Akifumi Maeda 1*, Akemi Hirao 1, Akiko Sugimoto 1, Motoko Hori 2
- Department of Critical Care and Emergency Nursing, Faculty of Nursing, Senri Kinran University, Osaka, Japan
- Department of Chronic Care Nursing, Faculty of Nursing, Senri Kinran University, Suita, Osaka, Japan
* Corresponding author: Akifumi Maeda, Department of Critical Care and Emergency Nursing, Faculty of Nursing, Senri Kinran University, 5-25-1 Fujishirodai, Suita, Osaka, Japan. ORCID: http://orcid.org/0000-0002-2628-2224. E-mail: ak-maeda@cs.kinran.ac.jp
Akifumi Maeda, Akemi Hirao, Akiko Sugimoto, Motoko Hori
Original Article
DOI:10.32549/OPI-NSC-124
Submitted: 07 May 2025
Revised: 17 July 2025
Accepted: 17 July 2025
Published online: 30 July 2025
License: This article is licensed under the Creative Commons Attribution - Non Commercial - No Derivatives 4.0 (CC BY NC ND 4.0) international license.
Keywords: Clinical Reasoning, Physical Assessment, Undergraduate Nursing Student, Cues
Abstract:
Introduction: Physical assessment is a fundamental clinical skill in nursing practice and crucial to
developing effective nursing care plans. Thus, acquiring knowledge and skills in physical assessment
is an essential competence for undergraduate nursing students.
Objective: This study aimed to investigate the effect of utilizing pre-assignment work and presenting
specific cues about a case on the clinical reasoning skills of undergraduate nursing students by
comparing an intervention group that received specific cues with a control group that did not.
Materials: This randomized controlled trial involved second-year undergraduate nursing students.
Participants were randomly assigned to an intervention or control group. Both groups completed a
pre-assignment related to heart failure and participated in a 60-minute group case study session. The
intervention group received specific cues related to the case during the session, guiding their
assessment and care planning. Clinical reasoning skills were evaluated subjectively using the Clinical
Reasoning Skills Self-Assessment Scale (CRSS) and objectively by analyzing the students’ responses
to the group task.
Results: A total of 94 participants were randomly assigned to either the intervention group (n= 47)
or the control group (n= 47). While the pre-session CRSS scores were similar between groups, the
post-session scores on several items related to information gathering, interpretation, problem
identification, and goal setting were significantly higher in the intervention group. Qualitative
analysis of narrative responses revealed that the intervention group provided more specific and
patient-centered nursing care plans based on the patient's symptoms, whereas the control group
offered more generalized interventions.
Conclusion: The use of pre-assignment and specific cues enhanced students’ ability to interpret
patient information and formulate individualized nursing care plans. This approach effectively
improved clinical reasoning skills in physical assessment and may serve as a practical alternative in
educational settings lacking simulation-based resources.
Cite this article
ABSTRACT
Introduction: Physical assessment is a fundamental clinical skill in nursing practice and crucial to developing effective nursing care plans. Thus, acquiring knowledge and skills in physical assessment is an essential competence for undergraduate nursing students.
Objective: This study aimed to investigate the effect of utilizing pre-assignment work and presenting specific cues about a case on the clinical reasoning skills of undergraduate nursing students by comparing an intervention group that received specific cues with a control group that did not.
Materials: This randomized controlled trial involved second-year undergraduate nursing students. Participants were randomly assigned to an intervention or control group. Both groups completed a pre-assignment related to heart failure and participated in a 60-minute group case study session. The intervention group received specific cues related to the case during the session, guiding their assessment and care planning. Clinical reasoning skills were evaluated subjectively using the Clinical Reasoning Skills Self-Assessment Scale (CRSS) and objectively by analyzing the students’ responses to the group task.
Results: A total of 94 participants were randomly assigned to either the intervention group (n= 47) or the control group (n= 47). While the pre-session CRSS scores were similar between groups, the post-session scores on several items related to information gathering, interpretation, problem identification, and goal setting were significantly higher in the intervention group. Qualitative analysis of narrative responses revealed that the intervention group provided more specific and patient-centered nursing care plans based on the patient’s symptoms, whereas the control group offered more generalized interventions.
Conclusion: The use of pre-assignment and specific cues enhanced students’ ability to interpret patient information and formulate individualized nursing care plans. This approach effectively improved clinical reasoning skills in physical assessment and may serve as a practical alternative in educational settings lacking simulation-based resources.
Keywords: Clinical Reasoning, Physical Assessment, Undergraduate Nursing Student, Cues.
INTRODUCTION
Physical assessment refers to the process of collecting and evaluating information about a patient’s physical condition through interviews and physical examination techniques, including inspection, palpation, percussion, and auscultation [1]. It is a core clinical competency in nursing practice [2] and is essential for developing effective nursing care plans [3]. Because accurately collecting both subjective and objective patient data enables nurses to appropriately assess a patient’s condition [4], acquiring physical assessment skills is critically important for undergraduate nursing students [5].
In recent years, simulation-based education has attracted attention as an effective method for undergraduate nursing students to acquire physical assessment skills and become clinically competent upon graduation [6,7]. However, implementing simulation-based education requires considerable time and effort, as well as dedicated facilities, expensive manikins, and trained instructors, thereby imposing significant material and human resource burdens [8]. Moreover, the number of students who can participate in a simulation session simultaneously is limited [6], and institutions with large class sizes face challenges in widely implementing this approach. Therefore, there is a need to explore alternative and efficient methods for teaching physical assessment.
The information obtained through physical examination provides specific cues that serve as the starting point for clinical reasoning [9]. Rather than separating physical assessment from clinical reasoning, integrating these two areas in the learning process is expected to enhance students’ practical judgment skills. Clinical reasoning in nursing is defined as the process through which nurses collect and interpret information based on cues, understand patients’ conditions and problems, plan and implement nursing interventions, and evaluate and reflect on outcomes [9]. Physical assessment and clinical reasoning share many commonalities: both involve collecting and interpreting information about a patient’s condition and making decisions regarding nursing care, which require observation, interpretation, and judgment skills [1,9]. By learning these processes in an integrated manner, students can move beyond mere observation of physical findings to logical analysis of the information, identification of patient problems, and development of appropriate nursing care plans.
A “cue” refers to an identifiable physiological or psychosocial change experienced by a patient and includes patient information and recalled knowledge obtained through history-taking and assessment [10]. Tanner positioned these cues, referred to as “noticing,” as the foundation of clinical reasoning [11]. New graduate nurses often collect excessive amounts of information due to underdeveloped skills in distinguishing relevant from irrelevant data when attempting to accurately assess patient conditions and situations [12]. This tendency is also seen in undergraduate nursing students, who frequently struggle to identify key information among a large volume of data, leading to unfocused assessments and disruption of the clinical reasoning process. Although simulation-based education has been explored to improve students’ clinical reasoning, there is limited evidence regarding alternative, low-cost instructional methods that integrate cue recognition with physical assessment in case-based learning [13]. In particular, few studies have rigorously examined whether providing targeted cues during group discussions can enhance the clinical reasoning process in undergraduate nursing education [14].
As one approach to addressing this issue, the present study aimed to examine the effect of using pre-assignment work to help undergraduate nursing students obtain cues during a case-based physical assessment on their clinical reasoning ability.
Objective
This study aimed to examine the effects of using pre-assignment work and presenting specific cues in a case on the clinical reasoning skills of second-year undergraduate nursing students during physical assessment by comparing an intervention group that received specific cues with a control group that did not.
