Hideaki Furuki 1*, Nao Sonoda 1, Akiko Morimoto 1
- Graduate School of Nursing, Osaka Metropolitan University, Osaka, Japan
* Corresponding author: Hideaki Furuki, MSc, RN, PHN, Osaka Metropolitan University, Graduate School of Nursing, 1–4–3 Asahi-machi, Abeno Ward, Osaka City, Osaka 545–8585, Japan. E-mail address: s21262g@omu.ac.jp
Hideaki Furuki, Nao Sonoda, Akiko Morimoto
Original article
DOI:10.32549/OPI-NSC-128
Submitted: 07 September 2025
Revised: 24 October 2025
Accepted: 29 October 2025
Published online: 05 November 2025
License: This article is licensed under the Creative Commons Attribution - Non Commercial - No Derivatives 4.0 (CC BY NC ND 4.0) international license.
Keywords: Education, Evidence-based practice, Nurse, Knowledge, Skills
Abstract:
Although evidence-based practice (EBP) is a core nursing competency, little is known about the extent to which nurses are educated on the five steps of EBP, including the specific educational content within each step, in pre-licensure and in-service education, and how these educational experiences relate to their knowledge and skills.
Cite this article
ABSTRACT
Introduction: Although evidence-based practice (EBP) is a core nursing competency, little is known about the extent to which nurses are educated on the five steps of EBP, including the specific educational content within each step, in pre-licensure and in-service education, and how these educational experiences relate to their knowledge and skills.
Objectives: To examine the extent of nurses’ experience of receiving specific educational content related to each step of EBP in pre-licensure and in-service education, and to evaluate the associations between these experiences and EBP knowledge and skills.
Methods: This cross-sectional questionnaire survey was conducted between June and September 2022 among 2,672 employed hospital nurses in Japan. EBP knowledge and skills were measured using the Japanese version of the EBP Questionnaire. Experience of receiving EBP education in pre-licensure and in-service education was assessed using items developed from EBP textbooks and core competency literature. Analysis of covariance and relative importance analysis were conducted to evaluate the association between the experience of receiving EBP education and EBP knowledge and skills.
Results: 718 nurses (26.9%) were included in the final analysis. The findings showed that nurses’ experience of receiving EBP education was generally limited, with fewer than 25% having learned any EBP-education item, except literature databases, in pre-licensure education. Similarly, fewer than 25% have learned each EBP-education item in in-service education. The adjusted mean EBP knowledge and skills score increased progressively with the extent of education received across the five steps of EBP (20.6 for no steps to 35.5 for five steps), showing a consistent dose–response relationship (p for trend < 0.001). Relative importance analysis showed that the Step 4 and Step 5 items were placed toward the upper end of the contribution rankings.
Conclusions: To effectively improve nurses’ EBP knowledge and skills, providing a practical, EBP-specific program that comprehensively covers all five EBP steps would be essential. Additionally, developing programs for training educators would also be essential.
Keywords: Education, Evidence-based practice, Nurse, Knowledge, Skills.
INTRODUCTION
Evidence-based practice (EBP) is defined as a problem-solving approach that can be used to deliver health care that integrates the best evidence from research and patient care data with clinician expertise as well as patient preferences and values [1]. The risks of adverse outcomes such as mortality, falls, and ventilator-associated pneumonia are reported to be reduced when EBP is implemented [2-5]. Both the American Nurses Association and the American Association of Colleges of Nursing have identified EBP as a core competency for nurses, reflecting its critical role in improving patient care [6,7]. Therefore, promoting EBP education for nurses is recognized as a global priority in nursing. Previous studies on the experience of receiving EBP education have reported its prevalence, instructional hours, and delivery formats (e.g., integration into research methodology or statistics courses) in pre-licensure education [8-11]. Since EBP implementation requires knowledge and skills related to its five steps (Step 1: ask, Step 2: acquire, Step 3: appraise, Step 4: apply, and Step 5: assess), it is essential to receive education on each of these steps. However, no study has examined the extent to which nurses have received specific educational content related to each step of EBP, such as how to formulate clinical questions using the PICO (Patient, Intervention, Comparison, Outcome) or PECO (Patient, Exposure, Comparison, Outcome) framework, and search using databases for clinical guidelines and systematic reviews [12]. Clarifying which aspects of EBP education have been adequately covered and which have not is essential for developing an effective EBP educational program. Additionally, although previous studies have examined the relationship between whether nurses received EBP education and EBP knowledge and skills, no research has assessed how the extent of education received across the five EBP steps relates to these competencies [13-15]. Furthermore, there has been no evaluation of which EBP-education items have a greater contribution to EBP knowledge and skills. Such evaluations would clarify how the comprehensiveness of EBP education relates to levels of EBP knowledge and skills, and which EBP-education items have a greater contribution to EBP competency. This, in turn, would inform the design and prioritization of more effective educational programs. Previous studies have identified factors associated with nurses’ EBP knowledge and skills, including age, gender, educational level, years of clinical nursing experience, employment position, advanced practice certification, participation in EBP education, experience conducting research, and resources and organizational support for EBP [12]. These factors are potential confounders when examining associations between educational exposure and EBP competency. This study was conceptually guided by Kirkpatrick’s evaluation model [16], which conceptualizes training outcomes across four cumulative levels: Level 1—Reaction (how favorable, engaging, and relevant the training is), Level 2—Learning (the degree to which participants acquire intended including knowledge, skills, and confidence), Level 3—Behavior (the degree to which participants apply what they learned on the job), and Level 4—Results (the degree to which targeted organizational outcomes occur).
In our study, the primary endpoints—EBP knowledge and skills—map to Level 2 (Learning), and the extent of experience of receiving EBP education was treated as the educational input expected to produce a dose–response in Level-2 outcomes.
Objective
This study aimed to examine the extent of hospital nurses’ experience of receiving specific educational content related to each step of EBP in both pre-licensure and in-service education in Japan. We also evaluated the associations between these educational experiences and EBP knowledge and skills, and which EBP-education items have a greater contribution.
MATERIALS AND METHODS
Study design and participants
This cross-sectional questionnaire survey was conducted between June and September 2022 among hospital nurses from six hospitals in Western Japan (three universities: two private and one public). Sites were selected for convenience based on pre-existing collaborations and confirmed site willingness. All registered nurses working at these hospitals who met the eligibility criteria were invited to participate. The inclusion criteria were as follows: 1) currently employed as a nurse at a hospital and 2) directly involved in patient care. Nurses in managerial positions, such as directors of nursing, assistant directors of nursing, and head nurses, were excluded. A structured, self-administered, paper-based questionnaire was distributed to participants, and completed questionnaires were returned in sealed envelopes via mail. The study protocol was prepared in accordance with the Declaration of Helsinki and approved by the institutional review board of Osaka Metropolitan University (approval date: June 24, 2022; approval number: 2022–215). The present study used data from the same project as our prior publication [17], though it addresses different research aims and conducts independent analyses.
Data collection procedures and instruments for data collection
Participants were provided with a written explanation of the study’s purpose, procedures, and measures to ensure confidentiality, and that participation was voluntary. Informed consent, considered “appropriate consent” under relevant ethical guidelines [18], was obtained by having participants check a box in the consent section of the questionnaire to indicate their agreement. Data collection was coordinated through the nursing departments at the participating hospitals. After obtaining site approvals, the research team mailed a paper-based questionnaire to the Director of Nursing at each collaborating hospital. The directors then distributed the questionnaire to unit head nurses, who in turn handed it to the eligible staff nurses. All questionnaires were self-administered in paper format; no electronic survey was used, and no individual email addresses or staff contact lists were provided to the researchers. Completed questionnaires were placed by respondents into sealed envelopes and returned by postal mail directly to the study office, thereby maintaining respondent anonymity and confidentiality.
EBP knowledge and skills
EBP knowledge and skills were measured using the Japanese version of the Evidence-Based Practice Questionnaire (EBPQ-J) [18], a validated translation of the original EBPQ developed by Upton and Upton (2006). Both versions have demonstrated high reliability and validity [19-21]. Total scores for EBP knowledge and skills range from 9 to 63, with higher scores indicating greater knowledge and skills. The original EBPQ comprises three subscales: EBP implementation, attitudes toward EBP, and EBP knowledge and skills. The EBPQ-J reorganizes these into four subscales by dividing the knowledge and skills domain into two components: EBP knowledge and skills related to research (score range: 7–49) and EBP knowledge and skills related to practice (score range: 2–14). EBP knowledge and skills were assessed using the total scores of the two subdomains in accordance with the components of the EBPQ. Questionnaire items on the EBP knowledge and skills related to research subscale include statements such as, “Ability to apply necessary information to hypotheses in research question studies,” “Knowledge of methods to search for and obtain evidence,” and “Ability to determine whether the contents of a study are valid (level of bias).” Questionnaire items on the EBP knowledge and skills related to practice subscale include statements such as “Ability to share ideas and information with colleagues” and “Ability to convey new information regarding care with colleagues.” Cronbach’s alpha for the EBP knowledge and skills subscale in the present study was 0.95.
Based on previous literature on factors associated with EBP knowledge and skills [12], we collected the following factors as potential confounders in evaluating the relationship between the experience of receiving EBP education and EBP knowledge and skills using a self-administered questionnaire. These included: age, gender, educational level (diploma, associate degree, bachelor’s degree, or master’s degree), years of clinical nursing experience, employment position (staff nurse, charge nurse, or assistant head nurse), advanced practice certification (none, certified nurse, or certified specialist nurse), number of times conducting research, access to a literature database (yes or no), and organizational attitude toward EBP (“Is your workplace a positive attitude toward EBP?” non-positive, neither, moderately positive, or very positive). Regarding advanced practice certification in Japan, certified nurse specialists are required to complete a graduate program, which aligns with the qualifications for advanced practice roles in other countries, such as nurse practitioners or clinical nurse specialists [22]. In contrast, certified nurses are registered nurses who have completed specialized clinical training, although a master’s degree is not required for this certification.
Experience of receiving EBP education
The experience of receiving EBP education was measured for both pre-licensure and in-service education. EBP-education items were developed based on key textbooks on EBP [23-25] and literature on EBP core competencies for healthcare professionals [26]. Items were categorized into knowledge and skills components and aligned with the five steps of EBP. Step 1 (Ask) included knowledge of clinical questions and the PICO or PECO framework, as well as skills in formulating clinical questions using that framework. Step 2 (Acquire) included knowledge of efficient evidence searching, such as searching in the following order: systems, summaries, clinical practice guidelines, systematic reviews, and original articles. It also encompassed knowledge of the characteristics and search methods of literature databases (e.g., PubMed and Ichushi Web, a bibliographic database indexing primarily Japanese-language literature on medicine, nursing, dentistry, and pharmacy) and of databases for clinical practice guidelines and systematic reviews (e.g., Minds Guideline Library, a database for domestic clinical practice guidelines published in Japan, and the Cochrane Library). Furthermore, Step 2 included skills in conducting searches for evidence using an efficient order and relevant databases. Step 3 (Appraise) included knowledge of differences in levels of evidence according to study design, random and systematic error, and descriptive and inferential statistics, along with skills in critically appraising literature based on these domains. Step 4 (Apply) included knowledge of the four components required to apply evidence in practice—patient’s clinical state and circumstances, research evidence, patient’s preferences and actions, and clinical expertise—as well as skills in applying these components in clinical decision-making. Step 5 (Assess) included the skill of evaluating the outcomes of EBP. For each EBP-education item, participants were asked to rate their experience on a five-point Likert scale: “Have not learned at all,” “Have not learned,” “Neither,” “Have learned,” and “Have learned a lot.”
