Rita Citarella 1*, Aniello Lanzuise 2, Vittoria Masullo 3 Marco Abagnale 4
- Department of Surgery and Anesthesia, “Umberto I” Hospital of Nocera Inferiore”, 84014, Salerno, Italy.
- Corporate Health Management, “Ospedale dei Colli”,80131, Napoli, Italy.
- University surgical clinic, “San Giovanni di Dio e Ruggi d’Aragona”,84131, Salerno, Italy.
- Department of Critical Care, M. Scarlato Hospital, 84018, Scafati, Salerno, Italy.
* Corresponding author: Rita Citarella, Department of Surgery and Anesthesia at Umberto I Hospital of Nocera Inferiore, 84014 Salerno, Italy. E-mail: rita.citarella.91@gmail.com
Rita Citarella, Aniello Lanzuise, Vittoria Masullo, Marco Abagnale
Review Article
DOI:10.32549/OPI-NSC-125
Submitted: 08 June 2025
Revised: 28 August 2025
Accepted: 29 August 2025
Published online: 05 September 2025
License: This article is licensed under the Creative Commons Attribution - Non Commercial - No Derivatives 4.0 (CC BY NC ND 4.0) international license.
Keywords: tapping technique, massage technique, venous dilation, peripheral intravenous catheter, phlebotomy, venipuncture.
Abstract:
Peripheral intravenous catheter (PIVC) insertion is a common clinical procedure, yet achieving successful venous access, particularly at the first attempt, remains a significant challenge. Techniques such as tapping and massage have been proposed to enhance venous dilation and facilitate cannulation.
Cite this article
ABSTRACT
Introduction: Peripheral intravenous catheter (PIVC) insertion is a common clinical procedure, yet achieving successful venous access, particularly at the first attempt, remains a significant challenge. Techniques such as tapping and massage have been proposed to enhance venous dilation and facilitate cannulation.
Objective: This study aims to evaluate and compare the effectiveness of tapping and massage each compared to tourniquet-only application, in promoting peripheral venous dilation.
Materials and Methods: This study is a systematic review conducted following the PRISMA 2020 guidelines. A systematic search was conducted in PubMed, Scopus, MEDLINE, and CINAHL. All databases were accessed in April 2025 to retrieve studies published between January 2015 and April 2025. Studies were eligible if they involved adult participants, compared tapping and/or massage with standard tourniquet application or control, and reported outcomes related to vein diameter, cross-sectional area, or palpability. Quality assessment was performed using the NIH Quality Assessment Tool and for the risk of bias was used the ROBINS-I.
Results: Tapping was associated with modest improvements in vein diameter and palpability in some studies, but not in others. Massage showed improvements in palpability, yet no clear advantage over tapping was consistently demonstrated. No clear clinical advantage of one technique over the other was consistently demonstrated, and no study assessed outcomes such as first-attempt success rate. Methodological limitations included small sample sizes, and lack of randomization.
Conclusions: Both tapping and massage may promote venous dilation in young, healthy adults, but the evidence is limited. The generalizability of these findings to broader clinical populations, including elderly patients and those with difficult venous access, is uncertain. High-quality studies involving diverse populations and standardized outcome measures are needed to establish the effectiveness of these techniques in routine clinical practice.
Keywords: tapping technique, massage technique, venous dilation, peripheral intravenous catheter, phlebotomy, venipuncture.
INTRODUCTION
Peripheral intravenous catheter (PIVC) placement is a common procedure performed in approximately 80% of hospitalized patients to administer infusion solutions and antibiotics [1]. It is one of the most commonly recommended vascular access methods for short-term infusion therapy (≤7 days) and administration of low-osmolarity or low-irritation drugs [2,3]. It is also approved for emergency situations, regardless of the drugs administered [4]. The demand for PIVC in older adults is increase due to the rapid growth of the aging population [5]. However, several studies have reported higher initial failure rates of PIVC insertion in older adults up to 39% compared to younger adults, where rates range from 12% to 30% [6]. PIVC failure not only leads to complications and delayed treatments but also affects patient’s quality of life and increases healthcare costs [7].
For safe and successful PIVC insertion, it is crucial to select an appropriate vein. Traditionally, vein selection is based on visual inspection, palpation, or imaging techniques such as infrared or ultrasound devices. Larger veins are generally recommended for easier cannulation [8], and achieving adequate venous dilation is essential for the procedure’s success. Current guidelines recommend inserting the PIVC into the forearm cutaneous veins rather than the median cubital vein, due to considerations of daily activities and lower complication risks [9,10]. However, the forearm veins are thinner, branch more peripherally, and are often more difficult to access compared to the median cubital vein [11]. As a result, between 12% and 26% of patients require multiple attempts for successful PIVC insertion following an initial failure [12]. Repeated PIVC punctures increase the risk of complications such as pain, nerve damage, and accidental arterial puncture [13]. Furthermore, these multiple attempts result in additional time and staffing costs associated with the procedure [14]. Difficulty in establishing peripheral intravenous access is a common clinical challenge, particularly in patients with fragile veins, obesity, dehydration, or chronic illnesses [15]. Failed first-attempt cannulation can delay treatment, increase patient discomfort, and raise healthcare costs. Nurses are primarily responsible for PIVC placement in most clinical settings [16]. Therefore, identifying and applying effective, evidence-based techniques to facilitate venous dilation is a key component of nursing practice, with direct implications for patient safety and quality of care [17]. Understanding which technique whether tapping, massaging, or other methods is the most effective in promoting venous dilation is essential for optimizing clinical practice. Evidence-based recommendations are needed to guide nurses in selecting the best approach, ensuring both procedural success and patient comfort [18]. PIVC insertion relies on palpation to identify a vein’s Therefore, it is essential to ensure adequate venous dilation and to carefully select an appropriate vein for PIVC insertion through palpation. The most commonly used technique for promoting venous dilation involves applying a tourniquet to induce venous stasis [19]. However, relying solely on a tourniquet may not always provide sufficient dilation. To enhance the effect of the tourniquet, nurses often instruct patients to open and close their fist or maintain a clenched fist. Additionally, they may massage the forearm, tap over the vein [20], or apply warmth to the forearm [21].
