Ifa Nofalia 1, Dwi Prasetianingati 1, Dessy Ekawati 1*
- Department of Nursing, Faculty of Health, Institute of Science and Health Technology Insan Cendekia Medika Jombang
* Corresponding author: Dessy Ekawati., Department of Nursing, Faculty of Health, Institute of Science and Health Technology Insan Cendekia Medika Jombang. E-mail: dessyekawati.s1201@gmail.com
Ifa Nofalia, Dwi Prasetianingati, Dessy Ekawati
Original article
DOI:10.32549/OPI-NSC-126
Submitted: 21 August 2025
Revised: 12 September 2025
Accepted: 13 September 2025
Published online: 19 September 2025
License: This article is licensed under the Creative Commons Attribution - Non Commercial - No Derivatives 4.0 (CC BY NC ND 4.0) international license.
Abstract:
Cryptic pregnancy, or the delayed recognition of pregnancy until late gestation, poses unique psychological challenges for mothers due to the lack of prenatal preparation and sudden transition to motherhood. These circumstances may increase the risk of postpartum depression. Protective factors such as maternal self-efficacy and family support are believed to play an important role in reducing depressive symptoms after childbirth.
Cite this article
ABSTRACT
Introduction: Cryptic pregnancy, or the delayed recognition of pregnancy until late gestation, poses unique psychological challenges for mothers due to the lack of prenatal preparation and sudden transition to motherhood. These circumstances may increase the risk of postpartum depression. Protective factors such as maternal self-efficacy and family support are believed to play an important role in reducing depressive symptoms after childbirth.
Objective: The purpose of this study is (1) to analyze the relationship between maternal self-efficacy and postpartum depression among mothers with a history of cryptic pregnancy, (2) to analyze the relationship between family support and postpartum depression, and (3) to assess the extent to which maternal self-efficacy and family support predict postpartum depression levels.
Materials and Methods: A cross-sectional study was conducted in Jombang Regency, East Java, Indonesia, from May to August 2025, involving 104 mothers with a history of cryptic pregnancy recruited by non-probability snowball sampling. Maternal self-efficacy was assessed using the 15-item questionnaire developed by Witungga et al. (2024; α = 0.916), family support with the 14-item questionnaire by the same authors (α = 0.836), and postpartum depression with the Edinburgh Postnatal Depression Scale (EPDS; Adli, 2022). Data were analyzed using Spearman’s rank correlation and ordinal logistic regression.
Results: Most respondents had moderate self-efficacy (72.1%), fair family support (65.4%), and no signs of postpartum depression (68.3%). Spearman’s correlation showed significant negative associations between self-efficacy (ρ = –0.426, p = 0.001) and family support (ρ = –0.398, p = 0.002) with postpartum depression. Multivariate ordinal logistic regression indicated that both self-efficacy (B = –0.462, p = 0.014, OR = 0.63, 95% CI = 0.44–0.91) and family support (B = –0.518, p = 0.012, OR = 0.60, 95% CI = 0.40–0.89) were significant protective factors, jointly explaining 28.9% of variance in postpartum depression (Nagelkerke R² = 0.289).
Conclusion: Maternal self-efficacy and family support are significant protective factors against postpartum depression in mothers with cryptic pregnancy. Strengthening maternal confidence and empowering family support systems are essential strategies to mitigate depressive symptoms in this vulnerable group.
Keywords: cryptic pregnancy, family support, maternal self-efficacy, postpartum depression
INTRODUCTION
Postpartum depression (PPD) is a major public health concern, affecting approximately 10–20% of mothers worldwide, with higher prevalence reported in low- and middle-income countries (LMICs) compared to high-income settings [1,2]. In Indonesia, national surveys have shown increasing rates of postpartum depressive symptoms, with prevalence reaching 11.2% in East Java in 2023, indicating a substantial and growing burden [3]. Despite these numbers, many cases remain undetected due to limited screening and strong sociocultural norms that discourage disclosure of psychological distress.
One critical factor influencing maternal adaptation is the level of social and family support. Numerous studies demonstrate that family support functions as a protective buffer against PPD, with inadequate support consistently linked to more severe depressive symptoms [4]. In particular, emotional responsiveness from partners and close relatives helps reduce maternal stress, facilitates the adjustment process to motherhood, and strengthens the bond between mother and infant. On the other hand, rejection, blame, or neglect from family members can worsen emotional instability and increase the risk of depressive outcomes.