Statistical analyses
First, descriptive statistics were used to summarize participants’ characteristics. Continuous variables, such as age and EBP knowledge and skills scores, are presented as means and standard deviations, and dichotomous and categorical data as frequencies and percentages. Next, the experience of receiving EBP education in both pre-licensure and in-service education was summarized for each EBP-education item using frequencies and percentages across the five response categories. Third, analysis of covariance (ANCOVA) was conducted to examine the association between the extent of education received across the five steps of EBP and EBP knowledge and skills. In this model, the extent of education received across the five steps of EBP was treated as the independent variable, and the EBP knowledge and skills score as the dependent variable. In this study, due to the small number of participants who responded “Have learned a lot,” this response was combined with “Have learned” into a single category labeled “Have learned” to improve interpretability. Consequently, the level to which EBP education has been experienced was categorized into four levels: “Have not learned at all,” “Have not learned,” “Neither,” and “Have learned.” For each EBP-education item, the level of educational experience was determined based on responses for both pre-licensure and in-service education. Specifically, when participants reported different amounts of education received across the two educational settings, the higher of the two responses was retained, based on the following rank order: “Have not learned at all” < “Have not learned” < “Neither” < “Have learned.” For instance, if a participant responded, “Have not learned at all” in pre-licensure education and “Have learned” in in-service education, their overall experience for that item was categorized as “Have learned.” The extent of education received across the five steps of EBP was derived by considering participants to have received education on a given step only if they responded “Have learned” to all items within that step. Based on the number of steps for which this condition was met, participants were categorized into one of six groups: those who had received education on no, one, two, three, four, or all five steps. The model included potential confounding variables, including gender, educational level, years of clinical nursing experience, position, advanced practice certification, number of times of experience conducting research, access to a literature database, and organizational attitude toward EBP. Adjusted means and 95% confidence intervals were determined for each category, and a p-value for linear trend was calculated from the linear component (F test) of a polynomial contrast within the ANCOVA framework. Fourth, ANCOVA was conducted for each EBP-education item to examine the association between item-specific experience of receiving EBP education and EBP knowledge and skills. All models used the same four ordered categories (“Have not learned at all,” “Have not learned,” “Neither,” “Have learned”) and the same set of covariates as above. Adjusted means and 95% confidence intervals were determined for each category of level to which EBP education has been experienced, and p-values for linear trends were calculated analogously from the linear component (F test) of a polynomial contrast. The effect sizes were calculated using partial η². For all ANCOVA models, we assessed residual normality with Q–Q plots and homogeneity of variance with residual-versus-fitted plots.
Finally, relative importance analysis was conducted using the Lindemann–Merenda–Gold (LMG) method with the R package “relaimpo” to quantify the contribution of each EBP-education item to EBP knowledge and skills [27,28]. The LMG method is particularly useful when explanatory variables are correlated, as it quantifies each variable’s relative importance by averaging its incremental contribution to R² across all possible orderings [29,30]. Each EBP-education item was dummy-coded as a four-level factor (“Have not learned at all,” “Have not learned,” “Neither,” or “Have learned”). The model included the same covariates as in the ANCOVA (gender, educational level, years of clinical nursing experience, employment position, advanced practice certification, number of times of experience conducting research, access to a literature database, and organizational attitude toward EBP). Contributions were expressed as the percentage of the EBP-education items-only R² (i.e., the proportion of variance explained by the EBP-education items after adjustment for covariates), and 95% confidence intervals were obtained via bootstrap resampling (B = 1,000). We used complete-case analysis because overall missingness was low and missingness often occurred in blocks across item batteries, limiting cross-variable information for imputation. All analyses were performed using IBM SPSS Statistics for Windows version 29 software (IBM SPSS Japan, Tokyo, Japan) or R version 4.4.2 (R Foundation for Statistical Computing, Vienna, Austria). All reported p-values were two-tailed, and values of <0.05 were considered statistically significant.
RESULTS
In total, 2,672 nurses were invited to participate. Of these, 766 (28.7%) responded to the mail survey. After excluding those with missing data, 718 nurses (26.9%) were included in the final analysis. The characteristics of the participants are presented in Table 1. The mean age (standard deviation) was 36.0 (10.0) years; more than 90% of the participants were female, 40.1% had a bachelor’s degree, and 4.0% had a master’s degree. More than half the participants had more than 10 years of clinical experience, most were employed at hospitals with access to a literature database, and more than 60% reported that their organization had a positive attitude toward EBP. The mean EBP knowledge and skills score (standard deviation) was 22.4 (10.4) points, indicating a relatively low level of EBP-related competency among the participants.
Variables Personal factors Age (years) 36.0 (10.0) Gender Women 663 (92.3) Men 55 (7.7) Educational level Diploma or associate degree 400 (55.7) Bachelor’s degree 287 (40.0) Master’s degree 31 (4.3) Years of clinical nursing experience ≤3 159 (22.1) 4–9 160 (22.3) ≥10 399 (55.6) Employment position Staff nurse 653 (90.9) Charge nurse or assistant head nurse 65 (9.1) Advanced practice certification No 692 (96.4) Certified nurse or certified specialist nurse 26 (3.6) Number of times conducting research 0 322 (44.9) 1 146 (20.3) ≥2 250 (34.8) Work-environment factors Literature database No 29 (4.0) Yes 689 (96.0) Organizational attitude toward EBP Nonpositive 82 (11.4) Neither 186 (25.9) Moderately positive 281 (39.2) Very positive 169 (23.5) Outcome EBP knowledge and skills score (points) 22.4 (10.4) Note: Age and EBP knowledge and skills score are presented as mean (standard deviation). Dichotomous data and categorical data are presented as n (%). EBP, evidence-based practice.
Table 1. Participants’ characteristics (n=718).
Experience of receiving EBP education in pre-licensure education
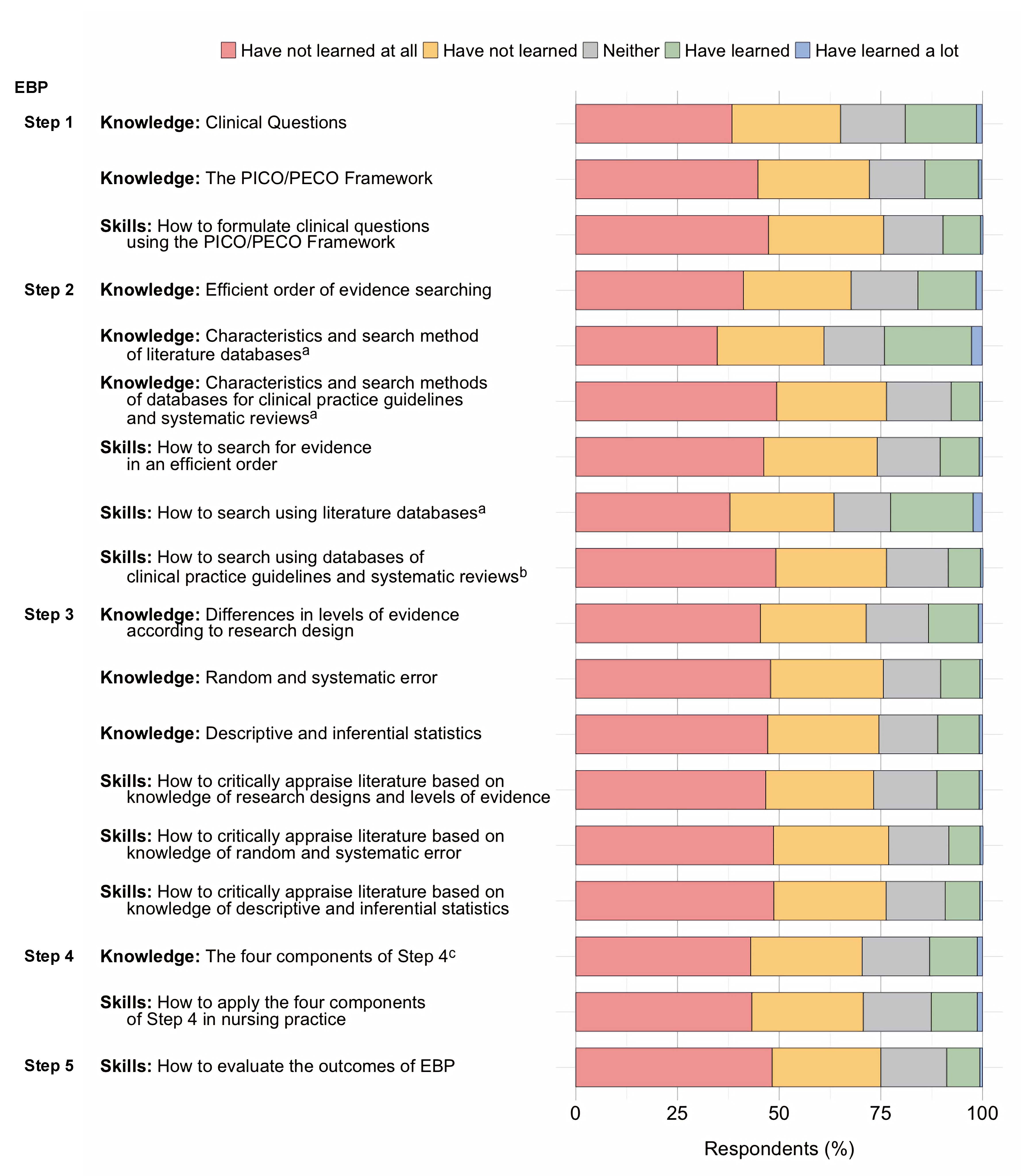
Figure 1 illustrates the experience of receiving EBP education in pre-licensure education among Japanese hospital nurses.
Figure 1. Experience of receiving EBP education in pre-licensure education among Japanese hospital nurses
Note on Figure 1
Proportions represent the distribution of responses to each EBP-education item. Items were categorized into knowledge and skills components and aligned with the five steps of EBP.
a Literature databases refer to resources such as PubMed and Ichushi Web, a bibliographic database indexing primarily Japanese-language literature on medicine, nursing, dentistry, and pharmacy.
b Databases for clinical practice guidelines and systematic reviews refer to resources such as the Minds Guideline Library, a database for domestic clinical practice guidelines published in Japan, and the Cochrane Library.
c The four components are as follows: (1) the patient’s clinical state and circumstances, (2) research evidence, (3) the patient’s preferences and actions, and (4) clinical expertise.
EBP: evidence-based practice; PECO: Patient, Exposure, Comparison, Outcome; PICO: Patient, Intervention, Comparison, Outcome.
Overall, participants’ experience of receiving pre-licensure EBP education was limited. The proportion of nurses who reported that they had learned about skills-related items was lower than the proportion who reported that they had learned about knowledge-related items. Approximately 40% of the nurses reported having learned about characteristics and search methods of literature databases, though fewer than 25% reported having learned about any of the other EBP-education items. Fewer than 10% of nurses reported that they had learned how to formulate clinical questions using the PICO/PECO framework regarding characteristics and search methods of databases for clinical practice guidelines and systematic reviews, how to conduct a search using databases for clinical practice guidelines and systematic reviews, and how to evaluate the outcomes of EBP. Table 2 provides detailed results for each EBP-education item.