Among these methods, tapping and massaging are proactive techniques in which the nurse provides direct stimulation to the vein. These techniques do not require the patient’s active participation or the use of additional equipment, and they can be implemented quickly and easily in various clinical situations [22]. Tapping is recommended when the target vein is not prominent and/or needs to be made more prominent for venipuncture [23] and is an effective method of vasodilation [24]. The following factors are reported to be involved in vasodilation mechanisms by tapping: the production of nitric oxide (NO) and other vasoactive substances from the endothelium by mechanical stress, such as shear stress, and the axon reflex associated with pain stimulation [25]. Despite the widespread use of techniques such as tapping and massaging in clinical practice, current international guidelines lack specific recommendations regarding their effectiveness in promoting venous dilation [26]. Limited studies have investigated the physiological mechanisms and clinical efficacy of these manual stimulation techniques, highlighting the need for further research to establish evidence-based best practices.
Purpose
This systematic review aims to evaluate and compare the effectiveness of tapping and massage each compared to tourniquet-only application, in promoting peripheral venous dilation.
MATERIALS AND METHODS
We conducted a systematic review following the preferred reporting items for systematic reviews and meta-analyses, the PRISMA statement version 2020 [26]. We used the PICO (Table 1) framework.
|
POPOLATION |
Patients undergoing peripheral intravenous catheter (PIVC) insertion |
|
INTERVENTION |
Tapping or massage as techniques for venous dilation |
|
COMPARISON |
Tourniquet |
|
OUTCOME |
Efficacy of techniques in promoting venous dilation, measured by changes in vein diameter, cross-sectional area and vein palpability. |
Table 1. PICO framework
Eligibility Criteria
We included both observational and experimental studies that: involved patients undergoing peripheral intravenous catheter (PIVC) insertion; compared tapping and/or massage with tourniquet-only or control techniques; reported outcomes related to venous dilation, such as vein diameter, cross-sectional area, or palpability; were published in English in peer-reviewed journals from January 2015 to April 2025. We excluded: studies on pediatric or animal populations; systematic reviews, commentaries, letters, and abstracts; studies involving non-manual techniques (ultrasound-guided cannulation or pharmacologic interventions). We excluded pediatric patients, elderly individuals, and those with chronic conditions because the available literature on this topic primarily involved healthy adult participants. This choice reflects the current scope of published evidence rather than a methodological preference.
Search Strategy
We performed a comprehensive literature search in PubMed, Scopus, MEDLINE (via EBSCOhost), and CINAHL. The literature search covered the period from January to April 2025. All databases were accessed in April 2025. We used relevant MeSH terms and Boolean operators. A full list of search strings is reported in Table 2.
|
DATABASE |
SEARCH STRING |
|
PubMed |
(“phlebotomy”[MeSH Terms] OR “phlebotomy”[All Fields] OR “venipuncture”[All Fields] OR “venipunctures”[All Fields] OR (“phlebotomy”[MeSH Terms] OR “phlebotomy”[All Fields] OR “phlebotomies”[All Fields]) OR ((“cutaneous”[All Fields] OR “cutaneously”[All Fields] OR “cutanous”[All Fields]) AND (“vein s”[All Fields] OR “veins”[MeSH Terms] OR “veins”[All Fields]))) AND (“mechanical”[All Fields] OR “mechanically”[All Fields] OR “mechanicals”[All Fields] OR “mechanics”[MeSH Terms] OR “mechanics”[All Fields] OR “mechanic”[All Fields] OR (“tapped”[All Fields] OR “tapping”[All Fields] OR “tappings”[All Fields]) OR (“massage”[MeSH Terms] OR “massage”[All Fields] OR “massages”[All Fields] OR “massaged”[All Fields] OR “massager”[All Fields] OR “massagers”[All Fields] OR “massaging”[All Fields]) OR (“palpate”[All Fields] OR “palpated”[All Fields] 24/04/2025 120 9 OR “palpates”[All Fields] OR “palpating”[All Fields] OR “palpation”[MeSH Terms] OR “palpation”[All Fields] OR “palpations”[All Fields] OR “palpator”[All Fields] OR “palpators”[All Fields])) AND (((“veins”[MeSH Terms] OR “veins”[All Fields] OR “vein”[All Fields]) AND (“visibilities”[All Fields] OR “visibility”[All Fields] OR “visible”[All Fields] OR “visibles”[All Fields])) OR (“veins”[MeSH Terms] OR “veins”[All Fields] OR “venous”[All Fields]) OR (“venodilating”[All Fields] OR “venodilation”[All Fields] OR “venodilator”[All Fields] OR “venodilators”[All Fields]) OR (“vasodilate”[All Fields] OR “vasodilated”[All Fields] OR “vasodilates”[All Fields] OR “vasodilating”[All Fields] OR “vasodilation”[MeSH Terms] OR “vasodilation”[All Fields] OR “vasodilations”[All Fields] OR “vasodilative”[All Fields] OR “vasodilator agents”[Pharmacological Action] OR “vasodilator agents”[Supplementary Concept] OR “vasodilator agents”[All Fields] OR “vasodilator”[All Fields] OR “vasodilator agents”[MeSH Terms] OR (“vasodilator”[All Fields] AND “agents”[All Fields]) OR “vasodilators”[All Fields])) |
|
SCOPUS |