MATERIALS AND METHODS
Study Design
This study employed a parallel-group, two-arm, randomized controlled trial (RCT) design conducted to evaluate the effectiveness of a cue-based educational intervention on clinical reasoning skills in physical assessment. The study was implemented as part of an existing physical assessment course at a private women’s university in western Japan.
The design and reporting followed the CONSORT 2025 guidelines for randomized trials [15] in educational research. Intervention and control groups received structured group learning sessions, with only the intervention group being exposed to specific case-related cues. Outcome assessments included both subjective (self-assessment scale) and objective (task-based) measures.
Conceptual Framework
Figure1 presents a conceptual diagram illustrating the process of clinical reasoning and the intervention applied during physical assessment. In this study, the process of clinical reasoning was defined as “the sequence from information collection regarding a case to the planning of interventions (nursing care).”
Participants in the intervention group progressed through the assignments by selecting and recording the information they deemed necessary, based on the “cues” presented by the researcher and the content of their pre-assignment work. This study aimed to examine how the provision of “cues” influenced the subsequent quality of information interpretation, patient understanding, and intervention planning.
The evaluation was structured to verify the effect of the intervention through both subjective and objective assessments, including scores from the Clinical Reasoning Skills Self-Assessment Scale (CRSS), and the content of students’ interviews, physical examinations, and nursing care descriptions related to the case.
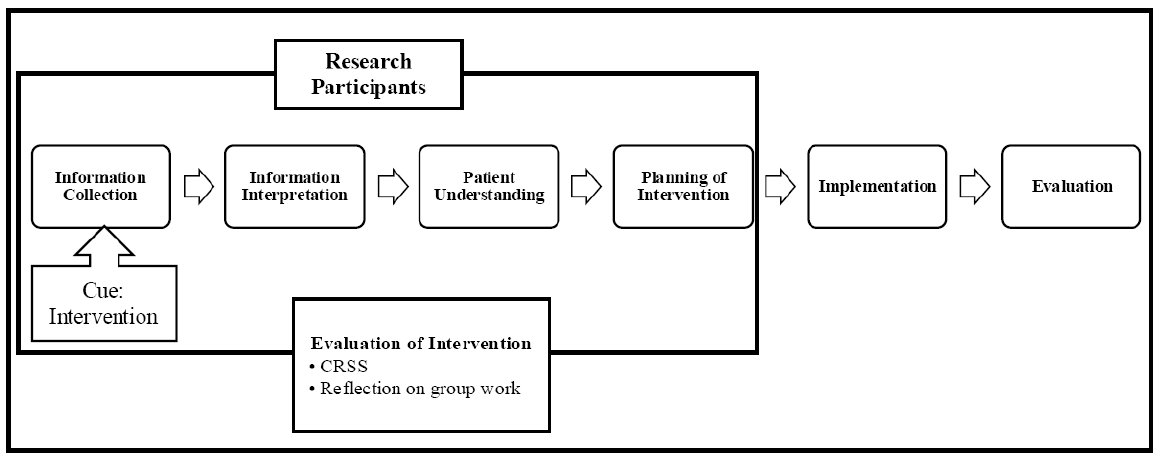
This diagram outlines the clinical reasoning process from information collection to evaluation.
The intervention group received cues to support reasoning during physical assessment, and outcomes were evaluated using CRSS and reflection.
CRSS = Clinical Reasoning Skills Self-Assessment Scale.
Figure 1. Conceptual Framework
Operational Definition
Cue: A cue refers to an identifiable physiological or psychosocial change experienced by a patient and includes patient information, and the recall of related knowledge obtained through history-taking and assessment [10]. In this study, a cue is operationally defined as the judgment material obtained by students through the use of pre-work and thinking based on mechanisms and rationales, enabling them to appropriately assess the condition of the case.
Sample Size
The sample size was calculated to compare the CRSS scores between the intervention and control groups at the end of the study. Based on an alpha level (α) of 0.05, a power (1-β) of 0.80, and a medium effect size of 0.7 (Cohen’s d), a minimum of 35 participants per group was required. Therefore, the minimum total sample size needed was 70 participants. The effect size was estimated based on results from previous similar educational intervention studies in nursing. Particularly, the total sample was expanded to 94 patients to reduce the possible bias due to missing information or data loss. In this way, 47 patients were assigned to each group. The sample size calculation was conducted using G*Power [16].
Study Population
The study was conducted at a private women’s university located in western Japan. The participants were second-year undergraduate students enrolled in the university’s Department of Nursing. All students were female by institutional policy.
Recruitment and Consent Procedure
Seven days prior to the study session, the researchers distributed an informed consent form and provided both verbal and written explanations of the study’s objectives and procedures. Students were instructed to submit the completed consent form into a designated collection box at the university by the day before the session. Submission of the form was considered as consent to participate in the study.
Exclusion Criteria
Students were excluded if they (1) were absent, arrived late, or left early on the day of the session; (2) failed to complete the required pre-assignment; or (3) submitted incomplete responses on the CRSS.
Group Allocation
The randomization sequence was generated by the researcher using a computer-generated random number table with a 1:1 allocation ratio. To ensure allocation concealment, group assignments were placed in opaque, sealed envelopes and numbered sequentially. After each participant submitted their informed consent form, a separate coordinator-who was not involved in enrollment, intervention delivery, or outcome assessment-opened the envelope corresponding to the participant. This procedure ensured that neither the personnel responsible for enrollment nor the participants had prior knowledge of group assignments. Participants were blinded to their assigned group throughout the study period. However, due to the nature of the intervention, researchers were not blinded.
This study was not registered in a clinical trial registry, as it involved an educational intervention implemented within an existing university course and did not fall under ICMJE [17] or CONSORT [15] requirements for mandatory trial registration. No changes were made to the original study protocol during the course of the study.
Pre-assignment
To prepare students for the group case study session, a pre-assignment related to heart failure was distributed 14 days in advance. The assignment consisted of six questions focusing on the pathophysiology, assessment, and nursing care of a patient suspected of heart failure (see Appendix Table A1). Students were instructed to complete the assignment individually at home and bring it with them on the day of the session. This pre-assignment was designed to encourage students to review fundamental knowledge about heart failure and to consider appropriate examination methods and nursing interventions. Given the increasing global prevalence of heart failure, particularly in aging populations [18-20], emphasis was placed on recognizing symptoms and planning care based on clinical reasoning.
Study Procedures
The study was conducted on July 11, 2024, during scheduled lectures on physical assessment. Prior to participation, all students had completed 540 minutes of practical training in interview techniques and physical assessments of the respiratory, cardiovascular, gastrointestinal, musculoskeletal, and neurological systems.
Intervention
The intervention and control groups conducted the group case study sessions at separate times and in different classrooms to avoid contamination. Each session was facilitated by four researchers, all of whom were experienced nursing educators with training in physical assessment and case-based learning. To ensure consistency across sessions, all researchers referred to a common set of verbal cues prepared in advance (see Appendix Table A2), which guided the timing and content of each task. Additionally, a pre-session briefing was conducted among all researchers to align their understanding of the procedures, clarify roles, and ensure a uniform approach to facilitation. Both groups received a pre-assignment related to heart failure and completed it individually before the session. Based on previous findings suggesting that collaborative learning enhances clinical reasoning skills among nursing students [21], students worked in teams of 5-6 during the 60-minute sessions and completed six tasks sequentially using written case materials (see Appendix Table A3). Each group’s responses were recorded on standardized answer sheets. In the intervention group, specific cues were presented by the researcher prior to each task to support students’ clinical reasoning. These cues guided students to apply their pre-assignment knowledge and consider pathophysiological mechanisms. For example, prior to the Inspection task, students were asked: “Think about the visible changes or symptoms caused by heart failure.” A complete list of the cues provided is shown in Appendix Table A2.