Another important determinant of maternal well-being is maternal self-efficacy, defined as a mother’s belief in her ability to successfully care for her infant. Evidence indicates that higher maternal self-efficacy is associated with reduced depressive symptoms, more effective coping strategies, and better overall postpartum adjustment [5,6]. Mothers with low self-efficacy often report feelings of helplessness, decreased motivation to provide infant care, and heightened vulnerability to depression. Strengthening maternal confidence is therefore essential to preventive and therapeutic interventions in postpartum mental health.
Cryptic or denied pregnancy represents a unique context that has received little empirical attention. In this condition, pregnancy remains unrecognized until late gestation or even the onset of labor. Although traditionally considered rare, recent reviews suggest cryptic pregnancies may occur more frequently than previously assumed, and they present distinct psychosocial challenges for both mothers and families [7]. The lack of preparedness, combined with social stigma and disrupted family dynamics, places these mothers at particular risk of postpartum psychological distress. Yet, systematic research on PPD in women with cryptic pregnancies remains extremely limited.
Nurses play a central role in maternal and child health by conducting early screening, providing psychosocial education, and strengthening family-centered care systems. Understanding how maternal self-efficacy and family support influence postpartum depressive symptoms among mothers with cryptic pregnancies is therefore critical for nursing practice and policy.
Objective: This study aims to (1) analyze the relationship between maternal self-efficacy and postpartum depression among mothers with a history of cryptic pregnancy, (2) to analyze the relationship between family support and postpartum depression among mothers with a history of cryptic pregnancy, and (3) to assess the extent to which maternal self-efficacy and family support predict postpartum depression levels among mothers with a history of cryptic pregnancy.
MATERIALS AND METHODS
Study Population
This study was conducted in Jombang Regency, East Java, Indonesia, from April to July 2025. The target population included women who had experienced a cryptic pregnancy within the last one to two years. Due to the rarity and sensitive nature of cryptic pregnancy, a non-probability snowball sampling technique was employed. An initial group of participants (seed respondents) identified through community health centers and local networks served as starting points, and they referred other eligible women who had undergone similar experiences. A total of 104 respondents were successfully recruited.
The study protocol adhered to the ethical principles outlined in the Declaration of Helsinki and was approved by the Scientific and Ethics Committee of the Institute for Learning Development and Quality Assurance, Institute of Science and Health Technology Insan Cendekia Medika Jombang (Ref: LP3M/ICME/ETIK/0425/2025). All participants were fully informed about the study’s objectives and procedures and provided written informed consent prior to participation.
Inclusion Criteria
Participants were eligible for inclusion if they were women aged 18–40 years who had experienced a cryptic pregnancy that resulted in a live birth within the previous 12 months. They were required to be able to read and write in Indonesian, possess adequate cognitive capacity to complete the questionnaire independently, and provide informed consent voluntarily. These criteria were established to ensure that participants could fully understand and respond to the study instruments with accuracy and autonomy.
Exclusion Criteria
Women were excluded from the study if they had a current diagnosis or documented history of major psychiatric disorders such as schizophrenia, bipolar disorder, or major depressive disorder prior to the pregnancy. Additionally, individuals who had experienced fetal loss (miscarriage or stillbirth), or who were undergoing psychiatric treatment unrelated to postpartum depression at the time of data collection, were also excluded. These exclusion criteria aimed to minimize potential confounding effects on the assessment of postpartum depression symptoms.
Instruments
Three validated instruments were used in this study. Maternal self-efficacy was measured using a 15-item Likert-scale questionnaire developed by Witungga et al. (2024), with a Cronbach’s alpha of 0.916; responses ranged from 1 (strongly disagree) to 4 (strongly agree), and scores were categorized as low, moderate, or high. Family support was assessed using a 14-item questionnaire also developed by Witungga et al. (2024), with a Cronbach’s alpha of 0.836; each item was scored dichotomously (yes = 2, no = 1), and total scores were classified into poor, sufficient, or good support [8]. Postpartum depression was evaluated using the Edinburgh Postnatal Depression Scale (EPDS), originally developed by Cox, Holden, and Sagovsky (1987) and adapted into Indonesian by Adli (2022); this 10-item scale assesses maternal mood in the past week, with each item scored from 0 to 3 for a total range of 0–30, where higher scores indicate greater depressive severity. The EPDS has consistently demonstrated robust psychometric properties across international studies, with Cronbach’s alpha values ranging from 0.80 to 0.88 and sensitivity above 85% in detecting postpartum depression [9].