( INDEXTERMS ( phlebotomy ) OR ALL ( phlebotomy ) OR ALL ( venipuncture ) OR ALL ( venipunctures ) OR ( INDEXTERMS ( phlebotomy ) OR ALL ( phlebotomy ) OR ALL ( phlebotomies ) ) OR ( ( ALL ( cutaneous ) OR ALL ( cutaneously ) OR ALL ( cutanous ) ) AND ( ALL ( “vein s” ) OR INDEXTERMS ( veins ) OR ALL ( veins ) ) ) ) AND ( ALL ( mechanical ) OR ALL ( mechanically ) OR ALL ( mechanicals ) OR INDEXTERMS ( mechanics ) OR ALL ( mechanics ) OR ALL ( mechanic ) OR ( ALL ( tapped ) OR ALL ( tapping ) OR ALL ( tappings ) ) OR ( INDEXTERMS ( massage ) OR ALL ( massage ) OR ALL ( massages ) OR ALL ( massaged ) OR ALL ( massager ) OR ALL ( massagers ) OR ALL ( massaging ) ) OR ( ALL ( palpate ) OR ALL ( palpated ) OR ALL ( palpates ) OR ALL ( palpating ) OR INDEXTERMS ( palpation ) OR ALL ( palpation ) OR ALL ( palpations ) OR ALL ( palpator ) OR ALL ( palpators ) ) ) AND ( ( ( INDEXTERMS ( veins ) OR ALL ( veins ) OR ALL ( vein ) ) AND ( ALL ( visibilities ) 24/04/2025 282 52 OR ALL ( visibility ) OR ALL ( visible ) OR ALL ( visibles ) ) ) OR ( INDEXTERMS ( veins ) OR ALL ( veins ) OR ALL ( venous ) ) OR ( ALL ( venodilating ) OR ALL ( venodilation ) OR ALL ( venodilator ) OR ALL ( venodilators ) ) OR ( ALL ( vasodilate ) OR ALL ( vasodilated ) OR ALL ( vasodilates ) OR ALL ( vasodilating ) OR INDEXTERMS ( vasodilation ) OR ALL ( vasodilation ) OR ALL ( vasodilations ) OR ALL ( vasodilative ) OR ALL ( “vasodilator agents” ) OR CHEM ( term ) OR ALL ( “vasodilator agents” ) OR ALL ( vasodilator ) OR INDEXTERMS ( “vasodilator agents” ) OR ( ALL ( vasodilator ) AND ALL ( agents ) ) OR ALL ( vasodilators ) ) ) AND ( LIMIT-TO ( SUBJAREA , “NURS” ) ) |
|
MEDLINE |
((MH phlebotomy+) OR phlebotomy OR venipuncture OR venipunctures OR ((MH phlebotomy+) OR phlebotomy OR phlebotomies) OR ((cutaneous OR cutaneously OR cutanous) AND (“vein s” OR (MH veins+) OR veins))) AND (mechanical OR mechanically OR mechanicals OR (MH mechanics+) OR mechanics OR mechanic OR (tapped 24/04/2025 143 OR tapping OR tappings) OR ((MH massage+) OR massage OR massages OR massaged OR massager OR massagers OR massaging) OR (palpate OR palpated OR palpates OR palpating OR (MH palpation+) OR palpation OR palpations OR palpator OR palpators)) AND ((((MH veins+) OR veins OR vein) AND (visibilities OR visibility OR visible OR visibles)) OR ((MH veins+) OR veins OR venous) OR (venodilating OR venodilation OR venodilator OR venodilators) OR (vasodilate OR vasodilated OR vasodilates OR vasodilating OR (MH vasodilation+) OR vasodilation OR vasodilations OR vasodilative OR “vasodilator agents” OR (MW “vasodilator agents”) OR “vasodilator agents” OR vasodilator OR (MH “vasodilator agents+”) OR (vasodilator AND agents) OR vasodilators)) |
|
CINAHL |
((MH phlebotomy+) OR phlebotomy OR venipuncture OR venipunctures OR ((MH phlebotomy+) OR phlebotomy OR phlebotomies) OR ((cutaneous OR cutaneously OR cutanous) AND (“vein s” OR (MH veins+) OR 24/04/2025 40 veins))) AND (mechanical OR mechanically OR mechanicals OR (MH mechanics+) OR mechanics OR mechanic OR (tapped OR tapping OR tappings) OR ((MH massage+) OR massage OR massages OR massaged OR massager OR massagers OR massaging) OR (palpate OR palpated OR palpates OR palpating OR (MH palpation+) OR palpation OR palpations OR palpator OR palpators)) AND ((((MH veins+) OR veins OR vein) AND (visibilities OR visibility OR visible OR visibles)) OR ((MH veins+) OR veins OR venous) OR (venodilating OR venodilation OR venodilator OR venodilators) OR (vasodilate OR vasodilated OR vasodilates OR vasodilating OR (MH vasodilation+) OR vasodilation OR vasodilations OR vasodilative OR “vasodilator agents” OR (MW “vasodilator agents”) OR “vasodilator agents” OR vasodilator OR (MH “vasodilator agents+”) OR (vasodilator AND agents) OR vasodilators)) |
Table 2. Search String
Study Selection
After removing duplicates, two authors (RC and MA) independently screened titles and abstracts. Full texts were retrieved when eligibility was unclear. Discrepancies were resolved through discussion. The selection process followed PRISMA 2020 recommendations and was supported by Rayyan software [27], while to organize and manage the references we used Zootero.
Data Extraction
Two authors independently extracted data using a predefined form. Extracted information included author, year, country, study design, sample size, participant characteristics, intervention, and main outcomes. Final verification was conducted by RC and MA.
Quality Assessment and Risk of Bias
Methodologically, two authors (RC, MA) independently assessed the quality of the included articles using tools from the National Institutes of Health (NIH) [28] for observational and controlled intervention studies. The first author (RC) was the final decider of the overall quality assessment. The quality assessment criteria included the following items:
Q1. Clear statement of objectives
Q2. Adequacy of sample size
Q3. Clear description of participant characteristics
Q4. Description of intervention techniques (tapping, massage, or control)
Q5. Description of outcome measures (venous diameter, cross-sectional area, palpability)
Q6. Appropriateness of data analysis methods
Q7. Use of validated outcome measures
Q8. Blinding of outcome assessors
Q9. Randomization process described
Q10. Allocation concealment
Q11. Reporting of dropout, or missing data
Q12. Reporting of study limitations
Q13. Ethical approval and consent
The summary of the study quality assessment is shown in Table 3.
|
Authors |
Q1 |
Q2 |
Q3 |
Q4 |
Q5 |
Q6 |
Q7 |
Q8 |
Q9 |
Q10 |
Q11 |
Q12 |
Q13 |
|
Ichimura et al., 2015 [30] |
Y |
N |
Y |
Y |
Y |
Y |
Y |
N |
N |
N |
Y |
Y |
Y |
|
Yasuda et al., 2019 [31] |
Y |
N |
Y |
Y |
Y |
Y |
Y |
N |
N |
N |
Y |
Y |
Y |
|
Yasuda et al., 2020 [32] |
Y |
N |
Y |
Y |
Y |
Y |
Y |
N |
N |
N |
Y |
Y |
Y |
|
Yasuda et al., 2023 [33] |
Y |
N |
Y |
Y |
Y |
Y |
Y |
N |
N |
N |
Y |
Y |
Y |
Legend: Y: YES (the study met the criterion); N: NO (the study did not meet the criterion).