Outcome Measures
The outcomes were evaluated using both subjective and objective measures.
CRSS Scores
Subjective evaluation of clinical reasoning skills was conducted using the Japanese version of the CRSS [22]. The original CRSS is a 26-item, five-point Likert scale developed to assess clinical reasoning processes in nursing [23]. The Japanese version has demonstrated high reliability (Cronbach’s alpha = 0.95) and acceptable content validity (CVI = 0.78) among nurses and undergraduate nursing students [22]. In the present study, 12 items specifically related to behaviors in direct clinical practice-such as implementing patient care, selecting appropriate interventions, and evaluating care outcomes-were excluded based on the consensus of the research team, as the intervention did not involve actual patient care or clinical settings. Consequently, 14 items that assessed cognitive and judgmental aspects of reasoning, including data gathering, interpretation, and planning, were retained for analysis. Although the original CRSS is multidimensional in design, the retained items in this study primarily reflect the cognitive components of clinical reasoning. The original Japanese version demonstrated acceptable content validity (CVI= 0.78); however, the modified 14-item version used in this study has not undergone a separate content validity evaluation. A total score was calculated by summing the responses to the 14 selected items (score range: 14-70), with higher scores indicating greater perceived clinical reasoning ability. The internal consistency of the modified scale was confirmed in this study, yielding a Cronbach’s alpha of 0.94. The use of the Japanese version of the CRSS was approved by the original developers.
Task Responses
Objective evaluation was conducted based on the written responses of each group to the six case-based tasks. Two evaluators-members of the research team with expertise in nursing education-assessed the specificity and appropriateness of the proposed nursing care using a predefined rubric developed for this study. The rubric included criteria such as: Alignment with the patient’s symptoms and condition, Clarity and feasibility of the proposed care, and Use of patient-specific data rather than generalized interventions. Prior to analysis, the evaluators reviewed several sample responses and calibrated their judgments through discussion to ensure consistency. Although the evaluators were members of the research team, the group allocation of each response was blinded during the assessment process to minimize potential bias.
Statistical Analysis
The CRSS scores for the intervention and control groups were confirmed to be non-normally distributed using the Shapiro-Wilk test. Therefore, the 15-item scores were summarized using the median and interquartile range. The Mann-Whitney U test was used to compare the CRSS scores between the intervention and control groups, and the Wilcoxon signed-rank test was used to compare pre-and post-session scores within each group. For the Mann-Whitney U test, mean rank values were reported in addition to p-values, particularly for items where the medians were equal between groups. For the Wilcoxon signed-rank test, we reported both the test statistic (W) and standardized Z values alongside p-values to enhance the clarity and rigor of the within-group comparisons. A two-tailed p-value less than the 5% significance level was considered statistically significant. All statistical analyses were performed using SPSS, Version 26.0 (IBM Corp, Armonk, NY, USA). Although students worked in small groups of 5-6 during the sessions, the statistical analysis did not account for potential cluster effects. This was because the CRSS was completed independently by each participant, and all instructional materials and procedures were standardized across groups to minimize variability related to group dynamics. Missing data were handled by complete case analysis; participants with incomplete CRSS responses were excluded from the final analysis.
Narrative Responses
Statistical analysis was not performed on the narrative responses. Instead, the responses were analyzed qualitatively using a basic content comparison approach. Two researchers independently reviewed the written narratives from each group and compared the content in terms of specificity and appropriateness of the proposed nursing care interventions. Discrepancies in interpretation were discussed and resolved through consensus to enhance the credibility of the analysis. While a formal thematic analysis was not conducted, this comparative review provided insights into differences in the depth and relevance of reasoning between groups. The lack of a formal qualitative methodology is acknowledged as a limitation of this study and is addressed in the limitations section.
Ethical Considerations
This study was approved by the Senri Kinran University Institutional Review Board (IRB; Approval Number: K24-007 dated May 27, 2024). Participants were informed that their participation and cooperation in the study were entirely voluntary and that non-participation would not result in any disadvantage. They were also informed, both in writing and verbally, that the study would be conducted during the lecture of the Physical Assessment course, and that their participation or non-participation would have no impact on their course grades. In addition, participants were advised that if they felt that their participation influenced their grades or if they perceived any misconduct or harassment related to the study, they could consult with the Harassment Advisory Committee established within the university.
For students who chose not to participate in the study, it was explained that while they would attend the lecture together with other students, they were not required to complete the CRSS and their data would not be included in the study analysis. Due to group assignment logistics, some students who declined to participate were included in the same groups as control group participants. These students were also given the supplementary exercise conducted for the intervention group after the completion of the study to ensure that no disadvantage would arise from their non-participation. Similarly, to prevent any disadvantage, participants assigned to the control group were provided with the same instructional content used for the intervention group after the study was completed.
RESULTS
Participant Flow
A total of 107 second-year undergraduate nursing students were eligible to participate. Of these, 94 students (87.8%) consented to take part in the study. Among those who consented, 93 were 20 years old and one was 22 years old. Participants were randomly assigned to either the intervention group (n = 47) or the control group (n = 47). However, one student in the control group was excluded due to late arrival, resulting in 93 students (86.9%) who completed the intervention as planned-47 in the intervention group and 46 in the control group. Each group was further subdivided into teams of five to six students, resulting in nine subgroups per condition. Due to missing responses on the post-session CRSS, three participants in the intervention group and four in the control group were excluded from the final analysis. Therefore, CRSS data from 44 participants in the intervention group and 42 in the control group were included in the analysis. The flow of participant enrollment, exclusion, allocation, and final inclusion for analysis is illustrated in Figure 2.