Variables
The independent variables in this study were maternal self-efficacy (categorized into low, moderate, and high) and family support (categorized into poor, fair, and good). The dependent variable was postpartum depression, measured by the Edinburgh Postnatal Depression Scale (EPDS) and categorized into three levels: no signs of depression, depression may be present, and clear signs of depression. Sociodemographic characteristics were included as control variables, consisting of age, last educational attainment, marital status, occupation, family income, place of residence, number of children (including the child from the cryptic pregnancy), gestational age at the time the pregnancy was discovered, previous pregnancy history, access to healthcare, mode of delivery, presence of a birth companion, complications during pregnancy or delivery, and history of mental health problems. Household income was recorded in Indonesian Rupiah (IDR) and converted to United States Dollars (USD) using the 2025 average exchange rate (1 USD ≈ 15,500 IDR) to enhance international readability.
Statistical Analysis
All data were analyzed using SPSS software version 26 for Windows. Descriptive statistics were employed to summarize the sociodemographic characteristics of the participants. The Kolmogorov–Smirnov test was used to assess data normality and indicated that the data were not normally distributed (p < 0.05). Spearman’s rank correlation test was used to evaluate the relationships between maternal self-efficacy, family support, and postpartum depression. To further identify the strength and direction of predictors on postpartum depression levels, ordinal logistic regression analysis was conducted. This method is appropriate given the ordinal nature of the dependent variable and non-normal data distribution. Statistical significance was defined as a p-value less than 0.05.
RESULTS
Sample Characteristics
The mean age of respondents was 28.45 years (SD = 6.14), with the largest proportion aged 25–29 years (32.7%). More than half had completed secondary education (55.8%), were married (89.4%), and worked as housewives (68.3%). More than half of the participants reported a monthly family income between 152 and less than 304 USD (55.8%), with a mean income of 139.78 USD (SD = 88.55) and a median of 187.46 USD (IQR = 44.87–210.26), and the majority resided in urban areas (60.6%). Nearly half had two children, including the child from the cryptic pregnancy (44.2%), and most discovered their pregnancy in the third trimester (≥ 28 weeks) (61.5%); a considerable proportion reported previous pregnancies, including unplanned pregnancy or miscarriage (44.2%). Access to healthcare was most frequently moderate, requiring 30–60 minutes with limited transportation (50%). The most common mode of delivery was spontaneous vaginal delivery at a healthcare facility (48.1%), with most accompanied by a husband or family member during childbirth (67.3%). The majority experienced no pregnancy or delivery complications (72.1%) and none reported a history of mental health disorders (100%). Self-efficacy assessments indicated that self-efficacy was predominantly moderate (72.1%), while family support was most often fair (65.4%). Regarding postpartum depression, most mothers exhibited no signs of depression (68.3%), while nearly one-third showed possible symptoms (31.7%). Table 1 shows the demographic data of respondents.
Characteristic Category n (%) M (SD) Median (IQR) Sociodemographic of Respondent