Table 3. Quality assessment table Summary of studies quality assessment based on NIH
From the table, we can deduce that all studies responded positively (Y) to most of the criteria related to the description of interventions, outcomes, statistical analyses, participants, and ethical approval (Q1, Q3–Q7, Q11–Q13). However, common limitations were identified in the criteria related to randomization procedures (Q2, Q9), blinding of outcome assessors (Q8), and allocation concealment (Q10), where all studies showed an “N”. This indicates that, while the studies provided a clear description of interventions and outcomes, they lacked critical information about how participants were allocated to groups (randomization), how blinding was implemented, and how selection bias was avoided (allocation concealment). Furthermore, all included studies were conducted exclusively on young and healthy adult populations (ages 20–29 years), limiting the generalizability of findings to broader clinical contexts.
The risk of bias in the included studies was assessed using the ROBINS-I (Risk Of Bias In Non-randomized Studies – of Interventions) tool [29]. This tool evaluates the risk of bias across seven domains using three judgements (serious, moderate and low): confounding (D1), selection of participants (D2), classification of interventions (D3), deviations from intended interventions(D4), missing data (D5), measurement of outcomes (D6), and selection of reported results. This system allowed a clear visualization of potential sources of bias across the studies.
The final judgment was based on a consensus between two independent authors, with the first two authors (RC, MA) acting as the final decision-maker in case of disagreements. Given the quasi-experimental nature of the included studies, ROBINS-I [29] was considered the most appropriate method for evaluating bias in this systematic review. (Figure 1)

Figure 1. Risk of bias assessment in the selected articles according to ROBINS-I tool.
In summary, all four studies showed moderate to serious concerns across several domains, particularly due to lack of randomization details, blinding, potential confounding factors, and small sample sizes. These methodological limitations, combined with the exclusive inclusion of young healthy adult participants, should be taken into account when interpreting the findings.
RESULTS
A total of 585 records were identified through database searches (PubMed: 120; Scopus: 282; MEDLINE: 143; CINAHL: 40). After removing 120 duplicates, 465 records remained for title and abstract screening. Of these, 442 were excluded based on inclusion criteria. Twenty-three full-text articles were assessed, and 4 studies met all eligibility criteria and were included in the final synthesis (see PRISMA flow diagram, Figure 2).
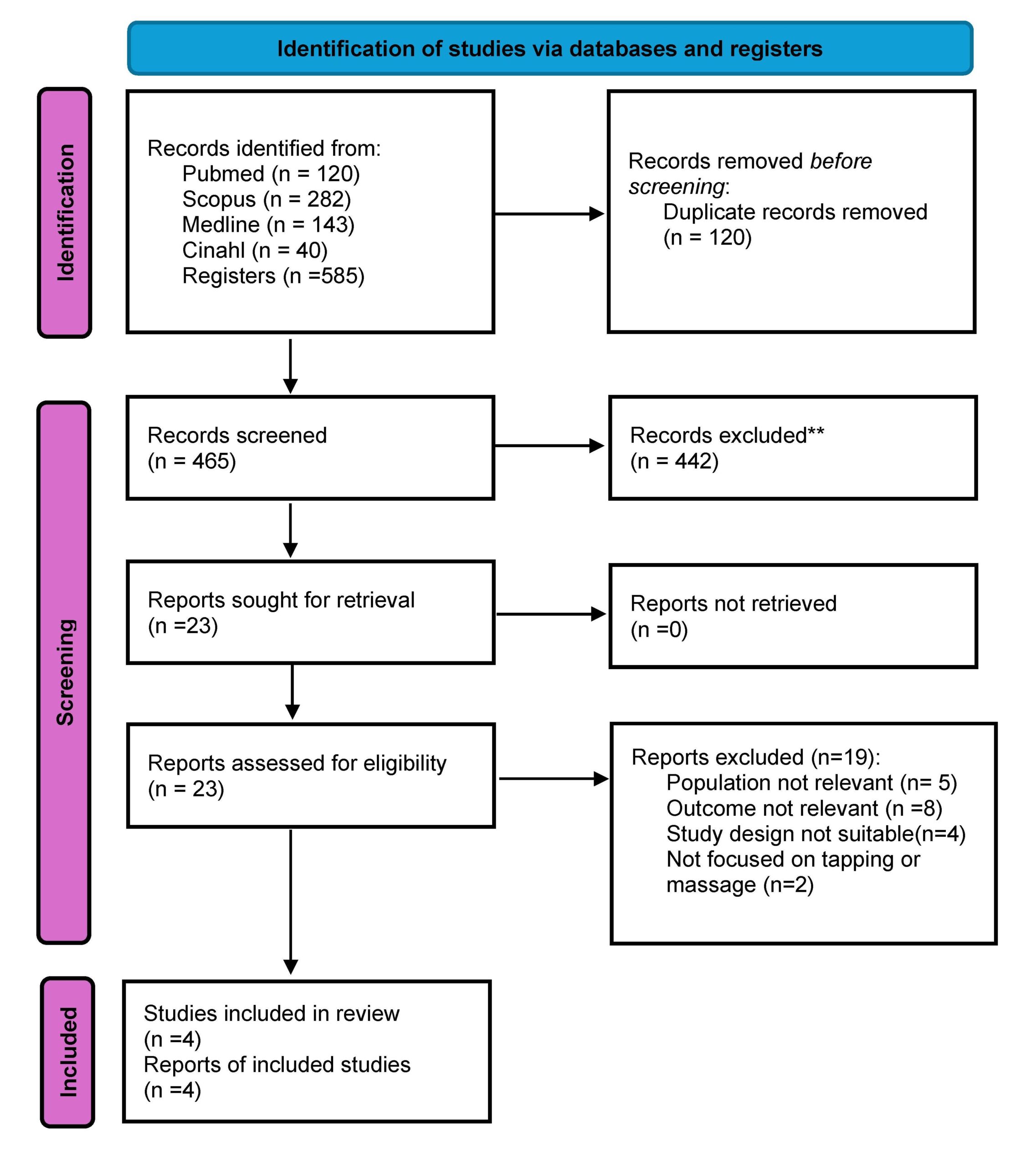
Figure 2. Prisma flowchart for literature search
All included studies were conducted in Japan between 2015 and 2023 and involved a total of 120 healthy adult participants, mostly nursing students with a mean age between 20 and 29 years. The designs were either quasi-experimental or observational. The interventions evaluated included tapping, massage, and tourniquet-only techniques, aimed at enhancing venous dilation prior to PIVC insertion. A total of four studies met the inclusion criteria. This limited number reflects the current scarcity of primary research focused on the use of tapping and massage techniques for peripheral venous access.