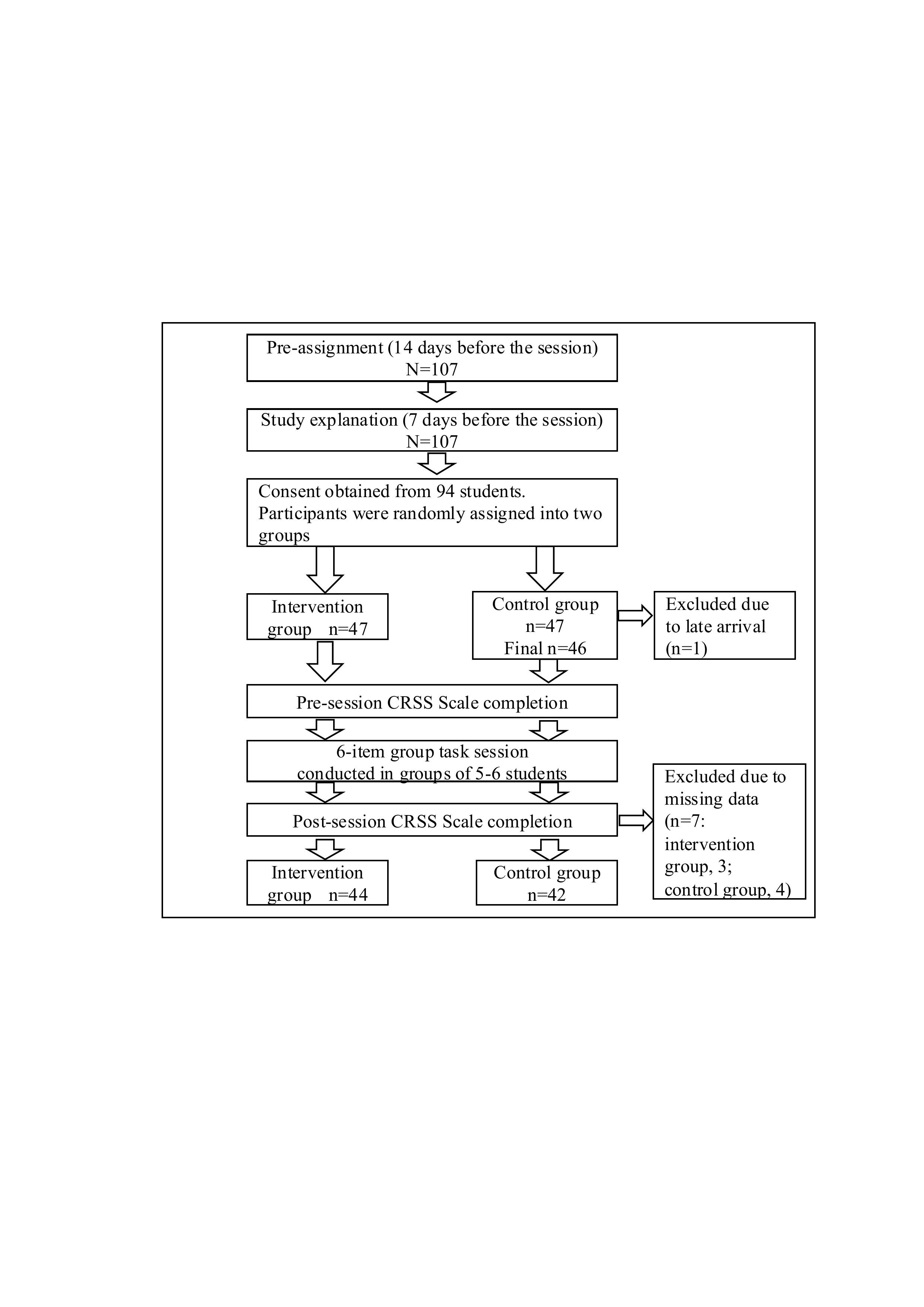
107 students were recruited; 94 consented and were assigned to two groups. After exclusions, CRSS data from 86 participants were analyzed (intervention: 44, control: 42).
CRSS = Clinical Reasoning Skills Self-Assessment Scale.
Figure 2. Study Flow and the Number of Study Participants.
Comparison of the CRSS Scores
The pre-session scores of the CRSS Scale showed no significant differences between the intervention and control groups on all 15 items. However, the post-session scores of the intervention group were significantly higher than those of the control group on ten items (Table 1, 2)
|
No. |
Question items |
Intervention group (n = 44) |
Control group (n = 42) |
Mean Rank (Intervention) |
Mean Rank (Control) |
P value |
|
1 |
I can apply the interview and physical examination to assess the patient’s condition. |
3.00 (2.25-4.00) |
3.00 (3.00-4.00) |
43.60 |
43.39 |
0.96 |
|
2 |
I can interpret the information collected. |
4.00 (3.00-4.00) |
3.50 (3.00-4.00) |
44.51 |
42.44 |
0.67 |
|
3 |
I can recognize the need for more information. |
3.00 (3.00-4.00) |
3.00 (2.75-4.00) |
46.86 |
39.98 |
0.16 |
|
4 |
I can distinguish between necessary and unnecessary information. |
3.00 (3.00-4.00) |
3.00 (2.00-4.00) |
44.50 |
42.45 |
0.68 |
|
5 |
I can anticipate how my decisions will affect the patient’s condition. |
4.00 (3.00-4.00) |
3.00 (2.00-4.00) |
47.65 |
39.15 |
0.09 |
|
6 |
I can assess the cause and effect relationships in the patient’s condition. |
3.00 (2.25-4.00) |
3.00 (3.00-3.00) |
45.64 |
41.26 |
0.38 |
|
7 |
I can recognize the need for patient care. |
4.00 (4.00-4.00) |
4.00 (3.75-4.00) |
43.98 |
43.00 |
0.82 |
|
8 |
I can identify nursing problems. |
3.00 (3.00-4.00) |
3.00 (3.00-4.00) |
42.78 |
44.25 |
0.76 |
|
9 |
I can notice changes in the patient’s condition. |
4.00 (4.00-4.00) |
4.00 (3.00-4.00) |
46.74 |
40.11 |
0.14 |
|
10 |
I can prioritize the patient’s needs. |
3.00 (3.00-4.00) |
3.00 (3.00-4.00) |
40.93 |
46.19 |
0.28 |
|
11 |
I can establish nursing plans. |
3.00 (2.00-4.00) |
3.00 (3.00-3.00) |
42.95 |
44.05 |
0.83 |
|
12 |
I can plan the necessary care. |
3.50 (3.00-4.00) |
3.00 (3.00-4.00) |
44.55 |
42.40 |
0.67 |
|
13 |
I can determine patient care. |
3.00 (2.25-4.00) |
3.00 (3.00-4.00) |
44.17 |
42.80 |
0.78 |
|
14 |
I can determine patient care quickly. |
3.00 (2.00-4.00) |
3.00 (2.00-3.00) |
45.16 |
41.76 |
0.50 |
|
15 |
Total |
49.00 (40.00-51.00) |
46.00 (41.0-50.25) |
45.50 |
41.40 |
0.44 |
Note 1: The scores for the question items and the total score are presented as medians (interquartile range).
Note 2: The data were analyzed using the Mann-Whitney U test.
Table 1. Comparison of the Pre-session Scores of the CRSS Between the Intervention and Control Groups.
|
No. |
Question items |
Intervention group (n = 44) |
Control group (n = 42) |
Mean Rank (Intervention) |
Mean Rank (Control) |
P value |
|
1 |
I can apply the interview and physical examination to assess the patient’s condition. |
4.00 (4.00-5.00) |
4.00 (4.00-4.00) |
48.17 |
38.61 |
0.039* |
|
2 |
I can interpret the information collected. |
4.00 (4.00-5.00) |
4.00 (4.00-4.00) |
49.07 |
37.67 |
0.014* |
|
3 |
I can recognize the need for more information. |
4.00 (4.00-5.00) |
4.00 (3.00-4.00) |
50.90 |
35.75 |
0.002* |
|
4 |
I can distinguish between necessary and unnecessary information. |
4.00 (4.00-4.00) |
4.00 (3.00-4.00) |
49.20 |
37.52 |
0.015* |
|
5 |
I can anticipate how my decisions will affect the patient’s condition. |
4.00 (4.00-5.00) |
4.00 (3.00-4.00) |
49.09 |
37.64 |
0.019* |
|
6 |
I can assess the cause and effect relationships in the patient’s condition. |
4.00 (4.00-5.00) |
4.00 (3.00-4.00) |
49.32 |
37.40 |
0.016* |
|
7 |
I can recognize the need for patient care. |
4.00 (4.00-5.00) |
4.00 (4.00-5.00) |
47.72 |
39.08 |
0.076 |
|
8 |
I can identify nursing problems. |
4.00 (3.00-5.00) |
4.00 (3.00-4.00) |
47.51 |
39.30 |
0.103 |
|
9 |
I can notice changes in the patient’s condition. |
4.00 (4.00-5.00) |
4.00 (3.00-4.00) |
50.27 |
36.40 |
0.005* |
|
10 |
I can prioritize the patient’s needs. |
4.00 (4.00-5.00) |
3.00 (3.00-4.00) |
47.36 |
39.45 |
0.111 |
|
11 |
I can establish nursing plans. |
4.00 (4.00-4.75) |
4.00 (3.00-4.00) |
48.42 |
38.35 |
0.040* |
|
12 |
I can plan the necessary care. |
4.00 (4.00-5.00) |
4.00 (3.00-4.00) |
48.07 |
38.71 |
0.062 |
|
13 |
I can determine patient care. |
4.00 (3.00-4.00) |
4.00 (3.00-4.00) |
47.75 |
39.05 |
0.076 |
|
14 |
I can determine patient care quickly. |
4.00 (4.00-4.00) |
3.00 (3.00-4.00) |
48.72 |
38.04 |
0.03* |
|
15 |
Total |
60.00 (53.50.-63.00) |
52.00 (48.00-59.00) |
51.84 |
34.76 |
0.002* |
Note 1: The scores for the question items and the total score are presented as medians (interquartile range).
