occurs in nurses who use shift work systems. A study by Murphy et al., [38] found that shift work was significantly associated with poor sleep quality after controlling for variables of age, gender, and length of work.
This study also found almost the same proportion of respondents between respondents who had good and bad sleep quality, while most of the respondents had the desired of vigilance, which was around 67%. A systematic review study conducted by Dall’Ora et al. [39] found that shift characteristics are related to employee performance, and having sufficient rest time positively affects employee vigilance. Furthermore, Wahyuni [40] found a decrease in vigilance in night shift nurses with a proportion of decreased vigilance of 71.1%. However, statistically, it was not proven
to have a significant effect. The factor that influences the level of alertness before office hours is the
sleep quality. Lack of sleep results in a person’s condition is less energetic and not enthusiastic [41].
We report that research data show that nurses predominately have a sleep latency of 1-2 hours, and only a small proportion (7.2%) have a sleep latency of 5-6 hours. Sleep latency is the length of sleep from start to fall asleep [42,43]. One of the factors that can affect sleep latency is bedtime habits that can disrupt a person’s sleep and have an impact on increasing sleep latency [44].
This result is in line with the results of a previous study [45] that most respondents (60.3%) shift nurses experienced sleep disturbances less than once a week. Of all the sleep quality components, the sleep disturbance component had the highest mean of 1.44 with a standard deviation of 0.90 in a study of nurses undergoing shifts in Jordan [46].
Nurses’ poor sleep quality leads to a number of negative health outcomes. Nurses suffering from
poor sleep quality were more prone to develop burnout [47], depression and anxiety [48]. In addition, poor sleep could impair cognitive performance, such as concentration and memory, which may lead to poor work performance and even affect patients’ safety [49-51].
Effective measures, such as education on sleep hygiene [48], yoga [52] and cognitive-behavioral therapy for insomnia [53], should be considered to improve nurses’ sleep quality, quality of life, and patients’ safety.
CONCLUSION
The current study found that sleep quality was not a significant factor contributing to nurses’ vigilance and medical error. Nevertheless, we still suggest that hospital managers should apply a 15-30 minute rest period during work shifts for nurses and pay attention to work rotation times, especially night shifts as a strategy to increase vigilance to prevent fatigue, sleepiness, and work errors.
LIMITATION OF STUDY
This study was only conducted in 3 hospital wards, so it cannot be compared with the same conditions in different hospitals. No intervention was carried out in this study to improve nurses’ sleep quality and increase alertness while working. Other factors that influence Precautions, such as lighting conditions, environment, pills, caffeine, and other ingredients, were not studied.
Authors’ contribution
All authors equally contributed to preparing this article.
Acknowledgement
We express our gratitude to the director Director of Health Polytechnic, Ministry of Health Jambi, Indonesia for its support for the implementation of this research
Funding
This research received funding from the Development and Empowerment of Human Resources in Public Health (BPPSDMK) Indonesia
Conflict Of Interest
The authors declare that there was no conflict of interest in this research.
REFERENCES
- Deng X, Liu X, Fang R. Evaluation of the correlation between job stress and sleep quality in community nurses. Medicine. 2020;99(4).
- Boll J. Development of a Measure of Nurse Vigilance from the Patient’s Perspective: A Content Validity Study. 2014;
- Surani S, Hesselbacher S, Guntupalli B, Surani S, Subramanian S. Sleep quality and vigilance differ among inpatient nurses based on the unit setting and shift worked. Journal of patient safety. 2015;11(4):215–20.
- Kaliyaperumal D, Elango Y, Alagesan M, Santhanakrishanan I. Effects of sleep deprivation on the cognitive performance of nurses working in shift. Journal of clinical and diagnostic research: JCDR. 2017;11(8):CC01.
- Sayilan AA, Kulakaç N, Uzun S. Burnout levels and sleep quality of COVID-19 heroes. Perspect Psychiatr Care. 2020;57(3):1231–6.
- PA Potter AP. Fundamental Keperawatan. Jakarta: EGC; 2006.
- Tsai J-C, Chou K-R, Tsai H-T, Yen Y-C, Niu S-F. Effects of nocturnal sleep quality on diurnal cortisol profiles and attention in nurses: A cross-sectional study. Biological Research for Nursing. 2019;21(5):510–8.
- Di Muzio M, Diella G, Di Simone E, Pazzaglia M, Alfonsi V, Novelli L, et al. Comparison of Sleep and Attention Metrics Among Nurses Working Shifts on a Forward-vs Backward-Rotating Schedule. JAMA network open. 2021;4(10):e2129906–e2129906.
- Rainbow JG, Drake DA, Steege LM. Nurse health, work environment, presenteeism and patient safety. Western journal of nursing research. 2020;42(5):332–9.
- Smith-Miller CA, Shaw-Kokot J, Curro B, Jones CB. An integrative review. The journal of nursing administration. 2014;44(9):487–94.
