Ubaldino Ubaldi1*, Valentina Accinno2, Margherita Ascione3, Concetta Pane4
- Department of Ageing, Neurological, Orthopaedic and Head and Neck Sciences C.E.M.I, IRCCS – Fondazione Policlinico Gemelli – Rome (Italy)
- Department of Women’s and Children’s Health Sciences and Public Health DH Clinical Pharmacology, IRCCS – Fondazione Policlinico Gemelli – Rome (Italy)
- Integrated Operative Unit Maternal and Childhood Coordination – ASL Napoli 3 SUD, Naples (Italy)
- Integrated Operative Unit Maternal and Childhood Coordination – ASL Napoli 3 SUD, Naples (Italy)
*Corresponding Author: Ubaldino Ubaldi, Clinical Nurse, IRCCS – Fondazione Policlinico Gemelli – Rome. Nurses Department of Ageing, Neurological, Orthopaedic and Head and Neck Sciences C.E.M.I
Cita questo articolo
ABSTRACT
Introduction: Management by processes and clinical care pathways are now fundamental and indispensable requirements for quality improvement in healthcare organisations. The basic idea is to design a system that allows for continuous improvement in the way in which the key player in healthcare, i.e. the patient, is managed. If this were to happen, the best experiences to date tell us, it would definitively improve outcomes, efficiency and appropriateness. Moreover, patients perceive and appreciate this difference, allowing health professionals to operate at their best.
Objective: To assess the knowledge and application of the DTCPs by the nursing staff.
Materials and methods: The cross-sectional study took place in the period between June and September 2019 at the Operative Units of digestive surgery, hepatobiliary surgery, breast surgery and gynaecological surgery of the “Fondazione Policlinico Gemelli IRCCS in Rome”. A questionnaire was administered only to permanent nurses.
Results: A total of 64 questionnaires were administered of which 27 were correctly completed (response rate 42.1%) and considered valid for analysis. The sample of respondents was predominantly female (74.07%), 81.48% held a Bachelor’s degree and 40.74% held a Master’s degree. 55.56% knew what DTCPs were, but there was no in-depth knowledge of them in the sample. In fact, 55.56% knew whether there were active DTCPs in their region; 7.41% that nurses cannot participate in DTCPs and only 11.11% that nurses cannot participate in the review of individual DTCPs, while 59.26% were aware of the professional figures involved in the drafting and review of DTCPs. 25.93% knew what the diagnostic phase was based on and 14.81% that there were no active memoranda of understanding with public or private facilities in the diagnostic phase. Finally, only 25.93% were aware that the user could not be used in the evaluation of the outcome.
Conclusions: Although the interviewees were familiar with clinical care pathways, for most of them there had never been active involvement, they agreed on user involvement instead.
Keywords: nursing care, clinical care pathways, patient safety, diagnostic-therapeutic care pathways
INTRODUCTION
The reorganisation of the hospital network (Ministerial Decree 70/2015) and the reorganisation of Primary Care (Law 189/2012 – Balduzzi Decree) have brought about a profound and structural change in patient care and treatment in the Italian National Health Service [1-2]. The reorganisation of Primary Care, with the establishment of the AFTs (Regional Functional Aggregations) and the UCCPs (Complex Units of Primary Care), has meant tackling the problem of chronicity, with patient care, according to the Chronic Care Model and the model of integrated and structured Clinical Networks. It is a process of structural change and as such entails the need for a new culture in the definition, management and verification of the process of taking care of chronic patients: all this represents the real ‘Reform’. The operational tool for treating chronic patients and co-morbidities is the Diagnostic-Therapeutic Care Pathways (DTCPs), which therefore represent the lintel of the new system [3-4].
Clinical/healthcare pathways predefine an optimal scheme of the sequence of behaviours in relation to the diagnostic, therapeutic and care pathway to be activated in the face of a typical clinical situation, in order to maximise the effectiveness and efficiency of activities [5]. DTCPs represent multidisciplinary care management technologies that map activities in a healthcare pathway, which are now considered fundamental and indispensable requirements for improving the quality of healthcare organisations in accordance with the logic of clinical governance [6]. The aim is to increase the quality of care across the continuum, improving risk-adjusted patient outcomes, promoting patient safety, increasing user satisfaction and optimising the use of resources [7].