Note 2: The data were analyzed using the Mann-Whitney U test. Significant differences are indicated by P < 0.05*.
Table 2. Comparison of the Post-session Scores of the CRSS Between the Intervention and Control Groups.
In the between-group comparisons, no significant differences were found between the intervention and control groups in any of the 15 items before the session (Table 3).
However, after the session, the intervention group scored significantly higher than the control group on 10 out of the 15 items (Table 4).
|
No. |
Question items |
Pre-session |
Post-session |
Test Statistic (W) |
Z value |
P value |
|
1 |
I can apply the interview and physical examination to assess the patient’s condition. |
3.00 (2.25-4.00) |
4.00 (4.00-5.00) |
498.00 |
-4.50 |
< 0.001* |
|
2 |
I can interpret the information collected. |
4.00 (3.00-4.00) |
4.00 (4.00-5.00) |
221.00 |
-3.15 |
0.002* |
|
3 |
I can recognize the need for more information. |
3.00 (3.00-4.00) |
4.00 (4.00-5.00) |
549.00 |
-5.01 |
< 0.001* |
|
4 |
I can distinguish between necessary and unnecessary information. |
3.00 (3.00-4.00) |
4.00 (4.00-4.00) |
423.00 |
-4.73 |
< 0.001* |
|
5 |
I can anticipate how my decisions will affect the patient’s condition. |
4.00 (3.00-4.00) |
4.00 (4.00-5.00) |
232.50 |
-2.96 |
0.003* |
|
6 |
I can assess the cause and effect relationships in the patient’s condition. |
3.00 (2.25-4.00) |
4.00 (4.00-5.00) |
506.00 |
-4.70 |
< 0.001* |
|
7 |
I can recognize the need for patient care. |
4.00 (4.00-4.00) |
4.00 (4.00-5.00) |
293.50 |
-3.76 |
< 0.001* |
|
8 |
I can identify nursing problems. |
3.00 (3.00-4.00) |
4.00 (3.00-5.00) |
425.00 |
-4.22 |
< 0.001* |
|
9 |
I can notice changes in the patient’s condition. |
4.00 (4.00-4.00) |
4.00 (4.00-5.00) |
277.00 |
-4.00 |
< 0.001* |
|
10 |
I can prioritize the patient’s needs. |
3.00 (3.00-4.00) |
4.00 (4.00-5.00) |
441.00 |
-4.54 |
< 0.001* |
|
11 |
I can establish nursing plans. |
3.00 (2.00-4.00) |
4.00 (4.00-4.75) |
528.00 |
-5.13 |
< 0.001* |
|
12 |
I can plan the necessary care. |
3.50 (3.00-4.00) |
4.00 (4.00-5.00) |
456.00 |
-4.21 |
< 0.001* |
|
13 |
I can determine patient care. |
3.00 (2.25-4.00) |
4.00 (3.00-4.00) |
419.00 |
-3.99 |
< 0.001* |
|
14 |
I can determine patient care quickly. |
3.00 (2.00-4.00) |
4.00 (4.00-4.00) |
496.00 |
-5.15 |
< 0.001* |
|
15 |
Total |
49.00 (40.00-51.00) |
60.00 (53.50.-63.00) |
939.00 |
-5.63 |
< 0.001* |
Note 1: The scores for the question items and the total score are presented as medians (interquartile range).
Note 2: The data were analyzed using the Wilcoxon signed-rank sum test. Significant differences are indicated by P < 0.05*.
Table 3. Comparison of the Pre-and Post-session Scores of the CRSS of the Intervention Group.
|
No. |
Question items |
Pre-session |
Post-session |
Test Statistic (W) |
Z value |
P value |
|
1 |
I can apply the interview and physical examination to assess the patient’s condition. |
3.00 (3.00-4.00) |
4.00 (4.00-4.00) |
345.00 |
-3.97 |
< 0.001* |
|
2 |
I can interpret the information collected. |
3.50 (3.00-4.00) |
4.00 (4.00-4.00) |
207.00 |
-2.24 |
0.02* |
|
3 |
I can recognize the need for more information. |
3.00 (2.75-4.00) |
4.00 (3.00-4.00) |
381.00 |
-4.28 |
< 0.001* |
|
4 |
I can distinguish between necessary and unnecessary information. |
3.00 (2.00-4.00) |
4.00 (3.00-4.00) |
234.00 |
-3.17 |
0.001* |
|
5 |
I can anticipate how my decisions will affect the patient’s condition. |
3.00 (2.00-4.00) |
4.00 (3.00-4.00) |
264.00 |
-2.84 |
0.004* |
|
6 |
I can assess the cause and effect relationships in the patient’s condition. |
3.00 (3.00-3.00) |
4.00 (3.00-4.00) |
391.50 |
-3.40 |
0.001* |
|
7 |
I can recognize the need for patient care. |
4.00 (3.75-4.00) |
4.00 (4.00-5.00) |
117.00 |
-2.02 |
0.04* |
|
8 |
I can identify nursing problems. |
3.00 (3.00-4.00) |
4.00 (3.00-4.00) |
253.00 |
-2.69 |
0.007* |
|
9 |
I can notice changes in the patient’s condition. |
4.00 (3.00-4.00) |
4.00 (3.00-4.00) |
109.00 |
-2.23 |
0.02* |
|
10 |
I can prioritize the patient’s needs. |
3.00 (3.00-4.00) |
3.00 (3.00-4.00) |
149.00 |
-2.30 |
0.02* |
|
11 |
I can establish nursing plans. |
3.00 (3.00-3.00) |
4.00 (3.00-4.00) |
318.50 |
-3.81 |
< 0.001* |
|
12 |
I can plan the necessary care. |
3.00 (3.00-4.00) |
4.00 (3.00-4.00) |
348.50 |
-3.49 |
< 0.001* |
|
13 |
I can determine patient care. |
3.00 (3.00-4.00) |
4.00 (3.00-4.00) |
288.00 |
-2.98 |
0.003* |
|
14 |
I can determine patient care quickly. |
3.00 (2.00-3.00) |
3.00 (3.00-4.00) |
295.00 |
-3.71 |
< 0.001* |
|
15 |
Total |
46.00 (41.0-050.25) |
52.00 (48.00-59.00) |
826.5 |
-4.69 |
< 0.001* |
Note 1: The scores for the question items and the total score are presented as medians (interquartile range).
Note 2: The data were analyzed using the Wilcoxon signed-rank sum test. Significant differences are indicated by P < 0.05*.
Table 4. Comparison of the Pre-and Post-session Scores of the CRSS of the Control Group.
Narrative Responses
During the session, participants in both the intervention and control groups provided narrative responses to a six-task group assignment.