- Asakura K, Asakura T, Satoh M, Watanabe I, Hara Y. Health indicators as moderators of occupational commitment and nurses’ intention to leave. Japan Journal of Nursing Science. 2020;17(1):e12277.
- Austin S, Fernet C, Trépanier S, Lavoie‐Tremblay M. Fatigue in new registered nurses: A 12‐month cross‐lagged analysis of its association with work motivation, engagement, sickness absence and turnover intention. Journal of nursing management. 2020;28(3):606–14.
- Bazazan A, Dianat I, Rastgoo L, Zandi H. Relationships between dimensions of fatigue and psychological distress among public hospital nurses. Health promotion perspectives. 2018;8(3):195.
- Han K, Trinkoff AM, Geiger-Brown J. Factors associated with work-related fatigue and recovery in hospital nurses working 12-hour shifts. Workplace health & safety. 2014;62(10):409–14.
- Fisman DN, Harris AD, Rubin M, Sorock GS, Mittleman MA. Fatigue increases the risk of injury from sharp devices in medical trainees results from a case-crossover study. Infection Control & Hospital Epidemiology. 2007;28(1):10–7.
- Barker LM, Nussbaum MA. Fatigue, performance and the work environment: a survey of registered nurses. Journal of advanced nursing. 2011;67(6):1370–82.
- Steege LM, Drake DA, Olivas M, Mazza G. Evaluation of physically and mentally fatiguing tasks and sources of fatigue as reported by registered nurses. Journal of Nursing Management. 2015;23(2):179–89.
- Reinke L, Özbay Y, Dieperink W, Tulleken JE. The effect of chronotype on sleepiness, fatigue, and psychomotor vigilance of ICU nurses during the night shift. Intensive care medicine. 2015;41(4):657–66.
- Geiger-Brown J, Rogers VE, Trinkoff AM, Kane RL, Bausell RB, Scharf SM. Sleep, sleepiness, fatigue, and performance of 12-hour-shift nurses. Chronobiology international. 2012;29(2):211–9.
- Ruggiero JS, Redeker NS, Fiedler N, Avi-Itzhak T, Fischetti N. Sleep and psychomotor vigilance in female shiftworkers. Biological research for nursing. 2012;14(3):225–35.
- Sun Q, Ji X, Zhou W, Liu J. Sleep problems in shift nurses: A brief review and recommendations at both individual and institutional levels. Journal of Nursing Management. 2019;27(1):10–8.
- Maurits LS, Widodo ID. Faktor dan Penjadualan Shift Kerja. Teknoin. 2008;13(2):18–22.
- Dong H, Zhang Q, Sun Z, Sang F, Xu Y. Sleep disturbances among Chinese clinical nurses in general hospitals and its influencing factors. BMC Psychiatry. 2017;17(1):1–9.
- Dorrian, J., Roach, Gregory.D., Fletcher, A., Dawson D. Simulated train driving: Fatigue, self awareness and cognitive disengagement. Applied Ergonomics. 2007;
- Desai A V., Haque MA. Vigilance monitoring for operator safety: A simulation study on highway driving. Journal of Safety Research. 2006;37(2):139–47.
- Zeng L-N, Yang Y, Wang C, Li X-H, Xiang Y-F, Hall BJ, et al. Prevalence of poor sleep quality in nursing staff: a meta-analysis of observational studies. Behavioral sleep medicine. 2020;18(6):746–59.
- Tu Z, He J, Zhou N. Sleep quality and mood symptoms in conscripted frontline nurse in Wuhan, China during COVID-19 outbreak: A cross-sectional study. Medicine. 2020;99(26).
- Arimura M, Imai M, Okawa M. Sleep, Mental Health and Errors in Nurses. Industrial health. 2010;48(6):811–7.
- Balas MC, Casey CM, Scott LD, Rogers AE. Maintain vigilance in the ICU. Nursing2020 Critical Care. 2007;2(4):38–44.
- Boughattas W, El Maalel O, Chikh R Ben, Maoua M, Houda K, Braham A, et al. Hospital night shift and its effects on the quality of sleep, the quality of life, and vigilance troubles among nurses. International Journal of Clinical Medicine. 2014;2014.
- Wang Y, Mei H, Jiang Y-R, Sun W-Q, Song Y-J, Liu S-J, et al. Relationship between duration of sleep and hypertension in adults: a meta-analysis. Journal of Clinical Sleep Medicine. 2015;11(9):1047–56.
- Cappuccio FP, Cooper D, D’Elia L, Strazzullo P, Miller MA. Sleep duration predicts cardiovascular outcomes: a systematic review and meta-analysis of prospective studies. European heart journal. 2011;32(12):1484–92.
- Alimoradi Z, Lin C-Y, Broström A, Bülow PH, Bajalan Z, Griffiths MD, et al. Internet addiction and sleep problems: A systematic review and meta-analysis. Sleep medicine reviews. 2019;47:51–61.