Have not learned at all Have not learned Neither Have learned Have learned a lot
EBP – Step 1 (Ask) Knowledge Clinical Questions 253 (35.2) 207 (28.8) 109 (15.2) 132 (18.4) 17 (2.4) The PICO/PECO framework 341 (47.5) 202 (28.1) 92 (12.8) 70 (9.7) 13 (1.8) Skills How to formulate clinical questions using the PICO/PECO framework 378 (52.6) 207 (28.8) 86 (12.0) 42 (5.8) 5 (0.7) EBP – Step 2 (Acquire) Knowledge Efficient order of evidence searching 250 (34.8) 215 (29.9) 109 (15.2) 128 (17.8) 16 (2.2) Characteristics and search methods of literature databases a 181 (25.2) 157 (21.9) 81 (11.3) 237 (33.0) 62 (8.6) Characteristics and search methods of databases for clinical practice guidelines and systematic reviews b 365 (50.8) 199 (27.7) 106 (14.8) 42 (5.8) 6 (0.8) Skills How to search for evidence in an efficient order 314 (43.7) 198 (27.6) 113 (15.7) 81 (11.3) 12 (1.7) How to search using literature databasesa 217 (30.2) 138 (19.2) 84 (11.7) 215 (29.9) 64 (8.9) How to search using databases for clinical practice guidelines and systematic reviews b 350 (48.7) 204 (28.4) 114 (15.9) 43 (6.0) 7 (1.0) EBP – Step 3 (Appraise) Knowledge Differences in levels of evidence according to research design 266 (37.0) 165 (23.0) 99 (13.8) 156 (21.7) 32 (4.5) Random and systematic error 285 (39.7) 162 (22.6) 99 (13.8) 143 (19.9) 29 (4.0) Descriptive and inferential statistics 266 (37.0) 155 (21.6) 112 (15.6) 162 (22.6) 23 (3.2) Skills How to critically appraise literature based on knowledge of research designs and levels of evidence 275 (38.3) 164 (22.8) 127 (17.7) 136 (18.9) 16 (2.2) How to critically appraise literature based on knowledge of random and systematic error 297 (41.4) 184 (25.6) 137 (19.1) 92 (12.8) 8 (1.1) How to critically appraise literature based on knowledge of descriptive and inferential statistics 292 (40.7) 186 (25.9) 140 (19.5) 92 (12.8) 8 (1.1) EBP – Step 4 (Apply) Knowledge The four components of Step 4c 270 (37.6) 202 (28.1) 152 (21.2) 88 (12.3) 6 (0.8) Skills How to apply the four components of Step 4 in nursing practice c 274 (38.2) 201 (28.0) 150 (20.9) 87 (12.1) 6 (0.8) EBP – Step 5 (Assess) Skills How to evaluate the outcomes of EBP 333 (46.4) 199 (27.7) 132 (18.4) 51 (7.1) 3 (0.4) Note: Experience of receiving EBP education is presented as the number of participants (%).
a Literature databases refer to resources such as PubMed and Ichushi Web, a bibliographic database indexing primarily Japanese-language literature on medicine, nursing, dentistry, and pharmacy.
b Databases for clinical practice guidelines and systematic reviews refer to resources such as the Minds Guideline Library, a database for domestic clinical practice guidelines published in Japan, and the Cochrane Library.
c The four components are as follows: (1) the patient’s clinical state and circumstances, (2) research evidence, (3) the patient’s preferences and actions, and (4) clinical expertise.
EBP: evidence-based practice: PECO: Patient, Exposure, Comparison, Outcome; PICO: Patient, Intervention, Comparison, Outcome.
Table 2. Experience of receiving EBP education in pre-licensure education among Japanese hospital nurses (n=718)
Experience of receiving EBP education in in-service education
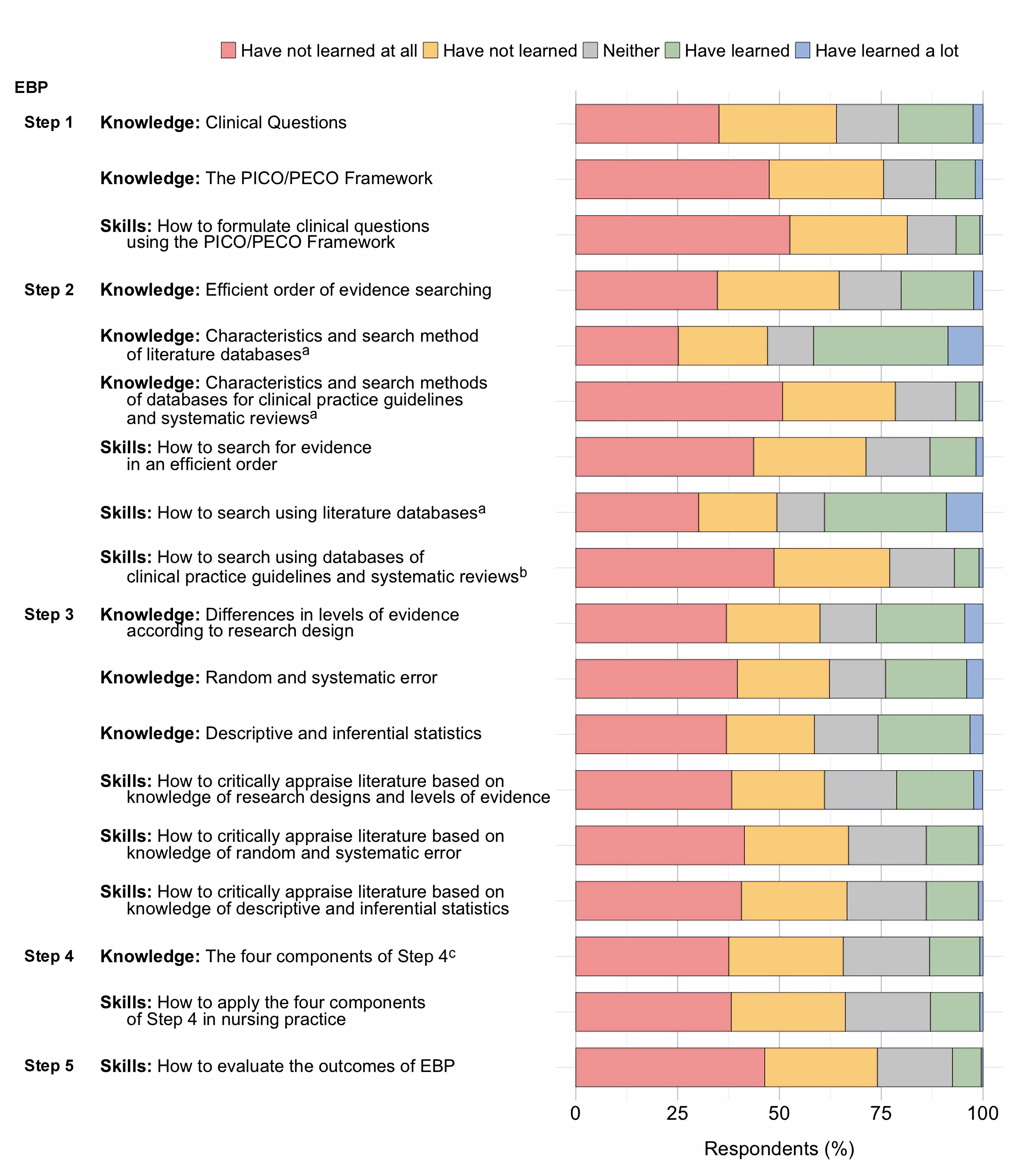
Figure 2 illustrates the experience of receiving EBP education in in-service education among Japanese hospital nurses.
Note on Figure 2
Proportions represent the distribution of responses to each EBP-education item. Items were categorized into knowledge and skills components and aligned with the five steps of EBP.
a Literature databases refer to resources such as PubMed and Ichushi Web, a bibliographic database indexing primarily Japanese-language literature on medicine, nursing, dentistry, and pharmacy.
b Databases for clinical practice guidelines and systematic reviews refer to resources such as the Minds Guideline Library, a database for domestic clinical practice guidelines published in Japan, and the Cochrane Library.
c The four components are as follows: (1) the patient’s clinical state and circumstances, (2) research evidence, (3) the patient’s preferences and actions, and (4) clinical expertise.
EBP, evidence-based practice, PECO, Patient, Exposure, Comparison, Outcome; PICO, Patient, Intervention, Comparison, Outcome.
Figure 2. Experience of receiving EBP education in in-service education among Japanese hospital nurses.
Overall, participants’ experience of receiving EBP education was limited. For all EBP-education items, fewer than 25% of nurses reported that they had learned about the content, with the percentage of respondents who reported learning about skills-related items being even lower than the percentage of those who reported learning about knowledge-related items. Fewer than 10% of nurses reported that they learned how to formulate clinical questions using the PICO/PECO framework, characteristics and search methods of databases for clinical practice guidelines and systematic reviews, how to conduct a search using databases for clinical practice guidelines and systematic reviews, how to critically appraise literature based on knowledge of random and systematic error, how to critically appraise literature based on knowledge of descriptive and inferential statistics, and how to evaluate the outcomes of EBP. Table 3 provides detailed results for each EBP-education item.
Have not learned at all Have not learned Neither Have learned Have learned a lot EBP – Step 1 (Ask) Knowledge Clinical Questions 276 (38.4) 192 (26.7) 114 (15.9) 126 (17.5) 10 (1.4) The PICO/PECO framework 322 (44.8) 197 (27.4) 98 (13.6) 95 (13.2) 6 (0.8) Skills How to formulate clinical questions using the PICO/PECO framework 340 (47.4) 203 (28.3) 105 (14.6) 66 (9.2) 4 (0.6) EBP – Step 2 (Acquire) Knowledge Efficient order of evidence searching 296 (41.2) 190 (26.5) 118 (16.4) 103 (14.3) 11 (1.5) Characteristics and search methods of literature databases a 250 (34.8) 188 (26.2) 107 (14.9) 154 (21.4) 19 (2.6) Characteristics and search methods of databases for clinical practice guidelines and systematic reviews b 355 (49.4) 194 (27.0) 114 (15.9) 50 (7.0) 5 (0.7) Skills How to search for evidence in an efficient order 332 (46.2) 200 (27.9) 111 (15.5) 69 (9.6) 6 (0.8) How to search using literature databasesa 272 (37.9) 184 (25.6) 100 (13.9) 146 (20.3) 16 (2.2) How to search using databases for clinical practice guidelines and systematic reviews b 353 (49.2) 195 (27.2) 109 (15.2) 57 (7.9) 4 (0.6) EBP – Step 3 (Appraise) Knowledge Differences in levels of evidence according to research design 326 (45.4) 187 (26.0) 110 (15.3) 88 (12.3) 7 (1.0) Random and systematic error 344 (47.9) 199 (27.7) 101 (14.1) 69 (9.6) 5 (0.7) Descriptive and inferential statistics 339 (47.2) 196 (27.3) 104 (14.5) 73 (10.2) 6 (0.8) Skills How to critically appraise literature based on knowledge of research designs and levels of evidence 335 (46.7) 190 (26.5) 112 (15.6) 75 (10.4) 6 (0.8) How to critically appraise literature based on knowledge of random and systematic error 349 (48.6) 203 (28.3) 106 (14.8) 55 (7.7) 5 (0.7) How to critically appraise literature based on knowledge of descriptive and inferential statistics 350 (48.7) 198 (27.6) 104 (14.5) 61 (8.5) 5 (0.7) EBP – Step 4 (Apply) Knowledge The four components of Step 4 c 309 (43.0) 197 (27.4) 119 (16.6) 84 (11.7) 9 (1.3) Skills How to apply the four components of Step 4 in nursing practice c 311 (43.3) 197 (27.4) 120 (16.7) 81 (11.3) 9 (1.3) EBP – Step 5 (Assess) Skills How to evaluate the outcomes of EBP 347 (48.3) 192 (26.7) 116 (16.2) 58 (8.1) 5 (0.7) Note: Experience of receiving EBP education is shown as the number of participants (%).
a Literature databases refer to resources such as PubMed and Ichushi Web, a bibliographic database indexing primarily Japanese-language literature on medicine, nursing, dentistry, and pharmacy.
b Databases for clinical practice guidelines and systematic reviews refer to resources such as the Minds Guideline Library, a database for domestic clinical practice guidelines published in Japan, and the Cochrane Library.
c The four components are as follows: (1) the patient’s clinical state and circumstances, (2) research evidence, (3) the patient’s preferences and actions, and (4) clinical expertise.