For five of the tasks-Interview, Inspection, Palpation, Percussion, and Auscultation-no notable differences were observed between the two groups. Therefore, the common themes identified from both groups are summarized in Appendix Tables A4-A8. Appendix Tables A4-A8 present representative excerpts of the written narrative responses from both the intervention and control groups for the five physical assessment tasks. These tables illustrate how students applied clinical reasoning to assess physical signs and symptoms through written responses.
However, clear differences emerged between the intervention and control groups in the sixth task, which required students to propose nursing care plans for the simulated patient. Table 5 summarizes these responses, categorized into common responses and those unique to each group.
The intervention group provided more specific nursing care plans based on the patient’s symptoms. Example responses included: “Have a lap blanket available for the patient during wheelchair transfer to address cold extremities.” “Accompany the patient to the tests/examinations, considering palpitations and shortness of breath.”
In contrast, the control group tended to offer general nursing care responses commonly associated with heart failure rather than case-specific interventions. Example responses included: “Provide guidance and management regarding restrictions on salt and water intake.”
|
Responses |
|
Common responses from the intervention and control groups |
|
Measure vital signs (respiration, percutaneous oxygen saturation, pulse, blood pressure, respiratory rate and body temperature). |
|
Ensure comfortable positions (Fowler’s position or the orthopneic position). |
|
Transfer the patient in a wheelchair due to shortness of breath and edema. |
|
Prepare and administer oxygen therapy. |
|
Explain what to expect before and after the tests/examinations and provide psychological care to reduce the patient’s anxiety. |
|
Provide care for edema. |
|
Responses unique to the intervention group |
|
Accompany the patient to the tests/examinations, considering palpitations and shortness of breath. |
|
As emotional support, ask the patient if they are cold or how they are feeling. |
|
Prepare a vomit disposal bag. |
|
Check for changes in the patient’s physical condition, facial color, and overall appearance during the examination. |
|
Used closed questions to make it easier for the patient to respond. |
|
Have a lap blanket available for the patient during transfer in a wheelchair to help with cold extremities. |
|
Responses unique to the control group |
|
Provide guidance and management regarding restrictions on salt and fluid intake. |
|
Provide nutritional guidance, including limiting indulgences and alcohol consumption. |
|
Provide bathing assistance. |
|
Perform measures to prevent pressure ulcers. |
|
Explain appropriate actions when symptoms worsen. |
|
Provide care for delirium. |
|
Provide rehabilitation exercise for range of motion. |
|
Provide guidance on lifestyle after discharge and outpatient follow-ups. |
|
Mange fluid balance by monitoring the body weight and urine output. |
|
Perform medication management and administration, including monitoring the effects and side effects. |
Table 5. Narrative Responses Provided by the Intervention and Control Groups: Nursing Care
DISCUSSION
This study aimed to examine the effectiveness of using pre-assignment work and specific cues in a case-based group learning session to enhance the clinical reasoning skills of undergraduate nursing students in physical assessment. The findings revealed two key outcomes that support the value of this educational approach.
First, although the pre-session scores of the CRSS Scale between the intervention and control groups showed no significant difference, the post-session scores of the intervention group were significantly higher on 10 items compared to the control group. The lack of significant differences in pre-session CRSS scores between groups supports the internal validity of the findings by indicating comparable baseline levels of clinical reasoning skills. The intervention group scored significantly higher on items related to information collection (No. 1) and interpretation (Nos. 2 and 6), problem identification (No. 9), and goal setting (Nos. 11 and 14).
Effective clinical reasoning requires nurses to accurately collect relevant cues and take appropriate action for the right patient, at the right time, and for the right reason [24]. Our findings suggest that the participants in the intervention group self-assessed improvements in their ability to collect and interpret information by utilizing the pre-assignment and interpreting the specific cues provided by the researcher as prompts for clinical reasoning. Furthermore, the significantly higher post-session scores in the intervention group indicate that the participants were able to recognize improvements not only in information collection and interpretation but also in planning appropriate nursing care interventions tailored to the patient’s needs. These results imply that the intervention strengthened their ability to link patient information to problem identification and appropriate decision-making.
These findings are consistent with previous research indicating that collaborative and cue-based learning strategies can enhance clinical reasoning skills among nursing students. For example, Levett-Jones et al. [10] found that structured case-based learning promoted deeper analysis and more accurate clinical judgments. However, whereas many previous studies focused primarily on simulation-based or full-scale clinical scenarios, the present study demonstrates that similar improvements in clinical reasoning can be achieved through brief, structured interventions embedded in routine coursework. This suggests that even short, well-designed activities can meaningfully contribute to students’ development of clinical reasoning competencies.
Second, regarding the task responses, there were no notable differences between the intervention and control groups in the Interview, Inspection, Palpation, Percussion, and Auscultation tasks. This result is likely because physical assessment skills are generally acquired through repeated practice [3], and both groups had already completed basic training in these skills before participating in the study. However, significant differences emerged in the Nursing Care task.
Participants in the intervention group provided more specific and patient-centered nursing care plans based on the symptoms presented in the case. For example, their responses included: “Have a lap blanket available for the patient during wheelchair transfer to address cold extremities.” “Accompany the patient to the tests/ examinations, considering palpitations and shortness of breath.”
In contrast, the control group tended to offer generalized nursing interventions typical for heart failure patients, without tailoring their care to the specific symptoms of the case. Example responses included: “Provide guidance and management regarding restrictions on salt and water intake.”
This difference suggests that participants in the control group lacked the ability to accurately identify and prioritize patient-specific cues, which was also reflected in their CRSS scores after the session. Supporting nursing students to focus on relevant cues, understand patient conditions and problems, and appreciate how these cues influence clinical judgments and patient outcomes is essential for the development of clinical reasoning skills [25]. In this study, specific cues provided by the researcher helped guide the intervention group participants to focus on the most relevant signs and symptoms, interpret them logically, and develop more targeted and appropriate nursing care interventions. The success of this intervention highlights the importance of structured support strategies in nursing education to bridge the gap between physical assessment findings and effective clinical decision-making. While this study demonstrated immediate improvements in clinical reasoning skills and nursing care specificity following the intervention, it did not assess long-term retention or the transfer of these skills to clinical practice. The sustainability of the observed learning gains and their impact on real-world nursing settings remain unknown. Future studies should incorporate follow-up assessments to evaluate whether these improvements are maintained over time and translated into clinical competence.
Implications for Practice and Future Research
The intervention used in this study, which encouraged undergraduate nursing students to utilize pre-assignment work and obtain specific cues during physical assessment, demonstrated potential for effectively fostering clinical reasoning skills even in settings with limited facilities and time.
This approach could be feasibly integrated into existing lecture-based curricula without the need for high-cost simulation equipment, making it particularly suitable for institutions with limited resources. For example, instructors can implement similar cue-enhanced case discussions in small group settings using printed case materials and structured prompts to guide clinical reasoning.
Future research should examine the long-term impact of this approach on knowledge retention and clinical performance. Additionally, comparative studies across multiple institutions and varying educational contexts are needed to assess the generalizability and scalability of the intervention. Investigating the effectiveness of this method in combination with simulation-based or OSCE-style assessments may also provide insights into optimizing nursing education strategies.
CONCLUSION
This study investigated the effectiveness of combining pre-assignment work with the provision of specific cues during a case-based group learning session to enhance clinical reasoning skills in undergraduate nursing students.
The findings indicate that the intervention group demonstrated significantly greater improvements in clinical reasoning ability compared to the control group, as evidenced by higher post-session scores on 10 items of the CRSS Scale. While no notable differences were observed in task responses related to Interview, Inspection, Palpation, Percussion, and Auscultation, the Nursing Care task revealed important distinctions. Students in the intervention group were more likely to identify relevant information and formulate specific, patient-centered care plans, suggesting a deeper understanding of the case context.