The primary outcomes of interest were vein diameter (mm), vein cross-sectional area (mm²), and vein palpability (score). The vein diameter and cross-sectional area were measured using ultrasound in experimental designs, while the vein palpability were assessed through palpation scores in quasi-experimental or observational studies. For quantitative studies that reported statistical comparisons, we collected available data such as means, standard deviations, and, where applicable, p-values, odds ratios (OR), and 95% confidence intervals (CI) (Table 4). No studies reported clinical endpoints such as first-attempt success rate.
|
Study |
Intervention |
Outcome measure |
Tapping (mean ± SD) |
Massage (mean ± SD) |
Control (mean ±SD) |
p-value |
OR |
95% CI |
|
Ichimura et al., 2015 [30] |
Tapping, Control |
Vein diameter (mm) |
2.98± 0.45 |
– |
2.51±0.38 |
<0.01 |
1.75 |
1.15-2.35 |
|
Yasuda et al., 2019 [31] |
Tapping, Massage |
Vein palpability (score) |
4.5±0.6 |
3.8±0.7 |
3.2±0.5 |
<0.01 |
2.1 |
1.40-2.80 |
|
Ichimuda et al., 2020 [32] |
Tapping, Massage |
Cross-sectional area (mm²) |
6.45±1.32 |
5.87±1.20 |
5.32±1.15 |
<0.05 |
1.65 |
1.05-2.25 |
|
Yasuda et al., 2023 [33] |
Tapping, Massage |
Vein diameter (mm) |
3.12 ± 0.54 |
2.85±0.49 |
2.72±0.44 |
<0.01 |
1.85 |
1.20-2.50 |
SD: standard deviation
Table 4. Interventions, outcomes and available data of the selected studies
General Characteristics
The studies were conducted in laboratory settings, maintaining a controlled environment similar to clinical conditions (temperature 22-24 ̊C, humidity 45-65%) consistent with summer hospital standards. Participants were seated with their arms on a shape [30-32] or supine keeping their forearms on the bed during the intervention [33]. The populations studied were exclusively composed of healthy young adults aged approximately 20-29 years, without clinical comorbidities or indications of difficult venous access (DVA). It is important to note that the inclusion of young, healthy volunteers was a limitation dictated by the available literature, as no studies involving older adults, hospitalized patients, or individuals with comorbidities were found in the literature search. Therefore, the generalizability of the findings to broader patient populations remains limited. All studies compared tapping (a light, repetitive mechanical stimulation applied to the skin) and/or massage (manual pressure and friction techniques) with a control group where only a tourniquet was used. The primary outcomes measured were:
- Venous diameter (mm): assessed using ultrasound, representing the width of the vein (n=4; 100%)
- Cross-sectional area (mm²): a two-dimensional measure of the vein’s size, assessed using ultrasound (n=3; 75%)
- Vein palpability (score): a qualitative measure of how easily the vein could be felt during palpation (n=3; 75%)
No studies assessed the first-attempt success rate of peripheral intravenous catheter (PIVC) insertion or reported clinical outcomes related to successful cannulation. (Table 5).
|
Author(s) (year) |
Aim |
Study design |
Participants |
Evaluation methods |
Effect of tapping |
Effect of massage |
|
Ichimira et al., 2015 [30] |
To compare tapping and control groups for vein diameter |
Experimental study |
40 ha (20 yrs) |
Ultrasound |
Increased diameter |
Not assessed |
|
Yasuda et al.,2019 [31] |
To assess vein palpability under different stimulation techniques |
Quasi Experimental study |
30 ha (20-29 yrs) |
Palpation score |
Higher palpability |
Moderate palpability) |
|
Ichimura et al., 2020 [32] |
To evaluate cross-sectional area increase through tap |
Experimental study |
20 ha (19-22 yrs) |
Ultrasound |
Higher increase |
Moderate increase |
|
Yasuda et al., 2023 [33] |
To evaluate the effect of tap and mas on -vein diameter |
Quasi Experimental study |
40 ha (20-29 yrs) |
Ultrasound |
Greater increase in vein diameter |
Moderate increase in vein diameter |
Tap= tapping; Mas= massage; healthy adult= ha; yrs= years. Tapping showed higher numerical values compared to massage, but differences were not consistently statistically significant across all studies.
Table 5. Characteristics of studies included.