EBP: evidence-based practice; PECO: Patient, Exposure, Comparison, Outcome; PICO: Patient, Intervention, Comparison, Outcome.
Table 3. Experience of receiving EBP education in in-service education among Japanese hospital nurses (n=718)
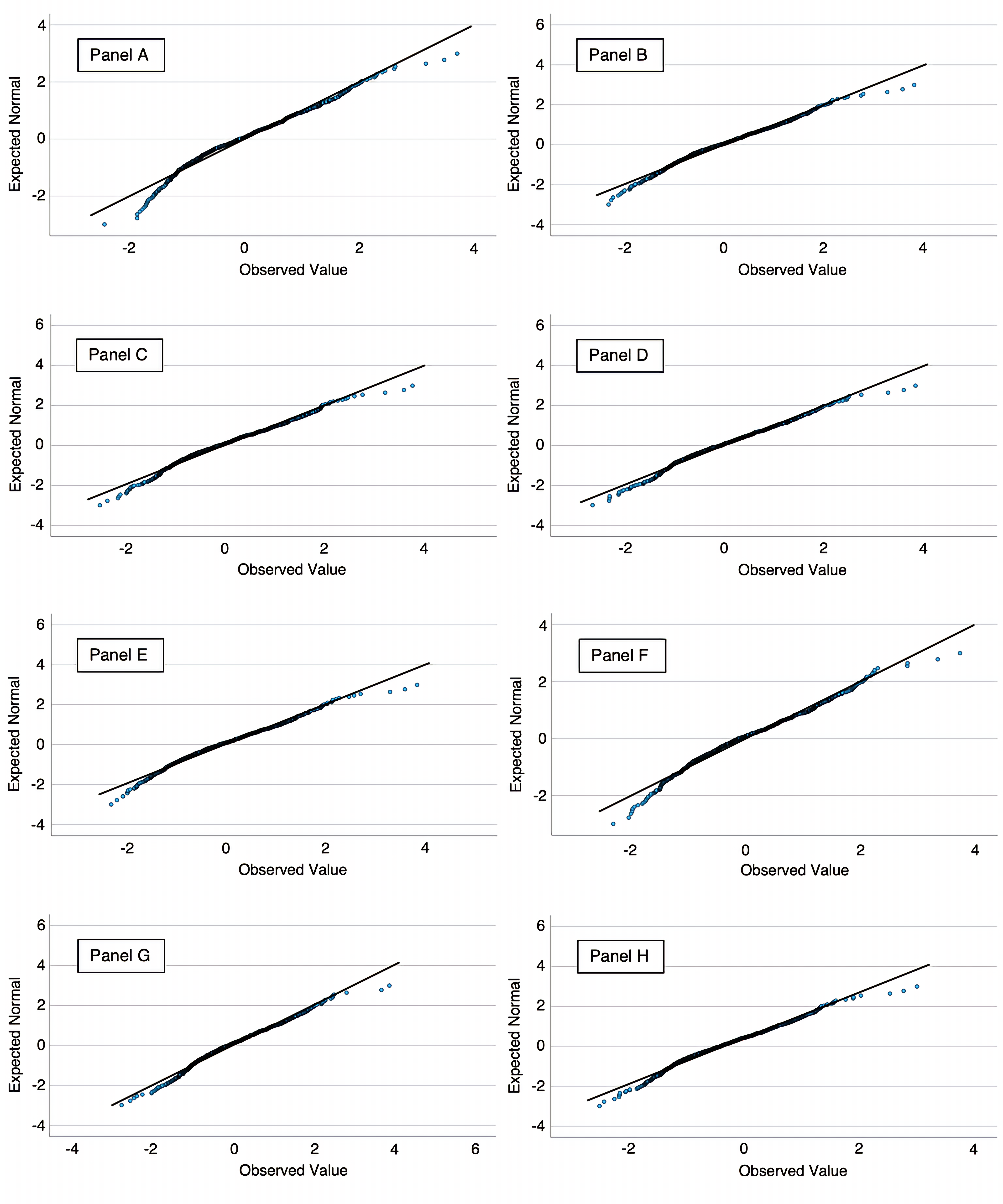
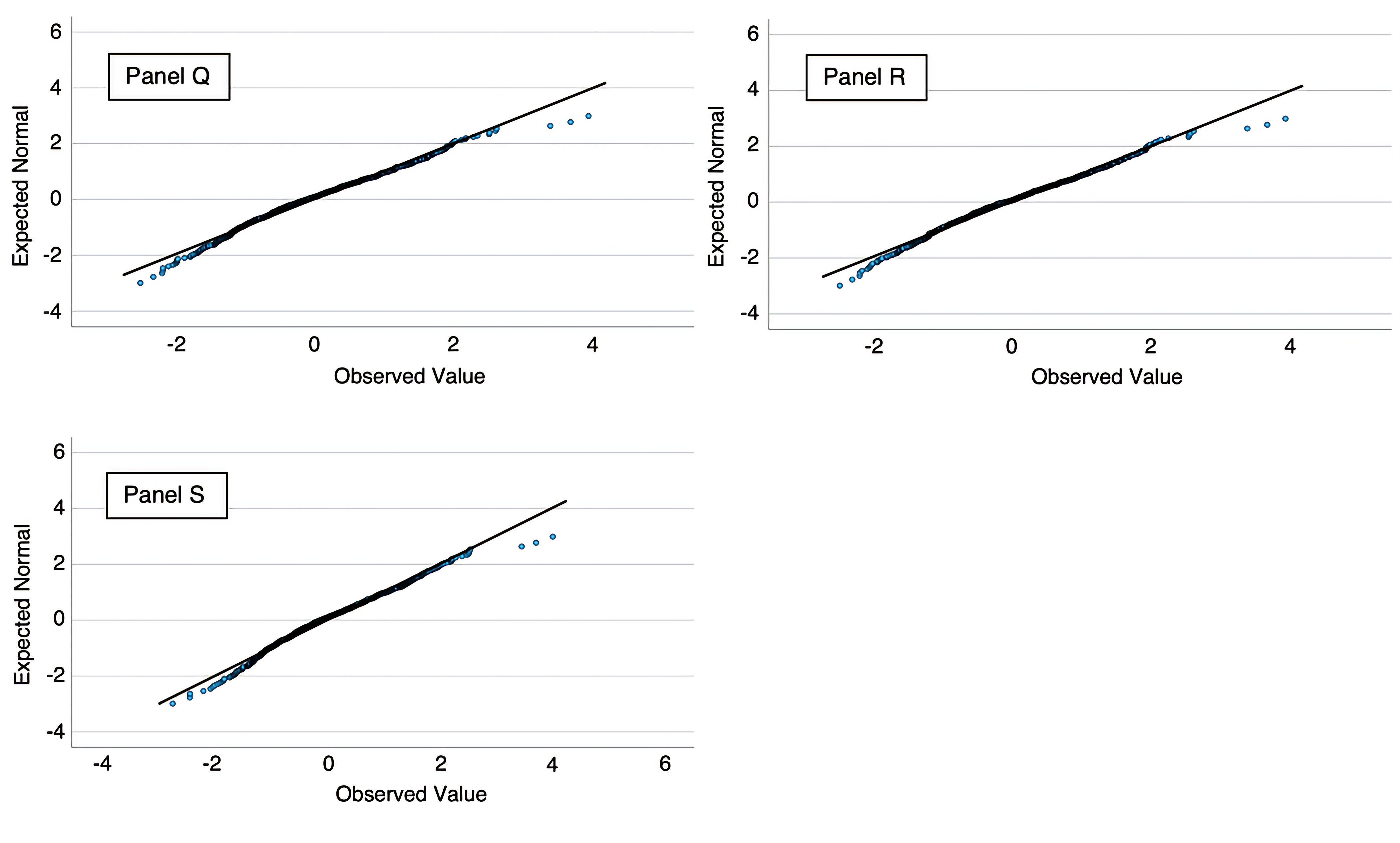
Q–Q plots (quantile–quantile plot)
The Q–Q plots (Figure 3, 4 and 5) indicated approximately normal residuals, and the residual-versus-fitted plots showed no funneling, suggesting no material heteroscedasticity.
Figure 3. Normal Q–Q plots of residuals for ANCOVA models (Panels A–H).
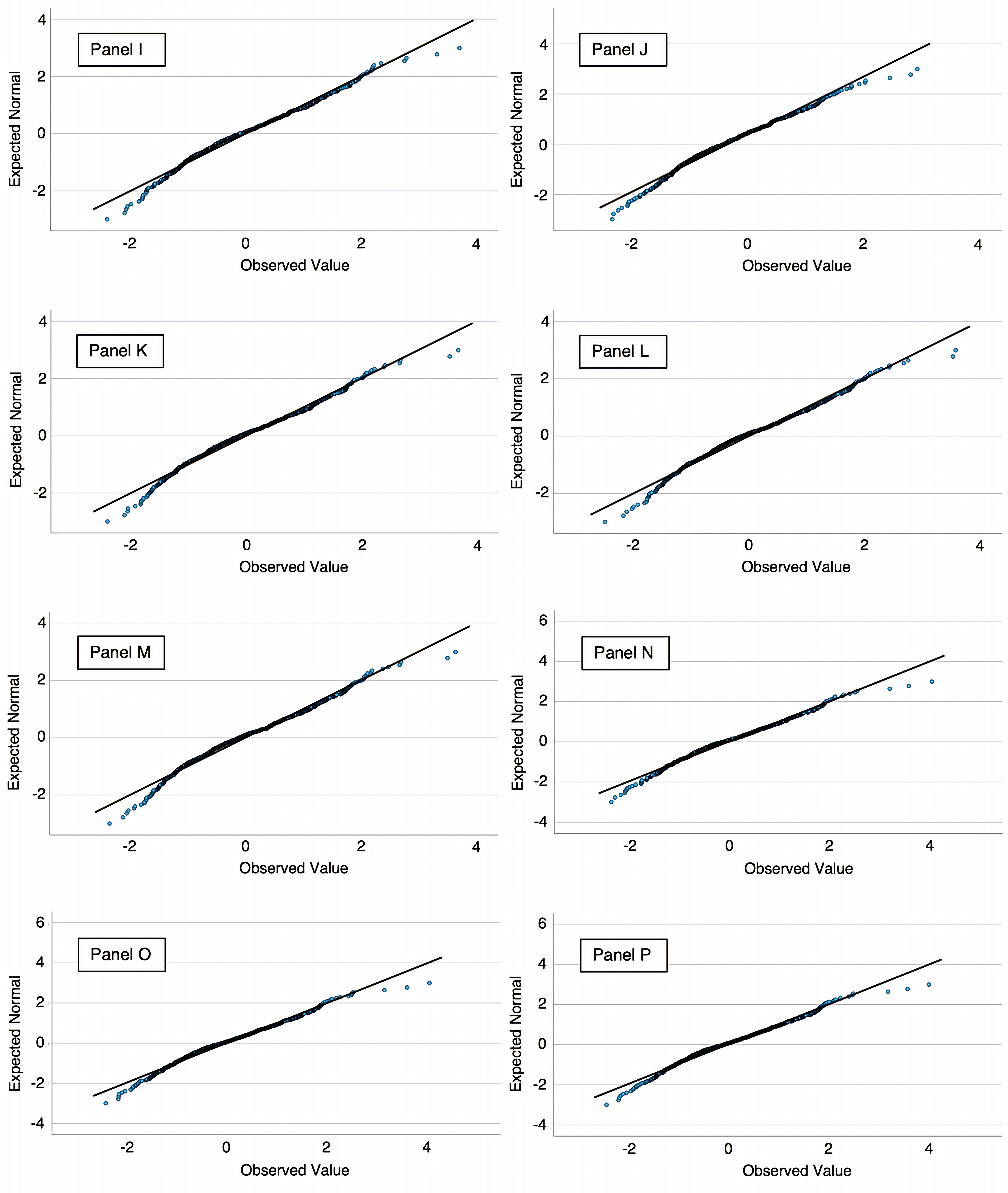
Figure 4. Normal Q–Q plots of residuals for ANCOVA models (Panels I–P).