Age < 20 9 (8.7%) 28.45 (6.137) 28 (24 – 33) 20–24 20 (19.2%) 25–29 34 (32.7%) 30–34 21 (20.2%) ≥ 35 20 (19.2%) Last educational attainment Basic education (Elementary School or equivalent) 46 (44.2%) Secondary education (Junior/Senior High School or equivalent) 58 (55.8%) Higher education (Diploma, Bachelor’s, or Postgraduate) 0 (0%) Marital Status Married 93 (89.4%) Unmarried 3 (2.9%) Divorced/Widowed 8 (7.7%) Occupation Housewife 71 (68.3%) Employed 22 (21.2%) Unemployed 4 (3.8%) Others 7 (6.7%) Family income < USD 60,79 45 (43.3%) USD 139.78 (88.55) USD 187.46 (44.87 – 210.26) USD 152 ≤ 304 58 (55.8%) ≥ USD 303,93 1 (1.0 %) Place of residence Urban 63 (60.6%) Rural 41 (39.4 %) Number of children (including children during cryptic pregnancy) 1 child 42 (40.4 %) 2 children 46 (44.2%) ≥ 3 children 16 (15.4%) Gestational age at the time the pregnancy was discovered < 12 weeks (1st trimester) 19 (18.3%) 12–27 weeks (2nd trimester) 21(20.2%) ≥ 28 weeks (3rd trimester) 64 (61.5%) Previous Pregnancy History No previous pregnancy 27 (26.0%) Yes, all planned pregnancies 31 (29.8%) Yes, including unplanned pregnancy/miscarriage 46 (44.2%) Access to healthcare Easy (≤ 30 minutes, transportation available) 32 (30.8%) Moderate (30–60 minutes, limited transportation) 52 (50%) Difficult (> 60 minutes, poor transportation access) 20 (19.2%) Mode of delivery Spontaneous/vaginal at a healthcare facility 50 (48.1%) Spontaneous/vaginal at home 20 (19.2%) Cesarean section (C-section) at a healthcare facility 24 (23.1%) Others (e.g., without medical assistance) 10 (9.6%) Presence of a birth companion Husband/Family 70 (67.3%) Healthcare provider 32 (30.8%) Alone/No attendant 2 (1.9%) Complications during Pregnancy or delivery None 75 (72.1%) Present 29 (27.9%) Mental health history None 104 (100%) Self – Efficacy Low 0 (0%) 32.45 (5.812) 32 (28 – 37) Moderate 75 (72.1%) High 29 (27.9%) Family Support Poor 0 (0%) 28.63 (4.925) 29 (25–32) Fair 68 (65.4%) Good 36 (34.6%) Postpartum Depression No signs of depression 71 (68.3%) 10.82 (3.214) 11 (9 – 13) Depression may be present 33 (31.7%) Clear signs of depression 0 (0%) Abbreviations: n = number; % = percentage; M = mean; SD = standard deviation; IQR = interquartile range; USD = United States Dollar. All variables had complete data (n = 104).
Table 1. Sociodemographic, Self – Efficacy, Family Support and Postpartum Depression.
Relationship Between Self-Efficacy and Postpartum Depression
The Spearman correlation test results indicate a negative and significant relationship between self-efficacy and postpartum depression, with a correlation coefficient of ρ = –0.426 and a significance value of p value = 0.001 (Table 2). This finding suggests that higher levels of self-efficacy are associated with lower levels of postpartum depression. The strength of the relationship is moderate and remains statistically significant.
Variable M (SD) Median (IQR) Sig. (2-tailed) Spearman Correlation Self-efficacy 32.45 (5.812) 32 (28 – 37) Correlation coefficient ρ = –0.426, p value = 0.001**
Postpartum depression 10.82 (3.214) 11 (9 – 13) *p < 0.05, **p < 0.01, SD = standard deviation, IRQ = interquartile range [Q1, Q3]; M = mean.
Table 2. Relationship Between Self-Efficacy and Postpartum Depression (N = 104).
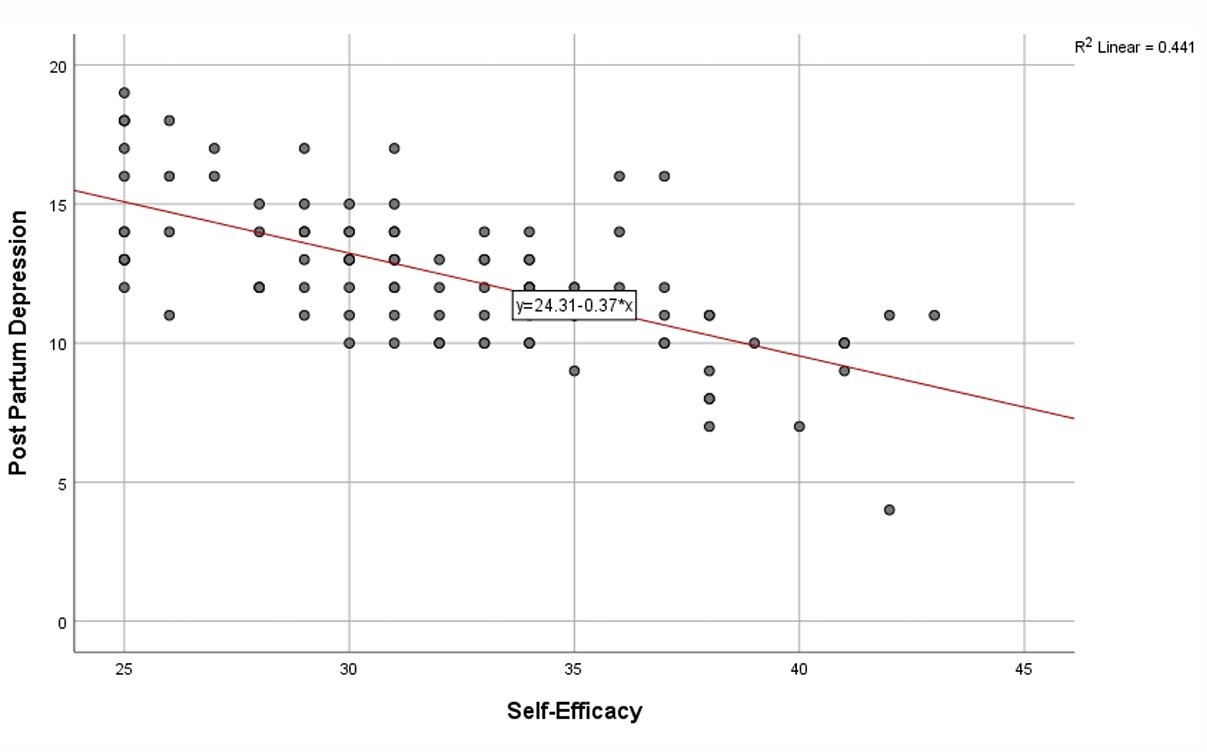
Figure 1 presents a scatter plot showing a moderate negative correlation (ρ = –0.426, p value = 0.001) between self-efficacy and postpartum depression. This correlation suggests that higher levels of maternal self-efficacy are associated with lower levels of postpartum depression. The results also indicate that the relationship between these two variables is moderate and statistically significant.