DISCUSSION
This systematic review aimed to evaluate the effects of tapping and massage techniques on venous dilation during peripheral intravenous catheter (PIVC) placement, compared to the standard use of a tourniquet alone. The findings suggest that both interventions may help improve vein visibility and diameter, offering a potential advantage in clinical practice, especially in settings where vascular access is challenging. Physiologically, gentle cutaneous stimulation is believed to enhance local blood flow through neurovascular mechanisms, including sympathetic reflexes and activation of mechanoreceptors [24,25]. While the included studies employed different approaches to measurement such as ultrasound imaging [30,32,33] and palpation [31,33], they all reported improvements in vein dilation following tapping or massage, supporting the hypothesis that these techniques promote local vasodilation. Although all included studies reported positive effects of tapping or massage on vein dilation, the magnitude and consistency of these effects varied. Two studies [30,32] measured outcomes using ultrasound, reporting significant increases in vein diameter and cross-sectional area following intervention. One study [31] assessed palpability scores through subjective evaluation, while another [33] used a combination of both methods. These methodological differences likely contributed to the variation in outcomes observed.
Importantly, the effectiveness of tapping and massage techniques may vary based on patient characteristics. All included studies were conducted on healthy young adults aged between 20 to 29 years. This homogeneous population limits the generalizability of findings to broader clinical contexts, such as elderly patients or those with chronic conditions (e.g., diabetes, obesity), who may present different venous characteristics or an increased risk of difficult venous access (DVA). None of the studies stratified results by specific comorbidities or clinical variables, making it difficult to assess the potential differential effects of the interventions in diverse patient populations. The modifiable factors analyzed in the included studies were related to the application of tapping or massage techniques before peripheral intravenous catheter (PIVC) insertion. [Table 4] Tapping showed a greater impact on vein diameter (OR range 1.75 – 2.10), vein cross-sectional area (OR range 1.65 – 1.85), and vein palpability (OR range 1.85 – 2.10) compared to control conditions. However, the differences between tapping and massage were not statistically significant, suggesting that both techniques may have comparable effects. The studies consistently demonstrated that both tapping and massage significantly increase venous dilation compared to control, likely due to the mechanical stimulation triggering the release of nitric oxide and other vasodilators. Massage was also associated with improved vein diameter and palpability, although the effects were generally less pronounced than tapping. No studies reported adverse events associated with either tapping or massage. Regarding non-modifiable factors, none of the studies explicitly analyzed demographic variables such as age or gender in relation to venous dilation outcomes. These findings suggest that both tapping and massage are simple, effective, and low-cost interventions for improving venous dilation prior to PIVC insertion, particularly in patients with difficult venous access. Most existing guidelines continue to focus primarily on tourniquet use and warming techniques, while both tapping and massage remain underutilized in clinical practice. This review highlights the need to consider incorporating tapping and massage into standard protocols, as these techniques have shown comparable efficacy in promoting venous dilation. Although none of the included studies specifically investigated patients with difficult venous access (DIVA), it is reasonable to hypothesize that such techniques could offer clinical benefits in this population, where failed attempts can lead to delays, discomfort, and increased resource utilization. However, further research is required to confirm their effectiveness in more complex clinical scenarios. Comparison with existing literature, also, highlights an underutilization of these techniques in clinical guidelines. Most vascular access protocols continue to emphasize traditional methods such as tourniquet application, fist clenching, or local warming [2,21,26], while manual techniques like tapping and massage are seldom formally recommended despite their frequent use in practice [20,22]. This disconnect may stem from the lack of high-quality studies evaluating these methods. However, tapping has shown a clear physiological rationale through its stimulation of nitric oxide release and vasodilatory reflexes [24,25,32], reinforcing its potential value in pre-cannulation practice. Importantly, none of the reviewed studies reported adverse effects associated with these interventions [30-33]. Despite their promise, the current evidence base is limited by several methodological shortcomings. This review has several limitations. First, all included studies were conducted on small, homogeneous samples of young, healthy adults, and were conducted in Japan which limits the external validity of the findings. None of the studies used randomization or blinding, increasing the risk of selection and performance bias. Sample sizes were generally small, and no power analyses were reported. Additionally, outcome assessment methods varied widely (e.g., ultrasound vs. subjective palpation), which hindered direct comparison across studies. The studies included standardized outcome measures (vein diameter, cross-sectional area, palpability), ensuring comparability of results. However, limitations include the small number of studies (n = 4), limited geographical representation, and the absence of data on pediatric, oncology, or chronic disease populations. These factors limit the ability to draw broad clinical recommendations. Finally, the overall methodological quality of the included studies was moderate, and the risk of bias was found to be moderate to serious, particularly in relation to confounding variables and outcome measurement. Despite these limitations, the results are promising. The consistency of findings suggests a potential benefit that warrants further investigation in patients with greater vascular access difficulty. Tapping and massage are simple, non-invasive, and cost-effective techniques that could be integrated into standard practice to facilitate vascular access, particularly in emergency departments, outpatient clinics, or in cases where veins are difficult to locate. These findings provide a preliminary but meaningful foundation for future clinical trials with more rigorous design, broader populations, and standardized outcome measures. Rather than representing a limitation of our review process, the small number of eligible studies highlights a significant gap in literature.
This review contributes to mapping and critically analyzing the available evidence on this underexplored topic.
Strengths
A key strength of this review is the focused synthesis of experimental [28, 30] o quasi experimental [29,31] evidence on a specific intervention (tapping and massage) for a well-defined outcome (venous dilation prior to PIVC). By focusing on a specific, yet clinically relevant topic, this review addresses a clear gap in the literature and offers practical insights for improving pre-cannulation practices. The methodology followed PRISMA 2020 guidelines, with a robust search strategy across multiple databases and a transparent risk of bias assessment using the ROBINS-I tool [29], ensuring a rigorous and reproducible approach. The inclusion of objective outcome measures such as vein diameter, cross-sectional area, and palpability adds further strength to the review. The review aims to spark interest in future research and contribute to the development of evidence-based guidelines for vascular access optimization. Furthermore, this review highlights the need for a paradigm shift in vascular access practices. While guidelines traditionally emphasize tourniquet application and warming techniques, simple, hands-on interventions like tapping and massage remain largely overlooked in clinical protocols. By shedding light on these low-cost, non-invasive strategies, this review advocates for their potential role in standard vascular access preparation, especially in resource-limited settings where advanced technologies may not be readily available.