In the entirety of its definition, construction, implementation and monitoring phases, it makes it possible to structure and integrate activities and interventions involved in the active and global care of citizens presenting health problems through a process approach, in a multidisciplinary context and on different areas of intervention (hospital, region, etc.), making it possible to assess the appropriateness of the activities carried out with regard to the objectives, the reference recommendations (Guidelines, good practices) and available resources [8]. It also allows for a measurement of activities and a comparison of results with specific indicators, leading to an improvement in each intervention in terms of effectiveness and efficiency. The need to find a shared theoretical and operational reference on what is meant by ‘diagnostic therapeutic care pathway’ is common among those who, at different levels and with different roles, deal with the planning of healthcare and social-health services and for those who work in them [9-10] .
The organisation of care by DTCPs is indirectly referred to by the ‘Gelli’ Legislative Decree (No 24/2017), the aim of which is to improve the quality of the National Health System, seeking to do so also by acting on the pillar of appropriateness of healthcare intervention, in particular, Article 5 of the aforementioned law regulates the way in which the healthcare profession is exercised, obliging healthcare professionals (doctors, nurses, physiotherapists, etc.) to adhere to the use of official guidelines and good clinical care practices [11]. Hence the need to investigate nurses’ knowledge of DTCPs.
Objective
Assessing nurses’ knowledge and perceptions of DTCPs
MATERIALS AND METHODS
The cross-sectional study was conducted during June-September 2019 at the Operative Units of digestive surgery, hepatobiliary surgery, breast surgery and gynaecological surgery at the “Fondazione Policlinico Gemelli Istituto di Ricovero e Cura a Carattere Scientifico in Rome (IT)”. Authorisation was requested and obtained from SITRA (Servizio Infermieristico Tecnico Riabilitazione Aziendale – Company Rehabilitation Technical Nursing Service) to proceed with the administration of a questionnaire, filled out anonymously, to the nurses on duty in the above-mentioned operational units.
The distribution took place after an interview with the nursing coordinators, providing verbal information on the questionnaire and confirmation of the processing of the data in aggregate form, not resulting in any distribution by name. After the distribution of the questionnaires to the nurses in the operating units by the coordinators, the latter collected them and placed them in a single container, which was then returned to the authors of the study.
All nurses who took part in the study well understood and signed the consent form, in which the purpose of the study and the methodology of conducting it were explained, and the personal data processing form.
The questionnaire, created ad hoc, was structured after a thorough literature search and listed in Appendix A, after the references section. The questionnaire was validated on a sub-sample of 10 nurses from the investigated sample, i.e. the questionnaire was submitted to them twice, at a minimum time interval of three days, and the statistical correlation between the two sets of answers was assessed, using the two-proportion test, with the two answers being statistically correlated if p-value >0.05 (i.e. the answers given, particularly with regard to the DTCP, were consistent at two different time points).
The questionnaire consists of 21 multiple-choice items structured as follows:
– 5 items on biographical characteristics: years of service, assigned operational unit, gender, educational qualification, post basic training;
– 16 items on DTCPs: what is a DTCP; participation of nurses in DTCP training courses; existence of DTCPs in their region and which types; whether clinical audits are planned and how often and others.
Informed consent was signed by all patients included in this study and anonymity was guaranteed. No economic incentives were offered or provided for participation in this study. The study was performed following the ethical considerations of the Helsinki Declaration[12].
Inclusion and exclusion criteria
All nurses of both sexes with a permanent contract type, who speak and understand Italian well, were included in this study, while all nurses temporarily assigned by the cooperatives (fixed-term and/or temporary assignment) were excluded from the study. However, this is a sample study with probabilistic sample selection (the only common element of inclusion is the existence of an open-ended contract).
Statistical analysis
Data was presented as numbers or percentages for categorical variables. Continuous data is expressed as the mean ± standard deviation (SD), or median with Interquartile Range (IQR).