Figure 5. Normal Q–Q plots of residuals for ANCOVA models (Panels Q–S).
Note on Figures 3-5
Panels: A, six-category model—those who had received education on no, one, two, three, four, or all five steps; B, Step 1—Knowledge: Clinical Questions; C, Step 1—Knowledge: The PICO/PECO Framework; D, Step 1—Skills: How to formulate clinical questions using the PICO/PECO Framework; E, Step 2—Knowledge: Efficient order of evidence searching; F, Step 2—Knowledge: Characteristics and search methods of literature databases; G, Step 2—Knowledge: Characteristics and search methods of databases for clinical practice guidelines and systematic reviews; H, Step 2—Skills: How to search for evidence in an efficient order; I, Step 2—Skills: How to search using literature databases; J, Step 2—Skills: How to search using databases of clinical practice guidelines and systematic review; K, Step 3—Knowledge: Differences in levels of evidence according to research design; L, Step 3—Knowledge: Random and systematic error; M, Step 3—Knowledge: Descriptive and inferential statistics; N, Step 3—Skills: How to critically appraise literature based on knowledge of research designs and levels of evidence; O, Step 3—Skills: How to critically appraise literature based on knowledge of random and systematic error; P, Step 3—Skills: How to critically appraise literature based on knowledge of descriptive and inferential statistics; Q, Step 4—Knowledge: The four components of Step 4; R, Step 4—Skills: How to apply the four components of Step 4 in nursing practice; S, Step 5—Skills: How to evaluate the outcomes of EBP.
Association between the extent of education received across the five steps of EBP and EBP knowledge and skills
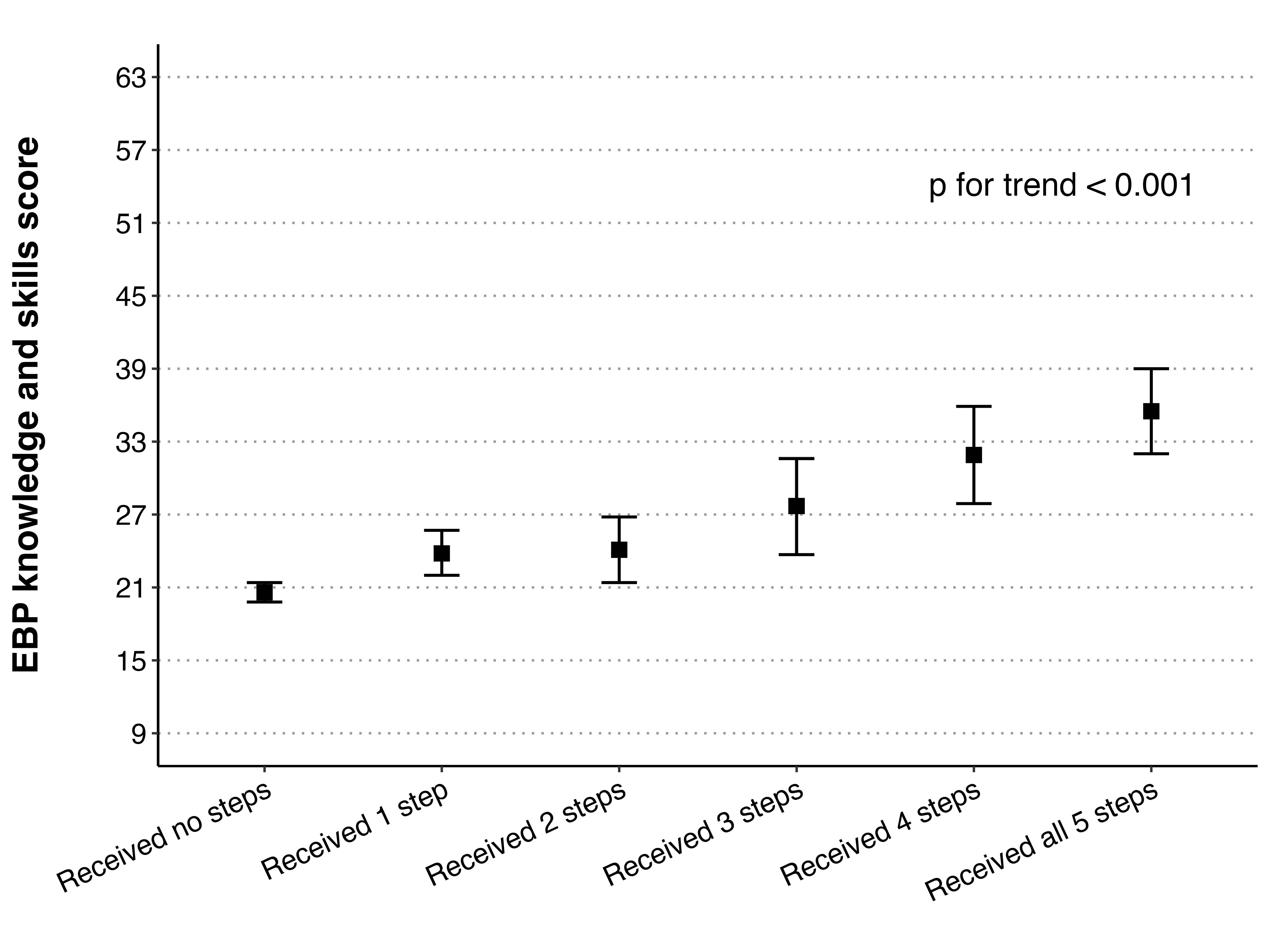
Figure 6 illustrates the association between the extent of received education across the five steps of EBP and EBP knowledge and skills scores.
Figure 6. Association between the extent of received education across the five steps of EBP and EBP knowledge and skills
Note on Figure 6
Adjusted mean scores were estimated using analysis of covariance. Scores were adjusted for gender, educational level, years of clinical nursing experience, employment position, advanced practice certification, number of times conducting research, access to a literature database, and organizational attitude toward EBP. Error bars represent 95% confidence intervals.
EBP, evidence-based practice.
The figure shows the mean score for EBP knowledge and skills increased progressively as the number of EBP steps for which education had been received increased. The lowest scores were observed among nurses who had not received education on any of the steps, whereas the highest scores were observed among those who had received education on all five steps. This trend was statistically significant, indicating a dose–response relationship (p for trend<0.001).
Associations between item-specific experience of receiving EBP education and EBP knowledge and skills
Table 4 shows the associations between item-specific experience of receiving EBP education and EBP knowledge and skills scores. For all EBP-education items, participants who reported receiving more EBP education had significantly higher adjusted mean scores for EBP knowledge and skills. The scores showed a consistent increasing trend across the four response categories, and the linear trend was statistically significant for all EBP-education items (p for trend<0.001).
Adjusted meana (95% CI)
p for trend Effect size: partial η² EBP – Step 1 (Ask) Knowledge: Clinical Questions <0.001 0.09 Have not learned at all 18.5 (17.1–20.0) Have not learned 20.5 (19.1–21.8) Neither 25.3 (23.6–26.9) Have learned b 25.7 (24.3–27.0) Knowledge: The PICO/PECO Framework <0.001 0.12 Have not learned at all 19.1 (17.9–20.3) Have not learned 20.8 (19.6–22.1) Neither 25.6 (23.9–27.4) Have learned b 27.8 (26.3–29.3) Skills: How to formulate clinical questions using the PICO/PECO Framework <0.001 0.12 Have not learned at all 19.2 (18.1–20.3) Have not learned 21.7 (20.5–22.9) Neither 25.5 (23.8–27.2) Have learned b 29.4 (27.5–31.3) EBP – Step 2 (Acquire) Knowledge: Efficient order of evidence searching <0.001 0.10 Have not learned at all 18.6 (17.3–20.0) Have not learned 20.5 (19.2–21.8) Neither 24.7 (23.0–26.3) Have learned b 26.4 (25.1–27.7) Knowledge: Characteristics and search methods of literature databases c <0.001 0.07 Have not learned at all 16.5 (14.7–18.4) Have not learned 20.4 (18.7–22.0) Neither 24.5 (22.5–26.4) Have learned b 24.4 (23.3–25.4) Knowledge: Characteristics and search methods of databases for clinical practice guidelines and systematic reviewsd <0.001 0.14 Have not learned at all 19.1 (18.0–20.2) Have not learned 21.9 (20.6–23.2) Neither 24.8 (23.3–26.3) Have learned b 31.1 (29.1–33.1) Skills: How to search for evidence in an efficient order <0.001 0.10 Have not learned at all 19.1 (17.9–20.3) Have not learned 21.3 (20.0–22.6) Neither 24.5 (22.9–26.0) Have learned b 27.9 (26.3–29.5) Skills: How to search using literature databasesc <0.001 0.08 Have not learned at all 17.1 (15.4–18.7) Have not learned 20.3 (18.6–22.1) Neither 23.1 (21.2–25.0) Have learned b 25.0 (24.0–26.0) Skills: How to search using databases for clinical practice guidelines and systematic reviewsd <0.001 0.11 Have not learned at all 19.2 (18.1–20.3) Have not learned 22.1 (20.8–23.4) Neither 25.0 (23.5–26.6) Have learned b 29.1 (27.1–31.0) EBP – Step 3 (Appraise) Knowledge: Differences in levels of evidence according to research design <0.001 0.07 Have not learned at all 18.5 (17.1–19.9) Have not learned 21.1 (19.6–22.6) Neither 24.3 (22.7–26.0) Have learned b 25.5 (24.2–26.8) Knowledge: Random and systematic error <0.001 0.07 Have not learned at all 18.5 (17.2–19.9) Have not learned 22.2 (20.7–23.6) Neither 24.9 (23.2–26.6) Have learned b 25.3 (23.9–26.7) Knowledge: Descriptive and inferential statistics <0.001 0.06 Have not learned at all 18.7 (17.3–20.1) Have not learned 21.5 (20.0–23.0) Neither 24.4 (22.8–26.0) Have learned b 25.3 (24.0–26.7) Skills: How to critically appraise literature based on knowledge of research designs and levels of evidence <0.001 0.09 Have not learned at all 18.3 (17.0–19.7) Have not learned 21.0 (19.5–22.5) Neither 23.9 (22.4–25.4) Have learned b 26.9 (25.4–28.3) Skills: How to critically appraise literature based on knowledge of random and systematic error <0.001 0.10 Have not learned at all 18.6 (17.3–19.8) Have not learned 21.8 (20.5–23.1) Neither 24.2 (22.7–25.7) Have learned b 28.0 (26.3–29.7) Skills: How to critically appraise literature based on knowledge of descriptive and inferential statistics <0.001 0.10 Have not learned at all 18.8 (17.5–20.1) Have not learned 21.2 (19.9–22.6) Neither 24.2 (22.7–25.6) Have learned b 28.1 (26.4–29.7) EBP – Step 4 (Apply) Knowledge: The four components of Step 4e <0.001 0.12 Have not learned at all 18.5 (17.2–19.8) Have not learned 20.7 (19.4–22.0) Neither 24.6 (23.1–26.0) Have learned b 28.2 (26.6–29.7) Skills: How to apply the four components of Step 4 in nursing practicee <0.001 0.12 Have not learned at all 18.4 (17.2–19.7) Have not learned 21.1 (19.8–22.4) Neither 24.6 (23.2–26.1) Have learned b 27.9 (26.3–29.5) EBP – Step 5 (Assess) Skills: How to evaluate the outcomes of EBP <0.001 0.15 Have not learned at all 18.5 (17.3–19.6) Have not learned 21.8 (20.5–23.1) Neither 24.9 (23.5–26.4) Have learned b 30.4 (28.6–32.3) Note: a Adjusted mean scores were estimated using analysis of covariance. Scores were adjusted for gender, educational level, years of clinical nursing experience, employment position, advanced practice certification, number of times conducting research, access to a literature database, and organizational attitude toward EBP.