Figure 1. Scatter Plot of Postpartum Depression Levels by Self-Efficacy Levels. The trend line is in red.
The crosstabulation analysis further shows the distribution of respondents based on self-efficacy levels and postpartum depression symptoms (Table 3).
Self-Efficacy Postpartum Depression Total No signs of depression Depression may be present Moderate 55 20 75 High 16 13 29 Total 71 33 104 Table 3. Crosstabulation of Self-Efficacy and Postpartum Depression.
Among those with moderate self-efficacy, 55 mothers reported no signs of depression, while 20 mothers showed possible signs of depression, totaling 75 individuals. In contrast, among those with high self-efficacy, 16 mothers reported no signs of depression and 13 mothers experienced possible depression, totaling 29 individuals.\
Relationship Between Family Support and Postpartum Depression
Correlation analysis using Spearman’s correlation coefficient indicates a negative and significant relationship between family support and postpartum depression, with a correlation coefficient of ρ = –0.398 and a significance value of p value = 0.002 (Table 4). This suggests that higher levels of family support are associated with lower levels of postpartum depression, and the strength of this relationship is moderate and statistically significant.
Variable M (SD) Median (IQR) Sig. (2-tailed) Spearman Correlation Family support 28.63 (4.925) 29 (25–32) Correlation coefficient ρ = –0.398, p value = 0.002**
Postpartum depression 10.82 (3.214) 11 (9–13) *p < 0.05, **p < 0.01, SD = standard deviation, IRQ = interquartile range [Q1, Q3]; M = mean.
Table 4. Relationship Between Family Support and Postpartum Depression (N = 104)
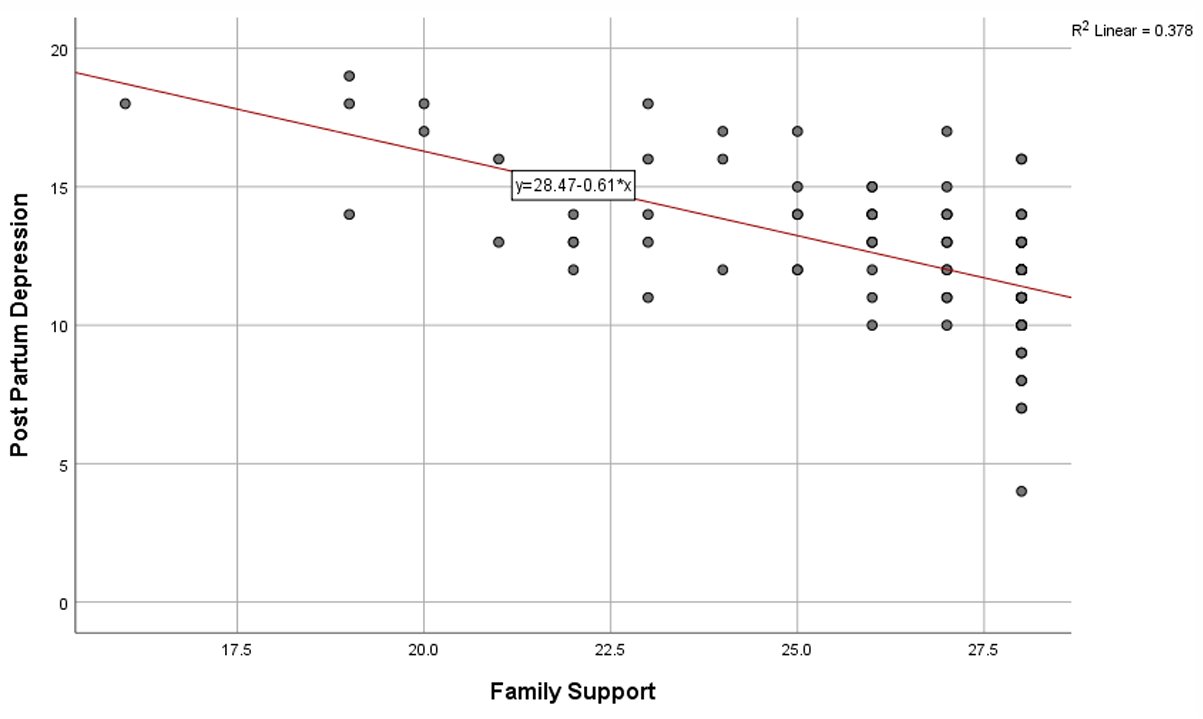
Figure 2 presents a scatter plot to visualize the joint values for the family support and postpartum depression variables, and to observe possible relationships, trends, between the variables. We observed from Figure 2 a moderate negative correlation (ρ = –0.398, p value = 0.002) between family support and postpartum depression. This correlation suggests that higher levels of family support are associated with lower levels of postpartum depression. The results also indicate that the relationship between these two variables is moderate and remains statistically significant.
Figure 2. Scatter Plot of Postpartum Depression Levels by Family Support Levels. The trend line is in red.
The crosstabulation analysis further shows the distribution of respondents based on family support and postpartum depression symptoms (Table 5).
Family Support Postpartum Depression Total No signs of depression Depression may be present Fair 44 24 68 Good 27 9 36 Total 71 33 104 Table 5. Crosstabulation of Family Support and Postpartum Depression
Among mothers with fair family support, 44 reported no signs of depression while 24 experienced possible signs of depression, totaling 68 individuals. Conversely, among those with good family support, 27 mothers reported no depression and 9 mothers experienced possible depression, totaling 36 individuals.