A binomial test was performed to compare two mutually exclusive proportions or percentages in groups. The chi square test and Fisher’s exact test were performed to evaluate significant differences in proportions or percentages between two groups. Particularly Fisher’s exact test was used where the chi-square test was not appropriate. The multiple comparison chi-square tests were used to define significant differences between percentages. In this case, if the chi-square test was significant (α level: 0.05), the residual analysis with the Z-test was performed. All tests with p-value(p) <0.05 were considered significant. The statistical analysis was performed by Matlab statistical toolbox version 2008 (MathWorks, Natick, MA, USA).
RESULTS
A total of 64 questionnaires were administered, 13 in digestive surgery, 14 in hepatobiliary surgery, 21 in breast surgery and 16 in cancer surgery. Only 27 questionnaires (42.8%) were returned and completed. Specifically:
– digestive surgery, 13 questionnaires delivered, 5 returned completed (38.4%).
– general surgery – hepatobiliary, 14 questionnaires delivered, 9 returned completed (64.2%);
– retroperitoneal cancer surgery, 21 questionnaires delivered, 6 returned completed (28.5%);
– gynaecological oncology, 16 questionnaires delivered, 7 returned and completed (43.7%);
In Table 1 below, we have reported the characteristics of our sample of nurses

Table 1. Characteristics of the 27 subjects participating in this study Items 1-5 of the questionnaire
Table 1 shows that the sample has a length of service ranging from 11 to 20 years (44%), is predominantly female (74%) and holds a bachelor’s degree (81%), while 40.7% of the respondents hold a Master’s degree.
Table 2 shows the interviewees’ knowledge of the Diagnostic-Therapeutic Care Pathway (DTCP).


Table 2. Knowledge of the interviewees about the DTCP. Items 6-15 of the questionnaire. The correct answer is indicated in bold and with an asterisk.
Table 3 shows the interviewees’ knowledge of the DTCP Protocols.

Table 3. Knowledge of the interviewees about the DTCP Protocols. Items 16-18 of the questionnaire The correct answer is indicated in bold and with an asterisk.
Table 4 shows the monitoring associated with the DTCP
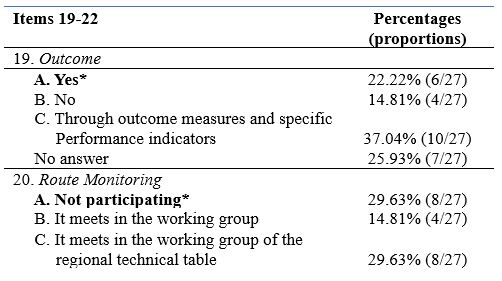

Table 4. Knowledge of the interviewees about the monitoring associated with the DTCP. Items 19-22 of the questionnaire The correct answer is indicated in bold and with an asterisk.
Finally, Table 5 shows all the statistical tests performed in this study


Table 5. Statistical tests performed in this study. Unanswered questions were not considered in the statistical analysis for each item. The correct answer in the questionnaire is indicated in bold
From Table 5, it can be seen that in our sample, there was no significant difference by seniority of service (p=0.368) and by medical area (p=0.730), while there was a significant presence of female gender (74.07%, p<0.0001) and of subjects with a Bachelor’s degree (81.48%, p<0.0001). On the other hand, with regard to postgraduate education, subjects with a Master’s degree were significantly more present (40.74%, p<0.0001), together with the option ‘Other’ (25.93%, p=0.0013).
With regard to knowledge of DTCP courses, the most frequent answer was Answer A: ‘DTCP describes the pathway that a person with health problems takes between one or more health organisations and defines the best sequence of actions necessary to achieve the health objectives identified a priori’ (55.56%, p<0.0001), whereas when asked about participation in DTCP courses, the answer ‘No’ was the significantly most frequent (74.08%, p<0.0001). Regarding knowledge of active DTCP courses in one’s region, the most frequent answer was ‘YES’ (55.56%, p<0.0001).