- Gómez-García T, Ruzafa-Martínez M, Fuentelsaz-Gallego C, Madrid JA, Rol MA, Martínez-Madrid MJ, et al. Nurses’ sleep quality, work environment and quality of care in the Spanish National Health System: observational study among different shifts. BMJ open. 2016;6(8):e012073.
- Kang J, Noh W, Lee Y. Sleep quality among shift-work nurses: A systematic review and meta-analysis. Applied nursing research. 2020;52:151227.
- Buysse DJ, Reynolds III CF, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry research. 1989;28(2):193–213.
- Basent B. Shift-work sleep disorder. New England Journal of Medicine. 2005;353(5):519–21.
- Murphy R, Osterweil D, MscED CMD, Spivack BS, Zee PC. Improving Sleep Management in the Elderly. Citeseer; 2010.
- Dall’Ora C, Ball J, Recio-Saucedo A, Griffiths P. Characteristics of shift work and their impact on employee performance and wellbeing: A literature review. International journal of nursing studies. 2016;57:12–27.
- Wahyuni I, Dirdjo MM. Hubungan Kelebihan Waktu Kerja dengan Kelelahan Kerja dan Kinerja pada Perawat di Ruang Perawatan Intensif RSUD Abdul Wahab Sjahranie Samarinda. Borneo Student Research (BSR). 2020;1(3):1715–24.
- Budiawan W, Prastawa H, Kusumaningsari A, Sari DN. Pengaruh Monoton, Kualitas Tidur, Psikofisiologi, Distraksi, Dan Kelelahan Kerja Terhadap Tingkat Kewaspadaan. J@Ti Undip : Jurnal Teknik Industri. 2016;11(1).
- Rocha MCP da, Martino MMF De. Stress and sleep quality of nurses working different hospital shifts. Revista da Escola de Enfermagem da USP. 2010;44:280–6.
- Fietze I, Knoop K, Glos M, Holzhausen M, Peter JG, Penzel T. Effect of the first night shift period on sleep in young nurse students. European journal of applied physiology. 2009;107(6):707–14.
- Mubarok. Buku Ajar Kebutuhan Dasar Manusia : Teori & Aplikasi dalam Praktik. Jakarta: EGC; 2007.
- Safitrie A, Ardani MH. Studi Komparatif Kualitas Tidur Perawat Shift dan Non Shift di Unit Rawat Inap dan Unit Rawat Jalan. Prosiding Konferensi Nasional PPNI Jawa Tengah. 2013;17–23.
- Suleiman K, Al-Khaleeb T, Al-Kaladeh M, Sharour LA. The Effect of Shift Fluctuations on Sleep Quality among Nurses Working in the Emergency Room in Amman, Jordan. International Journal of Occupational Safety and Health. 2020;10(1):11–7.
- Giorgi, F., Mattei, A., Notarnicola, I., Petrucci, C., & Lancia, L. Can sleep quality and burnout affect the job performance of shift-work nurses? A hospital cross-sectional study. Journal of Advanced Nursing, 2018; 74, 698–708. doi:10.1111/jan.13484
- Baroni, A., Bruzzese, J. M., Di Bartolo, C. A., Ciarleglio, A., & Shatkin, J. P. Impact of a sleep course on sleep, mood and anxiety symptoms in college students: A pilot study. Journal of American College Health, 2018; 66, 41–50. doi:10.1080/07448481.2017.1369091
- Barbe, T., Kimble, L. P., & Rubenstein, C. Subjective cognitive complaints, psychosocial factors and nursing work function in nurses providing direct patient care. Journal of Advanced Nursing, 2018; 74, 914–925. doi:10.1111/ jan.13505
- Caruso, C. C. Negative impacts of shiftwork and long work hours. Rehabilitation Nursing, 2014; 39, 16–25. doi:10.1002/rnj.107
- Park, E., Lee, H. Y., & Park, C. S. Association between sleep quality and nurse productivity among Korean clinical nurses. Journal of Nursing Management. 2018; doi:10.1111/jonm.12634
- Fang, R., & Li, X. A regular yoga intervention for staff nurse sleep quality and work stress: A randomised controlled trial. Journal of Clinical Nursing, 2015; 24, 3374–3379. doi:10.1111/jocn.12983
- Kalmbach, D. A., Cheng, P., Arnedt, J. T., Anderson, J. R., Roth, T., Fellman-Couture, C., … Drake, C. L. Treating insomnia improves depression, maladaptive thinking, and hyperarousal in postmenopausal women: Comparing cognitive-behavioral therapy for insomnia (CBTI), sleep restriction therapy, and sleep hygiene education. Sleep Medicine, 2019; 55, 124–134. doi:10.1016/j.sleep.2018.11.019
![]() This work is licensed under a Creative Commons
This work is licensed under a Creative Commons
Attribution-NonCommercial-NoDerivatives 4.0 International License.