The Combined Effect of Maternal Self-Efficacy and Family Support on Postpartum Depression
The results of the multivariate ordinal logistic regression analysis showed that both maternal self-efficacy and family support have significant effects on postpartum depression. The overall model shows a Nagelkerke R² value of 0.289, indicating that the combination of maternal self-efficacy and family support explains 28.9% of the variability in postpartum depression levels.
In Table 6, we reported the results of the multivariate ordinal logistic regression analysis of maternal self-efficacy and family support on postpartum depression.
Predictor B SE Wald OR (Exp(B)) 95% CI for OR p value Maternal self-efficacy -0.462 0.188 6.030 0.63 0.44 – 0.91 0.014 * Family support -0.518 0.205 6.367 0.60 0.40 – 0.89 0.012 * -2 Log Likelihood 178.21 Nagelkerke R² 0.289 *Significant at p < 0.05
Table 6. Multivariate Ordinal Logistic Regression of Maternal Self-Efficacy and Family Support on Postpartum Depression (n = 104).
The parameter estimates indicate that maternal self-efficacy has a significant negative association with postpartum depression (B = –0.462, Wald = 6.018, p value = 0.014, OR = 0.63, 95% CI = 0.44–0.91). This means that mothers with higher self-efficacy are less likely to experience postpartum depression. Similarly, family support also shows a significant negative association with postpartum depression (B = –0.518, Wald = 6.367, p value = 0.012, OR = 0.60, 95% CI = 0.40–0.89), indicating that greater family support reduces the risk of postpartum depression. These findings suggest that maternal self-efficacy and family support are both protective factors against postpartum depression, and their combined contribution highlights the importance of strengthening personal and social resources for mothers during the postpartum period.
DISCUSSION
This study demonstrates that maternal self-efficacy has a significant negative relationship with postpartum depression among mothers with a history of cryptic pregnancy. This aligns with the first objective of the study, which was to examine the association between self-efficacy and depressive symptoms. The finding supports Bandura’s theory of self-efficacy, which emphasizes the individual’s belief in their ability to organize and carry out tasks as a key factor in managing stress and emotional well-being [9]. Mothers with higher self-efficacy are able to adapt more effectively to the demands of motherhood, thereby lowering their vulnerability to depression. In the context of cryptic pregnancy, where mothers experience limited prenatal preparation, reduced medical supervision, and a sudden transition to motherhood, self-efficacy becomes an essential psychological resource [10]. Similar results have been reported in other countries. For instance, Chase et al. (2021) found that low maternal self-efficacy was strongly associated with higher levels of postpartum depression, suggesting that interventions aimed at improving confidence can be applied across different cultural settings [11].