When asked about knowledge of which DTCPs were active (Item 9) and of DTCPs for neurodegenerative diseases (Item 10), there was no significant difference between the answers.
In Item 11, concerning ‘nurse participation’, Answer C: ‘partly’ was the most frequent (55.56%, p<0.0001), similarly for Item 12 (Answer C: 70.37%, p<0.0001).
With regard to the clinical audit (Item 13), there was no significant difference between the various answers. In contrast, for audit cadence (Item 14), Answer D: ‘1/year‘ was the most frequent (55.56%, p<0.0001).
With regard to knowledge of published audits (Item 15), there was no significant difference between the various answers.
With regard to Item 16 (Other professional figures), the significantly more frequent answer was Answer C: ‘all professional, rehabilitation medical figures provided in the multidisciplinary teams specific to that clinical condition’ (59.26%, p<0.0001).
For Item 17 (DTCP phases), the most frequent answer was ‘YES’ (48.15%,p=0.0084). Similarly for Item 18 (SI: 51.85%, p<0.0001).
There was no significant difference between the responses associated with Items 19, 20 and 21, whereas for Item 22 (user involvement), the ‘YES’ response was the significantly more present (48.15%, p=0.0084),
DISCUSSION
The cross-sectional study was conducted with the aim of exploring and assessing the knowledge of DTCPs by nurses in service at the Fondazione Policlinico Gemelli (IRCCS) assigned to the Operative Units of digestive surgery, hepatobiliary surgery, breast surgery and gynaecological surgery through the administration of a questionnaire.
Almost half of the nurses interviewed to date, despite having completed a Bachelor’s and a Master’s degree, are not aware of the importance of DTCPs in terms of quality of care and the achievement of health outcomes: all organisations, including health care organisations, are composed of a series of processes or sets of actions, oriented towards creating value for those who know and use them [13]. It is likely that the study of Guidelines, Protocols, Procedures and DTCPs undertaken in the 1st year programme should also be taken up in the following years in the degree course, combining theory with practice.
Almost all of the nurses (74.08%), who participated in the study, were never involved in participating in the drafting of such pathways, without considering the importance of a broadly participatory approach of all components (management and technical-professional) of the organisation and the use of decision-support techniques (use of scientific evidence, audits between professionals) [14].
Healthcare institutions can use DTCPs and promote evidence-based practice to benefit quality and reduce costs [15]; however, research suggests that compliance with the use of DTCPs is low [16].
Another barrier could be resistance to the practice of change in working environments
[17], however with a proper implementation and evaluation process, change in healthcare is achievable [18].
The nurses’ thoughts on user involvement are significant: in the light of these results, it can be stated that the attempt to introduce a multidisciplinary logic in healthcare organisations is hindered by the very peculiarity of the context, which is of a professional nature, in which management cannot impose itself on professionals, but must instead involve them. The task of management today is to succeed in creating those conditions that actively involve health professionals in spontaneously innovating clinical practice [19].
CONCLUSION
The implementation of DTCPs can offer the patient timely and real continuity of care, through the identification of qualified care and the integration of all professional figures. The study conducted included the assessment of nurses’ knowledge on DTCPs. The results obtained show a gap in nurses’ knowledge of DTCPs and this preliminary study provides several insights to improve the knowledge of DTCPs among nurses in order to ensure better continuity of patient care.
Strengths and Limitations of the study
The study has some limitations. In particular, the sample examined is a monocentric and small sample; a larger sample could have provided additional insights, reducing the possibility of statistical bias.
The study could be a preliminary step to a larger one including other operating units, not previously taken into account, so as to offer new insights given the importance of the topic for nurses.
Funding
This research did not receive any form of funding.
Conflict of interest
The authors declare that they have no conflicts of interest associated with this study.