Overall, the results suggest that integrating structured pre-assignment learning with cue-based support can effectively foster clinical reasoning skills. This approach may be particularly beneficial in educational environments where access to simulation-based instruction is limited, offering a practical and scalable strategy to strengthen students’ reasoning capabilities in physical assessment.
Limitations
This study has several limitations. First, it was conducted at a single private women’s university, potentially limiting generalizability due to contextual factors such as instructional style. Additionally, gender-related differences in clinical reasoning ability and learning preferences were not examined. These differences may influence how students engage with cue-based learning strategies, and therefore, the applicability of the results to mixed-gender or male student populations remains uncertain.
Second, the study assessed only immediate post-session outcomes; thus, the long-term retention and transfer to clinical practice remain unknown.
Third, while narrative responses were qualitatively reviewed, the absence of a formal thematic or content analysis may have limited the depth of qualitative insights.
Fourth, the sample size calculation followed a parametric approach based on an independent samples t-test using Cohen’s d index, which is commonly employed in educational intervention research.
We acknowledge that Cohen’s d is not the standard effect size for non-parametric tests like the Mann-Whitney U test used in this study. However, due to the lack of established tools supporting a priori power analysis for non-parametric effect sizes such as η² or rank-biserial correlation, we used Cohen’s d as a practical approximation.
Finally, the analysis did not account for potential clustering effects or use an intention-to-treat approach, which may introduce bias and affect the robustness of the findings.
Conflict of interest
The authors declare that they have no conflicts of interest.
Funding
This study was funded by a 2024 Cardiovascular Disease Nursing Research Grant (No. 12) from the Japan Cardiovascular Research Foundation.
Authors contribution
Author 1: Akifumi Maeda, MNS, RN, Lecturer, Faculty of Nursing, Senri Kinran University, Osaka, Japan, Contribution: Conception, design, supervision, funding, materials, data collection and processing, analysis and interpretation, literature review, writing, and critical review. E-mail: ak-maeda@cs.kinran.ac.jp; ORCID; http://orcid.org/0000-0002-2628-2224
Author 2: Akemi Hirao, PhD, RN, Professor, Faculty of Nursing, Senri Kinran University, Osaka, Japan, Contribution: Analysis and interpretation, literature review, writing, and critical review. E-mail: a-hirao@cs.kinran.ac.jp; ORCID: http://orcid.org/0009-0004-2902-5372
Author 3: Akiko Sugimoto, MNS, RN, Assistant Professor, Faculty of Nursing, Senri Kinran University, Osaka, Japan, Contribution: Conception, design, supervision, literature review, and writing. E-mail: a-sugimoto@cs.kinran.ac.jp; ORCID: http://orcid.org/0009-0003-0506-8370
Author 4: Motoko Hori, MNS, RN, Assistant Professor, Faculty of Nursing, Senri Kinran University, Osaka, Japan, Contribution: Conception, design, supervision, literature review, and writing. E-mail: m-hori@cs.kinran.ac.jp; ORCID; http://orcid.org/0000-0003-0864-2473
Acknowledgment
The authors wish to thank Nakaba Cosley for reviewing and providing English language editing on an earlier draft of the manuscript. We also express our sincere gratitude to the developers of the Japanese version of the CRSS for granting us permission to adapt and use the instrument in this study.
AI tools Usage
During the preparation of this manuscript, ChatGPT (OpenAI, https://openai.com/chatgpt) was utilized to assist with the initial English translation of the Japanese manuscript into English. The authors critically reviewed, edited, and validated all AI-generated outputs to ensure their accuracy, clarity, and appropriateness for scholarly publication. Additionally, professional English language editing was performed by Nakaba Cosley to finalize the manuscript. Importantly, no parts of the research data, study results, analysis, or scientific content were generated or altered using AI tools.
Appendix
|
No. |
Pre-assignment |
|
1 2 3 4 5 6 |
What diseases can cause heart failure? What symptoms are associated with failure of the right and left heart? What mechanisms cause those symptoms? What types of physical examinations are performed to address these symptoms? What nursing care can be provided to patients with heart failure? What tests are needed to diagnose and determine the treatment of heart failure? |
Table A1. Pre-assignment
|
The instructor asked participants to refer to their pre-assignment responses and provided the following verbal cues before they began working on each item as a group. |
|
|
Interview |
Think about the mechanism of heart failure that causes the patient’s symptoms (dyspnea and edema) and interview the patient, including any associated symptoms. |
|
Inspection |
Think about the visible changes or symptoms caused by heart failure. |
|
Palpation |
Think about the palpable changes or symptoms caused by heart failure. |
|
Percussion |
Think about the symptoms or changes caused by heart failure that can be identified by percussing the body. |
|
Auscultation |
Think about auscultatory changes, such as heart or lung sounds, or symptoms caused by heart failure. |
|
Nursing care |
Think about the nursing care needed based on the patient’s current condition and situation. |
Table A2. Verbal Cues Presented to the Intervention Group
|
Case scenario |
|
78-year-old female. The patient has been followed up on an outpatient basis after valve replacement surgery for mitral regurgitation. During her outpatient visit, she says, “I get short of breath when I walk a little, and the legs are swollen.” You’re an outpatient clinic nurse and suspect the patient may be suffering from heart failure. |
|
Group task |
|
Think about the interview and physical examination, using the answers in the pre-assignment to gather information that will provide evidence of heart failure. Also think about the specific nursing care based on the patient’s current condition. Describe the contents of the interview, physical examination, and nursing care on the answer sheet. |
Table A3. Case scenario and Group task
|
Responses |
|
Symptom location |
|
Interview the patient about edema of the legs (left-right differences, one leg or both legs). |
|
Symptom history |
|
Interview the patient about when edema of the legs and shortness of breath started and any subsequent changes. |
|
Symptom severity |
|
Interview the patient about the severity of shortness of breath (on a scale of 1 to 10) and the severity of edema (whether socks leave marks or shoes can be worn). |
|
Associated symptoms |
|
Interview the patient if any associated symptoms are present, including loss of appetite, nausea, weight changes, fatigue, and sensation of coldness. |
|
Contributing factors |
|
Interview the patient about situations in which shortness of breath occurs (when walking or at rest). |
|
Interview the patient about lifestyle (physical activity and salt and fluid intake). |
|
Medication |
|
Interview the patient about whether or not the patient is taking any medication, the type of medication, and the medication status. |
Table A4. Narrative Responses Provided by the Intervention and Control Groups: Interview
|
Responses |
|
Respiration |
|
Observe respiratory rate, rhythm, depth, and the presence of orthopnea. |
|
Cyanosis |
|
Observe changes in the color of the skin, nails, and lips. |
|
Distension of the jugular veins |
|
Observe for distension and pulsation of the jugular veins. |
|
Facial color and complexion |
|
Observe for pallor, jaundice, and fatigue in facial complexion. |
|
Edema |
|
Observe for edema, left-right differences, the degree of swelling, and its location (legs and face). |
|
Sweating |
|
Observe for cold sweats and sweating. |
|
Somatotype and abdominal distention |
|
Observe for obesity and abdominal distention. |
Table A5. Narrative Responses Provided by the Intervention and Control Groups: Inspection
|
Responses |
|
Vocal fremitus |
|
Check for decreased or absent vibration of the thorax. |
|
Pulse |
|
Check the pulse rate, rhythm, presence of arrhythmia, left-right differences, and strength. |
|
Coldness of limbs |
|
Check the temperature and presence of coldness in the limbs. |
|
Edema |
|
Press the shin or ankle with a finger to check for indentation, depth, and the time to return. |
|
Liver |
|
Check the size, shape, and tenderness of the liver. |
Table A6. Narrative Responses Provided by the Intervention and Control Groups: Palpation
|
Responses |
|
Pleural effusion |
|
Check for pleural effusion. |
|
Ascites |
|
Check for ascites. |
|
Liver |
|
Check the size of the liver. |
Table A7. Narrative Responses Provided by the Intervention and Control Groups: Percussion
|
Responses |
|
Breath sounds |
|
Check for left-right differences, moist rales, dry rales, and adventitious sounds. |
|
Heart sounds |
|
Check for an accentuated or diminished first heart sound, a loud second heart sound, a third heart sound, and a fourth heart sound. |
|
Vascular murmurs |
|
Check for murmurs in the carotid artery, abdominal aorta, renal artery, and arteries of the lower extremities. |
|
Abdomen |
|
Check for bowel sounds. |
Table A8. Narrative Responses Provided by the Intervention and Control Groups: Auscultation
REFERENCES
- Alfaro-LeFevre R. Nursing process and clinical reasoning. Nurs Educ Perspect. 2012; 33(1): 7, doi: 10.5480/1536-5026-33.1.7.