The second objective of the study was to examine the role of family support in maternal mental health. Family support also showed a significant negative association with postpartum depression, reinforcing the importance of social and cultural contexts. Support from close relatives, especially spouses, provides emotional reassurance, practical help, and a sense of security, all of which buffer against the stress of childbirth and early parenting [12]. This result echoes findings from Delong et al. (2022), who demonstrated that social support plays a protective role in maternal well-being and strengthens maternal–infant interactions [13]. In Indonesia, where collectivist culture and family involvement in childcare are deeply rooted, family support becomes even more crucial. Mothers who experience cryptic pregnancy may feel shocked, unprepared, or even stigmatized due to the late discovery of their condition. In such situations, family members, particularly nurses within the community or family health settings, play a vital role in reducing stigma and supporting maternal adjustment [14].
The third objective of the study was to explore the combined effects of maternal self-efficacy and family support. The multivariate regression analysis confirmed that these two factors jointly predict postpartum depression, explaining nearly one-third of the variance. This suggests that personal psychological resources and external social support interact to shape maternal mental health outcomes. Comparable results have been found in other regions, where interventions that simultaneously enhance coping skills and involve family members proved more effective in reducing postpartum depression than those focusing on a single factor [15]. From a nursing perspective, this highlights the need for nurses to not only build mothers’ confidence through education and counseling but also to engage families in the care process [16]. The clinical implication is that nursing practice in both community and hospital settings should adopt a family-centered approach to maternal mental health. Furthermore, for future research, cross-cultural studies could provide valuable insights into how these factors operate in different healthcare systems and societies, and how nurses can tailor interventions to local needs.
Limitations
This study has several limitations. First, the use of a snowball sampling technique limits the representativeness of the sample and increases the risk of selection bias, as respondents were recruited through networks and may not reflect the broader population of mothers with cryptic pregnancy. Second, the reliance on self-reported questionnaires raises the possibility of recall bias and social desirability bias, where participants may underreport depressive symptoms or overstate family support. Third, this study did not control for other important psychosocial or environmental variables, such as marital conflict, domestic violence, or financial instability, which may independently contribute to postpartum depression. Fourth, the research was conducted in a single geographic area (Jombang Regency, East Java), and thus the findings may be influenced by local cultural norms and may not be generalizable to other populations with different sociocultural backgrounds. Finally, the cross-sectional design of this study prevents causal inferences, as it only identifies associations rather than longitudinal patterns. Future studies should adopt prospective or longitudinal designs with random sampling to establish causal pathways and improve external validity.
CONCLUSION
According to this study, maternal self-efficacy and family support are significant protective factors against postpartum depression among mothers with a history of cryptic pregnancy. Mothers with higher self-efficacy and stronger family support are less likely to experience depressive symptoms after childbirth. These findings reinforce previous evidence that both personal psychological resources and social environments are central in determining maternal mental health outcomes. The study highlights the urgent need for interventions that not only enhance maternal self-efficacy through counseling, psychoeducation, and peer support but also strengthen family involvement in postpartum care. Given that cryptic pregnancy presents unique psychological challenges due to the sudden recognition of pregnancy, integrated strategies focusing on both individual empowerment and family support systems may serve as effective preventive measures for postpartum depression.
Author Contributions
Study conceptualization and design (I.N., D.P., D.E.), data collection and analysis (I.N., D.E.), interpretation and manuscript drafting (I.N., D.P., D.E.), critical manuscript revision (D.E., D.P.). All authors have read and approval the final version of the manuscript.
Local Ethics Committee approval
This study was approved by the Research Ethics Committee of the Institute of Science and Health Technology Insan Cendekia Medika Jombang (reference number LP3M/ICME/ETIK/0425/2025 on February 10, 2025.
Conflict of Interest
The authors declare no conflicts of interest.
Funding Sources
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Acknowledgements
We extend our deepest gratitude to the mothers who shared their experiences of cryptic pregnancy and postpartum adjustment, as well as their families who supported this study by participating in interviews and completing the questionnaires. Without their openness, trust, and participation, this research would not have been possible.