b The responses “Have learned” and “Have learned a lot” were combined into a single category labeled “Have learned.” For each EBP-education item, the level of educational experience was determined based on responses for both pre-licensure and in-service education. When participants reported different levels of experience across the two educational settings, the higher of the two was retained, following the rank order: “Have not learned at all” < “Have not learned” < “Neither” < “Have learned.”
c Literature databases refer to resources such as PubMed and Ichushi Web, a bibliographic database indexing primarily Japanese-language literature on medicine, nursing, dentistry, and pharmacy.
d Databases for clinical practice guidelines and systematic reviews refer to resources such as the Minds Guideline Library, a database for domestic clinical practice guidelines published in Japan, and the Cochrane Library.
e The four components are as follows: (1) the patient’s clinical state and circumstances, (2) research evidence, (3) the patient’s preferences and actions, and (4) clinical expertise.
CI: confidence interval; EBP: evidence-based practice; PECO: Patient, Exposure, Comparison, Outcome; PICO: Patient, Intervention, Comparison, Outcome.
Table 4. Associations between item-specific experience of receiving EBP education and EBP knowledge and skills (n=718).
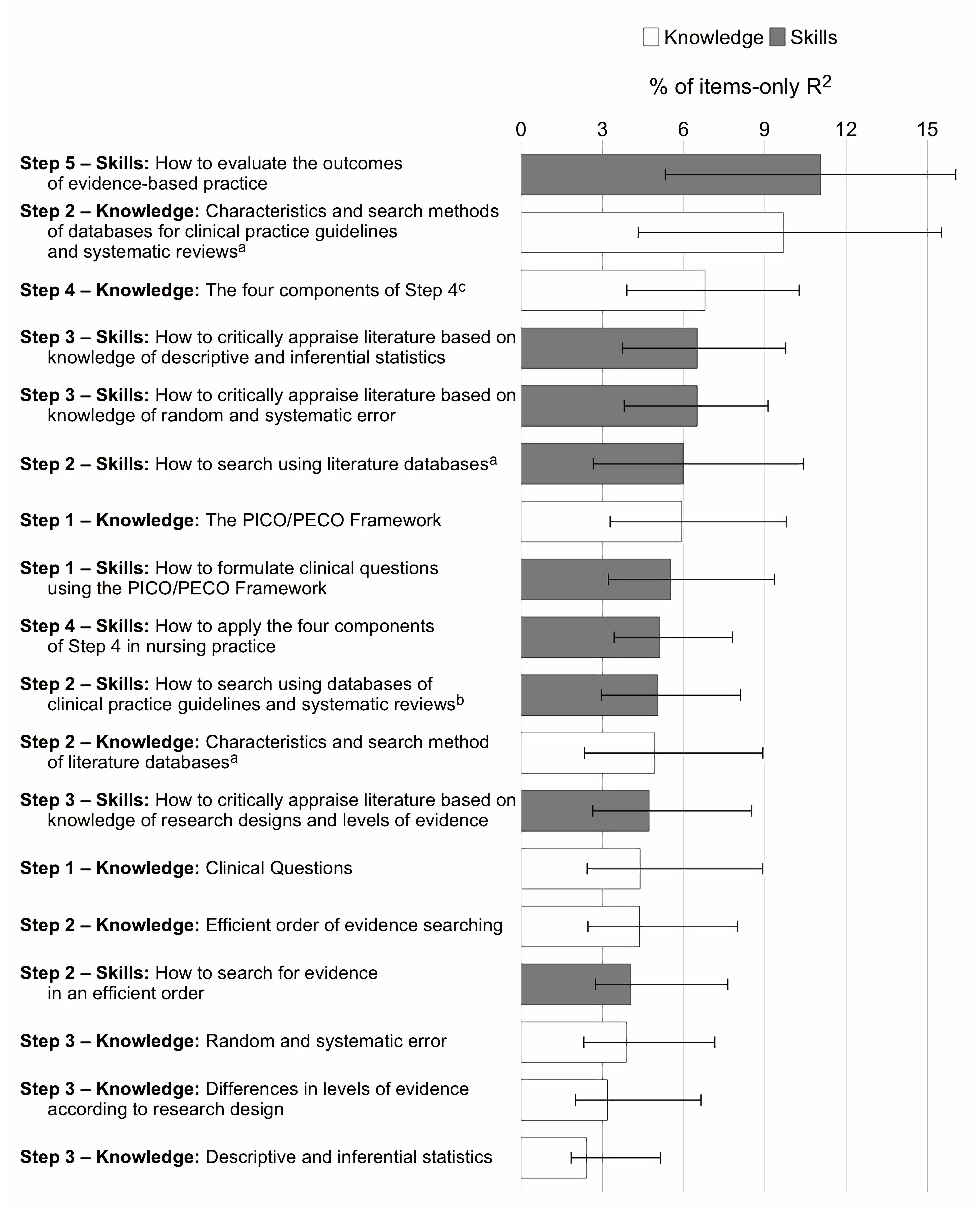
Relative importance of EBP-education items for the EBP knowledge and skills
Figure 7 illustrates the relative importance of EBP-education items for the EBP knowledge and skills score.
Figure 7. Relative importance of EBP-education items for the EBP knowledge and skills score.
Note on Figure 7
Bars show the % of EBP education items-only R² contributed by each item, computed using the Lindeman–Merenda–Gold method; error bars are bootstrapped 95% confidence intervals. R²=0.338; adjusted R²=0.270; EBP education items-only R²=0.217. The model included EBP-education items, gender, educational level, years of experience as a clinical nurse, employment position, advanced practice certification, number of experiences conducting research, literature database, and organizational attitude toward EBP.
a Literature databases refer to resources such as PubMed and Ichushi Web, a bibliographic database indexing primarily Japanese-language literature on medicine, nursing, dentistry, and pharmacy.
b Databases for clinical practice guidelines and systematic reviews refer to resources such as the Minds Guideline Library, a database for domestic clinical practice guidelines published in Japan, and the Cochrane Library.
c The four components are as follows: (1) the patient’s clinical state and circumstances, (2) research evidence, (3) the patient’s preferences and actions, and (4) clinical expertise.
EBP, evidence-based practice, PECO, Patient, Exposure, Comparison, Outcome; PICO, Patient, Intervention, Comparison, Outcome.
Ranked by relative importance, the three items accounting for the largest proportion of explained variance were Step 5—Skills (evaluating EBP outcomes), Step 2—Knowledge (characteristics and search methods of databases for clinical practice guidelines and systematic reviews), and Step 4—Knowledge (the four components of Step 4).
Table 5 shows detailed results for the same linear regression model, including unstandardized coefficients, standard errors, p-values, and the change-in-R² (ΔR²) and partial F (ΔF) statistics for all variables.