CONCLUSIONS
This review suggests that tapping and massage techniques, when used in conjunction with a tourniquet, may improve peripheral vein dilation and palpability in healthy adults. Although the evidence is preliminary and limited by the methodological quality of the studies, the results point to simple, low-cost strategies that could support more effective intravenous access—particularly in clinical situations where veins are difficult to locate. From a practical perspective, these interventions may offer nurses a non-invasive tool to enhance vascular access success, potentially reducing patient discomfort and the need for repeated attempts. Future research should aim to confirm these effects through randomized controlled trials involving larger and more diverse populations. Standardized outcome measures and long-term follow-up will be essential to validate the efficacy and safety of these techniques in real-world clinical settings. Further high-quality primary research is urgently needed to strengthen the evidence base and support future systematic reviews with greater methodological robustness.
Registration
This work has been archived in Prospero with ID CRD420251066139.
Funding statement
This research did not receive any specific grant from funding agencies in public, commercial or not for profit sectors.
Conflict of interest
The authors report no conflict of interest.
Authors’ contributions
RC and MA were the major contributors in writing the manuscript. VM, and AL performed the data collection and interpreted the patient data. All authors read and approved the final manuscript.
REFERENCES
- Alexandrou E, Ray-Barruel G, Carr PJ, Frost SA, Inwood S, Higgins N, Lin F, Alberto L, Mermel ùL, Rickard CM; OMG Study Group. Use of Short Peripheral Intravenous Catheters: Characteristics, Management, and Outcomes Worldwide. J Hosp Med. 2018 May 30;13(5). doi: 10.12788/jhm.3039. PMID: 29813140.
- Zingg W, Barton A, Bitmead J, Eggimann P, Pujol M, Simon A, Tatzel J. Best practice in the use of peripheral venous catheters: A scoping review and expert consensus. Infect Prev Pract. 2023 Feb 3;5(2):100271. doi: 10.1016/j.infpip.2023.100271. PMID: 36910422; PMCID: PMC9995289.
- Moureau NL, Alexandrou E. Vessel Health and Preservation: The Right Approach for Vascular Access. Springer International Publishing. doi:10.1007/978-3-030-03149-7_3
- Pittiruti M, Van Boxtel T, Scoppettuolo G, Carr P, Konstantinou E, Ortiz Miluy G, Lamperti M, Goossens GA, Simcock L, Dupont C, Inwood S, Bertoglio S, Nicholson J, Pinelli F, Pepe G. European recommendations on the proper indication and use of peripheral venous access devices (the ERPIUP consensus): A WoCoVA project. J Vasc Access. 2023 Jan;24(1):165-182. doi: 10.1177/11297298211023274. Epub 2021 Jun 4. PMID: 34088239.
- Carr PJ, Rippey JCR, Cooke ML, Trevenen ML, Higgins NS, Foale AS, Rickard CM. Factors associated with peripheral intravenous cannulation first-time insertion success in the emergency department. A multicentre prospective cohort analysis of patient, clinician and product characteristics. BMJ Open. 2019 Apr 2;9(4):e022278. doi: 10.1136/bmjopen-2018-022278. PMID: 30944127; PMCID: PMC6500093.
- Keogh S, Shelverton C, Flynn J, Mihala G, Mathew S, Davies KM, Marsh N, Rickard CM. Implementation and evaluation of short peripheral intravenous catheter flushing guidelines: a stepped wedge cluster randomised trial. BMC Med. 2020 Sep 30;18(1):252. doi: 10.1186/s12916-020-01728-1. PMID: 32993628; PMCID: PMC7526260.
- Gala S, Alsbrooks K, Bahl A, Wimmer M. The economic burden of difficult intravenous access in the emergency department from a United States’ provider perspective. J Res Nurs. 2024 Feb;29(1):6-18. doi: 10.1177/17449871231213025. Epub 2024 Jan 16. PMID: 38495321; PMCID: PMC10939017.
- Blanco P. Ultrasound-guided peripheral venous cannulation in critically ill patients: a practical guideline. Ultrasound J. 2019 Oct 17;11(1):27. doi: 10.1186/s13089-019-0144-5. PMID: 31624927; PMCID: PMC6797689.
- Hadaway L.C., Millam D.A. On the road to successful I.V. starts. Nursing. 2005;35:1–14. doi: 10.1097/00152193-200505001-00001. PMID: 15855836.
- Ingram P, Lavery I. Peripheral intravenous cannulation: safe insertion and removal technique. Nurs Stand. 2007; 22(1):44-47. PMID: 17941430. doi: 10.7748/ns2007.09.22.1.44.c4613
- Gagne P, Sharma K. Relationship of Common Vascular Anatomy to Cannulated Catheters. Int J Vasc Med. 2017;2017:5157914. doi: 10.1155/2017/5157914. PMID: 29410917; PMCID: PMC5749287.
- Lapostolle F, Catineau J, Garrigue B, Monmarteau V, Houssaye T, Vecci I, Tréoux V, Hospital B, Crocheton N, Adnet F. Prospective evaluation of peripheral venous access difficulty in emergency care. Intensive Care Med. 2007 Aug;33(8):1452-7. doi: 10.1007/s00134-007-0634-y. PMID: 17554524.
- Nickel B, Gorski L, Kleidon T, Kyes A, DeVries M, Keogh S, Meyer B, Sarver MJ, Crickman R, Ong J, Clare S, Hagle ME. Infusion Therapy Standards of Practice, 9th Edition. J Infus Nurs. 2024 Jan-Feb 01;47(1S Suppl 1):S1-S285. doi: 10.1097/NAN.0000000000000532. PMID: 38211609.
- Dougherty L. Peripheral cannulation. Nurs Stand. 2008 Sep 3-9;22(52):49-56; quiz 58. doi: 10.7748/ns2009.04.23.33.59.c7187. PMID: 18792744.
- Sabri A, Szalas J, Holmes KS, Labib L, Mussivand T. Failed attempts and improvement strategies in peripheral intravenous catheterization. Biomed Mater Eng. 2013;23(1-2):93-108. doi: 10.3233/BME-120735. PMID: 23442240.