REFERENCES
- Roddy Mitchell A, Gordon H, Lindquist A, Walker SP, Homer CSE, Middleton A, et al. Prevalence of Perinatal Depression in Low- and Middle-Income Countries: A Systematic Review and Meta-analysis. JAMA Psychiatry 2023;80:425–31. https://doi.org/10.1001/jamapsychiatry.2023.0069.
- Shorey S, Chee CYI, Ng ED, Chan YH, Tam WWS, Chong YS. Prevalence and incidence of postpartum depression among healthy mothers: A systematic review and meta-analysis. J Psychiatr Res 2018;104:235–48. https://doi.org/10.1016/j.jpsychires.2018.08.001.
- Bestari, A. D., Westriningrum, L., Didah, D., Gumilang, L., & Mandiri,
(2025). Faktor-Faktor yang Berhubungan dengan Resiko Depresi
Postpartum pada Ibu Nifas di Kota Bandung. Malahayati Nursing Journal,
7(2), 658-674. https://doi.org/10.33024/mnj.v7i2.17747- Cho H, Lee K, Choi E, Cho HN, Park B, Suh M, et al. Association between social support and postpartum depression. Sci Rep 2022;12. https://doi.org/10.1038/S41598-022-07248-7,.
- Han L, Zhang J, Yang J, Yang X, Bai H. Between Personality Traits and Postpartum Depression: The Mediated Role of Maternal Self-Efficacy. Neuropsychiatr Dis Treat 2022;18:597. https://doi.org/10.2147/NDT.S346327.
- Zarroug M, Altaf MF, Shaikh S, Tidjani A, Bashir O, Ayash MI, et al. The Prevalence and Risk Factors of Postpartum Depression Among Saudi Arabian Women—A Systematic Review and Meta-Analysis. Healthc 2025;13:2040. https://doi.org/10.3390/HEALTHCARE13162040/S1.
- Duckitt K. Cryptic pregnancy. Case Reports Women’s Heal 2023;38:e00503. https://doi.org/10.1016/J.CRWH.2023.E00503.
- Witungga RAA, Purwatiningrum DA, Gumanti KA, Sariati Y. The Relationship Of Maternal Self-Efficacy And Family Social Support To The Achivement Of Maternal Identity In Postpartum Women With A History Of Early Marriage. JKM (Jurnal Kebidanan Malahayati) 2024;10:1349–58. https://doi.org/10.33024/jkm.v10i12.17682.
- Adli FK. Edinburgh Post-natal Depression Scale (EPDS): Deteksi Dini dan Skrining Depresi Post-partum. J Kesehat 2022;13:430–6. https://doi.org/10.26630/JK.V13I2.2741.
- Shuriah NN, McFarland E, Spenn B, Butz McManus K, McManus B. Denial of Pregnancy or Cryptic Pregnancy. BIO4960 Pract Biol I 2024.
- Chase T, Shah A, Maines J, Fusick A. Psychotic pregnancy denial: a review of the literature and its clinical considerations. J Psychosom Obstet Gynecol 2021;42:253–7. https://doi.org/10.1080/0167482X.2020.1789584,.
- Chechko N, Losse E, Stickel S. A case report involving the experience of pervasive pregnancy denial: detailed observation of the first 12 postpartum weeks. BMC Psychiatry 2022;22. https://doi.org/10.1186/s12888-022-04377-1.
- Delong H, Eutrope J, Thierry A, Sutter-Dallay AL, Vulliez L, Gubler V, et al. Pregnancy denial: a complex symptom with life context as a trigger? A prospective case–control study*. BJOG An Int J Obstet Gynaecol 2022;129:485–92. https://doi.org/10.1111/1471-0528.16853,.
- Dlamini LP, Hsu YY, Shongwe MC, Wang ST, Gau ML. Maternal Self-Efficacy as a Mediator in the Relationship Between Postpartum Depression and Maternal Role Competence: A Cross-Sectional Survey. J Midwifery Women’s Heal 2023;68:499–506. https://doi.org/10.1111/JMWH.13478;JOURNAL:JOURNAL:18791565B;WGROUP:STRING:PUBLICATION.
- Mercan Y, Selcuk KT. Association between postpartum depression level, social support level and breastfeeding attitude and breastfeeding self-efficacy in early postpartum women. PLoS One 2021;16:e0249538. https://doi.org/10.1371/JOURNAL.PONE.0249538.
- César-Santos B, Bastos F, Dias A, Campos MJ. Family Nursing Care during the Transition to Parenthood: A Scoping Review. Healthcare 2024;12:515. https://doi.org/10.3390/HEALTHCARE12050515.
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.