REFERENCES
- Decreto Ministeriale 2 aprile 2015 n. 70 Regolamento recante definizione degli standard qualitativi, strutturali, tecnologici e quantitativi relativi all’assistenza ospedaliera. (G.U. 4 giugno 2015, n. 127)
- LEGGE 8 novembre 2012, n. 189Conversione in legge, con modificazioni, del decreto-legge 13 settembre 2012, n. 158, recante disposizioni urgenti per promuovere lo sviluppo del Paese mediante un piu’ alto livello di tutela della salute. (12G0212) (GU n. 263 del 10-11-2012 – Suppl. Ordinario n. 201)
- Casati G., Panella M., Di Stanislao F., Gestione per processi professionali e percorsi assistenziali, terza edizione, Roma Ancona, Marzo 2005.
- Casati G., Vichi M.C., Il percorso assistenziale del paziente in ospedale, McGraw-Hill Companies SRL, Milano, 2002.
- Specchia M.L., Poscia A., Volpe M., Parente P., Capizzi S., Cambieri A., De Belvis A.G., Does Clinical Governance Influence the appropriateness of hospital stay? Bio Med Central Health Services Research, Aprile 2015.
- Broda et Al., Clinical Pathway: un metodo per il miglioramento della qualità in ambito ospedaliero, Scuola di Specializzazione di Igiene e Medicina Preventiva, Università di Torino.
- Janicek M., Casi clinici ed evidence – based medicine, Roma 2001.
- Atwal A., Caldwell K., Do multidisciplinary integrated care pathways improve interprofessional collaboration, Scandinavian Journal of Caring Sciences, 16(4):360-7,2002.
- Croce D., Sebastiano A., Castiglioni Rusconi M., Carenzi A., I PDT/PDTA nelle organizzazioni sanitarie: una meta-analisi della letteratura internazionale, economia e management “s.d” pp38-39 [online]Casati G., La gestione per processi in sanità, QA Vol 13. 1, (2002).
- Casati G., Vichi C. Il percorso assistenziale del paziente: partener di Sanità & Management Consulting Srl. Giornale di tecniche nefrologiche & dialitiche, anno XV n 2., S. Donato Milanese, Milano 2002.
- LEGGE 8 marzo 2017, n. 24 “Disposizioni in materia di sicurezza delle cure e della persona assistita, nonché in materia di responsabilità professionale degli esercenti le professioni sanitarie.” (17G00041) (GU Serie Generale n.64 del 17-03-2017)
- World Medical Association; “Dichiarazione di Helsinki della World MedicalAssociation: principi etici per la ricerca biomedica che coinvolge gli esseri umani”; 2013; Volume 5:Issue 10; e1000059
- ARESS (Agenzia Regionale per i Servizi Sanitari della Regione) Piemonte, Raccomandazioni per la costruzione dei PDTA e PIC nelle aziende sanitarie della Regione Piemonte, 2007
- Noto G, Raschetti R, Maggini M,. Gestione integrata e percorsi assistenziali. Roma: Il Pensiero Scientifico Editore. 2011
- Every N., Hochman J., Becker R., Kopecky S., & Cannon C. Critical pathways: A review. Circulation, 10, 461. 2000
- Kinsman, L. Clinical pathway compliance and quality improvement. Nursing Standard, 18, 33–35. 2004
- Seckel M., & Miller, K. Potential barriers to implementing practice alerts. AACN Reseach Work Group. 2005–2006
- Goudreau K. Notes from the board. Clinical Nurse Specialist, 20, 215–216. 2006.
- Kingston, M., Krumberger, J., & Peruzzi, W., Enhancing outcomes: Guidelines, standards, and protocols AACN Clinical Issues: Advanced Practice in Acute and Critical Care, 11, 363–374. 2000.
Appendix A
COGNITIVE QUESTIONNAIRE ON NURSES’ PERCEPTIONS OF DTCPs.
Dear colleague,
We are two nurses who work at the Fondazione Policlinico Gemelli and we are conducting a cognitive survey, with the aim of surveying the knowledge of health workers on the subject of Diagnostic-Therapeutic Care Pathways.
We ask you to take a few minutes of your time to answer the questions in the questionnaire, assuring you that the results will be treated absolutely anonymously and used for statistical purposes only.
Thank you for your participation.