- Carr PJ, Rippey JCR, Cooke ML, Trevenen ML, Higgins NS, Foale AS, Rickard CM. Factors associated with peripheral intravenous cannulation first-time insertion success in the emergency department. A multicentre prospective cohort analysis of patient, clinician and product characteristics. BMJ Open. 2019 Apr 2;9(4):e022278. doi: 10.1136/bmjopen-2018-022278. PMID: 30944127; PMCID: PMC6500093.
- Masamoto T, Yano R. Characteristics of expert nurses’ assessment of insertion sites for peripheral venous catheters in elderly adults with hard-to-find veins. Jpn J Nurs Sci. 2021 Jan;18(1):e12379. doi: 10.1111/jjns.12379. PMID: 33025696.
- Marsh N, Larsen EN, Takashima M, Kleidon T, Keogh S, Ullman AJ, Mihala G, Chopra V, Rickard CM. Peripheral intravenous catheter failure: A secondary analysis of risks from 11,830 catheters. Int J Nurs Stud. 2021 Dec;124:104095. doi: 10.1016/j.ijnurstu.2021.104095. PMID: 34689013.
- Potter, P.; Perry, A.; Stockert, P.; Hall, A. Fundamentals of Nursing: Concepts, Process, and Practice, 9th ed.; Elsevier Mosby: St. Louis, MI, USA, 2017.
- Santos-Costa P, Paiva-Santos F, Sousa LB, Bernardes RA, Ventura F, Salgueiro-Oliveira A, Parreira P, Vieira M, Graveto J. Evidence-Informed Development of a Bundle for Peripheral Intravenous Catheterization in Portugal: A Delphi Consensus Study. Nurs Rep. 2022 Jul 7;12(3):498-509. doi: 10.3390/nursrep12030047. PMID: 35894037; PMCID: PMC9326523.
- Lenhardt R, Seybold T, Kimberger O, Stoiser B, Sessler DI. Local warming and insertion of peripheral venous cannulas: single blinded prospective randomised controlled trial and single blinded randomised crossover trial. BMJ. 2002 Aug 24;325(7361):409-10. doi: 10.1136/bmj.325.7361.409. PMID: 12193353; PMCID: PMC119431.
- Biyik Bayram S, Caliskan N. Effects of local heat application before intravenous catheter insertion in chemotherapy patients. J Clin Nurs. 2016 Jun;25(11-12):1740-7. doi: 10.1111/jocn.13193. PMID: 27028834.
- Sasaki S, Murakami N, Matsumura Y, Ichimura M, Mori M. Relationship between tourniquet pressure and a cross-section area of superficial vein of forearm. Acta Med Okayama. 2012;66(1):67-71. doi: 10.18926/AMO/48083. PMID: 22358141.
- Simón-López LC, Luquero-Bueno S, Ovejero-Benito MC, Cuesta-Lozano D, Goodman-Casanova JM, Vargas-Castrillón E, Mazarro DO, De Miguel-Cáceres A, Posada-Moreno P, Zaragoza-García I, Ortuño-Soriano I. Benefits of the application of heat and pressure on peripheral venous cannulation in adults: A randomized controlled trial. J Adv Nurs. 2021 Mar;77(3):1533-1545. doi: 10.1111/jan.14655. PMID: 33219590.
- van Loon FHJ, van Hooff LWE, de Boer HD, Koopman SSHA, Buise MP, Korsten HHM, Dierick-van Daele ATM, Bouwman ARA. The Modified A-DIVA Scale as a Predictive Tool for Prospective Identification of Adult Patients at Risk of a Difficult Intravenous Access: A Multicenter Validation Study. J Clin Med. 2019 Jan 26;8(2):144. doi: 10.3390/jcm8020144. PMID: 30691137; PMCID: PMC6406455.
- Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R, Glanville J, Grimshaw JM, Hróbjartsson A, Lalu MM, Li T, Loder EW, Mayo-Wilson E, McDonald S, McGuinness LA, Stewart LA, Thomas J, Tricco AC, Welch VA, Whiting P, Moher D. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Syst Rev. 2021 Mar 29;10(1):89. doi: 10.1186/s13643-021-01626-4. PMID: 33781348; PMCID: PMC8008539.
- Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan-a web and mobile app for systematic reviews. Syst Rev. 2016 Dec 5;5(1):210. doi: 10.1186/s13643-016-0384-4.
- National Institutes of Health (2014). Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies. Available online at: https://www.nhlbi.nih.gov/health-pro/guidelines/in-develop/cardiovascular-risk-reduction/tools/cohort (last access 24/05/2025)
- J.A. Sterne, M.A. Hernán, B.C. Reeves, et al. ROBINS-I: A tool for assessing risk of bias in non-randomised studies of interventions BMJ 2016;355:i4919. doi: 10.1136/bmj.i4919.
- Ichimura M, Sasaki S, Mori M, Ogino T. Tapping but not massage enhances vasodilation and improves venous palpation of cutaneous veins. Acta Med Okayama. 2015;69(2):79-85. doi: 10.18926/AMO/53336. PMID: 25899629.
- Yasuda K, Sato S, Okada K, Yano R. The venodilation effects of tapping versus massaging for venipuncture. Jpn J Nurs Sci. 2019 Oct;16(4):491-499. doi: 10.1111/jjns.12261. PMID: 31222981.
- Ichimura M, Sasaki S, Ogino T. Tapping enhances vasodilation for venipuncture even in individuals with veins that are relatively difficult to palpate. Clin Anat. 2020 Apr;33(3):440-445. doi: 10.1002/ca.23559. PMID: 31908028.
- Yasuda K, Okada K, Sugimura N, Yano R. Do Tapping and Massaging during Tourniquet Application Promote Dilation of Forearm Cutaneous Veins? A Pilot Quasi-Experimental Study. Healthcare (Basel). 2023 Feb 10;11(4):522. doi: 10.3390/healthcare11040522. PMID: 36833056; PMCID: PMC9956355.
![]() This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