Factors Reference B (SE) p-value for B ΔR² ΔF p-value for ΔF Experience of receiving EBP education Step 1 (Ask) Knowledge: Clinical Questions 0.002 0.788 0.501 Have not learned vs have not learned at all 0.134 (1.388) 0.923 Neither vs have not learned at all 1.537 (1.698) 0.366 Have learned b vs have not learned at all −0.550 (1.580) 0.728 Knowledge: The PICO/PECO Framework 0.001 0.434 0.729 Have not learned vs have not learned at all −0.868 (2.001) 0.665 Neither vs have not learned at all 1.066 (2.569) 0.678 Have learned b vs have not learned at all 0.981 (2.541) 0.700 Skills: How to formulate clinical questions using the PICO/PECO Framework 0.001 0.316 0.814 Have not learned vs have not learned at all 0.869 (1.991) 0.663 Neither vs have not learned at all −0.061 (2.572) 0.981 Have learned b vs have not learned at all 1.561 (2.668) 0.559 Step 2 (Acquire) Knowledge: Efficient order of evidence searching 0.001 0.457 0.712 Have not learned vs have not learned at all −0.983 (1.418) 0.489 Neither vs have not learned at all 0.700 (1.742) 0.688 Have learned b vs have not learned at all −0.285 (1.630) 0.861 Knowledge: Characteristics and search methods of literature databases c 0.006 1.806 0.145 Have not learned vs have not learned at all 2.983 (1.721) 0.084 Neither vs have not learned at all 3.361 (2.181) 0.124 Have learned b vs have not learned at all 1.291 (1.862) 0.488 Knowledge: Characteristics and search methods of databases for clinical practice guidelines and systematic reviews d 0.007 2.450 0.063 Have not learned vs have not learned at all 0.126 (1.712) 0.941 Neither vs have not learned at all 0.161 (2.044) 0.937 Have learnedb vs have not learned at all 5.267 (2.362) 0.026 Skills: How to search for evidence in an efficient order 0.002 0.622 0.601 Have not learned vs have not learned at all −1.987 (1.546) 0.199 Neither vs have not learned at all −2.202 (1.974) 0.265 Have learned b vs have not learned at all −1.849 (1.936) 0.340 Skills: How to search using literature databases c 0.005 1.553 0.200 Have not learned vs have not learned at all 0.170 (1.801) 0.925 Neither vs have not learned at all 0.507 (2.071) 0.807 Have learned b vs have not learned at all 2.977 (1.820) 0.102 Skills: How to search using databases for clinical practice guidelines and systematic reviews d 0.003 0.920 0.431 Have not learned vs have not learned at all 2.449 (1.877) 0.192 Neither vs have not learned at all 2.042 (2.235) 0.361 Have learned b vs have not learned at all −0.141 (2.382) 0.953 Step 3 (Appraise) Knowledge: Differences in levels of evidence according to research design 0.002 0.687 0.560 Have not learned vs have not learned at all −1.849 (1.875) 0.324 Neither vs have not learned at all −2.001 (2.234) 0.371 Have learned b vs have not learned at all −0.229 (1.980) 0.908 Knowledge: Random and systematic error 0.003 1.088 0.354 Have not learned vs have not learned at all 2.687 (2.142) 0.210 Neither vs have not learned at all 2.707 (2.698) 0.316 Have learned b vs have not learned at all 0.051 (2.387) 0.983 Knowledge: Descriptive and inferential statistics 0.0003 0.110 0.954 Have not learned vs have not learned at all −1.099 (2.165) 0.612 Neither vs have not learned at all −0.453 (2.457) 0.854 Have learned b vs have not learned at all −0.272 (2.189) 0.901 Skills: How to critically appraise literature based on knowledge of research designs and levels of evidence 0.002 0.609 0.609 Have not learned vs have not learned at all 0.132 (2.120) 0.950 Neither vs have not learned at all 1.613 (2.322) 0.487 Have learned b vs have not learned at all 2.325 (2.262) 0.304 Skills: How to critically appraise literature based on knowledge of random and systematic error 0.008 2.664 0.047 Have not learned vs have not learned at all 8.249 (3.581) 0.022 Neither vs have not learned at all −2.465 (4.695) 0.600 Have learned b vs have not learned at all 2.502 (4.050) 0.537 Skills: How to critically appraise literature based on knowledge of descriptive and inferential statistics 0.007 2.342 0.072 Have not learned vs have not learned at all −8.528 (3.629) 0.019 Neither vs have not learned at all 0.019 (4.635) 0.997 Have learned b vs have not learned at all −2.651 (3.863) 0.493 Step 4 (Apply) Knowledge: The four components of Step 4 e 0.002 0.532 0.660 Have not learned vs have not learned at all −0.384 (2.540) 0.880 Neither vs have not learned at all 1.302 (3.083) 0.673 Have learned b vs have not learned at all 2.645 (3.052) 0.387 Skills: How to apply the four components of Step 4 in nursing practicee 0.0005 0.162 0.922 Have not learned vs have not learned at all −0.611 (2.588) 0.814 Neither vs have not learned at all −0.356 (3.182) 0.911 Have learnedb vs have not learned at all −1.695 (3.115) 0.587 Step 5 (Assess) Skills: How to evaluate the outcomes of EBP 0.009 2.948 0.032 Have not learned vs have not learned at all 2.054 (1.560) 0.188 Neither vs have not learned at all 2.006 (1.771) 0.258 Have learned b vs have not learned at all 5.608 (1.960) 0.004 Potential confounding factors Gender 0.001 1.448 0.229 Men vs women 1.584 (1.316) 0.229 Educational level 0.016 8.043 <0.001 Bachelor’s degree vs diploma or associate degree −0.158 (0.932) 0.865 Master’s degree vs diploma or associate degree 7.161 (1.869) <0.001 Years of clinical nursing experience 0.001 0.266 0.766 4–9 vs ≤3 −0.16 (1.079) 0.882 ≥10 vs ≤3 −0.757 (1.129) 0.503 Employment position 0.001 0.607 0.436 Charge nurse or assistant head nurse vs staff nurse 1.006 (1.292) 0.436 Advanced practice certification 0.003 2.475 0.116 Certified nurse or certified specialist nurse vs no 3.073 (1.953) 0.116 Number of times conducting research 0.013 6.433 0.002 1 vs 0 1.893 (1.001) 0.059 ≥2 vs 0 3.698 (1.032) <0.001 Literature database 0.001 0.628 0.428 Yes vs no 1.405 (1.773) 0.428 Organizational attitude toward EBP 0.002 0.581 0.628 Neither vs non-positive −0.921 (1.232) 0.455 Moderately positive vs non-positive −0.305 (1.179) 0.796 Very positive vs non-positive 0.388 (1.280) 0.762 Note: These results are from the same model used for the relative-importance analysis in Figure 7.
Dummy variables coded 0 for “have not learned at all”/ 1 for “have not learned”/ 2 for “neither”/ 3 for “have learned” (EBP education items); 0 for women/1 for men (gender); 0 for diploma or associate degree/1 for bachelor’s degree/2 for master’s degree (educational level); 0 for “≤3”/1 for “4–9”/2 for “≥10” (years of clinical nursing experience); 0 for staff nurse/1 for charge nurse and assistant head nurse (employment position); 0 for “no”/1 for certified nurse or certified specialist nurse (advanced practice certification); 0 for “0”/1 for “1”/2 for “≥2” (number of times conducting research); 0 for “no”/1 for “yes” (literature database); and 0 for non-positive/1 for neither /2 for moderately positive /3 for very positive (organizational attitude toward EBP).
R²=0.338; adjusted R²=0.270; EBP education items-only R²=0.217.
a EBP knowledge and skills measured by the Evidence-Based Practice Questionnaire Japanese version. EBP knowledge and skills score ranges from 9 to 63, with higher scores indicating more EBP knowledge and skills.
b The responses “Have learned” and “Have learned a lot” were combined into a single category labeled “Have learned.” For each EBP-education item, the level of educational experience was determined based on responses for both pre-licensure and in-service education. When participants reported different levels of experience across the two educational settings, the higher of the two was retained, following the rank order: “Have not learned at all” < “Have not learned” < “Neither” < “Have learned.”
c Literature databases refer to resources such as PubMed and Ichushi Web, a bibliographic database indexing primarily Japanese-language literature on medicine, nursing, dentistry, and pharmacy.
d Databases for clinical practice guidelines and systematic reviews refer to resources such as the Minds Guideline Library, a database for domestic clinical practice guidelines published in Japan, and the Cochrane Library.
e The four components are as follows: (1) the patient’s clinical state and circumstances, (2) research evidence, (3) the patient’s preferences and actions, and (4) clinical expertise.
B: unstandardized coefficients; CI: confidence interval; EBP: evidence-based practice; PECO: Patient, Exposure, Comparison, Outcome; PICO: Patient, Intervention, Comparison, Outcome; SE: standard error; ΔR²: increase in R-squared attributable to adding the variable to a model that already contains all other variables; i.e., the variable’s semi-partial R² (unique contribution); ΔF: partial F statistic for adding the variable to the model.
Table 5. Regression results for the EBP knowledge and skills score a, including all variables.
DISCUSSION
This study investigated the extent of Japanese hospital nurses’ experience of receiving specific educational content related to each step of EBP in both pre-licensure and in-service education and examined its association with EBP knowledge and skills. The findings showed that the experience of receiving EBP education was limited overall, with even lower levels observed for skills-related items. In both pre-licensure and in-service education, fewer than 10% of nurses reported having learned how to formulate clinical questions using the PICO/PECO framework, characteristics and search methods of databases for clinical practice guidelines and systematic reviews, how to search using databases for clinical practice guidelines and systematic reviews, and how to evaluate the outcomes of EBP. Additionally, a statistically significant dose-response relationship was observed between the extent of education received across the five EBP steps and the level of EBP knowledge and skills. Furthermore, in all EBP-education items, higher item-specific experience of receiving EBP education was significantly associated with greater EBP knowledge and skills scores. Furthermore, relative importance analysis showed three leading contributors. These were Step 5—Skills (evaluating EBP outcomes), Step 2—Knowledge (characteristics and search methods of databases for clinical practice guidelines and systematic reviews), and Step 4—Knowledge (the four components of Step 4). These findings suggest that comprehensive exposure to EBP education may play a critical role in developing EBP competencies. Additionally, the observed dose–response between the extent of experience of EBP education and knowledge/skills aligns with Kirkpatrick Level 2 (Learning)—i.e., greater educational coverage is associated with stronger learning outcomes [16]. While our endpoints were confined to Level 2, the model indicates that strengthened learning can support subsequent behavior (Level 3) and results (Level 4). Thus, future studies should extend the evaluation to Levels 3 and 4.
Our findings indicated that nurses’ experience of receiving EBP education was generally limited. Except for items related to literature databases, fewer than 25% of nurses reported having learned about any of the EBP-education items in pre-licensure education. The percentage of nurses who had learned about each EBP-education item in in-service education was consistently below 25%. Although EBP education has been insufficiently embedded in both pre-licensure and in-service curricula in Japan [31,32], such limited exposure is not unique to Japan. Recent reviews have reported that, worldwide, many nurses have never received EBP education [12] and that the overall level of EBP knowledge and skills among nurses remains low [33]. These findings highlight the urgent global need to improve EBP education. However, both pre-licensure and in-service education settings lack sufficient educators capable of providing EBP education [8, 34]. This shortage is likely a major contributor to nurses having limited experience in receiving EBP education. Therefore, developing and implementing training programs to equip educators with the competencies needed to provide EBP education is important. In so doing, the infrastructure for teaching EBP could be strengthened, and EBP implementation in nursing practice can be promoted.
In the present study, a stepwise increase in EBP knowledge and skills scores was observed as the number of EBP steps for which education had been received increased, indicating an association between the comprehensiveness of the EBP education and competency level. Additionally, the item-specific experience of receiving EBP education was positively associated with EBP knowledge and skills scores across all EBP-education items, and a relative importance analysis indicated that the Step 4 and Step 5 items were placed toward the upper end of the contribution rankings. These findings provide quantitative evidence that supports the argument that education encompassing all five steps of EBP is important to improve EBP knowledge and skills [35]. One systematic review has indicated that EBP educational programs tend to focus solely on Steps 1 to 3 of the five steps of EBP [36]. Therefore, future EBP education programs must comprehensively incorporate all five steps rather than only focus on specific ones. At the same time, in the present study, even among nurses who had received education on all five steps, the mean EBP knowledge and skills score was 35.5 on a scale ranging from 9 to 63, indicating that their competency levels remained insufficient. This suggests that to develop EBP competencies, both an adequate extent of educational content and appropriate educational delivery methods are required. In other words, providing practical education programs focused on EBP could be necessary to improve EBP competency levels among nurses effectively. However, EBP education is often integrated into broader courses, such as nursing research or statistics, and is rarely offered as a stand-alone program [8, 9, 10, 11]. Therefore, developing practical, EBP-specific educational programs would be essential to improve nurses’ EBP knowledge and skills effectively.
Limitations
This study had several limitations. First, because of the cross-sectional design, a causal association between the experience of receiving EBP education and EBP knowledge and skills cannot be established; however, a statistically significant trend was observed in which EBP knowledge and skills scores increased with the amount of EBP education received, as indicated by the p for trend. This finding serves as additional evidence supporting a dose-response relationship between the two. Second, because the response rate was 28.7%, we must include the possibility of selection bias in which people with relatively more interest in EBP were selected. Third, the study relied on self-reported participant experience with EBP education, which may have introduced recall bias. To obtain a more objective understanding of EBP education’s current status, future research should directly investigate institutions such as universities, vocational schools, and healthcare facilities by examining their course offerings, content, and number of instructional hours. Fourth, because our survey data were collected in 2022 (June–September), the findings may not fully reflect the current landscape of EBP education. However, the first explicit mention of EBP in Japan’s pre-licensure education was included in the Model Core Curriculum for Nursing Education (2024 revision) in March 2025 [37]; as this reform will chiefly affect future cohorts, any immediate influence on the educational exposure of the current hospital nursing workforce is likely modest. Finally, this study was conducted in Japan, where EBP education has not been fully promoted. This geographic specificity means that comparisons with findings from countries having more advanced EBP education should be made with caution. Despite this, the results may offer valuable insights, particularly for countries where EBP education is still in its early stages of promotion.