- Chua WL, Legido-Quigley H, Ng PY, Ali S, Arora S, Liaw SY, et al. Seeing the whole picture in enrolled and registered nurses’ experiences in recognizing clinical deterioration in general ward patients: a qualitative study. Int J Nurs Stud. 2019; 95: 56-64. doi: 10.1016/j.ijnurstu.2019.04.012.
- Goto H, Yamauchi T. Nurse perceptions of physical assessment skills for detecting acute progression of heart failure. Jpn J Nurs Sci. 2020; 18(1): e12368. doi:10.1111/jjns.12368.
- Zambas S, Smythe E A, Koziol-Mclaine J. The consequences of using advanced physical assessment skills in medical and surgical nursing: A hermeneutic pragmatic study. Int J Qual Stud Health Well-being. 2016; 11: 32090. doi: 10.3402/qhw.v11.32090.
- Morrell S, Giannotti N, Pittman G, Roche M, McKinlay L, et al. Physical assessment skills taught in nursing curricula: a scoping review. JBI Evid Synth. 2021; 19(11): 2929-2957. doi: 10.11124/JBIES-20-00086.
- Cant R. P, Cooper, S J. Simulation-based learning in nurse education: systematic review. J Adv Nurs. 2010; 66(1): 3-15. doi:10.1111/j.1365-2648.2009.05240.x.
- Tawalbeh L. Effect of simulation on the confidence of university nursing students in applying cardiopulmonary assessment skills: A randomized controlled trial. J Nurs Res. 2017; 25(4): 289-295. doi: 10.1097/JNR.0000000000000170.
- Ferrari A, Maglio S, Tamirat S, Tesfaye M, Wolde M, Manenti F, et al. Nursing and midwifery simulation training with a newly developed low-cost high-fidelity placenta simulator: a collaboration between Italy and Ethiopia. BMC Med Educ. 2024; 24(1): 42. doi: 10.1186/s12909-024-06152-0.
- Hoffman K. A Comparison of decision-making by expert and novice nurses in the clinical setting, monitoring patient haemodynamic status post abdominal aortic aneurysm surgery. PhD Thesis. University of Technology, Sydney; 2007 [cited 2025 May 2]. Available from: http://hdl.handle.net/10453/21800.
- 10.Levett-Jones T, Hoffman K, Dempsey J, Jeong SY, Noble D, Norton C, et al. The ‘five rights’ of clinical reasoning: an educational model to enhance nursing students’ ability to identify and manage clinically ‘at risk’ patients. Nurse Educ Today. 2010; 30(6): 515-520. doi: 10.1016/j.nedt.2009.10.020.
- Tanner CA. Thinking like a nurse: a research based model of clinical judgment. J Nurs Educ. 2006; 45(6): 204-211. doi: 10.3928/01484834-20060601-04.
- Hoffman A K, Aitken L M, Duffield C. A comparison of novice and expert nurses’ cue collection during clinical decision-making: Verbal protocol analysis. Nurse Educ Today. 2016; 46:1335-1344. doi: 10.1016/j.nedt.2016.04.001.
- Shin S, Park J H, Kim J H. Effectiveness of patient simulation in nursing education: Meta-analysis. Nurse Educ Today. 2015;35(1):176–182. doi:10.1016/j.nedt.2014.09.009.
- Bahramnezha F, Shakour M, Ravanipour M, Moattari M. Clinical reasoning education: Evaluating the effect of script strategy and reflective practice on nursing students’ reasoning development. BMC Res Notes. 2024;17:240. doi:10.1186/s13104-025-07338-5.
- Hopewell S, Chan AW, Collins GS, Hróbjartsson A, Moher D, Schulz KF, et al. CONSORT 2025 Statement: updated guideline for reporting randomised trials. BMJ. 2025; 388: e081123. doi: 10.1136/bmj-2024-081123.
- Faul F, Erdfelder E, Lang AG, Buchner A. GPower 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behavior Research Methods. 2007; 39(2):175–191. doi:10.3758/BF03193146.
- International Committee of Medical Journal Editors. Clinical Trials Registration. ICMJE. 2022 [cited 2025 Jun 2]. Available from: http://www.icmje.org/recommendations/browse/publishing-and-editorial-issues/clinical-trial-registration.html
- Ponikowski P, Anker SD, AlHabib KF, Cowie MR, Force TL, Hu S, et al. Heart failure: preventing disease and death worldwide. ESC Heart Failure. 2014; 1(1): 4–25. doi: 10.1002/ehf2.12005.
- Okura Y, Ramadan MM, Ohno Y, Suzuki K, Tanaka F, Matsumoto Y, et al. Impending epidemic: future projection of heart failure in Japan to the year 2055. Circ J. 2008; 72(3): 489-491.
- Conrad N, Judge A, Tran J, Mohseni H, Hedgecott D, Crespillo AP, et al. Temporal trends and patterns in heart failure incidence: a population-based study of 4 million individuals. The Lancet. 2018; 391(10120): 572-580. doi: 10.1016/S0140-6736(17)32520-5.
- Harmon MM, Thompson C. Clinical reasoning in pre-licensure nursing students. Teach Learn Nurs. 2015; 10(2): 63-70. doi: 10.1016/j.teln.2014.12.001.
- Naya K, Sakuramoto H, Nojima K, Ohkawa M, Tanaka Y, et al. Translation, reliability, and validity of the Japanese clinical reasoning skills self-evaluation scale: An instrument design study. Cureus. 2024; 16(1): e53177. doi: 10.7759/cureus.53177.
- Havola S, Haavisto E, Mäkinen H, Jalonen P, Koivisto J. The effects of computer-based simulation game and virtual reality simulation in nursing students’ self-evaluated clinical reasoning skills. Comput Inform Nurs. 2021; 39(11): 725-735. doi: 10.1097/CIN.0000000000000748.
- Andersen B. Mapping the terrain of the discipline. In: Gray G, Pratt R, editors. Towards a Discipline of Nursing. Melbourne: Churchill Livingstone; 1991. p. 95-124.
- Benner P. From novice to expert: Excellence and power in clinical nursing practice. 2nd ed. Upper Saddle River (NJ): Prentice Hall; 2001.
![]() This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