1. Years of service:
A. less than 10
B. 11-20
C. More than 20
2. In which area are you assigned?
A. critical area
B. medicine
C. surgery
D. Other……
3. Gender:
A. M
B. F
4. Basic qualification:
A. Qualifying title
B. University diploma
C. Bachelor’s degree
5. Post-basic training (multiple answers possible)
A. Advanced training courses……………………………………………..
B. Master’s degree (one or more) ………………………………………
C. Master’s/Specialist Degree
D. Level II Master’s degree (one or more)………………………………………
E. Other………………………
6. What is a Diagnostic-Therapeutic Care Pathway (DTCP)?
A. The DTCP describes the ‘journey’ that a person with health problems takes between one or morehealth organisations and defines the best sequence of actions necessary to achieve thehealth objectives identified a priori.
B. The DTCP is a set of guidelines, protocols and procedures
C. The DTCP is a structured pathway of healthcare acts
7. Have you ever participated in DTCP training courses?
A. Yes
B. No
C. I have never been contacted
8. Are there active DTCPs in your region?
A. Yes
B. No
C. In the planning stage for implementation
9. If you answered ‘Yes’ to the previous question, which one?
A. Single integrated rehabilitation pathway for the stroke patient
B. Pathway for the care and rehabilitation of patients with disorders of consciousness due to severe acquired brain injury
C. Diagnostic and therapeutic care pathway for chronic obstructive pulmonary disease
D. Definition of the pathway for early detection of suspected cases of DSA and indication for diagnosis and certification
E. Operational guidelines for the implementation in the regional network of social and health services and integrated pathways for adults with SLA
F. Operational guidelines for the prevention, diagnosis, treatment and care of people with dementia
G. Other DTCPs …………………………………………………………………………………………………………………………………………………………………
10. In your Regional Health Agency, have DTCPs been activated that may affect Neurodegenerative and Neurodevelopmental diseases?
A. Yes
B. No
C. They are in the planning stage
11. Does the professional figure of the nurse participate, and to what extent, in the drafting of the specific DTCP?
A. Yes
B. No
C. Partially
D. Participates in specific regional technical tables as a representative of the professional association
12. Does the nurse participate, and to what extent, in the review of individual DTCPs?
A. Yes
B. No
C. Only partially
13. Are clinical audits of individual DTCPs planned?
A. YES
B. NO
C. Partially
14. How often are specific audits planned for each DTCP?
A. One/month
B. One/every two months
C. One/semester
D. One/year
E. Other…
15. Are the DTCPs published on the company website or in the appropriate sections and therefore consultable by the various professionals?
A. YES
B. No
C. Only partially
16. What other professional figures are envisaged in the drafting/revision of individual DTCPs?
A. Only doctors
B. Only physiotherapists
C. All the professional, medical and rehabilitation figures foreseen in the multidisciplinary teams specific to that clinical condition
17. The DTCP envisages a Diagnostic phase and a Therapeutic-Assistance phase: are PACC, PIC and Day Service envisaged in the diagnostic phase?
A. Yes
B. No
18. Are memoranda of understanding currently in place with accredited public and/or private healthcare facilities in the Diagnostic phase?
A. Yes
B. No
C. Partially (please specify)………………………………………………….
19. In DTCPs, is the outcome used, and in what way, as a check on the effectiveness, efficiency, cost-effectiveness and appropriateness of the Pathway?
A. Yes
B. No
C. Through outcome measures and specific performance indicators set out in individual documents
20. To what extent does the nurse participate in pathway monitoring activities?
A. Not participating
B. Meetings in the working group
C. Meeting in the working group of the regional technical table
21. Are teleconsultation, telemonitoring and teleassistance activities provided for within the individual DTCPs?
A. Yes
B. No
C. In part (specify)………………………………………………….
22. Is user involvement in outcome assessment foreseen in the DTCPs?
A. Yes
B. No
Authorisation for data processing for statistical purposes consent
□ ………………………………………………………….
□ ………………………………………………………….
![]() This work is licensed under a Creative Commons
This work is licensed under a Creative Commons
Attribution-NonCommercial-NoDerivatives 4.0 International License.