CONCLUSION
We investigated the extent to which hospital nurses in Japan had experienced receiving specific educational content related to each step of EBP in both pre-licensure and in-service education; we also examined its association with EBP knowledge and skills. Fewer than 25% of nurses reported having learned about any of the EBP-education items except for characteristics and search methods of literature databases in pre-licensure education, and fewer than 25% reported having learned about each EBP-education item in in-service education. A dose–response relationship was observed between the number of EBP steps for which education was received and the level of EBP competency. Additionally, the item-specific experience of receiving EBP education was positively associated with EBP knowledge and skills scores across all EBP-education items, and a relative importance analysis indicated that the Step 4 and Step 5 items were placed toward the upper end of the contribution rankings. In the future, to effectively improve the EBP knowledge and skills of nurses, it would be essential to: (1) design educational programs that comprehensively cover all five steps rather than only placing focus on specific steps; (2) develop practical, EBP-specific educational programs; and (3) develop educational programs that enable EBP educators to cultivate professionals capable of delivering such education.
List of abbreviations
EBP: evidence-based practice
PICO: Patient, Intervention, Comparison, Outcome
PECO: Patient, Exposure, Comparison, Outcome
Competing interest
The authors declare that they have no competing financial interests or personal relationships that may have influenced the work reported in this study.
Funding sources
No external funding.
Author contributions
All authors listed meet the authorship criteria according to the guidelines of the International Committee of Medical Journal Editors and agree with the manuscript. Hideaki Furuki: Conceptualization, Methodology, Formal analysis, Investigation, Data curation, Visualization, writing – original draft, writing – review, and editing, and project administration. Nao Sonoda: Conceptualization, Methodology, Formal analysis, Investigation, Data curation, Visualization, writing-review and editing, and project administration. Akiko Morimoto: Conceptualization, Methodology, Formal analysis, Investigation, Data curation, Visualization, writing – review and editing, project administration.
Acknowledgments
We are grateful to all the participants who participated in this study. We thank Miwa Fukumitsu, Haruna Sakamoto, and Risa Koike for their contributions to this study.
REFERENCES
- Melnyk BM, Fineout-Overholt E, Stillwell SB, Williamson KM. Evidence-based practice: Step by step: The seven steps of evidence-based practice. Am J Nurs. 2010;110(1):51–53. doi:10.1097/01.NAJ.0000366056.06605.d2
- Connor L, Dean J, McNett M, Tydings DM, Shrout A, Gorsuch PF, et al. Evidence-based practice improves patient outcomes and healthcare system return on investment: Findings from a scoping review. Worldviews Evid Based Nurs. 2023;20:6–15. doi:10.1111/wvn.12621
- Melnyk BM, Fineout-Overholt E, Giggleman M, Choy K. A test of the ARCC model improves implementation of evidence-based practice, healthcare culture, and patient outcomes. Worldviews Evid Based Nurs. 2017;14(1):5–9. doi:10.1111/wvn.12188
- Wu Y, Brettle A, Zhou C, Ou J, Wang Y, Wang S. Do educational interventions aimed at nurses to support the implementation of evidence-based practice improve patient outcomes? A systematic review. Nurse Educ Today. 2018;70:109–114. doi:10.1016/j.nedt.2018.08.026
- Knežević D, Jović D, Petković M. The impact of introducing a nursing education protocol on the incidence of Clostridium difficile infections in the hospital environment: A quasi-experimental study. NSC Nursing. 2023;2(4):62–84. doi:10.32549/OPI-NSC-89.
- American Association of Colleges of Nursing. The Essentials: Core Competencies for Professional Nursing Education. Washington (DC): AACN; 2021. [Internet]. Available from: https://www.aacnnursing.org/Portals/0/PDFs/Publications/Essentials-2021.pdf (Accessed: September 6, 2025).
- American Nurses Association. Nursing: Scope and Standards of Practice. 4th ed. Silver Spring (MD): American Nurses Association; 2021.
- Hung HY, Huang YF, Tsai JJ, Chang YJ. Current state of evidence-based practice education for undergraduate nursing students in Taiwan: A questionnaire study. Nurse Educ Today. 2015;35:1262–1267. doi:10.1016/j.nedt.2015.05.001
- Malik G, McKenna L, Griffiths D. An analysis of evidence-based practice curriculum integration in Australian undergraduate nursing programs. GSTF J Nurs Health Care. 2015;3(1):158–164. doi:10.7603/s40743-015-0029-z
- Skela-Savič B, Gotlib J, Panczyk M, Patelarou AE, Bole U, Ramos-Morcillo AJ, et al. Teaching evidence-based practice (EBP) in nursing curricula in six European countries – A descriptive study. Nurse Educ Today. 2020;94:104561. doi:10.1016/j.nedt.2020.104561
- Song CE, Kim WG, Lim YJ. An analysis of evidence-based practice courses in Korean nursing education systems. 2019;5(10):e02650. doi:10.1016/j.heliyon.2019.e02650
- Furuki H, Sonoda N, Morimoto A. Factors related to the knowledge and skills of evidence-based practice among nurses worldwide: A scoping review. Worldviews Evid Based Nurs. 2023;20:16–26. doi:10.1111/wvn.12623
- Alqahtani N, Oh KM, Kitsantas P, Rodan M. Nurses’ evidence-based practice knowledge, attitudes and implementation: A cross-sectional study. J Clin Nurs. 2020;29(1–2):274–283. doi:10.1111/jocn.15097
- Filippini A, Sessa A, Di Giuseppe G, Angelillo IF. Evidence-based practice among nurses in Italy. Eval Health Prof. 2011;34(3):371–382. doi:10.1177/0163278710387924
- Tomotaki A, Fukahori H, Sakai I. Exploring sociodemographic factors related to practice, attitude, knowledge, and skills concerning evidence-based practice in clinical nursing. Jpn J Nurs Sci. 2020;17(1):e12260. doi:10.1111/jjns.12260
- Kirkpatrick JD, & Kirkpatrick WK. Kirkpatrick’s four levels of training evaluation. Alexandria: ATD Press; 2016.
- Ministry of Education, Culture, Sports, Science and Technology; Ministry of Health, Labour and Welfare; Ministry of Economy, Trade and Industry. Ethical guidelines for medical and biological research involving human subjects. 2024. Japanese. [Internet]. Available from: https://www.lifescience.mext.go.jp/files/pdf/n2181_01.pdf (Accessed: September 6, 2025).
- Furuki H, Sonoda N, Morimoto A. Relationship between evidence-based practice knowledge and skills and evidence-based practice implementation in subgroups of professional and work environment factors among hospital nurses: A cross-sectional study. Jpn J Nurs Sci. 2025;22(4):e70018. doi:10.1111/jjns.70018
- Tomotaki A, Fukahori H, Sakai I, Kurokohchi K. The development and validation of the Evidence-Based Practice Questionnaire: Japanese version. Int J Nurs Pract. 2018;24(2):e12617. doi:10.1111/ijn.12617
- Leung K, Trevena L, Waters D. Systematic review of instruments for measuring nurses’ knowledge, skills and attitudes for evidence-based practice. J Adv Nurs. 2014;70:2181–2195. doi:10.1111/jan.12454
- Upton D, Upton P. Development of an evidence-based practice questionnaire for nurses. J Adv Nurs. 2006;53(4):454–458. doi:10.1111/j.1365-2648.2006.03739.x
- International Council of Nurses. Guidelines on Advanced Practice Nursing 2020. Geneva: International Council of Nurses; 2020. Available from: https://www.icn.ch/resources/publications-and-reports/guidelines-advanced-practice-nursing-2020 (Accessed: September 6, 2025).
- Guyatt G, Rennie D, Meade MO, Cook DJ, editors. Users’ Guides to the Medical Literature: A Manual for Evidence-Based Clinical Practice. 3rd ed. New York: McGraw-Hill Education; 2015.
- Melnyk BM, Fineout-Overholt E. Evidence-based Practice in Nursing & Healthcare: A Guide to Best Practice. 5th ed. Philadelphia: Wolters Kluwer; 2023.
- Straus SE, Glasziou P, Richardson WS, Haynes RB. Evidence-Based Medicine: How to Practice and Teach EBM. 5th ed. Edinburgh: Elsevier; 2018.
- Albarqouni L, Hoffmann T, Straus S, Olsen NR, Young T, Ilic D, et al. Core competencies in evidence-based practice for health professionals: Consensus statement based on a systematic review and Delphi survey. JAMA Netw Open. 2018;1:e180281. doi:10.1001/jamanetworkopen.2018.0281
- Groemping U. Relative importance for linear regression in R: The package relaimpo. J Stat Softw. 2006;17(1):1–27. doi:10.18637/jss.v017.i01
- Groemping U. relimpo: Relative Importance of Regressors in Linear Models. Version 2.2-7; 2023. [Internet]. Available from: https://cran.r-project.org/web/packages/relaimpo/relaimpo.pdf (Accessed: September 6, 2025).
- Bi J. A review of statistical methods for determination of relative importance of correlated predictors and identification of drivers of consumer liking. J Sens Stud. 2012;27(2):87–101. doi:10.1111/j.1745-459X.2012.00370.x
- Tonidandel S, LeBreton JM. Relative importance analysis: A useful supplement to regression analysis. J Bus Psychol. 2011;26(1):1–9. doi:10.1007/s10869-010-9204-3
- Ministry of Education, Culture, Sports, Science and Technology. Model Core Curriculum for Nursing Education (2024 Revised Edition). 2025. Japanese. [Internet]. Available from: https://www.mext.go.jp/a_menu/koutou/iryou/mext_00021.html (Accessed: October 22, 2025).
- Tomotaki A, Sakai I, Fukahori H, Tsuda Y, Okumura-Hiroshige A. Factors affecting the critical appraisal of research articles in Evidence-Based practices by advanced practice nurses: A descriptive qualitative study. Nurs Open. 2023;10(6):3719-3727. doi:10.1002/nop2.1628
- Li H, Xu R, Gao D, Fu H, Yang Q, Chen X, et al. Evidence-based practice attitudes, knowledge and skills of nursing students and nurses: A systematic review and meta-analysis. Nurse Educ Pract. 2024;78:104024. doi:10.1016/j.nepr.2024.104024
- Abu-Odah H, Said NB, Nair SC, Allsop MJ, Currow DC, Salah MS, et al. Identifying barriers and facilitators of translating research evidence into clinical practice: A systematic review of reviews. Health Soc Care Community. 2022;30:e3265–e3276. doi:10.1111/hsc.13898
- Stevens KR. The impact of evidence-based practice in nursing and the next big ideas. Online J Issues Nurs. 2013;18(2):4.
- Albarqouni L, Hoffmann T, Glasziou P. Evidence-based practice educational intervention studies: A systematic review of what is taught and how it is measured. BMC Med Educ. 2018;18(1):177. doi:10.1186/s12909-018-1284-1
- Ministry of Education, Culture, Sports, Science and Technology. Model Core Curriculum for Nursing Education (2024 Revised Edition). 2025. Japanese. [Internet]. Available from: https://www.mext.go.jp/a_menu/koutou/iryou/mext_00021.html (Accessed: October 12, 2025).
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.